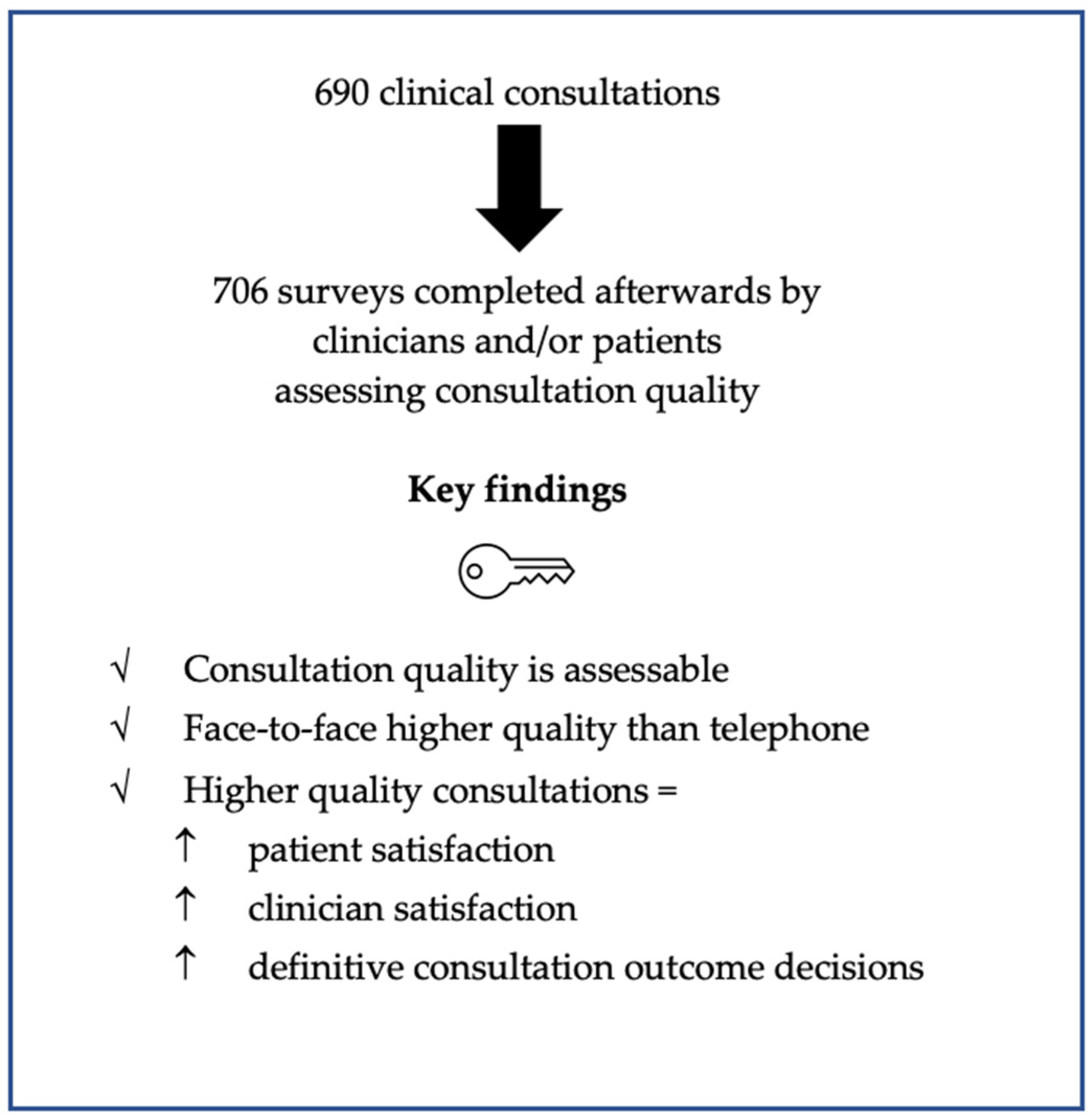
Quality in Clinical Consultations: A Cross-Sectional Study
Abstract
1. Introduction
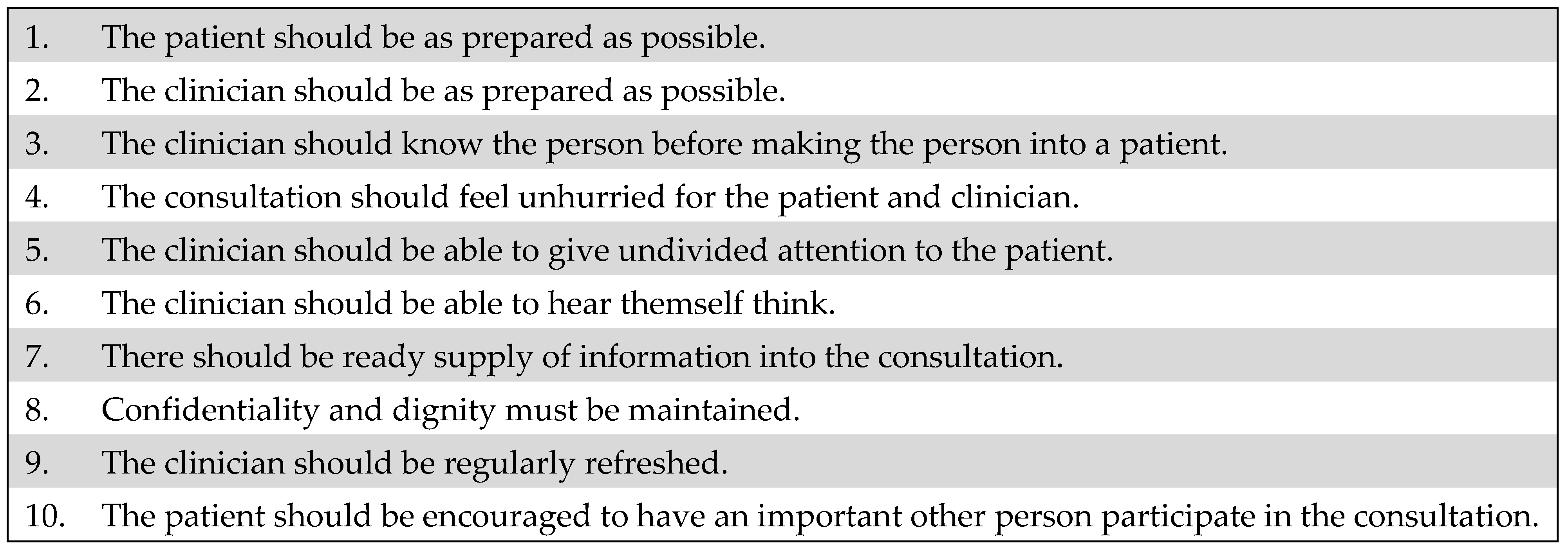
2. Materials and Methods
2.1. Settings and Participants
2.2. Variables and Data Sources
2.3. Study Size and Statistical Methods
3. Results
3.1. Quality of Consultation
3.2. Quality of Consultation and Consultation Method
3.3. Quality of Consultation and Satisfaction
3.4. Quality of Consultation and Consultation Outcome
3.5. Other Survey Results
4. Discussion
4.1. Principal Findings
4.2. Comparison to Other Studies
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- General Medical Council. Outcomes for Graduates; General Medical Council: London, UK, 2019; Available online: https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates/outcomes-for-graduates/outcomes-2---professional-skills (accessed on 25 October 2021).
- General Medical Council. Good Medical Practice; General Medical Council: London, UK, 2013; Available online: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice (accessed on 25 October 2021).
- Launer, J. Is there a crisis in clinical consultations? Postgrad. Med. J. 2017, 93, 58. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, G. The process of clinical consultation is crucial to patient outcomes and safety: 10 quality indicators. Clin. Med. 2019, 19, 503–506. [Google Scholar] [CrossRef] [PubMed]
- Graf, A.; Marcus, H.J.; Baldeweg, S.E. The direct and indirect impact of the COVID-19 pandemic on the care of patients with pituitary disease: A cross sectional study. Pituitary 2021, 24, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Hutchings, R. The Impact of COVID-19 on the Use of Digital Technology in the NHS; Nuffield Trust: London, UK, 2020; Available online: https://www.nuffieldtrust.org.uk/research/the-impact-of-COVID-19-on-the-use-of-digital-technology-in-the-nhs (accessed on 25 October 2021).
