Managing Healthcare Service Ecosystems: Abstracting a Sustainability-Based View from Hospitalization at Home (HaH) Practices
Abstract
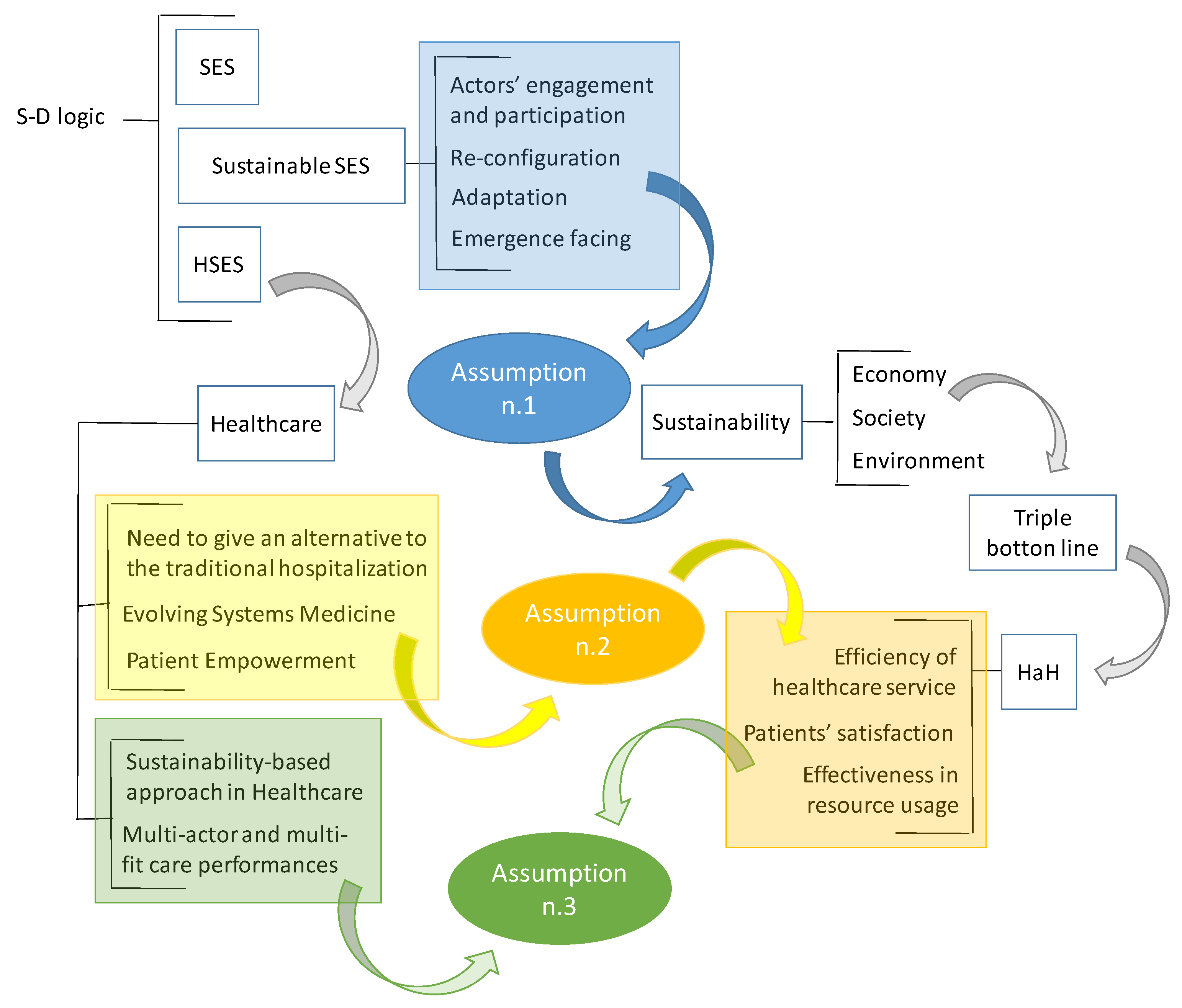
1. Introducing a Sustainability-Based View for Hospitalization at Home: A Conceptual Framework
2. Theoretical Background and Assumptions Development
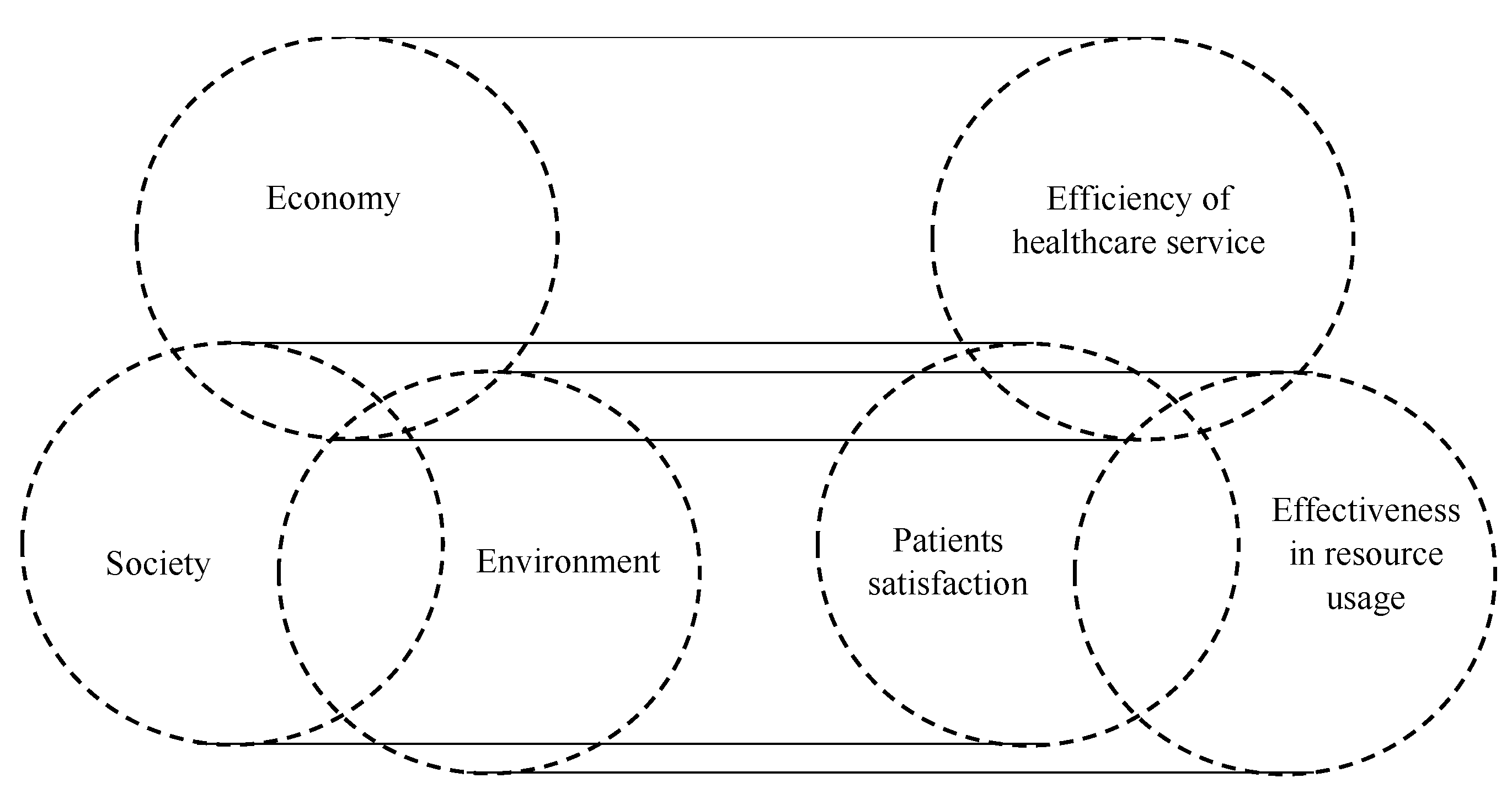
2.1. A Road-Map for Sustainability through the Service Ecosystems View
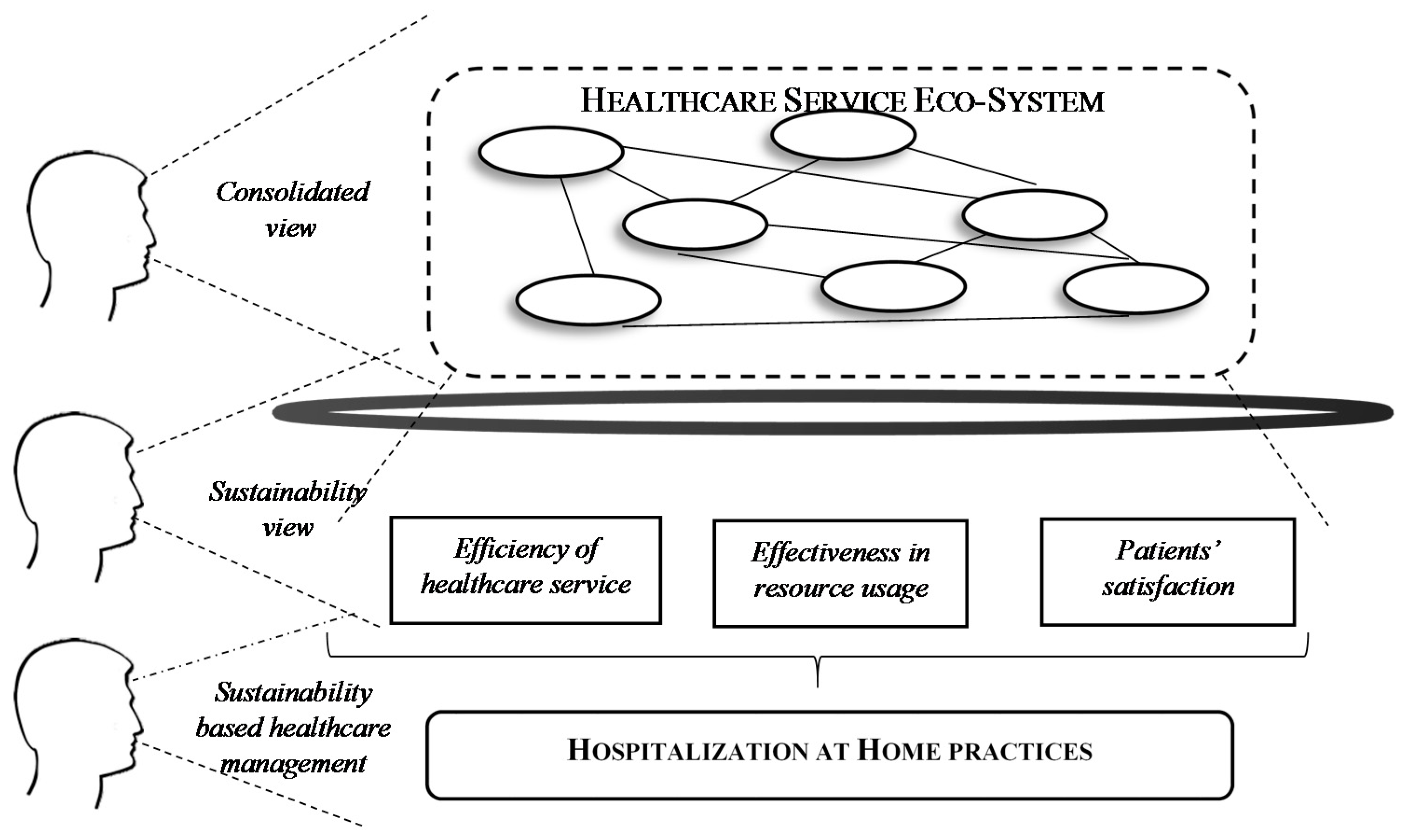
2.2. Healthcare as Service Ecosystem
3. Shaping a Sustainability-Based Healthcare Service Ecosystem: A Focus on HaH
3.1. What Is Hospitalization to Home
3.2. How Does HaH Make the Healthcare SES Sustainable?
4. Discussion, Implications, and Preliminary Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gupta, A.K.; Govindarajan, V. Business unit strategy, managerial characteristics, and business unit effectiveness at strategy implementation. Acad. Manag. J. 1984, 27, 25–41. [Google Scholar]
- Mahoney, J.T.; Pandian, J.R. The resource-based view within the conversation of strategic management. Strateg. Manag. J. 1992, 13, 363–380. [Google Scholar] [CrossRef]
- Hopwood, A.G.; Miller, P. (Eds.) Accounting as Social and Institutional Practice; Cambridge University Press: Cambridge, UK, 1994; Volume 24. [Google Scholar]
- Carayannis, E.; Caputo, F.; Del Giudice, M. Technology transfer as driver of smart growth: A quadruple/quintuple innovation framework approach. In Proceedings of the 10th Annual Conference of the EuroMed Academy of Business, Rome, Italy, 13–15 September 2017. [Google Scholar]
- Miles, R.E.; Snow, C.C. Organizations: New concepts for new forms. Calif. Manag. Rev. 1986, 28, 62–73. [Google Scholar] [CrossRef]
- Foss, N.J. (Ed.) Resources, Firms, and Strategies: A Reader in the Resource-Based Perspective; Oxford University Press on Demand: Oxford, UK, 1997. [Google Scholar]
- Barkema, H.G.; Baum, J.A.; Mannix, E.A. Management challenges in a new time. Acad. Manag. J. 2002, 45, 916–930. [Google Scholar]
- Van de Vrande, V.; De Jong, J.; Vanhaverbeke, W.; De Rochemont, M. Open innovation in SMEs: Trends, motives and management challenges. Technovation 2009, 29, 423–437. [Google Scholar] [CrossRef]
- Del Giudice, M.; Maggioni, V. Managerial practices and operative directions of knowledge management within inter-firm networks: A global view. J. Knowl. Manag. 2014, 18, 841–846. [Google Scholar] [CrossRef]
- Del Giudice, M.; Caputo, F.; Evangelista, F. How are decision systems changing? The contribution of social media to the management of decisional liquefaction. J. Decis. Syst. 2016, 25, 214–226. [Google Scholar] [CrossRef]
- Barile, S.; Saviano, M. Complexity and sustainability in management: Insights from a systems perspective. In Social Dynamics in a Systems Perspective; Springer: Cham, Switzerland, 2018; pp. 39–63. [Google Scholar]
- Calabrese, M.; Iandolo, F.; Caputo, F.; Sarno, D. From mechanical to cognitive view: The changes of decision making in business environment. In Social Dynamics in a Systems Perspective; Springer: Cham, Switzerland, 2018; pp. 223–240. [Google Scholar]
