Regulating AMPA Receptors with Isoxazole-4-Carboxamide Derivatives: An Electrophysiological Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemical Caracterization and Analysis
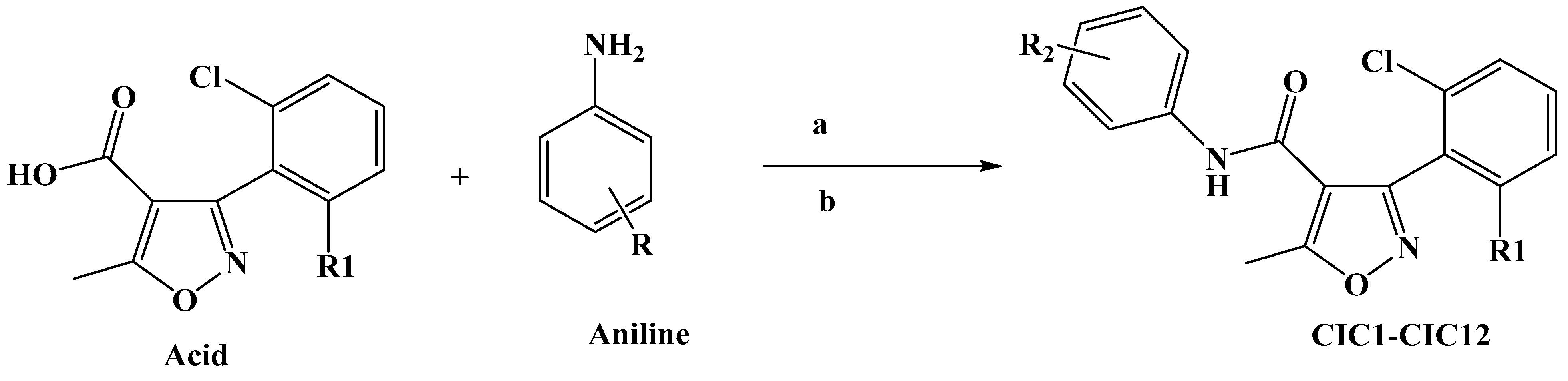
Synthesis of Isoxazole–Carboxamide Derivatives
2.2. Streamlined DNA Preparation and AMPA Receptor Transfection in HEK293 Cells
2.2.1. DNA Preparation
2.2.2. Human Embryonic Kidney Cell Preparation
2.2.3. Transient cDNA Transfection
2.3. Electrophysiology Recordings
2.3.1. Experimental Setup
2.3.2. Statistical Analysis
3. Results
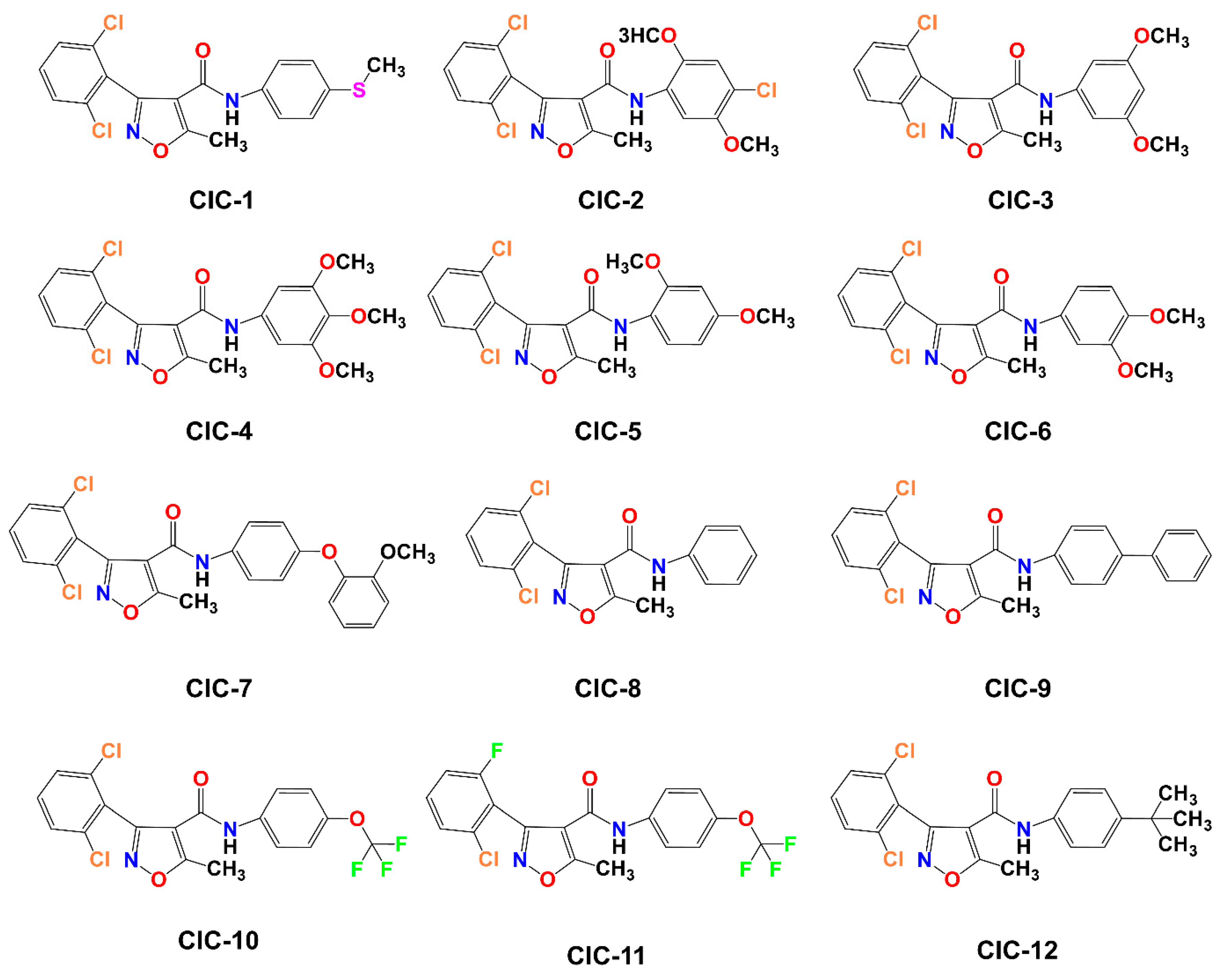
3.1. Chemistry
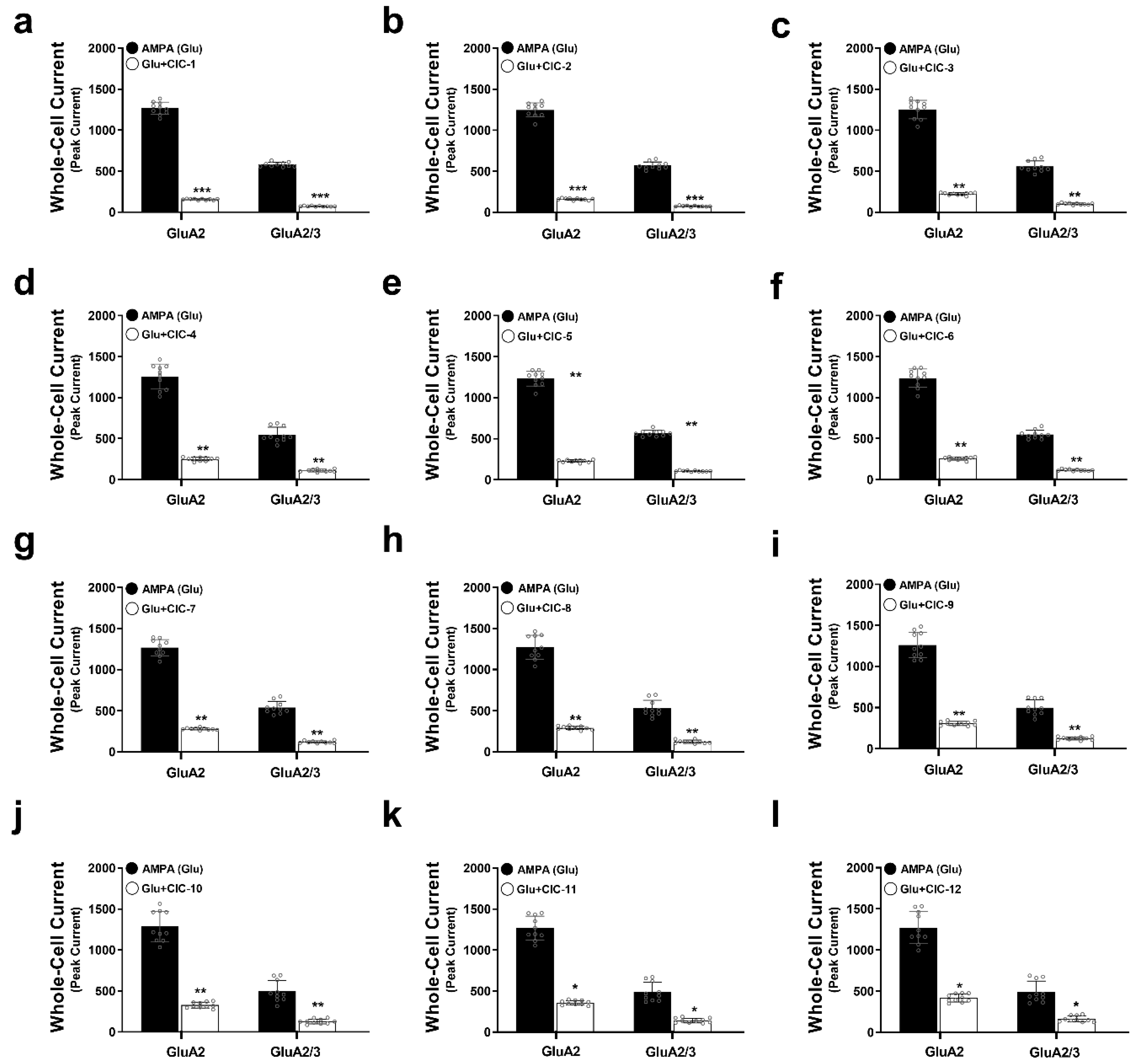
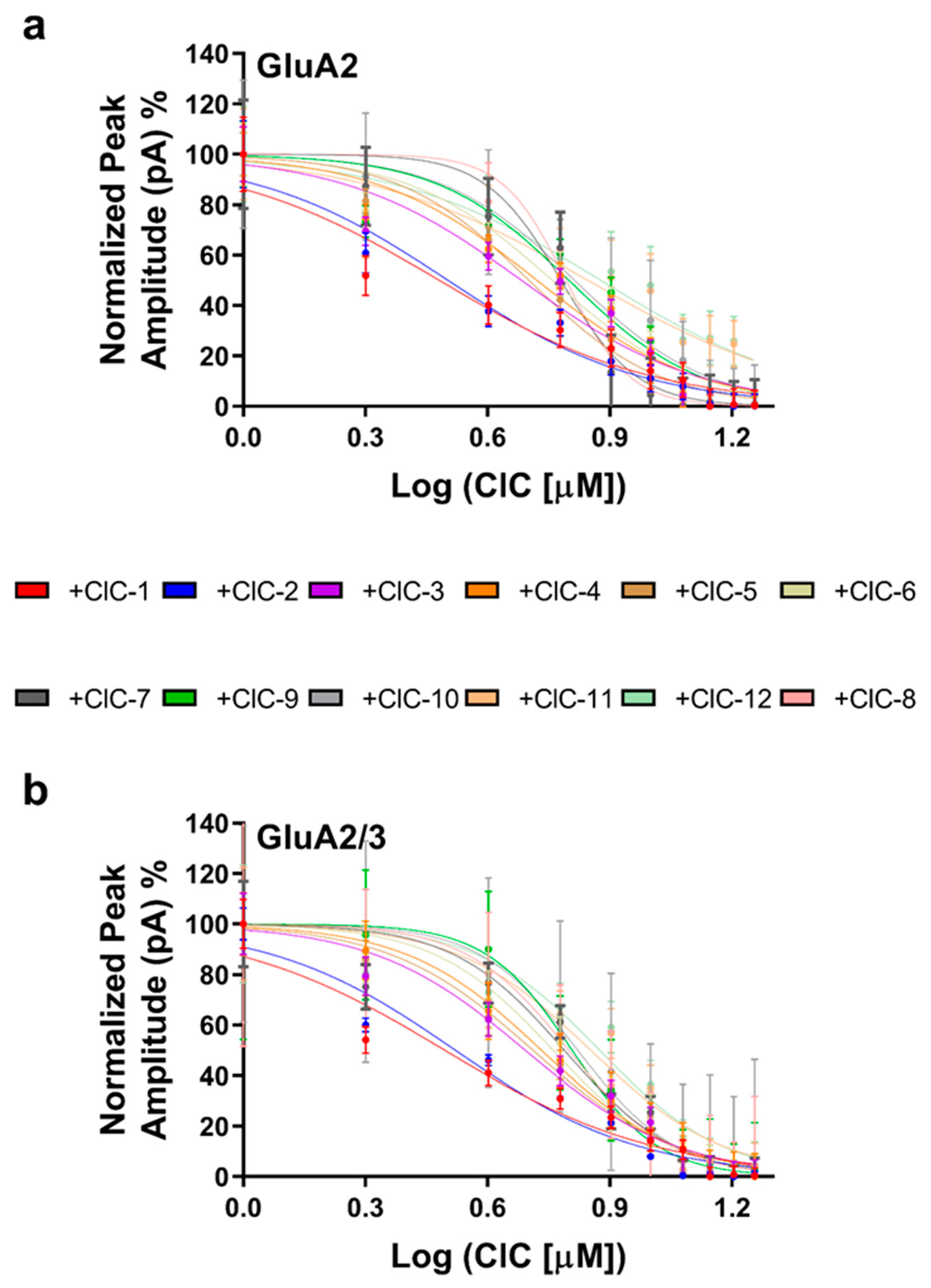
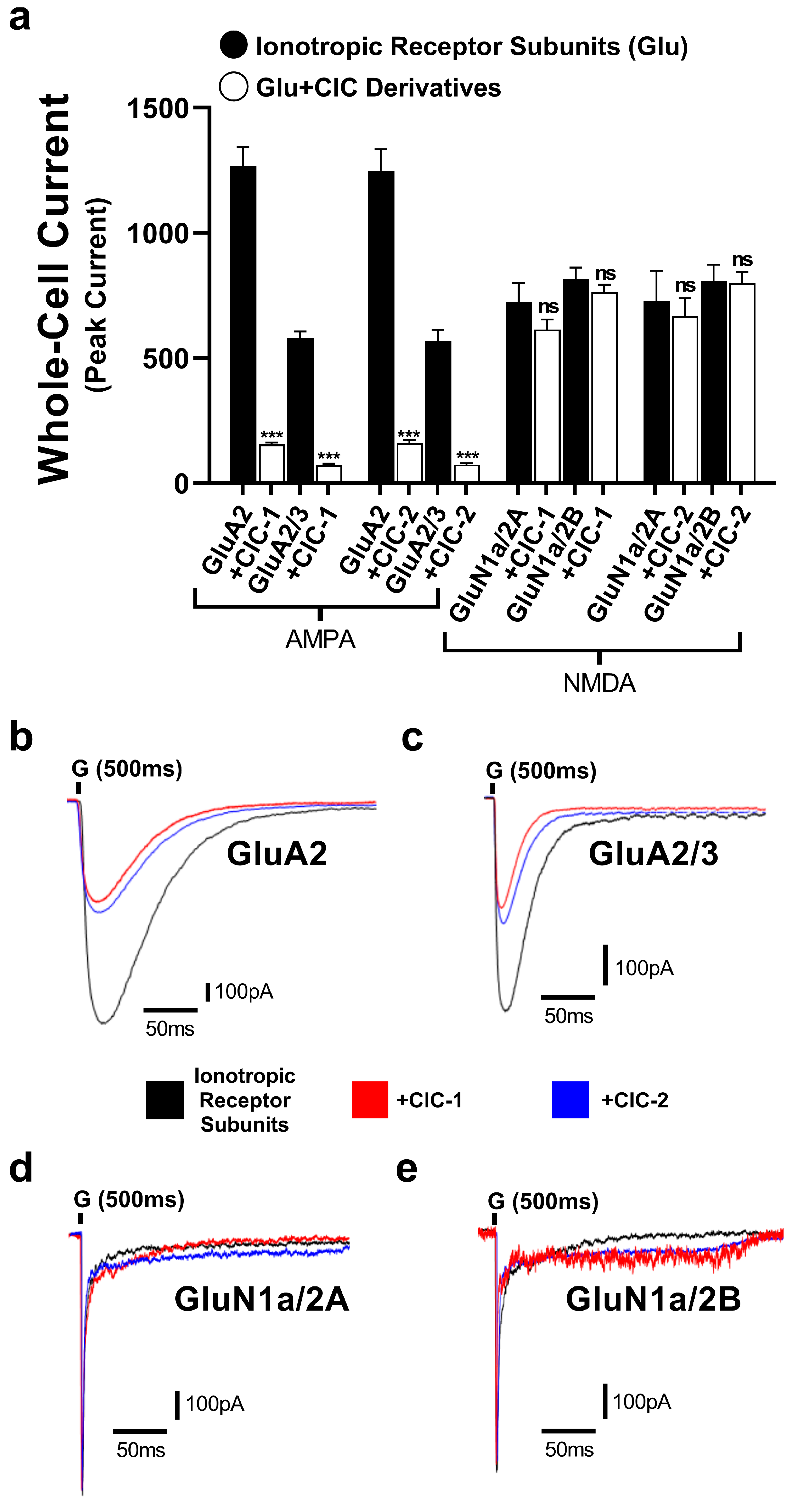
3.2. Inhibitory Effects of Isoxazole-4-Carboxamide Derivatives on the AMPA Receptor
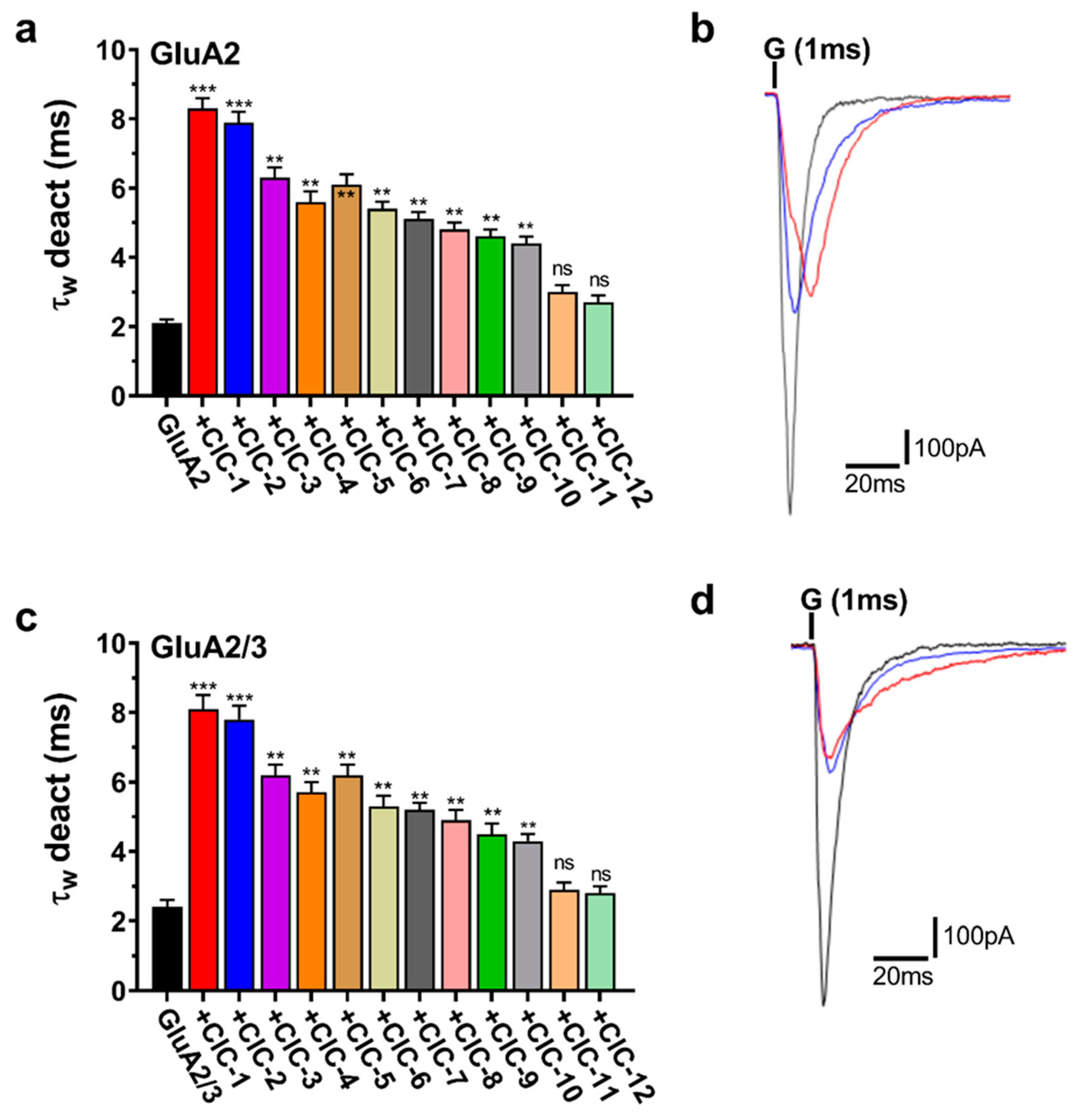
3.3. Effects of Isoxazole-4-Carboxamide Derivatives on AMPA Receptor Deactivation and Desensitization Kinetics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schirbel, A.; Reichert, A.; Roll, S.; Baumgart, D.C.; Büning, C.; Wittig, B.; Wiedenmann, B.; Dignass, A.; Sturm, A. Impact of pain on health-related quality of life in patients with inflammatory bowel disease. World J. Gastroenterol. 2010, 16, 3168–3177. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097. [Google Scholar] [CrossRef]
- Ji, J.; Yuan, M.; Ji, R.-R. Inflammation and pain. In Neuroimmune Interactions in Pain: Mechanisms and Therapeutics; Springer: Berlin/Heidelberg, Germany, 2023; pp. 17–41. [Google Scholar]
- Omoigui, S. The biochemical origin of pain: The origin of all pain is inflammation and the inflammatory response. Part 2 of 3—Inflammatory profile of pain syndromes. Med. Hypotheses 2007, 69, 1169–1178. [Google Scholar] [CrossRef]
- Briggs, A.M.; Cross, M.J.; Hoy, D.G.; Sànchez-Riera, L.; Blyth, F.M.; Woolf, A.D.; March, L. Musculoskeletal Health Conditions Represent a Global Threat to Healthy Aging: A Report for the 2015 World Health Organization World Report on Ageing and Health. Gerontologist 2016, 56 (Suppl. S2), S243–S255. [Google Scholar] [CrossRef]
