A Bibliometric Analysis on No-Show Research: Status, Hotspots, Trends and Outlook
Abstract
1. Introduction
2. Methodology
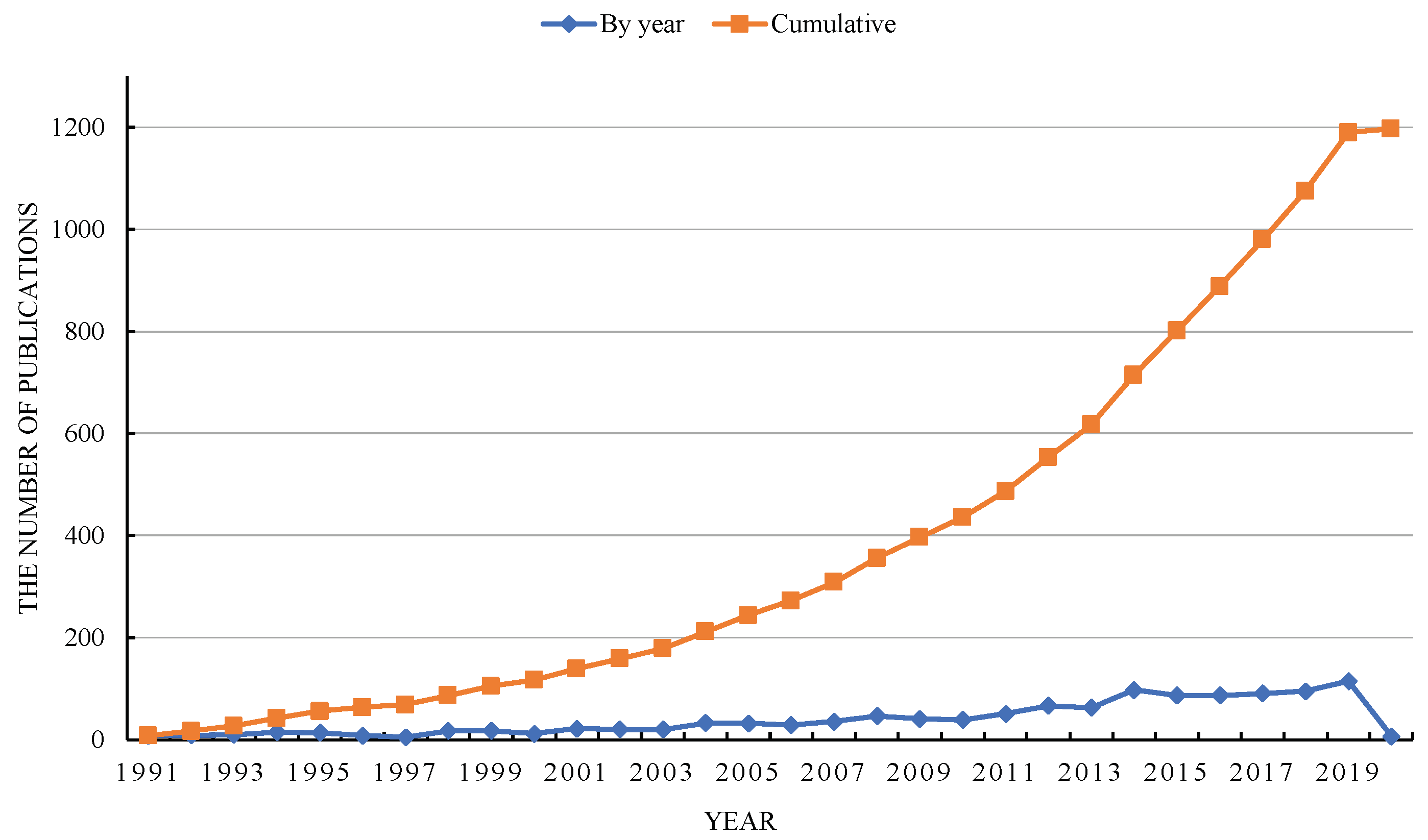
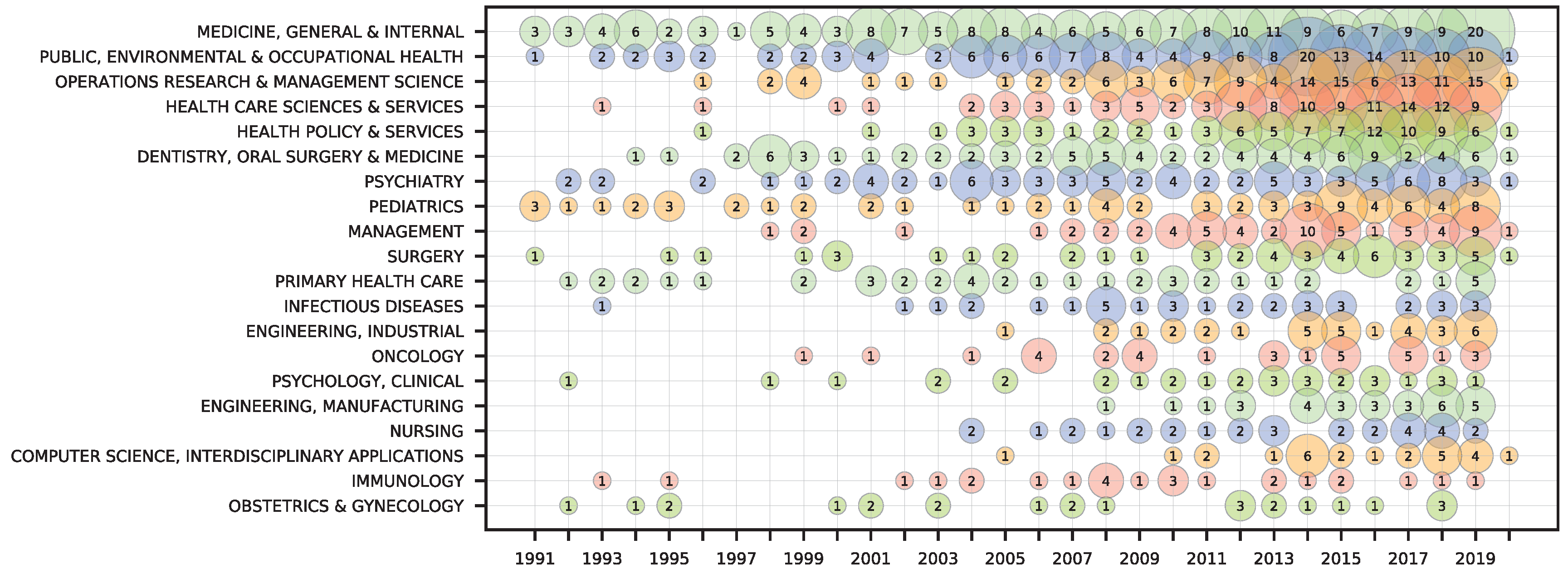
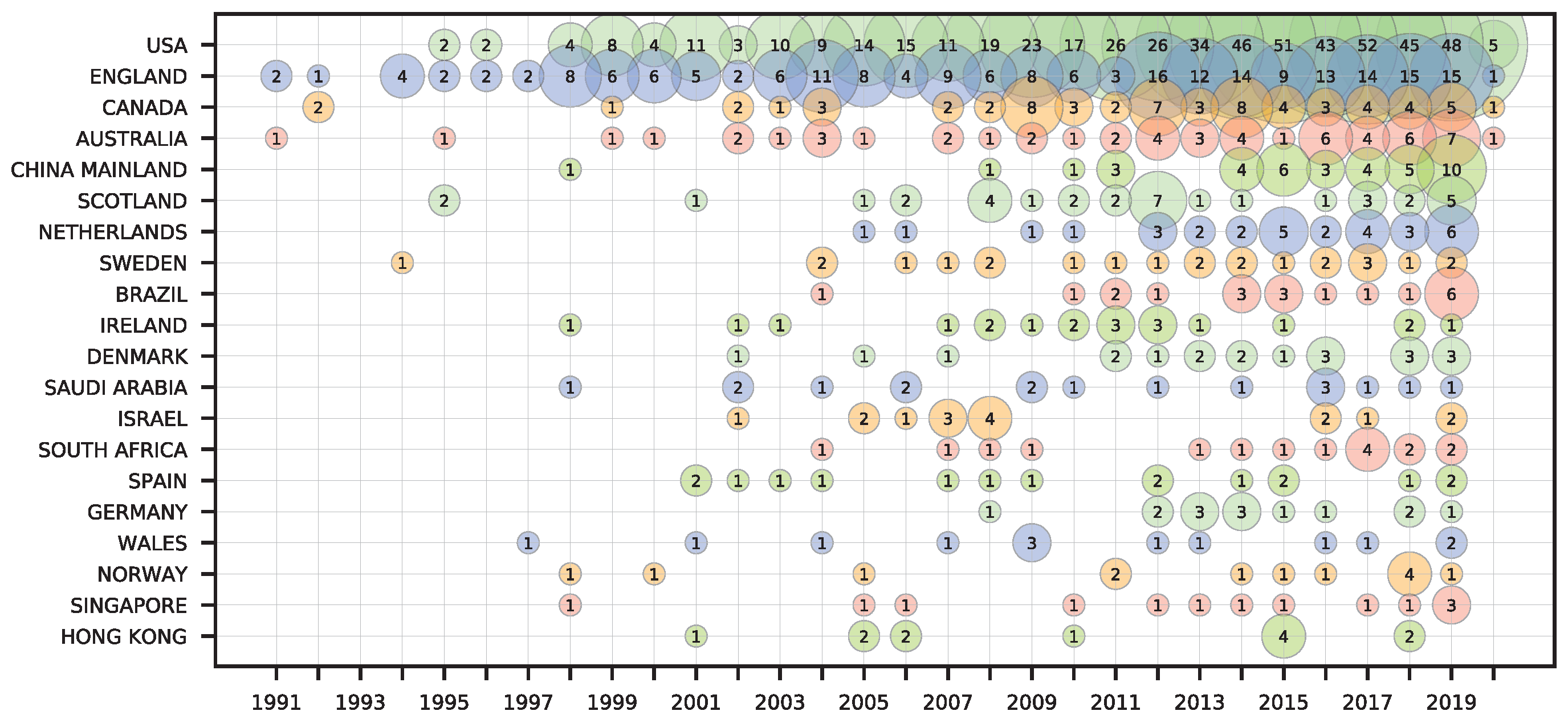
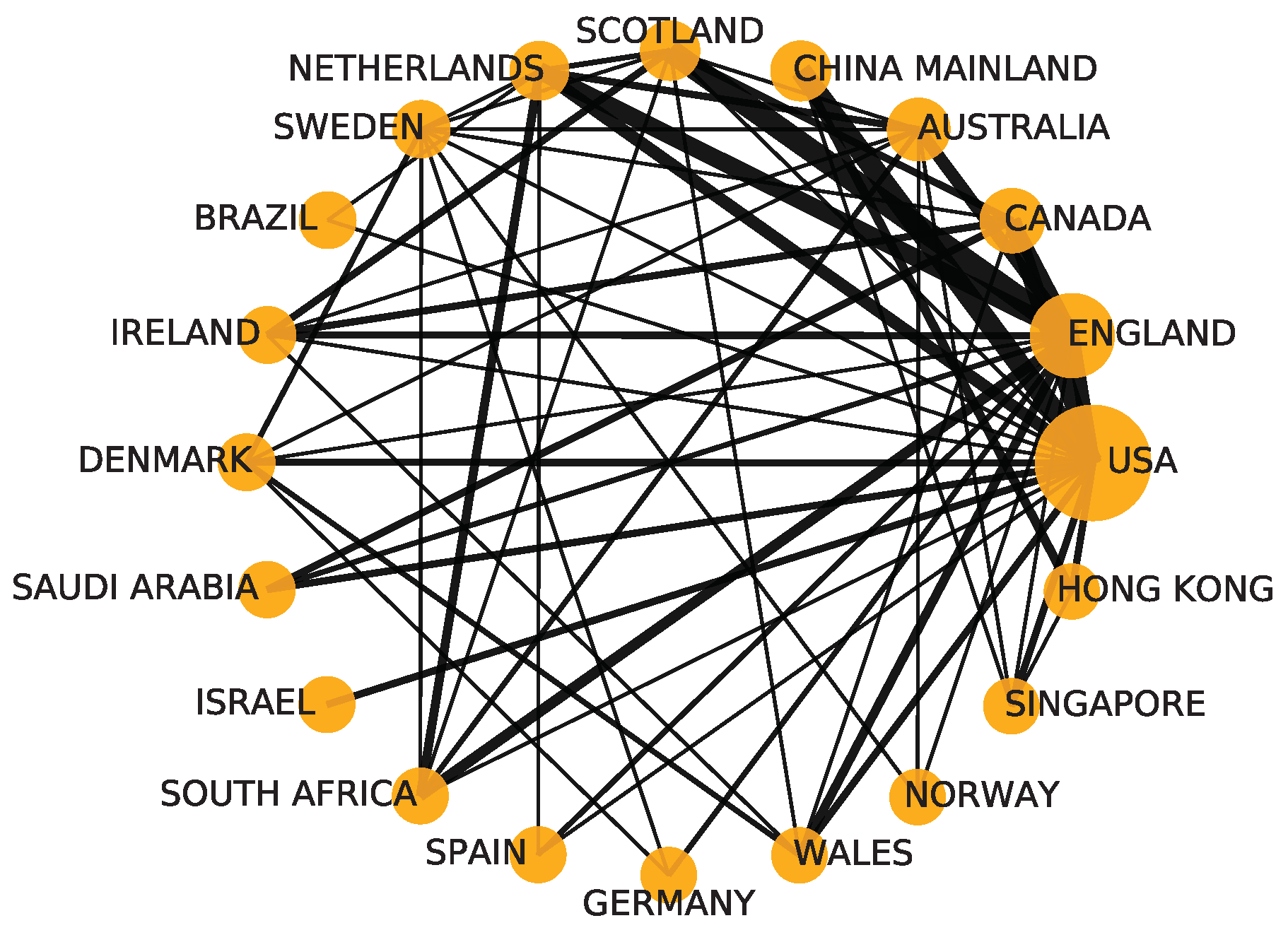
3. Results Analysis
3.1. Research Areas and Leading Countries/Regions
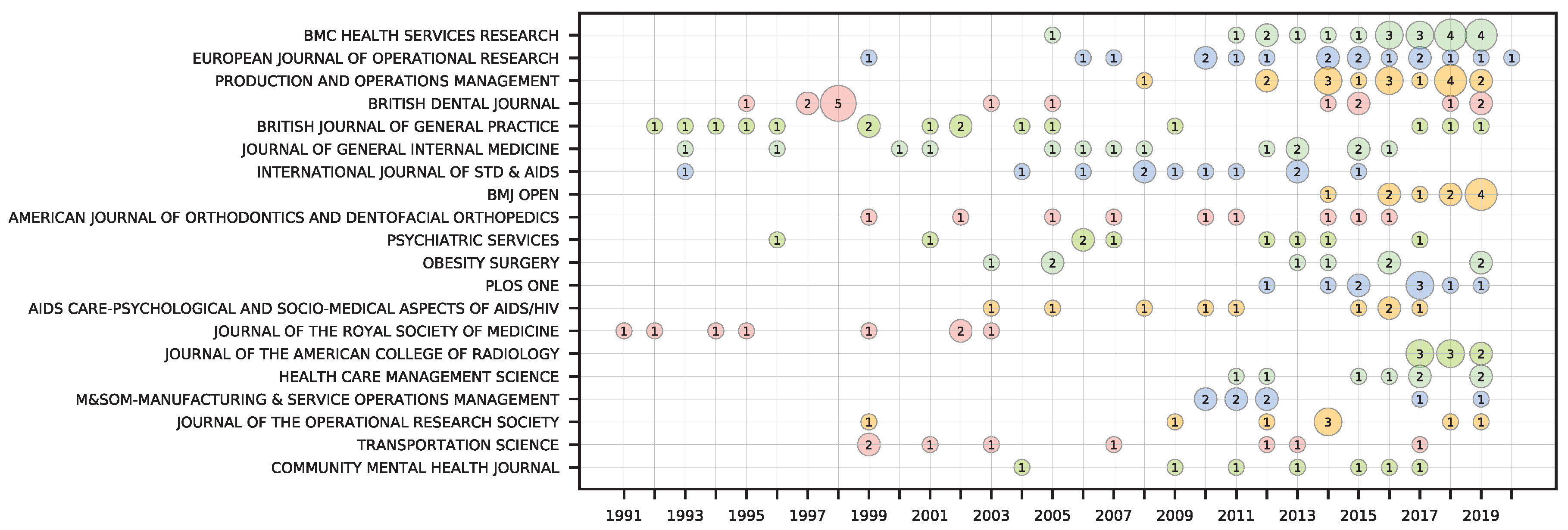
3.2. Contribution of Leading Journals
3.3. Contribution of Leading Authors
3.4. An Analysis of the Most Cited Papers
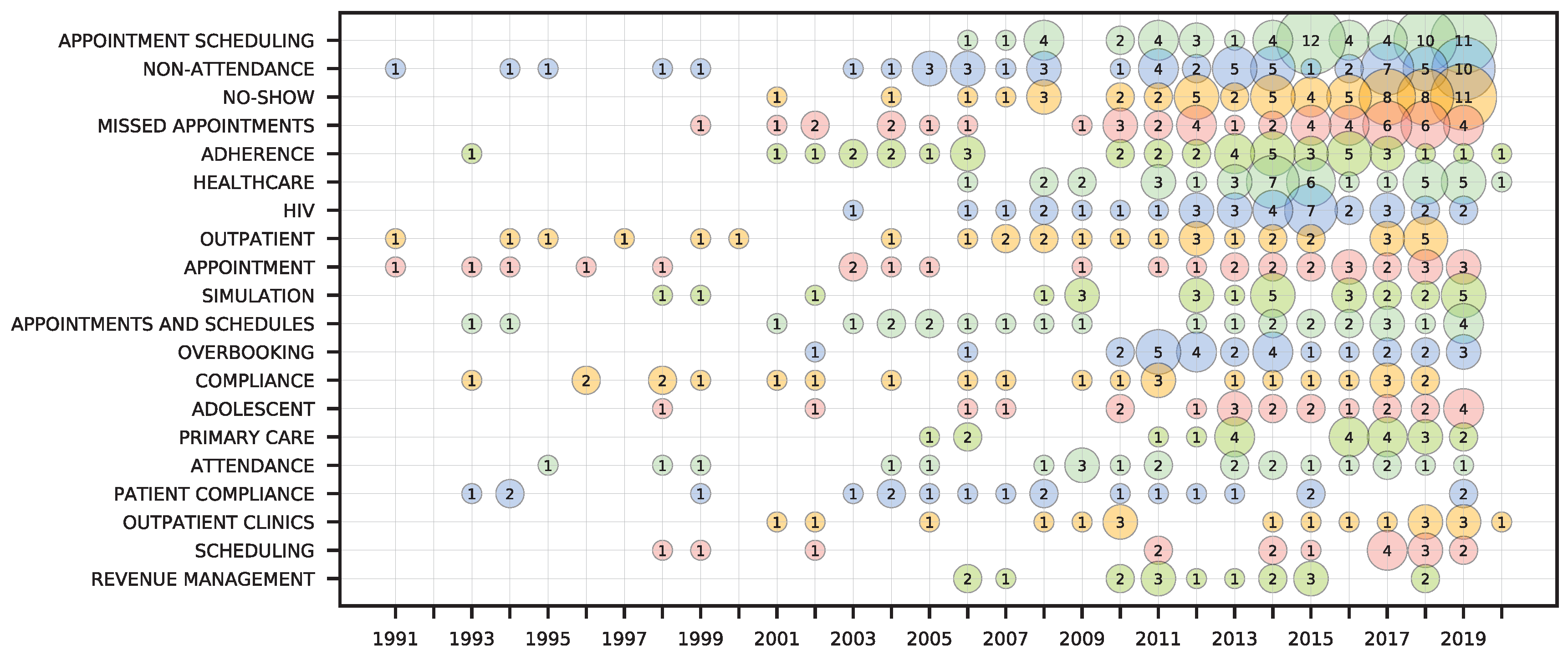
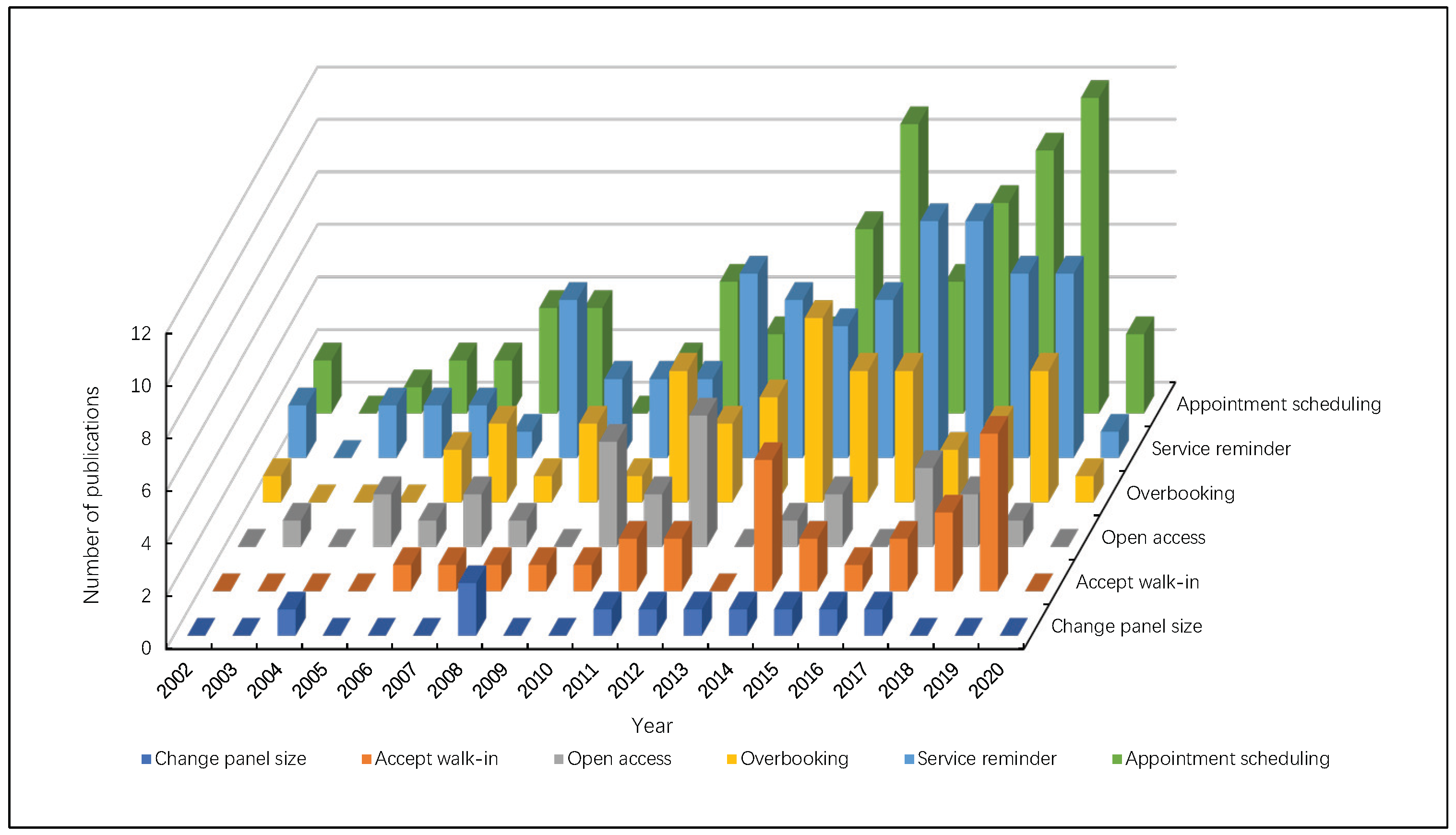
3.5. Methods for No-Show Issues
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| WoS | Web of Science database |
| SCIE | Science Citation Index Expanded |
| SSCI | Social Sciences Citation Index |
| DDA | Dervent data analyzer software |
| IF | Impact factors |
| TA | Total articles |
| TC | Total citations |
| ACPP | Average citations per publication |
| IC | Number of international collaboration papers |
| TPR% | The percentage of articles of journals in total publications |
| PY | Publishing year |
| TCY | Total citations per year |
| ESI | Essential Science Indicators |
| SMS | Short messaging service |
References
- Gupta, D.; Denton, B. Appointment scheduling in health care: Challenges and opportunities. IIE Trans. 2008, 40, 800–819. [Google Scholar] [CrossRef]
- Moore, C.G.; Wilson-Witherspoon, P.; Probst, J.C. Time and money: Effects of no-shows at a family practice residency clinic. Fam. Med. 2001, 33, 522–527. [Google Scholar] [PubMed]
- Geraghty, M.; Glynn, F.; Amin, M.; Kinsella, J. Patient mobile telephone ’text’ reminder: A novel way to reduce non-attendance at the ENT out-patient clinic. J. Laryngol. Otol. 2008, 122, 296–298. [Google Scholar] [CrossRef] [PubMed]
- Dreiher, J.; Froimovici, M.; Bibi, Y.; Vardy, D.A.; Cicurel, A.; Cohen, A.D. Nonattendance in obstetrics and gynecology patients. Gynecol. Obstet. Investig. 2008, 66, 40–43. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.E.; Matthews, B.S.; Gao, D.X. Effect of open access scheduling on missed appointments, immunizations, and continuity of care for infant well-child care visits. Arch. Pediatr. Adolesc. Med. 2006, 160, 889–893. [Google Scholar] [CrossRef]
- Schectman, J.M.; Schorling, J.B.; Voss, J.D. Appointment adherence and disparities in outcomes among patients with diabetes. J. Gen. Intern. Med. 2008, 23, 1685–1687. [Google Scholar] [CrossRef]
- Schwebel, F.J.; Larimer, M.E. Using text message reminders in health care services: A narrative literature review. Internet Interv. 2018, 13, 82–104. [Google Scholar] [CrossRef]
- Dai, J.G.; Kleywegt, A.J.; Xiao, Y.B. Network Revenue Management with Cancellations and No-Shows. Prod. Oper. Manag. 2019, 28, 292–318. [Google Scholar] [CrossRef]
- Han, S.H.; Zhao, L.; Chen, K.; Luo, Z.W.; Mishra, D. Appointment scheduling and routing optimization of attended home delivery system with random customer behavior. Eur. J. Oper. Res. 2017, 262, 966–980. [Google Scholar] [CrossRef]
- Guse, C.E.; Richardson, L.; Carle, M.; Schmidt, K. The effect of exit-interview patient education on no-show rates at a family practice residency clinic. J. Am. Board Fam. Pract. 2003, 16, 399–404. [Google Scholar] [CrossRef]
