Abstract
When urgent situations occur (e.g., inaccurate demand forecast, traffic accidents, or infectious disease outbreaks), the stock of rescue medical items in the hospital might not be enough to cater to the drastically increased demand. Comparing with placing an expensive emergent replenishment order with dealers, requesting inventory sharing from another hospital with excessive stocks could save time and cost. This paper investigates the operation of the inventory sharing mechanism between two independent hospitals with the consideration of patient behavior. We first identified the inventory decisions when hospitals are under a no-sharing scenario, and derive hospitals’ sharing policies and inventory policies under the sharing scenario. Through numerical experiments, we found that the inventory sharing option is profitable for hospitals compared to emergent replenishment. Furthermore, we investigated the effects of patient behavior, safety inventory level of the hospital, and other cost parameters on inventory decisions. Under the sharing policy, the increase of hospital j’s emergent request rate and safety inventory level increased the optimal initial inventory level of hospital i, while the increase of hospital j’s initial inventory level decreased the optimal inventory level of hospital i. This paper provides more practical suggestions for hospitals’ inventory sharing operation.
1. Introduction
Compared with industrial products, inventory management in a hospital is more difficult to manage as the demand for medical items is difficult to predict and critical to patients. Natural disasters, massive traffic accidents, and infectious disease outbreaks bring a steep increase of emergent patients and increase the difficulty in order-related decision-making for hospitals. The occurrence of medical inventory stockout is not rare, especially for disposable medical equipment such as sanitary materials, disposable medical gloves, disposable infusion/blood transfusion, medical textiles, surgical instruments, disposable catheters, vascular surgical instruments, anesthesia instruments, obstetric instruments, oxygen masks, and other necessities [1]. Besides, bed utilization is generally high when urgent situations occur, and some small hospitals cannot provide enough beds for patients. For example, in Hong Kong, the bed utilization of some public hospitals reaches 120% in flu outbreak season such that patient transfer between hospitals may further affect the medical service offered to patients. In such situations, the demand for medical items at a hospital increases suddenly, and stockout occurs because the regular safety stock in a hospital cannot handle such a demand increase [2]. Unlike industrial products, stockout of critical medical supplies may result in a life-threatening situation for patients, thus the hospital tries to ensure an adequate quantity of various medical supplies is available, even in unanticipated situations [3,4]. However, the inventory holding cost is high if hospital stocks a large number of various medical items. Wang et al. [5] mention that inventory cost is a major component among all expenses in a hospital. To reduce the inventory cost, hospitals always choose expensive and emergent replenishment to address the stockout problem. Emergent replenishment can guarantee immediate supply, but requires that the hospital pay a higher price and an additional delivery charge. Therefore, there are currently some management issues regarding the medical inventory system. (1) Because of high inventory holding cost and limited warehouse capacity, hospitals face practical limitations to stocking a large volume of inventory. To satisfy the sudden demand caused by massive accidents, the hospital can only adopt an expensive emergent replenishment policy. From a financial perspective, this is not an economical inventory policy as it incurs higher purchase price and expensive delivery charges. (2) When one hospital faces stockout on some medical items due to unexpected events, another hospital located nearby may be holding idle inventory that incurs an inventory holding cost. Hence, for hospitals, it is critical to explore more effective inventory policies to mitigate the risk of stockout with a lower operating cost [6,7,8].
Based on the above medical inventory management problems, we propose a sharing mechanism for disposable medical inventories between two cooperative hospitals. Inventory sharing in the traditional supply chain has received some attention, but its application in the hospital setting is rare. However, medical inventory sharing is feasible for hospitals. When a huge traffic accident happens or there is an infectious disease outbreak in a region, the local hospitals may anticipate medical inventory stockout; at that time, it is possible that hospitals in other regions are keeping enough inventory. Based on the setting, inventory sharing can be conducted when one hospital has excess demand and another hospital has excess inventory. Additionally, compared with transferring patients, sharing inventory is more feasible and cost-saving since patient transfer may worsen their health conditions and delay treatment. Second, medical inventory sharing is more specialized than retail inventory sharing. In contrast to customer demands, patients’ demands cannot be backlogged, which means patients’ behaviors or actions have a greater effect on hospitals’ decisions. For example, for an unsatisfied customer, a retailer may compensate the customer in the future. However, for unsatisfied patients, a hospital should make replenishment decisions or request possible sharing to fulfill patients’ demands according to patients’ actions.
Our paper proposes a two-period inventory sharing model between two decentralized hospitals, where they make independent inventory decisions in each period. At the beginning of each period, these two hospitals place a regular replenishment order for the next period according to demand forecast information. Demand realization also happens at the beginning of each period. Then, the hospitals fulfill the demand by a regular order placed in the last period together with the inventory carried forward from the last period. If stockout is anticipated to occur, the hospital takes actions according to patient behavior. For example, some patients choose to “stay in” the hospital and wait for needed service (i.e., emergent request rate), and some patients leave the hospital. In our paper, we mainly focus on emergent patients and the mentioned “patient behavior” denotes the actions of emergent patients. Since elective patients make appointments in advance, their demands can be forecasted by hospitals. Emergent patients arrive at hospital randomly. It is a common phenomenon that less-urgent patients give up waiting and turn to another hospital, especially in flu season when medical inventory stockout happens frequently. To satisfy the requests of “stay in” patients, the hospital makes emergent orders to dealers or requests inventory sharing to the partner hospital according to the transaction cost to be incurred. If emergent replenishment is preferred, the regular inventory decisions of the two hospitals are not influenced by each other. If inventory sharing is preferred, then the partner hospital decides the sharing quantity according to multiple factors, including its own demand and the safety inventory level. The inventory sharing mechanism benefits both hospitals intuitively: (1) If inventory sharing is adopted, for the hospital that facing stockout, it saves the emergent procurement cost. For the hospital with excessive inventory, it saves some inventory holding cost by sharing inventories to the partner hospital. (2) The resource utilization rate of medical supplies is enhanced from the perspective of social sustainability. However, when the inventory sharing policy is more profitable than emergent replenishment policy, how the hospitals decide order quantities with the sharing option, and whether there is an interaction in their decisions when considering patient behavior still need further investigation.
