Early Ambulation Shortened the Length of Hospital Stay in ICU Patients after Abdominal Surgery
Abstract
:1. Introduction
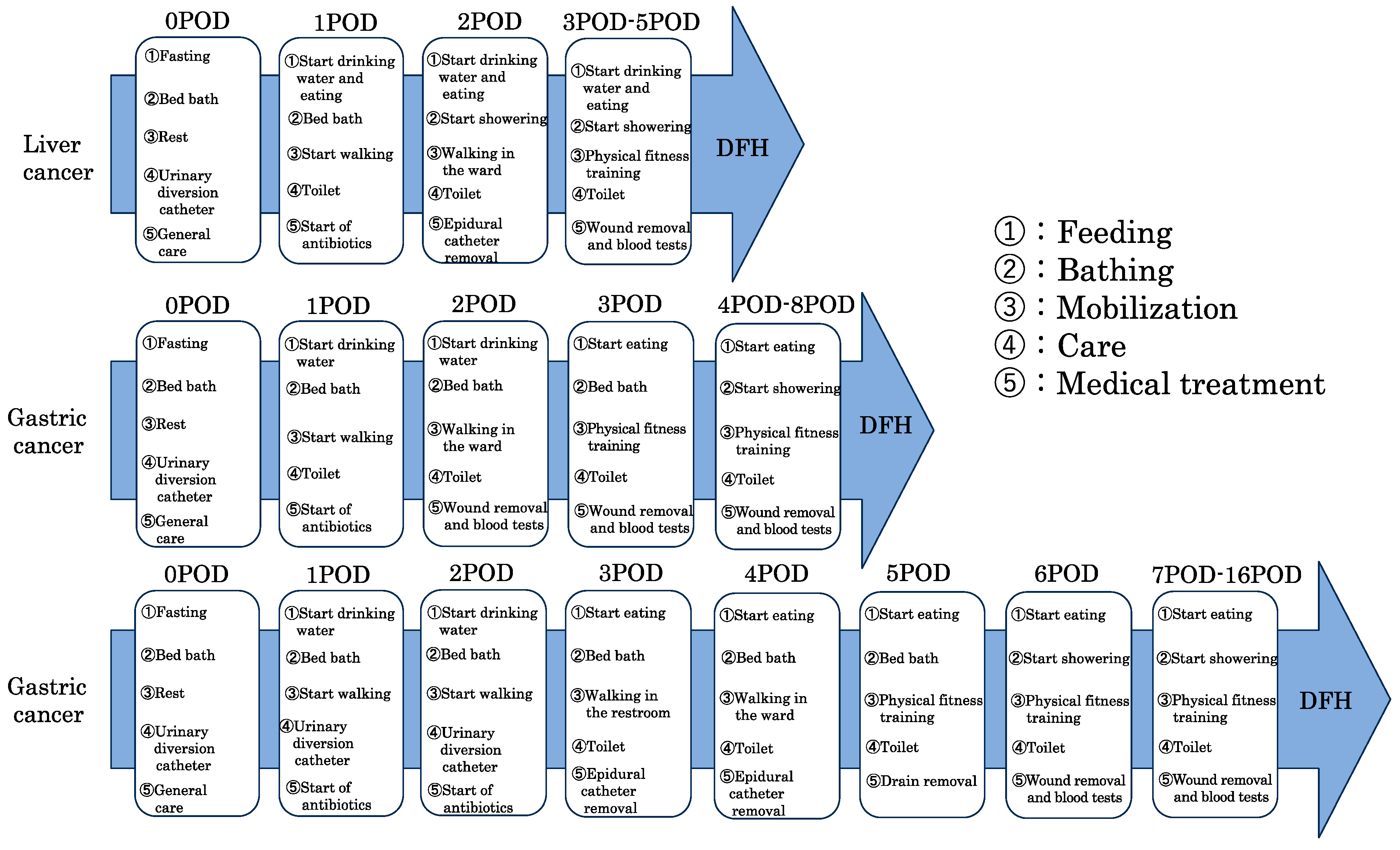
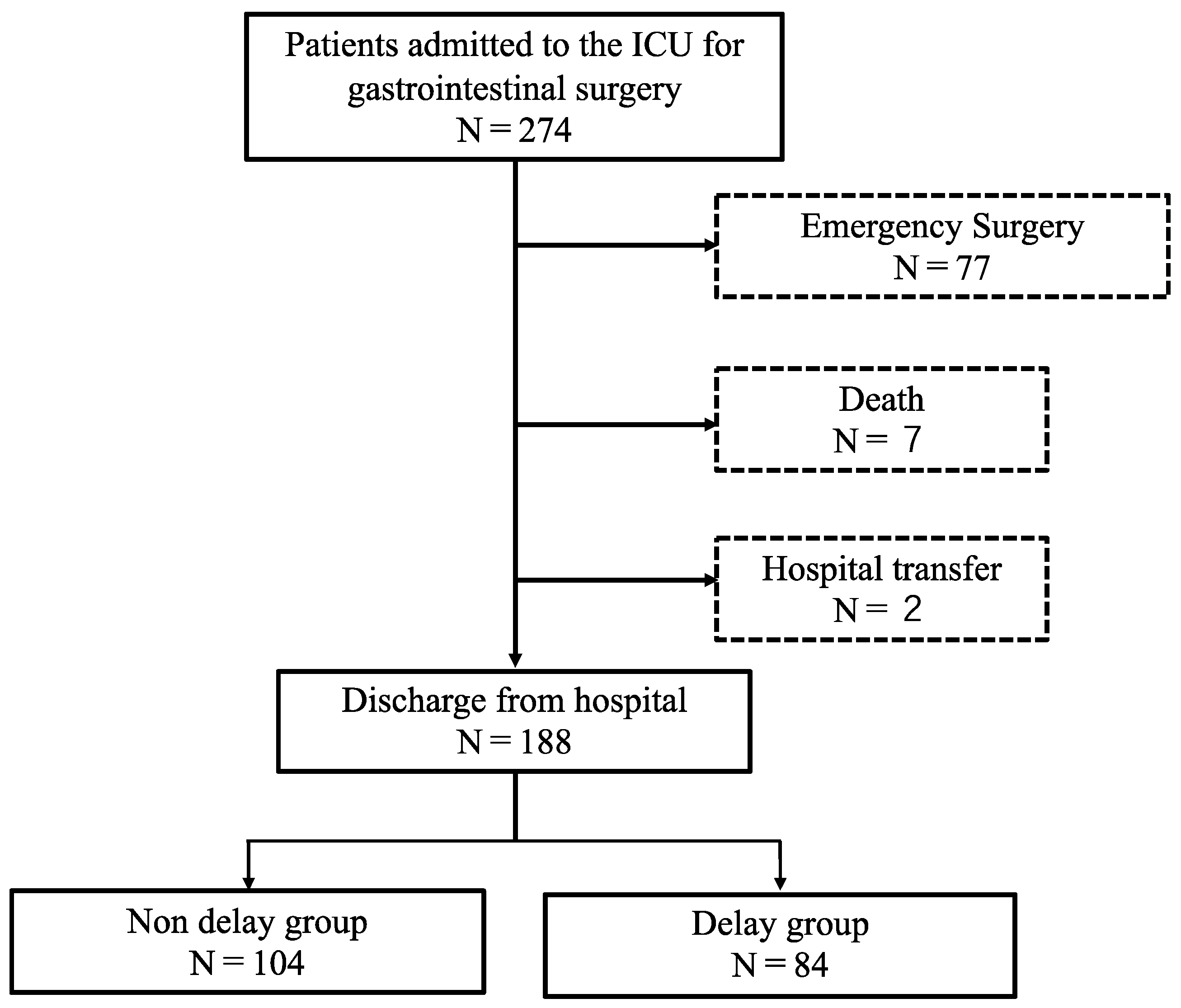
2. Materials and Methods
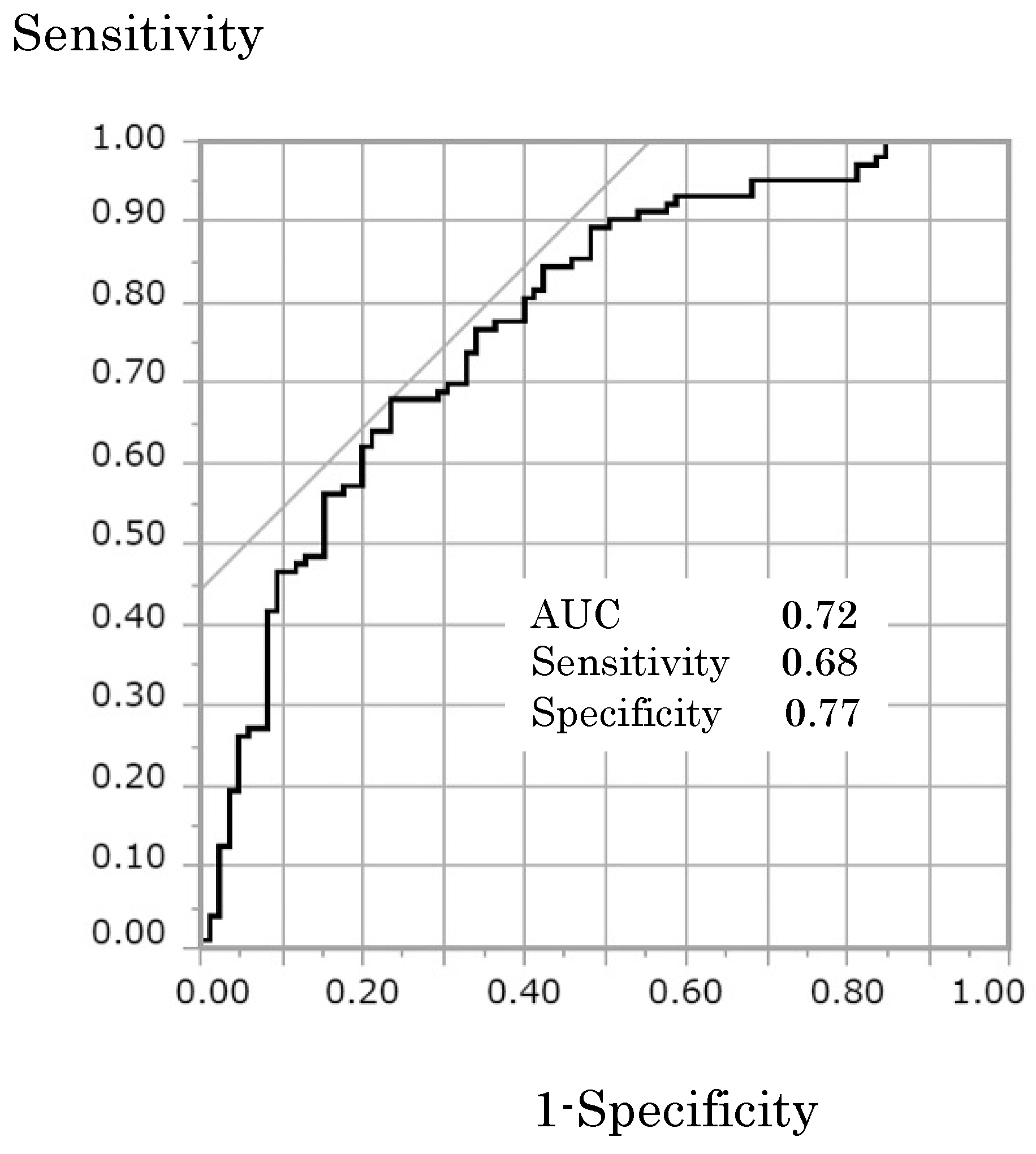
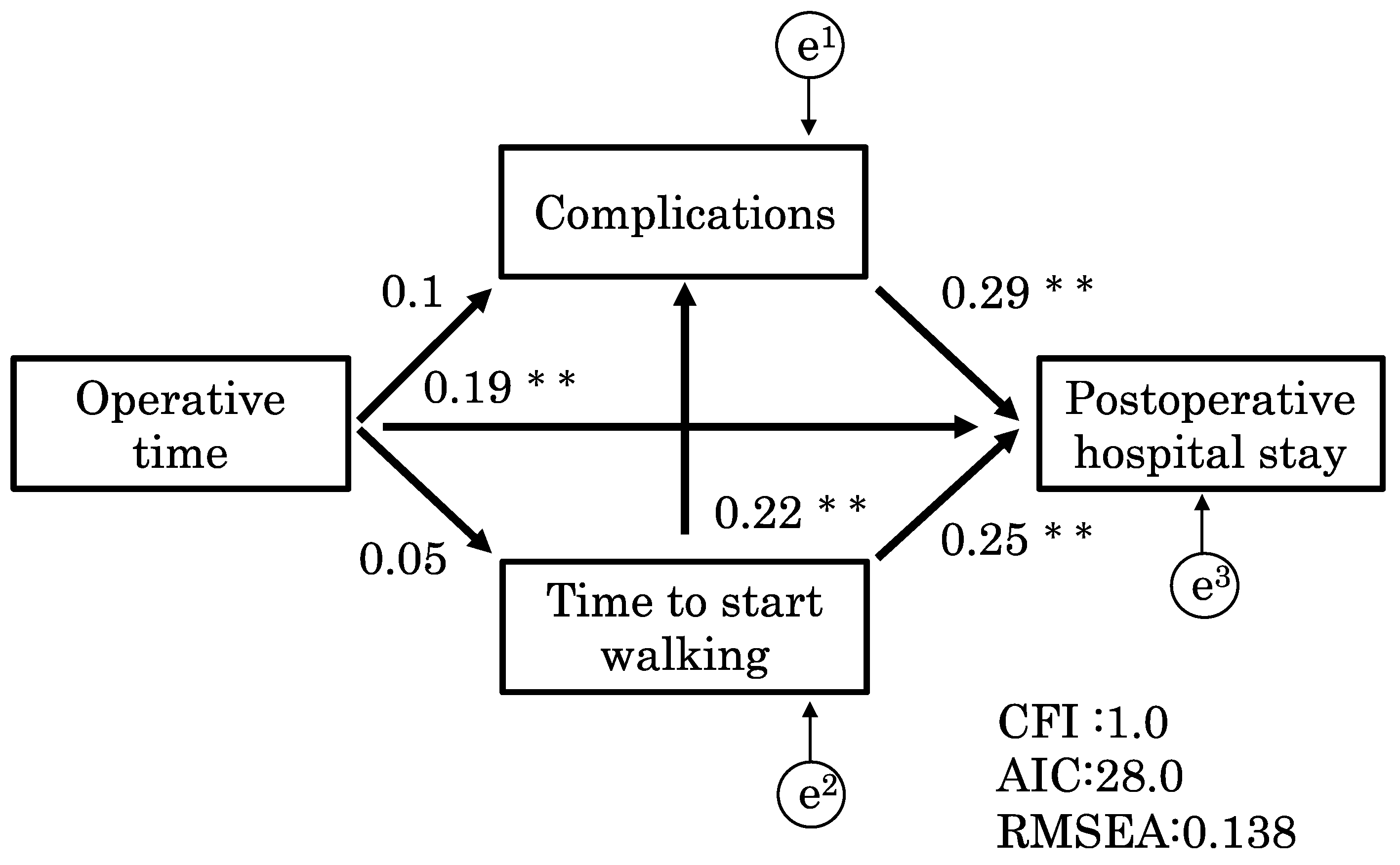
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kramer, C.L. Intensive care unit-acquired weakness. Neurol. Clin. 2017, 35, 723–736. [Google Scholar] [CrossRef]
- Denehy, L.; Lanphere, J.; Needham, D.M. Ten reasons why ICU patients should be mobilized early. Intensive Care Med. 2017, 43, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Tazreean, R.; Nelson, G.; Twomey, R. Early mobilization in enhanced recovery after surgery pathways: Current evidence and recent advancements. J. Comp. Eff. Res. 2022, 11, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Amari, T.; Hirukawa, C.; Fukuda, T.; Hidaka, Y.; Makita, Y.; Fukuda, K.; Sakamoto, Y.; Kimura, M.; Yamaguchi, K. Factors affecting the length of hospital days after laparoscopic gastrectomy for elderly patients with gastric cancer. J. Gastrointest. Cancer 2022, 53, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Hu, W.; Cai, Z.; Liu, J.; Wu, J.; Deng, Y.; Yu, K.; Chen, X.; Zhu, L.; Ma, J.; et al. Early mobilization of critically ill patients in the intensive care unit: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0223185. [Google Scholar] [CrossRef] [PubMed]
- Schweickert, W.D.; Kress, J.P. Implementing early mobilization interventions in mechanically ventilated patients in the ICU. Chest 2011, 140, 1612–1617. [Google Scholar] [CrossRef] [PubMed]
