Abstract
The optimal time to ambulation remains unclear for intensive care unit (ICU) patients following abdominal surgery. While previous studies have explored various mobilization techniques, a direct comparison between ambulation and other early mobilization methods is lacking. Additionally, the impact of time to ambulation on complications and disuse syndrome prevention requires further investigation. This study aimed to identify the optimal time to ambulation for ICU patients after abdominal surgery and considered its potential influence on complications and disuse syndrome. We examined the relationship between time to ambulation and hospital length of stay (LOS). Patients were categorized into the nondelayed (discharge within the protocol time) and delayed (discharge later than expected) groups. Data regarding preoperative functioning, postoperative complications, and time to discharge were retrospectively collected and analyzed. Of the 274 postsurgical patients managed in the ICU at our hospital between 2018 and 2020, 188 were included. Time to ambulation was a significant prognostic factor for both groups, even after adjusting for operative time and complications. The area under the curve was 0.72, and the cutoff value for time to ambulation was 22 h (sensitivity, 68%; specificity, 77%). A correlation between time to ambulation and complications was observed, with both impacting the hospital LOS (model 1: p < 0.01, r = 0.22; model 2: p < 0.01, r = 0.29). Specific cutoff values for time to ambulation will contribute to better surgical protocols.
1. Introduction
During the perioperative period of abdominal surgery, postoperative bed rest leads to intensive care unit (ICU)-acquired weakness (ICU-AW) and disuse syndrome [1], which not only prolong the hospital length of stay but also reduce patients’ quality of life (QOL) and increase medical costs. Early mobilization is a general activity that prevents disuse syndrome [2]. Specific techniques include standing from the bed, sitting up in bed, and walking. However, there is no consensus regarding which mobilization technique is most effective [3]. One study has shown that the length of time before walking independently (time to ambulation) is important to early mobilization, which can affect the hospital length of stay [4]. Therefore, it is necessary to consider ambulation as a mobilization technique that can prevent disuse syndrome.
Early ambulation is critical in intensive care physiotherapy because it significantly improves physical functions that have been reduced by lying in bed and improves QOL after discharge. Early ambulation in the ICU minimizes the effects of ICU-AW [5], shortens the hospital length of stay, and reduces complications [6]. Similarly, enhanced recovery after surgery (ERAS) protocols recommend early mobilization to promote postoperative recovery [7] and shorter hospital stays [8] in the surgical ICU.