- Gaskin, D.J.; Richard, P. The Economic Costs of Pain in the United States. J. Pain 2012, 13, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Varrassi, G.; Müller-Schwefe, G.; Pergolizzi, J.; Orónska, A.; Morlion, B.; Mavrocordatos, P.; Margarit, C.; Mangas, C.; Jaksch, W.; Huygen, F.; et al. Pharmacological treatment of chronic pain—The need for CHANGE. Curr. Med. Res. Opin. 2010, 26, 1231–1245. [Google Scholar] [CrossRef] [PubMed]
- El-Tallawy, S.N.; Nalamasu, R.; Salem, G.I.; LeQuang, J.A.K.; Pergolizzi, J.V.; Christo, P.J. Management of Musculoskeletal Pain: An Update with Emphasis on Chronic Musculoskeletal Pain. Pain Ther. 2021, 10, 181–209. [Google Scholar] [CrossRef]
- da Costa, B.R.; Pereira, T.V.; Saadat, P.; Rudnicki, M.; Iskander, S.M.; Bodmer, N.S.; Bobos, P.; Gao, L.; Kiyomoto, H.D.; Montezuma, T.; et al. Effectiveness and safety of non-steroidal anti-inflammatory drugs and opioid treatment for knee and hip osteoarthritis: Network meta-analysis. BMJ 2021, 375, n2321. [Google Scholar] [CrossRef]
- Fokunang, C.; Fokunang, E.T.; Frederick, K.; Ngameni, B.; Ngadjui, B.T. Overview of non-steroidal anti-inflammatory drugs (nsaids) in resource limited countries. Molecules 2018, 4, 5–13. [Google Scholar]
- Bennett, J.M.; Reeves, G.; Billman, G.E.; Sturmberg, J.P. Inflammation-Nature’s Way to Efficiently Respond to All Types of Challenges: Implications for Understanding and Managing “the Epidemic” of Chronic Diseases. Front. Med. 2018, 5, 316. [Google Scholar] [CrossRef]
- Teleanu, R.I.; Niculescu, A.G.; Roza, E.; Vladâcenco, O.; Grumezescu, A.M.; Teleanu, D.M. Neurotransmitters-Key Factors in Neurological and Neurodegenerative Disorders of the Central Nervous System. Int. J. Mol. Sci. 2022, 23, 5954. [Google Scholar] [CrossRef]
- Brechet, A.; Buchert, R.; Schwenk, J.; Boudkkazi, S.; Zolles, G.; Siquier-Pernet, K.; Schaber, I.; Bildl, W.; Saadi, A.; Bole-Feysot, C.; et al. AMPA-receptor specific biogenesis complexes control synaptic transmission and intellectual ability. Nat. Commun. 2017, 8, 15910. [Google Scholar] [CrossRef] [PubMed]
- Kadir, M.F. Visualizing the Dynamics of Ionotropic Glutamate Receptors Using Atomic Force Microscopy. Ph.D. Thesis, Apollo—University of Cambridge Repository, Cambridge, UK, 2017. [Google Scholar]
- Guo, C.; Ma, Y.-Y. Calcium permeable-AMPA receptors and excitotoxicity in neurological disorders. Front. Neural Circuits 2021, 15, 711564. [Google Scholar] [CrossRef]
