Healthcare Waste Toxicity: From Human Exposure to Toxic Mechanisms and Management Strategies
Abstract
1. Introduction
2. Methodology of Research
3. Categories, Origins, and Production of HCW
3.1. Types and Description of HCW
3.2. Sources of HCW
3.3. Generation of HCW
3.4. HCW Composition
4. Health Hazards of Toxic HCW Exposure
4.1. Individuals Potentially Exposed to HCW Toxicity
4.2. Toxicity Risks to Health
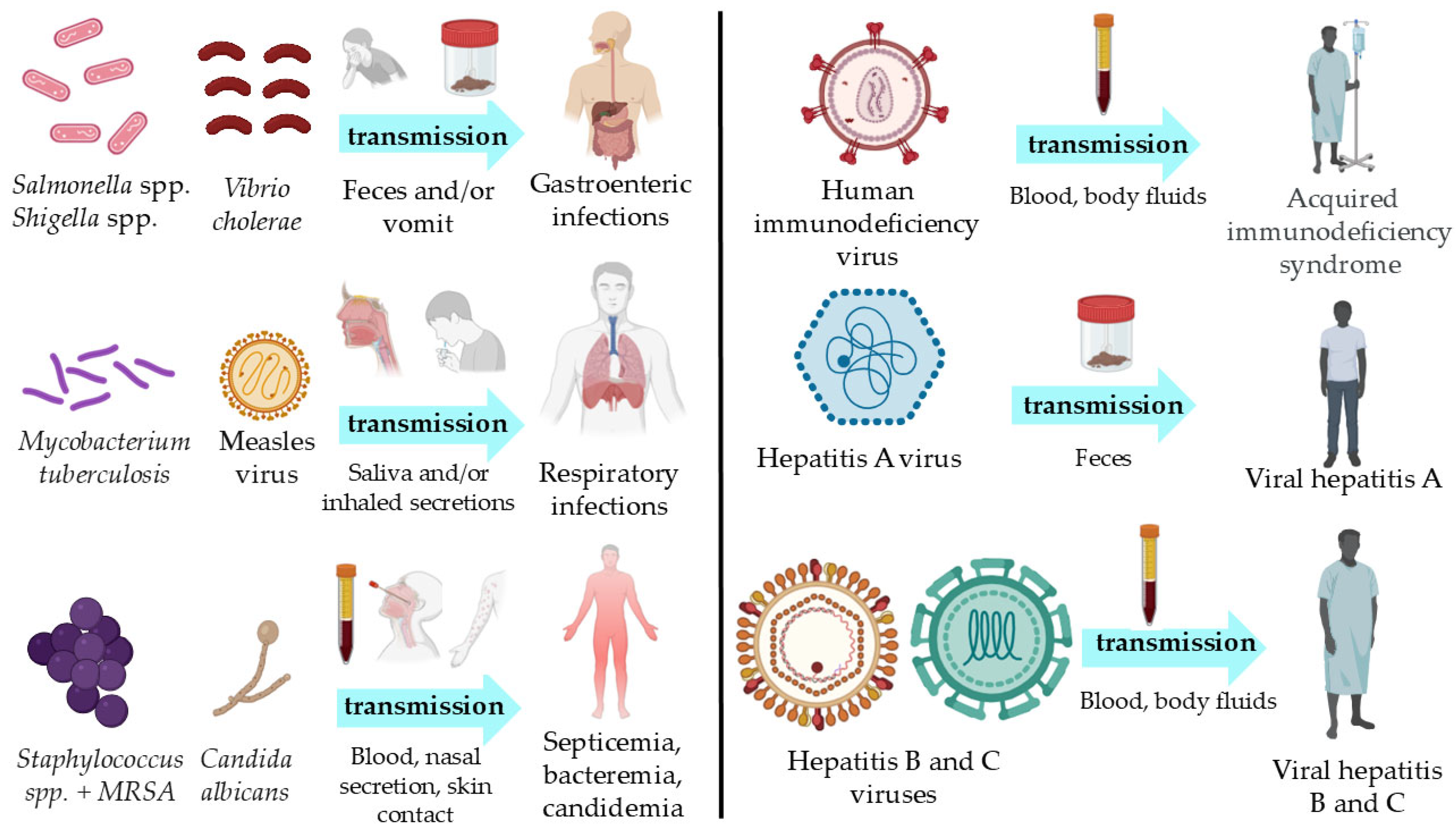
4.2.1. Toxicity from Sharps, Pathological and Infectious Waste
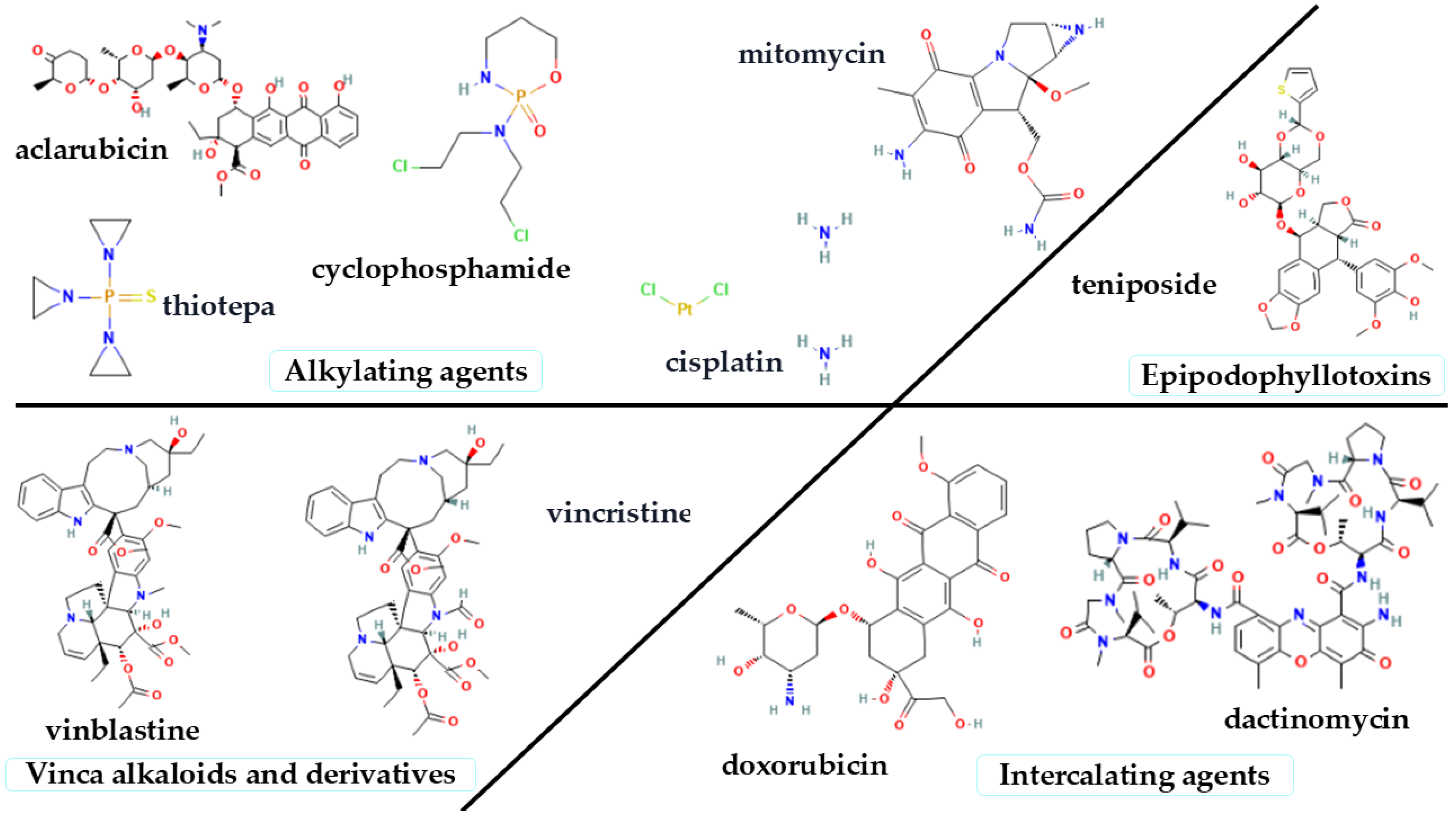
4.2.2. Toxicity from Pharmaceutical and Genotoxic Waste
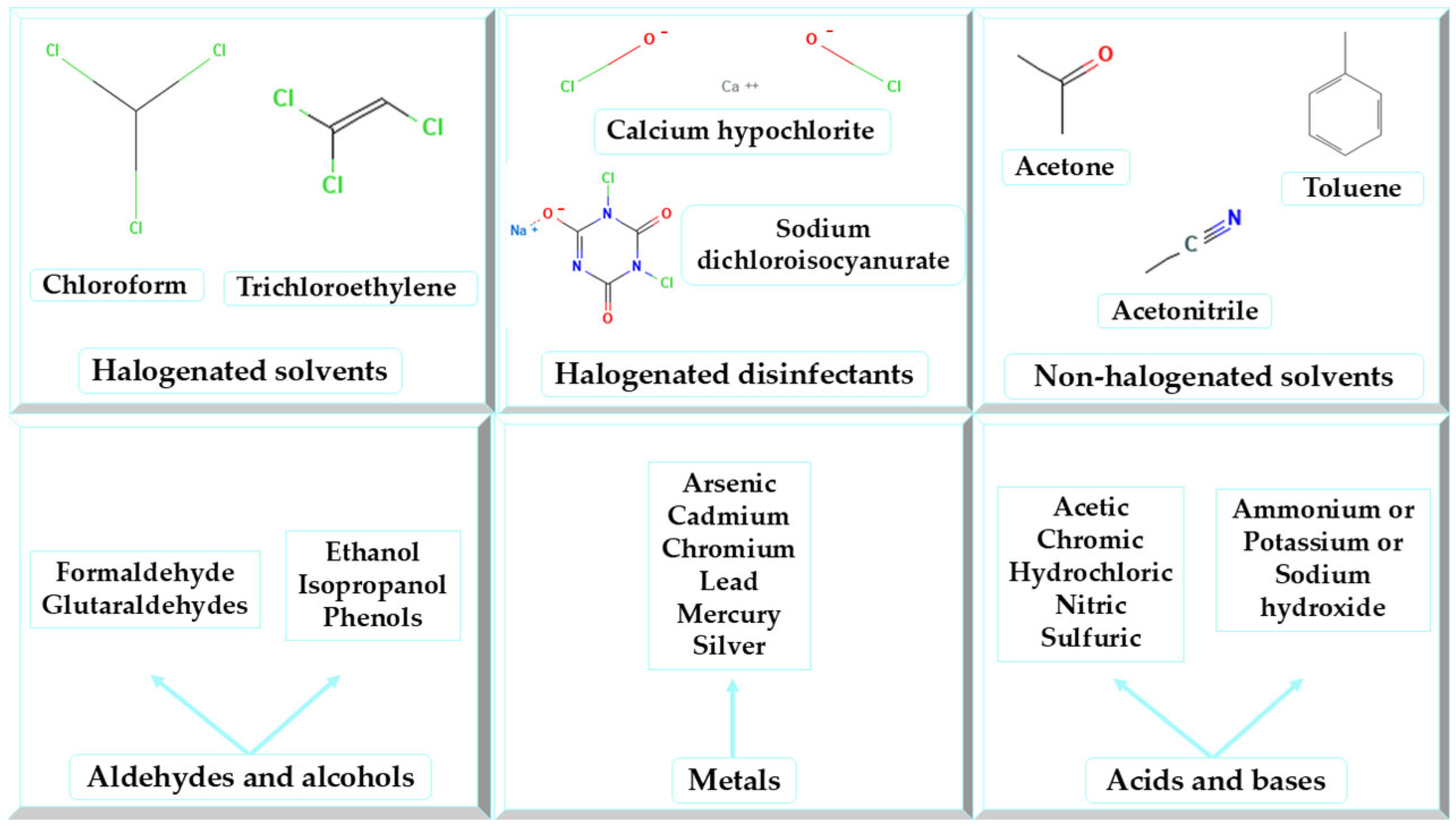
4.2.3. Toxicity from Chemical Wastes
4.2.4. Toxicity from Radioactive Wastes
4.2.5. Toxicity from HCW Management Practices
4.2.6. Mechanism of Toxic Action
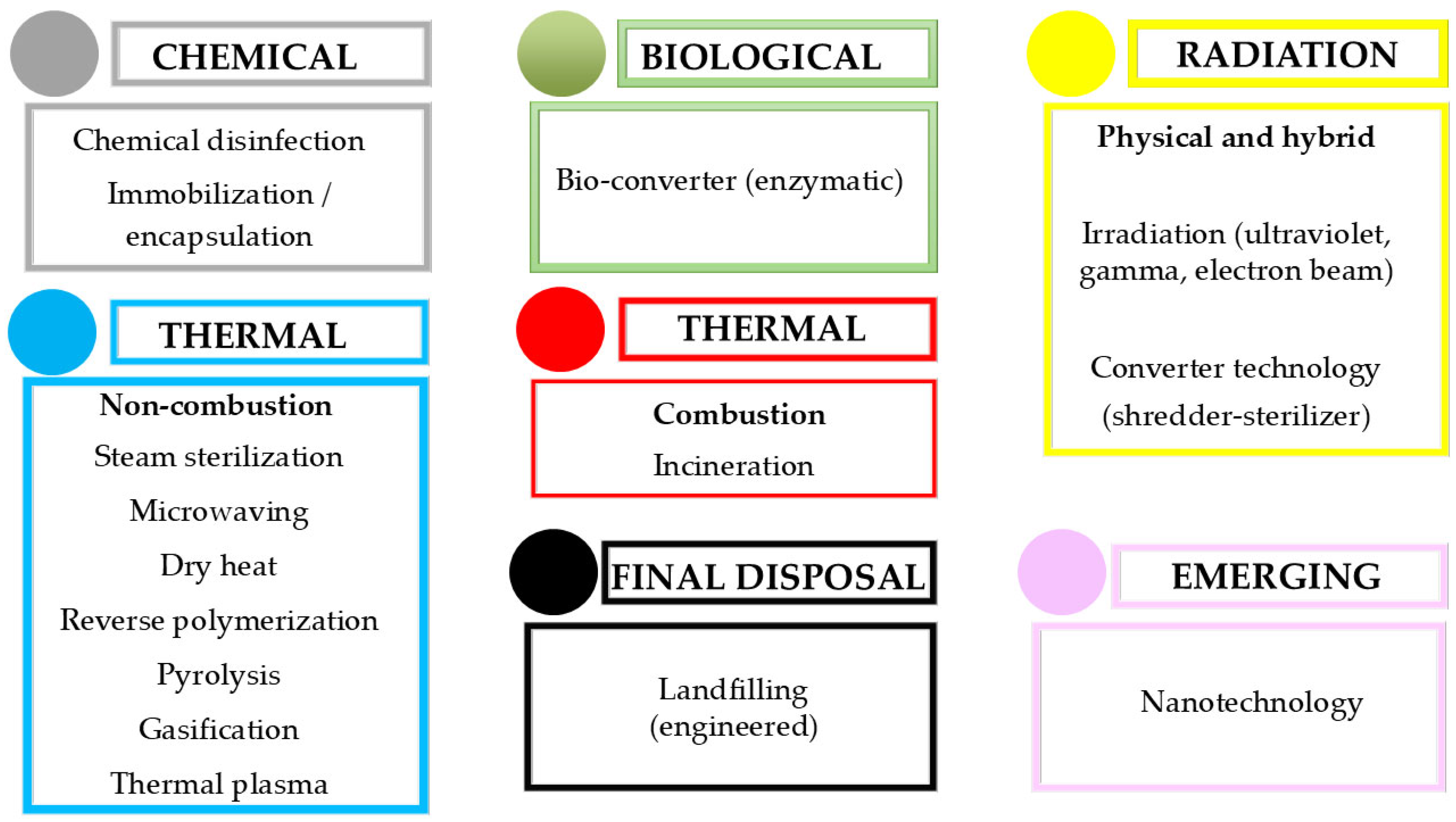
5. HCW Management
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HCW | Healthcare Waste |
| WHO | Directory of open access journals |
| HIV | Human Immunodeficiency Virus |
| HCV | Hepatitis C Virus |
| HBV | Hepatitis B Virus |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| DNA | Deoxyribonucleic Acid |
| UV | Ultraviolet |
References
- Janik-Karpinska, E.; Brancaleoni, R.; Niemcewicz, M.; Wojtas, W.; Foco, M.; Podogrocki, M.; Bijak, M. Healthcare Waste—A Serious Problem for Global Health. Healthcare 2023, 11, 242. [Google Scholar] [CrossRef]
- World Health Organization. Protecting Health Through Health Care Waste Management. Available online: https://www.who.int/docs/default-source/wpro---documents/hae---regional-forum-(2016)/hcwmanagement-factsheet-rfhe.pdf?sfvrsn=6d59d7e_2 (accessed on 6 March 2025).
- de Aquino, A.C.T.; Gonçalves, M.F.S.; Mol, M.P.G. Healthcare Waste and Circular Economy Principles: It Is Time to Improve! Waste Manag. Res. J. Sustain. Circ. Econ. 2024, 42, 857–859. [Google Scholar] [CrossRef]
- Attrah, M.; Elmanadely, A.; Akter, D.; Rene, E.R. A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options. Environments 2022, 9, 146. [Google Scholar] [CrossRef]
- Kenny, C.; Priyadarshini, A. Review of Current Healthcare Waste Management Methods and Their Effect on Global Health. Healthcare 2021, 9, 284. [Google Scholar] [CrossRef] [PubMed]
- Windfeld, E.S.; Brooks, M.S.-L. Medical Waste Management—A Review. J. Environ. Manag. 2015, 163, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Gusca, J.; Kalnins, S.N.; Blumberga, D.; Bozhko, L.; Khabdullina, Z.; Khabdullin, A. Assessment Method of Health Care Waste Generation in Latvia and Kazakhstan. Energy Procedia 2015, 72, 175–179. [Google Scholar] [CrossRef]
- Farzadkia, M.; Emamjomeh, M.; Golbaz, S.; Sajadi, H. An Investigation on Hospital Solid Waste Management in Iran. Glob. Nest J. 2015, 17, 771–783. [Google Scholar]
