Hyponatraemia After Hip and Knee Replacement: Incidence, Risk Factors, Clinical Consequences and Management in the Era of Enhanced Recovery
Abstract
1. Introduction
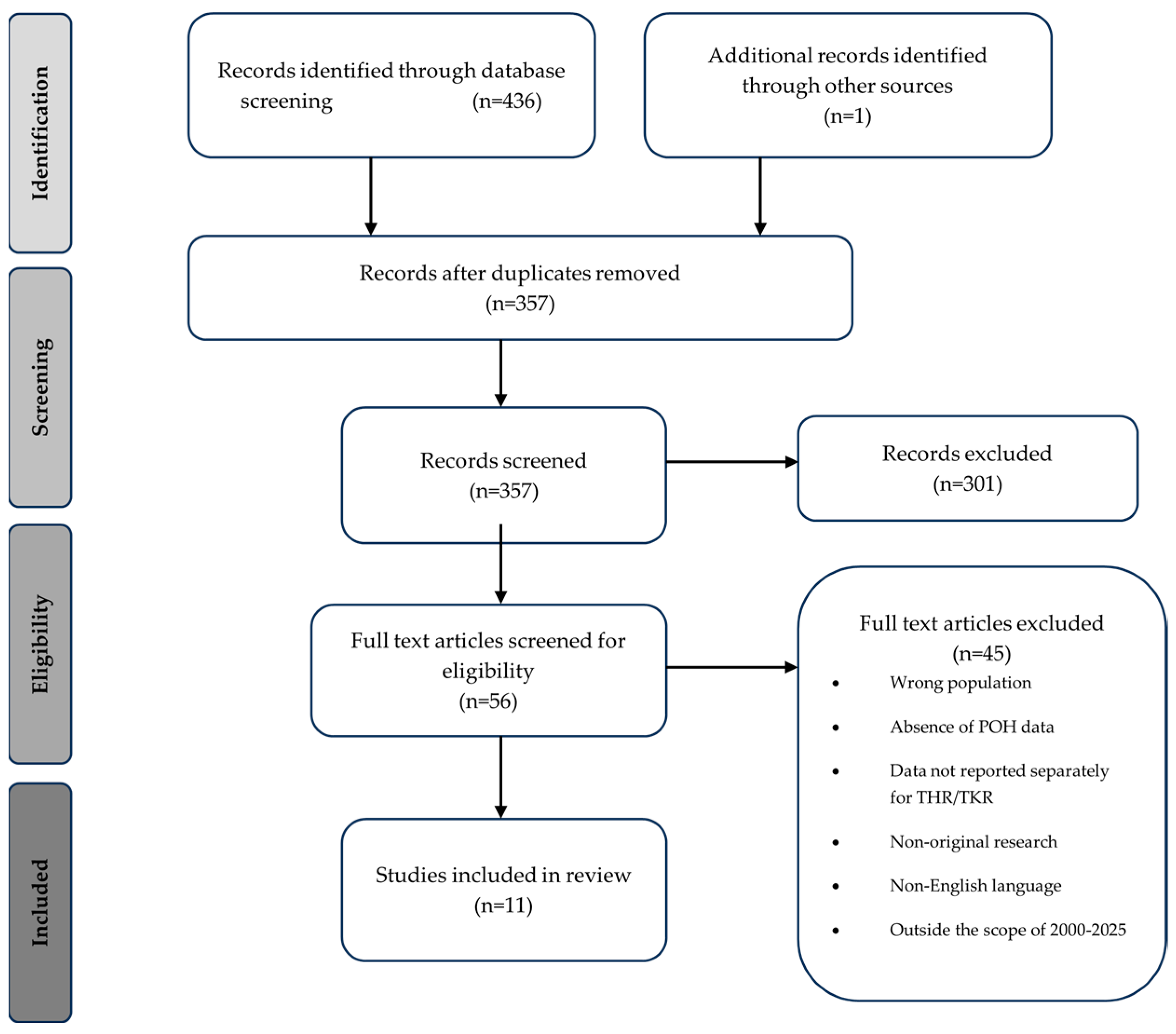
2. Materials and Methods
3. Discussion
- Definition and classification of hyponatraemia.
- Incidence of postoperative hyponatraemia.
- Risk factors.
- Clinical consequences.
- Prevention and management strategies.
