Temporal Evolution of the Profile of Patients Hospitalized with Heart Failure (2000–2022)
Abstract
1. Introduction
2. Materials and Methods
Data Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Rules of Association 2000–2004 | Support | Confidence | Lift | Number | ||
|---|---|---|---|---|---|---|
| {Cardiomyopathy} | => | {Congestive heart failure} | 0.0191 | 0.7208 | 1.5891 | 581 |
| {Pulmonary hypertension} | => | {Congestive heart failure} | 0.025 | 0.5958 | 1.3133 | 759 |
| {Valvular heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0121 | 0.5919 | 1.3049 | 367 |
| {Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0268 | 0.5824 | 1.2838 | 813 |
| {Valvular heart disease} | => | {Congestive heart failure} | 0.0431 | 0.5761 | 1.2701 | 1309 |
| {Diabetes Mellitus 2, Arrhythmias} | => | {Congestive heart failure} | 0.0107 | 0.5755 | 1.2686 | 324 |
| {Other infections, Arrhythmias} | => | {Congestive heart failure} | 0.0128 | 0.5742 | 1.2657 | 387 |
| {Acute kidney failure} | => | {Congestive heart failure} | 0.0393 | 0.5741 | 1.2656 | 1193 |
| {Valvular heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.0112 | 0.5736 | 1.2645 | 339 |
| {Arrhythmias, chronic obstructive pulmonary disease} | => | {Congestive heart failure} | 0.0113 | 0.5736 | 1.2644 | 343 |
| {Valvular heart disease, Hypertension} | => | {Congestive heart failure} | 0.0112 | 0.5721 | 1.2613 | 341 |
| {Atrial fibrillation} | => | {Congestive heart failure} | 0.0143 | 0.5606 | 1.2357 | 435 |
| {Chronic kidney disease} | => | {Congestive heart failure} | 0.0378 | 0.5584 | 1.231 | 1147 |
| {Arrhythmias} | => | {Congestive heart failure} | 0.0799 | 0.5548 | 1.2231 | 2423 |
| {Other pulmonary disease} | => | {Congestive heart failure} | 0.01 | 0.5497 | 1.2118 | 304 |
| {Acute respiratory failure} | => | {Congestive heart failure} | 0.0432 | 0.5437 | 1.1986 | 1312 |
| {Dementia} | => | {Congestive heart failure} | 0.0245 | 0.5319 | 1.1725 | 742 |
| {Anemia} | => | {Congestive heart failure} | 0.0413 | 0.5208 | 1.148 | 1253 |
| {Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0239 | 0.5197 | 1.1456 | 726 |
| {Abnormality on additional tests} | => | {Congestive heart failure} | 0.0194 | 0.5162 | 1.1379 | 590 |
| {Diffuse Parenchymal Lung Disease} | => | {Congestive heart failure} | 0.0165 | 0.516 | 1.1374 | 501 |
| {Drug adverse effects} | => | {Congestive heart failure} | 0.018 | 0.5156 | 1.1365 | 547 |
| {Goiter} | => | {Congestive heart failure} | 0.0137 | 0.5142 | 1.1335 | 417 |
| {Other kidney diseases} | => | {Congestive heart failure} | 0.012 | 0.507 | 1.1176 | 363 |
| Rules of association 2005–2009 | Support | Confidence | Lift | Number | ||
| {Chronic kidney disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0102 | 0.7583 | 1.5523 | 182 |
| {Valvular heart disease, Pulmonary hypertension} | => | {Congestive heart failure} | 0.0121 | 0.7465 | 1.5281 | 215 |
| {Arrythmias, Acute kidney failure} | => | {Congestive heart failure} | 0.0126 | 0.7329 | 1.5002 | 225 |
| {Pleural effusion} | => | {Congestive heart failure} | 0.0184 | 0.7321 | 1.4987 | 328 |
| {Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0121 | 0.7264 | 1.4868 | 215 |
| {Acute respiratory failure, Acute renal failure} | => | {Congestive heart failure} | 0.0116 | 0.7263 | 1.4867 | 207 |
| {Chronic kidney disease, Arrhythmias} | => | {Congestive heart failure} | 0.013 | 0.7108 | 1.4549 | 231 |
| {Cardiomyopathy} | => | {Congestive heart failure} | 0.0175 | 0.7107 | 1.4548 | 312 |
| {Anemia, Arrhythmias} | => | {Congestive heart failure} | 0.0121 | 0.7036 | 1.4402 | 216 |
| {Pulmonary hypertension} | => | {Congestive heart failure} | 0.0335 | 0.6945 | 1.4217 | 598 |
| {Other mental disorders, Arrhythmias} | => | {Congestive heart failure} | 0.0104 | 0.6877 | 1.4078 | 185 |
| {Arrhythmias, Hydronephrosis/Acute Urinary Retention} | => | {Congestive heart failure} | 0.0124 | 0.6863 | 1.4049 | 221 |
| {Other infections, Arrhythmias} | => | {Congestive heart failure} | 0.0183 | 0.6579 | 1.3468 | 327 |
| {Valvular heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0216 | 0.6559 | 1.3426 | 385 |
| {Other infections, Chronic kidney disease} | => | {Congestive heart failure} | 0.011 | 0.6384 | 1.3069 | 196 |
| {Valvular heart disease, Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0103 | 0.6354 | 1.3007 | 183 |
| {Chronic kidney disease, Acute renal failure} | => | {Congestive heart failure} | 0.0164 | 0.6342 | 1.2982 | 293 |
| {Valvular heart disease} | => | {Congestive heart failure} | 0.0621 | 0.634 | 1.2978 | 1107 |
| {Valvular heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.0193 | 0.6335 | 1.2968 | 344 |
| {Acute respiratory failure} | => | {Congestive heart failure} | 0.065 | 0.6233 | 1.2758 | 1158 |
| {Myopericarditis} | => | {Congestive heart failure} | 0.0154 | 0.6222 | 1.2736 | 275 |
| {Acute respiratory failure, miscellaneous} | => | {Congestive heart failure} | 0.018 | 0.6209 | 1.2709 | 321 |
| {Arrhythmias, Chronic obstructive pulmonary disease} | => | {Congestive heart failure} | 0.0113 | 0.6204 | 1.2699 | 201 |
| {Acute Renal failure, miscellaneous} | => | {Congestive heart failure} | 0.0127 | 0.6192 | 1.2674 | 226 |
| {Hypertension, Acute respiratory failure} | => | {Congestive heart failure} | 0.011 | 0.6183 | 1.2656 | 196 |
| {Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.04 | 0.6182 | 1.2654 | 714 |
| {Diabetes Mellitus 2, Arrhythmias} | => | {Congestive heart failure} | 0.0153 | 0.6085 | 1.2456 | 272 |
| {Other infections, Acute respiratory failure} | => | {Congestive heart failure} | 0.0173 | 0.6063 | 1.2411 | 308 |
| {Valvular heart disease, Hypertension} | => | {Congestive heart failure} | 0.0214 | 0.6038 | 1.236 | 381 |
| {Chronic kidney disease} | => | {Congestive heart failure} | 0.0545 | 0.6034 | 1.235 | 972 |
| {Arrhythmias} | => | {Congestive heart failure} | 0.0992 | 0.6031 | 1.2346 | 1769 |
| {Anemia, Chronic kidney disease} | => | {Congestive heart failure} | 0.0121 | 0.6022 | 1.2328 | 215 |
| {Other infections, Acute renal failure} | => | {Congestive heart failure} | 0.0135 | 0.6015 | 1.2313 | 240 |
| {Other endocrine disease, Atrial fibrillation} | => | {Congestive heart failure} | 0.0107 | 0.5969 | 1.2218 | 191 |
| {Chronic kidney disease, Miscellaneous} | => | {Congestive heart failure} | 0.0133 | 0.5906 | 1.2089 | 238 |
| {Other pulmonary disease} | => | {Congestive heart failure} | 0.019 | 0.5885 | 1.2047 | 339 |