In the next sections, we study three problems in disposable inventory sharing for a single item between two hospitals. (1) When a stockout on some disposable medical items happens, what is the best response for the hospital—to place an emergency order or to request sharing? (2) In each period, what is the optimal regular replenishment quantity and the optimal inventory order-up-to level for the next period’s consumption? (3) How are the stockout response decision and optimal order-up-to level affected by the cost features of the hospital and patient behavior? Park et al. [9] present a model that addresses the first and second issues in a similar setting. They study the multi-period inventory sharing problem in the spot and forward market, in which a firm facing excessive demand can either purchase from the spot/forward market or send a sharing request to other firms. Meanwhile, the firm that has excess inventory can sell to the spot/forward market or accept another firm’s request. Equilibrium strategies of two firms are investigated and a structured transshipment pricing scheme is developed to increase the value of inventory sharing. Their work and ours both assume that the demand cannot be backlogged and needs to be satisfied immediately (no delay) by the spot market (“emergent replenishment” in our paper) or sharing. The main difference between their work and ours lays in their focus on the sharing price structure, and we assume that sharing price equals the regular replenishment price. In addition, we extend their model by considering the effects of patient behavior, safety inventory level on sharing decision, and the mutual effect on inventory decisions between two cooperative hospitals.
This study explores the optimal equilibrium inventory policy under different scenarios and analyzes the effects of patients’ emergent replenishment request rate and the safety inventory level on hospitals’ inventory decisions. The rest of the paper is structured as follows. Section 2 reviews related literature on inventory sharing and inventory transshipment and shows the main contribution of our work. Section 3 describes the background and setting of our model. Section 4 and Section 5 analyze the emergent replenishment/emergent sharing decision as well as the optimal inventory policy under the no-sharing case and under the sharing case, respectively. Then, we discuss the preliminary results by several numerical experiments in Section 6 and summarize conclusions in Section 7.
2. Literature Review
Our model setting considers a distinctive feature: inventory sharing of medical supply between two hospitals. As there is very little literature on inventory sharing in the hospital setting, we review literature mainly in three relevant categories: (1) inventory sharing literature in the setting of industry or enterprise; (2) inventory transshipment, which is similar to the concept of inventory sharing in the operations perspective; and (3) research on healthcare materials and logistics management. The corresponding literature is summarized in more detail below.
The first stream of literature is relevant to inventory sharing, which includes several common considerations: priorities of demand classes (high priority and low priority), single period or multiperiod, and sharing between two parties or among multiple parties. Zhao et al. [10] consider the inventory sharing problem in a decentralized dealer network where each dealer faces high-priority demand and low-priority demand. They address two main issues. The first issue is, when one dealer accepts the sharing request of another dealer, which dealer should place a replenishment order to their common manufacturer? The second problem is about how to determine the amount of replenished inventory for each dealer after sharing their inventory. It is found that there exists a pure-strategy equilibrium under the full-inventory-sharing game and fixed-portion-sharing game. In their work, the unsatisfied sharing request can be backlogged if it is rejected and the rejected request is supposed to be made up later. In contrast to their model setting, we assume that unsatisfied demand cannot be backlogged. Once the sharing request is rejected, the hospital that anticipates stockout needs to place an emergent replenishment order, which fits the hospital setting. Based on the two-dealer sharing problem, Yan and Zhao [11] develop a multi-dealer (n > 2) inventory sharing mechanism, where n dealers make their replenishment decisions independently but share inventory cooperatively. In the case of asymmetric demand information, the effects of complete information sharing and no information sharing on the coordination mechanism are respectively analyzed. This study provides insights on coordinating a multi-dealer inventory sharing mechanism when considering asymmetric information. Yan and Zhao [12] also consider the effects of asymmetric information on inventory sharing in a decentralized system. To induce the truth in inventory sharing between retailers, a coordination mechanism is proposed for the sharing relationship between manufacturer and retailer to achieve the maximal benefit. Park et al. [9] consider the multi-period inventory sharing problem in the spot and forward market. They develop optimal equilibrium strategies of two firms and construct a structured transshipment pricing mechanism to benefit from inventory sharing.
The second relevant category of literature concerns the inventory transshipment problem. Inventory transshipment implies transferring inventory from one location to another when a retailer has excess demand of a certain inventory item and another retailer has excess inventory of the same item. However, due to long procurement lead time and the difficulty of predicting demand in some industrial operations, transshipment becomes a routine activity to better match supply and demand. In general, transshipment occurs when demands are observed/realized and before they are satisfied [13]. Transshipment is investigated under two different inventory distribution systems—centralized and decentralized. Under the centralized system, a centralized decision maker (supplier/distributor) makes a replenishment and transshipment decision among retailers aiming at maximizing the total profits of all retailers in the system. While in a decentralized system, each retailer makes replenishment and transshipment decisions independently, aiming at maximizing their own profit. The literature on these two categories of transshipment is summarized as follows. Earlier research studies focus on the inventory transshipment problem under a centralized setting. Tagaras [14] proposes the optimal ordering and transshipment policy for a two-location centralized system. Robinson [13] considers the multi-period inventory problem with transshipment among multiple locations. From previous research outputs, Dong and Rudi [15] consider which party benefits more from transshipment under a centralized distribution system when a common manufacturer serves multiple retailers. Then, the impact of transshipment on retailers and manufacturer are compared under two cases—that is, where the manufacturer is a wholesale price setter or a wholesale price taker. Liao et al. [16] tackle a similar inventory transshipment problem in an industrial setting; they compare the options of lateral transshipment and placing an emergent order when stockout occurs for one retailer. In their study, making an emergent order is expensive and needs more time, while lateral transshipment between two retailers saves some cost and time. The authors propose several optimal inventory response policies for different scenarios under a single-period setting. In addition, the effects of customer behavior on inventory decision are considered in the model, such as customer request rate and rate of switching to another store. However, there are two main differences between their work and our study. They investigate the inventory transshipment between two centralized retailers under a single-period setting, while we explore the sharing problem between two decentralized hospitals under a two-period setting. There are some studies about decentralized inventory transshipment. Anupindi et al. [17], Granot and Sošić [18], and Slikker et al. [19] mainly study the transshipment problem in a decentralized distribution system using cooperative game theory and aim at obtaining Nash equilibrium on the inventory decision. Besides, Rudi [20] consider two independent inventory locations and examine the effects of intrafirm transshipment and interfirm transshipment on optimal inventory choice. In their paper, the intrafirm transshipment is the inventory transshipment under a centralized system while interfirm transshipment is equivalent to transshipment under a decentralized system. After comparing these two cases, it is found that when each retailer makes an inventory decision to maximize its independent profit, the joint profit of a centralized system cannot be realized. Zhao et al. [21] study two issues about emergent transshipment among multiple independent dealers under a decentralized system. When one dealer faces stockout, the first problem is when to send a transshipment request to another dealer with excess inventory (requesting decision), and the second problem is when the dealer with excess inventory fills the request (filling demand decision). It is proved that the transshipment decision can be determined by a threshold rationing policy. Hu et al. [22] generalize the study of Rudi [20]. They prove that the conclusion that a transshipment price always exists is wrong by a counterexample, and explore the sufficient and necessary conditions under which the transshipment price does exist. Hanany et al. [23] propose a new transshipment coordination mechanism, in which a third-party coordinates the inventory transshipment among multiple independent and noncooperative retailers. The aforementioned research works consider a single transshipment problem under decentralized policy, but we examined how to construct a sharing mechanism when there is an emergent replenishment option.
