Abstract
Background: Scars affect patients after trauma, burns, or surgical procedures and can generate both physical and psychosocial changes. The aesthetic damage represents the modification of a person’s physical appearance, in its bodily integrity, causing numerous sufferings and determining social or economic consequences. The aim of this research is to evaluate the advantages and disadvantages offered by the available psychosocial and physical scar scales in assessing the physical, aesthetic, psychosocial, and juridical consequences of scars. This will aid to inform medical examiners about the most valued existing scales to allow them to select the most appropriate instrument to manage their patient. Methods: A broad search of relevant scientific studies on the psychosocial determinants of post-traumatic and surgical scars was conducted by using the following international database tools: PsycINFO, MedLine Social Science Index, Scopus, Web of Science, published from 1960 until 2022. Results: We analyzed 63 scientific studies to assess the advantages and limits of several psychometric and physical scar evaluation scales. Conclusions: The researchers analyzed in this review highlight the advantages and limitation of existing instruments, evidencing the demand for future scar evaluation instruments and a scar-assessing algorithm that takes into account the physical, aesthetic, psychosocial, and legal consequences of scars.
1. Introduction
Traumas on the skin and mucous membranes, burns, or surgical procedures are healed by scarring, which may generate physical and psychosocial changes as well [1,2,3,4]. Several modalities have been developed to quantify scars in order to establish the response to treatment and to evaluate the physical component of the results, but the psychological component is little studied [5,6]. The most used scar assessment scales are the Vancouver Scar Scale (VSS) and Patient and Observer Scar Assessment Scale (POSAS) [7,8]. Scar measuring scales have difficulties in assessing the role of mental suffering induced by the process of their formation, which sometimes generates a change in the physiognomy or even alters the victim’s aesthetic perception of his/her own body. There are multiple consequences of scars such as pain, itching, aesthetic discomfort, and prejudice, or even functional impairment, mainly in the periarticular surface, that can determine physical, aesthetic, psychosocial, and juridic repercussions. Many studies refer only to the epidemiology and management of scars, while very few are interested in developing methods to objectify the consequences of scars [9]. Scar management should be approached by taking into account five main areas of impact on patients’ needs: physical comfort and function; acceptability for himself and others; social integration; trust in the healing process; emotional well-being. Medical staff should be available to develop proper management and help to reduce patient suffering [10]. One juridical repercussion is the aesthetic damage that represents the changes of a person’s physical appearance, in its bodily integrity, which causes numerous sufferings and which will have social or economic consequences [11,12,13]. Moreover, scars remain a trauma marker that represent an element of identification of a person, provides information about the nature of the weapon that cased it, the age of the scar, and can be used as evidence in court [14,15]. However, the individual can adopt coping behavior toward the scar-triggering event without affecting their body image and relationships with others through internalization of the scar [11]. If touching or observing the scar constantly reminds the person of the traumatic event and negatively influences their daily activities, it is considered that the patients have not internalized the scar and need a medico-legal examination [16]. Some psychosocial effects of scars are described by public or social stigma that occurs when a society has a belief about a certain group of people, resulting in a negative emotional impact and/or discrimination, feelings of hopelessness, fear, loss of identity, low self-esteem, guilt, isolation, anxiety, and depression [17,18]. Depression and post-traumatic stress disorder were evidenced in 13–45% of cases according to scientific studies in patients with burns [19]. Social problems include difficulties in sexual life and social interactions. The quality of life appears to be initially lower in scarred patients compared to the general population [20]. The main objective of plastic surgeons and dermatologists should be the improvement of the scar’s appearance and therefore to enhance the patient’s well-being. The medical examiner should refer the patient to plastic surgery to correct the physical aspects of the scar and to follow the patient’s evolution over time to decide if the patient has internalized the scar or if there is an aesthetic damage [21,22].
The aim of this research is to evaluate the advantages and disadvantages offered by the available psychosocial and physical scar scales in assessing their physical, aesthetic, psychosocial, and juridical consequences. This will aid to inform medical examiners about the most valued existing scales to allow them to select the most appropriate instrument to manage their patient.
2. Methods
A broad search of relevant scientific studies on the psychosocial determinants of post-traumatic and surgical scars was conducted by using international database tools: PsycINFO, MedLine Social Science Index, Scopus, Web of Science. We researched these databases for articles published from 1960 until 2022 discussing psychosocial and physical scales which are still in use. Keywords included in the process of surveying the specialized literature were as follows: psychosocial scar scale, physical scar scale, hopelessness depression, social support scale, aesthetic prejudice, scar consequences. An important step was to establish the selection criteria for the inclusion and exclusion of the studies identified in the international specialized literature. The articles were introduced in Microsoft Excel, then sorted by title and author’s name; duplicates were removed semiautomatically. Inclusion criteria were as follows: systematic reviews and literature reviews, and full text original articles, published in English in international journals as full text that measure the appraisal of surgical and traumatic scars, and developed and validated tools in the surgical and traumatic scar population. Exclusion criteria for the study were as follows: qualitative studies that reported data on scarring in children, studies that did not contain a comparison group, studies that were not published in English, conference abstracts, and case reports.