- Tronvoll, B.; Barile, S.; Caputo, F. A systems approach to understanding the philosophical foundation of marketing studies. In Social Dynamics in a Systems Perspective; Springer: Cham, Switzerland, 2018; pp. 1–18. [Google Scholar]
- Tian, K.T.; Bearden, W.O.; Hunter, G.L. Consumers’ need for uniqueness: Scale development and validation. J. Consum. Res 2001, 28, 50–66. [Google Scholar] [CrossRef]
- Badinelli, R.; Barile, S.; Ng, I.; Polese, F.; Saviano, M.; Di Nauta, P. Viable service systems and decision-making in-service management. J. Serv. Manag. 2012, 23, 498–526. [Google Scholar] [CrossRef]
- Scuotto, V.; Caputo, F.; Villasalero, M.; Del Giudice, M. A multiple buyer–supplier relationship in the context of SMEs’ digital supply chain management. Prod. Plan. Control 2017, 28, 1378–1388. [Google Scholar] [CrossRef]
- Granovetter, M. The impact of social structure on economic outcomes. J. Econ. Perspect. 2005, 19, 33–50. [Google Scholar] [CrossRef]
- Caputo, F.; Walletzky, L.; Štěpánek, P. Towards a Systems Thinking Based View for the Governance of a Smart City’s Ecosystem: A Bridge to Link Smart Technologies and Big Data. Kybernetes 2018. [Google Scholar] [CrossRef]
- Del Giudice, M.; De Silva, M.; Scuotto, V.; Caputo, F.; Carayannis, E. The microlevel actions undertaken by owner-managers in improving the sustainability practices of cultural and creative small and medium enterprises: A United Kingdom–Italy comparison. J. Organ. Behav. 2017, 38, 1396–1414. [Google Scholar] [CrossRef]
- Di Nauta, P.; Merola, B.; Caputo, F.; Evangelista, F. Reflections on the role of university to face the challenges of knowledge society for the local economic development. J. Knowl. Econ. 2018, 9, 180–198. [Google Scholar] [CrossRef]
- Golinelli, G.M.; Barile, S.; Saviano, M.; Polese, F. Perspective shifts in marketing: Toward a paradigm change? Serv. Sci. 2012, 4, 121–134. [Google Scholar] [CrossRef]
- Vargo, S.L.; Lusch, R.F. Service-dominant logic. In The Service-Dominant Logic of Marketing: Dialog, Debate, and Directions; Routledge: London, UK, 2006. [Google Scholar]
- Lusch, R.F.; Vargo, S.L.; O’brien, M. Competing through service: Insights from service-dominant logic. J. Retail. 2007, 83, 5–18. [Google Scholar] [CrossRef]
- Lusch, R.F.; Vargo, S.L. The Service-Dominant Logic of Marketing: Dialog, Debate, and Directions; Routledge: London, UK, 2014. [Google Scholar]
- Vargo, S.L.; Lusch, R.F. From repeat patronage to value co-creation in service ecosystems: A transcending conceptualization of relationship. J. Bus. Mark. Manag. 2010, 4, 169–179. [Google Scholar] [CrossRef]
- Wieland, H.; Polese, F.; Vargo, S.; Lusch, R. Toward a service (eco) systems perspective on value creation. Int. J. Serv. Sci. Manag. Eng. Technol. 2012, 3, 12–24. [Google Scholar] [CrossRef]
- Vargo, S.L.; Koskela-Huotari, K.; Baron, S.; Edvardsson, B.; Reynoso, J.; Colurcio, M. A systems perspective on markets–Toward a research agenda. J. Bus. Res. 2017, 79, 260–268. [Google Scholar] [CrossRef]