Because our paper focuses on hospital inventory replenishment and transshipment, we also review literatures about hospitals’ materials and logistics management. Volland et al. [24] provide a detailed survey to summarize the previous research on hospitals’ logistics problems. Wieser [25] concentrate on healthcare logistics optimization. They also suggest considering the service level of patients in operational practice, such as the service quality, traceability, and information system. Kritchanchai and MacCarthy [26] investigate the application of vendor-managed inventory (VMI) in the pharmaceutical transportation for hospitals, while Kritchanchai et al. [27] analyze the performance of healthcare logistics from the perspective of purchasing and supply policy, warehousing, inventory management, transportation and distribution, and information and technologies. Scholars also propose incorporating the behavior of healthcare personnel when optimizing the medical inventory transportation efficiency. For instance, Stefanini et al. [28] consider the behaviors of medical staff and health managers when developing resource planning strategies for lung cancer patients. In addition, Adida et al. [29] explore the hospital stockpiling policy for disaster prevention, which is a proactive inventory transshipment policy before the disaster happens. In contrast to their work, our paper analyzes the emergency inventory sharing policy for hospital stockout, which is a reactive inventory transshipment policy after the stockout happens. Another difference is that Adida et al. [29] only focus on the stockpile decision-making and neglect hospitals’ safety stock, while our paper explores the sharing decision-making when considering the effects of hospitals’ safety stock level. Most importantly, we also investigate the impacts of patients’ behavior on hospitals’ inventory decisions.
Therefore, although there are some studies on the inventory transshipment or sharing issue, our research is different from previous studies in the following ways: (1) the demand for disposable medical inventory cannot be backlogged in a hospital setting; (2) it is under a two-period setting; (3) it is in a decentralized system, where two hospitals operate independently; (4) it proposes the sharing mechanism when an emergent replenishment option is available; (5) it also investigates the effects of patients’ behavior and safety inventory level on sharing decisions.
3. Model Formulation
We consider the sharing problem of a single item inventory in two cooperative hospitals i and j () in a time horizon of T periods. Each hospital faces independent stochastic demand and , with probability density function , and distribution function , in period t. In a hospital setting, the demand for medical items should be satisfied within the same period and cannot be backlogged to the next period. Daily demand includes appointment patients and emergent patients. Emergent patient demand is difficult to forecast, and therefore stockout happens occasionally. In the following section, we assume that hospital i faces stockout and hospital j has adequate inventory in period t; the opposite case is symmetric.
For some medical items, hospitals apply a periodic review policy and make replenishment decisions at the beginning of each period. Since the lead time of regular replenishment is one period (i.e., the order is placed in period , with order amount , and the order is received at the beginning of period t), hospital i can only use the inventory carried forward and the amount ordered in period to fulfill the demand in period t. If stockout happens, the hospital chooses either emergent replenishment or inventory sharing from the cooperative hospital in consideration of the related cost of these options. In general, the hospital pays a higher price and transportation cost for emergent replenishment. If the inventory sharing request is accepted by the partner hospital, the hospital with excess demand needs to bear the transshipment cost. Considering the specialty of patient demands and medical inventory in a hospital setting, the hospital is risk-averse compared with commercial organizations. Hence, we take the safety inventory level into consideration, which is a fraction of the order-up-to level . The partner hospital j will reject any inventory sharing request when its on-hand inventory level is lower than its safety inventory level. In general, two cooperative hospitals are willing to share with each other when one hospital faces stockout and the partner hospital has enough inventory in excess of the safety stock level. In addition, we consider the patient behavior in our model. When stockout happens in a hospital, some patients may decide to leave the hospital, while others stay and wait for emergent service until replenishment inventory arrives. We use the emergent request rate to denote the rate of patients that stay in hospital. (i.e., ) patients are willing to wait in hospital i in period t when stockout of medical items happens. Hospitals have unique . For instance, for a large and famous hospital which offers better service, the corresponding is high, patients are more willing to stay in the hospital waiting for service. In contrast, for a hospital in a central location where many other hospitals are located nearby, the corresponding is low because patients may choose another hospital.
In each time period, the sequence of events is illustrated as follows (taking hospital i as an example). At the beginning of period t, the hospital receives the regular replenishment order and observes the order-up-to level . Meanwhile, the hospital realizes demand as well as the regular replenishment price and emergent replenishment price . We define and to represent the demand and initial inventory level for hospital i and j in period t respectively. Then, if stockout occurs in hospital i, hospital i will either place an emergent replenishment order from the dealer or request sharing from partner hospital j according to the operating costs. Under the emergent replenishment policy, the hospital needs to pay and as emergent procurement and transportation cost, respectively. Under the inventory sharing policy, the partner hospital j can share excess inventory with hospital i at regular replenishment price , but the sharing amount is determined by the request level of i, the internal demand of j, and safety inventory . Hospital i also pays as transshipment cost in the sharing process. After demand is satisfied, the remaining inventory is carried forward to the next period with holding cost h. Note that hospital j can save relative holding cost in period t by sharing its inventory. We supposed that hospital i will return the sharing inventory to hospital j in the next period and ignore the unpunctual return issue in this paper. In addition, we assumed that , , and in order to prevent a hospital from always choosing to request sharing instead of making regular replenishment orders to their dealer. We set in the numerical experiments to prove that inventory sharing may still occur even if the sharing transportation cost is higher than the emergent transportation cost. The savings from emergent purchase price and inventory holding cost is enough to outweigh the additional transportation cost.
We define the following notations applied in our model in Table 1.

Table 1.
Notations in the model.
