Abstract
Background: Digital health literacy is crucial for navigating social media as a primary health information source. However, its interactive and unregulated nature fosters misinformation, requiring critical evaluation skills. Existing tools assess general internet use, but no validated instrument measures competencies specific to social media. This study aimed to adapt and validate the eHealth Literacy Scale (eHEALS) for this context. Methods: A content validation process was conducted with 33 experts, who evaluated the clarity, coherence, and relevance of the adapted questionnaire using item-level (I-CVI) and scale-level (S-CVI) content validity indices. A pilot study was then carried out with 250 participants to assess the instrument’s reliability and feasibility, measured through Cronbach’s alpha and McDonald’s Omega. Results: The adapted eHEALS demonstrated excellent content validity (S-CVI > 0.90) and high internal consistency (Cronbach’s α = 0.92; McDonald’s Ω = 0.92). The tool effectively captures key competencies for evaluating and applying health information in social media contexts, with exploratory factor analysis confirming a unidimensional structure that explained over 60% of the variance, supporting its robustness for use in population-based studies. Conclusions: This validated instrument provides a reliable method for assessing digital health literacy in social media, supporting the development of educational interventions to enhance critical appraisal skills and mitigate the impact of misinformation.
1. Introduction
In recent decades, patterns of information consumption in society have undergone a significant transformation, particularly in the domain of health-related information [1,2]. Social media has emerged as one of the primary sources of information for the general population, substantially displacing traditional media [1,3]. The increasing reliance on platforms such as Facebook, YouTube, and Instagram for health-related information has facilitated more immediate and dynamic access to healthcare content, enabling users to obtain information on diseases, treatments, and well-being in a manner that is both convenient and economical [4,5,6].
Social media has become a space where people seek health-related information, and this brings both positive aspects and significant challenges. Among the advantages are users’ access not only to a wealth of information, but also to the exchange of experiences and support from others facing similar health concerns [7,8,9]. These interactions serve as an additional form of health education, offering users practical suggestions and examples that help them feel more confident and capable of managing their own care [10]. Furthermore, when health professionals use these platforms to interact directly with users, communication can strengthen health literacy and encourage the adoption of healthier behaviors in everyday life [7].
However, social media also poses substantial limitations as a source of health information. The lack of stringent regulation and the rapid dissemination of content make it challenging to ensure the accuracy and quality of the information available. The ease of access to platforms where individuals without medical training can publish health-related content contributes to the proliferation of misinformation and pseudoscience, a phenomenon that became particularly evident during public health emergencies, such as the COVID-19 pandemic [11,12,13]. This “infodemic” on social media represents a tangible public health risk, generating confusion, anxiety, and even encouraging harmful health behaviors [14]. These challenges highlight the urgent need to develop tools that enable users to critically assess the reliability of the health information they encounter on social media.
Given this landscape, it is essential to assess users’ digital health literacy in the context of social media to promote the safe use of these platforms and improve the quality of the information they receive. Digital health literacy encompasses not only the ability to access and comprehend health information but also the capacity to critically evaluate and appropriately apply it in daily life [15]. Recent studies indicate that high levels of digital health literacy can protect users from misinformation and enhance their ability to manage their own health, particularly when critical thinking is encouraged and trust in reliable sources is strengthened. As a result, digital health literacy is increasingly recognized as a key determinant of health [16].
In this context, several instruments have been developed to measure digital health literacy in the broader internet environment. Among them, the eHealth Literacy Scale (eHEALS) [17]—originally designed to assess health literacy in relation to internet use—remains the most widely applied and has been adapted across diverse populations and digital settings. Other tools have also been introduced, such as the Digital Health Literacy Instrument (DHLI) developed by van der Vaart and Drossaert (2017) [18] and its Brazilian adaptation for adolescents (DHLI-BrA) validated by Barbosa et al. (2024) [19], which extend the assessment to a wider range of skills and cultural contexts. However, none of these questionnaires specifically addresses the use of social media for health-related purposes. A recent scoping review by Faux-Nightingale et al. (2022) [20] confirmed that, despite the growing relevance of social media as a primary source of health information, no validated instrument currently exists to evaluate digital health literacy in this setting. This gap underscores the need to adapt and validate measurement tools that can capture users’ competencies in navigating, appraising, and applying health information within social media environments.