Therefore, early ambulation can effectively reduce the hospital length of stay for ICU patients with disuse syndrome. However, the optimal time to ambulation after surgery for ICU patients has not been fully investigated. Recently, because the number of elderly patients undergoing surgery has increased, the number of patients who have been admitted to the ICU after abdominal surgery has increased [9,10,11]. Therefore, early ambulation in the ICU should be considered after abdominal surgery. Furthermore, the importance of early mobilization after abdominal surgery has been suggested in recent years, and it is actively being considered for ERAS protocols [3].
A study of patients who underwent minimally invasive surgery for gastric cancer found that respiratory function and time to ambulatory independence were factors that affect the hospital length of stay [4]. In the case of surgery, such as pancreaticoduodenectomy and hepatectomy, early ambulation on postsurgical day 1 is recommended; however, the level of evidence is low [12]. Compared to minimally invasive surgeries, highly invasive surgeries place a heavier burden on the body. Therefore, postoperative vital signs are more labile, resulting in delayed ambulation. Additionally, complications may prolong the hospital length of stay. Regarding abdominal surgery, examining the relationship between the specific time to ambulation and hospital length of stay may provide a specific indicator of when patients should start ambulating in the ICU, thus possibly contributing to shorter hospital stays.
This study aimed to determine the relationship between the time to ambulation initiation and other factors that prolong the hospital length of stay of patients admitted to the ICU after abdominal surgery and investigate specific time to ambulation cutoff values for prolonged lengths of stay.
2. Materials and Methods
This retrospective study investigated the causal relationship between time to ambulation initiation and hospital length of stay. Patients included in the study were divided into two groups. The nondelayed group included those who were discharged within the number of days stated in the hospital disease protocol, and the delayed group included those who were discharged later than expected according to the hospital disease protocol.
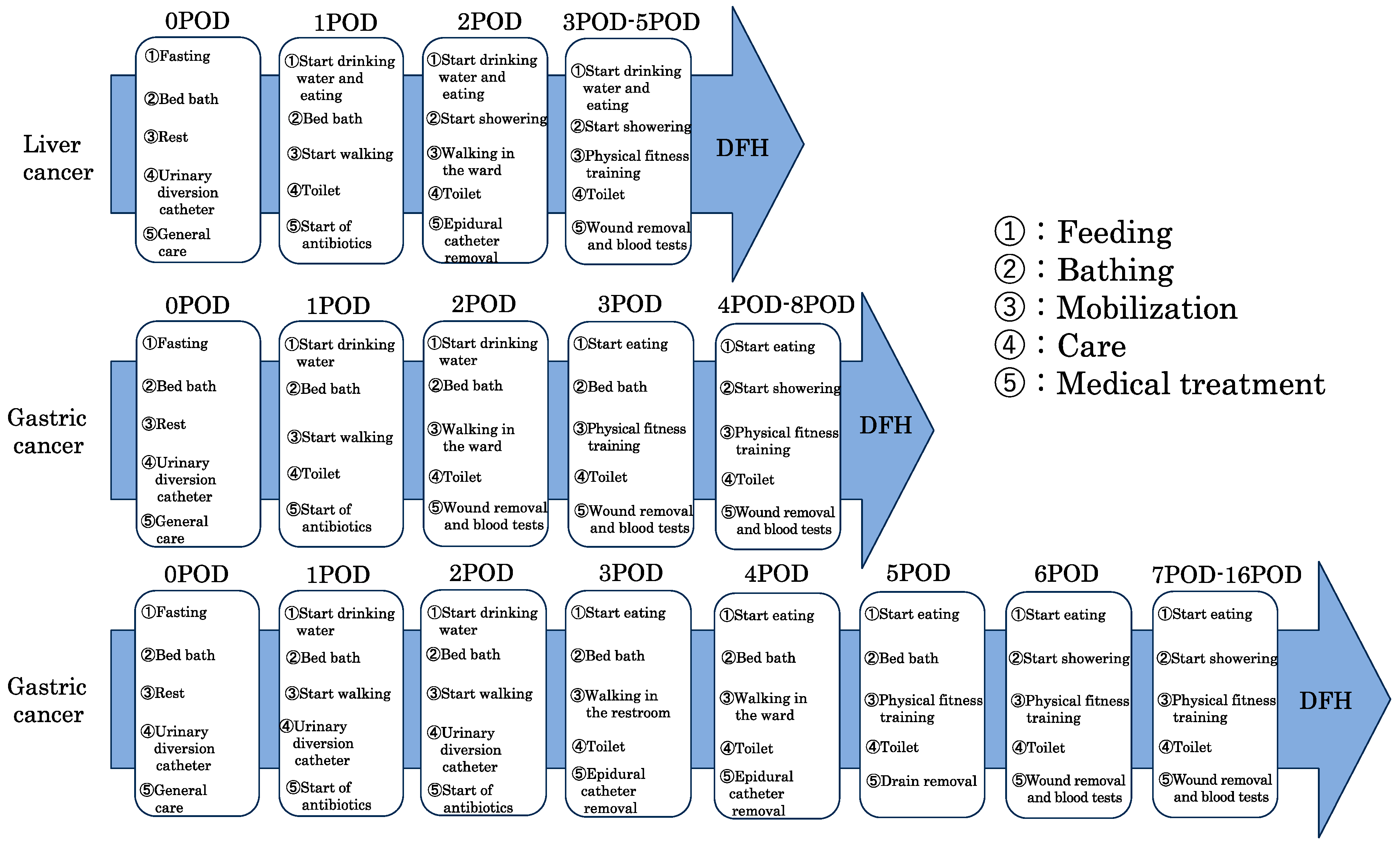
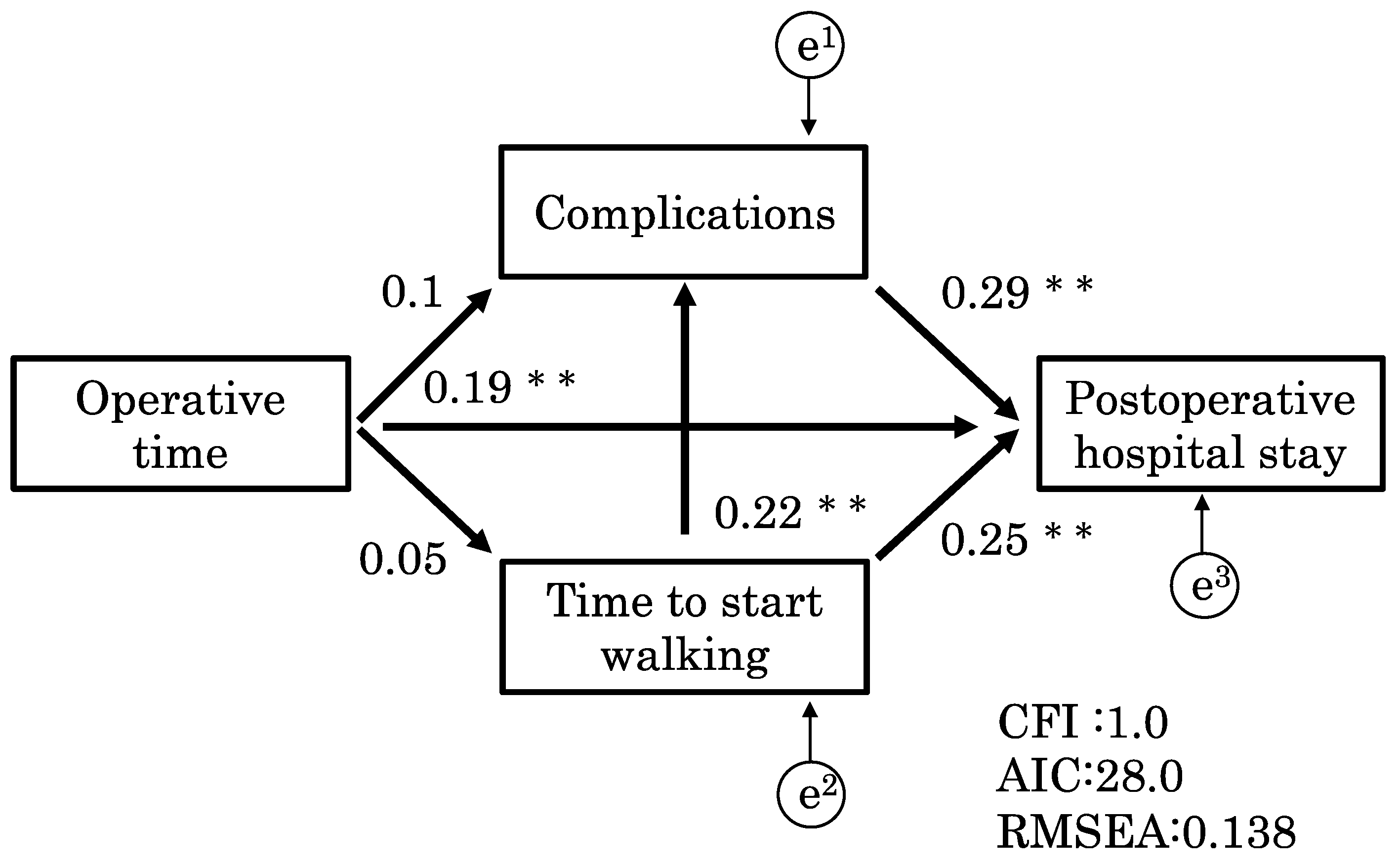
The inclusion criteria were gastrointestinal surgery, admission to the ICU, and rehabilitation between 2018 and 2020. This study was conducted at a large hospital that can handle major surgeries and employs many physical therapists dedicated to the ICU. Additionally, well-trained staff members are available for patient interventions. Perioperative protocols for typical diseases are shown in Figure 1. The protocols are shared by the ICU team, and treatment is performed according to these protocols. Mobilization is handled by physical therapists.
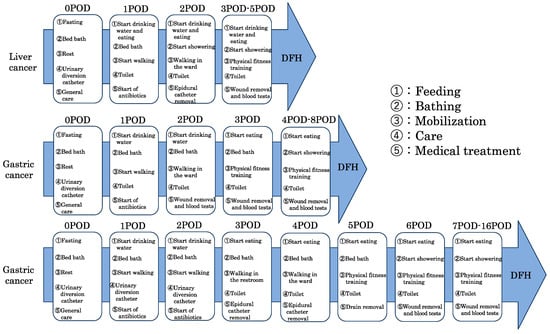
Figure 1.
