Zero-Fluoroscopy Catheter Ablation of Right Appendage Focal Atrial Tachycardia in a Pregnant Woman
Abstract
1. Introduction
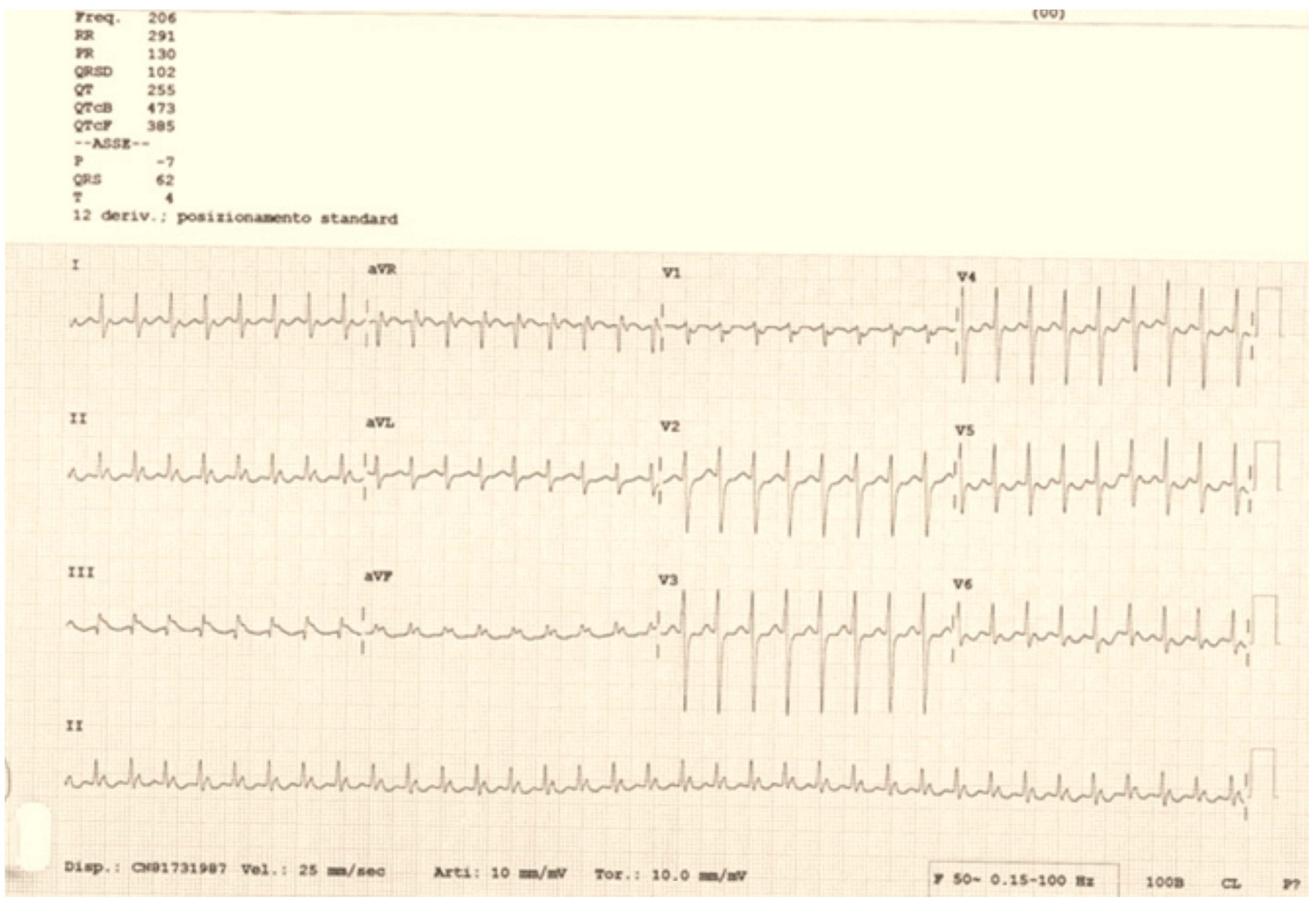
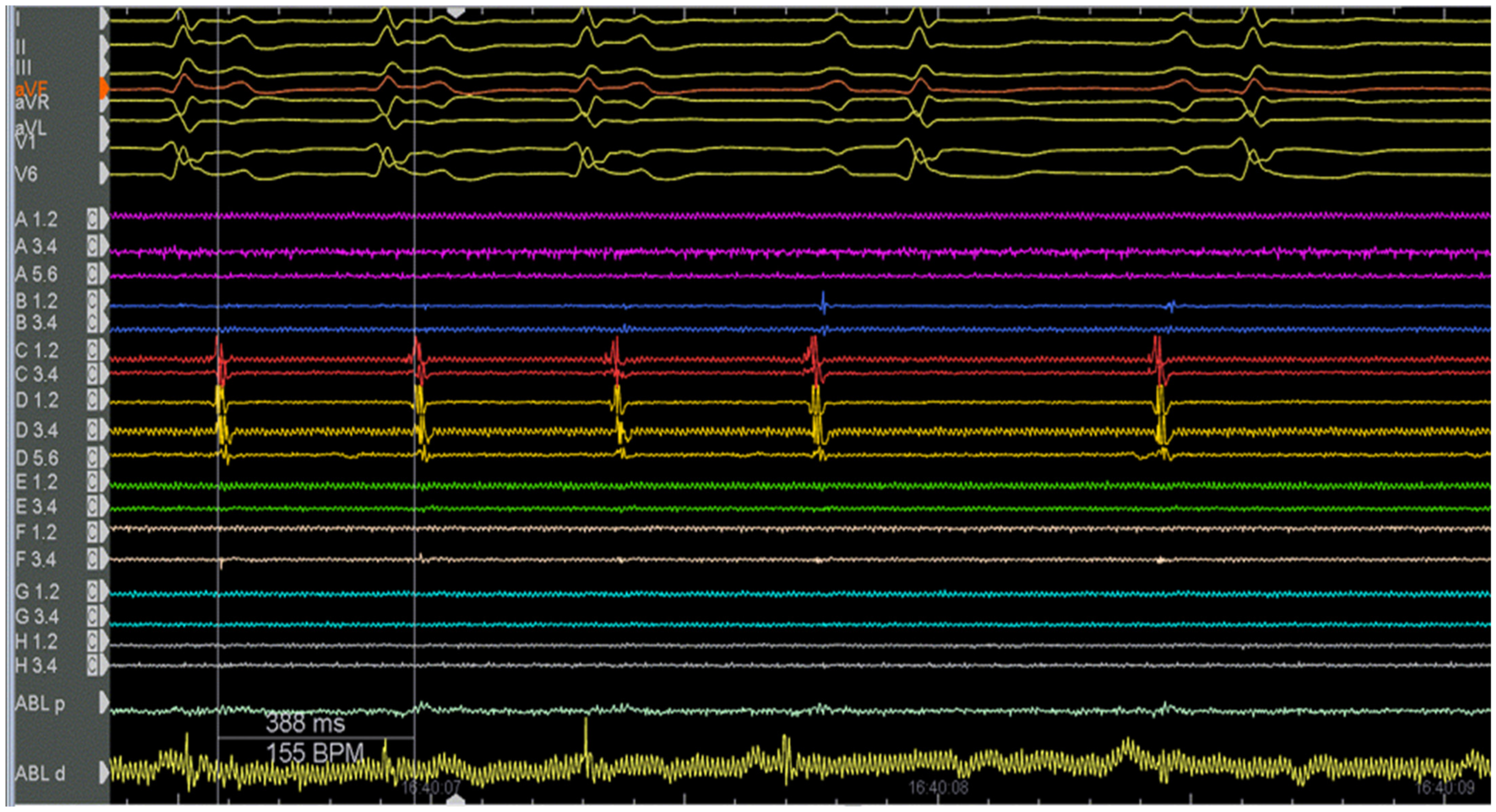
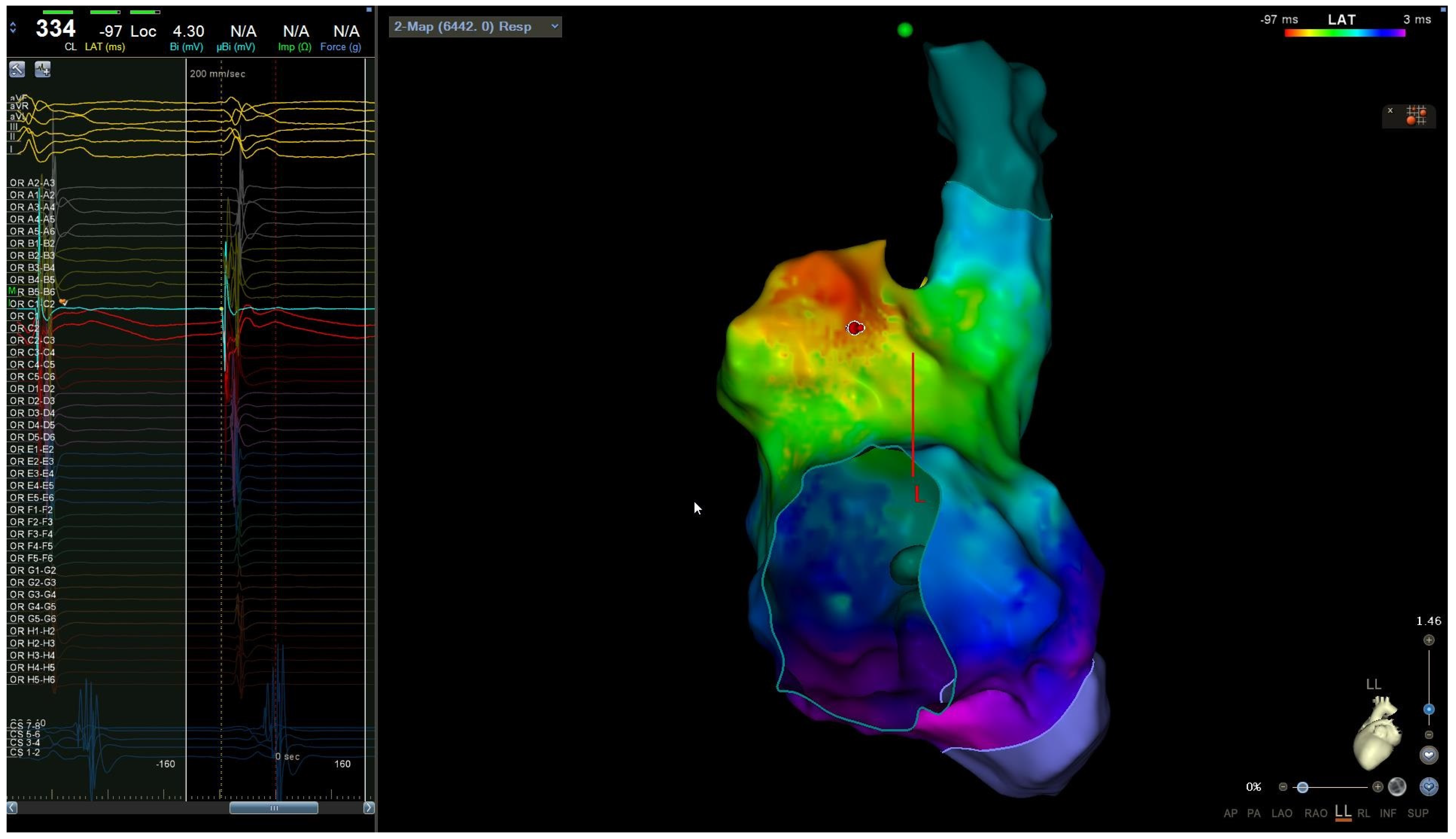
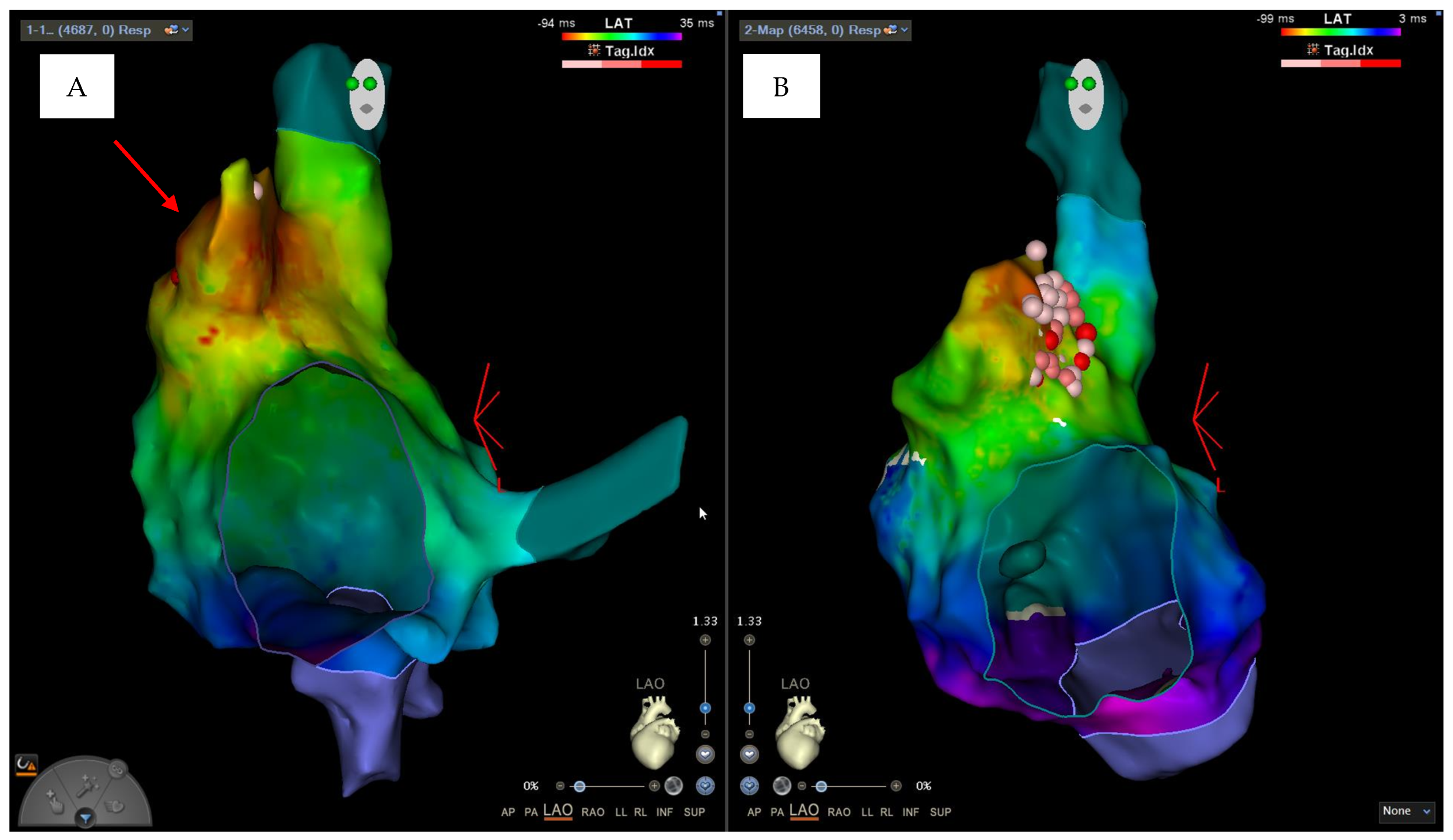
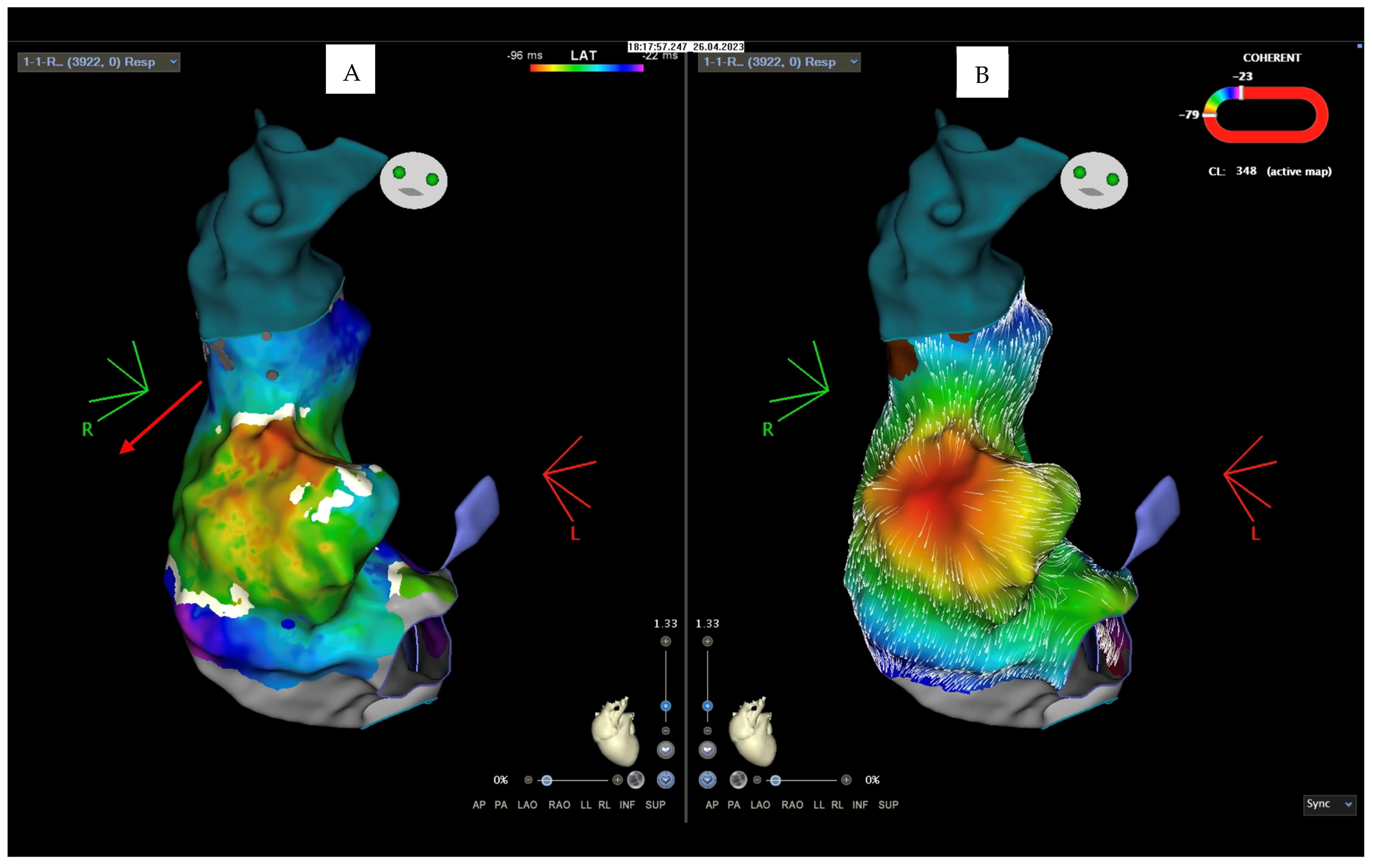
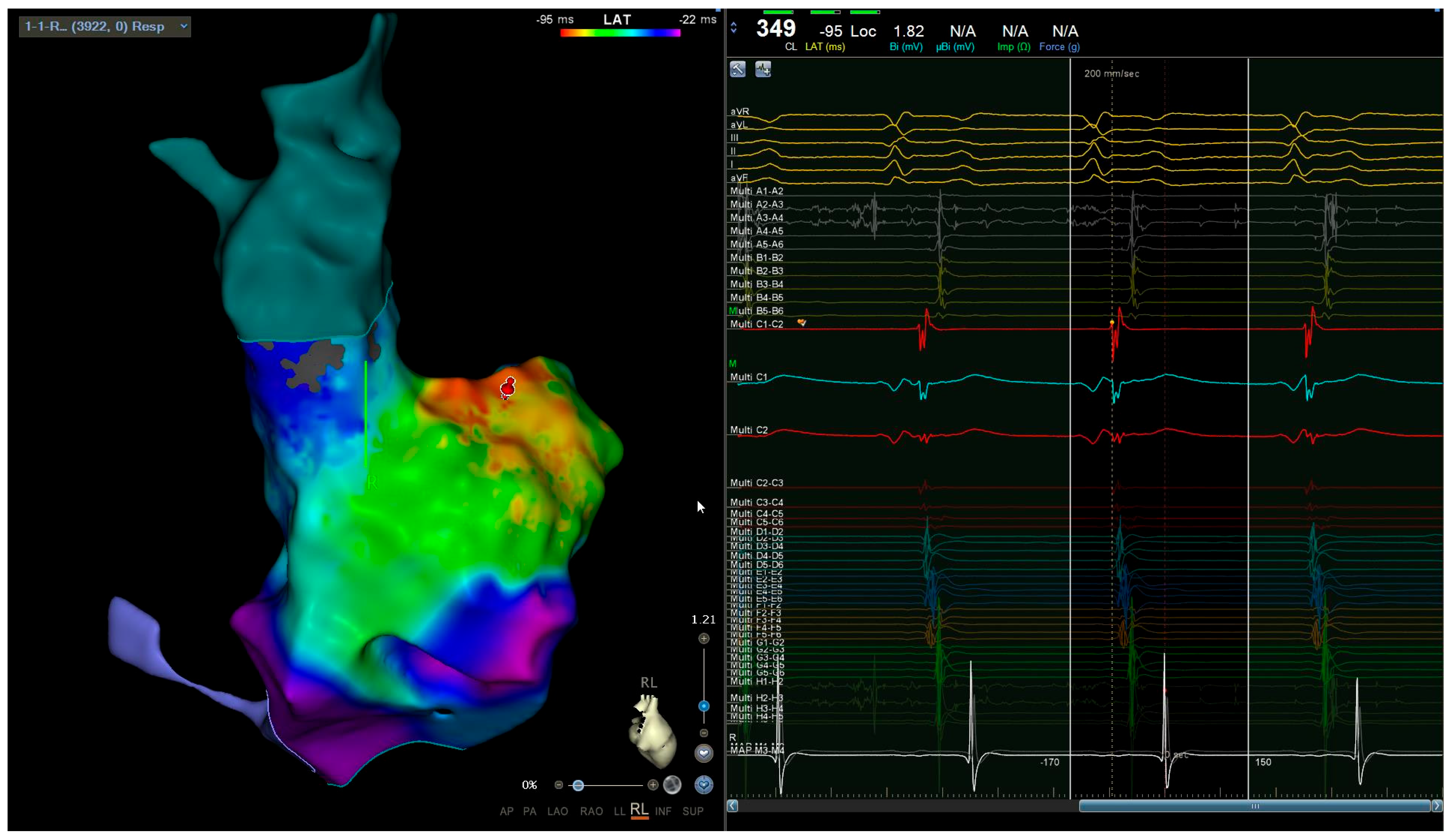
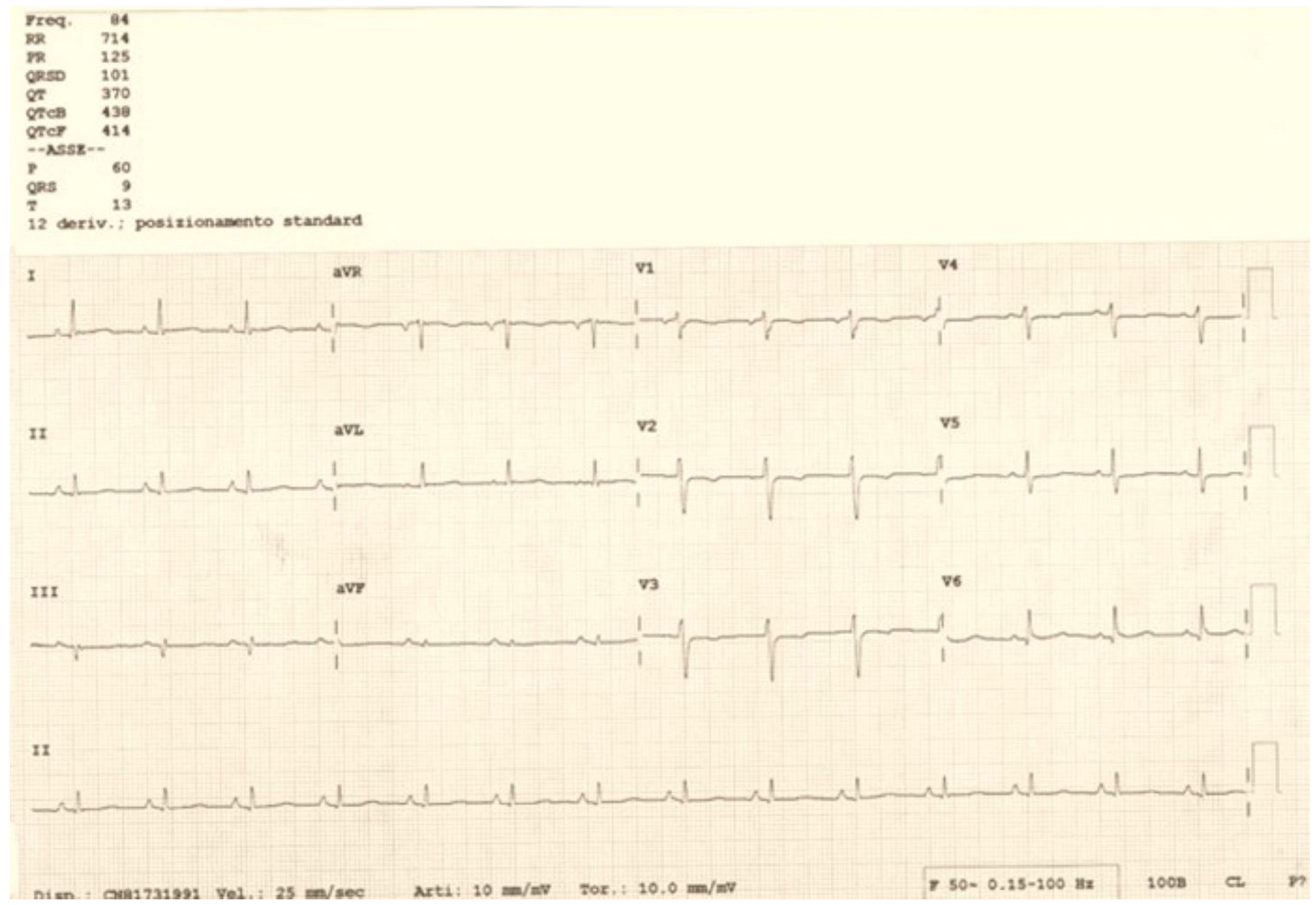
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Regitz-Zagrosek, V.; Roos-Hesselink, J.W.; Bauersachs, J.; Blomström-Lundqvist, C.; Cífková, R.; De Bonis, M.; Iung, B.; Johnson, M.R.; Kintscher, U.; Kranke, P.; et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy: The Task Force for the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 3165–3241. [Google Scholar] [CrossRef] [PubMed]
- Tamirisa, K.P.; Elkayam, U.; Briller, J.E.; Mason, P.K.; Pillarisetti, J.; Merchant, F.M.; Patel, H.; Lakkireddy, D.R.; Russo, A.M.; Volgman, A.S.; et al. Arrhythmias in Pregnancy. Clin. Electrophysiol. 2022, 8, 120–135. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.-M. Catheter ablation for tachyarrhythmias during pregnancy. Adv. Interv. Cardiol. 2022, 18, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Ramlakhan, K.P.; Kauling, R.M.; Schenkelaars, N.; Segers, D.; Yap, S.-C.; Post, M.C.; Cornette, J.; Roos-Hesselink, J.W. Supraventricular arrhythmia in pregnancy. Heart 2022, 108, 1674–1681. [Google Scholar] [CrossRef] [PubMed]
- Driver, K.; Chisholm, C.A.; Darby, A.E.; Malhotra, R.; Dimarco, J.P.; Ferguson, J.D. Catheter Ablation of Arrhythmia during Pregnancy. J. Cardiovasc. Electrophysiol. 2015, 26, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Troisi, F.; Guida, P.; Quadrini, F.; Di Monaco, A.; Vitulano, N.; Caruso, R.; Orfino, R.; Cecere, G.; Anselmino, M.; Grimaldi, M. Zero Fluoroscopy Arrhythmias Catheter Ablation: A Trend toward More Frequent Practice in a High-Volume Center. Front. Cardiovasc. Med. 2022, 9, 804424. [Google Scholar] [CrossRef]