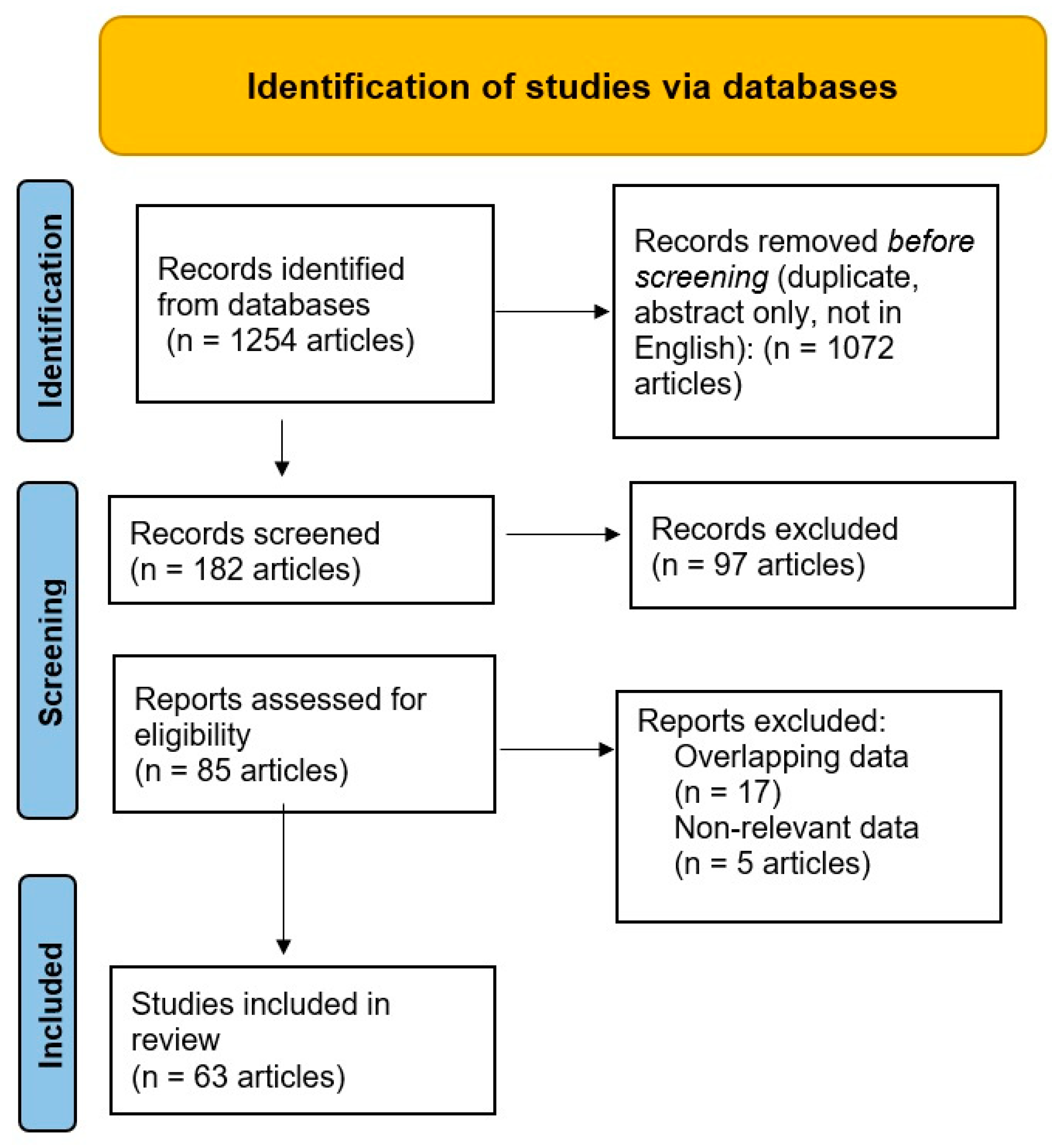
The review identified 1254 articles in the employed databases; of them, 1072 were removed before screening, Figure 1. Throughout the screening process, the remaining 182 articles were manually reviewed by GMM, and further assessed by another two authors (ANC and FM). As a consequence, the other 97 records were excluded (no full-text available in English, modified version of scar rating scale). The remaining 85 articles were reanalyzed, and after excluding another 22, the remaining 63 articles were included in this review. The GMM performed the final manual selection of the studies we analyzed.
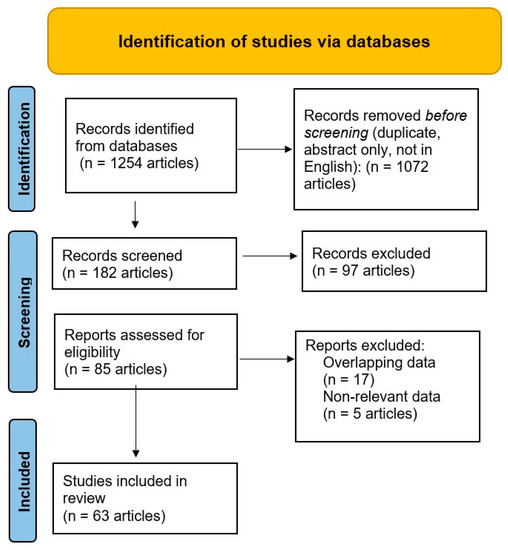
Figure 1.
PRISMA flow diagram of the selection of medical articles [23].
3. Results
Aiming to synthetize the information gathered from the 63 analyzed scientific articles, of which 8 were meta-analyses, 8 reviews, and 47 original articles, we divided them into three categories depending on the type of employed scales: physical, psychosocial, and combined methodology. The tables were structured based on the year of publication of the presented scales, starting with the most recent one.
3.1. Scales for Physical Assessment of Scars
The scales that evaluate the morphological characteristics of scars were designed to assess their appearance in response to the treatment, but these scales are observer-dependent, most of them only considering clinical aspects such as scar height or thickness, surface, texture, flexibility, vascularity, and pigmentation (Table 1). The scar rating scales are frequently used in scientific research and are beneficial for the study of small, linear scars, the main disadvantage being the minimal utility of evaluating large scars and their functional effects [24].

Table 1.
Scales for physical assessment of scars.
