Asthma Hospitalizations in Children Before and After COVID-19: Insights from Northern Colombia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area and General Description of the Population
2.2. Statistical Analysis
3. Results
3.1. Observed Patterns of Asthma Severity in Individual Groups Before and After the Pandemic
3.1.1. Binary Logistic Regression Model Analysis—Pre-Pandemic, Subgroup 1
3.1.2. Binary Logistic Regression Model Analysis Pandemic, Subgroup 2
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| °C | Celsius |
| R2 | Coefficient of determination |
| COVID-19 | Coronavirus Disease 2019 |
| MDLB | Binary Logistic Regression Model |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome due to Coronavirus 2 |
| VSR | Respiratory Syncytial Virus |
References
- Aydin, M. Maintenance of Medical Care of Children and Adolescents with Asthma during the SARS-CoV-2/COVID-19 Pandemic: An Opinion. Int. J. Public Health 2022, 67, 1604849. [Google Scholar] [CrossRef]
- Altman, M.C.; Kattan, M.; O’Connor, G.T.; Murphy, R.C.; Whalen, E.; LeBeau, P.; Calatroni, A.; Gill, M.A.; Gruchalla, R.S.; Liu, A.H.; et al. Associations between Outdoor Air Pollutants and Non-Viral Asthma Exacerbations and Airway Inflammatory Responses in Children and Adolescents Living in Urban Areas in the USA: A Retrospective Secondary Analysis. Lancet Planet. Health 2023, 7, e33–e44. [Google Scholar] [CrossRef] [PubMed]
- Herrera, A.M.; Brand, P.; Cavada, G.; Koppmann, A.; Rivas, M.; Mackenney, J.; Sepúlveda, H.; Wevar, M.; Cruzat, L.; Soto, S.; et al. Hospitalizations for Asthma Exacerbation in Chilean Children: A Multicenter Observational Study. Allergol. Immunopathol. 2018, 46, 533–538. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Farzan, N.; Vijverberg, S.J.; Andiappan, A.K.; Arianto, L.; Berce, V.; Blanca-López, N.; Bisgaard, H.; Bønnelykke, K.; Burchard, E.G.; Campo, P.; et al. Rationale and Design of the Multiethnic Pharmacogenomics in Childhood Asthma Consortium. Pharmacogenomics 2017, 18, 931–943. [Google Scholar] [CrossRef]
- Liang, Y.; Li, Q.; Wang, M.; Zhou, K.; Yan, X.; Lu, J.; Li, Q.; Yu, H.; Xu, C.; Liu, X.; et al. Differences in the Prevalence of Allergy and Asthma among US Children and Adolescents during and before the COVID-19 Pandemic. BMC Public Health 2024, 24, 2124. [Google Scholar] [CrossRef]
- Bergmann, K.C.; Brehler, R.; Endler, C.; Höflich, C.; Kespohl, S.; Plaza, M.; Raulf, M.; Standl, M.; Thamm, R.; Traidl-Hoffmann, C.; et al. Impact of Climate Change on Allergic Diseases in Germany. J. Health Monit. 2023, 8 (Suppl. S4), 76. [Google Scholar] [CrossRef]
- García, E.; Rojas, M.X.; Ardila, M.C.; Rondón, M.A.; Peñaranda, A.; Barragán, A.M.; Pérez, A.; Moreno, S.; Sotaquirá, L.; Caraballo, L.; et al. Factors Associated with Asthma Symptoms in Colombian Subpopulations Aged 1 to 17 and 18 to 59: Secondary Analysis of the Study “Prevalence of Asthma and Other Allergic Diseases in Colombia 2009–2010”. Allergol. Immunopathol. 2025, 53, 69–85. [Google Scholar] [CrossRef]
- Moreno-López, S.; Pérez-Herrera, L.C.; Peñaranda, D.; Hernández, D.C.; García, E.; Peñaranda, A. Prevalence and Associated Factors of Allergic Diseases in School Children and Adolescents Aged 6–7 and 13–14 Years from Two Rural Areas in Colombia. Allergol. Immunopathol. 2021, 49, 153–161. [Google Scholar] [CrossRef]
- Rodríguez-Villamizar, L.A.; Rojas-Roa, N.Y.; Blanco-Becerra, L.C.; Herrera-Galindo, V.M.; Fernández-Niño, J.A. Short-Term Effects of Air Pollution on Respiratory and Circulatory Morbidity in Colombia 2011–2014: A Multi-City, Time-Series Analysis. Int. J. Environ. Res. Public Health 2018, 15, 1610. [Google Scholar] [CrossRef]
- Bolaño-Díaz, S.; Camargo-Caicedo, Y.; Tovar-Bernal, F.; Bolaño-Ortiz, T.R. The effect of forest fire events on air quality: A case study of northern Colombia. Fire 2022, 5, 191. [Google Scholar] [CrossRef]
- Jamali, A.A.; Langah, A.; Memon, N.A.; Siyal, M.A.; Khushik, K.; Siyal, A.A. Prevalence and Management of Pediatric Asthma in Urban Versus Rural Settings. Med. Forum 2024, 35, 76–80. Available online: https://medicalforummonthly.com/index.php/mfm/article/view/5093 (accessed on 16 August 2025).