| {Anemia, Miscellaneous} | => | {Congestive heart failure} | 0.0148 | 0.5884 | 1.2044 | 263 |
| {Acute kidney failure} | => | {Congestive heart failure} | 0.056 | 0.5871 | 1.2017 | 998 |
| {Atrial fibrillation} | => | {Congestive heart failure} | 0.0273 | 0.5825 | 1.1924 | 487 |
| {Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0356 | 0.5695 | 1.1658 | 635 |
| {Hypertension, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0171 | 0.569 | 1.1648 | 305 |
| {Ischemic heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0124 | 0.5638 | 1.154 | 221 |
| {Hydronephrosis/Acute Urinary Retention, Miscellaneous} | => | {Congestive heart failure} | 0.0118 | 0.5627 | 1.1518 | 211 |
| {Dementia} | => | {Congestive heart failure} | 0.034 | 0.5616 | 1.1496 | 606 |
| {Chronic respiratory failure} | => | {Congestive heart failure} | 0.0129 | 0.561 | 1.1483 | 230 |
| {Adverse drug event} | => | {Congestive heart failure} | 0.0293 | 0.5607 | 1.1477 | 522 |
| {Cardiac prosthesis or device} | => | {Congestive heart failure} | 0.0201 | 0.5508 | 1.1274 | 358 |
| {Anemia} | => | {Congestive heart failure} | 0.0523 | 0.5466 | 1.1189 | 932 |
| {Other endocrine disease, Miscellaneous} | => | {Congestive heart failure} | 0.0105 | 0.5374 | 1.0999 | 187 |
| {Goiter} | => | {Congestive heart failure} | 0.0136 | 0.5352 | 1.0956 | 243 |
| {Other infections, anemia} | => | {Congestive heart failure} | 0.0102 | 0.5339 | 1.0929 | 181 |
| {Acute-on-chronic respiratory failure} | => | {Congestive heart failure} | 0.0164 | 0.528 | 1.0809 | 292 |
| {Other mental disorders, Miscellaneous} | => | {Congestive heart failure} | 0.0108 | 0.5246 | 1.0738 | 192 |
| {Dyslipidemia, Arrhythmias} | => | {Congestive heart failure} | 0.0132 | 0.5244 | 1.0735 | 236 |
| {Social problems} | => | {Congestive heart failure} | 0.0179 | 0.5212 | 1.067 | 319 |
| {Oxygen therapy dependence} | => | {Congestive heart failure} | 0.0132 | 0.521 | 1.0664 | 236 |
| {Anemia, Hypertension} | => | {Congestive heart failure} | 0.0113 | 0.5206 | 1.0657 | 202 |
| {Electrolyte disorders} | => | {Congestive heart failure} | 0.0342 | 0.5201 | 1.0646 | 609 |
| {Hydronephrosis/Acute Urinary Retention} | => | {Congestive heart failure} | 0.0453 | 0.5193 | 1.0629 | 808 |
| {Personal history of neoplasm} | => | {Congestive heart failure} | 0.0154 | 0.5159 | 1.0561 | 275 |
| {Ischemic heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.014 | 0.5155 | 1.0551 | 250 |
| {Other kidney diseases} | => | {Congestive heart failure} | 0.0131 | 0.5143 | 1.0529 | 233 |
| {Other infections, Miscellaneous} | => | {Congestive heart failure} | 0.0186 | 0.514 | 1.0521 | 331 |
| {Diffuse Parenchymal Lung Disease} | => | {Congestive heart failure} | 0.0169 | 0.5119 | 1.0478 | 302 |
| {Other endocrine disease} | => | {Congestive heart failure} | 0.0373 | 0.5076 | 1.0391 | 665 |
| {Other infections, Hydronephrosis/Acute Urinary Retention} | => | {Congestive heart failure} | 0.022 | 0.5064 | 1.0367 | 393 |
| {Asthma} | => | {Congestive heart failure} | 0.0132 | 0.5054 | 1.0345 | 235 |
| {Other mental disorders} | => | {Congestive heart failure} | 0.0374 | 0.5053 | 1.0343 | 667 |
| {Abnormality on additional tests} | => | {Congestive heart failure} | 0.0252 | 0.5017 | 1.0269 | 449 |
| {Atherosclerosis} | => | {Congestive heart failure} | 0.0115 | 0.5012 | 1.026 | 205 |
| Rules of association 2010–2014 | Support | Confidence | Lift | Number | ||
| {Hypertension, Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0112 | 0.9058 | 1.609 | 125 |
| {Hypertension, Arrhythmias, Acute respiratory failure, Atrial fibrillation} | => | {Congestive heart failure} | 0.0102 | 0.8976 | 1.5945 | 114 |
| {Hypertension, Acute respiratory failure, Atrial fibrillation} | => | {Congestive heart failure} | 0.0104 | 0.8931 | 1.5865 | 117 |
| {Hypertension, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.014 | 0.8771 | 1.558 | 157 |
| {Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0176 | 0.8717 | 1.5484 | 197 |
| {Cardiomyopathies, Miscellaneous} | => | {Congestive heart failure} | 0.011 | 0.8662 | 1.5387 | 123 |
| {Acute respiratory failure, Atrial fibrillation, Miscellaneous} | => | {Congestive heart failure} | 0.0138 | 0.8652 | 1.5368 | 154 |
| {Arrhythmias, Acute respiratory failure, Atrial fibrillation, Miscellaneous} | => | {Congestive heart failure} | 0.013 | 0.8639 | 1.5346 | 146 |
| {Arrythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0278 | 0.8567 | 1.5219 | 311 |
| {Valvular heart disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0127 | 0.8503 | 1.5104 | 142 |
| {Chronic kidney disease, Arrhythmias, Acute renal failure} | => | {Congestive heart failure} | 0.0101 | 0.8496 | 1.5092 | 113 |
| {Arrhythmias, Acute respiratory failure, Atrial fibrillation} | => | {Congestive heart failure} | 0.0166 | 0.8493 | 1.5087 | 186 |
| {Acute respiratory failure, Atrial fibrillation} | => | {Congestive heart failure} | 0.018 | 0.8487 | 1.5076 | 202 |
| {Dyslipidemia, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.01 | 0.8358 | 1.4847 | 112 |
| {Chronic kidney disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0162 | 0.8341 | 1.4816 | 181 |
| {Valvular heart disease, Acute renal failure} | => | {Congestive heart failure} | 0.0126 | 0.8294 | 1.4733 | 141 |
| {Ischemic heart disease, Acute renal failure} | => | {Congestive heart failure} | 0.0101 | 0.8248 | 1.4652 | 113 |
| {Other infections, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.01 | 0.8235 | 1.4629 | 112 |
| {Chronic kidney disease, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0142 | 0.8196 | 1.4559 | 159 |
| {Valvular heart disease, pulmonary hypertension} | => | {Congestive heart failure} | 0.0164 | 0.8142 | 1.4462 | 184 |
| {Other endocrine disease, Cardiomyopathy} | => | {Congestive heart failure} | 0.01 | 0.8116 | 1.4417 | 112 |
| {Chronic kidney disease, Arrhythmias, Atrial fibrillation} | => | {Congestive heart failure} | 0.0115 | 0.8063 | 1.4322 | 129 |
| {Acute respiratory failure, acute renal failure} | => | {Congestive heart failure} | 0.0202 | 0.8014 | 1.4236 | 226 |
| {Anemia, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.014 | 0.801 | 1.4229 | 157 |
| {Acute respiratory failure, Hydronephrosis/Acute Urinary Retention} | => | {Congestive heart failure} | 0.0129 | 0.8 | 1.4211 | 144 |
| {Arrhythmias, Other pulmonary disease, Miscellaneous} | => | {Congestive heart failure} | 0.0121 | 0.8 | 1.4211 | 136 |