One of the first methods, the esthetic method, was proposed by Greff and Hodin, and quantifies the aesthetic damage according to the morphological characteristics of the scar. It is a laborious method, difficult to be utilized because it divides the face into 122 facial sectors, but a lesion can affect one or more sectors. To determine the degree of disfigurement, each sector is scored according to several coefficients, then a calculation is made for all affected sectors. The aesthetic coefficient (Cs) is calculated by multiplying the value of each coefficient for each affected sector, the total aesthetic coefficient (Ct) resulting from the sum of all aesthetic coefficients for the affected sectors. The maximum aesthetic deficit is 100% and corresponds to a total destruction of the face. The main counter-arguments for the use of the esthetic method are as follows: the division of the face into too many sectors (122), to which the associated parameters are added; the role of the forensic doctor in assessing the damage could be replaced by entering the data into an image processing software with the exact calculation of the damage according to the parameters introduced and analyzed; it does not quantify all body areas [50,51].
VSS, also called the Burn Scar Index, a method of measuring scars first described by Sullivan in 1990 [41], is probably the most recognized method of evaluating scars formed after burns. The VSS is a scale that assesses risk factors for the development of hypertrophic scars and the effectiveness of their treatment. This scale analyzes scar vascularity, pigmentation, foldability, and height to diagnose hypertrophic scars [43,44].
POSAS, proposed by Draaijers et al. [28] in 2004, allows a structured clinical evaluation of scar quality, reflecting both the observer’s and the patient’s opinions. This tool has been shown to be consistent and reliable for burn scars. The characteristics of scars such as vascularity, pigmentation, firmness, pliability, affected area, and scar height are scored. The POSAS is a standardized and validated instrument in the clinical, objective assessment of scars, also taking into account the patient’s symptoms related to the scar, such as pain and pruritus, which were not considered in previous scales [29,52].
3.2. Psychometric Scales for the Assessment of Scars
The psychosocial components and consequences of the presence of a scar are represented by the internalization of this particular scar, the social significance of the aesthetic injury, its experiences, the perceived social and family support at the time of the traumatic event, and the stage of personality development [16]. By inserting these psychosocial considerations that guide scar treatment decisions, future scar assessment tools can accomplish far more than characterizing the clinical aspects of scars (Table 2) [47].

Table 2.
Psychometric scales for the assessment of scars.
MPIS was validated in 2021 following a study including 204 participants presenting scars. The lot, aged between 18 to 81 years old, was split into two groups, of which 105 were women and 99 men. Each individual had to answer 15 questions marked from 1 (not agree) to 5 (totally agree) using the Likert scale. Therefore, the MPIS score was a total sum anywhere between 15 to 75. Moreover, proved to have a good consistency (Cronbach, 0.943), the scale highlights the individual’s scar awareness, gender, the morphological aspect of the scar, as well as its social and professional impact on the affected patients [16].
Developed by Zimet, Dahlem, Zimet, and Farley, (1988), MSPSS comprises 12 items based on 3 main factors, such as family, friends, and significant people, each item being designed according to the above factors. Showing a high internal consistency (alfa Cronbach 0.91) [58], the scale was built to reflect the highest social support known based on the highest scoring.
HDSQ (Metalsky and Joiner,1997) was introduced to help monitor hopelessness depression [62]. The tool is based on 32 items, allowing the examiner to observe various symptoms on individuals. HDSQ’s structure is similar to DBI’s, where each symptom is measured in a group of four items. Therefore, the tool totals a number of eight subscales (Motivational Deficit—retarded initiation of voluntary responses, Interpersonal dependency, Psychomotor retardation, lack of energy, Apathy/anhedonia, Insomnia, Concentration difficulty and Suicidality), each element including four items, each measuring a different symptom of hopelessness depression. The above scale showed a high internal consistency (alfa Cronbach 0.70 and 0.93) [62,63].
3.3. Scales for Physical and Psychosocial Assessment of Scars
The Scar-Q Aesthetics is a new tool that evaluates all types of scars, consisting of three subscales: the appearance scale (19 items) that assesses size, width, color, and contour of scar; the scar symptoms scale (17 items); and the psychosocial impact scale (12 items). Each part is a set of items with 4-point responses (1 = most favorable–4 = least favorable). The sum of the items measures each subscale. If the patients have more than one scar, instructions elucidate that the answer should be thinking about the scar that bothers them the most (Table 3) [66].

Table 3.
Scales for Physical and Psychosocial Assessment of Scars.
PSAQ is a valid measure developed by Durani et al. in 2009. This reliable measure took into account physical, aesthetic, and psychosocial consequences of surgical scars. Except the Symptoms subscale, the other four subscales indicated a high internal consistency (Cronbach α, 0.73 to 0.93) [72].
4. Discussion
It is highly important that the scales for scar evaluation should be well known by clinicians considering the multiple morpho-functional, aesthetic, psycho-social, and legal consequences of scars. Acknowledging the benefits and downsides of these scales could help clinicians choose the most appropriate method of approach.
The aesthetic method derived from Greff’s and Hodin’s methods [50], VSS [41], MSS [33], and SBSES [24] analyzes the morpho-functional and topographic aspect of the scars; POSAS additionally assesses pain and itching symptoms. The POSAS is a standardized and validated instrument in the clinical, objective assessment of burn scars, also taking into account patient symptoms related to the scar, such as pain and pruritus, which were not considered in previous scales [28]. The VSS is a scale that assesses risk factors for the development of hypertrophic scars and the effectiveness of treatment on burn scars [41,69]. The disadvantage of these clinical tools is the lack of a psychosocial and juridical component in assessing scars. The Hamilton Scale [37] and SSS [39] assess scars through photographs.