- Arregocés, H.A.; Gómez, D.; Castellanos, M.L. Annual and monthly precipitation trends: An indicator of climate change in the Caribbean region of Colombia. Case Stud. Chem. Environ. Eng. 2024, 10, 100834. [Google Scholar] [CrossRef]
- Domingo, K.N.; Gabaldon, K.L.; Hussari, M.N.; Yap, J.M.; Valmadrid, L.C.; Robinson, K.; Leibel, S. Impact of Climate Change on Paediatric Respiratory Health: Pollutants and Aeroallergens. Eur. Respir. Rev. 2024, 33, 230249. [Google Scholar] [CrossRef]
- Salud Total EPS-S. Perfil Epidemiológico Distrito Barranquilla: Caracterización Poblacional Año 2023; Versión 1.0; Salud Total EPS-S: Barranquilla, Colombia, 2024; Available online: https://saludtotal.com.co/wp-content/uploads/2024/06/PERFIL-EPIDEMIOLOGICO_BARRANQUILLA_2023.pdf (accessed on 23 September 2025).
- Ministry of Health and Social Protection. Resolution 385 of 2020, “By Which the Health Emergency is Declared due to the Coronavirus COVID-19 and Measures are Adopted to Address the Virus.”; Ministry of Health and Social Protection: Bogotá, Colombia, 2020. Available online: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=119957 (accessed on 25 September 2025).
- Ministerio de Salud y Protección Social (Colombia). Resolución 666 de 2022: Por la cual se Prorroga la Emergencia Sanitaria por el Coronavirus COVID-19 Declarada Mediante Re-Solución 385 de 2020, Hasta el 30 de Junio de 2022; Diario Oficial de Colombia: Bogotá, Colombia, 2022. Available online: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=186026 (accessed on 23 September 2025).
- Ministry of Health and Social Protection of Colombia. Resolution 1738 of 2021, “By Which the National COVID-19 Vaccination Plan Is Modified and Children Aged 3 to 11 Years are Included.”; MinSalud: Bogotá, Colombia, 2021. Available online: https://www.minsalud.gov.co (accessed on 18 August 2025).
- Ministry of Health and Social Protection of Colombia. Resolution 1151 of 2021, “By which the National COVID-19 Vaccination Plan Is Modified and Adolescents Aged 12 to 17 Years are Included.”; MinSalud: Bogotá, Colombia, 2021. Available online: https://www.minsalud.gov.co (accessed on 18 August 2025).
- Ministry of Health and Social Protection of Colombia. Resolution 986 of 2023, “By Which Technical and Operational Guidelines for COVID-19 Vaccination are Adopted.”; MinSalud: Bogotá, Colombia, 2023. Available online: https://www.minsalud.gov.co (accessed on 18 August 2025).