Therefore, this study had two aims: (1) to adapt the eHealth Literacy Scale (eHEALS) to explicitly assess competencies for finding, appraising, and using health information on social media; and (2) to examine its content validity and preliminary reliability and factor structure in a pilot sample from the general population.
2. Material and Methods
- Phase 1. Adaptation and Translation Process
Prior to the validation stages, the original English version of the eHEALS was adapted to explicitly assess health information in the context of social media. Each item was reformulated to replace references to “the Internet” with “social media platforms” (e.g., Facebook, Instagram, YouTube), while preserving the original construct. The questionnaire underwent a process of translation and cross-cultural adaptation following international recommendations [21]. First, two independent bilingual translators, native Spanish speakers with advanced English skills, performed a direct translation from the original version. Subsequently, a third translator, a native English speaker with no prior knowledge of the original version, performed the reverse translation.
The versions obtained were reviewed by the research team, made up of professionals in nursing, health communication, and psychometric methodology, selected based on their academic and practical experience in digital health literacy. The panel evaluated the semantic, idiomatic, and conceptual equivalence of each item, proposing adjustments when necessary until consensus was reached.
Finally, a cognitive adaptation was carried out through cognitive interviews with ten participants from the target population, with the aim of verifying the comprehensibility, relevance, and cultural appropriateness of the items. The observations collected were used to refine the final version prior to the content validation phase.
- Phase 2. Validation of the instrument’s content
Content validity indicates whether the items of an instrument accurately represent the concept being measured. It is usually evaluated by a panel of experts who assess each item for clarity, coherence, and relevance.
Specifically, clarity refers to the comprehensibility of the items in terms of syntax and semantics; coherence assesses the logical alignment of the item with the overall scale; and relevance determines whether the inclusion of the item is necessary to ensure an adequate representation of the construct.
- Selection of the expert panel
The questionnaire validation was conducted through the selection of an expert panel using purposive sampling, following predefined criteria. Experts (n = 16) were selected through purposive sampling, following the methodological recommendations of Polit and Beck (2004) [22]. Eligibility criteria included: (a) advanced academic or professional training in nursing, psychology, communication, or health sciences; (b) research or professional experience in health literacy, digital communication, or education; and (c) at least three years of professional experience. Candidates were identified through academic networks and professional associations and invited via institutional mailing lists. Only those who provided informed consent participated. In addition, a complementary panel of lay participants (n = 17) with high digital literacy was recruited to evaluate comprehension and cultural relevance. Lay participants were selected based on high digital literacy, assessed through a short screening questionnaire adapted from the Digital Health Literacy Instrument (DHLI). The screening evaluated frequency of social media use, diversity of platforms used, and self-reported ability to search, critically evaluate, and share health-related information online. Only individuals scoring above the 75th percentile were included in this group. Their participation contributed to assessing the clarity, comprehensibility, and cultural relevance of the adapted questionnaire from the perspective of the target audience.
- Validation session
After the research team presented the study objectives, the expert panel assessed the clarity, coherence, and relevance of each questionnaire item using a survey administered via Google Forms. To ensure ethical compliance, all participants signed an informed consent form prior to their involvement.
During the validation session, each item of the questionnaire was evaluated independently for clarity, coherence, and relevance. These three dimensions were assessed separately using a 4-point Likert scale (1 = not at all clear/coherent/relevant, 4 = very clear/coherent/relevant). This procedure allowed the computation of item-level (I-CVI) and scale-level (S-CVI) Content Validity Indices for each dimension. In addition, an open-ended section was included to collect comments and suggestions for improving the items.
