Relationship between Resilience and Quality of Life in Patients with Fear of Hypoglycemia: The Mediating Effects of Anxiety and Depression
Abstract
1. Introduction
2. Background
3. The Study
Aims
4. Method
4.1. Design
4.2. Participants
4.3. Data Collection
4.4. Measures
4.5. Ethical Considerations
5. Results
5.1. Data Analyses
5.2. Socio-Demographic and Clinical Characteristics of the Participants
5.3. Descriptive Analyses
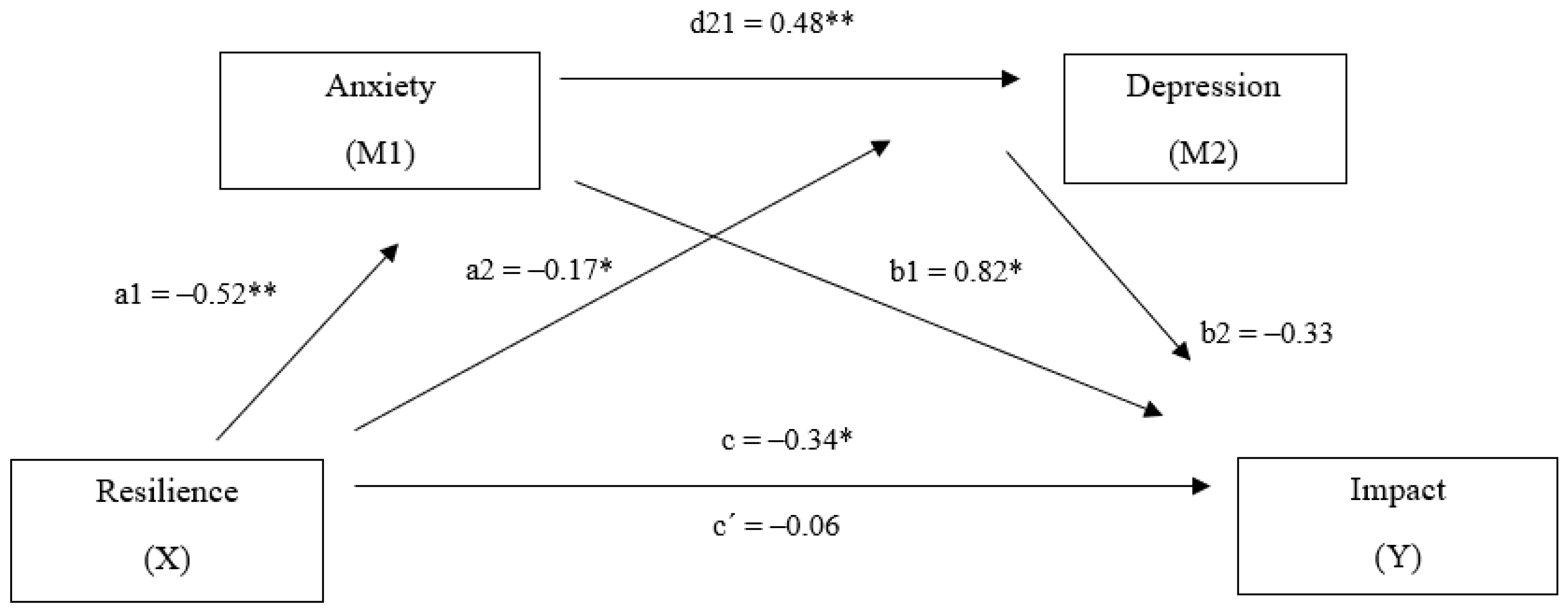
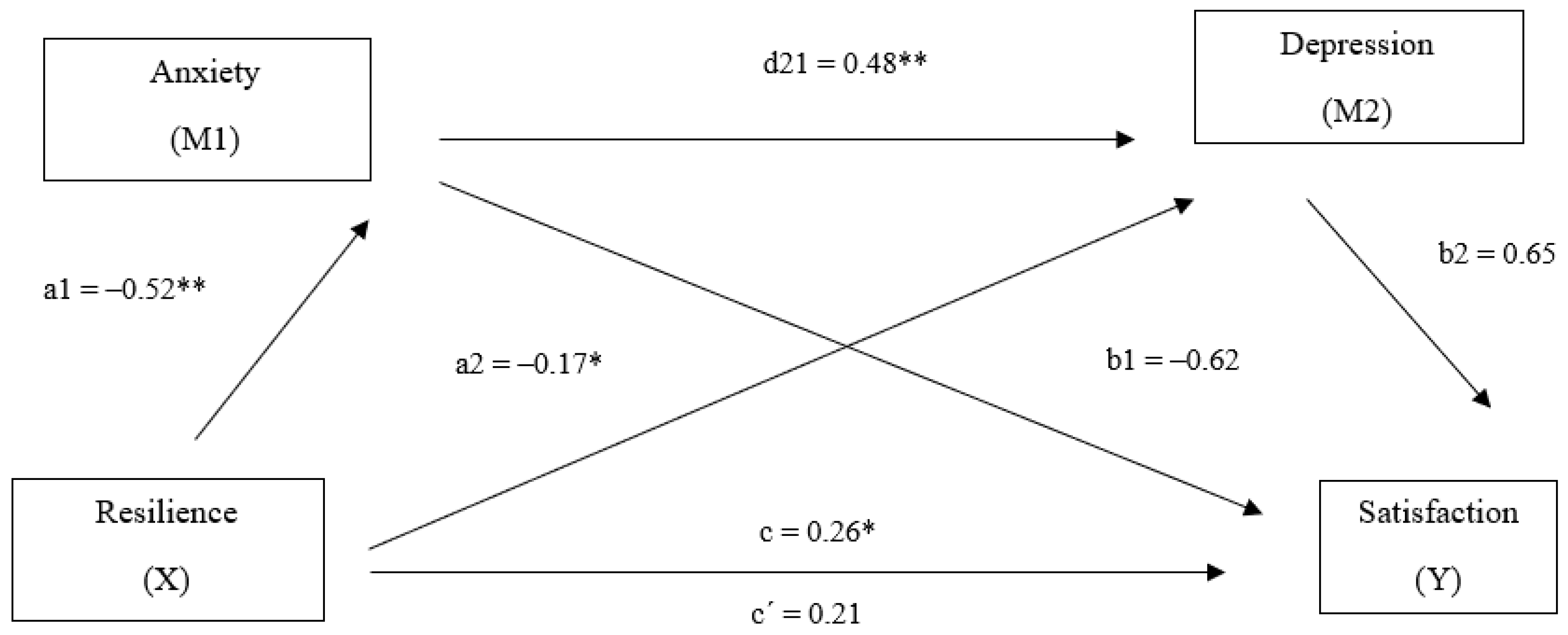
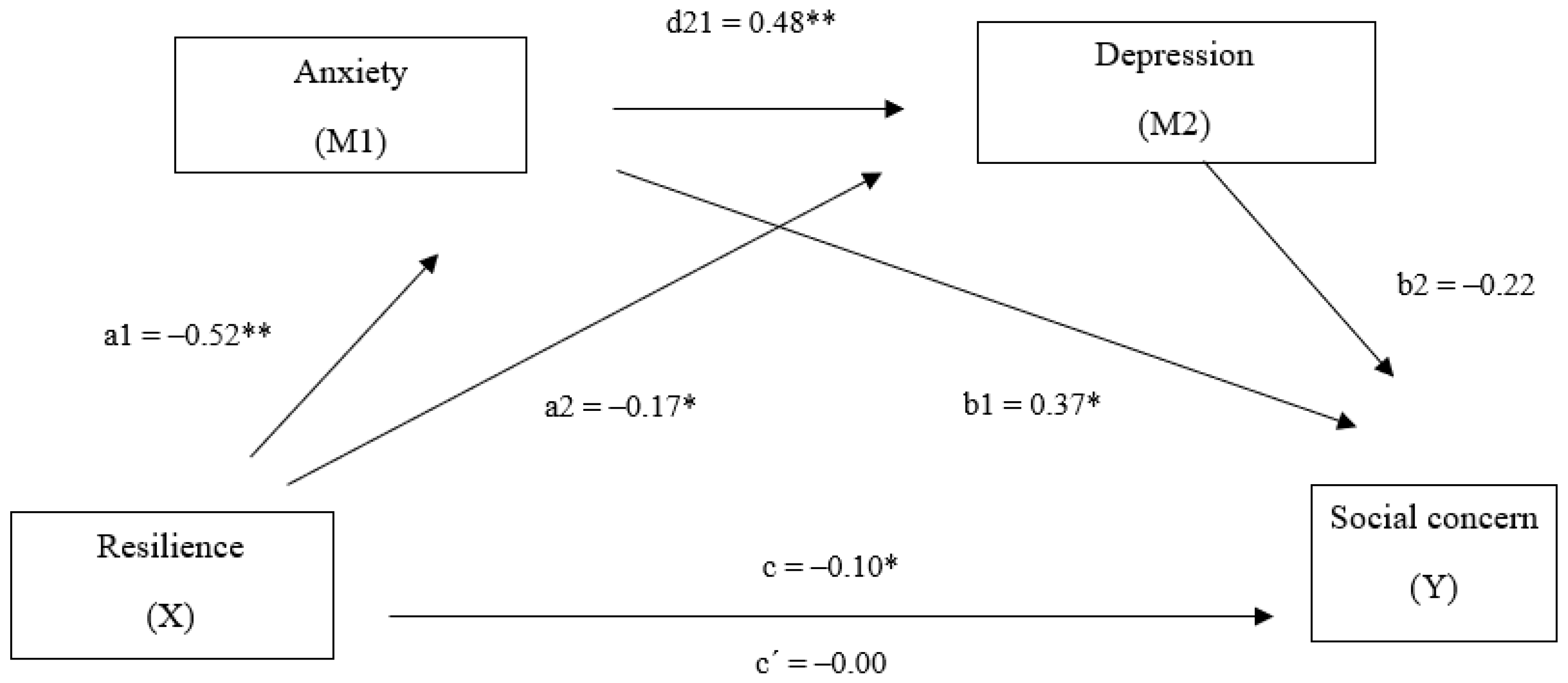
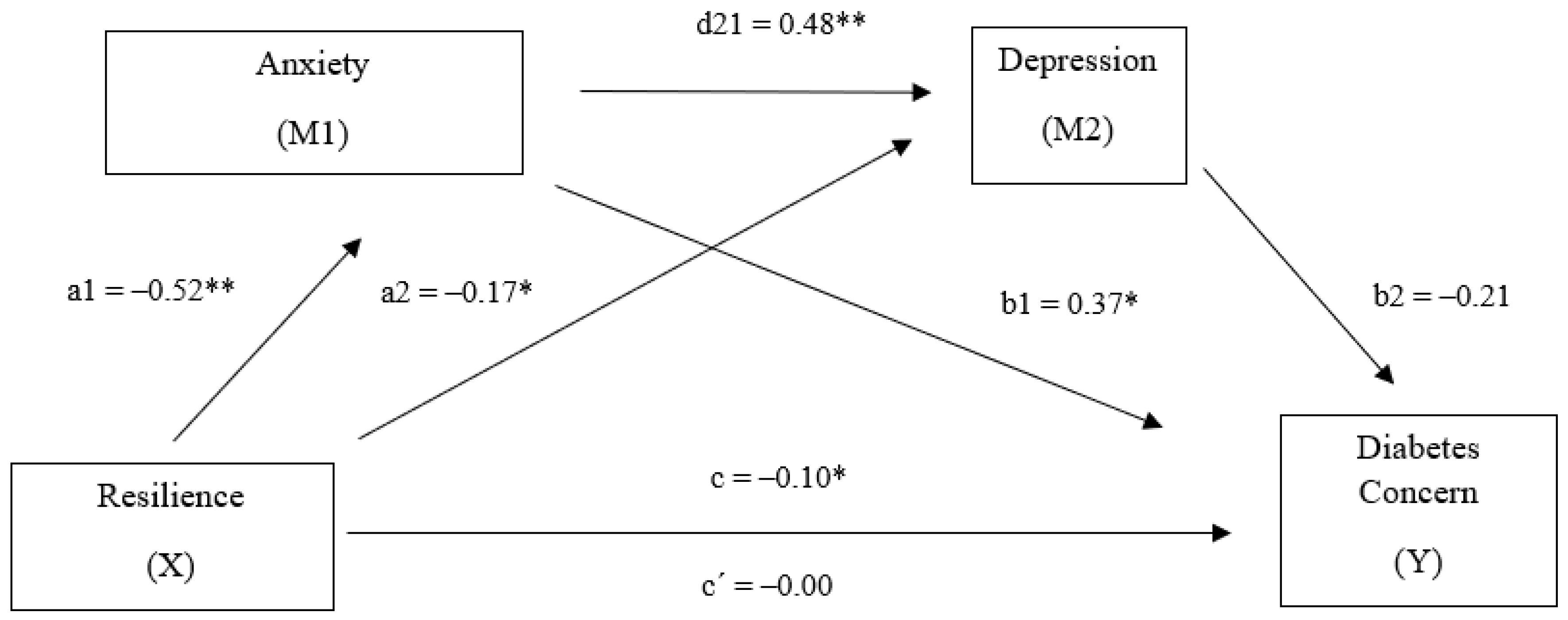
5.4. Multiple Mediating Effects of Anxiety and Depression
6. Discussion
7. Limitations
8. Implications for Research and Practice
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- American Diabetes Association. Glycemic Targets: Standards of Medical Care in Diabetes. Diabetes Care 2020, 43, 66–76. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial Research Group; Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O.; Davis, M.; Rand, L.; Siebert, C. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. New Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef]
- Schram, M.T.; A Baan, C.; Pouwer, F. Depression and Quality of Life in Patients with Diabetes: A Systematic Review from the European Depression in Diabetes (EDID) Research Consortium. Curr. Diabetes Rev. 2009, 5, 112–119. [Google Scholar] [CrossRef]
- Chew, B.-H.; Shariff-Ghazali, S.; Fernandez, A. Psychological aspects of diabetes care: Effecting behavioral change in patients. World J. Diabetes 2014, 5, 796–808. [Google Scholar] [CrossRef]
- Chamberlain, J.J.; Kalyani, R.R.; Leal, S.; Rhinehart, A.S.; Shubrook, J.; Skolnik, N.S.; Herman, W.H. Treatment of Type 1 Diabetes: Synopsis of the 2017 American Diabetes Association Standards of Medical Care in Diabetes. Ann. Intern. Med. 2017, 167, 493. [Google Scholar] [CrossRef]
- Böhme, P.; Bertin, É.; Cosson, E.; Chevalier, N. Fear of hypoglycaemia in patients with type 1 diabetes: Do patients and diabetologists feel the same way? Diabetes Metab. 2013, 39, 63–70. [Google Scholar] [CrossRef]