The evaluation of the aesthetic prejudice remains a component of the medical examiner’s activity where the expected criteria are insufficiently outlined as a consequence of the weight of the subjective elements related to the traumatized victim. The difficulties reside in the fact that moral suffering cannot be objectively evaluated, which causes impediments in the stability of the compensation value to those qualified [51]. The aesthetic method derived from Greff’s and Hodin’s method, used to establish the aesthetic damage, presents multiple limitations (the division of the face in 122 sectors plus associated parameters, lack of interpretation of the result) [11,50]. MPIS includes the psycho-social component in scar evaluation in its legal aspect, making the obtained scale score influence the existence of aesthetic damage, disfigurement, and scar internalization [16]. To internalize the scar more easily, people try to hide the scar; this makes them unsociable and interferes with their communication skills, personal relationships, professional life, and agreed activities [11,16].
Scars can negatively affect body image and self-confidence. Scars have been stigmatized in society since cartoons and horror movies depict them as embodying a bad person. Moreover, scars can also cause functional disorders and have professional and financial repercussions [76,77]. From a physical point of view, people with scars can develop psychiatric conditions manifested by depressive symptoms, anxiety, shame, and sometimes anger and aggression or avoidance behavior. After the occurrence of the traumatic injury, the social support of the family and those close to them is important in order to internalize the scar as easily as possible in order to receive psychological acceptance [78]. Facial scars cause a high level of anxiety and decreased self-confidence [20]. Brown et al. (2010) examined the physical comfort and functionality of patients with scars as well as their confidence, the way they manage their affections, the way they accept themselves and others, their wellbeing, and social interactions. The results showed that more than half of the participants were unhappy with their scar appearance, about 20% of them developed anxiety, and 50% felt their private and intimate relationships were compromised [35]. The above-mentioned psycho-social consequences relate to other studies in which scarred patients felt condemned and labelled, leading them to social isolation, difficulties to adapt in society, and the need to hide their scars [22]. MBSRQ and HDSQ are successfully used in body image research and scar assessment.
Social problems include difficulties in sex life and social interactions. Quality of life appears to be lower in patients with burns compared to the general population. Mental health problems are more significant than physical problems. For many years, quality of life was reported to be quite good [79,80,81]. MSPSS can be used to assess the psychosocial effects of scars, mediating variables such as low social support, avoidant coping styles, and personality traits negatively that affect postburn adjustment [58]. Optimizing adaptation after the formation of post-traumatic scars requires the support of family and friends who promote socialization, acceptance of the scar, and, if necessary, special psychological or psychiatric help. Most studies were conducted using physical assessment scales. However, PSAQ and Scar Q explored the psychosocial components of scars and the notion of recognition and acceptance [66,72].
Kim et al. (2022) published a study in which 60 patients with keloid scars were investigated. The patients completed all three subscales of the SCAR-Q (symptoms, appearance, and psychosocial impact). The study’s aim was to compare pre- and postoperative scar perception. The study showed that the patients felt a significant improvement in all parts of the SCAR-Q [71].
Moreover, a study comparing laparoscopic cholecystectomy to single incision intervention, conducted by Ostlie et al. (2013) across 60 patients, aimed to establish the possible existing cosmetic advantages, analyzing the difference between the two procedures. Each patient was asked to complete a PSAQ survey containing four parts: Appearance, Satisfaction with Appearance, Consciousness, and Satisfaction with Symptoms. The last subscale was omitted from the analysis because of deficient reliability [72]. The results of this research showed that both the appearance and the number of scars is important, the aesthetic benefit favoring the one-site approach. Another study used the PSAQ to evaluate improvements of conscious scar location after breast cancer surgery, comparing the preferred port between arm and chest. In conclusion, although most of the patients were conscious of their scar location, the arm site was preferred rather than the chest [73].
Mundy et al., in a systematic review published in 2016, analyzed four patient-reported outcome (PRO) instruments POSAS, Bock quality of life questionnaire for patients with keloid and hypertrophic scarring (Bock), PSAQ, and patient-reported impact of scars measure (PRISM). All used tools, measured symptoms, and psychosocial aspects of scars; additionally, PSAQ had physical assessment. The limit of this tool was the lack of legal aspect [74].
In this day and age, we are lacking a scale assessment tool that would appreciate all physical, aesthetic, psycho-social, and legal aspects of scars. Following this research, we appreciate that a scar evaluation algorithm containing several scales applied according to the age of the scar (0–6 months and >6 months) would be useful. Firstly, following a plastic surgery clinician review, the injury would be evaluated from a morpho-functional point of view and initial treatment would be commenced. Therefore, SBSES can be used at this stage, having the advantage of cosmetically assessing the outcomes of a wound up to 5–10 days from the injury until the sutures are removed. Moreover, if the injury is located on victim’s face, the Scar-Q scale is recommended, having higher outcomes on facial aesthetic treatments. Secondly, a medical examination will be required to evaluate the gravity of the injury from its legal aspect, to determine the psychological impact, and, therefore, help identify post-traumatic stress disorder (PTSD). HDSQ and MSPSS can be used at this stage to help identify the most appropriate psychological support and ensure an adequate psychological or psychiatric evaluation. Nonetheless, if the scar is more than 6 months old, the plastic clinician could use the POSAS and Scar-Q or PSAQ scales that take into account both patient and observer points of view, plus psychosocial aspects. A further medical legal consultation must be considered to determine the legal repercussions of the scar; however, using MPIS can still aid the internalization of the scar without legal consequences, aesthetic prejudice, or disfigurement with legal repercussions.
5. Conclusions
In the literature, little is known about how scars affect patients’ lives. This review debates the advantages and limitation of some existing instruments, focusing on demand for future a scar instrument development or a scar evaluation algorithm that takes into account the physical, aesthetic, psychosocial, and legal consequences of scars.