- Data analysis
The statistical analysis involved calculating both the Item-Level Content Validity Index (I-CVI) and the Scale-Level Content Validity Index (S-CVI). The I-CVI reflected the proportion of experts who rated an item as valid, with values above 0.78 indicating excellent content validity [22].
To assess the overall validity of the instrument, the S-CVI was computed as the mean of all I-CVI values. An S-CVI greater than 0.90 was interpreted as evidence of excellent content validity for the entire questionnaire [22].
- Preliminary Version of the Questionnaire
Following an in-depth analysis and the incorporation of recommendations obtained during the peer-review phase, the preliminary version of the questionnaire was developed. This version included both original items and revised elements, ensuring greater clarity, coherence, and representativeness of the construct. The preliminary questionnaire consisted of only eight items.
- Phase 3. Pilot study
Following the integration of expert feedback, a pilot study (n = 250) was carried out between February and March 2024 using a non-probabilistic convenience sample.
Data were collected online through Google Forms, and the questionnaire was completed individually and anonymously, without the presence of a researcher. Recruitment was carried out via institutional mailing lists and social media platforms. Participation was voluntary and without incentives.
The objective of the pilot study was to validate the revised version of the instrument and assess key aspects such as question comprehension, language clarity, completion time, and any other relevant observations for further improvement, to assess the reliability of the instrument and its factor structure.
- Data analysis
The data obtained from the pilot study were used to evaluate the instrument’s reliability through Cronbach’s alpha and McDonald’s Omega [23], which assess internal consistency. A preliminary analysis was also conducted to estimate the required sample size for future studies at the population level. This phase helped identify areas for improvement and reinforced the methodological soundness of the instrument for broader application.
To explore the underlying factor structure of the digital health literacy in social media questionnaire, an exploratory factor analysis (EFA) was performed using Principal Components as the extraction method. Prior to conducting the EFA, the adequacy of the data was assessed through Bartlett’s test of sphericity and the Kaiser–Meyer–Olkin (KMO) measure. The number of factors retained was determined using the Kaiser criterion (eigenvalues greater than 1) and by examining the inflection point of the scree plot [24]. All data analyses were performed with SPSS v29.
3. Results
- Phase 1. Adaptation and translation
The forward–backward translation process confirmed the semantic equivalence between the Spanish version and the original English eHEALS. Minor wording adjustments were made during cognitive pre-testing (n = 10) to improve readability and contextual clarity, particularly replacing general references to “the Internet” with “social media platforms.” All items were considered comprehensible and relevant by participants, and no item was excluded at this stage. The final adapted Spanish version was then submitted to expert validation.
- Phase 2. Validation of the instrument’s content
The validation sample comprised two complementary groups. The first group consisted of 16 experts with professional profiles in health, teaching, and communication, including university professors, nurses, midwives, psychologists, and health content creators. Of these participants, 56.3% were women and 43.7% men, with a mean age of 31.4 years. Of the 16 experts, nine (56.3%) held doctoral degrees and seven (43.7%) were university professors. Their fields of expertise were nursing (n = 5), psychology (n = 3), communication (n = 2), and health sciences education (n = 6). This profile ensured that the panel provided both academic and professional expertise relevant to digital health literacy and instrument validation.
The second group included 17 lay participants from the general population with high digital literacy and frequent social media use. In this group, 52.9% were female and 47.1% male, with a mean age of 26 years. Regarding educational level, 70.6% had university studies, 17.6% vocational training, and 11.8% secondary education.
The results of the validation process for the adaptation of the eHEALS questionnaire for use in social media are presented in Table 1, which displays the item-level content validity index (I-CVI) for clarity, coherence, and relevance. Across all three evaluated aspects (clarity, coherence, and relevance), all questionnaire items achieved I-CVI values exceeding 0.78, indicating excellent content validity according to established criteria. The calculated scale-level content validity index (S-CVI) for each dimension was 0.93 for clarity, 0.95 for coherence, and 0.98 for relevance, reinforcing the overall quality of the instrument in terms of item representativeness and appropriateness. These findings demonstrate that the questionnaire meets high standards of excellence in its design and content.

Table 1.