- Tikani, H.; Honarvar, M.; Mehrjerdi, Y.Z. Developing an integrated hub location and revenue management model considering multi-classes of customers in the airline industry. Comput. Appl. Math. 2018, 37, 3334–3364. [Google Scholar] [CrossRef]
- Subramanian, J.; Stidham, S.; Lautenbacher, C.J. Airline yield management with overbooking, cancellations, and no-shows. Transp. Sci. 1999, 33, 147–167. [Google Scholar] [CrossRef]
- Berrouiguet, S.; Baca-Garcia, E.; Brandt, S.; Walter, M.; Courtet, P. Fundamentals for Future Mobile-Health (mHealth): A Systematic Review of Mobile Phone and Web-Based Text Messaging in Mental Health. J. Med. Internet Res. 2016, 18, 15. [Google Scholar] [CrossRef] [PubMed]
- Free, C.; Phillips, G.; Watson, L.; Galli, L.; Felix, L.; Edwards, P.; Patel, V.; Haines, A. The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis. PLos Med. 2013, 10, 26. [Google Scholar] [CrossRef]
- LaGanga, L.R.; Lawrence, S.R. Clinic overbooking to improve patient access and increase provider productivity. Decis. Sci. 2007, 38, 251–276. [Google Scholar] [CrossRef]
- Muthuraman, K.; Lawley, M. A stochastic overbooking model for outpatient clinical scheduling with no-shows. IIE Trans 2008, 40, 820–837. [Google Scholar] [CrossRef]
- Pritchard, A. Statistical biblography or bibliometrics? J. Doc. 1969, 25, 348–349. [Google Scholar]
- Wallin, J.A. Bibliometric methods: Pitfalls and possibilities. Basic Clin. Pharmacol. Toxicol. 2005, 97, 261–275. [Google Scholar] [CrossRef]
- Du, H.B.; Li, N.; Brown, M.A.; Peng, Y.N.; Shuai, Y. A bibliographic analysis of recent solar energy literatures: The expansion and evolution of a research field. Renew. Energy 2014, 66, 696–706. [Google Scholar] [CrossRef]
- Merigo, J.M.; Rocafort, A.; Aznar-Alarcon, J.P. Bibliometric overview of business & economics research. J. Bus. Econ. Manag. 2016, 17, 397–413. [Google Scholar] [CrossRef]
- Torres-Salinas, D.; Moed, H.F. Library Catalog Analysis as a tool in studies of social sciences and humanities: An exploratory study of published book titles in Economics. J. Informetr. 2009, 3, 9–26. [Google Scholar] [CrossRef]
- Hernandez-Garcia, Y.I.; Chamizo, J.A.; Kleiche-Dray, M.; Russell, J.M. The scientific impact of mexican steroid research 1935-1965: A bibliometric and historiographic analysis. J. Assoc. Inf. Sci. Technol. 2016, 67, 1245–1256. [Google Scholar] [CrossRef]
- Franceschet, M. The skewness of computer science. Inf. Process. Manag. 2011, 47, 117–124. [Google Scholar] [CrossRef]
- Chen, H.Q.; Wan, Y.H.; Jiang, S.A.; Cheng, Y.X. Alzheimer’s disease research in the future: Bibliometric analysis of cholinesterase inhibitors from 1993 to 2012. Scientometrics 2014, 98, 1865–1877. [Google Scholar] [CrossRef]
- Calma, A.; Davies, M. Academy of Management Journal, 1958–2014: A citation analysis. Scientometrics 2016, 108, 959–975. [Google Scholar] [CrossRef]
- Chen, Y.; Jin, Q.X.; Fang, H.; Lei, H.; Hu, J.R.; Wu, Y.Q.; Chen, J.; Wang, C.; Wan, Y.H. Analytic network process: Academic insights and perspectives analysis. J. Clean Prod. 2019, 235, 1276–1294. [Google Scholar] [CrossRef]
- Chen, H.Q.; Wang, X.P.; He, L.; Chen, P.; Wan, Y.H.; Yang, L.Y.; Jiang, S.A. Chinese energy and fuels research priorities and trend: A bibliometric analysis. Renew. Sustain. Energy Rev. 2016, 58, 966–975. [Google Scholar] [CrossRef]
