Barriers and Facilitators to the Use of Capnography for Respiratory Monitoring by Nurses in Phase I Post-Anesthesia Care Unit: A Scoping Review
Abstract
1. Introduction
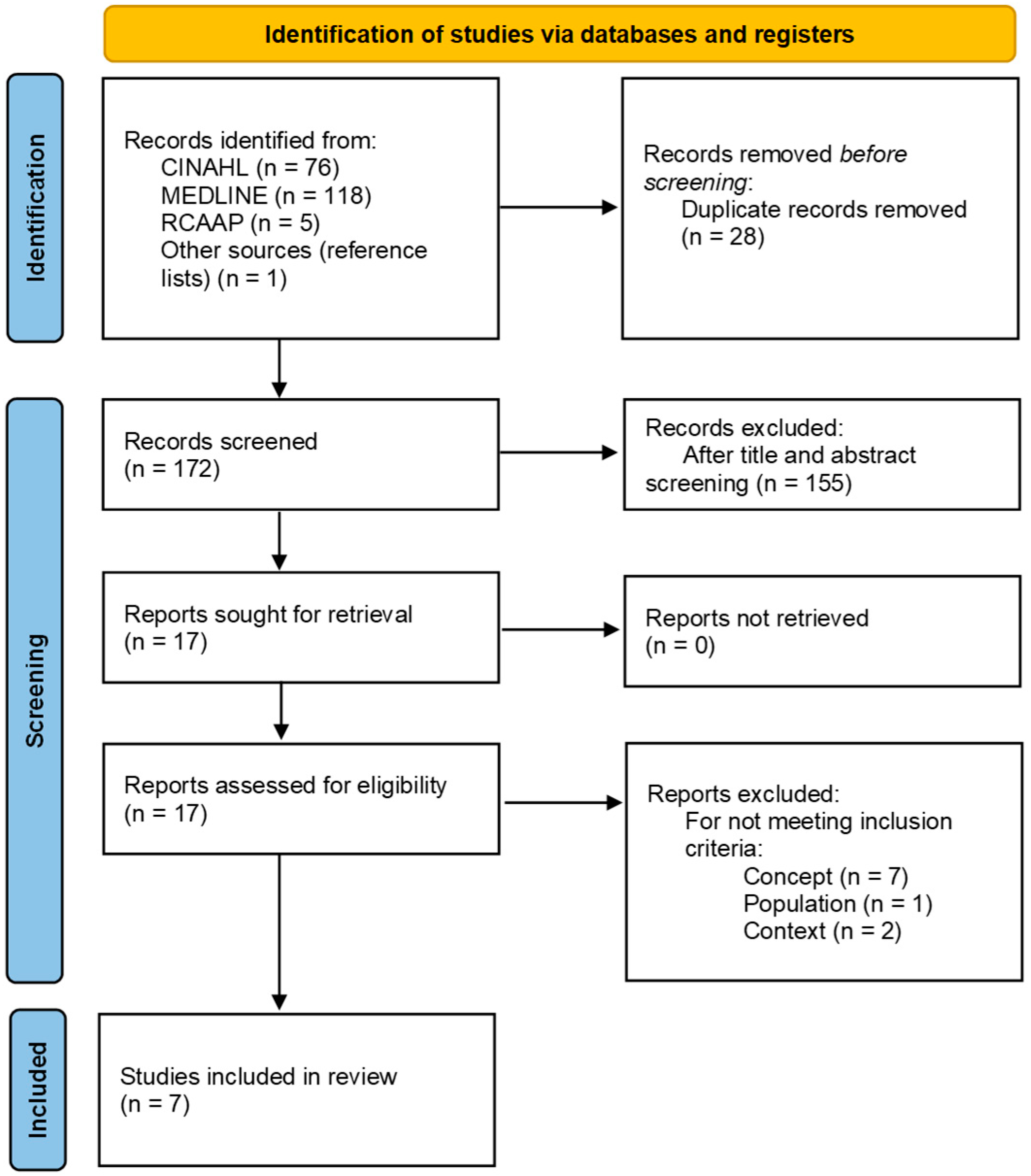
2. Methods
2.1. Identifying the Research Question
- Population: Nurses
- Concept: Barriers and facilitators to the use of capnography for respiratory monitoring
- Context: Phase I PACU
2.2. Identifying Relevant Studies
2.3. Study Selection
2.4. Data Extraction and Comprehensive Analysis
2.5. Reporting the Results
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
Abbreviations
| PACU | Post-Anesthesia Care Unit |
| AORN | Association of periOperative Registered Nurses |
| JBI | Joanna Briggs Institute |
| RCAAP | Open Access Scientific Repositories of Portugal |
| OSA | Obstructive Sleep Apnea |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews |
| PCC | Population/Concept/Context |
| QCRI | Qatar Computing Research Institute |
| PRISMA | Preferred Reporting Items for Systematic Reviews e Meta-Analyses |
| PCA | Patient Controlled-Analgesia |
| etCO2 | End-tidal Carbon Dioxide Concentration |
| USA | United States of America |
Appendix A. Search Strategy
| Search | Search Terms | Results |
|---|---|---|
| #1 | nurs* [Title/Abstract] | 546,738 |
| #2 | “Postanesthesia Nursing” [MeSH Terms] OR “Nurses” [MeSH Terms] OR “Nursing” [MeSH Terms] | 338,351 |
| #3 | “nurs*” [Title/Abstract] OR “Postanesthesia Nursing” [MeSH Terms] OR “Nurses” [MeSH Terms] OR “Nursing” [MeSH Terms] | 696,705 |
| #4 | “capno*” [Title/Abstract] OR “respiratory monitoring” [Title/Abstract] OR “carbon dioxide” [Title/Abstract] OR “end tidal carbon dioxide” [Title/Abstract] OR “respiratory assessment” [Title/Abstract] OR “respiratory complications” [Title/Abstract] | 76,533 |
| #5 | “Capnography” [MeSH Terms] OR “blood gas monitoring, transcutaneous” [MeSH Terms] OR “Carbon Dioxide” [MeSH Terms] OR “Pulmonary Ventilation” [MeSH Terms] OR “signs and symptoms, respiratory” [MeSH Terms] | 322,554 |
| #6 | “capno*” [Title/Abstract] OR “respiratory monitoring” [Title/Abstract] OR “Carbon Dioxide” [Title/Abstract] OR “end tidal carbon dioxide” [Title/Abstract] OR “respiratory assessment” [Title/Abstract] OR “respiratory complications” [Title/Abstract] OR “Capnography” [MeSH Terms] OR “blood gas monitoring, transcutaneous” [MeSH Terms] OR “Carbon Dioxide” [MeSH Terms] OR “Pulmonary Ventilation” [MeSH Terms] OR “signs and symptoms, respiratory” [MeSH Terms] | 366,211 |
| #7 | “Postanesthesia” [Title/Abstract] OR “Recovery” [Title/Abstract] OR “Postoperative” [Title/Abstract] OR “PACU” [Title/Abstract] OR “Post anesthesia care unit” [Title/Abstract] OR “Immediate postoperative” [Title/Abstract] | 1,188,357 |