- Ben Letaifa, S.; Reynoso, J. Toward a service ecosystem perspective at the base of the pyramid. J. Serv. Manag. 2015, 26, 684–705. [Google Scholar] [CrossRef]
- Banoun, A.; Dufour, L.; Andiappan, M. Evolution of a service ecosystem: Longitudinal evidence from multiple shared services centers based on the economies of worth framework. J. Bus. Res. 2016, 69, 2990–2998. [Google Scholar] [CrossRef]
- Díaz-Méndez, M.; Saren, M.; Gummesson, E. Considering pollution in the higher education (HE) service ecosystem: The role of students’ evaluation surveys. TQM J. 2017, 29, 767–782. [Google Scholar] [CrossRef]
- Akaka, M.A.; Vargo, S.L.; Lusch, R.F. The complexity of context: A service ecosystems approach for international marketing. J. Mark. Res. 2013, 21, 1–20. [Google Scholar] [CrossRef]
- Chen, Z.; Dahlgaard-Park, S.M.; Yu, L. Service quality management and ecosystem theory. Total Qual. Manag. Bus. Excell. 2014, 25, 1190–1205. [Google Scholar] [CrossRef]
- Vargo, S.L.; Wieland, H.; Akaka, M.A. Innovation through institutionalization: A service ecosystems perspective. Ind. Mark. Manag. 2015, 44, 63–72. [Google Scholar] [CrossRef]
- Lusch, R.F.; Vargo, S.L.; Gustafsson, A. Fostering a trans-disciplinary perspectives of service ecosystems. J. Bus. Res. 2016, 69, 2957–2963. [Google Scholar] [CrossRef]
- Koskela-Huotari, K.; Edvardsson, B.; Jonas, J.M.; Sörhammar, D.; Witell, L. Innovation in service ecosystems—Breaking, making, and maintaining institutionalized rules of resource integration. J. Bus. Res. 2016, 69, 2964–2971. [Google Scholar] [CrossRef]
- Barile, S.; Lusch, R.; Reynoso, J.; Saviano, M.; Spohrer, J. Systems, networks, and ecosystems in service research. J. Serv. Manag. 2016, 27, 652–674. [Google Scholar] [CrossRef]
- Polese, F.; Carrubbo, L.; Bruni, R.; Maione, G. The viable system perspective of actors in eco-systems. TQM J. 2017, 29, 783–799. [Google Scholar] [CrossRef]
- Kaartemo, V.; Akaka, M.A.; Vargo, S.L. A Service-Ecosystem Perspective on Value Creation: Implications for International Business. In Value Creation in International Business; Springer International Publishing: Cham, Switzerland, 2017; pp. 131–149. [Google Scholar]
- Miller, T.R.; Wiek, A.; Sarewitz, D.; Robinson, J.; Olsson, L.; Kriebel, D.; Loorbach, D. The future of sustainability science: A solutions-oriented research agenda. Sustain. Sci. 2014, 9, 239–246. [Google Scholar] [CrossRef]
- Saviano, M.; Barile, S.; Spohrer, J.C.; Caputo, F. A service research contribution to the global challenge of sustainability. J. Serv. Theory Pract. 2017, 27, 951–976. [Google Scholar] [CrossRef]
- Komiyama, H.; Takeuchi, K. Sustainability science: Building a new discipline. Sustain. Sci. 2006, 1, 1–6. [Google Scholar] [CrossRef]
- Caputo, F.; Carrubbo, L.; Sarno, D. The Influence of Cognitive Dimensions on the Consumer-SME Relationship: A Sustainability-Oriented View. Sustainability 2018, 10, 3238. [Google Scholar] [CrossRef]