3.1. Definition and Classification of Hyponatraemia
3.2. Incidence of Hyponatraemia in THR and TKR
3.3. Risk Factors for Postoperative Hyponatraemia
3.3.1. Patient Demographics
3.3.2. Comorbidities and Medications
3.3.3. Surgical and Anaesthesia
3.3.4. Fluid Management
3.4. Clinical Consequences of Hyponatraemia
3.5. Prevention and Management Strategies
3.6. Relevance to Enhanced Recovery Pathways
3.7. Gaps in Knowledge and Future Research Directions
3.8. Strengths and Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| POH | Postoperative hyponatraemia |
| THR | Total hip replacement |
| TKR | Total knee replacement |
| SIADH | Syndrome of inappropriate antidiuretic hormone |
| Na | Sodium |
| POD | Postoperative day |
| SSRI | Selective serotonin reuptake inhibitors |
| PPI | Proton pump inhibitors |
| LOS | Length of stay |
| ITU | Intensive treatment unit |
References
- Matharu, G.S.; Culliford, D.J.; Blom, A.W.; Judge, A. Projections for primary hip and knee replacement surgery up to the year 2060: An analysis based on data from The National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Ann. R. Coll. Surg. Engl. 2022, 104, 443–448. [Google Scholar] [CrossRef]
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J. Bone Jt. Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Jørgensen, C.C.; Petersen, M.A.; Kehlet, H. Preoperative prediction of potentially preventable morbidity after fast-track hip and knee arthroplasty: A detailed descriptive cohort study. BMJ Open 2016, 6, e009813. [Google Scholar] [CrossRef]
- Vehmeijer, S.B.W.; Husted, H.; Kehlet, H. Outpatient total hip and knee arthroplasty. Acta. Orthop. 2018, 89, 141–144. [Google Scholar] [CrossRef]
- Wainwright, T.W.; Memtsoudis, S.G.; Kehlet, H. Fast-track hip and knee arthroplasty...how fast? Br. J. Anaesth. 2021, 126, 348–349. [Google Scholar] [CrossRef]
- Oh, G.J.; Sutherland, S.M. Perioperative fluid management and postoperative hyponatremia in children. Pediatr. Nephrol. 2016, 31, 53–60. [Google Scholar] [CrossRef]
- Mentrasti, G.; Scortichini, L.; Torniai, M.; Giampieri, R.; Morgese, F.; Rinaldi, S.; Berardi, R. Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH): Optimal Management. Ther. Clin. Risk Manag. 2020, 16, 663–672. [Google Scholar] [CrossRef]
- Pillai, B.P.; Unnikrishnan, A.G.; Pavithran, P.V. Syndrome of inappropriate antidiuretic hormone secretion: Revisiting a classical endocrine disorder. Indian J. Endocrinol. Metab. 2011, 15, S208–S215. [Google Scholar] [CrossRef]
- Spasovski, G.; Vanholder, R.; Allolio, B.; Annane, D.; Ball, S.; Bichet, D.; Decaux, G.; Fenske, W.; Hoorn, E.J.; Ichai, C.; et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol. Dial. Transplant. 2014, 29, i1–i39. [Google Scholar] [CrossRef]
- Upadhyay, A.; Jaber, B.L.; Madias, N.E. Incidence and prevalence of hyponatremia. Am. J. Med. 2006, 119, S30–S35. [Google Scholar] [CrossRef] [PubMed]
- Gill, G.; Huda, B.; Boyd, A.; Skagen, K.; Wile, D.; Watson, I.; van Heyningen, C. Characteristics and mortality of severe hyponatraemia—A hospital-based study. Clin. Endocrinol. 2006, 65, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Waikar, S.S.; Mount, D.B.; Curhan, G.C. Mortality after Hospitalization with Mild, Moderate, and Severe Hyponatremia. Am. J. Med. 2009, 122, 857–865. [Google Scholar] [CrossRef]
- Asadollahi, K.; Beeching, N.; Gill, G. Hyponatraemia as a risk factor for hospital mortality. QJM 2006, 99, 877–880. [Google Scholar] [CrossRef] [PubMed]
- Crestanello, J.A.; Phillips, G.; Firstenberg, M.S.; Sai-Sudhakar, C.; Sirak, J.; Higgins, R.; Abraham, W.T. Postoperative Hyponatremia Predicts an Increase in Mortality and In-Hospital Complications after Cardiac Surgery. J. Am. Coll. Surg. 2013, 216, 1135–1143. [Google Scholar] [CrossRef]
- Upadhyay, U.M.; Gormley, W.B. Etiology and Management of Hyponatremia in Neurosurgical Patients. J. Intensive Care Med. 2012, 27, 139–144. [Google Scholar]