- Gray, C.; Collings, M.; Benito, J.; Velasco, R.; Lyttle, M.D.; Roland, D.; Schuh, S.; Shihabuddin, B.; Kwok, M.; Mahajan, P.; et al. Analysis of the asthma scores recommended in guidelines for children presenting to the emergency department: A Pediatric Emergency Research Networks study. Arch. Dis. Child. 2025, 110, 110–428. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group; U.S. Department of Health and Human Services: Bethesda, MD, USA, 2020. Available online: https://www.nhlbi.nih.gov/health-topics/asthma-management-guidelines-2020-updates (accessed on 8 July 2025).
- Liu, S.; Zhi, Y.; Ying, S. COVID-19 and Asthma: Reflection during the Pandemic. Clin. Rev. Allergy Immunol. 2021, 61, 26–33. [Google Scholar] [CrossRef]
- Butt, A.A.; Dargham, S.R.; Loka, S.; Shaik, R.M.; Chemaitelly, H.; Tang, P.; Abu-Raddad, L.J. Coronavirus Disease 2019 Disease Severity in Children Infected with the Omicron Variant. Clin. Infect. Dis. 2022, 75, e361–e367. [Google Scholar] [CrossRef]
- Bhopal, S.S.; Bagaria, J.; Olabi, B.; Bhopal, R. Children and Young People Remain at Low Risk of COVID-19 Mortality. Lancet Child Adolesc. Health 2021, 5, e12–e13. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Silva, C.; Rivero, R.; Douglas, J.; Bouckaert, R.; Villabona-Arenas, C.J.; Atkins, K.E.; Gastelbondo, B.; Calderon, A.; Guzman, C.; Echeverri-De la Hoz, D.; et al. Genomic Epidemiology of SARS-CoV-2 Variants during the First Two Years of the Pandemic in Colombia. Commun. Med. 2023, 3, 97. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Cortes-Ramirez, J.; Gan, T.; Davies, J.M.; Hu, W. Effects of Climate and Environmental Factors on Childhood and Adolescent Asthma: A Systematic Review Based on Spatial and Temporal Analysis Evidence. Sci. Total Environ. 2024, 951, 175863. [Google Scholar] [CrossRef] [PubMed]
- Jartti, T.; Bønnelykke, K.; Elenius, V.; Feleszko, W. Role of Viruses in Asthma. Semin. Immunopathol. 2020, 42, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Moitra, S.; Carsin, A.; Abramson, M.J.; Accordini, S.; Amaral, A.F.S.; Anto, J.; Bono, R.; Ruiz, L.C.; Cerveri, I.; Chatzi, L.; et al. Long-Term Effect of Asthma on the Development of Obesity among Adults: An International Cohort Study. Thorax 2023, 78, 128–135. [Google Scholar] [CrossRef]