- Ruokolainen, T. A Model-Driven Approach to Service Ecosystem Engineering. Ph.D. Thesis, University of Helsinki, Helsinki, Finland, 2013. [Google Scholar]
- Frow, P.; McColl-Kennedy, J.R.; Hilton, T.; Davidson, A.; Payne, A.; Brozovic, D. Value propositions. A service ecosystems perspective. Mark. Theory 2014, 14, 327–351. [Google Scholar] [CrossRef]
- Frow, P.; McColl-Kennedy, J.R.; Payne, A. Co-creation practices: Their role in shaping a health care ecosystem. Ind. Mark. Manag. 2016, 56, 24–39. [Google Scholar] [CrossRef]
- Di Nauta, P.; Sarno, D. Possono le pratiche di value co-creation contribuire allo sviluppo di un ecosistema sanitario efficace? Prospett. Organ. ASSIOA 2017, 7, 1–9. [Google Scholar]
- Norton, B.G. Sustainability: A Philosophy of Adaptive Ecosystem Management; University of Chicago Press: Chicago, IL, USA, 2005. [Google Scholar]
- Leff, B. Acute? Care at home. The health and cost effects of substituting home care for inpatient acute care: A review of the evidence. J. Am. Geriatr. Soc. 2001, 49, 1123–1125. [Google Scholar] [CrossRef] [PubMed]
- Taillard, M.; Peters, L.D.; Pels, J.; Mele, C. The role of shared intentions in the emergence of service ecosystems. J. Bus. Res. 2016, 69, 2972–2980. [Google Scholar] [CrossRef]
- Beirão, G.; Patrício, L.; Fisk, R. Value cocreation in service ecosystems: Investigating health care at the micro, meso, and macro levels. J. Serv. Manag. 2017, 28, 227–249. [Google Scholar] [CrossRef]
- Polese, F.; Carrubbo, L. Eco-Sistemi di Servizio in Sanità; G. Giappichelli Editore: Torino, Italy, 2016. [Google Scholar]
- Ciasullo, M.V.; Troisi, O. La Visione Relazionale Dell’Impresa: Un Approccio per la Strategic Governance; G. Giappichelli Editore: Torino, Italy, 2017; Volume 68. [Google Scholar]
- Vargo, S.L.; Lusch, R.F. Service-dominant logic 2025. Int. J. Res. Mark. 2017, 34, 46–67. [Google Scholar] [CrossRef]
- Vargo, S.L.; Lusch, R.F. Institutions and axioms: An extension and update of service-dominant logic. J. Acad. Mark. Sci. 2016, 44, 5–23. [Google Scholar] [CrossRef]
- Tregua, M.; Carrubbo, L.; Iandolo, F.; Cosimato, S. New trends for service eco-systems analysis, a ‘sustainable’ approach, Implications for destination management. In Proceedings of the XXVI RESER Conference, Naples, Italy, 8–9 September 2016. [Google Scholar]
- Siltaloppi, J.; Koskela-Huotari, K.; Vargo, S.L. Institutional Complexity as a Driver for Innovation in Service Ecosystems. Serv. Sci. 2016, 8, 333–343. [Google Scholar] [CrossRef]
- Costanza, R.; Low, B.; Ostrom, E.; Wilson, J. Institutions, Ecosystems, and Sustainability; CRC Press: Boca Raton, FL, USA, 2000. [Google Scholar]
- Vargo, S.L.; Maglio, P.P.; Akaka, M.A. On value and value co-creation: A service systems and service logic perspective. Eur. Manag. J. 2008, 26, 145–152. [Google Scholar] [CrossRef]
- Chandler, J.D.; Vargo, S.L. Contextualization and value-in-context: How context frames exchange. Mark. Theory 2011, 11, 35–49. [Google Scholar] [CrossRef]