- Murphy, M.; Scott, L.J.; Salisbury, C.; Turner, A.; Scott, A.; Denholm, R.; Lewis, R.; Iyer, G.; Macleod, J.; Horwood, J. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: A mixed-methods longitudinal study. Br. J. Gen. Pract. 2021, 71, e166–e177. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018; Available online: https://www.R-project.org/ (accessed on 9 June 2021).
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Stat. Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Howie, J.G.; Heaney, D.J.; Maxwell, M.; Walker, J.J.; Freeman, G.K. Developing a ‘consultation quality index’ (CQI) for use in general practice. Fam. Pract. 2000, 17, 455–461. [Google Scholar] [CrossRef][Green Version]
- Burt, J.; Abel, G.; Elmore, N.; Campbell, J.; Roland, M.; Benson, J.; Silverman, J. Assessing communication quality of consultations in primary care: Initial reliability of the Global Consultation Rating Scale, based on the Calgary-Cambridge Guide to the Medical Interview. BMJ Open 2014, 4, e004339. [Google Scholar] [CrossRef]
- NHS England. The NHS Long Term Plan; NHS England: England, UK, 2019; Available online: https://www.longtermplan.nhs.uk (accessed on 17 August 2021).
- World Health Organisation. Global Strategy on Digital Health 2020–2025; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 25 October 2021).
- Hammersley, V.; Donaghy, E.; Parker, R.; McNeilly, H.; Atherton, H.; Bikker, A.; Campbell, J.; McKinstry, B. Comparing the content and quality of video, telephone, and face-to-face consultations: A non-randomised, quasi-experimental, exploratory study in UK primary care. Br. J. Gen. Pract. 2019, 69, e595–e604. [Google Scholar] [CrossRef]
- Efthymiadis, A.; Hart, E.J.; Guy, A.M.; Harry, R.; Mahesan, T.; Chedid, W.A.; Uribe-Lewis, S.; Perry, M.J. Are telephone consultations the future of the NHS? The outcomes and experiences of an NHS urological service in moving to telemedicine. Future Healthc. J. 2021, 8, e15–e20. [Google Scholar] [CrossRef]
- Martos-Pérez, F.; Martín-Escalante, M.D.; Olalla-Sierra, J.; Prada-Pardal, J.L.; García-De-Lucas, M.D.; González-Vega, R.; Jiménez-Puente, A.; García-Alegría, J. The value of telephone consultations during COVID-19 pandemic. An observational study. QJM Int. J. Med. 2021, 114, 715–720. [Google Scholar] [CrossRef]
- Holtz, B.E. Patients Perceptions of Telemedicine Visits before and after the Coronavirus Disease 2019 Pandemic. Telemed. e-Health 2021, 27, 107–112. [Google Scholar] [CrossRef]
- Kludacz-Alessandri, M.; Hawrysz, L.; Korneta, P.; Gierszewska, G.; Pomaranik, W.; Walczak, R. The impact of medical teleconsultations on general practitioner-patient communication during COVID-19: A case study from Poland. PLoS ONE 2021, 16, e0254960. [Google Scholar] [CrossRef] [PubMed]
- McKinstry, B.; Hammersley, V.S.; Burton, C.; Pinnock, H.; Elton, R.; Dowell, J.; Sawdon, N.; Heaney, D.; Elwyn, G.; Sheikh, A. The quality, safety and content of telephone and face-to-face consultations: A comparative study. Qual. Saf. Health Care 2010, 19, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Verma, P.; Kerrison, R. Patients’ and physicians’ experiences with remote consultations in primary care during the COVID-19 pandemic: A multi-method rapid review of the literature. BJGP Open 2022, BJGPO.2021.0192. [Google Scholar] [CrossRef] [PubMed]