- Lai, H.C.; Lin, Y.W.; Hsieh, C.L. Acupuncture-Analgesia-Mediated Alleviation of Central Sensitization. Evid.-Based Complement. Altern. Med. 2019, 2019, 6173412. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.B.; Zhang, M.M.; Cheng, L.F.; Shi, J.; Lu, J.S.; Zhuo, M. Long-term upregulation of cortical glutamatergic AMPA receptors in a mouse model of chronic visceral pain. Mol. Brain 2015, 8, 76. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Lei, M.; Wen, Q.; Zhang, D.; Qin, G.; Zhou, J.; Chen, L. Dopamine receptor D2 regulates GLUA1-containing AMPA receptor trafficking and central sensitization through the PI3K signaling pathway in a male rat model of chronic migraine. J. Headache Pain 2022, 23, 98. [Google Scholar] [CrossRef]
- Latrémolière, A. Spinal plasticity of the nociceptive system. In An Introduction to Pain and Its Relation to Nervous System Disorders; John Wiley & Sons: Hoboken, NJ, USA, 2016; pp. 35–87. [Google Scholar] [CrossRef]
- Qneibi, M.; Bdir, S.; Bdair, M.; Aldwaik, S.A.; Sandouka, D.; Heeh, M.; Idais, T.I. AMPA receptor neurotransmission and therapeutic applications: A comprehensive review of their multifaceted modulation. Eur. J. Med. Chem. 2024, 266, 116151. [Google Scholar] [CrossRef]
- Qneibi, M.; Hawash, M.; Gümüş, M.; Çapan, İ.; Sert, Y.; Bdir, S.; Koca, İ.; Bdair, M. Deciphering the Biophysical Properties of Ion Channel Gating Pores by Coumarin–Benzodiazepine Hybrid Derivatives: Selective AMPA Receptor Antagonists. Mol. Neurobiol. 2023, 61, 4565–4576. [Google Scholar] [CrossRef]
- Arai, A.C.; Kessler, M. Pharmacology of ampakine modulators: From AMPA receptors to synapses and behavior. Curr. Drug Targets 2007, 8, 583–602. [Google Scholar] [CrossRef]
- Lianfang, H.E. Involvement of endogenous opioid peptides in acupuncture analgesia. Pain 1987, 31, 99–121. [Google Scholar] [CrossRef]
- Jayakar, S.S.; Dikshit, M. AMPA receptor regulation mechanisms: Future target for safer neuroprotective drugs. Int. J. Neurosci. 2004, 114, 695–734. [Google Scholar] [CrossRef] [PubMed]
- Abu-Hashem, A.A.; Fathy, U.; Gouda, M.A. Synthesis of 1,2,4-triazolopyridazines, isoxazolofuropyridazines, and tetrazolopyridazines as antimicrobial agents. J. Heterocycl. Chem. 2020, 57, 3461–3474. [Google Scholar] [CrossRef]