- Wolfson, A.; Tavor, D.; Mark, S.; Schermann, M.; Krcmar, H. Better Place: A case study of the reciprocal relations between sustainability and service. Serv. Sci. 2011, 3, 172–181. [Google Scholar] [CrossRef]
- Waage, S.A. Re-considering product design: A practical “road-map” for integration of sustainability issues. J. Clean. Prod. 2007, 15, 638–649. [Google Scholar] [CrossRef]
- Barile, S.; Saviano, M.; Polese, F. Information asymmetry and co-creation in health care services. Aust. Mark. J. 2014, 22, 205–217. [Google Scholar] [CrossRef]
- Barile, S.; Saviano, M.; Polese, F.; Di Nauta, P. Reflections on service systems boundaries: A viable systems perspective: The case of the London Borough of Sutton. Eur. J. Manag. 2012, 30, 451–465. [Google Scholar] [CrossRef]
- Rivera-Santos, M.; Rufín, C. Global village vs. small town: Understanding networks at the Base of the Pyramid. Int. Bus. Rev. 2010, 19, 126–139. [Google Scholar] [CrossRef]
- Capunzo, M.; Polese, F.; Boccia, G.; Carrubbo, L.; Clarizia, F.; De Caro, F. Advances in Service Research for the understanding and the management of service in healthcare networks. In System Theory and Service Science: Integrating Three Perspectives in a New Service Agenda; Gummesson, E., Mele, C., Polese, F., Eds.; Giannini: Naples, Italy, 2013. [Google Scholar]
- Carrubbo, L.; Clarizia, F.; Hisa, X.; Bilotta, A. New Smarter solutions for the Healthcare Complex Service System. In System Theory and Service Science: Integrating Three Perspectives in a New Service Agenda; Gummesson, E., Mele, C., Polese, F., Eds.; Giannini: Naples, Italy, 2013. [Google Scholar]
- Ignone, G.; Mossa, G.; Mummolo, G.; Pilolli, R.; Ranieri, L. Increasing public healthcare network performance by de-hospitalization: A patient pathway perspective. Strateg. Outsour. Int. J. 2013, 6, 85–107. [Google Scholar] [CrossRef]
- Iandolo, F.; Calabrese, M.; Antonucci, E.; Caputo, F. Towards a value co-creation based healthcare system. In The 2013 Naples Forum on Service. Service Dominant Logic, Networks and Systems Theory and Service Science: Integrating three Perspective for a new Service Agenda; Gummesson, E., Mele, C., Polese, F., Eds.; Giannini: Napoli, Italy, 2013. [Google Scholar]
- Saviano, M.; Bassano, C.; Piciocchi, P.; Di Nauta, P.; Lettieri, M. Monitoring Viability and Sustainability in Healthcare Organizations. Sustainability 2018, 10, 3548. [Google Scholar] [CrossRef]
- Hysa, X.; Zerba, E.; Calabrese, M.; Bassano, C. Social business as a sustainable business model: Making capitalism antifragile. Sustain. Sci. 2018, 13, 1345–1356. [Google Scholar] [CrossRef]
- Cano, I.; Alonso, A.; Hernandez, C.; Burgos, F.; Barberan-Garcia, A.; Roldan, J.; Roca, J. An adaptive case management system to support integrated care services: Lessons learned from the NEXES project. J. Biomed. Inform. 2015, 55, 11–22. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Disease; World Health Organization: Geneva, Switzerland, 2014; ISBN 9789241597418. [Google Scholar]
- World Health Organization (WHO). World Health Statistics 2010. Available online: http://www.who.int (accessed on 30 October 2018).