- Sharma, V.; Ricketts, H.C.; Steffensen, F.; Goodfellow, A.; Cowan, D.C. Obesity Affects Type 2 Biomarker Levels in Asthma. J. Asthma 2022, 60, 385–392. [Google Scholar] [CrossRef]
- Vassilopoulou, E.; Venter, C.; Roth-Walter, F. Malnutrition and Allergies: Tipping the Immune Balance towards Health. J. Clin. Med. 2024, 13, 4713. [Google Scholar] [CrossRef]
- Lister, N.B.; Baur, L.A.; Felix, J.F.; Hill, A.J.; Marcus, C.; Reinehr, T.; Summerbell, C.; Wabitsch, M. Child and Adolescent Obesity. Nat. Rev. Dis. Primers 2023, 9, 24. [Google Scholar] [CrossRef]
- Pertuz-Guzmán, D.L.; Chams-Chams, L.M.; Valencia-Jiménez, N.N.; Arrieta-Díaz, J.; Luna-Carrascal, J. Comprendiendo la Inseguridad Alimentaria en Familias Rurales: Un Estudio de Caso en Pueblo Nuevo (Córdoba, Colombia). Aten. Primaria 2025, 57, 103109. [Google Scholar] [CrossRef]
- Abdul-Razzak, J.; Ionescu, M.; Diaconu, R.; Popescu, A.D.; Niculescu, E.C.; Petrescu, I.O.; Dima, R. Impact of the COVID-19 Pandemic on Lung Function and Treatment Decisions in Children with Asthma: A Retrospective Study. J. Clin. Med. 2025, 14, 3289. [Google Scholar] [CrossRef]
- Rodríguez-Martínez, C.E.; Sossa-Briceño, M.P.; Castro-Rodriguez, J.A. Factors Predicting Persistence of Early Wheezing through Childhood and Adolescence: A Systematic Review of the Literature. J. Asthma Allergy 2017, 10, 83–98. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.Q.; Özuygur Ermis, S.S.; Rådinger, M.; Bossios, A.; Kankaanranta, H.; Nwaru, B. Sex Disparities in Asthma Development and Clinical Outcomes: Implications for Treatment Strategies. J. Asthma Allergy 2022, 15, 231–247. [Google Scholar] [CrossRef] [PubMed]