- Gomha, S.; Khalil, K.; Abdel-Aziz, H. Synthesis and anti-hypertensive α-blocking activity evaluation of thiazole derivatives bearing pyrazole moiety. Heterocycles Int. J. Rev. Commun. Heterocycl. Chem. 2015, 91, 1763–1773. [Google Scholar]
- Abdalla, M.; Gomha, S.; Abd Elaziz, M.; Serag, N. Synthesis and evaluation of some novel thiazoles and 1, 3-thiazines as potent agents against the rabies virus. Turk. J. Chem. 2016, 40, 441–453. [Google Scholar] [CrossRef]
- Abu-Melha, S.; Edrees, M.M.; Riyadh, S.M.; Abdelaziz, M.R.; Elfiky, A.A.; Gomha, S.M. Clean grinding technique: A facile synthesis and in silico antiviral activity of hydrazones, pyrazoles, and pyrazines bearing thiazole moiety against SARS-CoV-2 main protease (Mpro). Molecules 2020, 25, 4565. [Google Scholar] [CrossRef]
- Gomha, S.M.; Farghaly, T.A.; Sayed, A.R.; Abdalla, M.M. Synthesis of Pyrazolyl-Pyrazoles and Pyrazolyl-[1,2,4]-Triazolo[3,4-d][1,5] Benzothiazepines as p53 Activators Using Hydrazonoyl Chlorides. J. Heterocycl. Chem. 2016, 53, 1505–1511. [Google Scholar] [CrossRef]
- Abdelhamid, A.O.; Gomha, S.M.; El-Enany, W.A. Efficient Synthesis and Antimicrobial Evaluation of New Azolopyrimidines-Bearing Pyrazole Moiety. J. Heterocycl. Chem. 2019, 56, 2487–2493. [Google Scholar] [CrossRef]
- Gomha, S.M.; Badrey, M.G.; Abdalla, M.M.; Arafa, R.K. Novel anti-HIV-1 NNRTIs based on a pyrazolo [4,3-d]isoxazole backbone scaffold: Design, synthesis and insights into the molecular basis of action. MedChemComm 2014, 5, 1685–1692. [Google Scholar] [CrossRef]
- Agrawal, N.; Mishra, P. The synthetic and therapeutic expedition of isoxazole and its analogs. Med. Chem. Res. 2018, 27, 1309–1344. [Google Scholar] [CrossRef]
- Yong, J.P.; Lu, C.Z.; Wu, X. Potential anticancer agents. I. Synthesis of isoxazole moiety containing quinazoline derivatives and preliminarily in vitro anticancer activity. Anticancer Agents Med. Chem. 2015, 15, 131–136. [Google Scholar] [CrossRef]
- Kumar, R.N.; Dev, G.J.; Ravikumar, N.; Swaroop, D.K.; Debanjan, B.; Bharath, G.; Narsaiah, B.; Jain, S.N.; Rao, A.G. Synthesis of novel triazole/isoxazole functionalized 7-(trifluoromethyl) pyrido [2,3-d] pyrimidine derivatives as promising anticancer and antibacterial agents. Bioorg. Med. Chem. Lett. 2016, 26, 2927–2930. [Google Scholar] [CrossRef]