- Deane, F.P. Improving attendance at intake in childrens outpatient services of a community mental-health-center. Child Care Health Dev. 1991, 17, 115–121. [Google Scholar]
- Tahamtan, I.; Afshar, A.S.; Ahamdzadeh, K. Factors affecting number of citations: A comprehensive review of the literature. Scientometrics 2016, 107, 1195–1225. [Google Scholar] [CrossRef]
- Mani, A.; Mullainathan, S.; Shafir, E.; Zhao, J.Y. Poverty Impedes Cognitive Function. Science 2013, 341, 976–980. [Google Scholar] [CrossRef]
- Menon, U.; Gentry-Maharaj, A.; Hallett, R.; Ryan, A.; Burnell, M.; Sharma, A.; Lewis, S.; Davies, S.; Philpott, S.; Lopes, A.; et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: Results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS). Lancet Oncol. 2009, 10, 327–340. [Google Scholar] [CrossRef]
- Krishna, S.; Boren, S.A.; Balas, E.A. Healthcare via Cell Phones: A Systematic Review. Telemed. J. e-Health 2009, 15, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Karter, A.J.; Ackerson, L.M.; Darbinian, J.A.; D’Agostino, R.B.; Ferrara, A.; Liu, J.; Selby, J.V. Self-monitoring of blood glucose levels and glycemic control: The Northern California Kaiser Permanente Diabetes Registry. Am. J. Med. 2001, 111, 1–9. [Google Scholar] [CrossRef]
- Macharia, W.M.; Leon, G.; Rowe, B.H.; Stephenson, B.J.; Haynes, R.B. An overview of interventions to improve compliance with appointment keeping for medical-services. JAMA J. Am. Med. Assoc. 1992, 267, 1813–1817. [Google Scholar] [CrossRef]
- Beach, M.C.; Keruly, J.; Moore, R.D. Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? J. Gen. Intern. Med. 2006, 21, 661–665. [Google Scholar] [CrossRef]
- Syed, S.T.; Gerber, B.S.; Sharp, L.K. Traveling Towards Disease: Transportation Barriers to Health Care Access. J. Community Health 2013, 38, 976–993. [Google Scholar] [CrossRef]
- Rhee, M.K.; Slocum, W.; Ziemer, D.C.; Culler, S.D.; Cook, C.B.; El-Kebbi, I.M.; Gallina, D.L.; Barnes, C.; Phillips, L.S. Patient adherence improves glycemic control. Diabetes Educ. 2005, 31, 240–250. [Google Scholar] [CrossRef]
- Leong, K.C.; Chen, W.S.; Leong, K.W.; Mastura, I.; Mimi, O.; Sheikh, M.A.; Zailinawati, A.H.; Ng, C.J.; Phua, K.L.; Teng, C.L. The use of text messaging to improve attendance in primary care: A randomized controlled trial. Fam. Pract. 2006, 23, 699–705. [Google Scholar] [CrossRef]
- Killaspy, H.; Banerjee, S.; King, M.; Lloyd, M. Prospective controlled study of psychiatric out-patient non-attendance—Characteristics and outcome. Br. J. Psychiatry 2000, 176, 160–165. [Google Scholar] [CrossRef]
- Yu, J.K.L.; Chen, S.C.C.; Wang, K.Y.; Chang, C.S.; Makombe, S.D.; Schouten, E.J.; Harries, A.D. True outcomes for patients on antiretroviral therapy who are “lost to follow-up” in Malawi. Bull. World Health Organ. 2007, 85, 550–554. [Google Scholar] [CrossRef]
- Swofford, C.D.; Kasckow, J.W.; SchellerGilkey, G.; Inderbitzin, L.B. Substance use: A powerful predictor of relapse in schizophrenia. Schizophr. Res. 1996, 20, 145–151. [Google Scholar] [CrossRef]