- Willis, Z.I.; Oliveira, C.R.; Abzug, M.J.; Anosike, B.I.; Ardura, M.I.; Bio, L.L.; Boguniewicz, J.; Chiotos, K.; Downes, K.; Grapentine, S.P.; et al. Guidance for Prevention and Management of COVID-19 in Children and Adolescents: A Consensus Statement from the Pediatric Infectious Diseases Society Pediatric COVID-19 Therapies Taskforce. J. Pediatric Infect. Dis. Soc. 2024, 13, 159–185. [Google Scholar] [CrossRef]
- Manti, S.; Leotta, M.; D’Amico, F.; Foti Randazzese, S.; Parisi, G.F.; Leonardi, S. Severe Asthma and Active SARS-CoV-2 Infection: Insights into Biologics. Biomedicines 2025, 13, 674. [Google Scholar] [CrossRef]
- Bleecker, E.R.; Al-Ahmad, M.; Bjermer, L.; Caminati, M.; Canonica, G.W.; Kaplan, A.; Papadopoulos, N.G.; Roche, N.; Ryan, D.; Tohda, Y.; et al. Systemic Corticosteroids in Asthma: A Call to Action from World Allergy Organization and Respiratory Effectiveness Group. World Allergy Organ. J. 2022, 15, 100726. [Google Scholar] [CrossRef]
- Martínez-González, M.B.; Milanes, C.B.; Moreno-Gómez, J.; Padilla-Llano, S.; Vásquez, A.; Lavell, A.; Saltarín-Jiménez, A.; Suárez, A. Understanding Social and Environmental Hazards in Urban Areas: An Analysis from Barranquilla, Colombia. Soc. Sci. 2021, 10, 411. [Google Scholar] [CrossRef]
- Khreis, H.; Kelly, C.; Tate, J.; Parslow, R.; Lucas, K.; Nieuwenhuijsen, M.J. Exposure to traffic-related air pollution and risk of development of childhood asthma: A systematic review and meta-analysis. Environ. Int. 2017, 100, 1–31. [Google Scholar] [CrossRef]
- Kabir, E.; Taneepanichskul, N.; Chuang, H.C.; Wongsanit, J.; Muanwongyathi, P.; Lim, A.; Guo, Y.L. Exposure to ambient PM2.5 and childhood asthma prevalence: A global update with regional emphasis. Int. J. Environ. Res. Public Health 2023, 20, 4217. [Google Scholar] [CrossRef]
- Tavakol, M.; Gharagozlou, S.; Abbasi, M.; Zamani, Z.; Gharagozlou, M. Pediatric asthma and COVID-19 vaccination: Unveiling patterns of hesitancy and acceptance. Therap. Adv. Vaccines Immunother. 2024, 12, 25151355241297874. [Google Scholar] [CrossRef]
- Valent, F.; Gongolo, F.; Licata, A.; Licata, M.; Russo, F.; Zanier, L. Childhood vaccination and risk of asthma: A population-based study. Vaccines 2023, 11, 948. [Google Scholar] [CrossRef]