- Martyn-Nemeth, P.; Farabi, S.S.; Mihailescu, D.; Nemeth, J.; Quinn, L. Fear of hypoglycemia in adults with type 1 diabetes: Impact of therapeutic advances and strategies for prevention—A review. J. Diabetes Complicat. 2016, 30, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E. Glycemic Goals in Diabetes: Trade-off Between Glycemic Control and Iatrogenic Hypoglycemia. Diabetes 2014, 63, 2188–2195. [Google Scholar] [CrossRef]
- Zoungas, S.; Patel, A.C.; Chalmers, J.; de Galán, B.E.; Li, Q.; Billiot, L.; Woodward, M.; Ninomiya, T.; Neal, B.; MacMahon, S.; et al. Severe hypoglycaemia and risks of vascular events and death. N. Engl. J. Med. 2010, 363, 1410–1418. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Von Maltzahn, R.; Brohan, E.; Christensen, T.; Clauson, P.; Gonder-Frederick, L. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Educ. Couns. 2007, 68, 10–15. [Google Scholar] [CrossRef]
- Green, L.; Feher, M.; Catalan, J. Fears and phobias in people with diabetes. Diabetes Metab. Res. Rev. 2000, 16, 287–293. [Google Scholar] [CrossRef]
- Anderson, R.J.; Freedland, K.E.; Clouse, R.E.; Lustman, P.J. The Prevalence of Comorbid Depression in Adults with Diabetes: A meta-analysis. Diabetes Care 2001, 24, 1069–1078. [Google Scholar] [CrossRef]
- Castellano-Guerrero, A.M.; Guerrero, R.; Relimpio, F.; Losada, F.; Mangas, M.A.; Pumar, A.; Martínez-Brocca, M.A. Prevalence and predictors of depression and anxiety in adult patients with type 1 diabetes in tertiary care setting. Acta Diabetol. 2018, 55, 943–953. [Google Scholar] [CrossRef]
- Edward, K.-L. Chronic illness and wellbeing: Using nursing practice to foster resilience as resistance. Br. J. Nurs. 2013, 22, 741–746. [Google Scholar] [CrossRef]
- Bazzazian, S.; Besharat, M.A. An explanatory model of adjustment to type I diabetes based on attachment, coping, and self-regulation theories. Psychol. Health Med. 2012, 17, 47–58. [Google Scholar] [CrossRef]
