Clinical Study of Biostimulation with Low-Power Diode Laser After Dental Extractions
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Groups
2.2. Procedure
2.2.1. a—First Session
- -
- Complete clinical and oral evaluation.
- -
- -
- Oral Health Impact Profile Questionnaire (OHIP-14sp) [22].
2.2.2. b—Second Visit After 7 Days
- -
- Collection of pain and inflammation questionnaire.
- -
- Evaluation of the healing index according to Hamzani and Chaushu (2018) [23].
- -
- Reevaluation of the MDAS and the OHIP-14sp questionnaire.
2.2.3. Variables (Outcomes)
- -
- Main:
2.3. Statistical Analysis
3. Results
3.1. Descriptive Results and Homogeneity of the Groups
3.2. Analysis of Pain
3.3. Analysis of Inflammation
3.4. Analysis of Post-Operative Complications
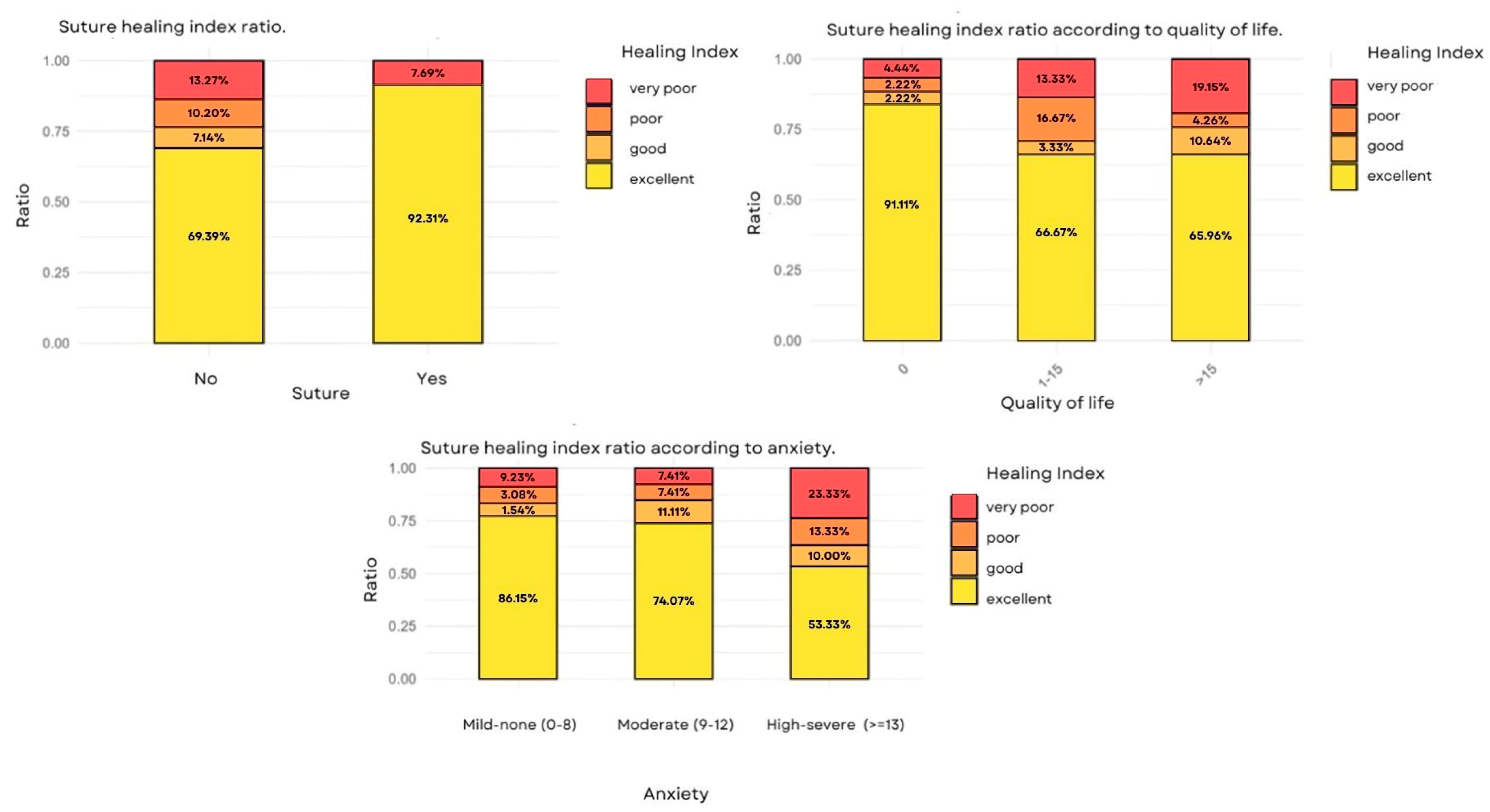
3.5. Analysis of the Healing Index
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Romero-Ruiz, M.M.; Herrero-Climent, M.; Torres-Lagares, D.; Gutiérrez-Pérez, J.L. Protocolo de control del dolor y la inflamación postquirúrgica: Una aproximación racional. RCOE 2006, 11, 205–215. [Google Scholar] [CrossRef]
- Puig, M.M.; Montes, A.; Marrugat, J. Management of postoperative pain in Spain. Acta Anaesthesiol. Scand. 2001, 45, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.S.; Seymour, R.A.; Chen, F.G.; Ho, V.C.L. Preoperative ketorolac has a preemptive effect for postoperative third molar surgical pain. Int. J. Oral Maxillofac. Surg. 2004, 33, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Seymour, R.A.; Blair, G.S.; Wyatt, F.A. Post-operative dental pain and analgesic efficacy. Part I. Br. J. Oral Surg. 1983, 21, 290–297. [Google Scholar] [CrossRef]
- Seymour, R.A.; Blair, G.S.; Wyatt, F.A. Post-operative dental pain and analgesic efficacy. Part II. Analgesic usage and efficacy after dental surgery. Br. J. Oral Surg. 1983, 21, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Seymour, R.A.; Meechan, J.G.; Blair, G.S. An investigation into post-operative pain after third molar surgery under local analgesia. Br. J. Oral Maxillofac. Surg. 1985, 23, 410–418. [Google Scholar] [CrossRef]
- Landaeta Bendezú, M.J.; Suazo Galdames, I.C.; Cantín López, M.; Roa Henriquez, I.J.; Zavando Matamata, D.A. Efecto de la Terapia láser de Baja Potencia sobre el Hueso Alveolar Dañado. Int. J. Morphol. 2008, 26, 639–642. [Google Scholar] [CrossRef]