- Piccirillo, G.; Ciancarella, P.; Conflitti, G.; Iafigliola, M.; Spinozzi, F. Safety of COVID-19 vaccination in children with allergic diseases and asthma: A multicenter prospective cohort study. Vaccines 2023, 11, 772. [Google Scholar] [CrossRef]
- Pham, H.; Duckett, K.; Nelson, R.; Tran, H.; Jayaram, L. Impact of influenza and pneumococcal vaccination on asthma control in children: A systematic review. Vaccines 2022, 10, 1374. [Google Scholar] [CrossRef]
- Fasola, S.; Ferrante, G.; Cilluffo, G.; Malizia, V.; Alfano, P.; Montalbano, L.; Cuttitta, G.; La Grutta, S. Asthma Comorbidities: Frequency, Risk Factors, and Associated Burden in Children and Adolescents. Children 2022, 9, 1001. [Google Scholar] [CrossRef]
- Di Filippo, P.; Lizzi, M.; Raso, M.; Di Pillo, S.; Chiarelli, F.; Attanasi, M. The Role of Breastfeeding on Respiratory Outcomes Later in Childhood. Front. Pediatr. 2022, 10, 829414. [Google Scholar] [CrossRef] [PubMed]
- Wrenger, J.; Martin, D.D.; Jenetzky, E. Infants’ Immunisations, Their Timing and the Risk of Allergic Diseases (INITIAL): An Observational Prospective Cohort Study Protocol. BMJ Open 2023, 13, e072722. [Google Scholar] [CrossRef] [PubMed]
| Period | Geographic Distribution/Total Patients | Hospitalization n (%) | Hospitalization n (%) | X2 |
|---|---|---|---|---|
| Pre-pandemic | Yes | No | ||
| Barranquilla | 23 (26.43) | 34 (39.08) | ||
| Metropolitan area | 7(8.04) | 23 (26.43) | ||
| Total patients = 87 | ||||
| Emergency COVID-19 | Yes | No | ||
| Barranquilla | 67 (38.28) | 37 (21.14) | * 0.008 | |
| Metropolitan area | 58 (33.14) | 13 (7.42) | ||
| Total patients = 175 | ||||
| Emergency post-COVID | Yes | No | ||
| Barranquilla | 17 (37.77) | 17 (37.77) | ||
| Metropolitan area | 10 (22.22) | 1 (2.22) | ||
| Total patients = 45 | ||||
| Period | Variable | Female n (%) | Male n (%) | X2 |
| Pre-pandemic | 32 (36.78) | 55 (63.21) | ||
| Emergency COVID-19 | Gender | 79 (45.14) | 96 (54.85) | * 0.003 |
| Emergency post-COVID | 11 (24.44) | 34 (75.55) | ||