In the remaining sections of this paper, we first analyze the emergent replenishment order policy with no inventory sharing, and we use superscript “e” to denote the policy. Then, we suggest a sharing policy that combines sharing action and emergent replenishment policy, represented by superscript “s”. Under these two policies, we aim at obtaining an optimal sharing/emergent replenishment order amount and optimal regular replenishment amount in the current period as well as the optimal order-up-to level at the beginning of the next period. In addition, we investigate the effects of hospital safety stock level and patients’ emergent request rate on the choices of optimal inventory policy. Finally, we explore the response function of one hospital to their partner hospital on the optimal inventory order-up-to level in a sharing mechanism.
4. Benchmark Case: Inventory Policies without Sharing
Before considering the sharing mechanism, we first analyzed the no sharing case as benchmark. Under this case, each hospital is independent and makes inventory decisions independently to minimize the expected cost of the next period. When stockout is anticipated to occur, the emergent replenishment policy is executed. denotes the total expected cost in period t.
where and represent the expected cost when stockout happens and when no stockout happens, respectively. The logic of the two-stage solution is, in period , hospital i determines the regular replenishment quantity and aims at minimizing the expected cost of period t. If stockout happens in period t, unsatisfied demand is fulfilled by emergent order. Therefore, we explore the order-up-to level which arrives at the beginning of period t (i.e., at the end of period ) that minimizes for hospital i under the emergent replenishment policy. More model setting details are attached in the Appendix A (Proof of Proposition 1).
Proposition 1.
Under the no sharing case, for hospital i, given and , increases as increases.
For the hospital, the emergent demand from patients cannot be backlogged to the next period and should be satisfied in the current period. Therefore, when a stockout is anticipated in hospital i, if is high (which means more emergent patients choose to stay and wait for medical supply), then the hospital needs to place a larger emergent order. We provide the proof of following propositions in the Appendix A.
Proposition 2.
Under the no sharing case, the expected cost of hospital i, , increases as increases. In period , there exists a unique that minimizes when .
Under the emergent replenishment policy, the emergent request rate increases the total operating cost of the hospital. If stockout happens in period t, a higher percentage of patients are willing to wait for emergent medical supply, then the hospital needs to pay more to satisfy the demand in period t. When the hospital decides the regular replenishment quantity in period , a unique optimal order-up-to level can be determined to minimize the cost of hospital i only when the emergent request rate of patients .
5. Inventory Policies with Sharing
In this section, we consider the inventory sharing mechanism between two hospitals. Two hospitals form an alliance make inventory decisions independently and share inventory cooperatively. We assumed that the two cooperative hospitals are willing to share with each other in order to improve social welfare when the sharing action is beneficial to the alliance.
5.1. Safety Complete Sharing Policy
Taking the case where hospital i faces stockout and hospital j has sufficient inventory in period t as an example, when the demand of hospital i exceeds the order-up-to level in period t (), hospital i prefers to send a sharing request to their partner hospital j if sharing saves costs compared to placing an emergent replenishment order (). If hospital j accepts the request and shares excess inventory with hospital i, the inventory holding cost h is reduced in the current period—especially when the medical items have special storage requirements, the holding cost could be very high. However, hospital j does not empty its warehouse but keeps inventory as safety stock and makes a sharing decision rationally. When the two hospitals are centralized, the sharing incentive is wider (). Two corollaries are derived based on the sharing condition.
Corollary 1.
Under the sharing mechanism, the positive cost reduction of two hospitals increases in , h and decreases in .
Compared to the emergent replenishment policy, the cost reduction (profit) of the sharing policy mainly comprises the savings in transportation cost and inventory holding cost. Corollary 1 shows that the positive cost reduction of sharing action increases as the emergent replenishment transportation cost and holding cost increase. It decreases as the sharing transshipment cost increases.
Corollary 2.
The sharing mechanism has positive benefits only if .
We obtain , which means that there exists the case when (the transportation cost to share the inventory from hospital j to hospital i is more expensive than the emergent transportation cost from dealer to hospital i), the inventory sharing is more economical. Therefore, when stockout happens in a hospital, transportation cost is not always considered as top priority.
Developed from the complete pooling policy [14], we propose the safety complete sharing policy as a sharing rule for two cooperative hospitals in Proposition 3.
Proposition 3.
When stockout is anticipated in hospital i at period t, for :
- i.
- If , then .
- ii.
- If , then .
In our model, we consider the effect of safety stock level and patients’ emergent request rate on the sharing amount. Only when hospital j has surplus inventory after satisfying its internal demand does it have the capacity to share. The “complete” in our proposition means that when the hospital has excess inventory, it has ability to share completely. Under scenario (i), when the surplus inventory of hospital j is enough to cover the emergent request amount of hospital i, then the sharing amount is equal to the requested amount, and no emergent replenishment is needed. Under scenario (ii), hospital j is capable of satisfying the partial amount of hospital i’s sharing request due to insufficient excess inventory, so hospital i still needs to place an emergent replenishment order to satisfy the remaining demand.
5.2. Six Scenarios under the Sharing Case
When the sharing option is available, the continuous decision process is slightly different from the decision process of no sharing. If the sharing condition is satisfied, the hospital that faces stockout sends a sharing request to the partner hospital that has surplus inventory. Under the sharing mechanism, we first obtain the optimal sharing/emergent replenishment quantity, then we explore the optimal regular replenishment quantity for the next period. In our proposed model, the total expected cost of the two cooperative hospitals is set as the objective function. For example, in period , an order-up-to level is decided to minimize the total cost when is given. The expected total cost of the hospital alliance is denoted as . Following the cost structure and the decision logic under the emergent replenishment policy, we consider the sharing policy between two cooperative hospitals under the following six scenarios.