- Lacy, N.L.; Paulman, A.; Reuter, M.D.; Lovejoy, B. Why we don’t come: Patient perceptions on no-shows. Ann. Fam. Med. 2004, 2, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Gurol-Urganci, I.; De Jongh, T.; Vodopivec-Jamsek, V.; Atun, R.; Car, J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2013, 12, 50. [Google Scholar] [CrossRef] [PubMed]
- Satterthwaite, T.D.; Elliott, M.A.; Ruparel, K.; Loughead, J.; Prabhakaran, K.; Calkins, M.E.; Hopson, R.; Jackson, C.; Keefe, J.; Riley, M.; et al. Neuroimaging of the Philadelphia Neurodevelopmental Cohort. NeuroImage 2014, 86, 544–553. [Google Scholar] [CrossRef]
- Gallacher, K.; May, C.R.; Montori, V.M.; Mair, F.S. Understanding Patients’ Experiences of Treatment Burden in Chronic Heart Failure Using Normalization Process Theory. Ann. Fam. Med. 2011, 9, 235–243. [Google Scholar] [CrossRef]
- Junghans, C.; Feder, G.; Hemingway, H.; Timmis, A.; Jones, M. Recruiting patients to medical research: Double blind randomised trial of “opt-in” versus “opt-out” strategies. Br. Med. J. 2005, 331, 940–942. [Google Scholar] [CrossRef]
- Zacharias, C.; Armony, M. Joint Panel Sizing and Appointment Scheduling in Outpatient Care. Manag. Sci. 2017, 63, 3978–3997. [Google Scholar] [CrossRef]
- Arora, S.; Burner, E.; Terp, S.; Lam, C.N.; Nercisian, A.; Bhatt, V.; Menchine, M. Improving Attendance at Post-Emergency Department Follow-up Via Automated Text Message Appointment Reminders: A Randomized Controlled Trial. Acad. Emerg. Med. 2015, 22, 31–37. [Google Scholar] [CrossRef]
- Lee, C.S.; McCormick, P.A. Telephone reminders to reduce non-attendance rate for endoscopy. J. R. Soc. Med. 2003, 96, 547–548. [Google Scholar] [CrossRef]
- Stubbs, N.D.; Geraci, S.A.; Stephenson, P.L.; Jones, D.B.; Sanders, S. Methods to Reduce Outpatient Non-attendance. Am. J. Med. Sci. 2012, 344, 211–219. [Google Scholar] [CrossRef]
- Zacharias, C.; Pinedo, M. Appointment Scheduling with No-Shows and Overbooking. Prod. Oper. Manag. 2014, 23, 788–801. [Google Scholar] [CrossRef]
- Parente, C.A.; Salvatore, D.; Gallo, G.M.; Cipollini, F. Using overbooking to manage no-shows in an Italian healthcare center. BMC Health Serv. Res. 2018, 18, 12. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.D.; Qu, X.L.; Shi, J. A hybrid simulation and genetic algorithm approach to determine the optimal scheduling templates for open access clinics admitting walk-in patients. Comput. Ind. Eng. 2014, 72, 282–296. [Google Scholar] [CrossRef]
- Ahmadi-Javid, A.; Jalali, Z.; Klassen, K.J. Outpatient appointment systems in healthcare: A review of optimization studies. Eur. J. Oper. Res. 2017, 258, 3–34. [Google Scholar] [CrossRef]
- Yan, C.J.; Tang, J.F.; Jiang, B.W. Sequential Appointment Scheduling Considering Walk-In Patients. Math. Probl. Eng. 2014, 2014, 12. [Google Scholar] [CrossRef]
- Luo, J.Z.; Kulkarni, V.G.; Ziya, S. Appointment Scheduling Under Patient No-Shows and Service Interruptions. Manuf. Serv. Oper. Manag. 2012, 14, 670–684. [Google Scholar] [CrossRef]
- Saure, A.; Begen, M.A.; Patrick, J. Dynamic multi-priority, multi-class patient scheduling with stochastic service times. Eur. J. Oper. Res. 2020, 280, 254–265. [Google Scholar] [CrossRef]
- Zhang, Z.; Berg, B.P.; Denton, B.T.; Xie, X.L. Appointment scheduling and the effects of customer congestion on service. IISE Trans. 2019, 51, 1075–1090. [Google Scholar] [CrossRef]
