Medical Professionals’ Opinions of and Attitudes Toward Uterus Transplantation in Hungary
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Development
2.2. Survey Distribution
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
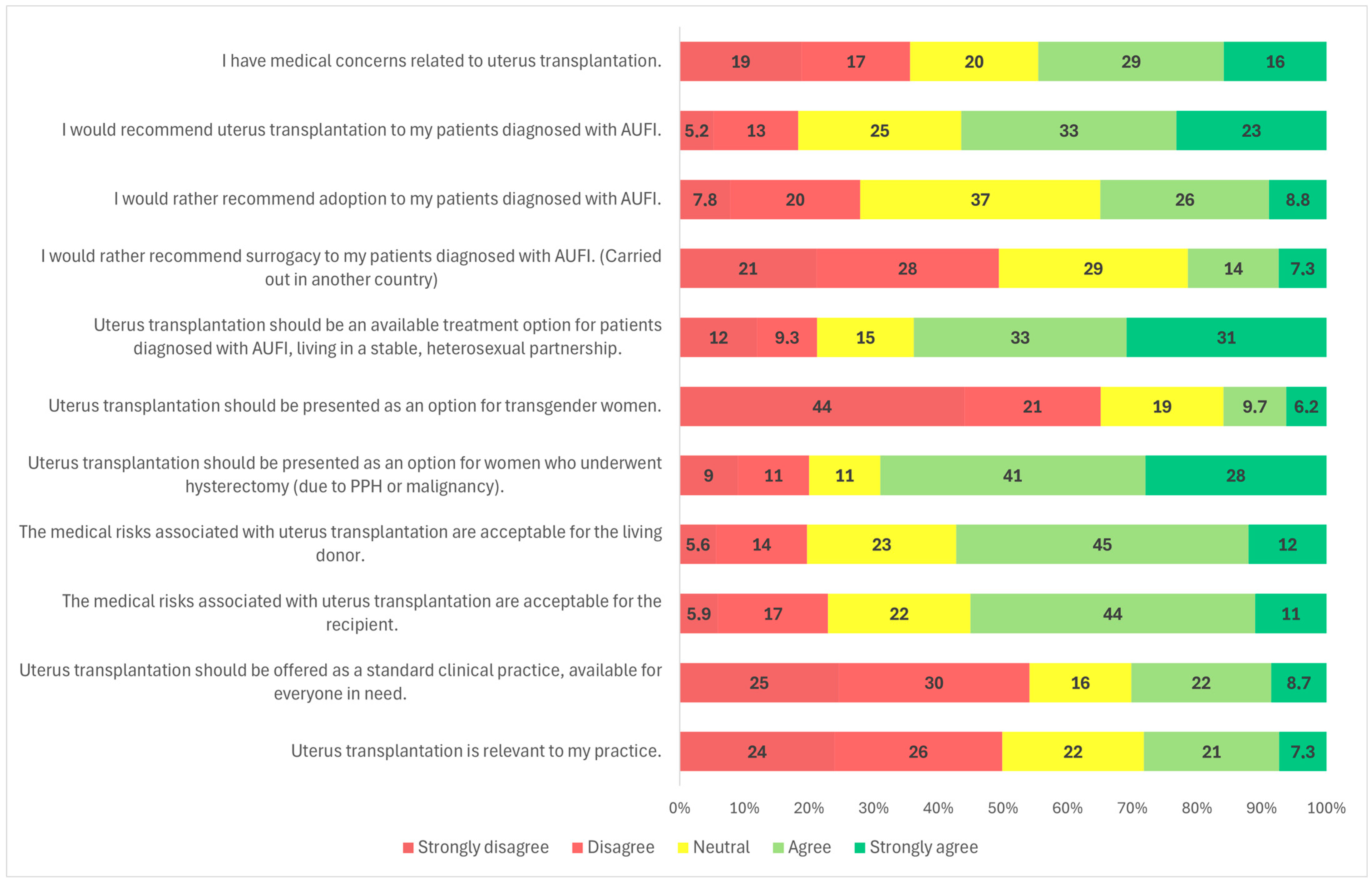
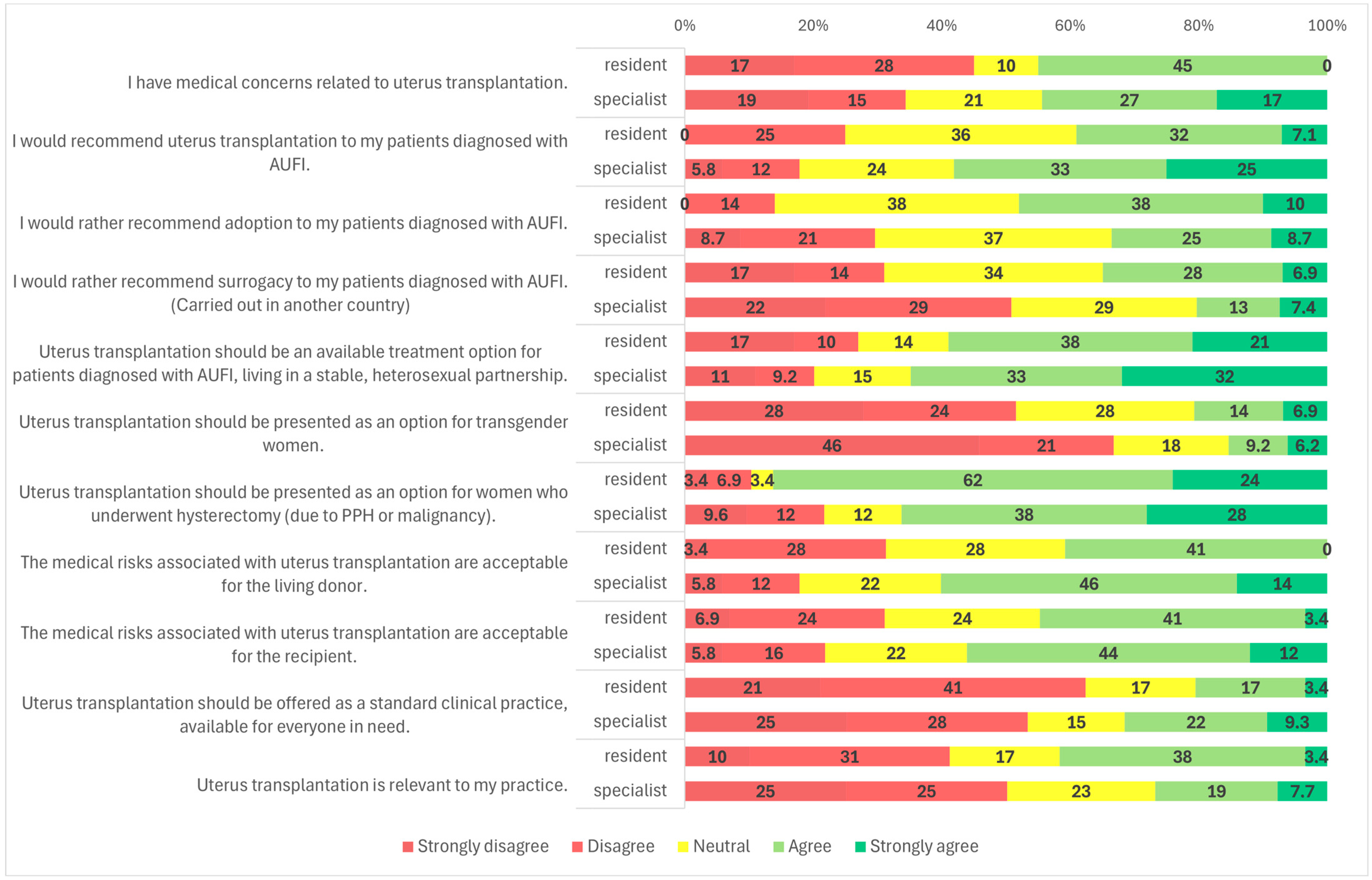
3.2. Candidates for UTx
3.3. Alternative Treatment Options for AUFI
3.4. Risk Assessment of the UTx Procedure
3.5. UTx as Standard Clinical Practice
3.6. Relevance to Practice
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUFI | absolute uterine factor infertility |
| MRKH | Mayer-Rokitansky-Küster-Hauser syndrome |
| UTx | uterus transplant |
| LD | live donor |
| DD | deceased donor |
Appendix A
Appendix A.1. Background Information
Appendix A.2. Survey
- Demographics
- What is your specialty? (multiple choice)
- ☐
- Obstetrician/gynecologist
- ☐
- Assisted reproduction specialist
- ☐
- Gynecological oncologist
- ☐
- Pediatric and adolescent gynecologist
- ☐
- Transplant surgeon
- ☐
- Fetal ultrasound specialist
- ☐
- Other (please specify)
- What is your current professional role?
- ☐
- Resident
- ☐
- Specialist
- Gender
- ☐
- Male
- ☐
- Female
- How old are you?
- ☐
- 25–35 years old
- ☐
- 36–45 years old
- ☐
- 46–55 years old
- ☐
- 56–55 years old
- ☐
- 66+ years old
- How long have you been practicing medicine?