- Suazo Galdames, I.C.; Lara Sepulveda, M.C.; Cantín López, M.G.; Zavando Matamala, D.A. Efecto de la Aplicación de Láser de Baja Potencia Sobre la Mucosa Oral Lesionada. Int. J. Morphol. 2007, 25, 523–528. [Google Scholar] [CrossRef]
- Migliario, M.; Sabbatini, M.; Mortellaro, C.; Renò, F. Near infrared low-level laser therapy and cell proliferation: The emerging role of redox sensitive signal transduction pathways. J. Biophotonics 2018, 11, e201800025. [Google Scholar] [CrossRef]
- Carroll, J.D.; Milward, M.R.; Cooper, P.R.; Hadis, M.; Palin, W.M. Developments in low level light therapy (LLLT) for dentistry. Dent. Mater. 2014, 30, 465–475. [Google Scholar] [CrossRef]
- Nadhreen, A.A.; Alamoudi, N.M.; Elkhodary, H.M. Low-level laser therapy in dentistry: Extra-oral applications. Niger. J. Clin. Pract. 2019, 22, 1313–1318. [Google Scholar] [PubMed]
- Brochado, F.T.; de Jesus, L.H.; Carrard, V.C.; Freddo, A.L.; Chaves, K.D.; Martins, M.D. Comparative effectiveness of photobiomodulation and manual therapy alone or combined in TMD patients: A randomized clinical trial. Braz. Oral Res. 2018, 32, e50. [Google Scholar] [CrossRef] [PubMed]
- Asutay, F.; Ozcan-Kucuk, A.; Alan, H.; Koparal, M. Three-dimensional evaluation of the effect of low-level laser therapy on facial swelling after lower third molar surgery: A randomized, placebo-controlled study. Niger. J. Clin. Pract. 2018, 21, 1107–1113. [Google Scholar] [PubMed]
- Camolesi, G.C.V.; Silva, F.F.V.E.; Aulestia-Viera, P.V.; Marichalar-Mendía, X.; Gándara-Vila, P.; Pérez-Sayáns, M. Is the Photobiomodulation Therapy Effective in Controlling Post-Surgical Side Effects After the Extraction of Mandibular Third Molars? A Systematic Review and Meta-Analysis. J. Evid.-Based Dent. Pract. 2024, 24, 101983. [Google Scholar] [CrossRef]
- Duarte De Oliveira, F.J.; Brasil, G.M.L.C.; Araújo Soares, G.P.; Fernandes Paiva, D.F.; De Assis De Souza Júnior, F. Use of low-level laser therapy to reduce postoperative pain, edema, and trismus following third molar surgery: A systematic review and meta-analysis. J. Cranio-Maxillofac. Surg. 2021, 49, 1088–1096. [Google Scholar] [CrossRef]
- Isolan, C.; Kinalski, M.D.; Leão, O.A.; Post, L.K.; Isolan, T.M.; Dos Santos, M.B. Photobiomodulation therapy reduces postoperative pain after third molar extractions: A randomized clinical trial. Med. Oral Patol. Oral Cir. Bucal 2021, 26, e341–e348. [Google Scholar] [CrossRef]
- Niemczyk, W.; Balicz, A.; Lau, K.; Morawiec, T.; Kasperczyk, J. Factors Influencing Peri-Extraction Anxiety: A Cross-Sectional Study. Dent. J. 2024, 12, 187. [Google Scholar] [CrossRef]