- Shah, S.J.; Cronin, P.; Hong, C.S.; Hwang, A.S.; Ashburner, J.M.; Bearnot, B.I.; Richardson, C.A.; Fosburgh, B.W.; Kimball, A.B. Targeted Reminder Phone Calls to Patients at High Risk of No-Show for Primary Care Appointment: A Randomized Trial. J. Gen. Intern. Med. 2016, 31, 1460–1466. [Google Scholar] [CrossRef]
- Percac-Lima, S.; Singer, D.E.; Cronin, P.R.; Chang, Y.C.; Zai, A.H. Can Text Messages Improve Attendance to Primary Care Appointments in Underserved Populations? J. Health Care Poor Underserved 2016, 27, 1709–1725. [Google Scholar] [CrossRef]
- Crutchfield, T.M.; Kistler, C.E. Getting patients in the door: Medical appointment reminder preferences. Patient Prefer. Adherence 2017, 11, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Parikh, A.; Gupta, K.; Wilson, A.C.; Fields, K.; Cosgrove, N.M.; Kostis, J.B. The Effectiveness of Outpatient Appointment Reminder Systems in Reducing No-Show Rates. Am. J. Med. 2010, 123, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Weaver, K.R.; Talley, M.; Mullins, M.; Selleck, C. Evaluating Patient Navigation to Improve First Appointment No-show Rates in Uninsured Patients with Diabetes. J. Community Health Nurs. 2019, 36, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Deng, L.L.; Han, Y. Optimal appointment reminder sending strategy for a single service scenario with customer no-show behaviour. J. Oper. Res. Soc. 2018, 69, 1863–1875. [Google Scholar] [CrossRef]
- Tan, J.; Christie, A.; Montalvo, S.K.; Wallace, C.; Yan, Y.L.; Folkerts, M.; Yingling, A.; Sher, D.; Choy, H.; Jiang, S.; et al. Automated Text Message Reminders Improve Radiation Therapy Compliance. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Ziya, S.; Kulkarni, V.G. Dynamic Scheduling of Outpatient Appointments Under Patient No-Shows and Cancellations. Manuf. Serv. Oper. Manag. 2010, 12, 347–364. [Google Scholar] [CrossRef]
- Cayirli, T.; Dursun, P.; Gunes, E.D. An integrated analysis of capacity allocation and patient scheduling in presence of seasonal walk-ins. Flex. Serv. Manuf. J. 2019, 31, 524–561. [Google Scholar] [CrossRef]
- Qu, X.L.; Peng, Y.D.; Shi, J.; LaGanga, L. An MDP model for walk-in patient admission management in care clinics. Int. J. Prod. Econ. 2015, 168, 303–320. [Google Scholar] [CrossRef]
- Liu, N.; Ziya, S. Panel Size and Overbooking Decisions for Appointment-Based Services under Patient No-Shows. Prod. Oper. Manag. 2014, 23, 2209–2223. [Google Scholar] [CrossRef]
- Topuz, K.; Uner, H.; Oztekin, A.; Yildirim, M.B. Predicting pediatric clinic no-shows: A decision analytic framework using elastic net and Bayesian belief network. Ann. Oper. Res. 2018, 263, 479–499. [Google Scholar] [CrossRef]
- Rosenbaum, J.I.; Mieloszyk, R.J.; Hall, C.S.; Hippe, D.S.; Gunn, M.L.; Bhargava, P. Understanding Why Patients No-Show: Observations of 2.9 Million Outpatient Imaging Visits Over 16 Years. J. Am. Coll. Radiol. 2018, 15, 944–950. [Google Scholar] [CrossRef] [PubMed]
| Rank | Country/Region | TA | TPR% | TC | ACPP | IC |
|---|---|---|---|---|---|---|
| 1 | United States | 539 | 45.03 | 12061 | 22.38 | 70 |
| 2 | England | 225 | 18.80 | 5851 | 26.00 | 41 |
| 3 | Canada | 65 | 5.43 | 1661 | 25.55 | 23 |
| 4 | Australia | 55 | 4.59 | 1004 | 18.25 | 15 |
| 5 | China Mainland | 38 | 3.17 | 274 | 7.21 | 13 |