- Hennrikus, E.; Ou, G.; Kinney, B.; Lehman, E.; Grunfeld, R.; Wieler, J.; Damluji, A.; Davis, C., III; Mets, B. Prevalence, Timing, Causes, and Outcomes of Hyponatremia in Hospitalized Orthopaedic Surgery Patients. J. Bone Jt. Surg. Am. 2015, 97, 1824–1832. [Google Scholar] [CrossRef]
- Singh, N.; Tai, J.Y.; Dimech, J.; Gormack, N.J.; Cameron, A.J.D.; Lightfoot, N.J. Predictors of hyponatremia following elective primary unilateral knee arthroplasty at a tertiary centre: A retrospective observational cohort and predictive model. J. Orthop. 2020, 21, 491–495. [Google Scholar] [CrossRef]
- Cunningham, E.; Gallagher, N.; Hamilton, P.; Bryce, L.; Beverland, D. Prevalence, risk factors, and complications associated with hyponatraemia following elective primary hip and knee arthroplasty. Perioper. Med. 2021, 10, 25. [Google Scholar] [CrossRef]
- Baker, C.M.; Goh, G.S.; Tarabichi, S.; Sherman, M.B.; Khan, I.A.; Parvizi, J. Hyponatremia Is an Overlooked Sign of Trouble Following Total Joint Arthroplasty. J. Bone Jt. Surg. Am. 2023, 105, 744–754. [Google Scholar] [CrossRef]
- Wester, C.; Zhang, T.S.; Harrington, M.A.; Halawi, M.J. Sodium Abnormalities Are an Independent Predictor of Complications in Total Joint Arthroplasty: A Cautionary Tale! J. Arthroplast. 2021, 36, 3859–3863. [Google Scholar] [CrossRef]
- National Joint Registry. NJR 22nd Annual Report 2025. 2025. Available online: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2022nd%20Annual%20Report%202025.pdf (accessed on 1 December 2025).
- Gregory, A.T.; Denniss, A.R. An Introduction to Writing Narrative and Systematic Reviews—Tasks, Tips and Traps for Aspiring Authors. Heart Lung Circ. 2018, 27, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.; Tareen, H.U.; Syed, F.O. Frequency and Risk Factors of Postoperative Hyponatremia in Primary Hip and Knee Arthroplasties Patients at a Tertiary Care Hospital, Karachi, Pakistan. J. Postgrad. Med. Inst. 2024, 38, 203–207. [Google Scholar] [CrossRef]
- Macdonald, J.; Cunningham, E.; Gallagher, N.; Hamilton, P.; Cassidy, R.; Bryce, L.; Beverland, D. Can patients with mild post-operative hyponatraemia following elective arthroplasty be discharged safely? A large-scale service evaluation suggests they can. Ann. Clin. Biochem. Int. J. Biochem. Lab. Med. 2022, 59, 116–124. [Google Scholar] [CrossRef]
- Orfanos, G.; Kumar, N.N.; Redfern, D.; Burston, B.; Banerjee, R.; Thomas, G. The incidence and risk factors for abnormal postoperative blood tests following primary total joint replacement. Bone Jt. Open 2023, 4, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Sinno, E.; De Meo, D.; Cavallo, A.U.; Petriello, L.; Ferraro, D.; Fornara, G.; Persiani, P.; Villani, C. Is postoperative hyponatremia a real threat for total hip and knee arthroplasty surgery? Medicine 2020, 99, e20365. [Google Scholar] [CrossRef]
- Sarkar, S.; Gautam, D.; Anand, R.K.; Goyal, D.; Batra, S.; Malhotra, R.; Khanna, P.; Baidya, D.K. Clinicoepidemiological profile of acute postoperative hyponatraemia in patients undergoing joint replacement surgery: A prospective observational study. J. Perioper. Pract. 2025. [Google Scholar] [CrossRef]
- Sah, A.P. Hyponatremia after primary hip and knee arthroplasty: Incidence and associated risk factors. Am. J. Orthop. 2014, 43, E69–E73. [Google Scholar]
- Mukartihal, R.; Puranik, H.G.; Patil, S.S.; Dhanasekaran, S.R.; Menon, V.K. Electrolyte imbalance after total joint arthroplasty: Risk factors and impact on length of hospital stay. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1467–1472. [Google Scholar] [CrossRef]
- Waller, M.; Barkley, S.; Harrison, T. Can introducing a direct endocrine pathway reduce hyponatraemia in elective knee and hip replacements? A closed-loop audit and service evaluation study. Ann. R. Coll. Surg. Engl. 2025, 107, 469–472. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE). Hyponatraemia: NICE Guideline. July 2025. Available online: https://cks.nice.org.uk/topics/hyponatraemia/background-information/causes/ (accessed on 15 September 2025).