- Wanat, M.; Hoste, M.E.; Gobat, N.H.; Anastasaki, M.; Böhmer, F.; Chlabicz, S.; Colliers, A.; Farrell, K.; Hollerbach, S.; Karkana, M.-N.; et al. Patients’ and clinicians’ perspectives on the primary care consultations for acute respiratory infections during the first wave of the COVID-19 pandemic: An eight-country qualitative study in Europe. BJGP Open 2022, BJGPO.2021.0172. [Google Scholar] [CrossRef]
- Donaghy, E.; Atherton, H.; Hammersley, V.; McNeilly, H.; Bikker, A.; Robbins, L.; Campbell, J.; McKinstry, B. Acceptability, benefits, and challenges of video consulting: A qualitative study in primary care. Br. J. Gen. Pract. 2019, 69, e586–e594. [Google Scholar] [CrossRef]
- Andrades, M.; Kausar, S.; Ambreen, A. Role and Influence of the Patient’s Companion in Family Medicine Consultations: “The Patient’s Perspective”. J. Fam. Med. Prim. Care 2013, 2, 283–287. [Google Scholar]
- Sharp, R.J.; Hobson, J. Patient and physician views of accompanied consultations in occupational health. Occup. Med. 2016, 66, 643–648. [Google Scholar] [CrossRef]
- Propper, C.; Stoye, G.; Zaranko, B. The Wider Impacts of the Coronavirus Pandemic on the NHS. Fisc. Stud. 2020, 4, 345–356. [Google Scholar] [CrossRef]
- Isautier, J.M.; Copp, T.; Ayre, J.; Cvejic, E.; Meyerowitz-Katz, G.; Batcup, C.; Bonner, C.; Dodd, R.; Nickel, B.; Pickles, K.; et al. People’s Experiences and Satisfaction With Telehealth During the COVID-19 Pandemic in Australia: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e24531. [Google Scholar] [CrossRef]
- Rimmer, A. COVID-19: NHS will take at least a year and a half to recover, doctors warn. BMJ 2021, 373, n999. [Google Scholar] [CrossRef] [PubMed]
- Allan, J.L.; Johnston, D.W.; Powell, D.J.H.; Farquharson, B.; Jones, M.C.; Leckie, G.; Johnston, M. Clinical decisions and time since rest break: An analysis of decision fatigue in nurses. Health Psychol. 2019, 38, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Hsiang, E.Y.; Mehta, S.J.; Small, D.S.; Rareshide, C.A.L.; Snider, C.K.; Day, S.C.; Patel, M.S. Association of Primary Care Clinic Appointment Time With Clinician Ordering and Patient Completion of Breast and Colorectal Cancer Screening. JAMA Netw. Open 2019, 2, e193403. [Google Scholar] [CrossRef]
- Kim, R.H.; Day, S.C.; Small, D.S.; Snider, C.K.; Rareshide, C.A.L.; Patel, M.S. Variations in Influenza Vaccination by Clinic Appointment Time and an Active Choice Intervention in the Electronic Health Record to Increase Influenza Vaccination. JAMA Netw. Open. 2018, 1, e181770. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Palepu, A.; Dodek, P.; Salmon, A.; Leitch, H.; Ruzycki, S.; Townson, A.; Lacaille, D. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: The role of gender, ethnicity and sexual orientation. BMJ Open 2021, 11, e050380. [Google Scholar] [CrossRef]
- Hlubocky, F.J.; Back, A.L.; Shanafelt, T.D.; Gallagher, C.M.; Burke, J.M.; Kamal, A.H.; Paice, J.A.; Page, R.D.; Spence, R.; McGinnis, M.; et al. Occupational and Personal Consequences of the COVID-19 Pandemic on US Oncologist Burnout and Well-Being: A Study From the ASCO Clinician Well-Being Task Force. JCO Oncol. Pract. 2021, 17, e427–e438. [Google Scholar] [CrossRef] [PubMed]
| Consultation Details n = 538 | |
|---|---|
| Setting | Medical clinic: 444 (83%) Surgical clinic: 94 (17%) |
| Type | Initial consultation: 55 (10%) Review consultation: 483 (90%) |
| Method | Face-to-face consultation: 168 (31%) Telephone consultation: 370 (69%) |
| Outcome | Decision pending: 471 (88%)
|
| Question (Q) Number | Clinician Survey Question | n = 291 | Patient Survey Question | n = 415 |