Clinical paths for typical diseases. DFH; discharge from hospital.
For surgeries without surgical protocols, patients who stayed in the hospital longer than the planned discharge date, which was set by the attending physician during the preoperative explanation to the patient, were classified as the delayed group.
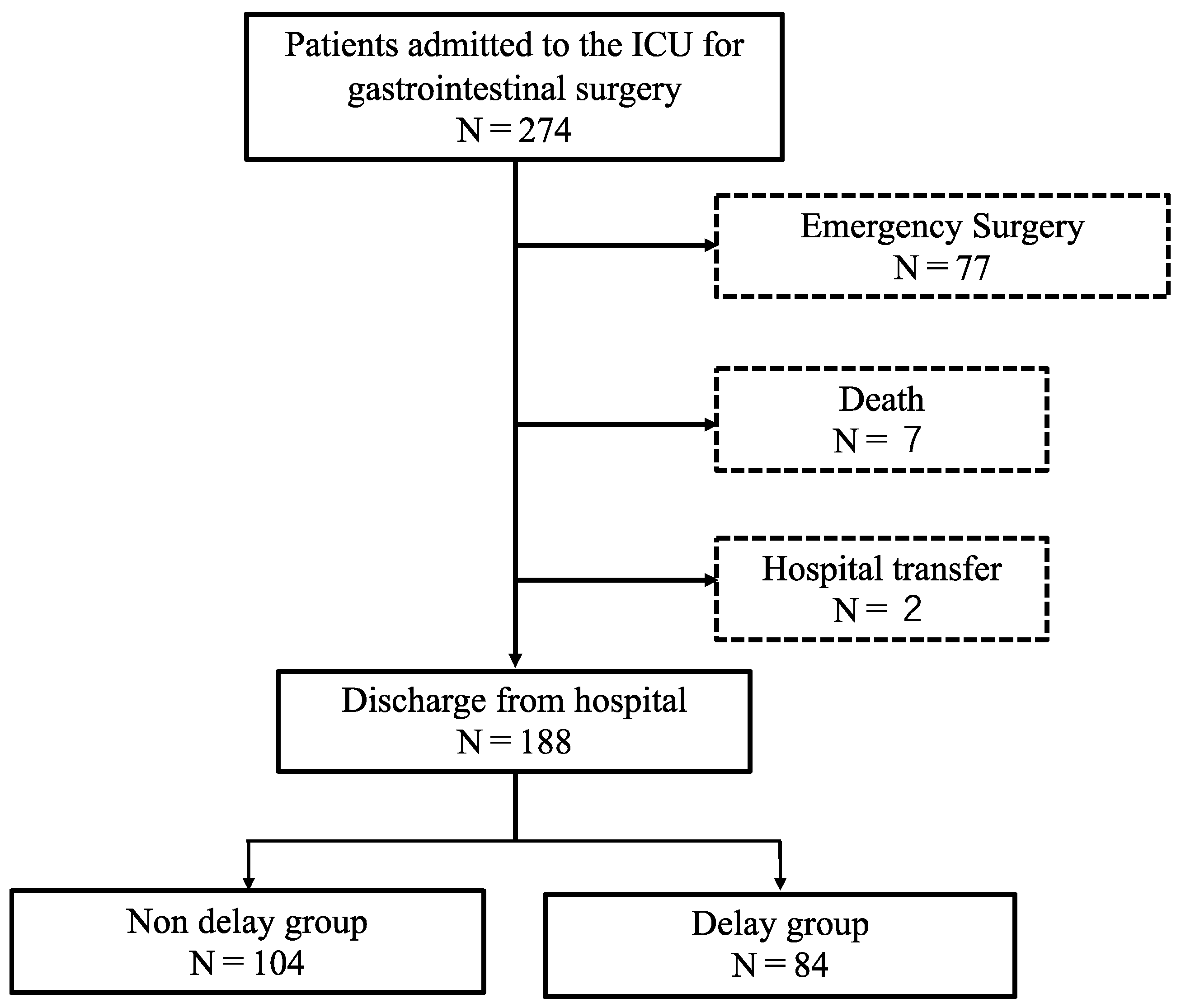
The exclusion criteria comprised emergency surgery, death, or hospital transfer. During this study, we excluded 77 patients who underwent emergency surgery, 7 patients who died, and 2 patients who were transferred to another hospital. The remaining 188 patients were included in the analysis. All these patients had no cognitive impairment before admission and were able to walk independently during their daily lives. The following data were retrospectively collected: age, sex, height, surgical procedure, preoperative vital capacity (%VC), in-hospital complications, postoperative hospital length of stay, operative time, total blood loss, time to ambulation, reasons for nonambulation, time to standing from the hospital bed, and Acute Physiologic Assessment and Chronic Health Evaluation (APACHE) II score. The postoperative hospital length of stay was from the day of surgery (day 0) to the day of discharge. Postoperative complications were defined as complications that required treatment. Preoperative vital capacity (%VC) is a pulmonary function used to assess the risk of complications before surgery during the perioperative period [4]. Previous studies have reported that %VC is associated with the hospital length of stay. According to previous studies, operative time and total blood loss also affect the hospital length of stay [13]. To further assess the weaning process, weaning data including the time to ambulation, time to wheelchair sitting, time to end of wheelchair dependence, and time to standing from the hospital bed were collected. Disease severity was assessed using the APACHE II score, which is the most commonly used scoring system for determining the severity of illness worldwide [14].
Statistical analyses were performed using JMP version 11.5 (SAS Institute Inc., Cary, NC, USA) and SPSS Amos (IBM Corp., Armonk, NY, USA). We compared the nondelayed and delayed groups according to differences in early discharge delays. The dependent variable for both the delayed and nondelayed groups was the postoperative hospital length of stay. This study was conducted at Ageo Central General Hospital in Japan between 2018 and 2020. Data regarding time to first ambulation, time to wheelchair sitting, time to end of sitting, and time to standing from the hospital bed were collected during a 4-month period from April to August 2020, and examined using the unpaired t-test or chi-squared test to determine each group’s attributes. During the analysis of factors associated with the hospital length of stay, the hospital length of stay was a binary variable (delayed group vs. nondelayed group). Therefore, we performed a logistic regression analysis.