- Hossain, M.S.; Santhanam, A.; Nik Norulaini, N.A.; Omar, A.K.M. Clinical Solid Waste Management Practices and Its Impact on Human Health and Environment—A Review. Waste Manag. 2011, 31, 754–766. [Google Scholar] [CrossRef]
- Johnson, K.M.; González, M.L.; Dueñas, L.; Gamero, M.; Relyea, G.; Luque, L.E.; Caniza, M.A. Improving Waste Segregation While Reducing Costs in a Tertiary-Care Hospital in a Lower-Middle-Income Country in Central America. Waste Manag. Res. 2013, 31, 733–738. [Google Scholar] [CrossRef]
- Diaz, L.F.; Eggerth, L.L.; Enkhtsetseg, S.; Savage, G.M. Characteristics of Healthcare Wastes. Waste Manag. 2008, 28, 1219–1226. [Google Scholar] [CrossRef]
- Maamari, O.; Brandam, C.; Lteif, R.; Salameh, D. Health Care Waste Generation Rates and Patterns: The Case of Lebanon. Waste Manag. 2015, 43, 550–554. [Google Scholar] [CrossRef] [PubMed]
- Rabeie, O.L.; Miranzadeh, M.B.; Fallah, S.H.; Dehqan, S.; Moulana, Z.; Amouei, A.; Mohammadi, A.A.; Asgharnia, H.A.; Babaie, M. Determination of Hospital Waste Composition and Management in Amol City, Iran. Health Scope 2012, 1, 127–131. [Google Scholar] [CrossRef]
- Phengxay, S.; Okumura, J.; Miyoshi, M.; Sakisaka, K.; Kuroiwa, C.; Phengxay, M. Health-Care Waste Management in Lao PDR: A Case Study. Waste Manag. Res. 2005, 23, 571–581. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Salam, M.M. Hospital Waste Management in El-Beheira Governorate, Egypt. J. Environ. Manag. 2010, 91, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Tesfahun, E.; Kumie, A.; Beyene, A. Developing Models for the Prediction of Hospital Healthcare Waste Generation Rate. Waste Manag. Res. 2016, 34, 75–80. [Google Scholar] [CrossRef]
- Mohee, R. Medical Wastes Characterisation in Healthcare Institutions in Mauritius. Waste Manag. 2005, 25, 575–581. [Google Scholar] [CrossRef]
- Mbarki, A.; Kabbachi, B.; Ezaidi, A.; Benssaou, M.; Mbarki, A.; Kabbachi, B.; Ezaidi, A.; Benssaou, M. Medical Waste Management: A Case Study of the Souss-Massa-Drâa Region, Morocco. J. Environ. Prot. 2013, 4, 914–919. [Google Scholar] [CrossRef]
- World Health Organization. Status of Health-Care Waste Management in Selected Countries of the Western Pacific Region. Available online: https://iris.who.int/bitstream/handle/10665/208230/9789290617228_eng.pdf?sequence=1 (accessed on 6 March 2025).
- Gizalew Snr, E.; Girma Snr, M.; Haftu Snr, D.; Churko, C.; Girma Snr, Z. Health-Care Waste Management and Risk Factors Among Health Professionals in Public Health Facilities of South Omo Zone, South West Ethiopia, 2018. J. Healthc. Leadersh. 2021, 13, 119–128. [Google Scholar] [CrossRef]
- World Health Organization. Global Healthcare Waste Project. MODULE 9: Classification of Healthcare Waste. Available online: https://cdn.who.int/media/docs/default-source/wash-documents/wash-in-hcf/training-modules-in-health-care-waste-management/module-9---classification-of-health-care-waste.pdf?sfvrsn=dd5e4e84_4 (accessed on 8 March 2025).