- Baumeister, H.; Hutter, N.; Bengel, J.; Härter, M. Quality of Life in Medically Ill Persons with Comorbid Mental Disorders: A Systematic Review and Meta-Analysis. Psychother. Psychosom. 2011, 80, 275–286. [Google Scholar] [CrossRef]
- Strandberg, R.B.; Graue, M.; Wentzel-Larsen, T.; Peyrot, M.; Wahl, A.K.; Rokne, B. The relationships among fear of hypoglycaemia, diabetes-related quality of life and psychological well-being in Norwegian adults with Type 1 diabetes. Diabetes Res. Clin. Pr. 2017, 124, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Maia, A.C.C.D.O.; Braga, A.D.A.; Paes, F.; Machado, S.; Carta, M.G.; Nardi, A.E.; Silva, A.C. Comorbidity of Depression and Anxiety: Association with Poor Quality of Life in Type 1 and 2 Diabetic Patients. Clin. Pr. Epidemiol. Ment. Health 2013, 9, 136–141. [Google Scholar] [CrossRef][Green Version]
- Norris, S.L. Health-related quality of life among adults with diabetes. Curr. Diabetes Rep. 2005, 5, 124–130. [Google Scholar] [CrossRef]
- Mosaku, K.S.; Kolawole, B.; Mume, C.; Ikem, R. Depression, anxiety and quality of life among diabetic patients: A comparative study. J. Natl. Med. Assoc. 2008, 100, 73–78. [Google Scholar] [CrossRef]
- Yao, X.; Zhang, L.; Du, J.; Gao, L. Effect of Information-Motivation-Behavioral Model Based on Protection Motivation Theory on the Psychological Resilience and Quality of Life of Patients with Type 2 DM. Psychiatr. Q. 2020, 1–14. [Google Scholar] [CrossRef]
- Ovaska-Stafford, N.; Maltby, J.; Dale, M. Literature Review: Psychological Resilience Factors in People with Neurodegenerative Diseases. Arch. Clin. Neuropsychol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Richardson, G.E. The metatheory of resilience and resiliency. J. Clin. Psychol. 2002, 58, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Massey, C.N.; Feig, E.H.; Duque, L.; Wexler, D.; Moskowitz, J.T.; Huffman, J.C. Well-being interventions for individuals with diabetes: A systematic review. Diabetes Res. Clin. Pr. 2019, 147, 118–133. [Google Scholar] [CrossRef]
- Ewu, G.; Efeder, A.; Cohen, H.; Kim, J.J.; Ecalderon, S.; Charney, D.S.; Mathé, A.A. Understanding resilience. Front. Behav. Neurosci. 2013, 7, 10. [Google Scholar] [CrossRef]