Author Contributions
Conceptualization, G.M.M., C.L.B., A.N.C., C.B., G.A., P.M., C.D.C., R.F. and F.M.; methodology, G.M.M., A.N.C. and F.M.; software, G.M.M., A.N.C. and F.M.; validation, G.M.M., C.L.B., A.N.C., C.B., G.A., P.M., C.D.C., R.F. and F.M.; formal analysis, G.M.M., A.N.C. and F.M.; investigation, G.M.M., A.N.C. and F.M.; resources, G.M.M., A.N.C. and F.M.; data curation, G.M.M., A.N.C. and F.M.; writing—original draft preparation, G.M.M., C.L.B., A.N.C., C.B., G.A., P.M, C.D.C., R.F. and F.M.; writing—review and editing, G.M.M., A.N.C. and F.M.; visualization, G.M.M., C.L.B., A.N.C., C.B., G.A., P.M., C.D.C., R.F. and F.M.; supervision, G.M.M., A.N.C. and F.M.; project administration, G.M.M., A.N.C. and F.M.; funding acquisition, G.M.M., A.N.C. and F.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Coentro, J.Q.; Pugliese, E.; Hanley, G.; Raghunath, M.; Zeugolis, D.I. Current and upcoming therapies to modulate skin scarring and fibrosis. Adv. Drug Deliv. Rev. 2019, 146, 37–59. [Google Scholar] [CrossRef]
- Paşcalău, A.V.; Cheregi, C.D.; Mureşan, M.Ş.; Şandor, M.I.; Huniadi, C.A.; Nikin, Z.; Pusta, C.T.; Bodog, F.D.; Ionescu, C.; Pop, O.L. CD4+ CD25+ regulatory T-cells role in tumor microenvironment of the squamous cell carcinoma. Rom. J. Morphol. Embryol. 2021, 62, 249. [Google Scholar] [CrossRef] [PubMed]
- Burd, A.; Huang, L. Hypertrophic response and keloid diathesis: Two very different forms of scar. Plast. Reconstr. Surg. 2005, 116, 150e–157e. [Google Scholar] [CrossRef] [PubMed]
- Boer, M.; Duchnik, E.; Maleszka, R.; Marchlewicz, M. Structural and biophysical characteristics of human skin in maintaining proper epidermal barrier function. Adv. Dermatol. Allergol. Postȩpy Dermatol. I Alergol. 2016, 33, 1–5. [Google Scholar] [CrossRef]
- Sidgwick, G.P.; McGeorge, D.; Bayat, A. A comprehensive evidence-based review on the role of topicals and dressings in the management of skin scarring. Arch. Dermatol. Res. 2015, 307, 461–477. [Google Scholar] [CrossRef] [PubMed]
- Ardeshirpour, Y.; Gandjbakhche, A.H.; Najafizadeh, L. Biophotonics techniques for structural and functional imaging, in vivo. Stud. Health Technol. Inf. 2013, 11, 265–297. [Google Scholar]
- Mobley, S.R.; Sjogren, P.P. Soft tissue trauma and scar revision. Facial Plast. Surg. Clin. 2014, 22, 639–651. [Google Scholar] [CrossRef]
- Chae, J.K.; Kim, J.H.; Kim, E.J.; Park, K. Values of a patient and observer scar assessment scale to evaluate the facial skin graft scar. Ann. Dermatol. 2016, 28, 615–623. [Google Scholar] [CrossRef]
- El Kinani, M.; Duteille, F. Scar Epidemiology and Consequences. 2020 December 8. In Textbook on Scar Management: State of the Art Management and Emerging Technologies; Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G., Eds.; Springer: Cham, Switzerland, 2020; Chapter 6. [Google Scholar]
- Brown, B.C.; McKenna, S.P.; Siddhi, K.; McGrouther, D.A.; Bayat, A. The hidden cost of skin scars: Quality of life after skin scarring. J. Plast. Reconstr. Aesthetic Surg. 2008, 61, 1049–1058. [Google Scholar] [CrossRef]
- Mekereș, F.; Voiță, G.F.; Mekereș, G.M.; Bodog, F.D. Psychosocial impact of scars in evaluation of aesthetic prejudice. Rom. J. Leg. Med. 2017, 25, 435–438. [Google Scholar]
- Chen, C.C.; Chen, S.P.; Lyu, S.Y.; Hsu, C.H. Application of Auriculotherapy for Post-Burn Scar Syndrome in Young Adults with Major Burns. J. Acupunct. Meridian Stud. 2021, 31, 127–136. [Google Scholar] [CrossRef]
- Russo, M.; Bolcato, M.; Sabadin, V.; Aprile, A. The medico-legal assessment of aesthetic damage. A correlation analysis between experts and an operative proposal. Leg. Med. 2019, 40, 47–53. [Google Scholar] [CrossRef]
- Mekereş, F.; Nicoară, N.; Roşu, B.; Mekereş, G.M.; Buhaş, C.L. The psychological impact of scars in forensic practice. Rom. J. Forensic. Sci. 2017, 18, 2552–2554. [Google Scholar]
- Franchitto, N.; Telmon, N.; Grolleau, J.L.; Gavarri, L.; Laguerre, J.; Rougé, D. Medicolegal evaluation of aesthetic impairment: Particularities of post-burn scars. Burns 2009, 35, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Voiță-Mekeres, F.; Buhaș, C.L.; Mekeres, G.M.; Tudoran, C.; Racovita, M.; Faur, C.I.; Tudoran, M.; Abu-Awwad, A.; Voiță, N.C.; Maghiar, T.A. Mekeres’ Psychosocial Internalization Scale: A Scale for the Evaluation of Aesthetic Prejudice in Victims of Accidents and Violence. Healthcare 2021, 9, 1440. [Google Scholar] [CrossRef] [PubMed]
- Maskell, J.; Newcombe, P.; Martin, G.; Kimble, R. Psychological and psychosocial functioning of children with burn scarring using cosmetic camouflage: A multi-centre prospective randomised controlled trial. Burns 2014, 40, 135–149. [Google Scholar] [CrossRef]