| 6 | Scotland | 36 | 3.01 | 631 | 17.53 | 9 |
| 7 | Netherlands | 30 | 2.51 | 590 | 19.67 | 17 |
| 8 | Sweden | 23 | 1.92 | 300 | 13.04 | 9 |
| 9 | Brazil | 20 | 1.67 | 205 | 10.25 | 2 |
| 10 | Ireland | 20 | 1.67 | 250 | 12.50 | 5 |
| 11 | Denmark | 20 | 1.67 | 330 | 16.50 | 9 |
| 12 | Saudi Arabia | 18 | 1.50 | 95 | 5.28 | 5 |
| 13 | Israel | 16 | 1.34 | 216 | 13.50 | 6 |
| 14 | South Africa | 16 | 1.34 | 175 | 10.94 | 9 |
| 15 | Spain | 15 | 1.25 | 92 | 6.13 | 3 |
| 16 | Germany | 14 | 1.17 | 208 | 14.86 | 4 |
| 17 | Wales | 13 | 1.09 | 627 | 48.23 | 4 |
| 18 | Norway | 13 | 1.09 | 228 | 17.54 | 3 |
| 19 | Singapore | 13 | 1.09 | 169 | 13.00 | 8 |
| 20 | Hong Kong | 12 | 1.00 | 133 | 11.08 | 3 |
| Rank | Institutions | TA | TPR% | TC | ACPP | H-Index | Country |
|---|---|---|---|---|---|---|---|
| 1 | University of London | 69 | 5.80 | 2571 | 37.26 | 20 | England |
| 2 | Harvard University | 53 | 4.43 | 1927 | 36.36 | 18 | USA |
| 3 | University of California System | 36 | 3.00 | 530 | 14.72 | 14 | USA |
| 4 | University College London | 35 | 2.92 | 1096 | 31.31 | 13 | England |
| 5 | University of Texas System | 30 | 2.51 | 506 | 16.87 | 11 | USA |
| 6 | University of North Carolina | 29 | 2.42 | 1000 | 34.48 | 13 | USA |
| 7 | Massachusetts General Hospital | 23 | 1.92 | 483 | 21.00 | 11 | USA |
| 8 | Johns Hopkins University | 19 | 1.59 | 613 | 32.26 | 11 | USA |
| 9 | Duke University | 18 | 1.50 | 357 | 19.83 | 9 | USA |
| 10 | Pennsylvania Commonwealth System of Higher Education | 18 | 1.50 | 281 | 15.61 | 8 | USA |
| 11 | University of North Carolina Chapel Hill | 17 | 1.42 | 515 | 30.29 | 9 | USA |
| 12 | University of Pennsylvania | 17 | 1.42 | 436 | 25.65 | 9 | USA |
| 13 | State University System of Florida | 17 | 1.42 | 237 | 13.94 | 7 | USA |
| 14 | University of Michigan System | 17 | 1.42 | 215 | 12.65 | 8 | USA |
| 15 | Imperial College London | 17 | 1.42 | 1260 | 74.12 | 10 | England |
| 16 | Kings College London | 17 | 1.42 | 453 | 26.65 | 9 | England |
| 17 | University of Michigan | 16 | 1.34 | 213 | 13.31 | 8 | USA |
| 18 | Columbia University | 16 | 1.34 | 599 | 37.44 | 11 | USA |
| 19 | US Department of Veteran Affairs | 16 | 1.34 | 198 | 12.38 | 8 | USA |
| 20 | University of Toronto | 15 | 1.25 | 202 | 13.47 | 8 | Canada |
| Rank | Journals | TA | TPR% | TC | ACPP | IF |
|---|---|---|---|---|---|---|
| 1 | BMC Health Services Research | 21 | 1.75 | 215 | 10.24 | 1.93 |
| 2 | European Journal of Operational Research | 17 | 1.42 | 300 | 18.75 | 3.81 |
| 2 | Production and Operations Management | 17 | 1.42 | 354 | 20.82 | 2.17 |
| 3 | British Journal of General Practice | 16 | 1.34 | 401 | 25.06 | 4.43 |
| 5 | British Dental Journal | 16 | 1.34 | 157 | 9.81 | 1.44 |
| 6 | Journal of General Internal Medicine | 14 | 1.17 | 585 | 41.79 | 4.61 |
| 7 | International Journal of STD & AIDS | 11 | 0.92 | 111 | 10.09 | 1.50 |
| 8 | BMJ Open | 10 | 0.84 | 33 | 3.30 | 2.38 |
| 9 | PLoS One | 9 | 0.75 | 68 | 7.56 | 2.78 |
| 10 | American journal of Orthodontics and Dentofacial Orthopedics | 9 | 0.75 | 179 | 19.89 | 1.91 |
| 11 | AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV | 9 | 0.75 | 248 | 27.56 | 2.11 |
| 12 | Obesity Surgery | 9 | 0.75 | 222 | 24.67 | 3.60 |