- Bolier, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E.T. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health 2013, 13, 119. [Google Scholar] [CrossRef]
- Celano, C.M.; Beale, E.; Moore, S.V.; Wexler, D.J.; Huffman, J.C. Positive psychological characteristics in diabetes: A review. Curr. Diabetes Rep. 2013, 13, 917–929. [Google Scholar] [CrossRef]
- Ortiz, M.T.A.; Caballero, F.F.; De Adana, M.S.R.; Rondán, R.M.; Carreira, M.; Dominguez-Lopez, M.; Machado, A.; Gonzalo-Marín, M.; Tapia, M.J.; Valdés, S.; et al. Development of a new Fear of Hypoglycemia Scale: FH-15. Psychol. Assess. 2011, 23, 398–405. [Google Scholar] [CrossRef]
- Wagnild, G.M.; Young, H.M. Development and psychometric evaluation of the Resilience Scale. J. Nurs. Meas. 1993, 1, 165–178. [Google Scholar]
- Heilemann, M.V.; Lee, K.; Kury, F.S. Psychometric Properties of the Spanish Version of the Resilience Scale. J. Nurs. Meas. 2003, 11, 61–72. [Google Scholar] [CrossRef]
- Beck, A.T.; Rush, A.J.; Shaw, B.F.; Emery, G. Cognitive Therapy of Depression; Guilford Press: New York, NY, USA, 1979. [Google Scholar]
- Sanz, J.; y Vázquez, C. Fiabilidad, validez y datos normativos del Inventario para la Depresión de Beck. Psicothema 1998, 10, 303–318. [Google Scholar]
- Van Der Donk, L.J.; Fleer, J.; Sanderman, R.; Emmelkamp, P.M.G.; Links, T.P.; Tovote, K.A.; Schroevers, M.J. Is type of depressive symptoms associated with patient-perceived need for professional psychological care in depressed individuals with diabetes? PLoS ONE 2019, 14, e0212304. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. The State-Tratit Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Seisdedos, N. Cuestionario de Ansiedad Estado-Rasgo. Adaptación Española; TEA: Madrid, España, 1998. [Google Scholar]