- Guillaumes, S.; O’Callaghan, C.A. Versión en español del software gratuito OxMaR para minimización y aleatorización de estudios clínicos. Gac. Sanit. 2019, 33, 395–397. [Google Scholar] [CrossRef]
- Morsy, D.A.; Negm, M.; Diab, A.; Ahmed, G. Postoperative pain and antibacterial effect of 980 nm diode laser versus conventional endodontic treatment in necrotic teeth with chronic periapical lesions: A randomized control trial. F1000Research 2018, 7, 1795. [Google Scholar] [CrossRef]
- Pitułaj, A.; Rajba, B.; Andrzejewska, B.; Kiejna, A.; Dominiak, M. Psychometric validation of Corah’s Dental Anxiety Scale in the Polish population. Adv. Clin. Exp. Med. 2020, 29, 45–49. [Google Scholar] [CrossRef]
- Leko, J.; Škrinjarić, T.; Goršeta, K. Reliability and Validity of Scales for Assessing Child Dental Fear and Anxiety. Acta Stomatol. Croat. 2020, 54, 22–31. [Google Scholar] [CrossRef]
- Montero-Martín, J.; Bravo-Pérez, M.; Albaladejo-Martínez, A.; Hernández-Martín, L.A.; Rosel-Gallardo, E.M. Validation the Oral Health Impact Profile (OHIP-14sp) for adults in Spain. Med. Oral Patol. Oral Cir. Bucal 2009, 14, E44–E50. [Google Scholar] [PubMed]
- Hamzani, Y.; Chaushu, G. Evaluation of early wound healing scales/indexes in oral surgery: A literature review. Clin. Implant. Dent. Relat. Res. 2018, 20, 1030–1035. [Google Scholar] [CrossRef] [PubMed]
- Pol, R.; Ruggiero, T.; Gallesio, G.; Riso, M.; Bergamasco, L.; Mortellaro, C.; Mozzati, M. Efficacy of Anti-Inflammatory and Analgesic of Superpulsed Low Level Laser Therapy After Impacted Mandibular Third Molars Extractions. J. Craniofac Surg. 2016, 27, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Bianchi De Moraes, M.; Gomes De Oliveira, R.; Raldi, F.V.; Nascimento, R.D.; Santamaria, M.P.; Loureiro Sato, F.R. Does the Low-Intensity Laser Protocol Affect Tissue Healing After Third Molar Removal? J. Oral Maxillofac. Surg. 2020, 78, 1920.e1–1920.e9. [Google Scholar] [CrossRef]
- Alkadi, S.; Stassen, L. Effect of One-Suture and Sutureless Techniques on Postoperative Healing After Third Molar Surgery. J. Oral Maxillofac. Surg. 2019, 77, 703.e1–703.e16. [Google Scholar] [CrossRef]