5.2.1. Scenario 1: ,
In this scenario, both hospital i and j have surplus inventory in period t, thus no sharing or emergent replenishment occurs. Both hospitals conduct inventory planning independently. At the beginning of period , the total expected cost of the hospital alliance is denoted as :
5.2.2. Scenario 2: , ,
In period t, hospital j has surplus inventory and hospital i has excess demand. Hospital i prefers inventory sharing instead of emergent replenishment to fulfill the emergent requesting patients. Meanwhile, the sharing quantity of j is enough to cover the requesting quantity of i, and thus the optimal sharing amount . The emergent replenishment amount is . Notice that if sharing occurs, the immediate cost structure changes since hospital i has to pay a sharing cost for transportation, denoted as . Hospital j saves the corresponding holding cost . The expected total cost of hospital i and j is denoted by in this case:
5.2.3. Scenario 3: , ,
In scenario 3, after keeping the safety stock, hospital j does not have enough inventory to satisfy the full amount requested by hospital i. Therefore, the optimal sharing amount and hospital i still places an emergent replenishment to the dealer for the remaining demand, that is, . The corresponding expected total cost is:
5.2.4. Scenario 4: , ,
The fourth scenario is symmetric to scenario 2, and the expected total cost can be represented as:
5.2.5. Scenario 5: , ,
The fifth scenario is a symmetric example of scenario 3, and the expected total cost is:
5.2.6. Scenario 6: ,
Scenario 6 shows that no inventory sharing occurs when both cooperative hospitals are facing stockout, and emergent replenishment is the only option. The emergent replenishment quantities of hospital i and j are and , respectively. Under this case, the expected total cost can be denoted by:
Combining the above six scenarios, the total expected cost of both hospitals under the inventory sharing mechanism is derived by the following equation:
The logic of the sharing policy is summarized as follows: inventory sharing only occurs when one hospital has excess demand and another hospital has excess inventory. For the hospital that receives a sharing request, if the surplus inventory is still more than the requested amount after maintaining sufficient safety stock, then it is optimal to fulfill the shortage of the partner hospital so as to minimize the total cost of both hospitals. In contrast, if the surplus inventory is not sufficient to fulfill the whole shortage amount, then it is optimal to share as much as possible and make up the remaining demand by emergent replenishment. Inventory sharing is a more efficient approach to allocate medical resources internally regardless of complete sharing or partial sharing.
We obtain more structural properties in the following propositions.
Proposition 4.
Under the sharing case, given and , the optimal increases as increases and decreases as increases.
For the hospital with excess demand, inventory sharing between the two cooperative hospitals is preferred when it saves more cost than emergent replenishment. Consider the case where hospital i faces stockout in period t and the partner hospital j has excess inventory. A higher increases the sharing amount when hospital j can cover all the shortage of hospital i. However, when hospital j can only fulfill the partial unsatisfied demand of hospital i, the final sharing amount depends on the safety stock requirement of hospital j. If hospital j keeps more safety stock, then the available sharing quantity is less. After obtaining the cost structure of the expected total cost of two cooperative hospitals under the inventory sharing mechanism, we aim at identifying the effects of patient’s behavior (emergent request rate) and hospital safety stock level on the expected total cost. The detailed observation is presented in Proposition 5.
Proposition 5.
Under the sharing case, for two cooperative hospitals, when , the optimal expected total cost increases as and increase. When , the optimal expected total cost increases as and increase.
With the mathematical proof, we find that only when does a higher or increase the total cost of the alliance. In general, for the alliance of two hospitals i and j, a higher or leads to a higher sharing amount/emergent replenishment amount as well as a higher total cost. However, if h is very high (), more holding cost is saved through the sharing mechanism and can offset some cost increase caused by increasing or , and the expected total cost may not increase as and increase. Similarly, only when is satisfied does a higher make hospital j share less inventory with hospital i, then hospital i spends more on emergent replenishment. Total cost increases as increases under the above condition. If is very high, , inventory sharing is not preferred for hospital i when stockout happens. Then, has no effect on sharing action and the expected total cost. Under this case, a higher total cost of the alliance is resulted by the emergent replenishment order placed by hospital i.
Proposition 6.
Under the sharing case, in each period , for two cooperative hospitals i and j, given , there exists a unique pair of order-up-to levels such that minimizes . When , has the following properties:
- i.
- increases as increases.
- ii.
- increases as increases.
- iii.
- decreases as increases.
Under the no sharing case, the inventory decisions in hospital j do not affect the inventory decisions of hospital i. However, in the sharing mechanism, the two hospitals form an alliance and aim at preventing stockout with a minimal total cost. Therefore, the emergent request rate of patients in hospital j, the safety stock level of hospital j, and the order-up-to quantity of hospital j impact the decision process of hospital i. Under the condition that , inventory sharing is preferred when stockout occurs in hospital i. However, if hospital i realizes that hospital j may face an increasing (which means hospital j needs more inventory to satisfy its internal demand), then hospital i will increase its inventory level in case of the stock out. On the other hand, if hospital i is informed that the safety stock level in hospital j increases (which means hospital j wants to keep more safety stock), the possible sharing amount to hospital i will decrease. Thus, hospital i can only increase in advance in case of expensive emergent replenishment. In addition, if inventory sharing is preferred for addressing stockout, when hospital j increases the inventory level , hospital i will decrease to avoid overstock.
6. Results and Discussion
In this section, we compare the two inventory policies (emergent replenishment policy and sharing policy) with various parameter settings (replenishment price, transportation cost, inventory handling cost, patients’ emergent request rate, and safety stock level of the hospitals) using numerical experiments. For simplicity, we denote the emergency replenishment policy as the no sharing policy. In our model setting, the decision process had Markov property, the decision in period t only depended on the decision in period , but was independent of any other previous periods. Therefore, we considered two periods to show the main results of our propositions when designing the experiments. This two-period model can be reiterated to a multiperiod setting. Our numerical experiments consisted of four components. The first part investigated the effects of emergency replenishment price and transportation cost on hospitals’ decisions and expected costs. In the second part, we explored the decision of optimal order-up-to level of hospitals under the two inventory policies. Then, in the third part, we compared the expected total cost of two hospitals when they are separated (under the no sharing policy) and in an alliance (under the sharing policy) to explore the cost reduction of the inventory sharing choice. In the final part, we investigated how hospital i determined the inventory order-up-to level according to the order-up-to level of hospital j.
In our numerical model, we assumed that the two hospitals faced stochastic demand, following a normal distribution with and standard deviation . Other parameters were: normal replenishment price for all t, emergent replenishment price in period t, per-unit transportation cost for regular replenishment , per-unit transportation cost for emergent replenishment , per-unit transportation cost for sharing , emergent request rate of hospital i, and safety stock rate of hospital i. Under the no sharing case, hospital i and hospital j are independent. For each hospital, the optimal inventory level depends on the demand forecast and the emergent request rate. Higher emergent request leads to higher emergent replenishment quantity and higher cost. Therefore, the impacts of on hospital i or on hospital j were not included in this experiment. Instead, we aimed to explore the effects of the emergent request rate of hospital j and the safety stock level of hospital j on the order-up-to level of hospital i under the sharing case. In the results, we denote the no-sharing policy as “N” and the sharing policy as “S”.