The logistic regression analysis was performed using the forced imputation method, with the hospital length of stay (in days) as the dependent variable, time to ambulation as the exposure, ambulation items as covariates, and preoperative items and ambulation-related items as confounders. To check for multicollinearity of the input items, a regression analysis was performed. Items with a regression coefficient ≥0.9 were excluded. Additionally, the goodness-of-fit of the model in the logistic regression analysis was determined using the Akaike information criterion (AIC). We conducted a path analysis for each factor to confirm the relationship between factors. A path analysis has validity in the medical field because it allows for the examination of inter-relationships of factors [15,16]. We created models using the obtained factors and then evaluated the validity of those models. The fit of the model in the path analysis was evaluated using a comparative fit index (CFI), AIC, and a root mean square error of approximation (RMSEA). In general, a CFI close to 1 and an RMSEA less than 0.07 are considered to indicate a good fit for the model [17].
This study was conducted with the approval of the Ethics Committee of Ageo Central General Hospital (approval no. 829). The study was conducted with the written consent of all research participants.
3. Results
Of the 274 patients who underwent invasive abdominal surgery and subsequent ICU management during this period, 188 patients who underwent surgery and rehabilitation were included in the analysis (Figure 2). During this study, 73% of patients underwent bile duct pancreatic surgery. The proportions of patients who underwent upper and lower digestive tract surgeries were similar (Table 1).
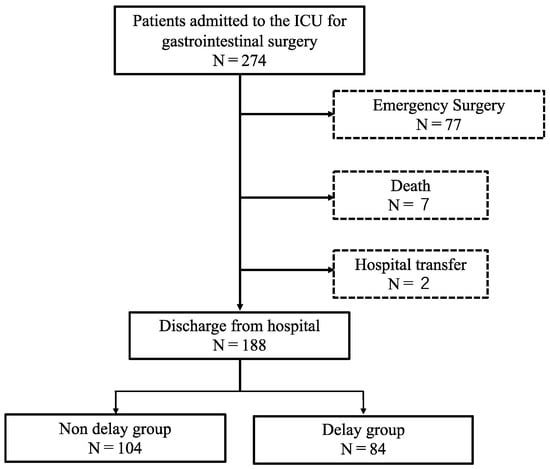
Figure 2.
Patient selection for this study.

Table 1.
Number of participants by surgery.
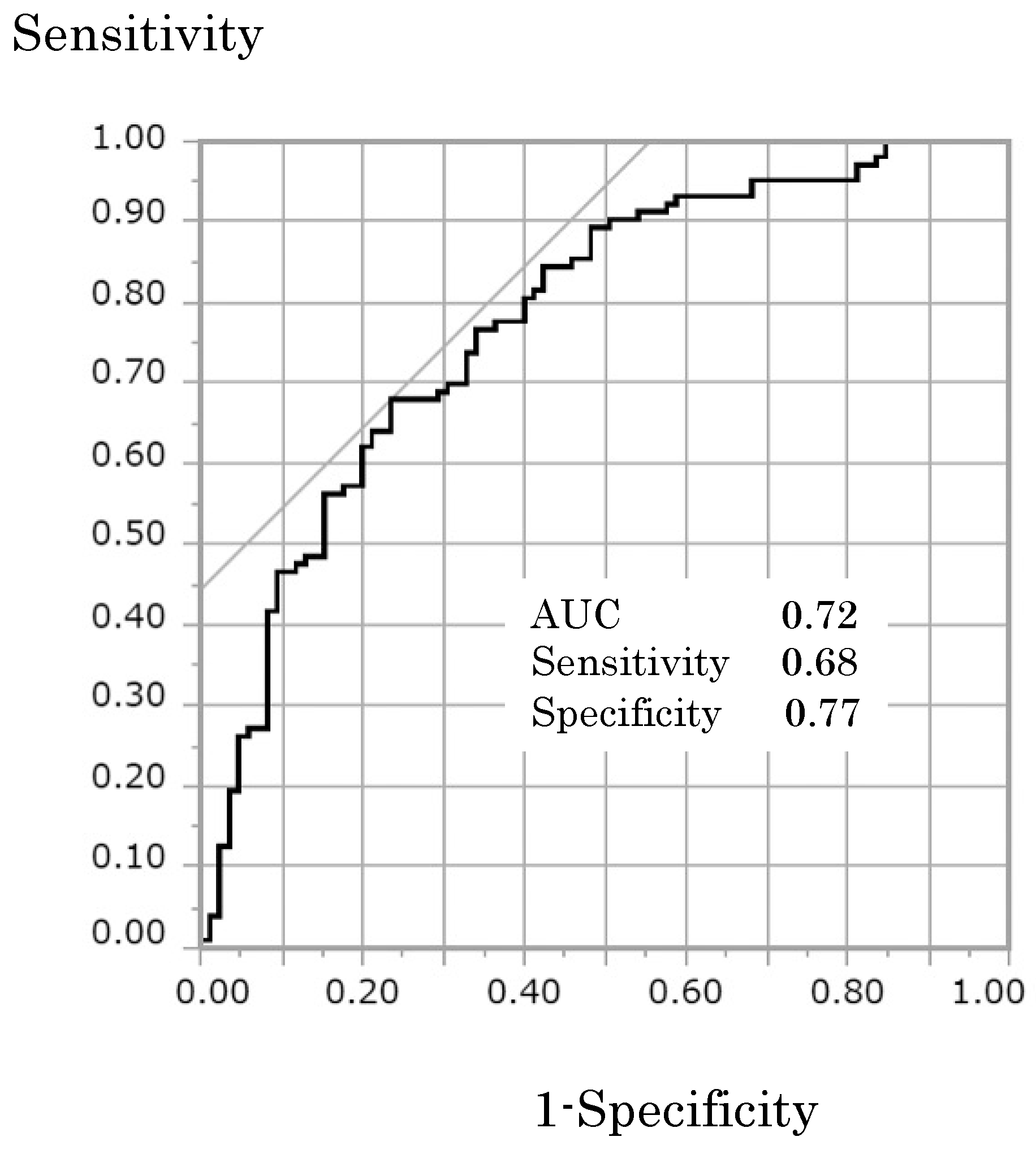
A comparison between the non-delayed and delayed groups showed that the delayed group had significantly longer operative times, greater total blood loss, more complications, and a longer time to ambulation (Table 2). The results of the logistic regression analysis depicted in Table 3 show that for both the delayed and non-delayed postoperative hospital stay groups, the time to ambulation (p < 0.01; odds ratio [OR], 0.99; 95% confidence interval [CI], 0.993–0.999) was a significant variable. The other significant factors were the presence of complications (p < 0.01; OR, 0.14; 95% CI, 0.054–0.345) and operative time (p < 0.05; OR, 0.99; 95% CI, 0.999–0.994). In Figure 3, the receiver operating characteristic (ROC) curve showed that the area under the curve (AUC) was 0.77; the cutoff value for time to ambulation was 22 h. The sensitivity and specificity of this cutoff value were 68% and 77%, respectively. The high specificity suggests that time to ambulation, together with other factors, may predict delayed hospital discharge.