- Wilcox, S. Multidimensional scale of perceived social support. Psychol. Trauma Theory Res. Pract. Policy 2010, 2, 175–182. [Google Scholar] [CrossRef]
- Van Loey, N.E.; Van Son, M.J. Psychopathology and psychological problems in patients with burn scars. Am. J. Clin. Dermatol. 2003, 4, 245–272. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.D.; Galambos, N.L.; Krahn, H.J. Vulnerability, scar, or reciprocal risk? Temporal ordering of self-esteem and depressive symptoms over 25 years. Longitud. Life Course Stud. 2016, 26, 304–319. [Google Scholar] [CrossRef]
- Lari, A.; Alherz, M.; Hussain, S.; Burhamah, W.; Alabbad, F.; Jarragh, A.; Lari, A. The Importance of Scar Cosmesis across the Surgical Specialties: Factors, Perceptions, and Predispositions. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4219. [Google Scholar] [CrossRef]
- Mekeres, G.M.; Voiţă-Mekereş, F.; Tudoran, C.; Buhaş, C.L.; Tudoran, M.; Racoviţă, M.; Voiţă, N.C.; Pop, N.O.; Marian, M. Predictors for Estimating Scars’ Internalization in Victims with Post-Traumatic Scars versus Patients with Postsurgical Scars. InHealthcare 2022, 16, 550. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 29, n71. [Google Scholar] [CrossRef] [PubMed]
- Fearmonti, R.; Bond, J.; Erdmann, D.; Levinson, H. A review of scar scales and scar measuring devices. Eplasty 2010, 10, e43. [Google Scholar] [PubMed]
- Singer, A.J.; Arora, B.; Dagum, A.; Valentine, S.; Hollander, J.E. Development and validation of a novel scar evaluation scale. Plast. Reconstr. Surg. 2007, 120, 1892–1897. [Google Scholar] [CrossRef] [PubMed]
- Vercelli, S.; Ferriero, G.; Sartorio, F.; Cisari, C.; Bravini, E. Clinimetric properties and clinical utility in rehabilitation of postsurgical scar rating scales: A systematic review. Int. J. Rehabil. Res. 2015, 38, 279–286. [Google Scholar] [CrossRef]
- Moran, B.; Humphrey, S.; Seal, A.; Berkowitz, J.; Zloty, D. Photographic assessment of postsurgical facial scars epidermally sutured with rapidly absorbable polyglactin 910 or nylon: A randomized clinical trial. J. Am. Acad. Dermatol. 2020, 83, 1395–1399. [Google Scholar] [CrossRef]
- Draaijers, L.J.; Tempelman, F.R.; Botman, Y.A.; Tuinebreijer, W.E.; Middelkoop, E.; Kreis, R.W.; Van Zuijlen, P.P. The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast. Reconstr. Surg. 2004, 113, 1960–1965. [Google Scholar] [CrossRef]
- Roques, C.; Teot, L. A critical analysis of measurements used to assess and manage scars. Int. J. Low. Extrem. Wounds 2007, 6, 249–253. [Google Scholar] [CrossRef]
- Park, J.W.; Koh, Y.G.; Shin, S.H.; Choi, Y.J.; Kim, W.S.; Yoo, H.H.; Lee, J.O.; Jang, Y.N.; Kim, J.; Li, K.; et al. Review of Scar Assessment Scales. Med. Lasers Eng. Basic Res. Clin. Appl. 2022, 30, 7. [Google Scholar] [CrossRef]
- Hjellestad, M.; Strand, L.I.; Eide, G.E.; Brekke, R.; Nesheim, A.; Gjelsvik, B.E. Clinimetric properties of a translated and culturally adapted Norwegian version of the Patient and Observer Scar Assessment Scale for use in clinical practice and research. Burns 2021, 47, 953–960. [Google Scholar] [CrossRef]
- Luze, H.; Nischwitz, S.P.; Smolle, C.; Zrim, R.; Kamolz, L.P. The Use of Acellular Fish Skin Grafts in Burn Wound Management—A Systematic Review. Medicina 2022, 58, 912. [Google Scholar] [CrossRef]
- Peinemann, F.; Behrouz-Pirnia, A. Quality issues identified in systematic reviews on early laser intervention to reduce scar formation in wound healing. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 1357–1404. [Google Scholar] [CrossRef]
- Beausang, E.; Floyd, H.; Dunn, K.W.; Orton, C.I.; Ferguson, M.W. A new quantitative scale for clinical scar assessment. Plast. Reconstr. Surg. 1998, 102, 1954–1961. [Google Scholar] [CrossRef]
- Brown, B.C.; Moss, T.P.; McGrouther, D.A.; Bayat, A. Skin scar preconceptions must be challenged: Importance of self-perception in skin scarring. J. Plast. Reconstr. Aesthetic Surg. 2010, 63, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.H.; Bae, Y.C. Analysis of frequency of use of different scar assessment scales based on the scar condition and treatment method. Arch. Plast. Surg. 2014, 41, 111–115. [Google Scholar] [CrossRef] [PubMed]
- van der Wal, M.B.; Verhaegen, P.D.; Middelkoop, E.; van Zuijlen, P.P. A clinimetric overview of scar assessment scales. J. Burn. Care Res. 2012, 33, e79–e87. [Google Scholar] [CrossRef]
- Crowe, J.M.; Simpson, K.; Johnson, W.; Allen, J. Reliability of photographic analysis in determining change in scar appearance. J. Burn. Care Rehabil. 1998, 19, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Brusselaers, N.; Pirayesh, A.; Hoeksema, H.; Verbelen, J.; Blot, S.; Monstrey, S. Burn scar assessment: A systematic review of different scar scales. J. Surg. Res. 2010, 164, e115–e123. [Google Scholar] [CrossRef]