6.1. The Impacts of Emergent Replenishment Price and Transportation Cost
In our model, hospitals’ inventory decisions, sharing decisions, and the expected total cost are affected by many factors, including some internal factors (replenishment price, transportation cost, inventory handling cost, safety inventory level) and some external factors (patient demands, patient behaviors). We first explored the impacts of replenishment price and transportation cost using numerical experiments. Figure 1 shows that a higher emergent replenishment price increased hospitals’ total cost in the ordering process, and induced the inventory sharing action between hospitals. Figure 2a,b identifies the effects of emergent replenishment transportation cost and sharing transportation cost on hospitals’ ordering decisions respectively. Under the sharing mechanism, a higher emergent replenishment transportation cost had similar impacts to a higher emergent replenishment price—it increased the hospitals’ cost reduction compared to the no sharing mechanism. However, a higher sharing transportation cost decreased hospitals’ cost reduction compared to the no sharing mechanism. These results verify Corollary 1 well.
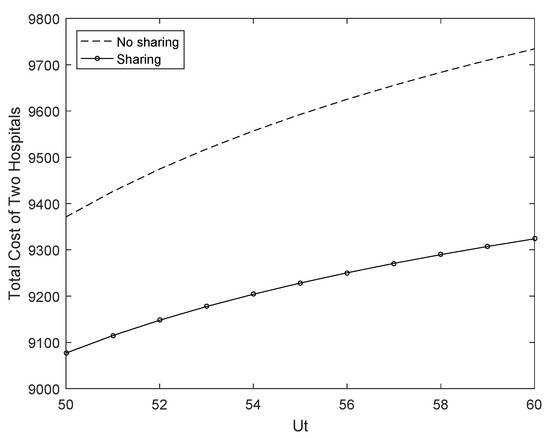
Figure 1.
The impacts of emergent replenishment price on hospitals’ total costs.
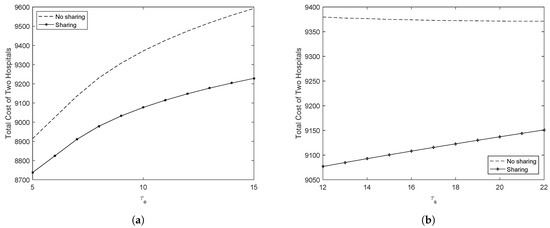
Figure 2.
The impacts of transportation cost on hospitals’ total costs. (a) The impacts of emergent replenishment transportation cost; (b) The impacts of sharing transportation cost.
6.2. The Optimal Order-up-to Levels of Hospitals
In this section, we explore the optimal order-up-to level of a hospital with and without the sharing option. Figure 3a shows that (a) under the no sharing policy, the optimal inventory level of hospital i was independent of the emergent request rate of hospital j. (b) Under the sharing policy, the optimal order-up-to level of hospital i increased as the emergent request rate increased, regardless of the holding cost. This means that when more patients requested emergent service in hospital j, then hospital j was not capable of sharing its inventory with hospital i. Hospital i could only increase the order-up-to level to reduce the risk of stockout. (c) Higher inventory holding cost decreased the optimal order-up-to level of both inventory policies. The explanation is intuitive—the hospital will decrease the order quantity for medical items with higher holding cost (e.g., some items needing cryopreservation) to minimize total inventory cost, especially when demand is uncertain. Figure 3b shows similar results to Figure 3a; by comparing two figures, it can be found that under the sharing policy, when the safety stock level of hospital j was higher , the corresponding order-up-to level of hospital i was slightly higher than that of the lower case . The main reason is that a higher safety stock level will decrease the sharing amount; hospital i that anticipates a stockout may not be satisfied by the sharing action and needs to improve the order-up-to level in advance.
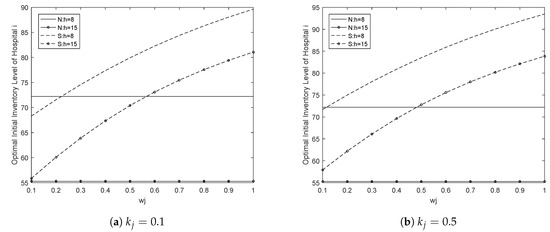
Figure 3.
Optimal order-up-to level of hospital i.
6.3. The Optimal Expected Total Cost of Hospitals
In the third part of the numerical experiments, we computed the expected total cost of hospitals under the two inventory policies. For the no sharing case, we considered the two hospitals separately and computed the sum of their expected cost. Hospital i determined its own optimal inventory level and the expected total cost unchanged by assuming was constant at . The cost of hospital j increased with increasing from to 1. Under the sharing case, we took the two hospitals as an alliance and computed the expected total cost of hospitals when increased from to 1. Figure 4 illustrates the following results: (a) When the per-unit holding cost was the same, the sharing policy saved more in costs than the no sharing policy, regardless of or . The results indicate that if the sharing condition is satisfied, inventory sharing is more economical than the no sharing policy (i.e., emergent replenishment). (b) In both no sharing and sharing cases, the optimal total cost increased as or increased (we only show the effects of here, as has a symmetric effect). When was small enough , we found that under the same policy, if h was higher, then the total cost was lower, since a higher holding cost encourages the hospital to order less (result from Figure 3). However, when was large enough , a higher h led to a higher total cost. Compared to the lower h case, hospital i provided less to hospital j and led to more under the higher h case. Therefore, under the same policy, if the emergent request rate is low, reducing the inventory level is economical for medical items with higher holding cost. However, if the emergent request rate is high, increasing the inventory level saves more cost.
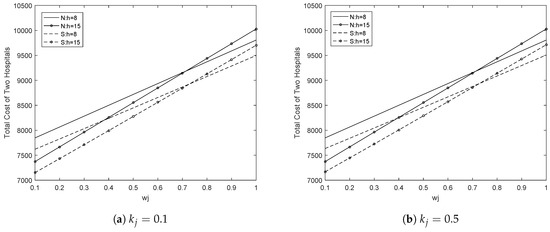
Figure 4.
Optimal expected total costs of the two hospitals.