- Auffray, C.; Chen, Z.; Hood, L. Systems medicine: The future of medical genomics and healthcare. Genome Med. 2009, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Auffray, C.; Charron, D.; Hood, L. Predictive, preventive, personalized and participatory medicine: Back to the future. Genome Med. 2010, 2, 57. [Google Scholar] [CrossRef] [PubMed]
- Saviano, M. Condizioni di Efficacia Relazionale e di Performance Nelle Aziende Sanitarie; G. Giappichelli Editore: Torino, Italy, 2012. [Google Scholar]
- Walshe, K.; Smith, J. (Eds.) Healthcare Management; McGraw-Hill Education: London, UK, 2011. [Google Scholar]
- Saviano, M.; Parida, R.; Caputo, F.; Kumar Datta, S. Health care as a worldwide concern. Insights on the Italian and Indian health care systems and PPPs from a VSA perspective. EuroMed J. Bus. 2014, 9, 198–220. [Google Scholar] [CrossRef]
- Leff, B.; Montalto, M. Home hospital-toward a tighter definition. J. Am. Geriatr. Soc. 2004, 52, 2141. [Google Scholar] [CrossRef] [PubMed]
- Leff, B.; Burton, L.; Mader, S.L.; Naughton, B.; Burl, J.; Inouye, S.K.; Greenough, W.B., 3rd; Guido, S.; Langston, C.; Frick, K.D. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann. Intern. Med. 2005, 143, 798–808. [Google Scholar] [CrossRef] [PubMed]
- Niccolai, F. L’ospedale in Evoluzione Continua; Laboratorio Regionale per la formazione Sanitaria: Florence, Italy, 2003. [Google Scholar]
- Voudris, K.V.; Silver, M.A. Home Hospitalization for Acute Decompensated Heart Failure: Opportunities and Strategies for Improved Health Outcomes. Healthcare 2018, 6, 31. [Google Scholar] [CrossRef] [PubMed]
- Caputo, F. Approccio Sistemico e Co-Creazione di Valore in Sanità; Edizioni Nuova Cultura: Roma, Italy, 2018. [Google Scholar]
- Rodríguez Verjan, C.; Augusto, V.; Xie, X.; Buthion, V. Economic comparison between Hospital at Home and traditional hospitalization using a simulation-based approach. J. Enterp. Inf. Manag. 2013, 26, 135–153. [Google Scholar] [CrossRef]
- Hwang, J.; Christensen, C.M. Disruptive innovation in health care delivery: A framework for business-model innovation. Health Aff. 2008, 27, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Costanza, R. Ecological Economics: The Science and Management of Sustainability; Columbia University Press: New York, NY, USA, 1992. [Google Scholar]
- Van Marrewijk, M. Concepts and definitions of CSR and corporate sustainability: Between agency and communion. J. Bus. Ethics 2003, 44, 95–105. [Google Scholar] [CrossRef]
- Nidumolu, R.; Prahalad, C.K.; Rangaswami, M.R. Why sustainability is now the key driver of innovation. Harv. Bus. Rev. 2009, 87, 56–64. [Google Scholar]
- Kuhlman, T.; Farrington, J. What is sustainability? Sustainability 2010, 2, 3436–3448. [Google Scholar] [CrossRef]
- Cislaghi, C.; Zocchetti, C.; Di Virgilio, E. Per valutare l’intensità della mobilità ospedaliera non basta contare quanti escono da una regione per farsi ricoverare. Epid. Prev. 2010, 34, 97–101. [Google Scholar]
- Cohen, S.R.; Hassan, S.A.; Lapointe, B.J.; Mount, B.M. Quality of life in HIV disease as measured by the McGill quality of life questionnaire. Aids 1996, 12, 1421–1427. [Google Scholar] [CrossRef]
- Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K. Patient self-management of chronic disease in primary care. JAMA 2002, 288, 2469–2475. [Google Scholar] [CrossRef] [PubMed]
- Al-Balushi, S.; Sohal, A.S.; Singh, J.; Al Hajri, A.; Al Farsi, Y.M.; Al Abri, R. Readiness factors for lean implementation in healthcare settings—A literature review. J. Health Organ. Manag. 2014, 28, 135–153. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.G. Rapid Synthesis: Identifying the Effects of Home Care on Improving Health Outcomes, Client Satisfaction and Health System Sustainability; McMaster Health Forum: Hamilton, ON, Canada, 2018. [Google Scholar]
- Boland, L.; Légaré, F.; Perez, M.M. Impact of home care versus alternative locations of care on elder health outcomes: An overview of systematic reviews. BMC Geriatr. 2017, 17, 20. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.; Calanzani, N.; Curiale, V.; McCrone, P.P.; Higginson, I.J.; Brito, M.D. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Sao Paulo Med. J. 2017, 134, 93–94. [Google Scholar] [CrossRef] [PubMed]
- Caplan, G.A.; Sulaiman, N.S.; Mangin, D.A.; Ricauda, N.A.; Wilson, A.D.; Barclay, L. A meta-analysis of “hospital in the home”. Med. J. Aust. 2012, 197, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Totten, A.M.; White-Chu, E.F.; Wasson, N. Home-Based Primary Care Interventions; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016.