- Parida, V.K.; Sikarwar, D.; Majumder, A.; Gupta, A.K. An Assessment of Hospital Wastewater and Biomedical Waste Generation, Existing Legislations, Risk Assessment, Treatment Processes, and Scenario during COVID-19. J. Environ. Manag. 2022, 308, 114609. [Google Scholar] [CrossRef]
- Chen, J.; Li, X.; Huang, K.; Eckelman, M.J.; Chertow, M.R.; Jiang, D. Non-Hazardous Industrial Waste in the United States: 100 Million Tonnes of Recoverable Resources. Resour. Conserv. Recycl. 2021, 167, 105369. [Google Scholar] [CrossRef]
- World Health Organization. Safe Management of Wastes from Health-Care Activities. Available online: https://iris.who.int/bitstream/handle/10665/85349/9789241548564_eng.pdf?sequence=1 (accessed on 8 March 2025).
- Tsai, W.-T. Analysis of Medical Waste Management and Impact Analysis of COVID-19 on Its Generation in Taiwan. Waste Manag. Res. 2021, 39, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Nwachukwu, N.C.; Orji, F.A.; Ugbogu, O.C. Health Care Waste Management—Public Health Benefits, and the Need for Effective Environmental Regulatory Surveillance in Federal Republic of Nigeria. In Current Topics in Public Health; IntechOpen: London, UK, 2013; pp. 149–178. ISBN 978-953-51-1121-4. [Google Scholar]
- World Health Organization. Healthcare Waste. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 8 March 2025).
- Zhou, H.; Yu, X.; Alhaskawi, A.; Dong, Y.; Wang, Z.; Jin, Q.; Hu, X.; Liu, Z.; Kota, V.G.; Abdulla, M.H.A.H.; et al. A Deep Learning Approach for Medical Waste Classification. Sci. Rep. 2022, 12, 2159. [Google Scholar] [CrossRef] [PubMed]
- Guidance on Using the European Waste Catalogue (EWC) to Code Waste. Available online: https://www.sepa.org.uk/media/163421/ewc_guidance.pdf (accessed on 28 July 2025).
- European Commission. Radioactive Waste and Spent Fuel. Available online: https://energy.ec.europa.eu/topics/nuclear-energy/radioactive-waste-and-spent-fuel_en?utm_source=chatgpt.com (accessed on 30 August 2025).
- International Committee of the Red Cross. Medical Waste Management. Available online: https://www.icrc.org/sites/default/files/external/doc/en/assets/files/publications/icrc-002-4032.pdf (accessed on 8 March 2025).
- Padmanabhan, K.K.; Barik, D. Health Hazards of Medical Waste and Its Disposal. In Energy from Toxic Organic Waste for Heat and Power Generation; Woodhead Publishing: Cambridge, UK, 2019; pp. 99–118. [Google Scholar]
- Wu, J.; Wang, M.; Yan, H. Status of Waste Disposal of Sharps Outside Medical Institutions for Patients with Diabetes: A Systematic Review. PLoS ONE 2023, 18, e0288993. [Google Scholar] [CrossRef] [PubMed]
- Zaha, D.C.; Bungau, S.; Aleya, S.; Tit, D.M.; Vesa, C.M.; Popa, A.R.; Pantis, C.; Maghiar, O.A.; Bratu, O.G.; Furau, C.; et al. What Antibiotics for What Pathogens? The Sensitivity Spectrum of Isolated Strains in an Intensive Care Unit. Sci. Total Environ. 2019, 687, 118–127. [Google Scholar] [CrossRef]
- Abidar, N.; Tiskat, S.; Zohra, M. Chemical Waste Management in Hospital; Impact on Environment and Health. J. Wet. Health 2020, 1, 36–41. [Google Scholar] [CrossRef]
- Deng, D.; Zhang, L.; Dong, M.; Samuel, R.E.; Ofori-Boadu, A.; Lamssali, M. Radioactive Waste: A Review. Water Environ. Res. 2020, 92, 1818–1825. [Google Scholar] [CrossRef]
- WHO Guideline on the Use of Safety-Engineered Syringes for Intramuscular, Intradermal and Subcutaneous Injections in Health Care Settings. Available online: https://www.ncbi.nlm.nih.gov/books/NBK390471/ (accessed on 8 March 2025).
- Arora, N.K. Injection Practices in India. WHO South-East Asia J. Public Health 2012, 1, 189–200. [Google Scholar] [CrossRef]
- Kazi, W.; Bhuiyan, S. A Systematic Review of the Literature on the Unsafe Injection Practices in the Health-Care Settings and the Associated Blood-Borne Disease Trend: Experiences from Selected South Asian Countries. J. Community Prev. Med. 2018, 1, 1–17. [Google Scholar] [CrossRef]
- Krishna, D.; Sachan, H.K. Hazardous Biomedical Waste Management Scenario in Developing Countries. In Waste Management and Resource Recycling in the Developing World; Elsevier: Amsterdam, The Netherlands, 2023; pp. 505–519. [Google Scholar]
- Pandey, A.; Ahuja, S.; Madan, M.; Asthana, A.K. Bio-Medical Waste Managment in a Tertiary Care Hospital: An Overview. J. Clin. Diagn. Res. 2016, 10, DC01–DC03. [Google Scholar] [CrossRef]
- Mohammed, S.A.; Kahissay, M.H.; Hailu, A.D. Pharmaceuticals Wastage and Pharmaceuticals Waste Management in Public Health Facilities of Dessie Town, North East Ethiopia. PLoS ONE 2021, 16, e0259160. [Google Scholar] [CrossRef]
- Tit, D.M.; Bungau, S.G.; Nistor-Cseppento, D.C.; Copolovici, D.M.; Buhas, C.L. Disposal of Unused Medicines Resulting from Home Treatment in Romania. J. Environ. Prot. Ecol. 2016, 17, 1425–1433. [Google Scholar]
- Bungau, S.; Bungau, C.; Tit, D.M. Studies on the Last Stage of Product Lifecycle Management for a Pharmaceutical Product. J. Environ. Prot. Ecol. 2015, 16, 56–62. [Google Scholar]
- Sasu, S.; Kümmerer, K.; Kranert, M. Assessment of Pharmaceutical Waste Management at Selected Hospitals and Homes in Ghana. Waste Manag. Res. 2012, 30, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Shaaban, H.; Alghamdi, H.S.; Alhamed, N.A.; Alziadi, A.; Mostafa, A. Environmental Contamination by Pharmaceutical Waste: Assessing Patterns of Disposing Unwanted Medications and Investigating the Factors Influencing Personal Disposal Choices. J. Pharmacol. Pharm. Res. 2018, 1, 003. [Google Scholar]
- Ghasemi, L.; Yousefzadeh, S.; Rastkari, N.; Naddafi, K.; Shariati Far, N.; Nabizadeh, R. Evaluate the Types and Amount of Genotoxic Waste in Tehran University of Medical Science’s Hospitals. J. Environ. Health Sci. Eng. 2018, 16, 171–179. [Google Scholar] [CrossRef]
- Stewart, B.W. Mechanisms of Carcinogenesis: From Initiation and Promotion to the Hallmarks. Available online: https://www.ncbi.nlm.nih.gov/books/NBK570326/ (accessed on 8 March 2025).
- McDiarmid, M.A. Chemical Hazards in Health Care: High Hazard, High Risk, but Low Protection. Ann. N. Y. Acad. Sci. 2006, 1076, 601–606. [Google Scholar] [CrossRef]
- National Library of Medicine. PubChem. Available online: https://pubchem.ncbi.nlm.nih.gov/ (accessed on 8 March 2025).
- Lee, S.; Kim, Y.; Park, J.; Shon, H.K.; Hong, S. Treatment of Medical Radioactive Liquid Waste Using Forward Osmosis (FO) Membrane Process. J. Memb. Sci. 2018, 556, 238–247. [Google Scholar] [CrossRef]
- Khobragade, D. Health Care Waste: Avoiding Hazards to Living and Non Living Environment by Efficient Management. Fortune J. Health Sci. 2019, 2, 14–29. [Google Scholar] [CrossRef]
- Aljabre, S.H.M. Hospital Generated Waste: A Plan for Its Proper Management. J. Family Community Med. 2002, 9, 61–65. [Google Scholar] [CrossRef]
- Aziz, H.A.; Omar, F.M.; Halim, H.A.; Hung, Y.-T. Health-Care Waste Management. In Solid Waste Engineering and Management; Springer International Publishing: Cham, Switzerland, 2022; pp. 180–251. [Google Scholar]
- Andeobu, L. Medical Waste and Its Management. In The Palgrave Handbook of Global Sustainability; Springer: Berlin/Heidelberg, Germany, 2023; Volume 1–3, pp. 761–789. [Google Scholar]
- Bokhoree, C.; Beeharry, Y.; Makoondlall-Chadee, T.; Doobah, T.; Soomary, N. Assessment of Environmental and Health Risks Associated with the Management of Medical Waste in Mauritius. APCBEE Procedia 2014, 9, 36–41. [Google Scholar] [CrossRef]
- Minoglou, M.; Gerassimidou, S.; Komilis, D. Healthcare Waste Generation Worldwide and Its Dependence on Socio-Economic and Environmental Factors. Sustainability 2017, 9, 220. [Google Scholar] [CrossRef]
- Slutzman, J.E.; Bockius, H.; Gordon, I.O.; Greene, H.C.; Hsu, S.; Huang, Y.; Lam, M.H.; Roberts, T.; Thiel, C.L. Waste Audits in Healthcare: A Systematic Review and Description of Best Practices. Waste Manag. Res. 2023, 41, 3–17. [Google Scholar] [CrossRef]
- Minoglou, M.; Komilis, D. Describing Health Care Waste Generation Rates Using Regression Modeling and Principal Component Analysis. Waste Manag. 2018, 78, 811–818. [Google Scholar] [CrossRef]
- Kumar, R.; Khan, E.; Ahmed, J.; Khan, Z.; Magan, M.; Nousheen; Mughal, M. Healthcare Waste Management (HCWM) in Pakistan:Current Situation and Training Options. J. Ayub Med. Coll. Abbottabad 2010, 22, 101–105. [Google Scholar]
- Mol, M.P.G.; Zolnikov, T.R.; Neves, A.C.; dos Santos, G.R.; Tolentino, J.L.L.; de Vasconcelos Barros, R.T.; Heller, L. Healthcare Waste Generation in Hospitals per Continent: A Systematic Review. Environ. Sci. Pollut. Res. 2022, 29, 42466–42475. [Google Scholar] [CrossRef]
- Mwaria, P.R.; Kaseva, M.; Manyele, S. Characterization of Healthcare Waste in Tanzanian Zonal Referral Hospitals as a Key Factor for Energy Recovery. Afr. J. Environ. Sci. Technol. 2021, 15, 349–365. [Google Scholar] [CrossRef]