| #8 | “Postoperative Period” [MeSH Terms] OR “Postoperative Care” [MeSH Terms] OR “Recovery Room” [MeSH Terms] | 122,244 |
| #9 | “Postanesthesia” [Title/Abstract] OR “Recovery” [Title/Abstract] OR “Postoperative” [Title/Abstract] OR “PACU” [Title/Abstract] OR “Post anesthesia care unit” [Title/Abstract] OR “Immediate postoperative” [Title/Abstract] OR “Postoperative Period” [MeSH Terms] OR “Postoperative Care” [MeSH Terms] OR “Recovery Room” [MeSH Terms] | 1,244,717 |
| #10 | (“nurs*” [Title/Abstract] OR (“Postanesthesia Nursing” [MeSH Terms] OR “Nurses” [MeSH Terms] OR “Nursing” [MeSH Terms])) AND (“capno*” [Title/Abstract] OR “respiratory monitoring” [Title/Abstract] OR “Carbon Dioxide” [Title/Abstract] OR “end tidal carbon dioxide” [Title/Abstract] OR “respiratory assessment” [Title/Abstract] OR “respiratory complications” [Title/Abstract] OR (“Capnography” [MeSH Terms] OR “blood gas monitoring, transcutaneous” [MeSH Terms] OR “Carbon Dioxide” [MeSH Terms] OR “Pulmonary Ventilation” [MeSH Terms] OR “signs and symptoms, respiratory” [MeSH Terms])) AND (“Postanesthesia” [Title/Abstract] OR “Recovery” [Title/Abstract] OR “Postoperative” [Title/Abstract] OR “PACU” [Title/Abstract] OR “Post anesthesia care unit” [Title/Abstract] OR “Immediate postoperative” [Title/Abstract] OR (“Postoperative Period” [MeSH Terms] OR “Postoperative Care” [MeSH Terms] OR “Recovery Room” [MeSH Terms])) | 277 |
| #11 | #10 FILTERS: English, Portuguese, Spanish | 255 |
| #12 | #10 FILTERS: English, Portuguese, Spanish; Adult: 19+ years | 118 |
| Search | Search Terms | Results |
|---|---|---|
| S1 | TI nurs* OR AB nurs* | 624,190 |
| S2 | (MH “Nurses+”) OR (MH “Perianesthesia Nursing”) OR (MH “Perioperative Nursing”) | 254,721 |
| S3 | S1 OR S2 | 719,008 |
| S4 | TI capno* OR AB capno* OR TI “respiratory monitoring” OR AB “Respiratory monitoring” OR TI “carbon dioxide” OR AB “carbon dioxide” OR TI “end tidal carbon dioxide” OR AB “end tidal carbon dioxide” OR TI “respiratory assessment” OR AB “respiratory assessment” OR TI “respiratory complications” OR AB “respiratory complications” | 9641 |
| S5 | (MH “Capnography”) OR (MH “Carbon Dioxide”) OR (MH “Signs and Symptoms, Respiratory+”) OR (MH “Blood Gas Monitoring, Transcutaneous”) | 44,729 |
| S6 | S4 OR S5 | 50,121 |
| S7 | TI “postanesthesia” OR AB “postanesthesia” OR TI “recovery” OR AB “recovery” OR TI “postoperative” OR AB “postoperative” OR TI PACU OR AB PACU OR TI “post anesthesia care unit” OR AB “post anesthesia care unit” OR TI “immediate postoperative” OR AB “immediate postoperative” | 212,894 |
| S8 | (MH “Post Anesthesia Care Units”) OR (MH “Post Anesthesia Care”) OR (MH “Postoperative Care”) OR (MH “Anesthesia Recovery”) OR (MH “Postoperative Period”) | 42,008 |
| S9 | S7 OR S8 | 234,949 |
| S10 | S3 AND S6 AND S9 | 205 |