- Stamp, K.D.; Machado, M.A.; Allen, N.A. Transitional care programs improve outcomes for heart failure patients: An integrative review. J. Cardiovasc. Nurs. 2014, 29, 140–154. [Google Scholar] [CrossRef] [PubMed]
- Fearon, P.; Langhorne, P. Services for reducing duration of hospital care for acute stroke patients. Cochrane Database Syst. Rev. 2012, 9, CD000443. [Google Scholar]
- Cochrane, A.; Furlong, M.; McGilloway, S.; Molloy, D.W.; Stevenson, M.; Donnelly, M. Time-limited home-care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst. Rev. 2016, 10, CD010825. [Google Scholar] [CrossRef] [PubMed]
- Tappenden, P.; Campbell, F.; Rawdin, A.; Wong, R.; Kalita, N. The clinical effectiveness and cost-effectiveness of home-based, nurse-led health promotion for older people: A systematic review. Health Technol. Assess. 2012, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- Shepperd, S.; Gonçalves-Bradley, D.C.; Straus, S.E.; Wee, B. Hospital at home: Home-based end-of-life care. Cochrane Database Syst. Rev. 2016, 2, CD009231. [Google Scholar] [CrossRef] [PubMed]
- Leppin, A.L.; Gionfriddo, M.R.; Kessler, M. Preventing 30-day hospital readmissions: A systematic review and meta-analysis of randomized trials. J. Am. Med. Assoc. Intern. Med. 2014, 174, 1095–1107. [Google Scholar] [CrossRef] [PubMed]
- Graybill, E.M.; McMeekin, P.; Wildman, J. Can aging in place be cost effective? A systematic review. PLoS ONE 2014, 9, e102705. [Google Scholar] [CrossRef] [PubMed]
- Linertová, R.; García-Pérez, L.; Vázquez-Díaz, J.R.; Lorenzo-Riera, A. Sarría-Santamera, A. Interventions to reduce hospital readmissions in the elderly: In-hospital or home care. A systematic review. J. Eval. Clin. Pract. 2011, 17, 1167–1175. [Google Scholar] [CrossRef] [PubMed]
- Stall, N.; Nowaczynski, M.; Sinha, S.K. Systematic review of outcomes from home-based primary care programs for homebound older adults. J. Am. Geriatr. Soc. 2014, 62, 2243–2251. [Google Scholar] [CrossRef] [PubMed]
- Feltner, C.; Jones, C.D.; Cené, C.W. Transitional care interventions to prevent readmissions for persons with heart failure: A systematic review and meta-analysis. Ann. Intern. Med. 2014, 160, 774–784. [Google Scholar] [CrossRef] [PubMed]
- Toot, S.; Devine, M.; Orrell, M. The effectiveness of crisis resolution/home treatment teams for older people with mental health problems: A systematic review and scoping exercise. Int. J. Geriatr. Psychiatry 2011, 26, 1221–1230. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, P.J.; Worthington, E.J.; Parry, R.H.; Walker, M.F.; Drummond, A.E. Interventions to reduce dependency in personal activities of daily living in community dwelling adults who use homecare services: A systematic review. Clin. Rehabil. 2015, 29, 1064–1076. [Google Scholar] [CrossRef] [PubMed]
- Shepperd, S.; Iliffe, S.; Doll, H.A. Admission avoidance hospital at home. Cochrane Database Syst. Rev. 2016, 9, CD007491. [Google Scholar] [CrossRef] [PubMed]
- Bainbridge, D.; Seow, H.; Sussman, J. Common components of efficacious in-home end-of-life care programs: A review of systematic reviews. J. Am. Geriatr. Soc. 2016, 64, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Low, L.F.; Yap, M.; Brodaty, H. A systematic review of different models of home and community care services for older persons. BMC Health Serv. Res. 2011, 11, 93. [Google Scholar] [CrossRef] [PubMed]
- Barile, S.; Saviano, M.; Polese, F.; Di Nauta, P. II rapporto impresa-territorio tra efficienza locale, efficacia di contesto e sostenibilità ambientale. Sinerg. Ital. J. Manag. 2013, 90, 25–49. [Google Scholar]
- Barile, S.; Pels, J.; Polese, F.; Saviano, M. An Introduction on the Viable Systems Approach and its contribution to Marketing. J. Bus. Mark. Manag. 2012, 2, 54–78. [Google Scholar]
- Kennedy, D.M.; Caselli, R.J.; Berry, L.L. A roadmap for improving healthcare service quality. J. Healthc. Manag. 2011, 56, 385–402. [Google Scholar] [CrossRef] [PubMed]
- Saviano, M.; Caputo, F. Managerial choices between Systems, Knowledge and Viability. In Contributions to Theoretical and Practical Advances in Management; Barile, S., Ed.; A Viable Systems Approach (VSA); ARACNE: Roma, Italy, 2013; pp. 219–242. [Google Scholar]
- Saviano, M.; Bassano, C.; Calabrese, M. A VSA-SS Approach to Healthcare Service Systems. The Triple Target of Efficiency, Effectiveness and Sustainability. Serv. Sci. 2010, 2, 41–61. [Google Scholar] [CrossRef]
- Barile, S.; Polese, F.; Saviano, M.; Carrubbo, L.; Clarizia, F. Service Research contribution to Healthcare Networks’ Understanding. In Proceedings of the AMA Servsig International Service Research Conference, Helsinki, Finland, 7–9 June 2012. [Google Scholar]
- Elg, M.; Engström, J.; Witell, L.; Poksinska, B. Co-creation and learning in health-care service development. J. Serv. Manag. 2012, 23, 328–343. [Google Scholar] [CrossRef]