Content Validity Indexes (I-CVI and S-CVI)–Specialists.
The items that received the highest scores in terms of relevance were items 1 and 4–8. Items 3–7 achieved the highest scores for clarity, while items 4–7 obtained the maximum score for coherence. However, it is important to note that none of these items were excluded, as their I-CVI values were deemed acceptable.
In the panel composed from the general population, the results were even more favourable (Table 2), with both the I-CVI and S-CVI reaching the maximum value of 1 across all dimensions—clarity, coherence, and relevance.

Table 2.
Content Validity Indexes (I-CVI and S-CVI) in the General Population.
- Phase 3. Pilot study
The questionnaire was administered to a pilot sample of 250 individuals from the general population (Table 3) to assess the clarity, applicability, and feasibility of the instrument, as well as to identify any potential difficulties in its administration. This phase aimed to ensure that respondents fully understood the questions and to determine the time required to complete the questionnaire. Based on the results obtained from the pilot sample, necessary modifications were made to the final version of the questionnaire, including adjustments to the wording and the order of certain questions.

Table 3.
Sociodemographic characteristics of the pilot sample.
Both the Cronbach’s alpha and McDonald’s omega showed high internal consistency (α = 0.92; Ω = 0.92). A preliminary estimate indicated that 69.6% of participants used social media for health information, which was used to calculate the required sample size for a larger population-based study (n = 913).
- Exploratory factor analysis (EFA)
The KMO value was 0.884, which is considered meritorious [24] and indicates a high proportion of common variance among the items. The χ2 value of Bartlett’s sphericity test was statistically significant (χ228 = 1475.78, p < 0.001), which indicated that the results were suitable for exploratory factor analysis. The scree plot revealed the presence of a single factor (Figure 1) with an eigenvalue of 5.11 which accounted for 63.87% of the total variance, which is over the threshold of 60% to consider the model adequate [25]. The communalities of the items were all above 0.50 (0.514–0.772) suggesting that the items explain a substantial proportion of their variance through the common factor. All item loadings were >0.70 (Table 4), so the 8 items were retained.
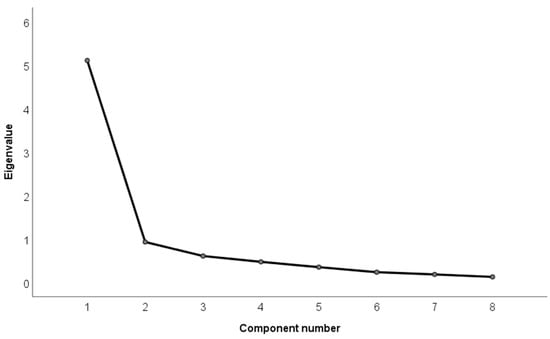
Figure 1.
Scree plot of the factors of the eHEALS questionnaire for use in social media extracted by principal component analysis.

Table 4.
EFA Factor Loadings of Digital Health Literacy in Social Media Items.
4. Discussion
Access to health information has undergone significant transformations in recent decades, not only altering the sources used by the population but also reshaping how this information is interpreted and applied in decision-making [26]. The continuous increase in social media use has contributed to the emergence of a new landscape, enabling a constant flow of digital content—often without users actively seeking it [27]. This shift presents unique challenges regarding digital health literacy, a field that has been extensively studied in general internet contexts but remains insufficiently explored within the specific domain of social media. The present study addresses this gap by providing an adapted and validated tool to assess critical competencies in a dynamic and frequently misinformation-prone environment.
Norman and Skinner [17], in their initial validation of the eHEALS, demonstrated that this instrument is a useful tool for measuring how users perceive their ability to search for, comprehend, and apply online health information. However, its design does not account for interaction, virality, or the social dynamics inherent to social media—factors that justified the need for this study.