- Ruccia, F.; Savage, J.A.; Sorooshian, P.; Lees, M.; Fesatidou, V.; Zoccali, G. Hyponatremia after Autologous Breast Reconstruction: A Cohort Study Comparing Two Fluid Management Protocols. J. Reconstr. Microsurg. 2023, 39, 35–42. [Google Scholar] [PubMed]
- Park, S.; An, J.N.; Lee, J.P.; Oh, Y.K.; Kim, D.K.; Joo, K.W.; Kim, Y.S.; Lim, C.S. Association between postoperative hyponatremia and renal prognosis in major urologic surgery. Oncotarget 2017, 8, 79935–79947. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, Y.; Tamai, K.; Oka, M.; Habibi, H.; Terai, H.; Hoshino, M.; Toyoda, H.; Suzuki, A.; Takahashi, S.; Nakamura, H. Prevalence, risk factors, and potential symptoms of hyponatremia after spinal surgery in elderly patients. Sci. Rep. 2022, 12, 18622. [Google Scholar] [CrossRef]
- Sherlock, M.; O’Sullivan, E.; Agha, A.; Behan, L.A.; Rawluk, D.; Brennan, P.; Tormey, W.; Thompson, C.J. The incidence and pathophysiology of hyponatraemia after subarachnoid haemorrhage. Clin. Endocrinol. 2006, 64, 250–254. [Google Scholar] [CrossRef]
- Filippatos, T.D.; Makri, A.; Elisaf, M.S.; Liamis, G. Hyponatremia in the elderly: Challenges and solutions. Clin. Interv. Aging 2017, 12, 1957–1965. [Google Scholar] [CrossRef]
- Davies, I.; O’Neill, P.A.; Mclean, K.A.; Catania, J.; Bennett, D. Age-associated Alterations in Thirst and Arginine Vasopressin in Response to a Water or Sodium Load. Age Ageing 1995, 24, 151–159. [Google Scholar] [CrossRef]
- Phillips, P.A.; Rolls, B.J.; Ledingham, J.G.; Forsling, M.L.; Morton, J.J.; Crowe, M.J.; Wollner, L. Reduced Thirst after Water Deprivation in Healthy Elderly Men. N. Engl. J. Med. 1984, 311, 753–759. [Google Scholar] [CrossRef]
- Cowen, L.E.; Hodak, S.P.; Verbalis, J.G. Age-Associated Abnormalities of Water Homeostasis. Endocrinol. Metab. Clin. North Am. 2023, 52, 277–293. [Google Scholar] [CrossRef]
- Hendriksen, L.C.; Mouissie, M.S.; Herings, R.M.C.; van der Linden, P.D.; Visser, L.E. Women have a higher risk of hospital admission associated with hyponatremia than men while using diuretics. Front. Pharmacol. 2024, 15, 1409271. [Google Scholar] [CrossRef] [PubMed]
- Filippone, E.J.; Ruzieh, M.; Foy, A. Thiazide-Associated Hyponatremia: Clinical Manifestations and Pathophysiology. Am. J. Kidney Dis. 2020, 75, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Mann, S.J. The Silent Epidemic of Thiazide-Induced Hyponatremia. J. Clin. Hypertens. 2008, 10, 477–484. [Google Scholar] [CrossRef]
- Falhammar, H.; Skov, J.; Calissendorff, J.; Nathanson, D.; Lindh, J.D.; Mannheimer, B. Associations Between Antihypertensive Medications and Severe Hyponatremia: A Swedish Population–Based Case–Control Study. J. Clin. Endocrinol. Metab. 2020, 105, e3696–e3705. [Google Scholar] [CrossRef] [PubMed]
- Rudge, J.E.; Kim, D. New-onset hyponatraemia after surgery for traumatic hip fracture. Age Ageing 2014, 43, 821–826. [Google Scholar] [CrossRef]
- Mannheimer, B.; Lindh, J.D.; Fahlén, C.B.; Issa, I.; Falhammar, H.; Skov, J. Drug-induced hyponatremia in clinical care. Eur. J. Intern. Med. 2025, 137, 11–20. [Google Scholar] [CrossRef]
- Falhammar, H.; Lindh, J.D.; Calissendorff, J.; Skov, J.; Nathanson, D.; Mannheimer, B. Associations of proton pump inhibitors and hospitalization due to hyponatremia: A population–based case–control study. Eur. J. Intern. Med. 2019, 59, 65–69. [Google Scholar] [CrossRef]