- Roberts-Thomson, K.C.; Kistler, P.M.; Haqqani, H.M.; McGavigan, A.D.; Hillock, R.J.; Stevenson, I.H.; Morton, J.B.; Vohra, J.K.; Sparks, P.B.; Kalman, J.M. Focal atrial tachycardias arising from the right atrial appendage: Electrocardiographic and electrophysiologic characteristics and radiofrequency ablation. J. Cardiovasc. Electrophysiol. 2007, 18, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Li, X.B.; Wang, Y.L.; Yin, J.X.; Zhang, P.; Zhang, H.C.; Xu, Y.; Guo, J.H. Focal atrial tachycardia arising from the right atrial appendage: Electrophysiologic and electrocardiographic characteristics and catheter ablation. Int. J. Clin. Pract. 2009, 63, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Cao, X.; Li, C.; Feng, X.; Sun, D.; Zhang, Y. Case report: Efficacy analysis of radiofrequency catheter ablation pk with atrial appendage resection for atrial tachycardia originating from the atrial appendage in children. Front. Cardiovasc. Med. 2022, 9, 990325. [Google Scholar] [CrossRef]
- Bai, Y.; Qiu, J.; Hu, M.; Chen, G. Emergent Zero-Fluoroscopy Mapping and Thoracoscopic Ectomy of Appendage in Pregnant Women with Life-Threatening Atrial Tachycardia: A Case Report and Literature Review. Medicina 2023, 59, 528. [Google Scholar] [CrossRef] [PubMed]