- Hawash, M.; Kahraman, D.C.; Ergun, S.G.; Cetin-Atalay, R.; Baytas, S.N. Synthesis of novel indole-isoxazole hybrids and evaluation of their cytotoxic activities on hepatocellular carcinoma cell lines. BMC Chem. 2021, 15, 66. [Google Scholar] [CrossRef]
- Kumar, C.; Veeresh, B.; Ramesha, K.; Raj, C.; Mahadevaiah, K.; Prasad, S.; Naveen, S.; Madaiah, M.; Rangappa, K. Antidiabetic studies of 1-benzhydryl-piperazine sulfonamide and carboxamide derivatives. J. Appl. Chem. 2017, 6, 232–240. [Google Scholar]
- Sysak, A.; Obmińska-Mrukowicz, B. Isoxazole ring as a useful scaffold in a search for new therapeutic agents. Eur. J. Med. Chem. 2017, 137, 292–309. [Google Scholar] [CrossRef] [PubMed]
- Govindappa, V.K.; Prabhashankar, J.; Khatoon, B.B.A.; Ningappa, M.B.; Kariyappa, A.K. Synthesis of 3, 5-diaryl-isoxazole-4-carbonitriles and their efficacy as antimicrobial agents. Pharm. Chem. 2012, 4, 2283–2287. [Google Scholar]
- Abu-Hashem, A.A. Synthesis and antimicrobial activity of new 1,2,4-triazole, 1,3,4-oxadiazole, 1,3,4-thiadiazole, thiopyrane, thiazolidinone, and azepine derivatives. J. Heterocycl. Chem. 2021, 58, 74–92. [Google Scholar] [CrossRef]
- Pedada, S.R.; Yarla, N.S.; Tambade, P.J.; Dhananjaya, B.L.; Bishayee, A.; Arunasree, K.M.; Philip, G.H.; Dharmapuri, G.; Aliev, G.; Putta, S. Synthesis of new secretory phospholipase A2-inhibitory indole containing isoxazole derivatives as anti-inflammatory and anticancer agents. Eur. J. Med. Chem. 2016, 112, 289–297. [Google Scholar] [CrossRef]
- Abu-Hashem, A.A.; El-Shazly, M. Synthesis of new isoxazole-, pyridazine-, pyrimidopyrazines and their anti-inflammatory and analgesic activity. Med. Chem. 2018, 14, 356–371. [Google Scholar] [CrossRef]
- Vasilenko, D.A.; Sadovnikov, K.S.; Sedenkova, K.N.; Karlov, D.S.; Radchenko, E.V.; Grishin, Y.K.; Rybakov, V.B.; Kuznetsova, T.S.; Zamoyski, V.L.; Grigoriev, V.V.J.M. A facile approach to bis (isoxazoles), promising ligands of the AMPA receptor. Molecules 2021, 26, 6411. [Google Scholar] [CrossRef]
- Hawash, M.J.B. Thiazole Derivatives as Modulators of GluA2 AMPA Receptors: Potent Allosteric Effects and Neuroprotective Potential. Biomolecules 2023, 13, 1694. [Google Scholar] [CrossRef]