- Millán, M.M.; Reviriego, J.; y del Campo, J. Reevaluación de la versión española del Cuestionario Diabetes Quality of Life (EsDQOL). Endocrinol. Nutr. 2002, 49, 322–324. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows; Version 25.0; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Cohen, A.; Peleg, O.; Sarhana, A.; Lam, S.; Haimov, I. Depressive Symptoms Mediate the Relationship between Emotional Cutoff and Type 2 Diabetes Mellitus. Int. J. Behav. Med. 2019, 26, 591–599. [Google Scholar] [CrossRef]
- Chen, C.; Fang, W.; An, Y.; Wang, L.; Fan, X. The multiple mediating effects of illness perceptions and coping strategies on the relationship between physical symptoms and depressive symptoms in patients with heart failure. Eur. J. Cardiovasc. Nurs. 2019, 19, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F.; Preacher, K.J. Conditional process modeling: Using structural equation modeling to examine contingent causal processes. In Structural Equation Modeling: A Second Course, 2nd ed.; Hancock, G.R., Mueller, R.O., Eds.; Information Age Publishing: Charlotte, NC, USA, 2013. [Google Scholar]
- Efron, B. Bootstrap Methods: Another Look at the Jackknife. Ann. Stat. 1979, 7, 1–26. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Erim, Y.; Tagay, S.; Beckmann, M.; Bein, S.; Cicinnati, V.; Beckebaum, S.; Senf, W.; Schlaak, J.F. Depression and protective factors of mental health in people with hepatitis C: A questionnaire survey. Int. J. Nurs. Stud. 2010, 47, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Ponarovsky, B.; Amital, D.; Lazarov, A.; Kotler, M.; Amital, H. Anxiety and depression in patients with allergic and non-allergic cutaneous disorders. Int. J. Dermatol. 2011, 50, 1217–1222. [Google Scholar] [CrossRef]
- Robottom, B.; Gruber-Baldini, A.; Anderson, K.; Reich, S.; Fishman, P.; Weiner, W.; Shulman, L.M. What determines resilience in patients with Parkinson’s disease? Park. Relat. Disord. 2012, 18, 174–177. [Google Scholar] [CrossRef]