| Rules of association 2015–2019 | Support | Confidence | Lift | Number | ||
| {Arrhythmias, Acute respiratory failure, acute renal failure} | => | {Congestive heart failure} | 0.0123 | 0.949 | 1.44 | 93 |
| {Chronic kidney disease, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0117 | 0.9263 | 1.4056 | 88 |
| {Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0459 | 0.9081 | 1.378 | 346 |
| {Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0275 | 0.9039 | 1.3716 | 207 |
| {Hypertension, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0218 | 0.9011 | 1.3673 | 164 |
| {Valvular heart disease, Cardiomyopathies} | => | {Congestive heart failure} | 0.0102 | 0.8953 | 1.3586 | 77 |
| {Other infections, Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0164 | 0.8921 | 1.3537 | 124 |
| {Other infections, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0252 | 0.892 | 1.3536 | 190 |
| {Hypertension, Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0147 | 0.888 | 1.3475 | 111 |
| {Chronic kidney disease, Acute respiratory failure, Acute renal failure} | => | {Congestive heart failure} | 0.0156 | 0.8872 | 1.3463 | 118 |
| {Valvular heart disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0198 | 0.8869 | 1.3458 | 149 |
| {Valvular heart disease, pulmonary hypertension} | => | {Congestive heart failure} | 0.0176 | 0.8867 | 1.3454 | 133 |
| {Other infections, Mental disorders, Arrhythmias} | => | {Congestive heart failure} | 0.0114 | 0.8866 | 1.3453 | 86 |
| {Anemia, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0103 | 0.8864 | 1.345 | 78 |
| {Ischemic heart disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0145 | 0.8862 | 1.3447 | 109 |
| {Dyslipidemia, Cardiomyopathies} | => | {Congestive heart failure} | 0.0113 | 0.8854 | 1.3435 | 85 |
| {Diabetes mellitus 2, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0106 | 0.8791 | 1.334 | 80 |
| {Pulmonary hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0143 | 0.878 | 1.3324 | 108 |
| {Dyslipidemia, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.013 | 0.875 | 1.3277 | 98 |
| {Other infections, Acute respiratory failure, Acute renal failure} | => | {Congestive heart failure} | 0.0182 | 0.8726 | 1.3241 | 137 |
| {Chronic kidney disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0135 | 0.8718 | 1.3229 | 102 |
| {Cardiomyopathies, Arrhythmias} | => | {Congestive heart failure} | 0.0131 | 0.8684 | 1.3177 | 99 |
| {Chronic kidney disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0292 | 0.8661 | 1.3143 | 220 |
| {Other infections, Hypertension, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0127 | 0.8649 | 1.3124 | 96 |
| {Other infections, Dementia, Arrhythmias} | => | {Congestive heart failure} | 0.0133 | 0.8621 | 1.3081 | 100 |
| {Acute respiratory failure, Acute renal failure, Miscellaneous} | => | {Congestive heart failure} | 0.0149 | 0.8615 | 1.3073 | 112 |
| {Acute respiratory failure, acute renal failure} | => | {Congestive heart failure} | 0.0338 | 0.8615 | 1.3072 | 255 |
| {Other infections, Arrhythmias, Acute renal failure, Miscellaneous} | => | {Congestive heart failure} | 0.0115 | 0.8614 | 1.3071 | 87 |
| {Other infections, Chronic kidney disease, Arrhythmias} | => | {Congestive heart failure} | 0.0139 | 0.8607 | 1.306 | 105 |
| {Cardiomyopathy} | => | {Congestive heart failure} | 0.0325 | 0.8596 | 1.3044 | 245 |
| {Cardiomyopathies, Miscellaneous} | => | {Congestive heart failure} | 0.0146 | 0.8594 | 1.304 | 110 |
| {Anemia, Acute respiratory failure} | => | {Congestive heart failure} | 0.0227 | 0.855 | 1.2974 | 171 |
| {Mental disorders, Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0133 | 0.8547 | 1.2969 | 100 |
| {Other infections, Arrhythmias, Acute renal failure} | => | {Congestive heart failure} | 0.0179 | 0.8544 | 1.2965 | 135 |
| {Mental disorders, Arrhythmias} | => | {Congestive heart failure} | 0.0247 | 0.8532 | 1.2947 | 186 |
| {Mental disorders, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.013 | 0.8522 | 1.2931 | 98 |
| {Electrolyte disorders, Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0113 | 0.85 | 1.2898 | 85 |
| {Other infections, Obesity, Arrhythmias} | => | {Congestive heart failure} | 0.0102 | 0.8462 | 1.284 | 77 |
| {Other infections, Acute respiratory failure, Hydronephrosis/Acute Urinary Retention} | => | {Congestive heart failure} | 0.0107 | 0.8438 | 1.2803 | 81 |
| {Other infections, Ischemic heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.0105 | 0.8404 | 1.2753 | 79 |
| {Electrolyte disorders, Valvular heart disease} | => | {Congestive heart failure} | 0.0111 | 0.84 | 1.2746 | 84 |
| {Pulmonary hypertension} | => | {Congestive heart failure} | 0.0381 | 0.8392 | 1.2734 | 287 |
| {Other infections, Anemia, Arrhythmias} | => | {Congestive heart failure} | 0.0138 | 0.8387 | 1.2727 | 104 |
| {Obesity, Valvular heart disease} | => | {Congestive heart failure} | 0.0143 | 0.8372 | 1.2704 | 108 |
| {Other infections, Ischemic heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.0163 | 0.8367 | 1.2697 | 123 |
| {Hypothyroidism, Arrhythmias} | => | {Congestive heart failure} | 0.0115 | 0.8365 | 1.2694 | 87 |
| {Obesity, Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0183 | 0.8364 | 1.2691 | 138 |
| {Other infections, Chronic kidney disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0142 | 0.8359 | 1.2685 | 107 |
| {Obesity, Arrhythmias} | => | {Congestive heart failure} | 0.029 | 0.8327 | 1.2635 | 219 |
| {Other infections. Vascular heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0145 | 0.8321 | 1.2626 | 109 |
| {Obesity, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0105 | 0.8316 | 1.2618 | 79 |
| {Pleural effusion} | => | {Congestive heart failure} | 0.0261 | 0.8312 | 1.2613 | 197 |
| {Diabetes mellitus 2, Acute respiratory failure} | => | {Congestive heart failure} | 0.0245 | 0.8296 | 1.2588 | 185 |
| {Other infections, Hypothyroidism} | => | {Congestive heart failure} | 0.0102 | 0.828 | 1.2563 | 77 |
| {Other endocrine disease, Acute respiratory failure.} | => | {Congestive heart failure} | 0.0159 | 0.8276 | 1.2558 | 120 |
| {Hypertension, Cardiomyopathies} | => | {Congestive heart failure} | 0.0114 | 0.8269 | 1.2548 | 86 |
| {Acute respiratory failure, Hydronephrosis/Acute Urinary Retention} | => | {Congestive heart failure} | 0.0183 | 0.8263 | 1.2539 | 138 |
| {Electrolyte disorders, Valvular heart disease} | => | {Congestive heart failure} | 0.0113 | 0.8252 | 1.2522 | 85 |