- Hawash, M.; Abdallah, S.; Abudayyak, M.; Melhem, Y.; Abu Shamat, M.; Aghbar, M.; Capan, I.; Abualhasan, M.; Kumar, A.; Kaminski, M.; et al. Exploration of isoxazole analogs: Synthesis, COX inhibition, anticancer screening, 3D multicellular tumor spheroids, and molecular modeling. Eur. J. Med. Chem. 2024, 271, 116397. [Google Scholar] [CrossRef] [PubMed]
- Qneibi, M.; Hamed, O.; Natsheh, A.-R.; Fares, O.; Jaradat, N.; Emwas, N.; AbuHasan, Q.; Al-Kerm, R.; Al-Kerm, R.J.P.o. Inhibition and assessment of the biophysical gating properties of GluA2 and GluA2/A3 AMPA receptors using curcumin derivatives. PLoS ONE 2019, 14, e0221132. [Google Scholar] [CrossRef]
- Jaradat, N.; Qneibi, M.; Hawash, M.; Hussein, F.; Issa, L.; Ghannam, R.; Ghanem, B.; Reddy, A.J.A.; Bdir, S.J.P.M.; Journal, P. Investigating the Diverse Therapeutic Potential of Hypericum triquetrifolium Aerial Parts in Palestine: Ranging from Examining Metabolic Enzyme Inhibition To Neuroprotective Effects. Palest. Med. Pharm. J. 2023, 9, 2. [Google Scholar] [CrossRef]
- Hawash, M.; Eid, A.M.; Jaradat, N.; Abualhasan, M.; Amer, J.; Naser Zaid, A.; Draghmeh, S.; Daraghmeh, D.; Daraghmeh, H.; Shtayeh, T.; et al. Synthesis and Biological Evaluation of Benzodioxole Derivatives as Potential Anticancer and Antioxidant agents. Heterocycl. Commun. 2020, 26, 157–167. [Google Scholar] [CrossRef]
- Hawash, M.; Jaradat, N.; Eid, A.M.; Abubaker, A.; Mufleh, O.; Al-Hroub, Q.; Sobuh, S. Synthesis of novel isoxazole-carboxamide derivatives as promising agents for melanoma and targeted nano-emulgel conjugate for improved cellular permeability. BMC Chem. 2022, 16, 47. [Google Scholar] [CrossRef] [PubMed]
- Kopach, O.; Voitenko, N. Spinal AMPA receptors: Amenable players in central sensitization for chronic pain therapy? Channels 2021, 15, 284–297. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, J.; Wu, Z.; Lin, Q.; Yue, Y.; Fang, L. Regulation of AMPA receptors in spinal nociception. Mol. Pain 2010, 6, 5. [Google Scholar] [CrossRef]
- Schwenk, J.; Harmel, N.; Brechet, A.; Zolles, G.; Berkefeld, H.; Müller, C.S.; Bildl, W.; Baehrens, D.; Hüber, B.; Kulik, A.; et al. High-resolution proteomics unravel architecture and molecular diversity of native AMPA receptor complexes. Neuron 2012, 74, 621–633. [Google Scholar] [CrossRef] [PubMed]