Table 2.
Basic characteristics of the participants.

Table 3.
Results of the logistic regression analysis of the hospital length of stay.
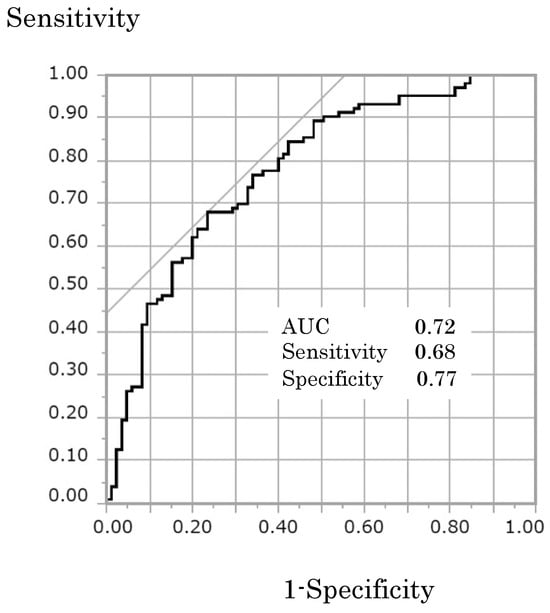
Figure 3.
Receiver-operating characteristic (ROC) curve associated with the cutoff time calculation for time to ambulation initiation related to the hospital length of stay. AUC is the area under the curve.
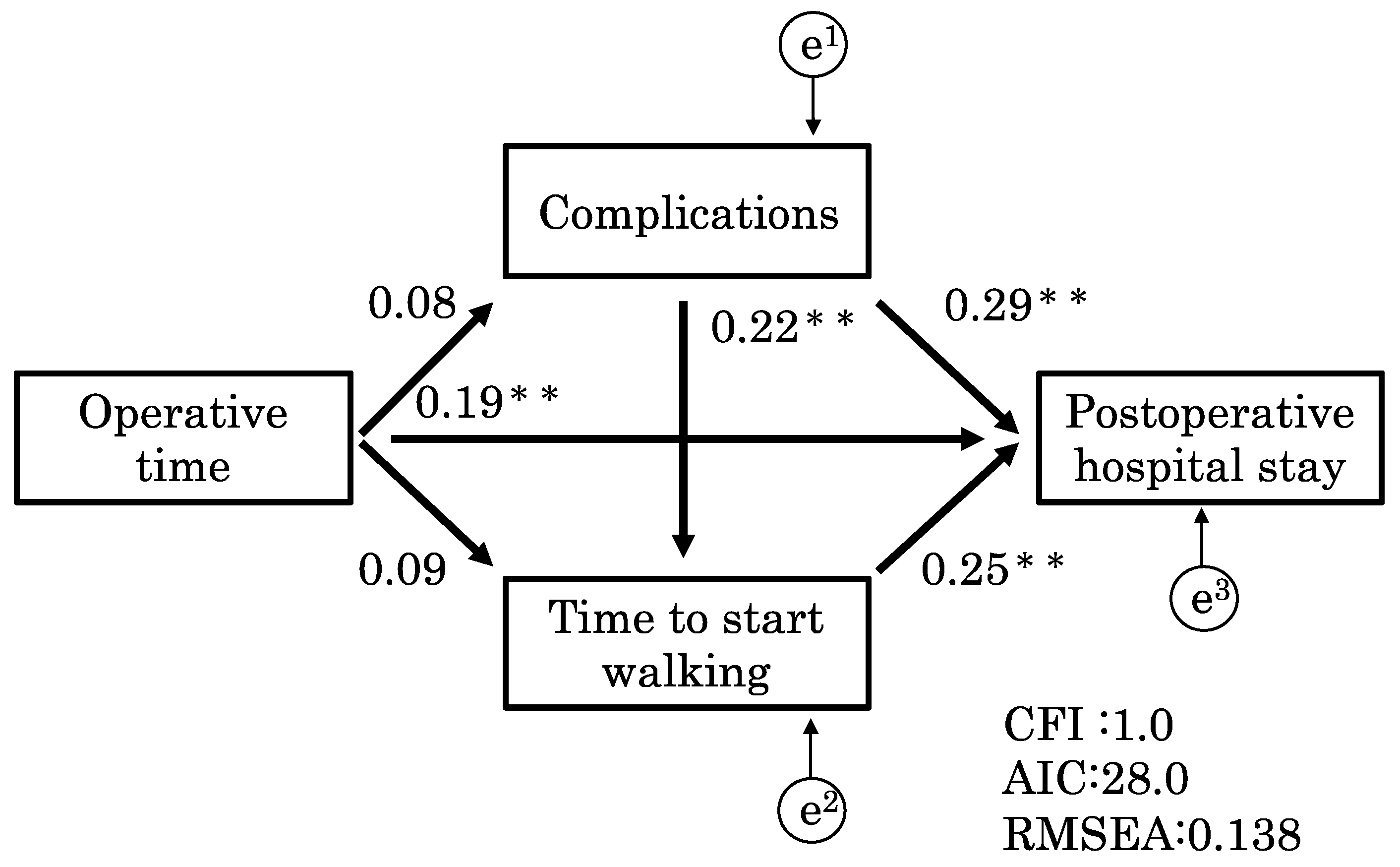
We investigated the relationship between factors related to the hospital length of stay using a path analysis. Operative time (r = 0.24; p < 0.01), complications (r = 0.43; p < 0.01), and time to ambulation (r = 0.27; p < 0.01) were related to the hospital length of stay, whereas complications were related to the time to ambulation (r = 0.17; p < 0.01) (Table 4). These results were significant for indicating an association, but the strength of the association was mild. A path analysis was performed to create two models. Model 1 (Figure 4) had a CFI of 1.0, AIC of 28.0, and RMSEA of 0.14. Similarly, model 2 (Figure 5) had a CFI of 1.0, AIC of 28.0, and RMSEA of 0.14. These models did not have significantly different fit, with a CFI of 1.0 indicating a good fit and an RMSEA of 0.14 indicating a fair fit.