- Yi, J.P.; Vitaliano, P.P.; Smith, R.E.; Yi, J.C.; Weinger, K. The role of resilience on psychological adjustment and physical health in patients with diabetes. Br. J. Health Psychol. 2007, 13, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Leppin, A.L.; Bora, P.R.; Tilburt, J.C.; Gionfriddo, M.R.; Zeballos-Palacios, C.; Dulohery, M.M.; Sood, A.; Erwin, P.J.; Brito, J.P.; Boehmer, K.R.; et al. The Efficacy of Resiliency Training Programs: A Systematic Review and Meta-Analysis of Randomized Trials. PLoS ONE 2014, 9, e111420. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Shao, H.; Zhao, Y.; A Thomas, N. Is hypoglycemia fear independently associated with health-related quality of life? Heal. Qual. Life Outcomes 2014, 12, 167. [Google Scholar] [CrossRef] [PubMed]
- Castellano-Guerrero, A.M.; Guerrero, R.; Ruiz-Aranda, D.; Perea, S.; Pumar, A.; Relimpio, F.; Mangas, M.A.; Losada, F.; Martínez-Brocca, M.A. Gender differences in quality of life in adults with long-standing type 1 diabetes mellitus. Diabetol. Metab. Syndr. 2020, 12, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Anderbro, T.; Amsberg, S.; Adamson, U.; Bolinder, J.; Lins, P.-E.; Wredling, R.; Moberg, E.; Lisspers, J.; Johansson, U.-B. Fear of hypoglycaemia in adults with Type 1 diabetes. Diabet. Med. 2010, 27, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Martínez Brocca, M.A.; Mayoral, E.; Irastorza, A.; Lama, C.; Martínez, E.; Sanz, R.; Candela, C. Plan. Integral de Diabetes de Andalucía: Evaluación del II Plan. Integral de Diabetes de Andalucía. Actualización 2016; Conserjería de Salud: Sevilla, España, 2016. [Google Scholar]
- Lawton, J.; Rankin, D.; Cooke, D.D.; Amiel, S.; Heller, S.; Elliott, J.; for the UK NIHR DAFNE Study Group. Self-treating hypoglycaemia: A longitudinal qualitative investigation of the experiences and views of people with Type 1 diabetes. Diabet. Med. 2013, 30, 209–215. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N | ||
|---|---|---|---|
| Marital Status | |||
| Married | 9 | ||
| Single | 6 | ||
| Divorced | 5 | ||
| Cohabiting | 3 | ||
| No reply | 7 | ||
| Clinical Variables | Range | Mean | SD |
| Years of evolution | 2–53 | 24.89 | 12.49 |
| HbA1c | 6.20–10.30% | 8.02 | 1.00 |
| Average blood glucose | 127–334 | 177.75 | 43.06 |
| Time in hypoglycemia (<70 mg/dL) | 0–39% | 7.57 | 9.30 |