|---|---|---|---|---|
| Q1 | Did the patient know why they were attending the consultation? | yes: 284 (98%) no: 7 (2%) | Did you know why you were attending the consultation? | yes: 400 (96%) no: 15 (4%) |
| Q2 | Did you have the opportunity to review the case before the consultation? | yes: 289 (99%) no: 2 (1%) | Did the clinician know the details of your case? | yes: 394 (95%) no: 21 (5%) |
| Q3 | Did you ask and document the patient’s occupation and/or interests? | yes: 203 (70%) no: 88 (30%) | Did the clinician ask about your occupation and/or interests? | yes: 203 (49%) no: 212 (51%) |
| Q4 | Did the consultation time feel adequate and unhurried? | yes: 275 (95%) no: 16 (5%) | Did the consultation time feel adequate and unhurried? | yes: 402 (97%) no: 13 (3%) |
| Q5 | Was the consultation free of interruptions? E.g., being called by a colleague during the consultation. | yes: 274 (94%) no: 17 (6%) Of those who answered no:
| Was the consultation free of interruptions? E.g., you or the clinician received other calls during the consultation. | yes: 409 (99%) no: 6 (1%) Of those who answered no:
|
| Q6 | Was the consultation free of distractions? E.g., nearby building works. | yes: 272 (93%) no: 19 (7%) Of those who answered no:
| Was the consultation free of distractions? E.g., nearby building works. | yes: 412 (99%) no: 3 (1%) Of those who answered no:
|
| Q7 | Did you have all the information needed to conduct the consultation? | yes: 137 (47%) no: 154 (53%) Of those who answered no:
| Did the clinician have the information needed to conduct the consultation? | yes: 374 (90%) no: 41 (10%) Of those who answered no:
|
| Q8 | Were confidentiality and dignity maintained throughout the consultation? E.g., was the telephone consultation able to be conducted in a confidential setting? | yes: 286 (98%) no: 5 (2%) Of those who answered no:
| Were confidentiality and dignity maintained throughout the consultation? E.g., was the telephone consultation able to be conducted in a confidential setting? | yes: 414 (100%) no: 1 (<1%) |
| Q9 | Were breaks taken as needed throughout the clinic and, if an afternoon clinic, did you have a lunch break? | yes: 253 (87%) no: 38 (13%) | No survey question | |
| Q10 | Was the patient’s friend or relative invited to participate in the consultation? E.g., via speaker phone or sitting next to the patient throughout the consultation. | yes: 68 (23%) no: 223 (77%) | Was your friend or relative invited to participate in the consultation? E.g., via speaker phone or sitting next to you throughout the consultation. | yes: 43 (10%) no 372 (90%) |
| Q11 | Overall, were you satisfied with the consultation? | yes: 285 (98%) no: 6 (2%) | Overall, were you satisfied with the consultation? | yes: 406 (98%) no: 9 (2%) |
| Question (Q) Number | Clinician Survey Question n = 168 | Patient Survey Question n = 168 | Number of Surveys with a Difference in y/n Survey Response for Patient and Clinician Assessing Same Consultation n = 168 |
|---|---|---|---|
| Q1 | Did the patient know why they were attending the consultation? | Did you know why you were attending the consultation? | 8 (5%) |
| Q2 | Did you have the opportunity to review the case before the consultation? | Did the clinician know the details of your case? | 9 (5%) |
| Q3 | Did you ask and document the patient’s occupation and/or interests? | Did the clinician ask about your occupation and/or interests? | 47 (30%) |