| 13 | Psychiatric Services | 9 | 0.75 | 260 | 28.89 | 2.25 |
| 14 | Transportation Science | 8 | 0.67 | 379 | 47.38 | 3.31 |
| 15 | Manufacturing & Service Operations Management | 8 | 0.67 | 289 | 36.13 | 2.67 |
| 16 | Health Care Management Science | 8 | 0.67 | 71 | 8.88 | 2.06 |
| 17 | Journal of The Operational Research Society | 8 | 0.67 | 115 | 14.38 | 1.75 |
| 18 | Journal of The Royal Society Medicine | 8 | 0.67 | 285 | 35.63 | 3.54 |
| 19 | Journal of The American College of Radiology | 8 | 0.67 | 33 | 4.13 | 3.79 |
| 20 | Family Practice | 7 | 0.58 | 368 | 52.57 | 1.99 |
| Rank | Author | TA | TPR% | TC | ACPP | H-Index | Affiliation |
|---|---|---|---|---|---|---|---|
| 1 | Tang, Jiafu | 7 | 0.58 | 32 | 4.57 | 3 | Dongbei University of Finance & Economics Northeastern University–China |
| 2 | Yan, Chongjun | 7 | 0.58 | 19 | 2.71 | 3 | Dongbei University of Finance & Economics Northeastern University—China |
| 3 | Lawley, Mark | 7 | 0.58 | 225 | 32.14 | 5 | Purdue University |
| 4 | Muthuraman, Kumar | 6 | 0.50 | 205 | 34.17 | 4 | University of Texas Austin |
| 5 | Jiang, Bowen | 6 | 0.50 | 19 | 3.17 | 3 | Northeastern University—China |
| 6 | Huang, Y. | 6 | 0.50 | 33 | 5.50 | 3 | New Mexico State University Mayo Clinic |
| 7 | Cayirli, Tugba | 5 | 0.42 | 145 | 29 | 3 | Ozyegin University |
| 8 | Ziya, Serhan | 5 | 0.42 | 243 | 48.60 | 4 | University of North Carolina Chapel Hill |
| 9 | Qu, Xiuli | 5 | 0.42 | 54 | 10.80 | 5 | North Carolina A&T State University |
| 10 | Shi, Jing | 5 | 0.42 | 48 | 9.60 | 5 | North Dakota State University Fargo |
| 11 | LaGanga, Linda R. | 5 | 0.42 | 305 | 61 | 4 | Mental Health Center of Denver |
| 12 | Ellis, David A. | 5 | 0.42 | 37 | 7.40 | 4 | Lancaster University University of Glasgow |
| 13 | Car, Josip | 5 | 0.42 | 359 | 71.80 | 4 | Imperial College London University of Ljubljana |
| 14 | Yang, Kum Khiong | 5 | 0.47 | 72 | 14.4 | 2 | Singapore Management University National University of Singapore |
| 15 | Denton, Brian T. | 4 | 0.47 | 83 | 20.75 | 3 | University of Michigan |
| 16 | Kulkarni, Vidyadhar G. | 4 | 0.47 | 160 | 40 | 3 | University of North Carolina Chapel Hill |
| 17 | Sockalingam, Sanjeev | 3 | 0.25 | 58 | 19.33 | 2 | University of Toronto |
| 18 | Bard, Jonathan F. | 3 | 0.25 | 8 | 2.67 | 2 | University of Texas Austin |
| 19 | Percac-Lima, Sanja | 3 | 0.25 | 45 | 15 | 3 | Harvard University Massachusetts General Hospital |
| 20 | Williamson, Andrea E. | 3 | 0.25 | 33 | 11 | 3 | University of Glasgow |
| Rank | Author(PY) | Title | Journal | TC | TCY |
|---|---|---|---|---|---|
| 1 | Free et al. (2013) [14] | The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis | PLoS Medicine | 904 | 129.14 |
| 2 | Mani et al. (2013) [30] | Poverty impedes cognitive function | Science | 575 | 82.14 |
| 3 | Krishna et al. (2009) [32] | Healthcare via cell phones: a systematic review | Telemedicine Journal and E-Health | 504 | 45.82 |
| 4 | Menon et al. (2009) [31] | Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) | Lancet Oncology | 485 | 44.09 |
| 5 | Karter et al. (2001) [33] | Self-monitoring of blood glucose levels and glycemic control: The Northern California Kaiser Permanente diabetes registry | American Journal of Medicine | 373 | 19.63 |