| {Other infections, Mental disorders, Arrhythmias} | => | {Congestive heart failure} | 0.0113 | 0.8252 | 1.2522 | 85 |
| {Valvular heart disease, Chronic kidney disease} | => | {Congestive heart failure} | 0.026 | 0.8235 | 1.2496 | 196 |
| {Anemia, Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0149 | 0.8235 | 1.2496 | 112 |
| {Diabetes mellitus 2, Hypertension, Acute respiratory failure} | => | {Congestive heart failure} | 0.013 | 0.8235 | 1.2496 | 98 |
| {Diabetes mellitus 2, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0129 | 0.822 | 1.2474 | 97 |
| {Electrolyte disorders, Arrhythmias} | => | {Congestive heart failure} | 0.0237 | 0.8211 | 1.2459 | 179 |
| {Mental disorders, Acute respiratory failure} | => | {Congestive heart failure} | 0.0188 | 0.8208 | 1.2455 | 142 |
| {Hypertension, pulmonary hypertension} | => | {Congestive heart failure} | 0.0109 | 0.82 | 1.2443 | 82 |
| {Electrolyte disorders, Acute respiratory failure} | => | {Congestive heart failure} | 0.0223 | 0.8195 | 1.2435 | 168 |
| {Acute respiratory failure, social problems} | => | {Congestive heart failure} | 0.0156 | 0.8194 | 1.2434 | 118 |
| {Other infections. Vascular heart disease, Arrythmia, Miscellaneous} | => | {Congestive heart failure} | 0.0102 | 0.8191 | 1.243 | 77 |
| {Hypertension, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0228 | 0.819 | 1.2428 | 172 |
| {Other infections, Arrhythmias} | => | {Congestive heart failure} | 0.0675 | 0.8183 | 1.2417 | 509 |
| {Hypertension, Ischemic heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0155 | 0.8182 | 1.2415 | 117 |
| {Other infections, Anemia, Acute respiratory failure} | => | {Congestive heart failure} | 0.0107 | 0.8182 | 1.2415 | 81 |
| {Anemia, Valvular heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.0101 | 0.8172 | 1.24 | 76 |
| {Ischemic heart disease, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0178 | 0.8171 | 1.2398 | 134 |
| {Acute respiratory failure, miscellaneous} | => | {Congestive heart failure} | 0.0525 | 0.8165 | 1.239 | 396 |
| {Arrhythmias, Social problems, Miscellaneous} | => | {Congestive heart failure} | 0.0123 | 0.8158 | 1.2379 | 93 |
| {Other infections, Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0363 | 0.8155 | 1.2374 | 274 |
| {Chronic kidney disease, Ischemic heart disease} | => | {Congestive heart failure} | 0.018 | 0.8144 | 1.2357 | 136 |
| {Hypertension, Arrhythmias, Chronic obstructive pulmonary disease} | => | {Congestive heart failure} | 0.0122 | 0.8142 | 1.2354 | 92 |
| {Dementia, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0139 | 0.814 | 1.2351 | 105 |
| {Other infections, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0427 | 0.8131 | 1.2339 | 322 |
| {Other infections, Electrolyte disorders, Acute respiratory failure} | => | {Congestive heart failure} | 0.0103 | 0.8125 | 1.2329 | 78 |
| {Valvular heart disease, Hypertension, Arrhythmias} | => | {Congestive heart failure} | 0.0276 | 0.8125 | 1.2329 | 208 |
| {Chronic kidney disease, Arrhythmias} | => | {Congestive heart failure} | 0.0424 | 0.8122 | 1.2324 | 320 |
| {Arrhythmias, Social problems} | => | {Congestive heart failure} | 0.0195 | 0.8122 | 1.2324 | 147 |
| {Diabetes mellitus 2, Dyslipidemia, Acute respiratory failure} | => | {Congestive heart failure} | 0.0109 | 0.8119 | 1.232 | 82 |
| {Chronic kidney disease, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0239 | 0.8108 | 1.2303 | 180 |
| {Other infections, Arrhythmias, Chronic obstructive pulmonary disease} | => | {Congestive heart failure} | 0.0102 | 0.8105 | 1.2299 | 77 |
| {Pulmonary hypertension, Miscellaneous} | => | {Congestive heart failure} | 0.0158 | 0.8095 | 1.2284 | 119 |
| {Dementia, Arrhythmias} | => | {Congestive heart failure} | 0.0236 | 0.8091 | 1.2277 | 178 |
| {Dementia, Acute respiratory failure} | => | {Congestive heart failure} | 0.0219 | 0.8088 | 1.2273 | 165 |
| {Valvular heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0488 | 0.8088 | 1.2273 | 368 |
| {Other infections. Hypertension, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0247 | 0.8087 | 1.2271 | 186 |
| {Hypertension, Arrhythmias, Social problems} | => | {Congestive heart failure} | 0.0106 | 0.8081 | 1.2262 | 80 |
| {Electrolyte disorders, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0139 | 0.8077 | 1.2256 | 105 |
| {Valvular heard disease, Hypertension, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0172 | 0.8075 | 1.2252 | 130 |
| {Other infections, Diabetes mellitus 2, Arrhythmias} | => | {Congestive heart failure} | 0.0145 | 0.8074 | 1.2252 | 109 |
| {Obesity, Hypertension, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0117 | 0.8073 | 1.2251 | 88 |
| => | {Congestive heart failure} | 0.0277 | 0.8069 | 1.2245 | 209 | |
| {Dyslipidemia, Ischemic heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0127 | 0.8067 | 1.2241 | 96 |
| {Valvular heard disease, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0292 | 0.8059 | 1.2228 | 220 |
| {Obesity, Acute respiratory failure} | => | {Congestive heart failure} | 0.0192 | 0.8056 | 1.2224 | 145 |
| {Valvular heart disease, Chronic kidney disease, Arrhythmias} | => | {Congestive heart failure} | 0.0121 | 0.8053 | 1.222 | 91 |
| {Valvular heart disease, Ischemic heart disease} | => | {Congestive heart failure} | 0.017 | 0.805 | 1.2216 | 128 |
| {Other infections, Arrhythmias, Hydronephrosis Acute Urinary Retention} | => | {Congestive heart failure} | 0.017 | 0.805 | 1.2216 | 128 |
| {Chronic kidney disease, Ischemic heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.0103 | 0.8041 | 1.2202 | 78 |
| {Electrolyte disorders, Arrhythmias, Acute renal failure} | => | {Congestive heart failure} | 0.0103 | 0.8041 | 1.2202 | 78 |
| {Obesity, Chronic kidney disease} | => | {Congestive heart failure} | 0.0135 | 0.8031 | 1.2187 | 102 |
| {Mental disorders, Chronic kidney disease} | => | {Congestive heart failure} | 0.0141 | 0.803 | 1.2185 | 106 |
| {Dyslipidemia, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0141 | 0.803 | 1.2185 | 106 |
| {Obesity, Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0172 | 0.8025 | 1.2177 | 130 |
| {Arrhythmias, Abnormality on additional tests} | => | {Congestive heart failure} | 0.0188 | 0.8023 | 1.2174 | 142 |
| {Arrythmias, Acute kidney failure} | => | {Congestive heart failure} | 0.0412 | 0.8015 | 1.2163 | 311 |