- Wielandts, J.Y.; Almorad, A.; Hilfiker, G.; Gillis, K.; Haddad, M.E.; Vijgen, J.; Berte, B.; Le Polain de Waroux, J.B.; Tavernier, R.; Duytschaever, M.; et al. Biosense Webster’s QDOT Micro™ radiofrequency ablation catheter. Future Cardiol. 2021, 17, 817–825. [Google Scholar] [CrossRef]
- Antic, D.; Lefkou, E.; Otasevic, V.; Banfic, L.; Dimakakos, E.; Olinic, D.; Milić, D.; Miljić, P.; Xhepa, S.; Stojkovski, I.; et al. Position Paper on the Management of Pregnancy-Associated Superficial Venous Thrombosis. Balkan Working Group for Prevention and Treatment of Venous Thromboembolism. Clin. Appl. Thromb. Hemost. 2022, 28, 1076029620939181. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Troisi, F.; Valenti, N.; Quadrini, F.; Vitulano, N.; Di Monaco, A.; Romanazzi, I.; Caruso, R.; Orfino, R.; Grimaldi, M. Zero-Fluoroscopy Catheter Ablation of Right Appendage Focal Atrial Tachycardia in a Pregnant Woman. Clin. Pract. 2024, 14, 946-953. https://doi.org/10.3390/clinpract14030075
Troisi F, Valenti N, Quadrini F, Vitulano N, Di Monaco A, Romanazzi I, Caruso R, Orfino R, Grimaldi M. Zero-Fluoroscopy Catheter Ablation of Right Appendage Focal Atrial Tachycardia in a Pregnant Woman. Clinics and Practice. 2024; 14(3):946-953. https://doi.org/10.3390/clinpract14030075
Chicago/Turabian StyleTroisi, Federica, Noemi Valenti, Federico Quadrini, Nicola Vitulano, Antonio Di Monaco, Imma Romanazzi, Rosa Caruso, Rocco Orfino, and Massimo Grimaldi. 2024. "Zero-Fluoroscopy Catheter Ablation of Right Appendage Focal Atrial Tachycardia in a Pregnant Woman" Clinics and Practice 14, no. 3: 946-953. https://doi.org/10.3390/clinpract14030075
APA StyleTroisi, F., Valenti, N., Quadrini, F., Vitulano, N., Di Monaco, A., Romanazzi, I., Caruso, R., Orfino, R., & Grimaldi, M. (2024). Zero-Fluoroscopy Catheter Ablation of Right Appendage Focal Atrial Tachycardia in a Pregnant Woman. Clinics and Practice, 14(3), 946-953. https://doi.org/10.3390/clinpract14030075