- Chakraborty, S.; Dobrzykowski, D. Examining value co-creation in healthcare purchasing: A supply chain view. Bus. Theory Pract. 2014, 15, 179. [Google Scholar] [CrossRef]
- Ciasullo, M.V.; Cosimato, S.; Pellicano, M. Service Innovations in Healthcare Service Ecosystem: A Case Study. Systems 2017, 5, 37. [Google Scholar] [CrossRef]
| Dimensions of HaH | Brief Description | Reference |
|---|---|---|
| The efficiency of healthcare service | Home rehabilitation has a positive impact on community-dwelling elders. | [96] |
| Home palliative-care services have a positive impact on reducing symptom burden for patients compared to hospital palliative-care services. | [97] | |
| Effects of “hospital-in-the-home” (HITH) services are associated with reductions in mortality, readmission rates, and cost, and increases in patient and carer satisfaction, and with no change in caregiver burden. | [98] | |
| Home-based primary-care (HBPC) interventions reduce the utilization of inpatient care and improve procedures clinically. | [99] | |
| HaH programs have the potential to reduce readmissions, enhance the quality of life, and reduce the cost of health care. | [100] | |
| Services for reducing the duration of hospital care for acute stroke patients have effects and costs of early supported discharge (ESD), compared to conventional services that involve in-hospital rehabilitation. | [101] | |
| Home-care rehabilitation services for maintaining and improving the functional independence of older adults may be more effective than usual. | [102] | |
| HaH practices improve health outcomes across a variety of clinical dimensions, including a reduction in mortality rates, a decrease in fall risks, and an increased level of independence. | [103] | |
| Effectiveness in resource usage | HaH practices are less expensive than hospitalization. | [104] |
| HaH practices acting on patient education and home visits prevent hospital re-admission. | [105] | |
| Assisted living technologies (ALTs) in HaH practices reduce hospital and nursing home stays for the intervention group. | [106] | |
| In-hospital and home-care interventions reduce hospital readmissions in the elderly. | [107] | |
| Interprofessional care teams in HaH practices reduce emergency department visits, hospitalizations, and long-term care admissions. | [108] | |
| Tele-monitoring, nurse-led clinics, and educational interventions reduce cases of readmission. | [109] | |
| Crisis resolution home-treatment teams (CRHTTs) for older people with mental health problems reduce the number of admissions to hospitals. | [110] | |
| Reducing the dependency in activities of daily living (ADL), HaH practices offer the possibility to maximize efficiency through the re-organization of approaches, tasks, and time. | [111] | |
| Patients’ satisfaction | Home-based end-of-life care generates high patient satisfaction. | [112] |
| Evaluations about in-home end-of-life practices (EOL) generates an improvement of patients’ satisfaction, with reference to the quality of life, health care services, performance status, pain management, non-pain symptom management, supporting home deaths, and reductions in healthcare costs. | [113] | |
| Patients involvement improves satisfaction with health care services. | [114] |
| Dimensions of Triple Bottom Line | Brief Description | Dimensions of HaH Practices |
|---|---|---|
| Economy | The value produced by an organization as a consequence to satisfy the market needs and expectations. | The efficiency of healthcare services |
| Society | The inclusion of peoples’ contributions in defining models and approaches able to promote equality and justice in organizational processes. | Patients’ satisfaction |
| Environment | Balanced use of available natural resources for satisfying actual needs, without reducing the possibility for future generation to satisfy their needs. | Effectiveness in resource usage |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polese, F.; Carrubbo, L.; Caputo, F.; Sarno, D. Managing Healthcare Service Ecosystems: Abstracting a Sustainability-Based View from Hospitalization at Home (HaH) Practices. Sustainability 2018, 10, 3951. https://doi.org/10.3390/su10113951
Polese F, Carrubbo L, Caputo F, Sarno D. Managing Healthcare Service Ecosystems: Abstracting a Sustainability-Based View from Hospitalization at Home (HaH) Practices. Sustainability. 2018; 10(11):3951. https://doi.org/10.3390/su10113951
Chicago/Turabian StylePolese, Francesco, Luca Carrubbo, Francesco Caputo, and Debora Sarno. 2018. "Managing Healthcare Service Ecosystems: Abstracting a Sustainability-Based View from Hospitalization at Home (HaH) Practices" Sustainability 10, no. 11: 3951. https://doi.org/10.3390/su10113951
APA StylePolese, F., Carrubbo, L., Caputo, F., & Sarno, D. (2018). Managing Healthcare Service Ecosystems: Abstracting a Sustainability-Based View from Hospitalization at Home (HaH) Practices. Sustainability, 10(11), 3951. https://doi.org/10.3390/su10113951