- Fearon, K.C.; Ljungqvist, O.; Von Meyenfeldt, M.; Revhaug, A.; Dejong, C.H.; Lassen, K.; Nygren, J.; Hausel, J.; Soop, M.; Andersen, J.; et al. Enhanced recovery after surgery: A consensus review of clinical care for patients undergoing colonic resection. Clin. Nutr. 2005, 24, 466–477. [Google Scholar] [CrossRef]
- Munitiz, V.; Martinez-de-Haro, L.F.; Ortiz, A.; Ruiz-de-Angulo, D.; Pastor, P.; Parrilla, P. Effectiveness of a written clinical pathway for enhanced recovery after transthoracic (Ivor Lewis) oesophagectomy. Br. J. Surg. 2010, 97, 714–718. [Google Scholar] [CrossRef]
- Bagshaw, S.M.; Webb, S.A.; Delaney, A.; George, C.; Pilcher, D.; Hart, G.K.; Bellomo, R. Very old patients admitted to intensive care in Australia and New Zealand: A multi-centre cohort analysis. Crit. Care 2009, 13, R45. [Google Scholar] [CrossRef]
- Docherty, A.B.; Anderson, N.H.; Walsh, T.S.; Lone, N.I. Equity of access to critical care among elderly patients in Scotland: A national cohort study. Crit. Care Med. 2016, 44, 3–13. [Google Scholar] [CrossRef]
- Nielsson, M.S.; Christiansen, C.F.; Johansen, M.B.; Rasmussen, B.S.; Tonnesen, E.; Norgaard, M. Mortality in elderly ICU patients: A cohort study. Acta Anaesthesiol. Scand. 2014, 58, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Melloul, E.; Lassen, K.; Roulin, D.; Grass, F.; Perinel, J.; Adham, M.; Wellge, E.B.; Kunzler, F.; Besselink, M.G.; Asbun, H.; et al. Guidelines for perioperative care for pancreatoduodenectomy: Enhanced recovery after surgery (ERAS) recommendations 2019. World J. Surg. 2020, 44, 2056–2084. [Google Scholar] [CrossRef] [PubMed]