- El-Alali, E.; Al Jaber, E. Association of proton pump inhibitor use and significant hyponatremia-a US population-based case-control study. Proc. (Bayl. Univ. Med. Cent.) 2022, 35, 434–436. [Google Scholar] [CrossRef]
- Desborough, J.P. The stress response to trauma and surgery. Br. J. Anaesth. 2000, 85, 109–117. [Google Scholar] [CrossRef]
- Ferré, F.; Martin, C.; Bosch, L.; Kurrek, M.; Lairez, O.; Minville, V. Control of Spinal Anesthesia-Induced Hypotension in Adults. Local Reg. Anesth. 2020, 13, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Cusack, B.; Buggy, D.J. Anaesthesia, analgesia, and the surgical stress response. BJA Educ. 2020, 20, 321–328. [Google Scholar] [CrossRef]
- Lane, N.; Allen, K. Hyponatraemia after orthopaedic surgery. BMJ 1999, 318, 1363–1364. [Google Scholar] [CrossRef]
- Tambe, A.A.; Hill, R.; Livesley, P.J. Post-operative hyponatraemia in orthopaedic injury. Injury 2003, 34, 253–255. [Google Scholar] [CrossRef]
- Semler, M.W.; Kellum, J.A. Balanced Crystalloid Solutions. Am. J. Respir. Crit. Care Med. 2019, 199, 952–960. [Google Scholar] [CrossRef]
- Gao, M.; Chen, M.; Dai, G.; Zhu, D.; Cai, Y. Clinical study: The impact of goal-directed fluid therapy on volume management during enhanced recovery after surgery in gastrointestinal procedures. Acta Biochim. Pol. 2024, 71, 12377. [Google Scholar] [CrossRef]
- Kendrick, J.B.; Kaye, A.D.; Tong, Y.; Belani, K.; Urman, R.D.; Hoffman, C.; Liu, H. Goal-directed fluid therapy in the perioperative setting. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, S29–S34. [Google Scholar] [CrossRef]
- Carlock, K.D.; Mills, Z.D.; Geiger, K.W.; Manner, P.A.; Fernando, N.D. Routine Indwelling Urinary Catheterization Is Not Necessary During Total Hip Arthroplasty Performed Under Spinal Anesthesia. Arthroplast. Today 2022, 16, 68–72. [Google Scholar] [CrossRef]
- Wainwright, T.W.; Gill, M.; McDonald, D.A.; Middleton, R.G.; Reed, M.; Sahota, O.; Yates, P.; Ljungqvist, O. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2020, 91, 3–19. [Google Scholar] [CrossRef]
- Halawi, M.J.; Plourde, J.M.; Cote, M.P. Routine Postoperative Laboratory Tests Are Not Necessary After Primary Total Hip Arthroplasty. J. Arthroplast. 2019, 34, 538–541. [Google Scholar] [CrossRef] [PubMed]
- Tischler, E.H.; Restrepo, C.; Ponzio, D.Y.; Austin, M.S. Routine Postoperative Chemistry Panels Are Not Necessary for Most Total Joint Arthroplasty Patients. J. Bone Jt. Surg. Am. 2021, 103, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Garg, V.; Byrom, I.; Agnew, N.; Starks, I.; Phillips, S.; Malek, I.A. Routine postoperative blood tests in all patients undergoing Total Hip Arthroplasty as part of an enhanced recovery pathway: Are they necessary? J. Clin. Orthop. Trauma 2021, 16, 114–118. [Google Scholar] [CrossRef]
- Zhu, A.C.; Agarwala, A.; Bao, X. Perioperative Fluid Management in the Enhanced Recovery after Surgery (ERAS) Pathway. Clin. Colon Rectal Surg. 2019, 32, 114–120. [Google Scholar] [CrossRef]
- Kim, S.; Joo, K.W. Electrolyte and Acid-Base Disturbances Associated with Non-Steroidal Anti-Inflammatory Drugs. Electrolytes Blood Press. 2007, 5, 116–125. [Google Scholar] [CrossRef]
- Falhammar, H.; Calissendorff, J.; Skov, J.; Nathanson, D.; Lindh, J.D.; Mannheimer, B. Tramadol- and codeine-induced severe hyponatremia: A Swedish population-based case-control study. Eur. J. Intern. Med. 2019, 69, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Canzan, F.; Longhini, J.; Caliaro, A.; Cavada, M.L.; Mezzalira, E.; Paiella, S.; Ambrosi, E. The effect of early oral postoperative feeding on the recovery of intestinal motility after gastrointestinal surgery: A systematic review and meta-analysis of randomized clinical trials. Front. Nutr. 2024, 11, 1369141. [Google Scholar] [CrossRef] [PubMed]