- Ramodipa, T.; Engelbrecht, K.; Mokgobu, I.; Mmereki, D. Status of Health Care Waste Management Plans and Practices in Public Health Care Facilities in Gauteng Province, South Africa. BMC Public Health 2023, 23, 246. [Google Scholar] [CrossRef]
- Sepetis, A.; Zaza, P.N.; Rizos, F.; Bagos, P.G. Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector. Int. J. Environ. Res. Public Health 2022, 19, 9821. [Google Scholar] [CrossRef]
- Singh, N.; Ogunseitan, O.A.; Tang, Y. Medical Waste: Current Challenges and Future Opportunities for Sustainable Management. Crit. Rev. Environ. Sci. Technol. 2022, 52, 2000–2022. [Google Scholar] [CrossRef]
- Bdour, A.; Altrabsheh, B.; Hadadin, N.; Al-Shareif, M. Assessment of Medical Wastes Management Practice: A Case Study of the Northern Part of Jordan. Waste Manag. 2007, 27, 746–759. [Google Scholar] [CrossRef]
- Gai, R.; Kuroiwa, C.; Xu, L.; Wang, X.; Zhang, Y.; Li, H.; Zhou, C.; He, J.; Tang, W. Hospital Medical Waste Management in Shandong Province, China. Waste Manag. Res. 2009, 27, 336–342. [Google Scholar]
- Zhang, H.-J.; Zhang, Y.-H.; Wang, Y.; Yang, Y.-H.; Zhang, J.; Wang, Y.-L.; Wang, J.-L. Investigation of Medical Waste Management in Gansu Province, China. Waste Manag. Res. 2013, 31, 655–659. [Google Scholar] [CrossRef]
- Patil, G.V.; Pokhrel, K. Biomedical Solid Waste Management in an Indian Hospital: A Case Study. Waste Manag. 2005, 25, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Cheng, L.; Khan, A.A.; Ahmed, H. Healthcare Waste Management in Asian Developing Countries: A Mini Review. Waste Manag. Res. 2019, 37, 863–875. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, C.E.; Hoppe, A.E.; Ravanello, M.M.; Mello, N. Medical Wastes Management in the South of Brazil. Waste Manag. 2005, 25, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Wassie, B.; Gintamo, B.; Mekuria, Z.N.; Gizaw, Z. Healthcare Waste Management Practices and Associated Factors in Private Clinics in Addis Ababa, Ethiopia. Environ. Health Insights 2022, 16, 11786302211073384. [Google Scholar] [CrossRef]
- Saad, S.A.G. Management of Hospitals Solid Waste in Khartoum State. Environ. Monit. Assess. 2013, 185, 8567–8582. [Google Scholar] [CrossRef]
- Li, H.; Dietl, H.; Li, J. Identifying Key Factors Influencing Sustainable Element in Healthcare Waste Management Using the Interval-Valued Fuzzy DEMATEL Method. J. Mater. Cycles Waste Manag. 2021, 23, 1777–1790. [Google Scholar] [CrossRef]
- Zhao, H.; Liu, H.; Wei, G.; Wang, H.; Zhu, Y.; Zhang, R.; Yang, Y. Comparative Life Cycle Assessment of Emergency Disposal Scenarios for Medical Waste during the COVID-19 Pandemic in China. Waste Manag. 2021, 126, 388–399. [Google Scholar] [CrossRef]
- Wang, F.; Yu, L.; Long, J.; Bu, H.; He, C.; Wu, A. Quantifying the Spatiotemporal Evolution Characteristics of Medical Waste Generation during the Outbreak of Public Health Emergencies. J. Mater. Cycles Waste Manag. 2023, 25, 221–234. [Google Scholar] [CrossRef]
- Martins, M.A.; Pataca, L.C.M.; Santos, E.d.S.; Faria, S.M.d.C.; Cruz, L.A.; Silva, G.A.S.; Mol, M.P.G. Generation of Infectious Waste during the COVID-19 Pandemic: The Case of a Brazilian Hospital. Waste Manag. Res. 2021, 39, 1245–1255. [Google Scholar] [CrossRef]
- Kaposi, A.; Nagy, A.; Gomori, G.; Kocsis, D. Analysis of Healthcare Waste and Factors Affecting the Amount of Hazardous Healthcare Waste in a University Hospital. J. Mater. Cycles Waste Manag. 2024, 26, 1169–1180. [Google Scholar] [CrossRef]
- Voudrias, E.A. Management of COVID-19 Healthcare Waste Based on the Circular Economy Hierarchy: A Critical Review. Waste Manag. Res. 2023, 42, 977–996. [Google Scholar] [CrossRef] [PubMed]
- Ranjbari, M.; Shams Esfandabadi, Z.; Shevchenko, T.; Chassagnon-Haned, N.; Peng, W.; Tabatabaei, M.; Aghbashlo, M. Mapping Healthcare Waste Management Research: Past Evolution, Current Challenges, and Future Perspectives towards a Circular Economy Transition. J. Hazard. Mater. 2022, 422, 126724. [Google Scholar] [CrossRef] [PubMed]
- Cirstea, I.; Radu, A.-F.; Tit, D.M.; Radu, A.; Bungau, G.; Negru, P.A. Bibliometric Analysis of Medical Waste Research Using Python-Driven Algorithm. Algorithms 2025, 18, 312. [Google Scholar] [CrossRef]
- United Nations Environment Programme. Waste Management During the COVID-19 Pandemic from Response to Recovery. Available online: https://wedocs.unep.org/bitstream/handle/20.500.11822/33416/WMC-19.pdf?sequence=1&isAllowed=y (accessed on 9 March 2025).
- Hasan, M.M.; Rahman, M.H. Assessment of Healthcare Waste Management Paradigms and Its Suitable Treatment Alternative: A Case Study. J. Environ. Public Health 2018, 2018, 6879751. [Google Scholar] [CrossRef]
- Abu Qdais, H.; Rabi, A.; Abdulla, F. Characteristics of the Medical Waste Generated at the Jordanian Hospitals. Clean Technol. Environ. Policy 2007, 9, 147–152. [Google Scholar] [CrossRef]
- Almomani, H.; Obaidat, M.; Khazaleh, A.; Muneizel, O.; Afyouni, N.; Fayyad, S. Review of Medical Waste Management in Jordanian Health Care Organisations. Br. J. Healthc. Manag. 2019, 25, 1–8. [Google Scholar]
- Suarez Rivadeneira, J.E.; Suarez Chavarry, E.B.; Ramirez, Í.M.; Camacho, W.R.; Calderón, E.V.; Astonitas, R.P.; Acosta, R.C.S.C.; Eli, M.-R.; Ventura, H.K.M.; Musayón Díaz, M.P. Generation Rate of Hospital Solid Waste from Different Services: A Case Study in the Province of Bagua, Northern Peru. Heliyon 2024, 10, e31814. [Google Scholar] [CrossRef]
- Korkut, E.N. Estimations and Analysis of Medical Waste Amounts in the City of Istanbul and Proposing a New Approach for the Estimation of Future Medical Waste Amounts. Waste Manag. 2018, 81, 168–176. [Google Scholar] [CrossRef]
- Aleisa, E.; Al-Jarallah, R. Characterization of Municipal Solid Waste in Kuwait: Sector-Specific Composition Analysis and Implications. J. Air Waste Manag. Assoc. 2024, 74, 623–638. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Kuwait. Manual for Safe Management of Wastes from Health-Care Activities. Available online: http://icdkwt.com/pdf/policiesandguidelines/ICforSupportiveServices/wastemanagement.pdf (accessed on 10 March 2025).
- Amariglio, A.; Depaoli, D. Waste Management in an Italian Hospital’s Operating Theatres: An Observational Study. Am. J. Infect. Control 2021, 49, 184–187. [Google Scholar] [CrossRef]
- Meleko, A.; Tesfaye, T.; Henok, A. Assessment of Healthcare Waste Generation Rate and Its Management System in Health Centers of Bench Maji Zone. Ethiop. J. Health Sci. 2018, 28, 125–134. [Google Scholar] [CrossRef]
- Sangkham, S. Face Mask and Medical Waste Disposal during the Novel COVID-19 Pandemic in Asia. Case Stud. Chem. Environ. Eng. 2020, 2, 100052. [Google Scholar] [CrossRef]
- Arab, M.; Baghbani, R.A.; Tajvar, M.; Pourreza, A.; Omrani, G.; Mahmoudi, M. Report: The Assessment of Hospital Waste Management:A Case Study in Tehran. Waste Manag. Res. 2008, 26, 304–308. [Google Scholar] [CrossRef]
- Sharma, H.B.; Vanapalli, K.R.; Cheela, V.S.; Ranjan, V.P.; Jaglan, A.K.; Dubey, B.; Goel, S.; Bhattacharya, J. Challenges, Opportunities, and Innovations for Effective Solid Waste Management during and Post COVID-19 Pandemic. Resour. Conserv. Recycl. 2020, 162, 105052. [Google Scholar] [CrossRef]
- Awodele, O.; Adewoye, A.A.; Oparah, A.C. Assessment of Medical Waste Management in Seven Hospitals in Lagos, Nigeria. BMC Public Health 2016, 16, 269. [Google Scholar] [CrossRef]
- Ozder, A.; Teker, B.; Eker, H.H.; Altındis, S.; Kocaakman, M.; Karabay, O. Medical Waste Management Training for Healthcare Managers—A Necessity? J. Environ. Health Sci. Eng. 2013, 11, 20. [Google Scholar] [CrossRef]
- Parida, A.; Capoor, M.R.; Bhowmik, K.T. Knowledge, Attitude, and Practices of Bio-Medical Waste Management Rules, 2016; Bio-Medical Waste Management (Amendment) Rules, 2018; and Solid Waste Rules, 2016, among Health-Care Workers in a Tertiary Care Setup. J. Lab. Physicians 2019, 11, 292–299. [Google Scholar] [CrossRef]
- Pandey, S.; Dwivedi, A. Nosocomial Infections through Hospital Waste. Int. J. Waste Resour. 2016, 6, 1000200. [Google Scholar] [CrossRef]
- Han, J.; He, S.; Shao, W.; Wang, C.; Qiao, L.; Zhang, J.; Yang, L. Municipal Solid Waste, an Overlooked Route of Transmission for the Severe Acute Respiratory Syndrome Coronavirus 2: A Review. Environ. Chem. Lett. 2023, 21, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Yazie, T.D.; Tebeje, M.G.; Chufa, K.A. Healthcare Waste Management Current Status and Potential Challenges in Ethiopia: A Systematic Review. BMC Res. Notes 2019, 12, 285. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Occupational Safety and Health. Chain of Infection Components. Available online: https://www.cdc.gov/niosh/learning/safetyculturehc/module-2/3.html (accessed on 10 March 2025).