| 6 | Gupta et al. (2008) [1] | Appointment scheduling in health care: Challenges and opportunities | IIE Transactions | 365 | 30.42 |
| 7 | Macharia et al. (1992) [34] | An overview of interventions to improve compliance with appointment keeping for medical-services | Journal of The American Medicine Association | 234 | 8.36 |
| 8 | Beach et al. (2006) [35] | Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? | Journal of General Internal Medicine | 217 | 15.50 |
| 9 | Syed et al. (2013) [36] | Traveling Towards Disease: Transportation Barriers to Health Care Access | Journal of Community Health | 210 | 30.00 |
| 10 | Rhee et al. (2005) [37] | Patient adherence improves glycemic control | Diabetes Educator | 194 | 12.93 |
| 11 | Leong et al. (2006) [38] | The use of text messaging to improve attendance in primary care: a randomized controlled trial | Family Practice | 180 | 12.86 |
| 12 | Killaspy et al. (2000) [39] | Prospective controlled study of psychiatric out-patient non-attendance - Characteristics and outcome | British Journal of Psychiatry | 178 | 8.90 |
| 13 | Yu et al. (2007) [40] | True outcomes for patients on antiretroviral therapy who are “lost to follow-up” in Malawi | Bulletin of The World Health Organization | 177 | 13.62 |
| 14 | Swofford et al. (1996) [41] | Substance use: A powerful predictor of relapse in schizophrenia | Schizophrenia Research | 172 | 7.17 |
| 15 | Lacy et al. (2004) [42] | Why we don’t come: Patient perceptions on no-shows | Annal of Family Medicine | 170 | 10.63 |
| 16 | Subramanian et al. (1999) [12] | Airline yield management with overbooking, cancellations, and no-shows | Transportation Science | 170 | 8.10 |
| 17 | Gurol et al. (2013) [43] | Mobile phone messaging reminders for attendance at healthcare appointments | Cochrane Database of Systematic Reviews | 164 | 23.43 |
| 18 | Satterthwaite et al. (2014) [44] | Neuroimaging of the Philadelphia Neurodevelopmental Cohort | Neuroimage | 159 | 26.50 |
| 19 | Gallacher et al. (2011) [45] | Understanding patients’ experiences of treatment burden in chronic heart failure using normalization process theory | Annals of Family Medicine | 157 | 17.44 |
| 20 | Junghans et al. (2005) [46] | Recruiting patients to medical research: double blind randomised trial of “opt-in” versus “opt-out” strategies | British Medical Journal | 157 | 10.47 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.; Wu, R.; Deng, L.; Chen, Y.; Li, Y.; Wan, Y. A Bibliometric Analysis on No-Show Research: Status, Hotspots, Trends and Outlook. Sustainability 2020, 12, 3997. https://doi.org/10.3390/su12103997
Wang C, Wu R, Deng L, Chen Y, Li Y, Wan Y. A Bibliometric Analysis on No-Show Research: Status, Hotspots, Trends and Outlook. Sustainability. 2020; 12(10):3997. https://doi.org/10.3390/su12103997
Chicago/Turabian StyleWang, Cheng, Runhua Wu, Lili Deng, Yong Chen, Yingde Li, and Yuehua Wan. 2020. "A Bibliometric Analysis on No-Show Research: Status, Hotspots, Trends and Outlook" Sustainability 12, no. 10: 3997. https://doi.org/10.3390/su12103997
APA StyleWang, C., Wu, R., Deng, L., Chen, Y., Li, Y., & Wan, Y. (2020). A Bibliometric Analysis on No-Show Research: Status, Hotspots, Trends and Outlook. Sustainability, 12(10), 3997. https://doi.org/10.3390/su12103997