- Tazreean, R.; Nelson, G.; Twomey, R. Early mobilization in enhanced recovery after surgery pathways: Current evidence and recent advancements. J. Comp. Eff. Res. 2022, 11, 121–129. [Google Scholar] [CrossRef]
| Concept 1 | Concept 2 |
|---|---|
| Hypon * Low sodium Electrolyte imbalance Electrolyte disturbance Combine with OR | Total hip replacement Total hip arthroplasty THR Total knee replacement Total knee arthroplasty TKR Joint replacement Arthroplasty Combine with OR |
| Combine with AND | |
| Author/Year | Population (n) | Procedure(s) | Definition of Hyponatraemia | Incidence of POH | |||
|---|---|---|---|---|---|---|---|
| Overall | Mild | Moderate | Severe | ||||
| Singh (2020) [19] | 236 | TKR | Na <135 mmol/L + drop ≥5 mmol/L | 36.4% | 67.4% | 23.3% | 9.3% |
| Cunningham (2021) [20] | 1000 | THR & TKR | Na <135 mmol/L | 21.70% | 81.6% | 17.1% | 1.4% |
| Baker (2023) [21] | 3071 | THR & TKR | Na <135 mmol/L | 12% | Not stated | Not stated | Not stated |
| Haider (2024) [25] | 189 | THR & TKR | Na <130 mmol/L | 44.40% | 24% | 57% | 19% |
| Macdonalds (2022) [26] | 1000 | THR & TKR | Na <135 mmol/L | 32.1% 25.7% | 87.5% 91% | 11.5% 6.6% | 0.9% 2.3% |
| Orfanos (2023) [27] | 2721 | THR & TKR | Not stated | 12.2% | Not stated | Not stated | Not stated |
| Sinno (2020) [28] | 402 | THR & TKR | Na <135 mmol/L | 26.90% | 98.2% | 1.8% | 0% |
| Sarkar (2025) [29] | 225 | THR & TKR | Na <135 mmol/L | 30.6% | 91.6% | 7.2% | 1.4% |
| Sah (2014) [30] | 392 | THR & TKR | Na <135 mmol/L | 40% | 81.9% | 14.2% | 3.9% |
| Mukartihal (2019) [31] | 546 | THR & TKR | Na <135 mmol/L | 85% | 80% | 16% | 4% |
| Waller (2025) [32] | Cycle 1–295 Cycle 2–263 | THR & TKR | Na <133 mmol/L | Cycle 1–12% Cycle 2–11.7% | 41.6% 38.7% | 27.8% 51.6% | 30.6% 9.7% |
| Author/Year | Population (n) | Procedure(s) | Risk Factors Identified | Outcomes/Complications |
|---|---|---|---|---|
| Singh (2020) [19] | 236 | TKR | Older age, lower preoperative sodium, diuretics, total intravenous and oral fluid intake | Reduction in Quality of Recovery-15 score, increased LOS but not clinically meaningful |
| Cunningham (2021) [20] | 1000 | THR & TKR | Older age, lower preoperative sodium, and fasting glucose on day 1 | No increase in LOS, no increased reattendance or readmission within 90 days, higher rates of inpatient complications |
| Baker (2023) [21] | 3071 | THR & TKR | Older age, congestive heart failure, chronic kidney disease, revision, general anaesthesia, higher Charlson Comorbidity Index score, stroke | Increased LOS, greater likelihood of inpatient complications and non-home discharge |
| Haider (2024) [25] | 189 | THR & TKR | Older age, increased duration of surgery | LOS increased |
| Macdonalds (2022) [26] | 1000 | THR & TKR | Older age, lower preoperative sodium, knee surgery | No impact |
| Sinno (2020) [28] | 402 | THR & TKR | Diabetes, blood transfusion, chronic use of beta blockers | No impact |
| Sarkar (2025) [29] | 225 | THR & TKR | Diabetes, volume of blood loss >300 mL, older age | No impact |