- Dehghani, M.H.; Omrani, G.A.; Karri, R.R. Solid Waste—Sources, Toxicity, and Their Consequences to Human Health. In Soft Computing Techniques in Solid Waste and Wastewater Management; Karri, R.R., Ravindran, G., Dehghani, M.H., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 205–213. [Google Scholar]
- Gańczak, M.; Milona, M.; Szych, Z. Nurses and Occupational Exposures to Bloodborne Viruses in Poland. Infect. Control Hosp. Epidemiol. 2006, 27, 175–180. [Google Scholar] [CrossRef]
- Jahangiri, M.; Rostamabadi, A.; Hoboubi, N.; Tadayon, N.; Soleimani, A. Needle Stick Injuries and Their Related Safety Measures among Nurses in a University Hospital, Shiraz, Iran. Saf. Health Work 2016, 7, 72–77. [Google Scholar] [CrossRef]
- Singh, N.; Tang, Y.; Ogunseitan, O.A. Environmentally Sustainable Management of Used Personal Protective Equipment. Environ. Sci. Technol. 2020, 54, 8500–8502. [Google Scholar] [CrossRef]
- Anagaw, B.; Shiferaw, Y.; Anagaw, B.; Belyhun, Y.; Erku, W.; Biadgelegn, F.; Moges, B.; Alemu, A.; Moges, F.; Mulu, A. Seroprevalence of Hepatitis B and C Viruses among Medical Waste Handlers at Gondar Town Health Institutions, Northwest Ethiopia. BMC Res. Notes 2012, 5, 55. [Google Scholar] [CrossRef]
- Alemayehu, T.; Worku, A.; Assefa, N. Medical Waste Collectors in Eastern Ethiopia Are Exposed to High Sharp Injury and Blood and Body Fluids Contamination. J. Prev. Infect. Control 2016, 2, 1–10. [Google Scholar] [CrossRef]
- Ghanei Gheshlagh, R.; Aslani, M.; Shabani, F.; Dalvand, S.; Parizad, N. Prevalence of Needlestick and Sharps Injuries in the Healthcare Workers of Iranian Hospitals: An Updated Meta-Analysis. Environ. Health Prev. Med. 2018, 23, 44. [Google Scholar] [CrossRef]
- Udofia, E.A.; Gulis, G.; Fobil, J. Solid Medical Waste: A Cross Sectional Study of Household Disposal Practices and Reported Harm in Southern Ghana. BMC Public Health 2017, 17, 464. [Google Scholar] [CrossRef]
- Blenkharn, J.I.; Odd, C. Sharps Injuries in Healthcare Waste Handlers. Ann. Occup. Hyg. 2008, 52, 281–286. [Google Scholar] [CrossRef][Green Version]
- Marfe, G.; Di Stefano, C. Risks and Challenges of Hazardous Waste Management: Reviews and Case Studies; Bentham Science Publishers: Sharjah, United Arab Emirates, 2020; ISBN 978-981-14-7248-0. [Google Scholar][Green Version]
- Bungau, S.; Tit, D.M.; Fodor, K.; Cioca, G.; Agop, M.; Iovan, C.; Cseppento, D.C.; Bumbu, A.; Bustea, C. Aspects Regarding the Pharmaceutical Waste Management in Romania. Sustainability 2018, 10, 2788. [Google Scholar] [CrossRef]
- Sangion, A.; Gramatica, P. Hazard of Pharmaceuticals for Aquatic Environment: Prioritization by Structural Approaches and Prediction of Ecotoxicity. Environ. Int. 2016, 95, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Kmmerer, K. Pharmaceuticals in the Environment. Annu. Rev. Environ. Resour. 2010, 35, 57–75. [Google Scholar] [CrossRef]
- Barathe, P.; Kaur, K.; Reddy, S.; Shriram, V.; Kumar, V. Antibiotic Pollution and Associated Antimicrobial Resistance in the Environment. J. Hazard. Mater. Lett. 2024, 5, 100105. [Google Scholar] [CrossRef]
- Anand, U.; Reddy, B.; Singh, V.K.; Singh, A.K.; Kesari, K.K.; Tripathi, P.; Kumar, P.; Tripathi, V.; Simal-Gandara, J. Potential Environmental and Human Health Risks Caused by Antibiotic-Resistant Bacteria (ARB), Antibiotic Resistance Genes (ARGs) and Emerging Contaminants (ECs) from Municipal Solid Waste (MSW) Landfill. Antibiotics 2021, 10, 374. [Google Scholar] [CrossRef] [PubMed]
- Adeel, M.; Song, X.; Wang, Y.; Francis, D.; Yang, Y. Environmental Impact of Estrogens on Human, Animal and Plant Life: A Critical Review. Environ. Int. 2017, 99, 107–119. [Google Scholar] [CrossRef]
- Marlatt, V.L.; Bayen, S.; Castaneda-Cortès, D.; Delbès, G.; Grigorova, P.; Langlois, V.S.; Martyniuk, C.J.; Metcalfe, C.D.; Parent, L.; Rwigemera, A.; et al. Impacts of Endocrine Disrupting Chemicals on Reproduction in Wildlife and Humans. Environ. Res. 2022, 208, 112584. [Google Scholar] [CrossRef]
- Lerdsuwanrut, N.; Zamani, R.; Akrami, M. Environmental and Human Health Risks of Estrogenic Compounds: A Critical Review of Sustainable Management Practices. Sustainability 2025, 17, 491. [Google Scholar] [CrossRef]
- Ibarluzea, J.M.; Fernández, M.F.; Santa-Marina, L.; Olea-Serrano, M.F.; Rivas, A.M.; Aurrekoetxea, J.J.; Expósito, J.; Lorenzo, M.; Torné, P.; Villalobos, M.; et al. Breast Cancer Risk and the Combined Effect of Environmental Estrogens. Cancer Causes Control 2004, 15, 591–600. [Google Scholar] [CrossRef]
- Xia, Y.; Chen, M.; Zhu, P.; Lu, C.; Fu, G.; Zhou, X.; Chen, D.; Wang, H.; Hang, B.; Wang, S.; et al. Urinary Phytoestrogen Levels Related to Idiopathic Male Infertility in Chinese Men. Environ. Int. 2013, 59, 161–167. [Google Scholar] [CrossRef]
- Gonsioroski, A.; Mourikes, V.E.; Flaws, J.A. Endocrine Disruptors in Water and Their Effects on the Reproductive System. Int. J. Mol. Sci. 2020, 21, 1929. [Google Scholar] [CrossRef]
- Connor, T.H.; Lawson, C.C.; Polovich, M.; McDiarmid, M.A. Reproductive Health Risks Associated with Occupational Exposures to Antineoplastic Drugs in Health Care Settings: A Review of the Evidence. J. Occup. Environ. Med. 2014, 56, 901–910. [Google Scholar] [CrossRef]
- Phillips, D.H.; Arlt, V.M. Genotoxicity: Damage to DNA and Its Consequences. EXS 2009, 99, 87–110. [Google Scholar] [PubMed]
- Shahrasbi, A.A.; Afshar, M.; Shokraneh, F.; Monji, F.; Noroozi, M.; Ebrahimi-Khojin, M.; Madani, S.F.; Ahadi-Barzoki, M.; Rajabi, M. Risks to Health Professionals from Hazardous Drugs in Iran: A Pilot Study of Understanding of Healthcare Team to Occupational Exposure to Cytotoxics. EXCLI J. 2014, 13, 491–501. [Google Scholar] [PubMed]
- Capoor, M.R.; Bhowmik, K.T. Cytotoxic Drug Dispersal, Cytotoxic Safety, and Cytotoxic Waste Management: Practices and Proposed India-Specific Guidelines. Indian J. Med. Paediatr. Oncol. 2017, 38, 190–197. [Google Scholar] [PubMed]
- Simegn, W.; Dagnew, B.; Dagne, H. Knowledge and Associated Factors towards Cytotoxic Drug Handling among University of Gondar Comprehensive Specialized Hospital Health Professionals, Institutional-Based Cross-Sectional Study. Environ. Health Prev. Med. 2020, 25, 11. [Google Scholar] [CrossRef]
- Doggalli, D.N. Hazards and Public Health Impacts of Hospital Waste. J. Appl. Res. 2014, 4, 384. [Google Scholar]
- Fazzo, L.; Minichilli, F.; Santoro, M.; Ceccarini, A.; Della Seta, M.; Bianchi, F.; Comba, P.; Martuzzi, M. Hazardous Waste and Health Impact: A Systematic Review of the Scientific Literature. Environ. Health 2017, 16, 107. [Google Scholar] [CrossRef]
- Greenwood, J.E.; Tan, J.L.; Ming, J.C.T.; Abell, A.D. Alkalis and Skin. J. Burn Care Res. 2016, 37, 135–141. [Google Scholar] [CrossRef]
- Basketter, D.; Jírova, D.; Kandárová, H. Review of Skin Irritation/Corrosion Hazards on the Basis of Human Data: A Regulatory Perspective. Interdiscip. Toxicol. 2012, 5, 98–104. [Google Scholar] [CrossRef]
- Chemical Laboratory Safety and Security: A Guide to Developing Standard Operating Procedures. Available online: https://www.ncbi.nlm.nih.gov/books/NBK379133/ (accessed on 11 March 2025).
- Gupta, P.K. Solvents, Gasses, and Vapors; Springer: Cham, Switzerland, 2020; ISBN 978-3-030-50408-3. [Google Scholar]
- Nabulo, G.; Black, C.R.; Young, S.D. Trace Metal Uptake by Tropical Vegetables Grown on Soil Amended with Urban Sewage Sludge. Environ. Pollut. 2011, 159, 368–376. [Google Scholar] [CrossRef]
- Filipoiu, D.C.; Bungau, S.G.; Endres, L.; Negru, P.A.; Bungau, A.F.; Pasca, B.; Radu, A.F.; Tarce, A.G.; Bogdan, M.A.; Behl, T.; et al. Characterization of the Toxicological Impact of Heavy Metals on Human Health in Conjunction with Modern Analytical Methods. Toxics 2022, 10, 716. [Google Scholar] [CrossRef]
- World Health Organization. Mercury in Health Care. Policy Paper. Available online: https://iris.who.int/bitstream/handle/10665/69129/WHO_SDE_WSH_05.08.pdf?sequence=1 (accessed on 11 March 2025).
- Peshin, S.S.; Halder, N.; Jathikarta, C.; Gupta, Y.K. Use of Mercury-Based Medical Equipment and Mercury Content in Effluents of Tertiary Care Hospitals in India. Environ. Monit. Assess. 2015, 187, 145. [Google Scholar] [CrossRef]
- Chadli-Debbiche, A.; Allani, R.; Jouini, R.; Abidi, E.; Nouri, A.; Laouini, S.; Ghrabi, A.; Mekni, L.; Chouchene, A.; Siala-Makni, A.; et al. Mercurial Hospital Waste: Management, Becoming and Recommendations. Tunis. Med. 2018, 96, 273–280. [Google Scholar] [PubMed]
- United States Environmental Protection Agency. Mercury in Batteries. Available online: https://www.epa.gov/mercury/mercury-batteries (accessed on 11 March 2025).
- Berlin, M. Mercury in Dental Amalgam: A Risk Analysis. Neurotoxicology 2020, 81, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Steck, M.B.; Murray, B.P. Silver Toxicity. Available online: https://www.ncbi.nlm.nih.gov/books/NBK604211/ (accessed on 11 March 2025).
- Morim, A.; Guldner, G.T. Chlorine Gas Toxicity. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537213/ (accessed on 11 March 2025).
- Mrema, E.J.; Rubino, F.M.; Colosio, C. Obsolete Pesticides—A Threat to Environment, Biodiversity and Human Health BT—Environmental Security Assessment and Management of Obsolete Pesticides in Southeast Europe; Simeonov, L.I., Macaev, F.Z., Simeonova, B.G., Eds.; Springer: Dordrecht, The Netherlands, 2013; ISBN 978-94-007-6461-3. [Google Scholar]
- Shekhar, C.; Khosya, R.; Thakur, K.; Mahajan, D.; Kumar, R.; Kumar, S.; Sharma, A.K. A Systematic Review of Pesticide Exposure, Associated Risks, and Long-Term Human Health Impacts. Toxicol. Rep. 2024, 13, 101840. [Google Scholar] [CrossRef]
- Comparative Toxicogenomics Database. Available online: https://ctdbase.org/ (accessed on 11 March 2025).