- Harrison, O.J.; Smart, N.J.; White, P.; Brigic, A.; Carlisle, E.R.; Allison, A.S.; Ockrim, J.B.; Francis, N.K. Operative time and outcome of enhanced recovery after surgery after laparoscopic colorectal surgery. JSLS 2014, 18, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Yao, Y.; Zhou, J.; Diao, X.; Chen, H.; Cai, K.; Ma, X.; Wang, S. Dynamic APACHE II score to predict the outcome of intensive care unit patients. Front. Med. 2021, 8, 744907. [Google Scholar] [CrossRef] [PubMed]
- Costello, R.M. Premorbid social competence construct generalizability across ethmic groups: Path analyses with two premorbid social competence components. J. Consult. Clin. Psychol. 1978, 46, 1164–1165. [Google Scholar] [CrossRef]
- Kunanitthaworn, N.; Wongpakaran, T.; Wongpakaran, N.; Paiboonsithiwong, S.; Songtrijuck, N.; Kuntawong, P.; Wedding, D. Factors associated with motivation in medical education: A path analysis. BMC Med. Educ. 2018, 18, 140. [Google Scholar] [CrossRef]
- Xia, Y.; Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behav. Res. Methods 2019, 51, 409–428. [Google Scholar] [CrossRef]
- Lassen, K.; Coolsen, M.M.; Slim, K.; Carli, F.; de Aguilar-Nascimento, J.E.; Schafer, M.; Parks, R.W.; Fearon, K.C.; Lobo, D.N.; Demartines, N.; et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin. Nutr. 2012, 31, 817–830. [Google Scholar] [CrossRef]
- Weinberg, L.; Wong, D.; Karalapillai, D.; Pearce, B.; Tan, C.O.; Tay, S.; Christophi, C.; McNicol, L.; Nikfarjam, M. The impact of fluid intervention on complications and length of hospital stay after pancreaticoduodenectomy (Whipple’s procedure). BMC Anesthesiol. 2014, 14, 35. [Google Scholar] [CrossRef]