| {Hypertension, Arrhythmias, Acute renal failure} | => | {Congestive heart failure} | 0.0139 | 0.8015 | 1.2162 | |
| {Hypertension, Acute respiratory failure} | => | {Congestive heart failure} | 0.0452 | 0.8005 | 1.2146 | 341 |
| {Valvular heart disease, Chronic obstructive pulmonary disease} | => | {Congestive heart failure} | 0.0106 | 0.8 | 1.2139 | 80 |
| {Chronic kidney disease, Chronic obstructive pulmonary disease} | => | {Congestive heart failure} | 0.0122 | 0.8 | 1.2139 | 92 |
| {Diabetes mellitus 2, Obesity, Arrhythmias} | => | {Congestive heart failure} | 0.0101 | 0.8 | 1.2139 | 76 |
| {Dyslipidemia, Anemia, Chronic kidney disease} | => | {Congestive heart failure} | 0.0101 | 0.8 | 1.2139 | 76 |
References
- Chamberlain, A.M.; Boyd, C.M.; Manemann, S.M.; Dunlay, S.M.; Gerber, Y.; Killian, J.M.; Weston, S.A.; Roger, V.L. Risk factors for heart failure in the community: Differences by age and ejection fraction. Am. J. Med. 2020, 133, e237–e248. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, A.M.; St Sauver, J.L.; Gerber, Y.; Manemann, S.M.; Boyd, C.M.; Dunlay, S.M.; Rocca, W.A.; Finney Rutten, L.J.; Jiang, R.; Weston, S.A.; et al. Multimorbidity in heart failure: A community perspective. Am. J. Med. 2015, 128, 38–45. [Google Scholar] [CrossRef]
- Matesanz-Fernández, M.; Seoane-Pillado, T.; Iñiguez-Vázquez, I.; Suárez-Gil, R.; Pértega-Díaz, S.; Casariego-Vales, E. Description of multimorbidity clusters of admitted patients in medical departments of a general hospital. Postgrad. Med. J. 2022, 98, 294–299. [Google Scholar] [CrossRef]
- Escobar, C.; Palacios, B.; Escobar, C.; Palacios, B.; Gonzalez, V.; Gutiérrez, M.; Duong, M.; Chen, H.; Justo, N.; Cid-Ruzafa, J.; et al. Burden of Illness beyond Mortality and Heart Failure Hospitalizations in Patients Newly Diagnosed with Heart Failure in Spain According to Ejection Fraction. J. Clin. Med. 2023, 12, 2410. [Google Scholar] [CrossRef]
- Bozkurt, B.; Ahmad, T.; Alexander, K.; Baker, W.L.; Bosak, K.; Breathett, K.; Carter, S.; Drazner, M.H.; Dunlay, S.M.; Fonarow, G.C.; et al. HF STATS 2024: Heart Failure Epidemiology and Outcomes Statistics an Updated 2024 Report from the Heart Failure Society of America. J. Card. Fail. 2024, 31, 66–116. [Google Scholar] [CrossRef]
- Tromp, J.; Ezekowitz, J.A.; Ouwerkerk, W.; Chandramouli, C.; Yiu, K.H.; Angermann, C.E.; Dahlstrom, U.; Ertl, G.; Hassanein, M.; Perrone, S.V.; et al. Global Variations According to Sex in Patients Hospitalized for Heart Failure in the REPORT-HF Registry. JACC Heart Fail. 2023, 11, 1262–1271. [Google Scholar] [CrossRef] [PubMed]
- Nakamaru, R.; Kohsaka, S.; Shiraishi, Y.; Kohno, T.; Goda, A.; Nagatomo, Y.; Kitamura, M.; Nakano, S.; Takei, M.; Mizuno, A.; et al. Temporal Trends in Heart Failure Management and Outcomes: Insights from a Japanese Multicenter Registry of Tertiary Care Centers. J. Am. Heart Assoc. 2023, 12, e031179. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Li, Z.; Li, X.; Yan, Y.; Liu, J.; Wang, J.; Guan, J.; Xin, A.; Zhang, F.; Ouyang, W.; et al. Global trends in heart failure from 1990 to 2019: An age-period-cohort analysis from the Global Burden of Disease study. ESC Heart Fail. 2024, 11, 3264–3278. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, K.; Tanabe, N.; Tanaka, K.; Ozeki, K.; Miyasaka, A.; Inazuki, T.; Abe, M.; Katagiri, H.; Kobayashi, R.; Kurashima, Y.; et al. Twelve-year trends of hospitalizations and survival of acute decompensated heart failure: Data from a regional tertiary center. J. Cardiol. 2025, 86, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Buja, A.; Rivera, M.; Soattin, M.; Corti, M.C.; Avossa, F.; Schievano, E.; Rigon, S.; Baldo, V.; Boccuzzo, G.; Damiani, G.; et al. Impactibility Model for Population Health Management in High-Cost Elderly Heart Failure Patients: A Capture Method Using the ACG System. Popul. Health Manag. 2019, 22, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Yao, H.; Jiang, X.; Bian, S.; Zhou, J.; Sun, X.; Hu, G.; Sun, L.; Xie, G.; He, K. Construction of a Non-Mutually Exclusive Decision Tree for Medication Recommendation of Chronic Heart Failure. Front. Pharmacol. 2022, 12, 758573. [Google Scholar] [CrossRef] [PubMed]
- R Foundation. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://www.R-project.org/ (accessed on 10 January 2024).
- Hahsler, M.; Grün, B.; Hornik, K. arules—A Computational Environment for Mining Association Rules and Frequent Item Sets. J. Stat. Softw. 2005, 14, 1–25. [Google Scholar] [CrossRef]
- Clark, K.A.A.; Reinhardt, S.W.; Chouairi, F.; Miller, P.E.; Kay, B.; Fuery, M.; Guha, A.; Ahmad, T.; Desai, N.R. Trends in Heart Failure Hospitalizations in the US from 2008 to 2018. J. Card. Fail. 2022, 28, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Gracia Gutiérrez, A.; Moreno-Juste, A.; Laguna-Berna, C.; Santos-Mejías, A.; Poblador-Plou, B.; Gimeno-Miguel, A.; Ruiz Laiglesia, F.J. Multimorbidity in Incident Heart Failure: Characterisation Impact on 1-Year Outcomes. J. Clin. Med. 2024, 13, 3979. [Google Scholar] [CrossRef]
- Abassi, N.K.; Nouhravesh, N.; Elmegaard, M.; Austreim, M.; Zahir, D.; Garred, C.H.; Butt, J.H.; Andersen, C.F.; Strange, J.E.; Sindet-Pedersen, C.; et al. Temporal Trends in Mortality and Hospitalization Risk in Patients with Heart Failure According to the Hospital Frailty Risk Score. J. Am. Heart Assoc. 2025, 14, e037973. [Google Scholar] [CrossRef]
- Caughey, G.E.; Inacio, M.C.; Bell, J.S.; Vitry, A.I.; Shakib, S. Inclusion of Older People Reflective of Real-World Clinical Practice in Cardiovascular Drug Trials. J. Am. Heart Assoc. 2020, 9, e016936. [Google Scholar] [CrossRef] [PubMed]
- Tomasoni, D.; Vitale, C.; Guidetti, F.; Benson, L.; Braunschweig, F.; Dahlström, U.; Melin, M.; Rosano, G.M.C.; Lund, L.H.; Metra, M.; et al. The role of multimorbidity in patients with heart failure across the left ventricular ejection fraction spectrum: Data from the Swedish Heart Failure Registry. Eur. J. Heart Fail. 2024, 26, 854–868. [Google Scholar] [CrossRef]
- Fuentes Artiles, R.; Meçani, R.; Muka, T.; Hunziker, L.; Capék, L. Investigation of left ventricular ejection fraction in a Swiss heart failure population: Insights into mortality and sex differences. ESC Heart Fail. 2024, 12, 1630–1639. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. Esperanza de Vidaen la Comunidad Autónoma de Galicia. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=27154#_tabs-grafico (accessed on 18 December 2024).