| S11 | S10 (Limited to English, Portuguese, and Spanish languages) | 197 |
| S12 | S10 (Limited to English, Portuguese, and Spanish languages; age group: all adults) | 74 |
| Search | Search Terms | Results |
|---|---|---|
| 1 | capnografia AND enfermagem | 5 |
Appendix B. Data Extraction from the Studies
| Study | Reference Number, First Author’s Surname, Year of Publication, Country | Type of Study | Objective(s) | Population | Context | Concept (Barriers and Facilitators to the Use of Capnography for Respiratory Monitoring by Nurses in Phase I PACU) |
|---|---|---|---|---|---|---|
| S1 | [26] Hutchison et al. (2008), United States of America (USA) | Randomized prospective study | Determine whether capnography used in isolation is more sensitive than pulse oximetry (with assessment of respiratory rate through observation or auscultation) | 54 adult patients following orthopedic surgery, monitored for respiratory depression using capnography by nurses | PACU and general nursing care unit | Barriers:
|
| S2 | [27] McCarter et al. (2008), USA | Quantitative, descriptive, cross-sectional study | Evaluate the effectiveness of monitoring in the postoperative period in patients with opioid PCA | 634 adult postoperative patients receiving PCA with opioids, monitored with capnography by nurses | Postoperative period (Phase I and Phase II) | Facilitators:
|
| S3 | [28] Lakdawala et al. (2017), USA | Quality improvement project | Assess patients using the STOP-Bang screening tool; Compare high-risk and low-risk groups with respect to respiratory complications; Use and evaluate capnography in the postoperative period; Evaluate nurses’ perception of the OSA care protocol; Assess patient satisfaction with the OSA care protocol. | 161 adult neuro-surgical patients screened for OSA using STOP-Bang, monitored with capnography by nurses | Preoperative unit, PACU, and neuro-surgery unit | Barriers:
|
| S4 | [29] Jungquist et al. (2019), USA | Prospective observational study | Explore the effectiveness of using pulse oximetry, capnography, and minute ventilation to identify and anticipate opioid-induced respiratory depression in the post-anesthesia period | 60 adult patients in PACU after spine, neck, hip, or knee surgery, monitored by nurses for opioid-induced respiratory depression | PACU | Barriers:
|
| S5 | [30] Scully (2019), USA | Quality improvement project (with mixed method) | Identify undiagnosed and high-risk patients with OSA in the preoperative period using the STOP-Bang screening tool; Train PACU nurses to recognize hypoventilation through capnography and intervene to prevent respiratory complications; Implement Practice Recommendation number 10 from the American Society of PeriAnesthesia Nurses (screening for OSA and monitoring of etCO2 in patients with OSA) | 314 adult patients diagnosed with OSA, monitored by multidisciplinary team | PACU | Facilitators:
|
| S6 | [31] Atherton et al. (2022), USA | Quantitative, descriptive-correlational, and longitudinal study | Evaluate the effectiveness of an educational program on ventilatory patterns using devices that assess carbon dioxide levels in postoperative patients | 176 nurses | PACU | Facilitators:
|
| S7 | [21] Potvin et al. (2022), France | Randomized, controlled, prospective study | Study the rate of patients with alveolar hypoventilation before tracheal extubation or removal of the laryngeal mask through continuous capnography monitoring in the PACU | 52 adult patients with endotracheal tube or laryngeal mask, monitored by nurses | PACU | Facilitators:
|
References
- Ganter, M.T.; Blumenthal, S.; Dübendorfer, S.; Brunnschweiler, S.; Hofer, T.; Klaghofer, R.; Zollinger, A.; Hofer, C. The length of stay in the post-anaesthesia care unit correlates with pain intensity, nausea and vomiting on arrival. Perioper. Med. 2014, 3, 10. [Google Scholar] [CrossRef] [PubMed]
- Mourão, J.; Pereira, L.; Alves, C.; Andrade, N.; Cadilha, S.; Perdigão, L. Indicadores de segurança e qualidade em anestesiologia. Rev. Soc. Port. Anestesiol. 2018, 27, 23–27. [Google Scholar] [CrossRef]
- Jaensson, M.; Nilsson, U.; Dahlberg, K. Methods and timing in the assessment of postoperative recovery: A scoping review. Br. J. Anaesth. 2022, 129, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Mert, S. The significance of nursing care in the post-anesthesia care unit and barriers to care. Intensive Care Res. 2023, 3, 272–281. [Google Scholar] [CrossRef]
- Karcz, M.; Papadakos, P.J. Respiratory complications in the postanesthesia care unit: A review of pathophysiological mechanisms. Can. J. Respir. Ther. 2013, 49, 21–29. [Google Scholar]
- Sampaio, A.; Almeida, A.L.; Bernardino, A.; Campos, A.C.; Raimundo, A.; Marques, A.; Moura, A.; Martins, A.A.; Silva, C.; Noversa, C.; et al. Manual de Cuidados Pós-Anestésicos; Centro de Simulação Biomédica de Coimbra: Coimbra, Portugal, 2017. [Google Scholar]
- Clifford, T.L. Phase I and phase II recovery. In Perianesthesia Nursing Care: A Bedside Guide for Safe Recovery; Stannard, D., Krenzischek, D., Duarte, O., Martins, O., Eds.; Jones & Bartlett Learning: Burlington, MA, USA, 2016; pp. 19–22. [Google Scholar]
- Dahlberg, K.; Brady, J.M.; Jaensson, M.; Nilsson, U.; Odom-Forren, J. Education, competence, and role of the nurse working in the PACU: An international survey. J. Perianesth Nurs. 2021, 36, 224–331. [Google Scholar] [CrossRef] [PubMed]
- Ordem dos Enfermeiros. Regulation No. 429/2018. Diário da República, 2nd Series, No. 135. 2018. Available online: https://diariodarepublica.pt/dr/detalhe/regulamento/429-2018-115698617 (accessed on 22 March 2025).