- Souza, M.R.J.; Meyfarth, S.; Fraga, R.S.; Fontes, K.B.F.C.; Guimarães, L.S.; Antunes, L.A.A.; Antunes, L.S. Do Antimicrobial Photodynamic Therapy and Low-Level Laser Therapy Influence Oral Health-Related Quality of Life After Molar Extraction? J. Oral Maxillofac. Surg. 2023, 81, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Tenis, C.A.; Martins, M.D.; Gonçalves, M.L.L.; da Silva, D.D.F.T.; da Cunha Filho, J.J.; Martins, M.A.T.; Mesquita-Ferrari, R.A.; Bussadori, S.K.; Fernandes, K.P.S. Efficacy of diode-emitting diode (LED) photobiomodulation in pain management, facial edema, trismus, and quality of life after extraction of retained lower third molars: A randomized, double-blind, placebo-controlled clinical trial. Medicine 2018, 97, e12264. [Google Scholar] [CrossRef]
- Metin, R.; Tatli, U.; Evlice, B. Effects of low-level laser therapy on soft and hard tissue healing after endodontic surgery. Lasers Med. Sci. 2018, 33, 1699–1706. [Google Scholar] [CrossRef]
- Ahrari, F.; Eshghpour, M.; Zare, R.; Ebrahimi, S.; Fallahrastegar, A.; Khaki, H. Effectiveness of low-level laser irradiation in reducing pain and accelerating socket healing after undisturbed tooth extraction. J. Lasers Med. Sci. 2020, 11, 274–279. [Google Scholar] [CrossRef]
- Momeni, E.; Kazemi, F.; Sanaei-Rad, P. Extraoral low-level laser therapy can decrease pain but not edema and trismus after surgical extraction of impacted mandibular third molars: A randomized, placebo-controlled clinical trial. BMC Oral Health 2022, 22, 417. [Google Scholar] [CrossRef] [PubMed]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| 1. Adult patients (>18 years) | 1. ASA preoperative evaluation: bad conditions for surgery |
| 2. Need of tooth extractions (for any reason) | 2. Inmunocompromised patients or taking inmunosuppressants |
| 3. Signed an informed consent form | 3. Patients with decompensated systemic diseases |
| 4. Patients undergoing chemotherapy treatment | |
| 5. Pregnant women | |
| 6. Patients with several mental disorders | |
| 7. Patients who had received head and neck radioteraphy |
| Group | p-Value | ||
|---|---|---|---|
| Sham (n = 62) | Experimental (n = 62) | ||
| Sex | 0.590 | ||
| Male | 31 (50%) | 28 (45.2%) | |
| Female | 31 (50%) | 34 (54.8%) | |
| Age (years) | 51.4 | 53.5 | 0.490 |
| Duration of Surgery (minutes) | 13 | 14.1 | 0.245 |
| Location | 0.814 | ||
| Anterior area | 8 (12.9%) | 10 (16.1%) | |
| Middle area | 13 (21%) | 13 (21%) | |
| Posterior area | 37 (59.7%) | 36 (58.1%) | |
| Posterior middle area | 1 (1.6%) | 2 (3.2%) | |
| Anterior middle area | 3 (4.8%) | 1 (1.6%) | |
| OHIP TOTAL (Day 1) | 14.6 | 12.7 | 0.854 |
| MDAS TOTAL (Day 1) | 7.9 | 7.7 | 0.503 |
| SUTURES | 1 | ||
| Yes | 13 (21%) | 13 (21%) | |