- van der Spek, S.J.F.; Pandya, N.J.; Koopmans, F.; Paliukhovich, I.; van der Schors, R.C.; Otten, M.; Smit, A.B.; Li, K.W. Expression and Interaction Proteomics of GluA1- and GluA3-Subunit-Containing AMPARs Reveal Distinct Protein Composition. Cells 2022, 11, 3648. [Google Scholar] [CrossRef]
- Aittoniemi, J.; Jensen, M.O.; Pan, A.C.; Shaw, D.E. Desensitization dynamics of the AMPA receptor. Structure 2023, 31, 724–734.e3. [Google Scholar] [CrossRef]
- Twomey, E.C.; Yelshanskaya, M.V.; Grassucci, R.A.; Frank, J.; Sobolevsky, A.I. Structural Bases of Desensitization in AMPA Receptor-Auxiliary Subunit Complexes. Neuron 2017, 94, 569–580.e5. [Google Scholar] [CrossRef]
- Viatchenko-Karpinski, V.; Kong, L.; Weng, H.R. Activation of microglial GPR109A alleviates thermal hyperalgesia in female lupus mice by suppressing IL-18 and glutamatergic synaptic activity. Glia 2022, 70, 634–649. [Google Scholar] [CrossRef] [PubMed]
- Latremoliere, A.; Woolf, C.J. Central sensitization: A generator of pain hypersensitivity by central neural plasticity. J. Pain 2009, 10, 895–926. [Google Scholar] [CrossRef]
- Ji, R.R.; Chamessian, A.; Zhang, Y.Q. Pain regulation by non-neuronal cells and inflammation. Science 2016, 354, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Kwak, D.G.; Lee, D.G. Sequential Activation of AMPA Receptors and Glial Cells in a Pain Model of Lumbar Spine Disc Herniation. Ann. Rehabil. Med. 2020, 44, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhao, Y.; Wang, Y.; Shekhar, M.; Tajkhorshid, E.; Gouaux, E. Activation and Desensitization Mechanism of AMPA Receptor-TARP Complex by Cryo-EM. Cell 2017, 170, 1234–1246.e14. [Google Scholar] [CrossRef]
- Golubeva, E.A.; Lavrov, M.I.; Veremeeva, P.N.; Vyunova, T.V.; Shevchenko, K.V.; Topchiy, M.A.; Asachenko, A.F.; Palyulin, V.A. New Allosteric Modulators of AMPA Receptors: Synthesis and Study of Their Functional Activity by Radioligand-Receptor Binding Analysis. Int. J. Mol. Sci. 2023, 24, 10293. [Google Scholar] [CrossRef]
- Herguedas, B.; Watson, J.F.; Ho, H.; Cais, O.; Garcia-Nafria, J.; Greger, I.H. Architecture of the heteromeric GluA1/2 AMPA receptor in complex with the auxiliary subunit TARP gamma8. Science 2019, 364, eaav9011. [Google Scholar] [CrossRef]