- Yeoung, E.K.; Mann, R.; Engrav, L.H.; Goldberg, M.; Cain, V.; Costa, B.; Moore, M.; Nakamura, D.; Lee, J. Improved burn scar assessment with use of a new scar-rating scale. J. Burn. Care Rehabil. 1997, 18, 353–355. [Google Scholar] [CrossRef]
- Furtado, F.; Hochman, B.; Ferreira, L.M. Evaluating keloid recurrence after surgical excision with prospective longitudinal scar assessment scales. J. Plast. Reconstr. Aesthetic Surg. 2012, 65, e175–e181. [Google Scholar] [CrossRef]
- Sundfeld Spiga Real, D.; Salvador Bagnato, V. Surgical Treatment of Keloids in the Ear: Prospective and Randomized Study Comparing Direct Surgical Excision vs. Keloid Fillet Flap. Asian J. Res. Surg. 2022, 7, 22–23. [Google Scholar]
- Sullivan, T.A.; Smith, J.; Kermode, J.; Mclver, E.; Courtemanche, D.J. Rating the burn scar. J. Burn. Care Rehabil. 1990, 11, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Baryza, M.J.; Baryza, G.A. The Vancouver Scar Scale: An administration tool and its interrater reliability. J. Burn. Care Rehabil. 1995, 16, 535–538. [Google Scholar] [CrossRef]
- Thompson, C.M.; Sood, R.F.; Honari, S.; Carrougher, G.J.; Gibran, N.S. What score on the Vancouver Scar Scale constitutes a hypertrophic scar? Results from a survey of North American burn-care providers. Burns 2015, 41, 1442–1448. [Google Scholar] [CrossRef] [PubMed]
- Mahar, P.D.; Spinks, A.B.; Cleland, H.; Bekhor, P.; Waibel, J.S.; Lo, C.; Goodman, G. Improvement of burn scars treated with fractional ablative CO2 lasers—A systematic review and meta-analysis using the Vancouver Scar Scale. J. Burn. Care Res. 2021, 42, 200–206. [Google Scholar] [CrossRef]
- Pertea, M.; Poroch, V.; Ciobanu, P.; Filip, A.; Velenciuc, N.; Lunca, S.; Panuta, A.; Buna-Arvinte, M.; Luca, S.; Veliceasa, B. Efficiency of Bromelain-Enriched Enzyme Mixture (NexoBrid™) in the Treatment of Burn Wounds. Appl. Sci. 2021, 11, 8134. [Google Scholar] [CrossRef]
- Shin, T.M.; Bordeaux, J.S. The role of massage in scar management: A literature review. Dermatol. Surg. 2012, 38, 414–423. [Google Scholar] [CrossRef]
- Deng, H.; Li-Tsang, C.W. Measurement of vascularity in the scar: A systematic review. Burns 2019, 45, 1253–1265. [Google Scholar] [CrossRef]
- Hodin, D. Esthétimètre: Barème esthétimétrique facial [Esthetimeter: Facial esthetimetric scale]. Med. Leg. Dommage Corpor. 1973, 6, 111–116. [Google Scholar]
- Stanculescu, S.; Hostiuc, S.; Dermengiu, D. The usefulness of evaluating aesthetic prejudice with aesthetimetric scales. Rom. J. Leg. Med. 2008, 16, 117–122. [Google Scholar] [CrossRef]
- Lipman, K.; Wang, M.; Berthiaume, E.; Holloway, J.; Da Lio, A.; Ting, K.; Soo, C.; Zheng, Z. Evaluating current scar assessment methods. Ann. Plast. Surg. 2020, 84, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Argyrides, M.; Kkeli, N. Multidimensional body-self relations questionnaire-appearance scales: Psychometric properties of the Greek version. Psychol. Rep. 2013, 113, 885–897. [Google Scholar] [CrossRef]
- Cash, T.E. Body-image attitudes: Evaluation, investment, and affect. Percept. Mot. Skills 1994, 78, 1168–1170. [Google Scholar] [CrossRef]
- Untas, A.; Koleck, M.; Rascle, N.; Borteyrou, X. Psychometric properties of the french adaptation of the multidimensional body self relations questionnaire–appearance scales. Psychol. Rep. 2009, 105, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Dyer, A.; Hennrich, L.; Borgmann, E.; White, A.J.; Alpers, G.W. Body image and noticeable self-inflicted scars. J. Nerv. Ment. Dis. 2013, 201, 1080–1084. [Google Scholar] [CrossRef]
- Juo, Y.Y.; Park, C.; Yoo, J.; Guerron, D.; Sudan, R.; Friedman, K.; Portenier, D.; Seymour, K.A. Technical Feasibility, Outcomes, and Patient Satisfaction After Needlescopic and Laparoscopic Bariatric Surgery: A Randomized Study. Obes. Surg. 2021, 31, 5085–5091. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Dambi, J.M.; Corten, L.; Chiwaridzo, M.; Jack, H.; Mlambo, T.; Jelsma, J. A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS). Health Qual. Life Outcomes 2018, 16, 9. [Google Scholar] [CrossRef]
- Waqas, A.; Turk, M.; Naveed, S.; Amin, A.; Kiwanuka, H.; Shafique, N.; Chaudhry, M.A. Perceived social support among patients with burn injuries: A perspective from the developing world. Burns 2018, 44, 168–174. [Google Scholar] [CrossRef]
- Abramson, L.Y.; Metalsky, G.I.; Alloy, L.B. Hopelessness depression: A theory-based subtype of depression. Psychol. Rev. 1989, 96, 358. [Google Scholar] [CrossRef]
- Metalsky, G.I.; Joiner, T.E. The hopelessness depression symptom questionnaire. Cogn. Ther. Res. 1997, 21, 359–384. [Google Scholar] [CrossRef]