- Williams, G.A.; Liu, J.; Chapman, W.C.; Hawkins, W.G.; Fields, R.C.; Sanford, D.E.; Doyle, M.B.; Hammill, C.W.; Khan, A.S.; Strasberg, S.M. Composite length of stay, an outcome measure of postoperative and readmission length of stays in pancreatoduodenectomy. J. Gastrointest. Surg. 2020, 24, 2062–2069. [Google Scholar] [CrossRef]
- Stethen, T.W.; Ghazi, Y.A.; Heidel, R.E.; Daley, B.J.; Barnes, L.; Patterson, D.; McLoughlin, J.M. Walking to recovery: The effects of missed ambulation events on postsurgical recovery after bowel resection. J. Gastrointest. Oncol. 2018, 9, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Ali, J.; Weisel, R.D.; Layug, A.B.; Kripke, B.J.; Hechtman, H.B. Consequences of postoperative alterations in respiratory mechanics. Am. J. Surg. 1974, 128, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.; Li, H.C.; Liang, J.T.; Lai, I.R.; Purnomo, J.D.T.; Yang, Y.T.; Lin, B.R.; Huang, J.; Yang, C.Y.; Tien, Y.W.; et al. Effect of a modified hospital elder life program on delirium and length of hospital stay in patients undergoing abdominal surgery: A cluster randomized clinical trial. JAMA Surg. 2017, 152, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Ni, C.Y.; Wang, Z.H.; Huang, Z.P.; Zhou, H.; Fu, L.J.; Cai, H.; Huang, X.X.; Yang, Y.; Li, H.F.; Zhou, W.P. Early enforced mobilization after liver resection: A prospective randomized controlled trial. Int. J. Surg. 2018, 54, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Fagevik Olsen, M.; Becovic, S.; Dean, E. Short-term effects of mobilization on oxygenation in patients after open surgery for pancreatic cancer: A randomized controlled trial. BMC Surg. 2021, 21, 185. [Google Scholar] [CrossRef]
- Allen, C.; Glasziou, P.; Del Mar, C. Bed rest: A potentially harmful treatment needing more careful evaluation. Lancet 1999, 354, 1229–1233. [Google Scholar] [CrossRef]