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Motiejunaite, J.; Akiyama, E.; Cohen-Solal, A.; Maggioni, A.P.; Mueller, C.; Choi, D.J.; Kavoliūnienė, A.; Čelutkienė, J.; Parenica, J.; Lassus, J.; et al. The association of long-term outcome and biological sex in patients with acute heart failure from different geographic regions. Eur. Heart J. 2020, 41, 1357–1364. [Google Scholar] [CrossRef]
- Blumer, V.; Greene, S.J.; Wu, A.; Butler, J.; Ezekowitz, J.A.; Lindenfeld, J.; Alhanti, B.; Hernandez, A.F.; O’Connor, C.M.; Mentz, R.J. Sex differences in clinical course patient-reported outcomes among patients hospitalized for heart failure. J. Am. Coll. Cardiol. HF 2021, 9, 336–345. [Google Scholar] [CrossRef]
- Meyer, S.; Teerlink, J.R.; Metra, M.; Ponikowski, P.; Cotter, G.; Davison, B.A.; Felker, G.M.; Filippatos, G.; Greenberg, B.H.; Hua, T.A.; et al. Sex differences in early dyspnea relief between men and women hospitalized for acute heart failure: Insights from the RELAX-AHF study. Clin. Res. Cardiol. 2017, 106, 280. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2220. [Google Scholar]
- Göbel, S.; Hobohm, L.; Ostad, M.A.; Lavie, C.J.; Gori, T.; Münzel, T.; Wenzel, P.; Keller, K. Sex-specific differences drive temporal trends and outcomes of patients hospitalized for heart failure in Germany. Prog. Cardiovasc. Dis. 2020, 63, 591–598. [Google Scholar] [CrossRef]
- Kuipers, S.; Biessels, G.J.; Greving, J.P.; Amier, R.P.; de Bresser, J.; Bron, E.E.; van der Flier, W.M.; van der Geest, R.J.; Hooghiemstra, A.M.; van Oostenbrugge, R.J.; et al. Sex and Cardiovascular Function in Relation to Vascular Brain Injury in Patients with Cognitive Complaints. J. Alzheimers Dis. 2021, 84, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Appunni, S.; Zhang, Y.; Khosla, A.A.; Rubens, M.; Giri, A.R.; Saxena, A.; Ramamoorthy, V.; Doke, M.; McGranaghan, P.; Chaparro, S.; et al. Sex disparities in outcomes among hospitalizations for heart failure. Sci. Rep. 2024, 14, 27054. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Fernández, A.; Anguita-Sánchez, M.; Bonilla-Palomas, J.L.; Anguita-Gámez, M.; García, M.; Bernal, J.L.; Prado, N.D.; Fernández-Pérez, C.; Pérez-Villacastin, J.; Gómez-Doblas, J.J.; et al. Characteristics and in-hospital mortality of elderly patients with heart failure in Spanish hospitals. J. Geriatr. Cardiol. 2023, 20, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Munir, M.B.; Sharbaugh, M.S.; Thoma, F.W.; Nisar, M.U.; Kamran, A.S.; Althouse, A.D.; Saba, S. Trends in hospitalization for congestive heart failure, 1996–2009. Clin. Cardiol. 2017, 40, 109–119. [Google Scholar] [CrossRef]
- Marcus, G.; Najjar, M.; Monayer, A.; Orbach, A.; Maymon, S.L.; Kalmanovich, E.; Moravsky, G.; Grupper, A.; Fuchs, S.; Minha, S. Temporal trends in acute decompensated heart failure outcomes: A single-center 11-year retrospective analysis. Int. J. Cardiol. Cardiovasc. Risk Prev. 2024, 22, 200306. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, R.A.; Rockenschaub, P.; Neuen, B.L.; Walter, I.J.; Conrad, N.; Mizani, M.A.; Bolton, T.; Lawson, C.A.; Tomlinson, C.; Logothetis, S.B.; et al. Contemporary epidemiology of hospitalised heart failure with reduced versus preserved ejection fraction in England: A retrospective, cohort study of whole-population electronic health records. Lancet Public Health 2024, 9, e871–e885. [Google Scholar] [CrossRef] [PubMed]
- Marenzi, G.; Cosentino, N.; Imparato, L.; Trombara, F.; Leoni, O.; Bortolan, F.; Franchi, M.; Rurali, E.; Poggio, P.; Campodonico, J.; et al. Temporal trends (2003–2018) of in-hospital and 30-day mortality in patients hospitalized with acute heart failure. Int. J. Cardiol. 2025, 419, 132693. [Google Scholar] [CrossRef] [PubMed]