| Period | Variable | Preschool children 3–6 years n (%) | Children and adolescents 7–17 years n (%) | X2 |
| Pre-pandemic | 77 (88.50) | 10 (11.49) | ||
| Emergency COVID-19 | Population/Age | 157 (89.71) | 18 (10.28) | 0.091 |
| Emergency post-COVID | 35 (77.77) | 10 (22.22) |
| Breastfed Infants | Use of Corticosteroids | COVID-19 Vaccine | Exposure to Contaminants | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Period | Preschool Children 3–6 Years n (%) | Children and Adolescents 7–17 Years n (%) | X2 | Yes n (%) | No n (%) | X2 | Yes n (%) | No n (%) | X2 | Yes n (%) | No n (%) | X2 | Total Population n (%) |
| Pre-pandemic | 34 (39.08) | 53 (60.91) | 30 (34.48) | 57 (65.51) | 0 (0) | 87 (100) | 42 (48.27) | 45 (51.72) | 87 | ||||
| Emergency COVID-19 | 67 (38.28) | 108 (61.71) | 0.078 | 88 (50.28) | 87 (49.71) | * 0.009 | 47 (26.85) | 128 (73.14) | * 0.000 | 52 (29.71) | 123 (70.28) | * 0.010 | 175 |
| Emergency post-COVID | 25 (55.55) | 20 (44.44) | 27 (60) | 18 (40) | 20 (44.44) | 25 (55.55) | 14 (31.11) | 31 (68.88) | 45 | ||||
| Period | Nutritional Status | Female n (%) | Male n (%) | X2 |
|---|---|---|---|---|
| Pre-pandemic | Malnutrition | 0 (0) | 1 (1.14) | |
| Appropriate | 30 (34.82) | 37 (42.52) | ||
| Overweight | 2 (2.29) | 10 (11.49) | * 0.018 | |
| Obesity | 0 (0) | 7 (8.04) | ||
| Emergency COVID-19 | Malnutrition | 3 (1.71) | 4 (2.28) | |
| Appropriate | 65 (37.14) | 70 (40) | ||
| Overweight | 6 (3.42) | 15 (8.57) | 0.303 | |
| Obesity | 7 (4) | 5 (2.85) | ||
| Emergency post-COVID | Malnutrition | 0 (0) | 1(2.22) | |
| Appropriate | 11 (24.4) | 26 (57.77) | ||
| Overweight | 0 (0) | 4 (8.88) | 0.612 | |
| Obesity | 0 (0) | 3 (6.66) | ||
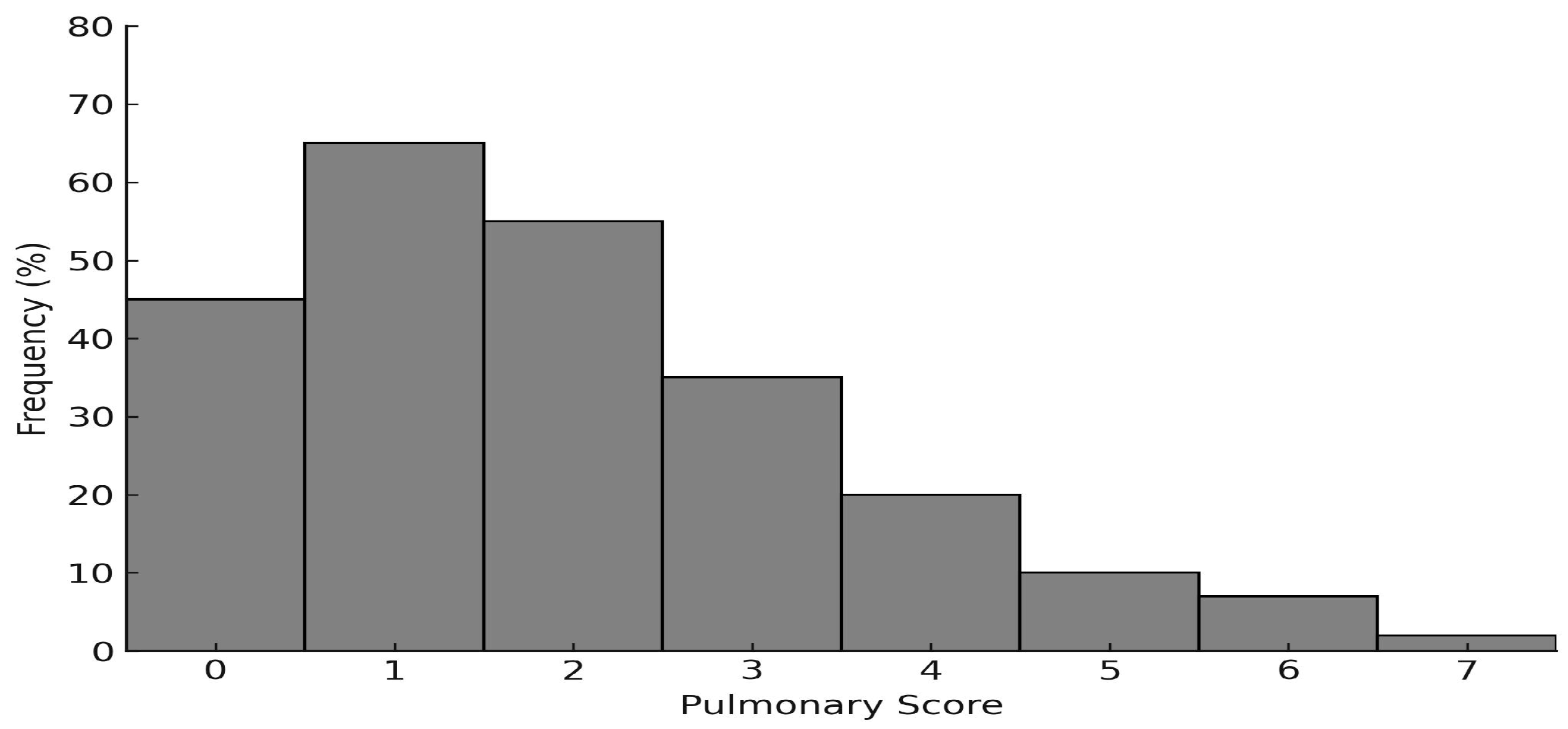
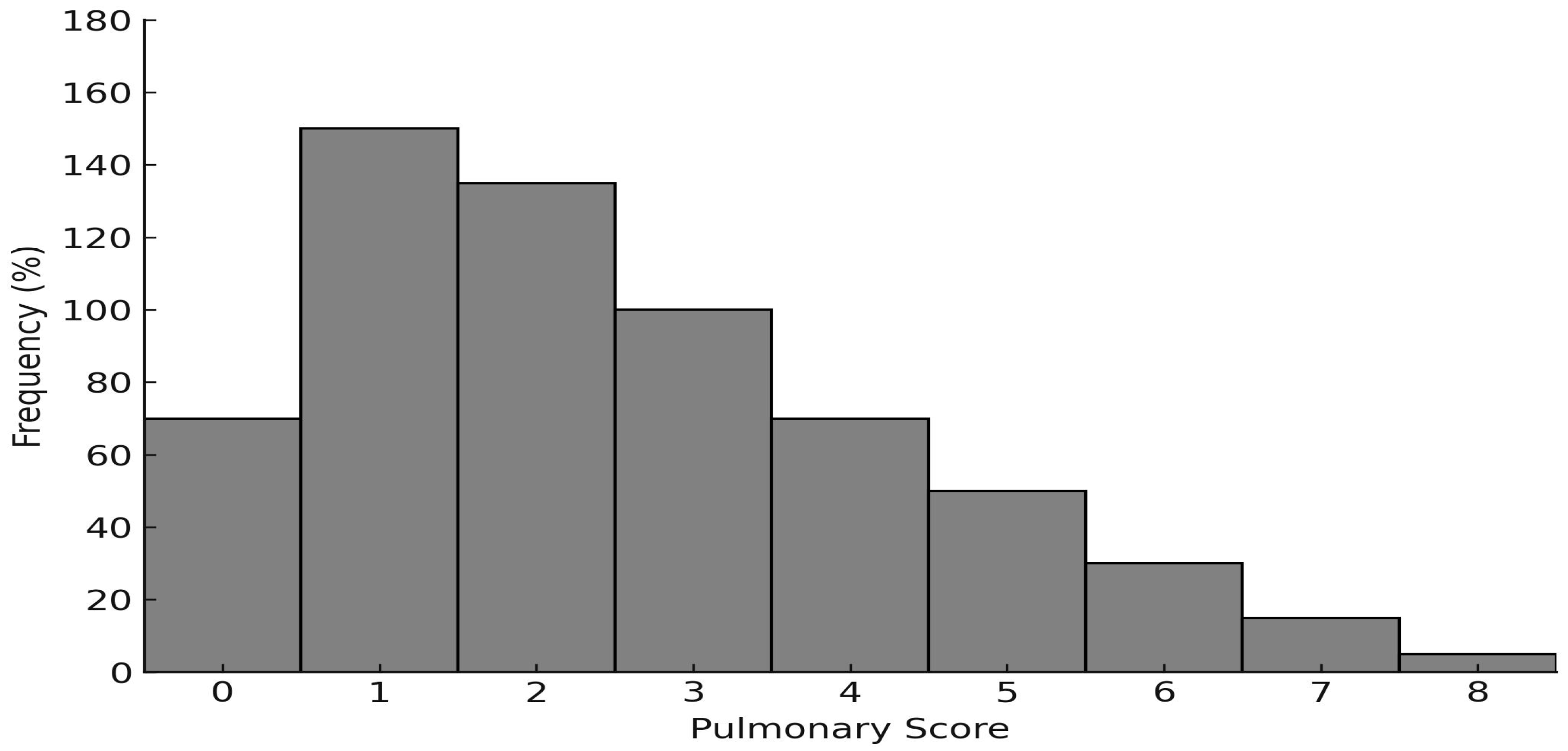
| Period | Pulmonary score | Female n (%) | Male n (%) | X2 |
| Pre-pandemic | Mild (0–3) | 29 (33.33) | 49 (56.32) | |
| Moderate (4–6) | 2 (2.29) | 6 (6.89) | 0.416 | |
| Severe (7–9) | 1 (1.14) | 0 (0) | ||
| Mild (0–3) | 65 (37.14) | 80 (45.71) | ||
| Emergency COVID-19 | Moderate (4–6) | 13(7.42) | 14 (8) | 0.932 |