Our results indicate that the adaptation and validation of the eHEALS maintain its optimal internal consistency (Cronbach’s α = 0.92: McDonalds Ω = 0.92), aligning with values reported in the instrument’s original validation [17]. At the same time, as highlighted by previous research, digital health literacy is a key determinant in improving health behaviors and reducing vulnerability to misinformation [28]. These findings are comparable to studies that have validated similar instruments, such as the Digital Health Literacy Instrument (DHLI-BrA) used by Barbosa [19] to measure digital health competencies among adolescents in internet-based settings. However, the adapted eHEALS has the distinct advantage of focusing specifically on social media, addressing a gap identified by other authors [29], who emphasized the need to develop specialized tools for interactive environments, recognizing the increasing influence of social media and other digital platforms in shaping how young individuals access and utilize health information.
The content validity analysis, supported by the I-CVI and S-CVI indices, confirms that experts deemed the questionnaire items to be relevant, clear, and coherent in assessing digital health literacy within social media contexts. This suggests that the semantic adaptation has not compromised the instrument’s ability to accurately measure this construct.
Recent studies have identified that digital health literacy in social media is not solely dependent on information-seeking abilities but also on the capacity to interpret, filter, and share content within an interactive ecosystem—where social validation and message virality can distort perceptions of informational accuracy [30]. In this regard, adapting the eHEALS questionnaire to the social media context represents a significant methodological advancement, as it enables a more precise evaluation of users’ ability to distinguish reliable sources in highly dynamic and misinformation-prone environments.
The adaptation and validation of the eHEALS, therefore, represent an important step in identifying factors that may predispose individuals to uncritical consumption of health-related information—an insight that could be pivotal for designing evidence-based educational interventions. Additionally, this validation provides key data on the digital competencies required to assess the quality of health information shared on social media and its impact on health decision-making. Finally, the questionnaire’s validation reinforces the idea that direct equivalencies cannot be assumed between digital health literacy in general internet use and in social media, as interaction dynamics, information overload, and content validation mechanisms function differently in each environment [31,32,33].
Finally, the exploratory factor analysis showed that the adapted scale maintains a unidimensional structure. This factorial solution is aligned with the theoretical structure of the original eHEALS scale, which also identified a single factor, thus favoring its applicability and comparability in different contexts. This result also indicates that the items assessed cluster coherently around a single construct: digital health literacy in the specific context of social networks. The strong correlation between the items suggests that they all contribute significantly to measuring this competency, which is particularly relevant to meet the study’s objective of having a useful and specific tool to assess such skills in today’s digital environment. The high internal consistency among the items, reflected in their high factor loadings, indicates that they all contribute significantly to the measurement of the same concept.
This study contributes to an emerging field of research by offering a validated tool that enables a more precise evaluation of digital health literacy in social media, facilitating the development of strategies aimed at enhancing the population’s critical capacity to counteract health-related misinformation.
This study has several limitations. The use of expert judgment introduces subjectivity, and the predominance of young and highly educated participants may limit the generalizability of the findings. Additionally, as the questionnaire was developed within a single cultural context, cross-cultural adaptations will be necessary for international use. Furthermore, since the instrument is based on self-report and administered through a convenience sample, participants’ responses may reflect subjective perceptions rather than actual digital health literacy skills. These aspects should be considered when interpreting the findings, and future studies should aim to include more representative samples and combine self-reported measures with objective performance-based assessments.
Finally, although the exploratory factor analysis supported a unidimensional structure consistent with the original version of the instrument, this unidimensionality could limit the questionnaire’s ability to capture more nuanced aspects of digital health literacy in social networks, such as critical thinking, interactive skills or trust in information sources. Future research could explore the presence of subdimensions through confirmatory factor analysis or other measurement models.
Although our design included an exploratory factor analysis (EFA), we acknowledge that a confirmatory factor analysis (CFA) on an independent sample would provide stronger evidence for the structure of the instrument. We have noted this as a limitation and suggested that future studies should incorporate CFA or, at minimum, parallel analysis to enhance robustness.
Finally, beyond these psychometric considerations, it would be important for future studies to explore the role of artificial intelligence (AI) in shaping the health information available on social media. Future research should consider how to integrate AI into health literacy frameworks, given its rapid evolution and influence on social platforms.