- Ran, J.; Zhou, P.; Wang, J.; Zhao, X.; Huang, Y.; Zhou, Q.; Zhai, M.; Zhang, Y. Global, regional, and national burden of heart failure and its underlying causes, 1990–2021: Results from the global burden of disease study 2021. Biomark Res. 2025, 13, 16. [Google Scholar] [CrossRef] [PubMed]
| Period 2000–2004 | Period 2005–2009 | Period 2010–2014 | Period 2015–2019 | Period 2020–2022 | p | |
|---|---|---|---|---|---|---|
| No. of cases | 7059 | 4697 | 3674 | 3238 | 1059 | |
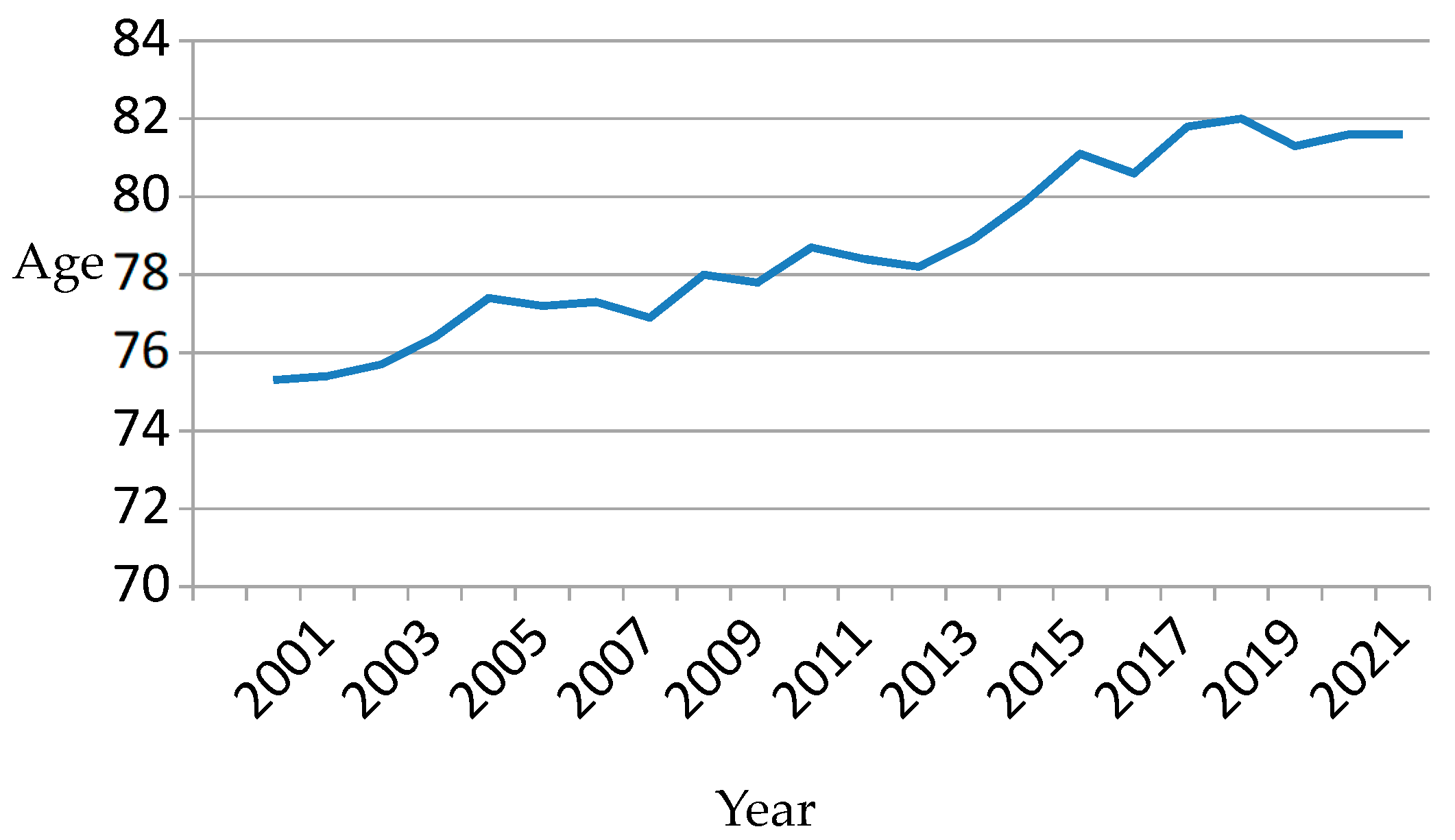
| Age (years) | 75.9 ± 11.2 | 77.4 ± 10.9 | 78.9 ± 11.4 | 81.4 ± 11.7 | 81.6 ± 11.5 | 0.0001 |
| Gender (male) | 51.7 | 49.5 | 49.1 | 45.7 | 48.6 | 0.0001 |
| Acute diseases | 1.1 ± 1.4 | 1.4 ± 1.6 | 3.5 ± 3.8 | 3 ± 3 | 2.7 ± 2.5 | 0.0001 |
| Chronic diseases | 3.6 ± 1.9 | 4.1 ± 2.1 | 7.7 ± 3.5 | 6.4 ± 3.5 | 6.5 ± 2.6 | 0.0001 |
| Readmissions | 4.8 ± 4.2 | 4 ± 3 | 3.2 ± 2.4 | 2.4 ± 1.7 | 1.5 ± 0.9 | 0.0001 |
| Follow-up time (days) | 2845.2 (2248.1) | 2559.7 (1773.4) | 1707.8 (1221.2) | 881.1 (718.9) | 291.9 (255.8) | 0.0001 |
| Period 2000–2004 | Period 2005–2009 | Period 2010–2014 | Period 2015–2019 | Period 2020–2022 | |
|---|---|---|---|---|---|
| No. of cases | 7059 | 4697 | 3674 | 3238 | 1059 |
| No. of transactions | 30,344 | 17,829 | 11,198 | 7540 | 1539 |
| No. of diagnoses | 252 | 251 | 245 | 238 | 207 |
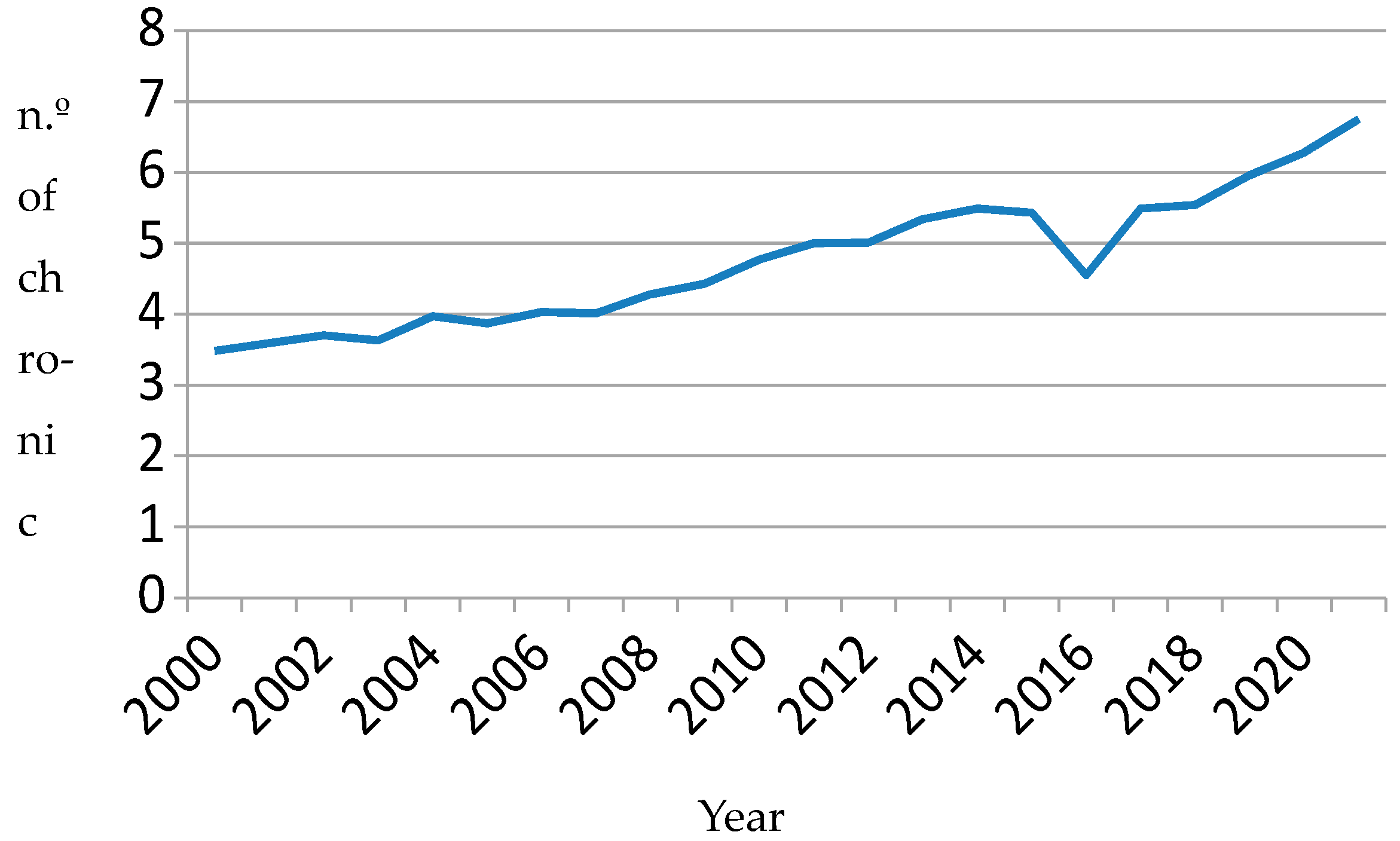
| Diagnoses per patient (median) | 3 | 4 | 5 | 5 | 7 |
| Itemset | 218 | 354 | 1134 | 1315 | 4241 |
| Majority No. items/itemset (%) | 2 Items (51.4%) | 2 Items (52.8%) | 3 Items (37.1%) | 3 Items (40.3%) | 4 Items (34.2%) |
| Items (median) | 2 | 2 | 3 | 3 | 3 |
| Items (mean) | 1.75 | 1.95 | 2.77 | 2.82 | 3.44 |
| Rules of Association 2000–2004 | Support | Confidence | Lift | Number | ||
|---|---|---|---|---|---|---|
| {Cardiomyopathy} | => | {Congestive heart failure} | 0.0191 | 0.7208 | 1.5891 | 581 |
| {Pulmonary hypertension} | => | {Congestive heart failure} | 0.025 | 0.5958 | 1.3133 | 759 |
| {Valvular heart disease, Arrhythmias} | => | {Congestive heart failure} | 0.0121 | 0.5919 | 1.3049 | 367 |
| {Arrhythmias, Miscellaneous} | => | {Congestive heart failure} | 0.0268 | 0.5824 | 1.2838 | 813 |
| {Valvular heart disease} | => | {Congestive heart failure} | 0.0431 | 0.5761 | 1.2701 | 1309 |
| {Diabetes mellitus 2, Arrhythmias} | => | {Congestive heart failure} | 0.0107 | 0.5755 | 1.2686 | 324 |
| {Other infections, Arrhythmias} | => | {Congestive heart failure} | 0.0128 | 0.5742 | 1.2657 | 387 |
| {Acute kidney failure} | => | {Congestive heart failure} | 0.0393 | 0.5741 | 1.2656 | 1193 |
| {Valvular heart disease, Miscellaneous} | => | {Congestive heart failure} | 0.0112 | 0.5736 | 1.2645 | 339 |
| {Arrhythmias, chronic obstructive pulmonary disease} | => | {Congestive heart failure} | 0.0113 | 0.5736 | 1.2644 | 343 |
| Rules of association 2005–2009 | Support | Confidence | Lift | Number | ||
| {Chronic kidney disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0102 | 0.7583 | 1.5523 | 182 |
| {Valvular heart disease, Pulmonary hypertension} | => | {Congestive heart failure} | 0.0121 | 0.7465 | 1.5281 | 215 |
| {Arrhythmias, Acute kidney failure} | => | {Congestive heart failure} | 0.0126 | 0.7329 | 1.5002 | 225 |
| {Pleural effusion} | => | {Congestive heart failure} | 0.0184 | 0.7321 | 1.4987 | 328 |
| {Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0121 | 0.7264 | 1.4868 | 215 |
| {Acute respiratory failure, Acute renal failure} | => | {Congestive heart failure} | 0.0116 | 0.7263 | 1.4867 | 207 |
| {Chronic kidney disease, Arrhythmias} | => | {Congestive heart failure} | 0.013 | 0.7108 | 1.4549 | 231 |
| {Cardiomyopathy} | => | {Congestive heart failure} | 0.0175 | 0.7107 | 1.4548 | 312 |
| {Anemia, Arrhythmias} | => | {Congestive heart failure} | 0.0121 | 0.7036 | 1.4402 | 216 |