| Severe (7–9) | 1 (0.57) | 2 (1.14) | ||
| Mild (0–3) | 10 (22.22) | 31 (68.88) | ||
| Emergency post-COVID | Moderate (4–6) | 0 (0) | 3 (6.66) | 0.357 |
| Severe (7–9) | 1 (0.2) | 0 (0) |
| Variable | Pulmonary Score | R2 (BLRM) | p-Value | Log-Likelihood Ratio |
|---|---|---|---|---|
| Breastfeeding | >0.3 | |||
| Weight | Mild | 0.1091 | >0.3 | 0.3887 |
| Hospitalization | Moderate/severe | 0.371 | ||
| Age | >0.3 | |||
| Variable | Pulmonary Score | R2 (BLRM) | p-Value | Log-Likelihood Ratio |
|---|---|---|---|---|
| Breastfeeding | * 0.022 | |||
| Weight | Mild | 0.891 | 0.087 | * 0.0097 |
| Hospitalization | Moderate/severe | * 0.012 | ||
| Age | 0.162 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Árquez-Mendoza, M.; Franco-Valencia, K.; Anaya-Romero, M.; Acevedo-Cerchiaro, M.; Fragozo-Messino, S.; Pertuz-Guzman, D.L.; Luna-Carrascal, J. Asthma Hospitalizations in Children Before and After COVID-19: Insights from Northern Colombia. Clin. Pract. 2025, 15, 184. https://doi.org/10.3390/clinpract15100184
Árquez-Mendoza M, Franco-Valencia K, Anaya-Romero M, Acevedo-Cerchiaro M, Fragozo-Messino S, Pertuz-Guzman DL, Luna-Carrascal J. Asthma Hospitalizations in Children Before and After COVID-19: Insights from Northern Colombia. Clinics and Practice. 2025; 15(10):184. https://doi.org/10.3390/clinpract15100184
Chicago/Turabian StyleÁrquez-Mendoza, Moisés, Karen Franco-Valencia, Marco Anaya-Romero, Maria Acevedo-Cerchiaro, Stacey Fragozo-Messino, Deiby Luz Pertuz-Guzman, and Jaime Luna-Carrascal. 2025. "Asthma Hospitalizations in Children Before and After COVID-19: Insights from Northern Colombia" Clinics and Practice 15, no. 10: 184. https://doi.org/10.3390/clinpract15100184
APA StyleÁrquez-Mendoza, M., Franco-Valencia, K., Anaya-Romero, M., Acevedo-Cerchiaro, M., Fragozo-Messino, S., Pertuz-Guzman, D. L., & Luna-Carrascal, J. (2025). Asthma Hospitalizations in Children Before and After COVID-19: Insights from Northern Colombia. Clinics and Practice, 15(10), 184. https://doi.org/10.3390/clinpract15100184