Table 4.
Correlations of each factor.
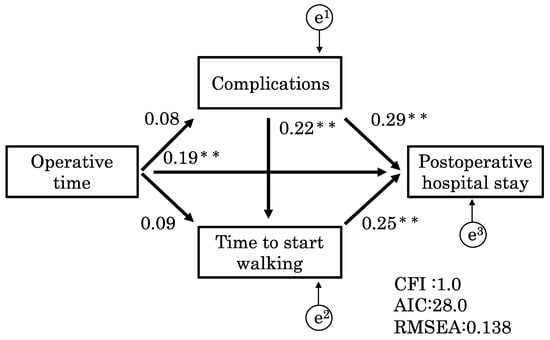
Figure 4.
Model 1. This model shows how complications affect time to ambulation. Model 1 had a CFI of 1.0, an AIC of 28.0, and an RMSEA of 0.14. The models demonstrated that the time to ambulation and complications (p < 0.01; r = 0.22) interacted with each other and affected the hospital length of stay. CFI, comparative fit index; AIC, Akaike information criterion; RMESEA, root mean square error of approximation. ** p < 0.01.
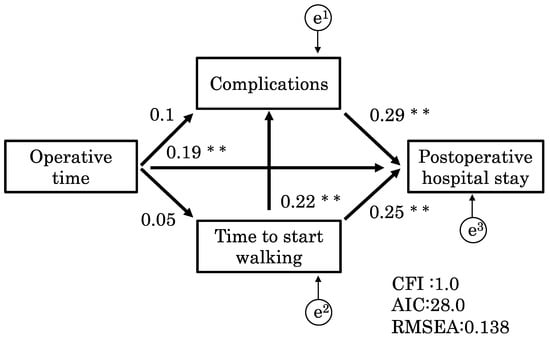
Figure 5.
Model 2. This model shows how time to ambulation affects complications. Model 2 had a CFI of 1.0, AIC of 28.0, and RMSEA of 0.14. Model 2 was more effective and had a stronger effect on the hospital length of stay than model 1 (p < 0.01; r = 0.29). CFI, comparative fit index; AIC, Akaike information criterion; RMESEA, root mean square error of approximation. ** p < 0.01.
The models demonstrated that the time to ambulation and complications (p < 0.01; r = 0.22) corresponded and affected the hospital length of stay. Additionally, model 2 was more effective and had a stronger effect on the hospital length of stay than model 1 (p < 0.01; r = 0.29). This suggests that these two models had the same fit, but that the path from time to ambulation to the hospital length of stay via complications was more strongly associated in model 2 than in model 1.
4. Discussion
The time to ambulation and its effect on the hospital length of stay for patients who underwent abdominal surgery and were admitted to the ICU were investigated. However, whether the process of initiating postsurgical ambulation affects the hospital length of stay or other factors during the course of hospitalization remains unclear. Although the ERAS protocols recommend that patients should start walking on the first postsurgical day after pancreaticoduodenal surgery, the degree to which varying times to ambulation affect outcomes has not yet been studied [18].
This study is clinically significant because it enabled us to examine the effect that time to ambulation has on the hospital length of stay and further allowed for more focus on initiating postsurgical ambulation in the ICU.
We hypothesized that the time to ambulation affects the hospital length of stay. A logistic regression analysis, including confounding, showed that the time to ambulation, even after adjusting for operative time and complications, had a crucial role in determining the hospital length of stay. Previous studies have reported that operative time and complications can prolong the hospital length of stay [19,20], and our results support those results. We demonstrated for the first time that not only the operative time and complications but also the time to ambulation are related to the hospital length of stay. The association between delayed time to ambulation (>1 day) and hospital length of stay has been shown previously [4,21]. Some previous studies have reported that comprehensive interventions, including walking, prevent complications and reduce the number of days in the hospital [22,23]. This is the first study to examine the cutoff of delayed ambulation for patients who have undergone abdominal surgery. Based on the ROC curve, the cutoff value for time to ambulation was 22 h.
Ni et al. reported that early mobilization (walking within 2 days of surgery) was associated with shorter hospital length of stay and improved gastrointestinal function of patients who underwent surgery for liver cancer, but there was no significant difference in complications [24]. However, other studies reported that early mobilization on the day of surgery for patients with pancreatic cancer can improve oxygenation in the short term [25] and that early mobilization may prevent postoperative complications. Based on these reports, the association between early mobilization and complications has not yet been definitively established.
The reason why this study defined early mobilization as walking is because many previous studies have not distinguished walking from sitting up in bed. During this study, we focused on walking for early mobilization. In particular, the cutoff time to ambulation of 22 h in this study referred to walking and was more exact than the goal of leaving the bed within 24 h used by previous studies. In clinical practice, it may be necessary to consider, for example, starting walking in the evening if surgery is completed in the morning, and starting walking in the morning or afternoon if surgery is completed in the evening. This suggests that early initiation of ambulation, as proposed by the ERAS protocol, can shorten the hospital length of stay for patients who have undergone abdominal surgery. Although the participants in this study were able to independently perform activities of daily living, their preoperative physical function [4] may have influenced the initiation of ambulation; however, the preoperative physical function was not considered during this study.
Operative time and complications affect the transfer destination of patients. Previous studies have shown that delayed postoperative ambulation after minimally invasive surgery increases the risk of complications [21,26,27]. Therefore, during this study, we performed a path analysis to examine factors that affect the hospital length of stay after invasive surgery. Significantly, these factors were sequentially quantified by the path analysis during this study. The results of models 1 (Figure 4) and 2 (Figure 5) indicated that, along with complications and operative time, postsurgical time to ambulation affects the hospital length of stay; however, complications and time to ambulation were related factors that affected hospital stay. Furthermore, this study showed that the time to ambulation and complications correspond to each other, suggesting that complications may affect the time to ambulation and increase the hospital length of stay.