5. Conclusions
Our results suggest that the adaptation and validation of the eHEALS questionnaire for the context of social media constitutes a reliable and valid instrument for measuring digital health literacy, facilitating the identification of training needs and the design of educational interventions aimed at the safe and effective use of these platforms.
The implications of this study on digital health literacy are numerous and significant, particularly in the design of educational interventions. The findings can guide the development of educational programs and resources aimed at enhancing digital health literacy skills, especially among populations with low educational attainment and limited access to technology. The tool developed in this study provides a foundation for identifying specific digital competencies that should be reinforced in educational campaigns.
Moreover, addressing disparities in digital health literacy is crucial to ensuring equitable and effective access to digital health tools. Enhancing digital literacy can have a positive impact on health outcomes and quality of life by facilitating the comprehension and use of digital health resources, improving communication with healthcare professionals, and promoting healthy behaviors.
Author Contributions
Conceptualization, R.Q.A. and L.C.E.; methodology, J.L.P.-F.; validation, R.Q.A., L.C.E., I.L. and J.L.P.-F.; formal analysis, J.L.P.-F. and A.B.; investigation, I.L. and E.C.R.; writing—original draft preparation, R.Q.A. and L.C.E.; writing—review and editing, A.B., R.Q.A. and L.C.E.; supervision, A.B. and J.L.P.-F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki (2013) and the Spanish Organic Law 3/2018 of 5 December on the Protection of Personal Data and Guarantee of Digital Rights. The present study did not involve clinical interventions, drug trials, or the collection of sensitive personal data, and all data were anonymized prior to analysis. The study involved voluntary participation by nursing professionals through anonymized questionnaires, without patient involvement, physical procedures, or any psychological or legal risk. Therefore, in accordance with Royal Decree 1090/2015 (which regulates clinical trials and Research Ethics Committees for Medicinal Products), Law 14/2007 on Biomedical Research, and Regulation (EU) 2016/679 (GDPR), formal review by an ethics committee was not required.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Public Involvement Statement
There was no public involvement in any aspect of this research.
Guidelines and Standards Statement
This manuscript was drafted against the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement for observational research [34].
Use of Artificial Intelligence
AI or AI-assisted tools were not used in drafting any aspect of this manuscript, except for minor improvements in translation and language clarity.
Acknowledgments
We deeply appreciate all participants and experts for their invaluable contribution to this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Deng, Z.; Liu, S. Understanding consumer health information-seeking behavior from the perspective of the risk perception attitude framework and social support in mobile social media websites. Int. J. Med. Inform. 2017, 105, 98–109. [Google Scholar]
- Lipschultz, J.H. Social Media Communication: Concepts, Practices, Data, Law and Ethics, 3rd ed.; Routledge: London, UK, 2020; Volume 9, pp. 41–51. ISBN 9780429202834. [Google Scholar] [CrossRef]