| Q4 | Did the consultation time feel adequate and unhurried? | Did the consultation time feel adequate and unhurried? | 11 (7%) |
| Q5 | Was the consultation free of interruptions? E.g., being called by a colleague during the consultation. | Was the consultation free of interruptions? E.g., you or the clinician received other calls during the consultation. | 13 (8%) |
| Q6 | Was the consultation free of distractions? E.g., nearby building works. | Was the consultation free of distractions? E.g., nearby building works. | 9 (5%) |
| Q7 | Did you have all the information needed to conduct the consultation? | Did the clinician have the information needed to conduct the consultation? | 88 (52%) |
| Q8 | Were confidentiality and dignity maintained throughout the consultation? E.g., was the telephone consultation able to be conducted in a confidential setting? | Were confidentiality and dignity maintained throughout the consultation? E.g., was the telephone consultation able to be conducted in a confidential setting? | 3 (2%) |
| Q10 | Was the patient’s friend or relative invited to participate in the consultation? E.g., via speaker phone or sitting next to the patient throughout the consultation. | Was your friend or relative invited to participate in the consultation? E.g., via speaker phone or sitting next to you throughout the consultation. | 18 (11%) |
| Q11 | Overall, were you satisfied with the consultation? | Overall, were you satisfied with the consultation? | 3 (2%) |
| Univariate Logistic Regression Analysis | Multivariate Logistic Regression Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Clinician | Patient | Clinician | Patient | |||||
| Survey Question (Q) | Log-Odds | p | Log-Odds | p | Log-Odds | p | Log-Odds | p |
| Q1 | 4.25 ± 1.88 | <0.001 | 2.80 ± 1.50 | 0.001 | 4.08 ± 2.13 | <0.001 | 1.93 ± 1.73 | 0.03 |
| Q2 | na * | na * | 2.38 ± 1.46 | 0.004 | ||||
| Q3 | 0.13 ± 1.72 | 0.99 | 2.07 ± 2.09 | 0.08 | ||||
| Q4 | 2.27 ± 1.78 | 0.04 | 2.99 ± 1.52 | <0.001 | 2.83 ± 1.86 | 0.003 | ||
| Q5 | 1.21 ± 2.21 | 0.42 | −13.77± 3165.60 | >0.99 | ||||
| Q6 | 2.76 ± 1.67 | 0.005 | −12.76 ± 2715.34 | >0.99 | 2.56 ± 2.03 | 0.01 | ||
| Q7 | 1.52 ± 2.16 | 0.30 | 2.05 ± 1.36 | 0.006 | 2.41 ± 1.56 | 0.002 | ||
| Q8 | 2.64 ± 2.36 | 0.06 | na * | na * | ||||
| Q9 | −15.85 ± 3419.28 | >0.99 | No survey question | |||||
| Q10 | −0.55 ± 1.72 | 0.69 | −0.08 ± 2.10 | >0.99 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graf, A.; Koh, C.H.; Caldwell, G.; Grieve, J.; Tan, M.; Hassan, J.; Bakaya, K.; Marcus, H.J.; Baldeweg, S.E. Quality in Clinical Consultations: A Cross-Sectional Study. Clin. Pract. 2022, 12, 545-556. https://doi.org/10.3390/clinpract12040058
Graf A, Koh CH, Caldwell G, Grieve J, Tan M, Hassan J, Bakaya K, Marcus HJ, Baldeweg SE. Quality in Clinical Consultations: A Cross-Sectional Study. Clinics and Practice. 2022; 12(4):545-556. https://doi.org/10.3390/clinpract12040058
Chicago/Turabian StyleGraf, Anneke, Chan Hee Koh, Gordon Caldwell, Joan Grieve, Melissa Tan, Jasmine Hassan, Kaushiki Bakaya, Hani J. Marcus, and Stephanie E. Baldeweg. 2022. "Quality in Clinical Consultations: A Cross-Sectional Study" Clinics and Practice 12, no. 4: 545-556. https://doi.org/10.3390/clinpract12040058
APA StyleGraf, A., Koh, C. H., Caldwell, G., Grieve, J., Tan, M., Hassan, J., Bakaya, K., Marcus, H. J., & Baldeweg, S. E. (2022). Quality in Clinical Consultations: A Cross-Sectional Study. Clinics and Practice, 12(4), 545-556. https://doi.org/10.3390/clinpract12040058