| Sah (2014) [30] | 392 | THR & TKR | Female sex, older age, lower body weight, and lower preoperative sodium, knee replacement, bilateral knee replacement, thiazide diuretics, angiotensin-converting-enzyme inhibitors | LOS increased for knee replacement |
| Mukartihal (2019) [31] | 546 | THR & TKR | Preoperative hyponatraemia, female sex, older age, thiazide diuretics, angiotensin-converting-enzyme inhibitors, knee replacement | No impact |
| Waller (2021) [32] | Cycle 1–295 Cycle 2–263 | THR & TKR | Knee replacement, older age, diuretics | Decreased incidence of POH after endocrine pathway introduced with markedly reduced severity, reduced LOS in the second cycle |
| Category | Criteria | Clinical Features | Common Causes | |
|---|---|---|---|---|
| Biochemical severity | Mild | Serum Na+ 130–135 mmol/L | Often asymptomatic; may have subtle cognitive or gait disturbance | |
| Moderate | Serum Na+ 125–129 mmol/L | Nausea, headache, confusion, weakness | ||
| Severe | Serum Na+ <125 mmol/L | Seizures, delirium, coma, risk of death | ||
| Fluid status | Hypovolaemia | Loss of total body water and sodium, with sodium loss greater than water | Dry mucous membranes, hypotension, prolonged capillary refill | Vomiting, diarrhoea, diuretic use |
| Euvolaemia | Increased total body water with stable sodium content | No oedema, normal blood pressure, normal fluid balance | SIADH, hypothyroidism, Addison’s disease | |
| Hypervolaemia | Increase in both water and sodium, with water gain exceeding sodium | Peripheral oedema, pulmonary oedema, raised jugular venous pressure | Cardiac failure, renal failure, liver failure | |
| Duration | Acute | Onset of <48 h | ||
| Chronic | Onset of >48 h |
| Phase | Recommendations | Rationale |
|---|---|---|
| Preoperative |
| Early recognition of high-risk patients allows risk stratification and targeted monitoring. |
| Intraoperative |
| Prevents dilutional hyponatraemia, maintains euvolaemia, reduces complications. |
| Immediate Postoperative |
| Detects early POH, limits contributing factors (nausea/vomiting, excessive opioid-related SIADH). |
| Ward-based Care |
| Supports enhanced recovery goals of early feeding/mobilisation while preventing fluid imbalance. |
| Future directions |
| Promotes proactive management and early detection of POH. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thornley, L.; Craig, J.; Wainwright, T.W.; Middleton, R.G. Hyponatraemia After Hip and Knee Replacement: Incidence, Risk Factors, Clinical Consequences and Management in the Era of Enhanced Recovery. Clin. Pract. 2025, 15, 236. https://doi.org/10.3390/clinpract15120236
Thornley L, Craig J, Wainwright TW, Middleton RG. Hyponatraemia After Hip and Knee Replacement: Incidence, Risk Factors, Clinical Consequences and Management in the Era of Enhanced Recovery. Clinics and Practice. 2025; 15(12):236. https://doi.org/10.3390/clinpract15120236
Chicago/Turabian StyleThornley, Lauren, James Craig, Thomas W. Wainwright, and Robert G. Middleton. 2025. "Hyponatraemia After Hip and Knee Replacement: Incidence, Risk Factors, Clinical Consequences and Management in the Era of Enhanced Recovery" Clinics and Practice 15, no. 12: 236. https://doi.org/10.3390/clinpract15120236
APA StyleThornley, L., Craig, J., Wainwright, T. W., & Middleton, R. G. (2025). Hyponatraemia After Hip and Knee Replacement: Incidence, Risk Factors, Clinical Consequences and Management in the Era of Enhanced Recovery. Clinics and Practice, 15(12), 236. https://doi.org/10.3390/clinpract15120236