- González Barberá, M.; Menárguez Puche, J.F.; Delsors Mérida-Nicolich, E.; Tello Royloa, C.; Sánchez Sánchez, J.A.; Alcántara Muñoz, P.Á.; Soler Torroja, M. Información sanitaria en la red. Necesidades, expectativas y valoración de la calidad desde la perspectiva de los pacientes. Investigación cualitativa con grupos focales. Rev. Clínica Med. Fam. 2021, 14, 131–139. Available online: https://www.revclinmedfam.com/article/informacion-sanitaria-en-la-red-necesidades-expectativas-y-valoracion-de-la-calidad-desde-la-perspectiva-de-los-pacientes-investigacion-cualitativa-con-grupos-focales (accessed on 8 July 2023). [CrossRef]
- Sumayyia, M.D.; Al-Madaney, M.M.; Almousawi, F.H. Health information on social media. Perceptions, attitudes, and practices of patients and their companions. Saudi Med. J. 2019, 40, 1294–1298. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, X.; Lin, X.; Hajli, M. Seeking and sharing health information on social media: A net valence model and cross-cultural comparison. Technol. Forecast. Soc. Chang. 2018, 126, 28–40. [Google Scholar] [CrossRef]
- Ren, J.; Dong, H.; Popovic, A.; Sabnis, G.; Nickerson, J. Digital platforms in the news industry: How social media platforms impact traditional media news viewership. Eur. J. Inf. Syst. 2024, 33, 1–18. [Google Scholar] [CrossRef]
- Wu, T.; He, Z.; Zhang, D. Impact of Communicating With Doctors Via Social Media on Consumers’ E-Health Literacy and Healthy Behaviors in China. Inq. J. Health Care Organ. Provis. Financ. 2020, 57, 0046958020971188. [Google Scholar] [CrossRef]
- Kanchan, S.; Gaidhane, A. Social Media Role and Its Impact on Public Health: A Narrative Review. Cureus 2023, 15, e33737. Available online: https://www.cureus.com/articles/115786-social-media-role-and-its-impact-on-public-health-a-narrative-review (accessed on 8 July 2023). [CrossRef] [PubMed]
- Afful-Dadzie, E.; Afful-Dadzie, A.; Egala, S.B. Social media in health communication: A literature review of information quality. Health Inf. Manag. J. 2023, 52, 3–17. [Google Scholar] [CrossRef]
- Niu, Z.; Willoughby, J.; Zhou, R. Associations of Health Literacy, Social Media Use, and Self-Efficacy With Health Information–Seeking Intentions Among Social Media Users in China: Cross-sectional Survey. J. Med. Internet Res. 2021, 23, e19134. Available online: http://www.jmir.org/2021/2/e19134/ (accessed on 8 July 2023). [CrossRef]
- Kington, R.S.; Arnesen, S.; Chou, W.Y.S.; Curry, S.J.; Lazer, D.; Villarruel, A.M. Identifying Credible Sources of Health Information in Social Media: Principles and Attributes. NAM Perspect. 2021, 2021, 10–31478. Available online: https://nam.edu/identifying-credible-sources-of-health-information-in-social-media-principles-and-attributes (accessed on 8 July 2023). [CrossRef]
- Li, Y.J.; Marga, J.J.; Cheung, C.M.K.; Shen, X.L.; Lee, M. Health Misinformation on Social Media: A Systematic Literature Review and Future Research Directions. AIS Trans. Hum.-Comput. Interact. 2022, 14, 116–149. Available online: https://aisel.aisnet.org/thci/vol14/iss2/2 (accessed on 8 July 2023). [CrossRef]
- Sylvia Chou, W.Y.; Gaysynsky, A.; Cappella, J.N. Where We Go From Here: Health Misinformation on Social Media. Am. J. Public Health 2020, 110, S273–S275. Available online: https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2020.305905 (accessed on 8 July 2023). [CrossRef] [PubMed]
- Organización Mundial de la Salud. Entender la Infodemia y la Desinformación en la Lucha Contra la COVID-19 [Internet]. 2020. Available online: https://iris.paho.org/bitstream/handle/10665.2/52053/Factsheet-Infodemic_spa.pdf (accessed on 8 July 2023).