- ☐
- 0–5
- ☐
- 6–10
- ☐
- 11–15
- ☐
- 16–20
- ☐
- 21–25
- ☐
- 26+ years
- What best describes the medical setting you practice in? (multiple choice)
- ☐
- University clinic
- ☐
- County hospital or teaching hospital
- ☐
- City hospital
- ☐
- Polyclinic
- ☐
- Private clinic
- ☐
- Private hospital
- ☐
- Private practice
- ☐
- Fertility center
- ☐
- Other (please specify)
- I have medical concerns related to uterus transplantation.
- I would recommend uterus transplantation to my patients diagnosed with AUFI.
- I would rather recommend adoption to my patients diagnosed with AUFI.
- I would rather recommend surrogacy to my patients diagnosed with AUFI. (Carried out in another country)
- Uterus transplantation should be an available treatment option for patients diagnosed with AUFI, living in a stable, heterosexual partnership.
- Uterus transplantation should be presented as an option for transgender women.
- Uterus transplantation should be presented as an option for women who underwent hysterectomy (due to PPH or malignancy).
- The medical risks associated with uterus transplantation are acceptable for the living donor.
- The medical risks associated with uterus transplantation are acceptable for the recipient.
- Uterus transplantation should be offered as a standard clinical practice, available for everyone in need.
- Uterus transplantation is relevant to my practice.
References
- Sieunarine, K.; Zakaria, F.B.; Boyle, D.C.; Corless, D.J.; Noakes, D.E.; Lindsay, I.; Lawson, A.; Ungar, L.; Del Priores, G.; Smith, J.R. Possibilities for fertility restoration: A new surgical technique. Int. Surg. 2005, 90, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Farkas, B.; Kolumban, S.; Papp, K.S.; Fazekas, G.; Kovacs, K.; Bodis, J. Current legal standpoint on surrogacy in Hungary. J. Assist. Reprod. Genet. 2024, 42, 343. [Google Scholar] [CrossRef] [PubMed]
- Brännström, M. A decade of human uterus transplantation. Acta Obstet. Gynecol. Scand. 2025, 104, 434–436. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brännström, M.; Racowsky, C.; Carbonnel, M.; Wu, J.; Gargiulo, A.; Adashi, E.Y.; Ayoubi, J.M. Uterus transplantation worldwide: Clinical activities and outcomes. Curr. Opin. Organ Transplant. 2021, 26, 616–626. [Google Scholar] [CrossRef] [PubMed]
- Brännström, M.; Tullius, S.G.; Fronek, J.; Brucker, S.Y. Meeting report: Third International Congress of the International Society of Uterus Transplantation (ISUTx). Transplantation 2022, 106, 2271–2274. [Google Scholar] [CrossRef] [PubMed]
- Brännström, M.; Tullius, S.G.; Brucker, S.; Dahm-Kahler, P.; Flyckt, R.; Kisu, I.; Andraus, W.; Wei, L.; Carmona, F.; Ayoubi, J.M.; et al. Registry of the International Society of uterus transplantation: First report. Transplantation 2023, 107, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Brännström, M.; Johannesson, L.; Bokstrom, H.; Kvarnstrom, N.; Molne, J.; Dahm-Kahler, P.; Enskog, A.; Milenkovic, M.; Ekberg, J.; Diaz-Garcia, C.; et al. Livebirth after uterus transplantation. Lancet 2015, 385, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Bortoletto, P.; Hariton, E.; Farland, L.V.; Goldman, R.H.; Gargiulo, A.R. Uterine Transplantation: A survey of perceptions and attitudes of American reproductive endocrinologists and gynecologic surgeons. J. Minim. Invasive Gynecol. 2018, 25, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Saso, S.; Clarke, A.; Bracewell-Milnes, T.; Al-Memar, M.; Hamed, A.H.; Thum, M.Y.; Ghaem-Maghami, S.; Del Priore, G.; Smith, J.R. Survey of perceptions of health care professionals in the United Kingdom toward uterine transplant. Prog. Transplant. 2015, 25, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Vyas, P.; Sader, D.; Testa, G.; Du, J.; Wall, A.; Johannesson, L. Exploring divergent views: A comparative study of uterus transplantation perceptions among transplant and Obstetrics/Gynecology providers. J. Clin. Med. 2024, 13, 3182. [Google Scholar] [CrossRef] [PubMed]