- Zhang, X.; Gu, P.; Liu, Y. Decontamination of Radioactive Wastewater: State of the Art and Challenges Forward. Chemosphere 2019, 215, 543–553. [Google Scholar] [CrossRef]
- Khan, S.; Syed, A.; Ahmad, R.; Rather, T.A.; Ajaz, M.; Jan, F. Radioactive Waste Management in a Hospital. Int. J. Health Sci. 2010, 4, 39–46. [Google Scholar]
- Borowy, I. Medical Waste: The Dark Side of Healthcare. Hist. Cienc. Saude. Manguinhos. 2020, 27, 231–251. [Google Scholar] [CrossRef]
- Yang, T.; Du, Y.; Sun, M.; Meng, J.; Li, Y. Risk Management for Whole-Process Safe Disposal of Medical Waste: Progress and Challenges. Risk Manag. Healthc. Policy 2024, 17, 1503–1522. [Google Scholar] [CrossRef]
- Franchini, M.; Rial, M.; Buiatti, E.; Bianchi, F. Health Effects of Exposure to Waste Incinerator Emissions: A Review of Epidemiological Studies. Ann. Ist. Super. Sanita 2004, 40, 101–115. [Google Scholar]
- Bolan, S.; Padhye, L.P.; Kumar, M.; Antoniadis, V.; Sridharan, S.; Tang, Y.; Singh, N.; Hewawasam, C.; Vithanage, M.; Singh, L.; et al. Review on Distribution, Fate, and Management of Potentially Toxic Elements in Incinerated Medical Wastes. Environ. Pollut. 2023, 321, 121080. [Google Scholar] [CrossRef]
- Loganathan, B.G.; Masunaga, S. PCBs, Dioxins, and Furans: Human Exposure and Health Effects. In Handbook of Toxicology of Chemical Warfare Agents, 3rd ed.; Gupta, R.C., Ed.; Academic Press: Boston, MA, USA, 2020; pp. 267–278. ISBN 978-0-12-819090-6. [Google Scholar]
- Kirkok, S.K.; Kibet, J.K.; Kinyanjui, T.K.; Okanga, F.I. A Review of Persistent Organic Pollutants: Dioxins, Furans, and Their Associated Nitrogenated Analogues. SN Appl. Sci. 2020, 2, 1729. [Google Scholar] [CrossRef]
- Bhandari, G.; Chaudhary, P.; Gangola, S.; Gupta, S.; Gupta, A.; Rafatullah, M.; Chen, S. A Review on Hospital Wastewater Treatment Technologies: Current Management Practices and Future Prospects. J. Water Process Eng. 2023, 56, 104516. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Noncommunicable Diseases. 2014. Available online: https://www.who.int/publications/i/item/9789241564854 (accessed on 15 October 2023).
- Mattiello, A.; Chiodini, P.; Bianco, E.; Forgione, N.; Flammia, I.; Gallo, C.; Pizzuti, R.; Panico, S. Health Effects Associated with the Disposal of Solid Waste in Landfills and Incinerators in Populations Living in Surrounding Areas: A Systematic Review. Int. J. Public Health 2013, 58, 725–735. [Google Scholar] [CrossRef]
- Eze, C.; Vinken, M. E-Waste: Mechanisms of Toxicity and Safety Testing. FEBS Open Bio 2024, 14, 1420–1440. [Google Scholar] [CrossRef] [PubMed]
- Woodham, A.W.; Skeate, J.G.; Sanna, A.M.; Taylor, J.R.; Da Silva, D.M.; Cannon, P.M.; Kast, W.M. Human Immunodeficiency Virus Immune Cell Receptors, Coreceptors, and Cofactors: Implications for Prevention and Treatment. AIDS Patient Care STDS 2016, 30, 291–306. [Google Scholar] [CrossRef] [PubMed]
- Saeed, U.; Waheed, Y.; Ashraf, M. Hepatitis B and Hepatitis C Viruses: A Review of Viral Genomes, Viral Induced Host Immune Responses, Genotypic Distributions and Worldwide Epidemiology. Asian Pacific J. Trop. Dis. 2014, 4, 88–96. [Google Scholar] [CrossRef]
- Ali, S.S.; Ali, A.; Elsamahy, T.; Okasha, K.M.; Sun, J. Toxicity Consideration of Antibiotics. In Antibiotics—Therapeutic Spectrum and Limitations Developments in Microbiology; Dhara, A.K., Nayak, A.K., Chattopadhyay, D., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 297–328. ISBN 978-0-323-95388-7. [Google Scholar]
- Bracci, L.; Schiavoni, G.; Sistigu, A.; Belardelli, F. Immune-Based Mechanisms of Cytotoxic Chemotherapy: Implications for the Design of Novel and Rationale-Based Combined Treatments against Cancer. Cell Death Differ. 2014, 21, 15–25. [Google Scholar] [CrossRef]
- Petejova, N.; Martinek, A.; Zadrazil, J.; Teplan, V. Acute Toxic Kidney Injury. Ren. Fail. 2019, 41, 576–594. [Google Scholar] [CrossRef]
- Eve, L.; Fervers, B.; Le Romancer, M.; Etienne-Selloum, N. Exposure to Endocrine Disrupting Chemicals and Risk of Breast Cancer. Int. J. Mol. Sci. 2020, 21, 9139. [Google Scholar] [CrossRef]
- Posin, S.L.; Kong, W.L.; Sandeep, S. Mercury Toxicity. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499935/ (accessed on 11 March 2025).
- Bernhoft, R.A. Mercury Toxicity and Treatment: A Review of the Literature. J. Environ. Public Health 2012, 2012, 460508. [Google Scholar] [CrossRef]
- Toxicological Profile for Chlorine. Available online: https://www.ncbi.nlm.nih.gov/books/NBK598759/ (accessed on 11 March 2025).
- Mnif, W.; Hassine, A.I.H.; Bouaziz, A.; Bartegi, A.; Thomas, O.; Roig, B. Effect of Endocrine Disruptor Pesticides: A Review. Int. J. Environ. Res. Public Health 2011, 8, 2265–2303. [Google Scholar] [PubMed]
- Garud, A.; Pawar, S.; Patil, M.S.; Kale, S.R.; Patil, S. A Scientific Review of Pesticides: Classification, Toxicity, Health Effects, Sustainability, and Environmental Impact. Cureus 2024, 16, e67945. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yang, Y.; He, X.; Yang, P.; Zong, T.; Sun, P.; Sun, R.-C.; Yu, T.; Jiang, Z. The Cellular Function and Molecular Mechanism of Formaldehyde in Cardiovascular Disease and Heart Development. J. Cell Mol. Med. 2021, 25, 5358–5371. [Google Scholar] [PubMed]
- Heston, T.F.; Tafti, D. Nuclear Medicine Safety. Available online: https://www.ncbi.nlm.nih.gov/books/NBK603730/ (accessed on 11 March 2025).
- Marques, C.T.; Fritzen Gomes, B.M. Reuse, Reduce, Recycle BT—Responsible Consumption and Production. In Responsible Consumption and Production; Leal Filho, W., Azul, A.M., Brandli, L., Özuyar, P.G., Wall, T., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 626–634. ISBN 978-3-319-95726-5. [Google Scholar]
- Conrardy, J.; Hillanbrand, M.; Myers, S.; Nussbaum, G.F. Reducing Medical Waste. AORN J. 2010, 91, 711–721. [Google Scholar] [CrossRef]
- Klemeš, J.J.; van Fan, Y.; Tan, R.R.; Jiang, P. Minimising the Present and Future Plastic Waste, Energy and Environmental Footprints Related to COVID-19. Renew. Sustain. Energy Rev. 2020, 127, 109883. [Google Scholar] [CrossRef]
- Kheirabadi, S.; Sheikhi, A. Recent Advances and Challenges in Recycling and Reusing Biomedical Materials. Curr. Opin. Green Sustain. Chem. 2022, 38, 100695. [Google Scholar] [CrossRef]
- Reid, S.; Juma, O.A. Minimum Infective Dose of HIV for Parenteral Dosimetry. Int. J. STD AIDS 2009, 20, 828–833. [Google Scholar] [CrossRef]
- Solon, J.G.; Killeen, S. Decontamination and Sterilization. Surgery 2019, 37, 51–57. [Google Scholar]
- Mazzei, H.G.; Specchia, S. Latest Insights on Technologies for the Treatment of Solid Medical Waste: A Review. J. Environ. Chem. Eng. 2023, 11, 109309. [Google Scholar] [CrossRef]
- Giakoumakis, G.; Politi, D.; Sidiras, D. Medical Waste Treatment Technologies for Energy, Fuels, and Materials Production: A Review. Energies 2021, 14, 8065. [Google Scholar] [CrossRef]
- Sanjeev Salvi, S.; Waghmare, S.; Thombare, V.; Mandlik, S.; Veer, S.; Walke, P.; Zambare, P.; Professor, A. Review on Bio-Medical Waste Management. Int. J. Eng. Res. Technol. 2022, 1, 63–69. [Google Scholar]
- Capoor, M.R.; Bhowmik, K.T. Current Perspectives on Biomedical Waste Management: Rules, Conventions and Treatment Technologies. Indian J. Med. Microbiol. 2017, 35, 157–164. [Google Scholar] [CrossRef] [PubMed]
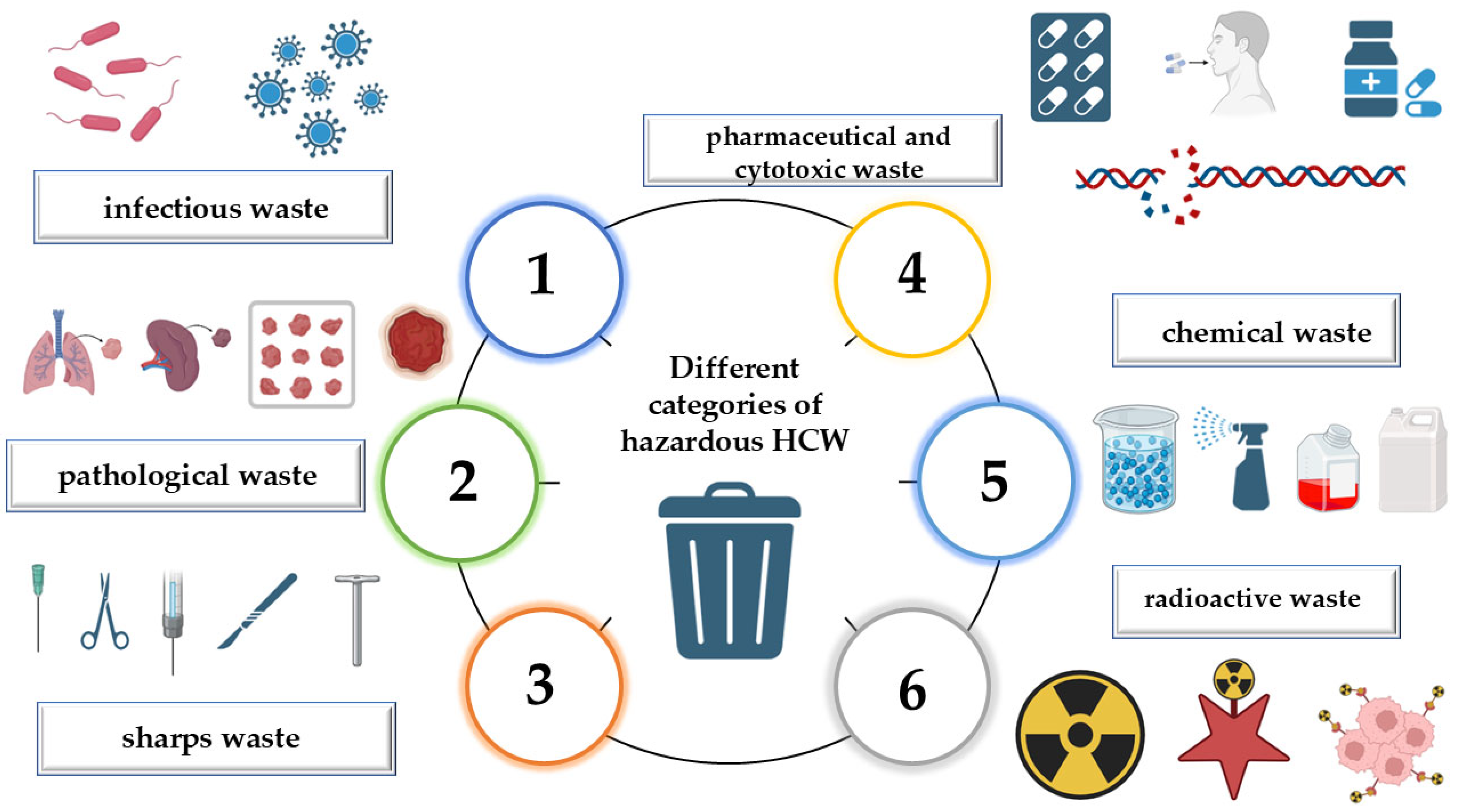
| Type of HCW | Examples | Description | Risks Associated | Refs. |
|---|---|---|---|---|
| Infectious | Wastewater and materials contaminated with blood or bodily fluids, including laboratory cultures, microbiological stocks, and items from isolation wards used for highly infectious patients | This category includes materials that may facilitate the spread of infectious microorganisms, such as cultures of pathogens and waste from quarantined patients with contagious diseases | Potential to contain pathogenic microorganisms capable of transmitting diseases to humans upon exposure | [27,31] |