Besides, under the sharing policy, the expected total cost increased as or increased (we only show the effects of , as has a symmetric effect). To show the slight difference between Figure 4a and b, we compared the expected percentage of cost reduction under the lower case and higher case . Figure 5 shows that hospitals in the sharing mechanism saved more in costs than in the no sharing mechanism when was lower. This is obvious, since if the sharing action is preferred, a higher safety stock level will decrease the sharing amount, and hospitals will satisfy the remaining demand by emergent replenishment, causing the the total cost to be higher.
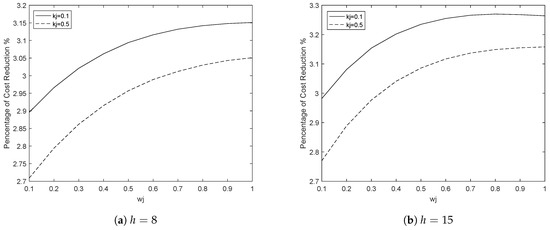
Figure 5.
Percentage of cost reduction for different .
6.4. The Response Inventory Decisions of Hospitals
This section investigates how the hospital responded to another hospital’s inventory decision under the sharing mechanism. Figure 6 presents the response inventory level of hospital i to hospital j with different values of . Under the sharing case, if inventory sharing is economical, one hospital will decrease the inventory level if the partner hospital increases its order-up-to level. This avoids the overstock problem at the hospital. Furthermore, when the emergent request rate of hospital j was higher, although hospital i had an incentive to decrease its order-up-to level as hospital j increased its inventory level, hospital i ordered more than that in the smaller case. Overall, compared to the no sharing case, the response policy in the hospital alliance improved the utilization rate of medical inventory.
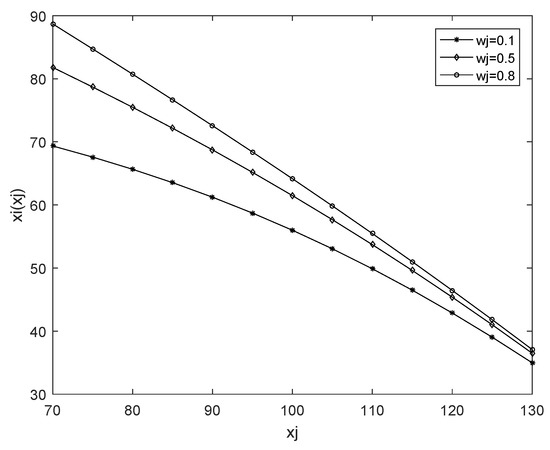
Figure 6.
The response order-up-to level of hospital i to hospital j.
7. Conclusions
This paper proposes a two-period inventory sharing model for two hospitals to address the inventory stockout problem. We first derived the emergent replenishment policy and optimal inventory order-up-to level for each hospital when there was no sharing option. Then we proposed an inventory sharing policy and obtained an optimal inventory order-up-to level when the two hospitals were cooperative. Furthermore, we explored the effects of patient’s emergent request rate and the safety stock level of the hospital as well as other cost parameters on the optimal inventory decision. It was found that when the sharing condition was satisfied, the inventory sharing policy was more economical than the no sharing policy (i.e., emergent replenishment policy). In the sharing case, the total expected cost of the two hospitals increased when one hospital’s emergent request rate and safety inventory level increased. The optimal order-up-to level of one hospital increased when the partner hospital’s emergent request rate increased, the partner hospital’s safety inventory level increased, or the partner hospital’s order-up-to level decreased.
In addition, the contribution of our paper is threefold: (1) it solves the stockout problem of medical items in hospitals; we propose a new inventory sharing mechanism and derive optimal inventory policies for two cooperative hospitals. The sharing policy benefits the alliance compared with the emergent replenishment policy. (2) Under the sharing policy, we investigated the impacts of patients’ behavior (emergent request rate), hospital safety inventory level, and other cost parameters on the inventory decisions. From the perspective of research novelty, our paper enriches the previous research on hospital operations management. (3) Our research scope is limited to a two-period inventory sharing model, but it can be extended to a multiperiod setting in other scenarios when the scenarios have the following features: demand updates in every period, and the inventory decision in one period only depends on the decisions of the previous period. Hence, our research could provide some guidelines for hospital operational practice.
Our research has some limitations in its research model and methodology, which can be considered in future work. First, although our mathematical model describes hospitals’ ordering process and inventory sharing process completely, it still neglects some complex characteristics in real healthcare operations, such as medical manager behaviors [28], the service level of patients [25], information asymmetry between the dealer and hospitals, and delivery reliability in transportation [26]. By considering these specific characteristics in the mathematical model, the research would provide more managerial insights for practice. Second, our research scope is in a two-hospital sharing setting. We will consider an n-hospitals inventory sharing problem and the sharing profit allocation problem among multiple hospitals in future research. Furthermore, in the current study, our sharing mechanism assumed that the borrowing hospital (requests sharing) would return the amount shared to the lending hospital (accepts a sharing request) in the next period. We will also consider the impacts of the unpunctual return problem on the sharing mechanism in further research.
Author Contributions
P.Z. proposed the theoretical framework and drafted the manuscript. H.Y. designed the numerical experiments and assisted in the mathematical proof. K.W.P. supervised the overall research progress and revised the manuscript.
Acknowledgments
The authors are very grateful to the anonymous referees for constructive suggestions to improve the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Proof of Proposition 1.
We first introduce more details in the benchmark case. In scenario 1: , we denote the total expected cost of hospital i as , which consists of two components. The first component is the cost of initial inventory (order-up-to level) , which represents the cost of the initial inventory, denoted by . The second component is the cost in period t, denoted by , which includes a single-period cost in period t and the expected cost of period . Therefore, and , for all . The immediate cost and .
Then, we obtain,
where represents the discount factor over one period and . Similarly, the expected cost of hospital i in scenario 2 is derived.
where represents the emergent replenishment order amount. Then is obtained in Section 4. □
Proof of Proposition 2.
Given ,
Thus, increases as increases.
if . Therefore, we notice that the above equation is positive, and is convex in when . □
Proof of Proposition 4.
We consider the cases where inventory sharing occurs:
in scenario 2, , , ,
in scenario 3, , , ,
In scenarios 4 and 5, taking the first derivative of with respect to , , we can draw similar conclusions. □
Proof of Proposition 5.
Given ,
Thus, if , the monotonicity maintains, increases as increases.
If , the monotonicity maintains, and increases as increases. The same result can be obtained by differentiating with respect to , . □
Proof of Proposition 6.