- Sykes, S.; Wills, J.; Rowlands, G.; Popple, K. Understanding critical health literacy: A concept analysis. BMC Public Health 2013, 13, 150. Available online: http://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-150 (accessed on 8 July 2023). [CrossRef]
- Van Kessel, R.; Wong, B.L.H.; Clemens, T.; Brand, H. Digital health literacy as a super determinant of health: More than simply the sum of its parts. Internet Interv. 2022, 27, 100500. [Google Scholar] [CrossRef]
- Norman, C.D.; Skinner, H.A. eHEALS: The eHealth Literacy Scale. J. Med. Internet Res. 2006, 8, e27. Available online: http://www.jmir.org/2006/4/e27/ (accessed on 8 July 2023). [CrossRef] [PubMed]
- Van Der Vaart, R.; Drossaert, C. Development of the digital health literacy instrument: Measuring a broad spectrum of health 1.0 and health 2.0 skills. J. Med. Internet Res. 2017, 19, e27. Available online: https://www.jmir.org/2017/1/e27/ (accessed on 8 July 2023). [CrossRef]
- Barbosa, M.C.F.; Baldiotti, A.L.P.; Firmino, R.T.; Paiva, S.M.; Granville-Garcia, A.F.; Ferreira, F.D.M. Evaluation of the Psychometric Properties of the Digital Health Literacy Instrument (DHLI-BrA) for Use in Brazilian Adolescents. Int. J. Environ. Res. Public Health 2024, 21, 1458. Available online: https://www.mdpi.com/1660-4601/21/11/1458 (accessed on 8 July 2024). [CrossRef]
- Faux-Nightingale, A.; Philp, F.; Chadwick, D.; Singh, B.; Pandyan, A. Available tools to evaluate digital health literacy and engagement with eHealth resources: A scoping review. Heliyon 2022, 8, e10380. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. Nursing Research: Principles and Methods, 7th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2004; ISBN 0781737338. [Google Scholar]
- Hayes, A.F.; Coutts, J.J. Use omega rather than Cronbach’s alpha for estimating reliability. But…. Commun. Methods Meas. 2020, 14, 1–24. [Google Scholar] [CrossRef]
- Kaiser, H.F. An Index of Factorial Simplicity. Psychometrics 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson: New York, NY, USA, 2010. [Google Scholar]
- Carton Erlandsson, L.; Martín Duce, A.; Gragera Martínez R de los, R.; Muriel García, A.; Mirón González, R.; Gigante Pérez, C. Uso de redes sociales como fuente de información sobre salud y alfabetización digital en salud en población general española. Rev. Esp. Salud Pública 2024, 98, e202405034. Available online: https://ojs.sanidad.gob.es/index.php/resp/article/view/213/863 (accessed on 8 July 2023).
- Erlandsson, L.C.; Guijo, M.S.; Quintana-Alonso, R. Decoding patterns: The crucial role of social media in health information consumption and user dynamics among the general population. J. Public Health 2024. [Google Scholar] [CrossRef]
- Belmonte, I.A.; Collado, R.S.; Yuguero, O.; Oliva, J.A.; Martínez-Millana, A.; Pérez, C.S. La alfabetización digital como elemento clave en la transformación digital de las organizaciones en salud. Atención Primaria 2024, 56, 102880. [Google Scholar] [CrossRef] [PubMed]
- Freeman, J.L.; Caldwell, P.H.Y.; Scott, K.M. How Adolescents Trust Health Information on Social Media: A Systematic Review. Acad. Pediatr. 2023, 23, 703–719. Available online: https://linkinghub.elsevier.com/retrieve/pii/S1876285922006374 (accessed on 8 September 2024). [CrossRef]
- Jiménez-Marín, G.; Bellido-Pérez, E.; Trujillo Sánchez, M. Publicidad en Instagram y riesgos para la salud pública: El influencer como prescriptor de medicamentos, a propósito de un caso. Rev. Española Comun. Salud 2021, 12, 43. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=7997527 (accessed on 8 July 2023). [CrossRef]
- Díaz Catalán, C.; Cabrera Álvarez, P. Desinformación Científica en España. Informe de Resultados; Fundación Española para la Ciencia y la Tecnología (FECYT): Madrid, Spain, 2022; pp. 1–228. [Google Scholar] [CrossRef]
- Roberts, M.; Callahan, L.; O’Leary, C. Social Media: A Path to Health Literacy; IOS Press: Amsterdam, The Netherlands, 2017; pp. 464–475. [Google Scholar] [CrossRef]
- Leaver, T.; Highfield, T.; Abidin, C. Instagram: Visual Social Media Cultures (Digital Media and Society); Polity Press: Cambridge, UK, 2019; ISBN 1932-8036/2022BKR0009. Available online: https://ijoc.org/index.php/ijoc/article/viewFile/19389/3705 (accessed on 8 September 2024).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).