| Pathological | Human remains such as tissues, organs, and fluids, as well as contaminated animal carcasses, fetal tissue, and unused blood products | Organic waste that contains bodily fluids, excreta, or blood, which can contribute to contamination if not managed correctly | May carry infectious agents that could spread diseases, particularly when sourced from infected individuals or animals. Inadequate disposal can lead to environmental contamination, affecting soil and water quality | [32] |
| Sharps waste | Needles, syringes, scalpels, infusion sets, pipettes, blades, broken glass, and other sharp medical instruments | There is limited research on the disposal of sharps in non-clinical environments, and incorrect disposal increases the likelihood of needle-stick injuries | Sharp objects can puncture or lacerate the skin, allowing direct exposure to infectious agents. Used needles and syringes frequently harbor bloodborne pathogens such as Human Immunodeficiency Virus (HIV), Hepatitis B, and Hepatitis C | [33] |
| Pharmaceutical and cytotoxic waste | Expired or unused medications, drug-contaminated materials, and cytotoxic waste containing substances with genotoxic properties, including chemotherapy drugs | Cytotoxic waste remains hazardous even after disposal due to its potential to cause genetic mutations, fetal abnormalities, or cancer. It includes chemotherapy agents, genotoxic chemicals, and excreta from patients undergoing cytostatic drug therapy | Improper elimination, such as flushing drugs into water systems, can contaminate natural water bodies, impacting aquatic ecosystems and human water supplies. Incorrect disposal of antibiotics contributes to antimicrobial resistance, making bacterial infections harder to treat | [1,34] |
| Chemical waste | Laboratory solvents, reagents, disinfectants, sterilants, and heavy metals from medical equipment (e.g., mercury in broken thermometers or discarded batteries) | Hazardous chemical waste exhibits toxic, flammable, corrosive, reactive, or oxidizing properties | Exposure to toxic chemicals can result in poisoning, particularly through inhalation, ingestion, or skin absorption. Strong acids and bases can cause severe tissue damage upon contact, leading to chemical burns or respiratory complications | [1,35] |
| Radioactive waste | Medical products contaminated with radionuclides, such as diagnostic radiopharmaceuticals and therapeutic radioactive materials | Waste containing radioactive substances that can emit ionizing radiation, requiring specialized disposal and containment methods | Exposure to radioactive materials poses health hazards, including radiation-induced illnesses, DNA mutations, and increased cancer risk. Proper disposal is essential to mitigate environmental and biological contamination | [36] |
| Large Sources | Medium Sources | Minor Sources | |
|---|---|---|---|
| Hospitals | University | Mortuary facilities | Primary Healthcare Physicians |
| General | |||
| District | |||
| Urgent Care and Trauma Units | Palliative Centers | Dental clinics | |
| Maternal Health and Birthing Centers | Agricultural and Equine Veterinary Clinics | Traditional Needle Therapy Practitioners | |
| Dialysis centers | Animal hospitals | Spinal Adjustment and Musculoskeletal Therapy Experts | |
| Blood Processing and Donation Units | Ambulatory Healthcare Facilities | Convalescent nursing homes | |
| Military medical services | - | Mental Health and Behavioral Therapy Institutions | |
| Medical research centers | Disabled persons’ institutions | ||
| Advanced Biotech Research Labs | Pharmacies | ||
| Animal research and testing | Aesthetic Body Modification Studios | ||
| Senior Assisted Living Centers | Residential Medical Assistance Services | ||
| Hematology Storage and Donation Centers | Ambulance services | ||
| Country | Overall HCW Generation (kg/bed/day) | Infectious Waste Generation (kg/bed/day) | Healthcare Institution | Refs. |
|---|---|---|---|---|
| Pakistan | 6.762 | 3.292 | Hospitals Clinics and dispensaries Basic health units Consulting clinics Nursing homes Maternity | [54,60,61] |
| Tanzania | 0.21 | 0.117 | Health centers (urban) Rural dispensaries Urban dispensaries | [54,62] |
| South Africa | – | 5.13 | Private community health center District hospital Provincial tertiary hospital Public community health center Private day-surgery clinic National central hospital Specialized hospital Regional hospital Public clinic | [54,63] |
| United States | 10.7 (metropolitan general hospitals), 7.7 (laboratories), 0.65 (veterinary, individual metropolitan), 0.93 (rural doctor’s office), 0.043 (psychiatric hospitals), 0.038 (nursing homes) | 2.79 (metropolitan general hospitals), 2.03 (rural general hospitals) | Dentist’s office (individual) Veterinary (rural) Doctor’s office (group practice, urban) Metropolitan general hospitals Doctor’s office (rural) Dentist’s office (rural) Nursing homes Veterinary (individual, metropolitan) Public community health center Private community health center Private day-surgery clinic Rural general hospitals Doctor’s office (individual, urban) Psychiatric and other hospitals Regional hospital Provincial tertiary hospital Specialized hospital District hospital Laboratories Public clinic | [1,54,64] |
| Canada | 8.2 | – | Hospitals | [57,64] |
| Spain | 3.5–4.4 | – | University Hospitals and Regional Hospitals | [6,65,66] |
| France | 0.3–3.6 | – | Public and Private Hospitals | [6,13,65] |
| China | 0.6–4.03 | – | Large Urban Hospitals | [65,67,68] |
| India | 0.8–2.31 | – | Public and Private Hospitals | [13,65,69] |
| Kazakhstan | 5.34–5.4 | – | Major Tertiary Hospitals | [7,65,70] |
| Brazil | 2.94–3.3 | – | Large University Hospitals and Specialized Care Centers | [6,65,71] |
| Ethiopia | 1.1–1.8 | – | District Hospitals and Regional Medical Centers | [16,65,72] |
| Morocco | 0.4–0.7 | – | Public Health Centers and Regional Hospitals | [18,65] |
| Sudan | 0.38–0.9 | – | District Hospitals and Rural Healthcare Centers | [65,73] |
| Chemical | Pathology | Inference Gene Network | Inference Score |
|---|---|---|---|
| Mercury | Diabetes Mellitus, Type 2 | AKT2|BAX|BCL2|BCL2L11|BRAF|C3|CASP3|CAT|CYP1A2|ENPP1|FAS|GCLC|GCLM|GPX1|GSTM1|HMOX1|HNF1A|HPX|IL6|INS1|IRS1|LEPR|MIR151A|MIR423|MIRLET7D|NFKB1|NOS2|OGG1|PAX6|SLC2A4|SOD1|TIMP1|TNF|TNFRSF1A|ZFAND3 | 52.32 |
| Autism Spectrum Disorder | ABCB1|ABCG2|ACHE|AHR|AKR7A3|ALAD|ALDH5A1|ALDH6A1|AQP4|AQP9|BDNF|CA2|CFTR|CHAT|COMT|CP|CRYZ|CYP1A1|CYP1A2|CYP27A1|CYP2U1|CYP7A1|DRD4|GNGT1|GSTA2|GSTM1|GSTP1|MTR|NOS2|NQO1|RELN|SLC3A2|SLC6A4|TJP1|TXNRD1|TXNRD2 | 51.93 | |
| Autistic Disorder | ADM|AQP4|BCL2|BDNF|CADM1|CAT|COMT|CP|DAB1|DRD3|EIF4G1|GPX1|GSTM1|GSTP1|HRAS|HTN1|IFNG|IGF1|IL10|IL13|IL2|IL4|IL6|MAPK3|MTF1|NAV3|NOS2|PAX6|PON1|PTGS2|RELN|SLC6A4|TF | 49.42 | |
| Chemical and Drug Induced Liver Injury | ABCB1|ABCB1B|ABCC1|ABCC2|ACSL1|ACTB|AHR|ALB|ANXA2|APOE|ARG1|ARNT|BAX|C3|CA3|CAT|CCR2|CP|CPS1|CRP|CYP1A1|CYP1A2|CYP1B1|CYP2A6|EIF2AK1|GCLC|GCLM|GPT|GSN|GSR|GSTA1|GSTM1|GSTM3|GSTP1|GSTT1|HAVCR1|HLADQB1|HMOX1|HPX|HSPA5|IFNG|IGF1|IL1B|IL4|IL6|LCN2|LTF|MIR10A|MIR193B|MIR423|MIRLET7B|MIRLET7C|MIRLET7D|MIRLET7G|MIRLET7I|MMP2|MMP9|NFATC4|NFE2L2|NOX4|PARK7|PON1|PTGS2|SERPING1|SHC1|SLC22A8|SOD1|SPP1|TF|TNF|VIM | 46.18 | |
| Obesity | ACHE|ACSL1|AHR|ALDH6A1|APOE|CA3|CASP1|CD40|CRP|CYP1B1|EFNB1|ENPP1|FOS|GAS7|GPX1|GPX3|HMOX1|HSPA5|IL6|IRS1|LEPR|MMP9|NQO1|OGG1|PARP1|PMCH|PTGS2|SLC22A1|SOD1|TF|TNF | 42.77 | |