Models 1 and 2 showed that the pathway from time to ambulation to hospital length of stay via complications was more significant than the pathway from complications to hospital length of stay via time to ambulation. This means that there is a series of pathways in which the time to ambulation affects the hospital length of stay attributable to complications. These results suggest that, in clinical practice, it is critical to focus attention on complications originating from delayed postsurgical ambulation to prevent a prolonged hospital stay.
Rivas et al. reported that the bed rest duration, including sitting and standing after surgery, was significantly associated with complications, with pneumonia being the most common postoperative complication [28]. The most common postoperative complication during this study was pancreatic fistula, followed by pneumonia, which is consistent with previous studies. This study included many pancreatic and liver surgeries, with an average operative time of 6 to 7 h, which means that patients were in the supine position during surgery for long periods. Anesthesia, muscle relaxants, and opioids used for postoperative pain management can decrease the cough reflex and accessory muscle function [22]. Additionally, staying in the same position for a long time can lead to decreased ventilation and difficulty expectorating sputum, thus increasing the risk of pneumonia [4]. Furthermore, abdominal surgery can cause abdominal edema, which can increase intra-abdominal pressure and impair ventilation function, even in the sitting position. Although the average preoperative %VC in this study was more than 100%, the increased risk of pulmonary complications may have been associated with the combination of long operative times and delayed walking. On the other hand, studies have shown that early mobilization compliance is quite low among patients who have undergone colorectal surgery. Specifically, it has been reported that less than 50% of patients left the bed on the first day after surgery [29]. During this study, the delayed group started sitting after approximately 25 h, and the average time to ambulation was 52 h. However, further investigation is necessary to understand the reasons for the lack of mobilization.
The results of this study provided time-based numerical values and specific mobilization methods that will contribute to the establishment of more detailed protocols. Additionally, sharing these results with various healthcare professionals and patients in the ICU will lead to beneficial outcomes. For example, by coordinating postoperative schedules to initiate walking as soon as possible, complications may be prevented. Additionally, explaining the importance of early walking to patients may increase their cooperation, and discharge can occur as planned.
This study was limited because we did not sufficiently examine each specific disease. For example, surgical invasiveness and postoperative complications differ between the lower gastrointestinal tract and pancreas. Therefore, disease-specific applications of this research are necessary. Future studies should consider separating various classes of diseases and examining them independently. Furthermore, because the time to ambulation was calculated from the time when surgery ended, the time to ambulation may have been delayed by factors related to the medical staff. For example, a patient whose surgery was completed during the day will have a longer time to ambulation than that of a patient whose surgery was completed at night. Therefore, future studies should include the time constraints of the medical staff.
5. Conclusions
We examined factors that influence the hospital length of stay after invasive abdominal surgery and found that time to ambulation was a significant factor when the cutoff value was 22 h. Further examination of the relationship between these factors revealed that although time to ambulation was associated with complications, it had a stronger effect on the hospital length of stay.
Author Contributions
Conceptualization, T.A. and D.M.; Software, K.F., H.M. and Y.S.; formal analysis, Y.M. and K.F.; investigation, D.M., Y.M. and H.M.; data curation, K.F. and H.M.; writing—original draft, T.A.; writing—review & editing, T.A., Y.M., M.K. and Y.S.; visualization, Y.S; supervision, D.M., M.K., S.S. and K.Y.; project administration, S.S.; funding acquisition, T.A.; data interpretation and interpretation of physical therapy after abdominal surgery, DM. and Y.M.; data collection and interpretation, K.F., H.M., M.K. and K.Y.; interpretation of ICU management, M.K. and K.Y.; overall organization of the paper and statistical analysis, Y.S. and S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant from the Saitama Chapter, Japanese Physical Therapy Association for Study Promotion (grant number 20-04) and an internal research grant from the University of Health Sciences (grant number 2021-21).
Institutional Review Board Statement
This study was conducted with the approval of the Ethics Committee of Ageo Central General Hospital (approval no. 829 and date of 22 May 2020). The study was conducted with the written consent of all research subjects.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data generated or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors thank Koichiro Ichimura (Department of Anatomy and Life Structure, Juntendo University Graduate School of Medicine, Tokyo, Japan) for their invaluable help and advice throughout the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kramer, C.L. Intensive care unit-acquired weakness. Neurol. Clin. 2017, 35, 723–736. [Google Scholar] [CrossRef]
- Denehy, L.; Lanphere, J.; Needham, D.M. Ten reasons why ICU patients should be mobilized early. Intensive Care Med. 2017, 43, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Tazreean, R.; Nelson, G.; Twomey, R. Early mobilization in enhanced recovery after surgery pathways: Current evidence and recent advancements. J. Comp. Eff. Res. 2022, 11, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Amari, T.; Hirukawa, C.; Fukuda, T.; Hidaka, Y.; Makita, Y.; Fukuda, K.; Sakamoto, Y.; Kimura, M.; Yamaguchi, K. Factors affecting the length of hospital days after laparoscopic gastrectomy for elderly patients with gastric cancer. J. Gastrointest. Cancer 2022, 53, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Hu, W.; Cai, Z.; Liu, J.; Wu, J.; Deng, Y.; Yu, K.; Chen, X.; Zhu, L.; Ma, J.; et al. Early mobilization of critically ill patients in the intensive care unit: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0223185. [Google Scholar] [CrossRef] [PubMed]