- Sobolevsky, A.I.; Rosconi, M.P.; Gouaux, E.J.N. X-ray structure, symmetry and mechanism of an AMPA-subtype glutamate receptor. Nature 2009, 462, 745–756. [Google Scholar] [CrossRef]
- Gangadharan, V.; Wang, R.; Ulzhofer, B.; Luo, C.; Bardoni, R.; Bali, K.K.; Agarwal, N.; Tegeder, I.; Hildebrandt, U.; Nagy, G.G.; et al. Peripheral calcium-permeable AMPA receptors regulate chronic inflammatory pain in mice. J. Clin. Investig. 2011, 121, 1608–1623. [Google Scholar] [CrossRef]
- Khalili, M.; Eghtesadi, S.; Mirshafiey, A.; Eskandari, G.; Sanoobar, M.; Sahraian, M.A.; Motevalian, A.; Norouzi, A.; Moftakhar, S.; Azimi, A.J.N.n. Effect of lipoic acid consumption on oxidative stress among multiple sclerosis patients: A randomized controlled clinical trial. Nutr. Neurosci. 2014, 17, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Son, S.; Nagahama, K.; Lee, J.; Jung, K.; Kwak, C.; Kim, J.; Noh, Y.W.; Kim, E.; Lee, S.; Kwon, H.-B.; et al. Real-time visualization of structural dynamics of synapses in live cells in vivo. Nat. Methods 2024, 21, 353–360. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qneibi, M.; Hawash, M.; Bdir, S.; Bdair, M.; Idais, T.; Sarhan, I.; Touqan, J. Regulating AMPA Receptors with Isoxazole-4-Carboxamide Derivatives: An Electrophysiological Study. J. Xenobiot. 2025, 15, 40. https://doi.org/10.3390/jox15020040
Qneibi M, Hawash M, Bdir S, Bdair M, Idais T, Sarhan I, Touqan J. Regulating AMPA Receptors with Isoxazole-4-Carboxamide Derivatives: An Electrophysiological Study. Journal of Xenobiotics. 2025; 15(2):40. https://doi.org/10.3390/jox15020040
Chicago/Turabian StyleQneibi, Mohammad, Mohammed Hawash, Sosana Bdir, Mohammad Bdair, Tala Idais, Iyas Sarhan, and Joud Touqan. 2025. "Regulating AMPA Receptors with Isoxazole-4-Carboxamide Derivatives: An Electrophysiological Study" Journal of Xenobiotics 15, no. 2: 40. https://doi.org/10.3390/jox15020040
APA StyleQneibi, M., Hawash, M., Bdir, S., Bdair, M., Idais, T., Sarhan, I., & Touqan, J. (2025). Regulating AMPA Receptors with Isoxazole-4-Carboxamide Derivatives: An Electrophysiological Study. Journal of Xenobiotics, 15(2), 40. https://doi.org/10.3390/jox15020040