- Riggan, K.A.; Khan, Z.; Langstraat, C.L.; Allyse, M.A. Provider Knowledge and Support of Uterus Transplantation: Surveying Multidisciplinary Team Members. Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Balayla, J.; Tulandi, T.; McGill University Uterine Transplantation Exploratory Committee. Provider Perceptions, Opinions, and Insights into Uterine Transplantation in Canada. J. Obstet. Gynaecol. Can. JOGC 2019, 41, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Farkas, B.; Kovács, K.; Kolumbán, S.; Rozanovic, M.; Hegedűs, E.; Jancsó, G.; Bódis, J.; Fazekas, G. The experimental uterus autotransplantation sheep model. Orvosi Hetil. 2024, 14, 1079–1085. (In Hungarian) [Google Scholar] [CrossRef] [PubMed]
- Farkas, B.; Kovács, K.; Kolumbán, S.; Papp, K.S.; Márton, Z.; Bódis, J.; Fazekas, G. Surgical steps of organ retrieval from deceased donor for uterus transplantation. Orvosi Hetil. 2025, 166, 385–391. (In Hungarian) [Google Scholar] [CrossRef]
- Brännström, M.; Racowsky, C.; Carbonnel, M.; Wu, J.; Gargiulo, A.; Adashi, E.Y.; Ayoubi, J.M. Uterus transplantation: From research, through human trials and into the future. Hum. Reprod. Update 2023, 29, 521–544. [Google Scholar] [CrossRef] [PubMed]
- Flyckt, R.L.; Farrell, R.M.; Perni, U.C.; Tzakis, A.G.; Falcone, T. Deceased Donor Uterine Transplantation: Innovation and Adaptation. Obstet. Gynecol. 2016, 128, 837–842. [Google Scholar] [CrossRef]
- Flyckt, R.; Kotlyar, A.; Arian, S.; Eghtesad, B.; Falcone, T.; Tzakis, A. Deceased donor uterine transplantation. Fertil. Steril. 2017, 107, e13. [Google Scholar] [CrossRef]
- Flyckt, R.; Davis, A.; Farrell, R.; Zimberg, S.; Tzakis, A.; Falcone, T. Uterine Transplantation: Surgical Innovation in the Treatment of Uterine Factor Infertility. J. Obstet. Gynaecol. Can. JOGC 2018, 40, 86–93. [Google Scholar] [CrossRef]



| Number of Participants (n) | Percentage (%) | ||
|---|---|---|---|
| Gender | Male | 195 | 67.2 |
| Female | 95 | 32.8 | |
| Age | 25–35 | 60 | 20.6 |
| 36–45 | 58 | 20 | |
| 46–55 | 61 | 21 | |
| 55–65 | 60 | 20.6 | |
| >66 | 51 | 17.6 | |
| Medical qualification | Specialist | 261 | 90 |
| Resident | 29 | 10 | |
| Years of experience | 0–5 | 30 | 10.3 |
| 6–10 | 38 | 13.1 | |
| 11–15 | 28 | 9.6 | |
| 16–20 | 25 | 8.6 | |
| 21–25 | 32 | 11 | |
| >26 | 137 | 47.2 | |
| Medical specialty | Anesthesiology | 1 | 0.3 |
| GP | 1 | 0.3 | |
| Internal Medicine | 2 | 0.7 | |
| OB/GYN | 245 | 84 | |
| Surgery | 1 | 0.3 | |
| Transplantation | 36 | 12 | |
| Vascular surgery | 4 | 1.4 | |
| Professional setting | Clinical centre | 123 | 42 |
| City/County hospital | 95 | 33 | |
| Polyclinic | 20 | 6.9 | |
| Private care | 46 | 16 | |
| Fertility center | 4 | 1.4 | |
| Blood bank | 2 | 0.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papp, K.S.; Szakaly, P.; Kolumban, S.; Kovács, K.A.; Bodis, J.; Farkas, N.; Fazekas, G.; Farkas, B. Medical Professionals’ Opinions of and Attitudes Toward Uterus Transplantation in Hungary. Clin. Pract. 2025, 15, 194. https://doi.org/10.3390/clinpract15110194
Papp KS, Szakaly P, Kolumban S, Kovács KA, Bodis J, Farkas N, Fazekas G, Farkas B. Medical Professionals’ Opinions of and Attitudes Toward Uterus Transplantation in Hungary. Clinics and Practice. 2025; 15(11):194. https://doi.org/10.3390/clinpract15110194
Chicago/Turabian StylePapp, Kata Szilvia, Peter Szakaly, Szilard Kolumban, Kálmán András Kovács, Jozsef Bodis, Nelli Farkas, Gabor Fazekas, and Balint Farkas. 2025. "Medical Professionals’ Opinions of and Attitudes Toward Uterus Transplantation in Hungary" Clinics and Practice 15, no. 11: 194. https://doi.org/10.3390/clinpract15110194
APA StylePapp, K. S., Szakaly, P., Kolumban, S., Kovács, K. A., Bodis, J., Farkas, N., Fazekas, G., & Farkas, B. (2025). Medical Professionals’ Opinions of and Attitudes Toward Uterus Transplantation in Hungary. Clinics and Practice, 15(11), 194. https://doi.org/10.3390/clinpract15110194