- Marian, M. Trial of hopelessness theory by the use of modeling. New psychometric data on the Hopelessness Depression Symptom Questionnaire. J. Psychol. Educ. Res. 2012, 20, 45–58. [Google Scholar]
- Chen, J.; Zhou, L. Savoring as a moderator between positive life events and hopelessness depression. Soc. Behav. Personal. Int. J. 2017, 45, 1337–1344. [Google Scholar] [CrossRef]
- Manna, G.; Falgares, G.; Ingoglia, S.; Como, M.R.; De Santis, S. The relationship between self-esteem, depression and anxiety: Comparing vulnerability and scar model in the Italian context. Mediterr. J. Clin. Psychol. 2016, 30, 4. [Google Scholar]
- Klassen, A.F.; Ziolkowski, N.; Mundy, L.R.; Miller, H.C.; McIlvride, A.; DiLaura, A.; Fish, J.; Pusic, A.L. Development of a new patient-reported outcome instrument to evaluate treatments for scars: The SCAR-Q. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1672. [Google Scholar] [CrossRef]
- Ziolkowski, N.I.; Pusic, A.L.; Fish, J.S.; Mundy, L.R.; Wong She, R.; Forrest, C.R.; Hollenbeck, S.; Arriagada, C.; Calcagno, M.; Greenhalgh, D.; et al. Psychometric findings for the SCAR-Q patient-reported outcome measure based on 731 children and adults with surgical, traumatic, and burn scars from four countries. Plast. Reconstr. Surg. 2020, 146, 331e–338e. [Google Scholar] [CrossRef]
- Ziolkowski, N.I.; Behman, R.; Klassen, A.F.; Fish, J.S.; Mundy, L.R.; She, R.W.; Forrest, C.R.; Hollenbeck, S.; Arriagada, C.; Greenhalgh, D.; et al. Determining the independent risk factors for worse SCAR-Q scores and future scar revision surgery. Plast. Reconstr. Surg. 2021, 148, 203–212. [Google Scholar] [CrossRef]
- Pusic, A.L.; Klassen, A.F.; Scott, A.M.; Cano, S.J. Development and psychometric evaluation of the FACE-Q satisfaction with appearance scale: A new patient-reported outcome instrument for facial aesthetics patients. Clin. Plast. Surg. 2013, 40, 249–260. [Google Scholar] [CrossRef]
- Durani, P.; McGrouther, D.A.; Ferguson, M.W. The Patient Scar Assessment Questionnaire: A reliable and valid patient-reported outcomes measure for linear scars. Plast. Reconstr. Surg. 2009, 123, 1481–1489. [Google Scholar] [CrossRef]
- Kim, M.; Mirsky, N.; Spielman, A.; Mathew, P.; Yechieli, R.; Tang, J.C.; Thaller, S.R. Evaluating Symptomatic and Psychosocial Well-being After Keloid Treatment With SCAR-Q. Aesthet Surg. J. 2022, 42, NP416–NP422. [Google Scholar] [CrossRef]
- Ostlie, D.J.; Sharp, N.E.; Thomas, P.; Sharp, S.W.; Holcomb, G.W., III; St Peter, S.D. Patient scar assessment after single-incision versus four-port laparoscopic cholecystectomy: Long-term follow-up from a prospective randomized trial. J. Laparoendosc. Adv. Surg. Tech. A 2013, 23, 553–555. [Google Scholar] [CrossRef] [PubMed]
- Voci, A.; Lee, D.; Ho, E.; Crane-Okada, R.; DiNome, M. Impact of port site scar on perception of patients with breast cancer: Patient-reported outcomes. Breast Cancer Res. Treat. 2018, 170, 569–572. [Google Scholar] [CrossRef]
- Mundy, L.R.; Miller, H.C.; Klassen, A.F.; Cano, S.J.; Pusic, A.L. Patient-Reported Outcome Instruments for Surgical and Traumatic Scars: A Systematic Review of their Development, Content, and Psychometric Validation. Aesthetic Plast Surg. 2016, 40, 792–800. [Google Scholar] [CrossRef]
- Economopoulos, K.P.; Petralias, A.; Linos, E.; Linos, D. Psychometric evaluation of Patient Scar Assessment Questionnaire following thyroid and parathyroid surgery. Thyroid 2012, 22, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Guest, E.; Griffiths, C.; Harcourt, D. A qualitative exploration of psychosocial specialists’ experiences of providing support in UK burn care services. Scars Burn. Health 2018, 4, 2059513118764881. [Google Scholar] [CrossRef] [PubMed]
- Hoogewerf, C.J.; van Baar, M.E.; Middelkoop, E.; van Loey, N.E. Impact of facial burns: Relationship between depressive symptoms, self-esteem and scar severity. Gen. Hosp. Psychiatry 2014, 36, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Macleod, R.; Shepherd, L.; Thompson, A.R. Posttraumatic stress symptomatology and appearance distress following burn injury: An interpretative phenomenological analysis. Health Psychol. 2016, 35, 1197–1204. [Google Scholar] [CrossRef]
- Betarbet, U.; Blalock, T.W. Keloids: A review of etiology, prevention, and treatment. J. Clin. Aesthetic Dermatol. 2020, 13, 33. [Google Scholar]
- Attoe, C.; Pounds-Cornish, E. Psychosocial adjustment following burns: An integrative literature review. Burns 2015, 41, 1375–1384. [Google Scholar] [CrossRef]
- Ngaage, M.; Agius, M. The psychology of scars: A mini-review. Psychiatr. Danub. 2018, 30 (Suppl. S7), 633–638. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).