| Silver | Diabetes Mellitus, Type 2 | ABCC8|ADAMTS9|ATF3|BAX|BCL2|BRAF|CASP3|CAT|CCDC92|CCND2|CYP1A2|EDN1|ENPP1|ETS1|GCG|GCLC|GCLM|GLIS3|GNB3|GPX1|GSTM1|HHEX|HK1|HMOX1|ICAM1|ID1|IL6|IRS2|ITGA1|MIR1226|MIR140|MIR141|MIR142|MIR17HG|MIR181C|MIR192|MIR200A|MIR214|MIR27A|MIR33B|MIR409|MIR483|MIR628|MIR92B|NFKB1|NOS2|NOS3|PAX6|PEPD|PPARG|PROX1|SFRP4|SIRT1|SLC2A4|SNAP25|SOD1|SOD2|ST6GAL1|TCF7L2|TNF | 54.74 |
| Chemical and Drug Induced Liver Injury | AASS|ABCC1|ABCC2|ACTB|ADAM8|AGT|AIFM1|ARG1|BAX|BLVRB|BMAL1|CAT|CCL2|CHRM3|CLU|CP|CTNNB1|CXCL1|CXCL10|CXCL14|CYP1A1|CYP1A2|EIF4EBP2|EPHX1|F3|FGA|FLT1|GADD45A|GCLC|GCLM|GDA|GSR|GSTA4|GSTM1|GSTM2|GSTO1|GSTP1|GSTT1|HADHA|HMOX1|HSPA5|IFNG|IGF1|IL11|IL18|IL1A|IL1B|IL1R2|IL22|IL6|IRAK1|KITL|LDLR|LTF|MALAT1|MAP1LC3B|MDH1|MIR122|MIR1247|MIR1290|MIR132|MIR141|MIR142|MIR150|MIR181C|MIR18A|MIR191|MIR192|MIR19A|MIR200C|MIR22|MIR23A|MIR23B|MIR27B|MIR29B2|MIR33B|MIR362|MIR455|MIR483|MIR484|MIR877|MIRLET7C|MIRLET7G|MMP2|MST1|MTHFR|NFATC4|NFE2L2|NFXL1|NOX4|NR0B2|NR1I2|NR2F2|NREP|NTN1|PARK7|PDK4|PNP|PTGS2|SERPINA6|SESN2|SOD1|SOD2|SOD3|SORD|SPP1|STING1|TBXA2R|TF|THBS1|TNF|TTR|UNC93B1|VEGFA|VIM | 20.88 | |
| Nerve Degeneration | ANGPT1|APLP2|APP|ATRN|BAX|BCL2|BDNF|CASP3|CDH1|CDK5R1|CNR1|CP|CTNNB1|DDIT4|EPOR|FGF2|IFNG|IGF1|MAPK1|MAPK3|MT1|MT2|NOS1|OTX2|PANK1|PARK7|PPARG|PSEN1|SELENOP|SIRT1|SLC18A2|SNCA|SOD1|SOD2|TFEB|TNF|XDH | 11.05 | |
| Poisoning | GCG|GSK3B | 10.4 | |
| Cardiomegaly | AGT|APLN|BAMBI|CCND2|CEBPB|CYP1A1|EDN1|FGF2|FHL2|GSK3B|HMOX1|IGF1|IL18|IL1B|MT2A|NOS3|NPPB|PRKCZ|REN|RRAD|SLC2A4|SOD2|SOX4|TNF|TRPC1 | 9.48 | |
| Chlorine | Myocardial Ischemia | ADRB2|ATP1A1|CCL2|CCL3|CCND1|CPT1B|CRK|CXCL10|EDN1|FABP5|FGF2|GHR|GSTM2|HMGCS2|HMOX1|ICAM1|IGFBP3|IL1A|IL1B|IL6|KCNJ8|MEOX2|NFKBIA|NOS3|NR4A1|PPP2CA|SELE|SELP|TFRC|TNF|TUBA1A | 59.7 |
| Inflammation | AGER|AKT1|APOA1|ATP7B|BDKRB2|CCL11|CCL2|CCL3|CHRNA4|CRHR2|CSF2|CXCL8|EDN1|EGR1|FGF2|HMOX1|ICAM1|IFNG|IL13|IL1A|IL1B|IL6|MMP9|MPO|NOS2|PTGS2|TFRC|TIMP1|TNF|TRPA1 | 34.3 | |
| Pulmonary Fibrosis | CAT|CCL11|CCL2|CCL3|CCL5|CSF2|CSF3|CXCL8|EDN1|FGF2|HMOX1|IL12B|IL13|IL1B|IL6|MECP2|MMP9|TIMP1|TNF | 33.8 | |
| Acute Lung Injury | ACVR1|APOA1|CASP3|CAT|EDN1|FAS|ICAM1|IL1B|IL1RL1|IL6|SFTPD|TNF | 20.24 | |
| Burns, Chemical | ALOX12|FGFR2|IL1A|IL1B|IL1R1|IL6 | 19.03 | |
| Aldrin | Prostatic Neoplasms | AR|CDH1|COL15A1|CTSB|CYP19A1|CYP3A4|CYP7B1|ERBB3|ESR1|ESR2|HMOX1|IVNS1ABP|NGFR|NOS3|SPON2|TET2 | 18.53 |
| Liver Neoplasms, Experimental | CAR3|CDH1|ESR1|NR1I3|TSC22D1 | 5.3 | |
| Diabetes Mellitus | NCF1|NR1I2|NR1I3 | 4.94 | |
| Mirex | Skin Neoplasms | CSF3|ODC1 | 5.41 |
| Chemical and Drug Induced Liver Injury | ADIPOQ | 3.57 | |
| Endrin | Adenocarcinoma | CEBPB|CYP26A1|ESR1|ESR2|NFKB1|NR1I2|PGR|PPARG|RARB|TRP53 | 26.87 |
| Obesity | ADIPOQ|CEBPA|CYCS|ESR1|FASN|NR1I2|NR1I3|NTRK2|PFKFB3|PPARG | 24.94 | |
| Breast Neoplasms | ADAMTS1|ALK|AR|CYP3A4|ESR1|ESR2|FASN|HSP90AA1|KIT|PGR|RARB|TRP53 | 20.66 |
| HCW | Mode of Exposure | Toxic Mechanism | Refs. |
|---|---|---|---|
| Bloodborne Pathogens (HIV, HBV, HCV) | Percutaneous Injuries (sharps, needles, scalpels) contaminated with blood from infected individuals | HIV enters the bloodstream, it binds to CD4 receptors on helper T-cells, fusing with the cell membrane, causing immunodeficiency and making individuals susceptible to opportunistic infections, cancers, and eventually leading to AIDS HBV infects hepatocytes and uses the host’s cellular machinery to replicate HCV targets the liver, leading to chronic infection and inflammation Both HBV and HCV can lead to fibrosis, cirrhosis, and hepatocellular carcinoma | [158,159] |
| Pharmaceutical and Genotoxic Waste (chemotherapy agents, cytotoxic drugs, expired pharmaceuticals) | Inhalation, dermal absorption, ingestion, or accidental puncture | Drugs like antibiotics can cause acute toxicity by disrupting metabolic processes Cytotoxic drugs interfere with DNA replication and cell division by targeting rapidly dividing cells. Alkylating agents add alkyl groups to DNA, leading to crosslinking and breakage, which results in mutagenesis, carcinogenesis, and teratogenesis. Acute toxicity causes liver, kidney, and gastrointestinal impairment, while prolonged exposure increases the risk of cancer, reproductive damage, and organ dysfunction. | [160,161,162,163] |
| Mercury | Inhalation (mercury vapor), ingestion, or dermal absorption | Mercury vapor is absorbed through the lungs, entering the bloodstream. It accumulates in organs, particularly the brain, kidneys, and liver. Mercury is neurotoxic and impairs neuronal function by binding to sulfur-containing groups on enzymes, disrupting neurotransmitter release and leading to cognitive dysfunction, tremors, visual and auditory impairments, and kidney damage | [164,165] |
| Silver | Inhalation of silver dust or fumes, ingestion of contaminated water or food, or dermal absorption from medical applications | Silver accumulates in tissues, particularly the skin, liver, kidneys, and nervous system. Silver ions bind to thiol (-SH) groups in proteins, disrupting enzymatic activity and cellular functions. Silver nanoparticles induce oxidative stress, leading to cellular damage, inflammation, and apoptosis. Argyria causes irreversible skin discoloration, while silver exposure leads to liver and kidney dysfunction, neurotoxicity, cognitive impairment, peripheral neuropathy, and long-term risks of metabolic disorders, immune suppression, and organ toxicity. | [141] |
| Chlorine | Inhalation, skin contact, or accidental ingestion | When chlorine interacts with water or organic matter, it forms chlorine gas, which can be inhaled. Chlorine gas is a potent respiratory irritant, causing bronchospasm, pulmonary edema, and airway inflammation. It also damages the mucous membranes of the eyes, skin, and respiratory tract by reacting with cellular proteins and lipids. It may cause respiratory distress, lung damage, and ocular irritation. | [166] |
| Pesticides (Aldrin, mirex, DDT) | Dermal contact, inhalation, or ingestion | Pesticides disrupt endocrine signaling by mimicking or blocking natural hormones. They can induce oxidative stress, which damages cellular components such as lipids, proteins, and DNA. Aldrin, Mirex, and DDT are known to cause cancers, endocrine disruptions and neurotoxicity, leading to tremors, convulsions | [167,168] |
| Formaldehyde | Inhalation, skin absorption, or ingestion | Causes DNA cross-linking and impairs protein synthesis, leading to cell death. It is a known carcinogen, particularly for nasopharyngeal and lung cancer and may also cause respiratory distress | [169] |
| Radioactive waste | Emission of gamma radiations, beta radiations and low-energy X-rays | The radiations can interact with DNA, causing mutations that may lead to cancer | [170] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cirstea, I.; Radu, A.-F.; Radu, A.; Tit, D.M.; Bungau, G.S. Healthcare Waste Toxicity: From Human Exposure to Toxic Mechanisms and Management Strategies. J. Xenobiot. 2025, 15, 155. https://doi.org/10.3390/jox15050155
Cirstea I, Radu A-F, Radu A, Tit DM, Bungau GS. Healthcare Waste Toxicity: From Human Exposure to Toxic Mechanisms and Management Strategies. Journal of Xenobiotics. 2025; 15(5):155. https://doi.org/10.3390/jox15050155
Chicago/Turabian StyleCirstea, Ilie, Andrei-Flavius Radu, Ada Radu, Delia Mirela Tit, and Gabriela S. Bungau. 2025. "Healthcare Waste Toxicity: From Human Exposure to Toxic Mechanisms and Management Strategies" Journal of Xenobiotics 15, no. 5: 155. https://doi.org/10.3390/jox15050155
APA StyleCirstea, I., Radu, A.-F., Radu, A., Tit, D. M., & Bungau, G. S. (2025). Healthcare Waste Toxicity: From Human Exposure to Toxic Mechanisms and Management Strategies. Journal of Xenobiotics, 15(5), 155. https://doi.org/10.3390/jox15050155