- Story, S.K.; Chamberlain, R.S. A comprehensive review of evidence-based strategies to prevent and treat postoperative ileus. Dig. Surg. 2009, 26, 265–275. [Google Scholar] [CrossRef]
- Rivas, E.; Cohen, B.; Pu, X.; Xiang, L.; Saasouh, W.; Mao, G.; Minko, P.; Mosteller, L.; Volio, A.; Maheshwari, K.; et al. Pain and opioid consumption and mobilization after surgery: Post hoc analysis of two randomized trials. Anesthesiology 2022, 136, 115–126. [Google Scholar] [CrossRef]
- Grass, F.; Pache, B.; Martin, D.; Addor, V.; Hahnloser, D.; Demartines, N.; Hubner, M. Feasibility of early postoperative mobilisation after colorectal surgery: A retrospective cohort study. Int. J. Surg. 2018, 56, 161–166. [Google Scholar] [CrossRef]

| Surgical Site | Surgery | Participants, No. | Hospital Length of Stay, Days (Quartile Range) |
|---|---|---|---|
| Upper digestive tube surgery (N = 23) 12% | Laparoscopic gastrectomy | 11 | 14 (10.8–30.5) |
| Thoracoscopic laparoscopic esophageal extraction | 10 | 20.5 (16.3–26.3) | |
| Open gastrectomy | 2 | 11 | |
| Lower digestive tube surgery (N = 28) 15% | Laparoscopic rectal resection | 9 | 21 (11–41.5) |
| Laparoscopic S-shaped colectomy | 9 | 16 (10–31) | |
| Laparoscopic colectomy | 4 | 18 (7.5–32) | |
| Laparoscopic ileal resection | 3 | 6 | |
| Open rectal resection | 2 | 15.5 (11–20) | |
| Open colectomy | 1 | 21 | |
| Bile duct pancreas surgery (N = 137) 73% | Laparoscopic hepatectomy | 78 | 8.5 (7–13.3) |
| Pancreatic head and duodenectomy | 47 | 22 (14.8–42.3) | |
| Caudal pancreatectomy | 5 | 44 (32–65) | |
| Central pancreatectomy | 2 | 28.5 (10–47) | |
| Other choledochopancreatic surgery | 5 | 23 (11–59) |