- Schweickert, W.D.; Kress, J.P. Implementing early mobilization interventions in mechanically ventilated patients in the ICU. Chest 2011, 140, 1612–1617. [Google Scholar] [CrossRef] [PubMed]
- Fearon, K.C.; Ljungqvist, O.; Von Meyenfeldt, M.; Revhaug, A.; Dejong, C.H.; Lassen, K.; Nygren, J.; Hausel, J.; Soop, M.; Andersen, J.; et al. Enhanced recovery after surgery: A consensus review of clinical care for patients undergoing colonic resection. Clin. Nutr. 2005, 24, 466–477. [Google Scholar] [CrossRef]
- Munitiz, V.; Martinez-de-Haro, L.F.; Ortiz, A.; Ruiz-de-Angulo, D.; Pastor, P.; Parrilla, P. Effectiveness of a written clinical pathway for enhanced recovery after transthoracic (Ivor Lewis) oesophagectomy. Br. J. Surg. 2010, 97, 714–718. [Google Scholar] [CrossRef]
- Bagshaw, S.M.; Webb, S.A.; Delaney, A.; George, C.; Pilcher, D.; Hart, G.K.; Bellomo, R. Very old patients admitted to intensive care in Australia and New Zealand: A multi-centre cohort analysis. Crit. Care 2009, 13, R45. [Google Scholar] [CrossRef]
- Docherty, A.B.; Anderson, N.H.; Walsh, T.S.; Lone, N.I. Equity of access to critical care among elderly patients in Scotland: A national cohort study. Crit. Care Med. 2016, 44, 3–13. [Google Scholar] [CrossRef]
- Nielsson, M.S.; Christiansen, C.F.; Johansen, M.B.; Rasmussen, B.S.; Tonnesen, E.; Norgaard, M. Mortality in elderly ICU patients: A cohort study. Acta Anaesthesiol. Scand. 2014, 58, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Melloul, E.; Lassen, K.; Roulin, D.; Grass, F.; Perinel, J.; Adham, M.; Wellge, E.B.; Kunzler, F.; Besselink, M.G.; Asbun, H.; et al. Guidelines for perioperative care for pancreatoduodenectomy: Enhanced recovery after surgery (ERAS) recommendations 2019. World J. Surg. 2020, 44, 2056–2084. [Google Scholar] [CrossRef] [PubMed]
- Harrison, O.J.; Smart, N.J.; White, P.; Brigic, A.; Carlisle, E.R.; Allison, A.S.; Ockrim, J.B.; Francis, N.K. Operative time and outcome of enhanced recovery after surgery after laparoscopic colorectal surgery. JSLS 2014, 18, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Yao, Y.; Zhou, J.; Diao, X.; Chen, H.; Cai, K.; Ma, X.; Wang, S. Dynamic APACHE II score to predict the outcome of intensive care unit patients. Front. Med. 2021, 8, 744907. [Google Scholar] [CrossRef] [PubMed]
- Costello, R.M. Premorbid social competence construct generalizability across ethmic groups: Path analyses with two premorbid social competence components. J. Consult. Clin. Psychol. 1978, 46, 1164–1165. [Google Scholar] [CrossRef]
- Kunanitthaworn, N.; Wongpakaran, T.; Wongpakaran, N.; Paiboonsithiwong, S.; Songtrijuck, N.; Kuntawong, P.; Wedding, D. Factors associated with motivation in medical education: A path analysis. BMC Med. Educ. 2018, 18, 140. [Google Scholar] [CrossRef]
- Xia, Y.; Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behav. Res. Methods 2019, 51, 409–428. [Google Scholar] [CrossRef]
- Lassen, K.; Coolsen, M.M.; Slim, K.; Carli, F.; de Aguilar-Nascimento, J.E.; Schafer, M.; Parks, R.W.; Fearon, K.C.; Lobo, D.N.; Demartines, N.; et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin. Nutr. 2012, 31, 817–830. [Google Scholar] [CrossRef]
- Weinberg, L.; Wong, D.; Karalapillai, D.; Pearce, B.; Tan, C.O.; Tay, S.; Christophi, C.; McNicol, L.; Nikfarjam, M. The impact of fluid intervention on complications and length of hospital stay after pancreaticoduodenectomy (Whipple’s procedure). BMC Anesthesiol. 2014, 14, 35. [Google Scholar] [CrossRef]
- Williams, G.A.; Liu, J.; Chapman, W.C.; Hawkins, W.G.; Fields, R.C.; Sanford, D.E.; Doyle, M.B.; Hammill, C.W.; Khan, A.S.; Strasberg, S.M. Composite length of stay, an outcome measure of postoperative and readmission length of stays in pancreatoduodenectomy. J. Gastrointest. Surg. 2020, 24, 2062–2069. [Google Scholar] [CrossRef]
- Stethen, T.W.; Ghazi, Y.A.; Heidel, R.E.; Daley, B.J.; Barnes, L.; Patterson, D.; McLoughlin, J.M. Walking to recovery: The effects of missed ambulation events on postsurgical recovery after bowel resection. J. Gastrointest. Oncol. 2018, 9, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Ali, J.; Weisel, R.D.; Layug, A.B.; Kripke, B.J.; Hechtman, H.B. Consequences of postoperative alterations in respiratory mechanics. Am. J. Surg. 1974, 128, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.; Li, H.C.; Liang, J.T.; Lai, I.R.; Purnomo, J.D.T.; Yang, Y.T.; Lin, B.R.; Huang, J.; Yang, C.Y.; Tien, Y.W.; et al. Effect of a modified hospital elder life program on delirium and length of hospital stay in patients undergoing abdominal surgery: A cluster randomized clinical trial. JAMA Surg. 2017, 152, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Ni, C.Y.; Wang, Z.H.; Huang, Z.P.; Zhou, H.; Fu, L.J.; Cai, H.; Huang, X.X.; Yang, Y.; Li, H.F.; Zhou, W.P. Early enforced mobilization after liver resection: A prospective randomized controlled trial. Int. J. Surg. 2018, 54, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Fagevik Olsen, M.; Becovic, S.; Dean, E. Short-term effects of mobilization on oxygenation in patients after open surgery for pancreatic cancer: A randomized controlled trial. BMC Surg. 2021, 21, 185. [Google Scholar] [CrossRef]
- Allen, C.; Glasziou, P.; Del Mar, C. Bed rest: A potentially harmful treatment needing more careful evaluation. Lancet 1999, 354, 1229–1233. [Google Scholar] [CrossRef]
- Story, S.K.; Chamberlain, R.S. A comprehensive review of evidence-based strategies to prevent and treat postoperative ileus. Dig. Surg. 2009, 26, 265–275. [Google Scholar] [CrossRef]
- Rivas, E.; Cohen, B.; Pu, X.; Xiang, L.; Saasouh, W.; Mao, G.; Minko, P.; Mosteller, L.; Volio, A.; Maheshwari, K.; et al. Pain and opioid consumption and mobilization after surgery: Post hoc analysis of two randomized trials. Anesthesiology 2022, 136, 115–126. [Google Scholar] [CrossRef]
- Grass, F.; Pache, B.; Martin, D.; Addor, V.; Hahnloser, D.; Demartines, N.; Hubner, M. Feasibility of early postoperative mobilisation after colorectal surgery: A retrospective cohort study. Int. J. Surg. 2018, 56, 161–166. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).