| {Pulmonary hypertension} | => | {Congestive heart failure} | 0.0335 | 0.6945 | 1.4217 | 598 |
| Rules of association 2010–2014 | Support | Confidence | Lift | Number | ||
| {Hypertension, Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0112 | 0.9058 | 1.609 | 125 |
| {Hypertension, Arrhythmias, Acute respiratory failure, Atrial fibrillation} | => | {Congestive heart failure} | 0.0102 | 0.8976 | 1.5945 | 114 |
| {Hypertension, Acute respiratory failure, Atrial fibrillation} | => | {Congestive heart failure} | 0.0104 | 0.8931 | 1.5865 | 117 |
| {Hypertension, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.014 | 0.8771 | 1.558 | 157 |
| {Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0176 | 0.8717 | 1.5484 | 197 |
| {Cardiomyopathies, Miscellaneous} | => | {Congestive heart failure} | 0.011 | 0.8662 | 1.5387 | 123 |
| {Acute respiratory failure, Atrial fibrillation, Miscellaneous} | => | {Congestive heart failure} | 0.0138 | 0.8652 | 1.5368 | 154 |
| {Arrhythmias, Acute respiratory failure, Atrial fibrillation, Miscellaneous} | => | {Congestive heart failure} | 0.013 | 0.8639 | 1.5346 | 146 |
| {Arrythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0278 | 0.8567 | 1.5219 | 311 |
| {Valvular heart disease, Acute respiratory failure} | => | {Congestive heart failure} | 0.0127 | 0.8503 | 1.5104 | 142 |
| Rules of association 2015–2019 | Support | Confidence | Lift | Number | ||
| {Arrhythmias, Acute respiratory failure, Acute renal failure} | => | {Congestive heart failure} | 0.0123 | 0.949 | 1.44 | 93 |
| {Chronic kidney disease, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0117 | 0.9263 | 1.4056 | 88 |
| {Arrythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0459 | 0.9081 | 1.378 | 346 |
| {Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0275 | 0.9039 | 1.3716 | 207 |
| {Hypertension, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0218 | 0.9011 | 1.3673 | 164 |
| {Valvular heart disease, Cardiomyopathies} | => | {Congestive heart failure} | 0.0102 | 0.8953 | 1.3586 | 77 |
| {Other infections, Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0164 | 0.8921 | 1.3537 | 124 |
| {Other infections, Arrhythmias, Acute respiratory failure} | => | {Congestive heart failure} | 0.0252 | 0.892 | 1.3536 | 190 |
| {Hypertension, Arrhythmias, Acute respiratory failure, Miscellaneous} | => | {Congestive heart failure} | 0.0147 | 0.888 | 1.3475 | 111 |
| {Chronic kidney disease, Acute respiratory failure, Acute renal failure} | => | {Congestive heart failure} | 0.0156 | 0.8872 | 1.3463 | 118 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seoane-Pillado, T.; Suárez-Gil, R.; Pértega-Díaz, S.; Piñeiro-Fernández, J.C.; Rodriguez-Ameijeiras, E.; Casariego-Vales, E. Temporal Evolution of the Profile of Patients Hospitalized with Heart Failure (2000–2022). Clin. Pract. 2025, 15, 187. https://doi.org/10.3390/clinpract15100187
Seoane-Pillado T, Suárez-Gil R, Pértega-Díaz S, Piñeiro-Fernández JC, Rodriguez-Ameijeiras E, Casariego-Vales E. Temporal Evolution of the Profile of Patients Hospitalized with Heart Failure (2000–2022). Clinics and Practice. 2025; 15(10):187. https://doi.org/10.3390/clinpract15100187
Chicago/Turabian StyleSeoane-Pillado, Teresa, Roi Suárez-Gil, Sonia Pértega-Díaz, Juan Carlos Piñeiro-Fernández, Elena Rodriguez-Ameijeiras, and Emilio Casariego-Vales. 2025. "Temporal Evolution of the Profile of Patients Hospitalized with Heart Failure (2000–2022)" Clinics and Practice 15, no. 10: 187. https://doi.org/10.3390/clinpract15100187
APA StyleSeoane-Pillado, T., Suárez-Gil, R., Pértega-Díaz, S., Piñeiro-Fernández, J. C., Rodriguez-Ameijeiras, E., & Casariego-Vales, E. (2025). Temporal Evolution of the Profile of Patients Hospitalized with Heart Failure (2000–2022). Clinics and Practice, 15(10), 187. https://doi.org/10.3390/clinpract15100187