| Characteristics | Nondelayed Group | Delayed Group | p-Value |
|---|---|---|---|
| Age | 70.2 ± 0.9 | 72.8 ± 1.1 | 0.07 |
| Diagnosis | |||
| Liver cancer | 60 | 17 | 0.01 ** |
| Pancreatic cancer | 7 | 27 | |
| Gastric cancer | 11 | 6 | |
| Colorectal cancer | 4 | 8 | |
| Esophageal cancer | 4 | 6 | |
| Bile duct cancer | 6 | 9 | |
| Other | 12 | 9 | |
| Tumor stage | |||
| 0 | 4 | 2 | 0.15 |
| Ⅰ | 0 | 0 | |
| Ⅱ | 15 | 7 | |
| Ⅲ | 78 | 66 | |
| Ⅳ | 7 | 9 | |
| BMI (%) a | 22.9 ± 0.3 | 22.1 ± 0.4 | 0.12 |
| Operative time (min) | 362.3 ± 16.2 | 434.6 ± 17.6 | 0.01 ** |
| Amount of blood loss (mL) | 331.6 ± 72.4 | 575.3 ± 78.6 | 0.02 * |
| Complications (N) | 7 | 34 | 0.01 ** |
| Delirium | 3 | 3 | – |
| Intestinal obstruction | 1 | 4 | |
| Atelectasis | 2 | 4 | |
| Pneumonia | 1 | 8 | |
| Decreased appetite caused by decreased activity | 0 | 1 | |
| Pancreatic fistula | 0 | 11 | |
| Rupture of false aneurysm | 0 | 3 | |
| APACHE II score b | 10.3 ± 0.2 | 10.9 ± 0.5 | 0.24 |
| %VC c | 103.6 ± 2.1 | 100.4 ± 2.2 | 0.29 |
| Postoperative hospital stay | 9.53 ± 2.29 | 39.9 ± 2.5 | 0.01 ** |
| Complications (yes/no) | 7/96 | 18/67 | 0.01 ** |
| Time to ambulation (min) | 2100.6 ± 224.9 | 3132.4 ± 247.1 | 0.01 ** |
| Time to wheelchair sitting (min) | 1704.9 ± 108.9 | 1943.6 ± 120.4 | 0.14 |
| Time to sitting upright (min) | 1343.6 ± 75.1 | 1511.3 ± 82.9 | 0.14 |
| Time to standing from bed (min) | 1083.9 ± 26.3 | 1055.1 ± 29.2 | 0.64 |
| p-Value | Odds Ratio | 95% CI | ||
|---|---|---|---|---|
| Upper Limit | Lower Limit | |||
| %VC | 0.17 | 1.01 | 1.023 | 0.998 |
| Time to sitting upright | 0.94 | 1.00 | 1.010 | 0.999 |