| No | 49 (79%) | 49 (79%) | |
| GROUP | p-Value | ||||
|---|---|---|---|---|---|
| TOTAL | Sham | Experimental | |||
| MDAS BASAL (T1) | Total | 124 (100%) | 62 (100%) | 62 (100%) | 0.503 |
| Slight-none (0–8) | 66 (53.2%) | 33 (53.2%) | 33 (53.2%) | ||
| Moderate (9–12) | 28 (22.6%) | 14 (22.6%) | 14 (22.6%) | ||
| High (13–14) | 7 (5.6%) | 3 (4.8%) | 4 (6.5%) | ||
| Severe (>15) | 23 (18.5%) | 12 (10.4%) | 11 (17.7%) | ||
| MDAS POST (T2) | Total | 124 (100% | 62 (100%) | 62 (100%) | |
| Slight-none (0–8) | 91 (73.4%) | 47 (75.8%) | 44 (71%) | ||
| Moderate (9–12) | 19 (15.3%) | 9 (14.5%) | 10 (16.1%) | ||
| High (13–14) | 2 (1.6%) | 1 (1.6%) | 1 (1.6%) | ||
| Severe (>15) | 12 (9.7%) | 5 (8.1%) | 7 (11.3%) | ||
| GROUP | |||||
|---|---|---|---|---|---|
| TOTAL | SHAM | Laser | p-Value | ||
| OHIP14-SP (T1) | N | 124 | 62 | 62 | 0.854 |
| Mean | 13.7 | 14.6 | 12.7 | ||
| Standard deviation | 15.9 | 18.5 | 12.8 | ||
| OHIP14-SP (T2) | N | 124 | 62 | 62 | |
| Mean | 8.9 | 7.5 | 10.2 | ||
| Standard deviation | 14.7 | 14.8 | 14.5 | ||
| F | p-Value | |
|---|---|---|
| TIME | 17.733 | <0.001 *** |
| GROUP | 1.273 | 0.261 |
| SUTURE | 1.995 | 0.160 |
| GROUP × SUTURE | 0.272 | 0.603 |
| GROUP × TIME | 0.332 | 0.715 |
| TIME × SUTURE | 3.158 | 0.045 * |
| GROUP × SUTURE × TIME | 0.293 | 0.743 |
| OR | 95% CI | p-Value | |
|---|---|---|---|
| GROUP | |||
| Control | 1 | ||
| Test | 0.539 | 0.22–1.26 | 0.157 |
| SUTURE | |||
| No | 1 | ||
| Yes | 4.634 | 1.24–30.33 | 0.048 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collado Murcia, Y.; Lopez-Jornet, P.; Parra Perez, F. Clinical Study of Biostimulation with Low-Power Diode Laser After Dental Extractions. Clin. Pract. 2025, 15, 90. https://doi.org/10.3390/clinpract15050090
Collado Murcia Y, Lopez-Jornet P, Parra Perez F. Clinical Study of Biostimulation with Low-Power Diode Laser After Dental Extractions. Clinics and Practice. 2025; 15(5):90. https://doi.org/10.3390/clinpract15050090
Chicago/Turabian StyleCollado Murcia, Yolanda, Pia Lopez-Jornet, and Francisco Parra Perez. 2025. "Clinical Study of Biostimulation with Low-Power Diode Laser After Dental Extractions" Clinics and Practice 15, no. 5: 90. https://doi.org/10.3390/clinpract15050090
APA StyleCollado Murcia, Y., Lopez-Jornet, P., & Parra Perez, F. (2025). Clinical Study of Biostimulation with Low-Power Diode Laser After Dental Extractions. Clinics and Practice, 15(5), 90. https://doi.org/10.3390/clinpract15050090