| Time in hyperglycemia (>180 mg/dL) | 9–90% | 50.89 | 20.85 |
| Time in range (70–180 mg/dL) | 10–79% | 41.60 | 17.23 |
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Total resilience | 129.04 | 23.78 | — | ||||||
| 2. Trait anxiety | 24.17 | 15.19 | −0.76 ** | — | |||||
| 3. Depression | 12.82 | 11.18 | −0.84 ** | 0.90 ** | — | ||||
| 4. Satisfaction | 40.43 | 11.86 | 0.49 * | −0.54 ** | −0.45 * | — | |||
| 5. Impact | 42.03 | 12.62 | −0.60 ** | 0.77 ** | 0.67 ** | −0.63 ** | — | ||
| 6. Social concern | 17.62 | 5.69 | −0.43 ** | 0.61 ** | 0.55 ** | −0.30 | 0.62 ** | — | |
| 7. Diabetes concern | 12.65 | 3.40 | −0.52 ** | 0.67 ** | 0.60 ** | −0.46 * | 0.70 ** | 0.54 ** | — |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Aranda, D.; Mateo-Rodriguez, C.; Olmedo, I.S.; García, C.G.; Enríquez, A.J.; Martinez-Brocca, M.A. Relationship between Resilience and Quality of Life in Patients with Fear of Hypoglycemia: The Mediating Effects of Anxiety and Depression. Sustainability 2020, 12, 8512. https://doi.org/10.3390/su12208512
Ruiz-Aranda D, Mateo-Rodriguez C, Olmedo IS, García CG, Enríquez AJ, Martinez-Brocca MA. Relationship between Resilience and Quality of Life in Patients with Fear of Hypoglycemia: The Mediating Effects of Anxiety and Depression. Sustainability. 2020; 12(20):8512. https://doi.org/10.3390/su12208512
Chicago/Turabian StyleRuiz-Aranda, Desireé, Carmen Mateo-Rodriguez, Isabel Serrano Olmedo, Clara García García, Alicia Justel Enríquez, and María Asunción Martinez-Brocca. 2020. "Relationship between Resilience and Quality of Life in Patients with Fear of Hypoglycemia: The Mediating Effects of Anxiety and Depression" Sustainability 12, no. 20: 8512. https://doi.org/10.3390/su12208512
APA StyleRuiz-Aranda, D., Mateo-Rodriguez, C., Olmedo, I. S., García, C. G., Enríquez, A. J., & Martinez-Brocca, M. A. (2020). Relationship between Resilience and Quality of Life in Patients with Fear of Hypoglycemia: The Mediating Effects of Anxiety and Depression. Sustainability, 12(20), 8512. https://doi.org/10.3390/su12208512