| Time to ambulation | 0.01 ** | 0.99 | 0.993 | 0.999 |
| Complications | 0.01 ** | 0.14 | 0.345 | 0.054 |
| Operative time | 0.05 * | 0.99 | 0.999 | 0.994 |
| Postoperative Hospital Stay | Operative Time | Complication | Time to Ambulation | |
|---|---|---|---|---|
| Postoperative hospital stay (days) | - | 0.24 ** | 0.43 ** | 0.27 ** |
| Operative time (min) | 0.24 ** | - | 0.12 | 0.07 |
| Complications | 0.43 ** | 0.12 | - | 0.17 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amari, T.; Matta, D.; Makita, Y.; Fukuda, K.; Miyasaka, H.; Kimura, M.; Sakamoto, Y.; Shimo, S.; Yamaguchi, K. Early Ambulation Shortened the Length of Hospital Stay in ICU Patients after Abdominal Surgery. Clin. Pract. 2023, 13, 1612-1623. https://doi.org/10.3390/clinpract13060141
Amari T, Matta D, Makita Y, Fukuda K, Miyasaka H, Kimura M, Sakamoto Y, Shimo S, Yamaguchi K. Early Ambulation Shortened the Length of Hospital Stay in ICU Patients after Abdominal Surgery. Clinics and Practice. 2023; 13(6):1612-1623. https://doi.org/10.3390/clinpract13060141
Chicago/Turabian StyleAmari, Takashi, Daiki Matta, Yukiho Makita, Kyosuke Fukuda, Hiroki Miyasaka, Masami Kimura, Yuta Sakamoto, Satoshi Shimo, and Kenichiro Yamaguchi. 2023. "Early Ambulation Shortened the Length of Hospital Stay in ICU Patients after Abdominal Surgery" Clinics and Practice 13, no. 6: 1612-1623. https://doi.org/10.3390/clinpract13060141
APA StyleAmari, T., Matta, D., Makita, Y., Fukuda, K., Miyasaka, H., Kimura, M., Sakamoto, Y., Shimo, S., & Yamaguchi, K. (2023). Early Ambulation Shortened the Length of Hospital Stay in ICU Patients after Abdominal Surgery. Clinics and Practice, 13(6), 1612-1623. https://doi.org/10.3390/clinpract13060141