We note that if the above items are positive, then is convex in . When is unimodal, we have:
since and . Therefore, if is satisfied, is unique when is given (the proof is according to the proof of Proposition 1 in [20]).
We obtain that there exists a unique , which decreases as increases. When , increases as increases if . When , increases as increases if . □
References
- Lapierre, S.D.; Ruiz, A.B. Scheduling logistic activities to improve hospital supply systems. Comput. Oper. Res. 2007, 34, 624–641. [Google Scholar] [CrossRef]
- Saedi, S.; Kundakcioglu, O.E.; Henry, A.C. Mitigating the impact of drug shortages for a healthcare facility: An inventory management approach. Eur. J. Oper. Res. 2016, 251, 107–123. [Google Scholar] [CrossRef]
- Little, J.; Coughlan, B. Optimal inventory policy within hospital space constraints. Health Care Manag. Sci. 2008, 11, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.Q.; Preston, D.S.; Xia, W. Enhancing hospital supply chain performance: A relational view and empirical test. J. Oper. Manag. 2013, 31, 391–408. [Google Scholar] [CrossRef]
- Wang, L.C.; Cheng, C.Y.; Tseng, Y.T.; Liu, Y.F. Demand-pull replenishment model for hospital inventory management: A dynamic buffer-adjustment approach. Int. J. Prod. Res. 2015, 53, 7533–7546. [Google Scholar] [CrossRef]
- Nicholson, L.; Vakharia, A.J.; Erenguc, S.S. Outsourcing inventory management decisions in healthcare: Models and application. Eur. J. Oper. Res. 2004, 154, 271–290. [Google Scholar] [CrossRef]
- Katsaliaki, K.; Brailsford, S.C. Using simulation to improve the blood supply chain. J. Oper. Res. Soc. 2007, 58, 219–227. [Google Scholar] [CrossRef]
- Royston, G. One hundred years of operational research in health—UK 1948–2048. J. Oper. Res. Soc. 2009, 60. [Google Scholar] [CrossRef]
- Park, S.J.; Lai, G.; Seshadri, S. Inventory Sharing in the Presence of Commodity Markets. Prod. Oper. Manag. 2016, 25, 1245–1260. [Google Scholar] [CrossRef]
- Zhao, H.; Deshpande, V.; Ryan, J.K. Inventory Sharing and Rationing in Decentralized Dealer Networks. Manag. Sci. 2005, 51, 531–547. [Google Scholar] [CrossRef]
- Yan, X.; Zhao, H. Inventory sharing and coordination among n independent retailers. Eur. J. Oper. Res. 2015, 243, 576–587. [Google Scholar] [CrossRef]
- Yan, X.; Zhao, H. TECHNICAL NOTE—Decentralized Inventory Sharing with Asymmetric Information. Oper. Res. 2011, 59, 1528–1538. [Google Scholar] [CrossRef]
- Robinson, L.W. Optimal and Approximate Policies in Multiperiod, Multilocation Inventory Models with Transshipments. Oper. Res. 1990, 38, 278–295. [Google Scholar] [CrossRef]
- Tagaras, G. Effects of pooling on the optimization and service levels of two-location inventory systems. IIE Trans. 1989, 21, 250–257. [Google Scholar] [CrossRef]
- Dong, L.; Rudi, N. Who Benefits from Transshipment? Exogenous vs. Endogenous Wholesale Prices. Manag. Sci. 2004, 50, 645–657. [Google Scholar] [CrossRef]
- Liao, Y.; Shen, W.; Hu, X.; Yang, S. Optimal responses to stockouts: Lateral transshipment versus emergency order policies. Omega 2014, 49, 79–92. [Google Scholar] [CrossRef]
- Anupindi, R.; Bassok, Y.; Zemel, E. A General Framework for the Study of Decentralized Distribution Systems. Manuf. Serv. Oper. Manag. 2001, 3, 349–368. [Google Scholar] [CrossRef]
- Granot, D.; Sošić, G. A Three-Stage Model for a Decentralized Distribution System of Retailers. Oper. Res. 2003, 51, 771–784. [Google Scholar] [CrossRef]
- Slikker, M.; Fransoo, J.; Wouters, M. Cooperation between multiple news-vendors with transshipments. Eur. J. Oper. Res. 2005, 167, 370–380. [Google Scholar] [CrossRef]
- Rudi, N.; Kapur, S.; Pyke, D.F. A Two-Location Inventory Model with Transshipment and Local Decision Making. Manag. Sci. 2001, 47, 1668–1680. [Google Scholar] [CrossRef]
- Zhao, H.; Deshpande, V.; Ryan, J.K. Emergency transshipment in decentralized dealer networks: When to send and accept transshipment requests. Nav. Res. Logist. 2006, 53, 547–567. [Google Scholar] [CrossRef]
- Hu, X.; Duenyas, I.; Kapuscinski, R. Existence of Coordinating Transshipment Prices in a Two-Location Inventory Model. Manag. Sci. 2007, 53, 1289–1302. [Google Scholar] [CrossRef]
- Hanany, E.; Tzur, M.; Levran, A. The transshipment fund mechanism: Coordinating the decentralized multilocation transshipment problem. Nav. Res. Logist. 2010, 57, 342–353. [Google Scholar] [CrossRef]
- Volland, J.; Fügener, A.; Schoenfelder, J.; Brunner, J.O. Material logistics in hospitals: A literature review. Omega 2017, 69, 82–101. [Google Scholar] [CrossRef]
- Wieser, P. From health logistics to health supply chain management. Supply Chain. Forum 2011, 12, 4–13. [Google Scholar] [CrossRef]
- Krichanchai, S.; MacCarthy, B.L. The adoption of vendor managed inventory for hospital pharmaceutical supply. Int. J. Logist. Manag. 2017, 28, 755–780. [Google Scholar] [CrossRef]
- Kritchanchai, D.; Hoeur, S.; Engelseth, P. Develop a strategy for improving healthcare logistics performance. Supply Chain Forum 2018, 19, 55–69. [Google Scholar] [CrossRef]
- Stefanini, A.; Aloini, D.; Benevento, E.; Dulmin, R.; Mininno, V. The transshipment fund mechanism: Coordinating the decentralized multilocation transshipment problem. Socio-Econ. Plan. Sci. 2019, in press. [Google Scholar]
- Adida, E.; DeLaurentis, P.C.C.; Lawley, M.A. Hospital stockpiling for disaster planning. IIE Trans. 2011, 43, 348–362. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).