- Association of periOperative Registered Nurses. Perioperative Nursing: Scope and Standards of Practice; Association of periOperative Registered Nurses: Denver, CO, USA, 2021. [Google Scholar]
- Eikermann, M.; Santer, P.; Ramachandran, S.K.; Pandit, J. Recent advances in understanding and managing postoperative respiratory problems. F1000Research 2019, 8, 197. [Google Scholar] [CrossRef]
- Chandler, D.; Mosieri, C.; Kallurkar, A.; Pham, A.D.; Okada, L.K.; Kaye, R.J.; Cornett, E.M.; Fox, C.J.; Urman, R.D.; Kaye, A.D. Perioperative strategies for the reduction of postoperative pulmonary complications. Best. Pr. Res. Clin. Anaesthesiol. 2020, 34, 153–166. [Google Scholar] [CrossRef]
- Fink, R.J.; Mark, J.B. Monitoração anestésica padrão e dispositivos. In Fundamentos de Anestesiologia Clínica; Barash, P., Cullen, B., Stoelting, R., Cahalan, M., Stock, M., Ortega, R., Sharar, S., Eds.; Artmed Editora: Porto Alegre, Brazil, 2017; pp. 277–297. [Google Scholar]
- Kerslake, I.; Kelly, F. Uses of capnography in the critical care unit. BJA Educ. 2017, 17, 178–183. [Google Scholar] [CrossRef]
- Chung, F.; Wong, J.; Mestek, M.L.; Niebel, K.H.; Lichtenthal, P. Characterization of respiratory compromise and the potential clinical utility of capnography in the post anesthesia care unit: A blinded observational trial. J. Clin. Monit. Comput. 2020, 34, 541–551. [Google Scholar] [CrossRef]
- Lam, T.; Nagappa, M.; Wong, J.; Singh, M.; Wong, D.; Chung, F. Continuous pulse oximetry and capnography monitoring for postoperative respiratory depression and adverse events: A systematic review and meta-analysis. Anesth. Analg. 2017, 125, 2019–2029. [Google Scholar] [CrossRef]
- Medtronic. Clinical Society Guidelines for Capnography Monitoring; Medtronic: Minneapolis, MN, USA, 2019. [Google Scholar]
- Royal College of Anaesthetists. Chapter 4: Guidelines for the Provision of Anaesthetic Services for Postoperative Care 2019; GPAS Editorial; Royal College of Anaesthetists: London, UK, 2019. [Google Scholar]
- Broens, S.; Prins, S.; Kleer, D.; Niesters, M.; Dahan, A.; Velzen, M. Postoperative respiratory state assessment using the integrated pulmonary index (IPI) and resultant nurse interventions in the post-anesthesia care unit: A randomized controlled trial. J. Clin. Monit. Comput. 2021, 35, 1093–1102. [Google Scholar] [CrossRef]
- Wilks, C.; Foran, P. Capnography monitoring in the post anaesthesia care unit (PACU). J. Perioper. Nurs. 2021, 34, 29–35. [Google Scholar] [CrossRef]
- Potvin, J.; Etchebarne, I.; Soubiron, L.; Biais, M.; Roullet, S.; Nouette-Gaulain, K. Effects of capnometry monitoring during recovery in the post-anaesthesia care unit: A randomized controlled trial in adults (CAPNOSSPI). J. Clin. Monit. Comput. 2022, 36, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Wollner, E.; Nourian, M.M.; Booth, W.; Conover, S.; Law, T.; Lilaonitkul, M.; Gelb, A.W.; Lipnick, M.S. Impact of capnography on patient safety in high-and low-income settings: A scoping review. Br. J. Anaesth. 2020, 125, 88–103. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromatis, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Int. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, P. Making sense of implementation theories, models and frameworks. Implement. Sci. 2015, 10, 53. [Google Scholar] [CrossRef]
- Hutchison, R.; Rodriguez, L. Capnography and respiratory depression. Am. J. Nurs. 2008, 108, 35–39. [Google Scholar] [CrossRef]
- McCarter, T.; Shaik, Z.; Scarfo, K.; Thompson, L.J. Capnography monitoring enhances safety of postoperative patient-controlled analgesia. Am. Health Drug Benefits. 2008, 1, 28–35. [Google Scholar]
- Lakdawala, L.; Dickey, B.; Alrawashdeh, M. Obstructive sleep apnea screening among surgical patients: A quality improvement project. J. Perianesth Nurs. 2018, 33, 814–821. [Google Scholar] [CrossRef]
- Jungquist, C.R.; Chandola, V.; Spulecki, C.; Nguyen, K.V.; Crescenzi, P.; Tekeste, D.; Sayapaneni, P.R. Identifying patients experiencing opioid-induced respiratory depression during recovery from anesthesia: The application of electronic monitoring devices. Worldviews Evid. Based Nurs. 2019, 16, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Scully, K.R.; Rickerby, J.; Dunn, J. Implementation science: Incorporating obstructive sleep apnea screening and capnography into everyday practice. J. Perianesth Nurs. 2020, 35, 7–16. [Google Scholar] [CrossRef]
- Atherton, P.; Jungquist, C.; Spulecki, C. An educational intervention to improve comfort with applying and interpreting transcutaneous CO2 and end-tidal CO2 monitoring in PACU. J. Perianesth Nurs. 2022, 37, 781–786. [Google Scholar] [CrossRef]
- Sajith, B. Respiratory depression: A case study of a postoperative patient with cancer. Clin. J. Oncol. Nurs. 2018, 22, 453–456. [Google Scholar] [CrossRef]
- Oliveira, A.E.C.; Machado, A.B.; Santos, E.D.; Almeida, E.B. Fadiga de alarmes e as implicações para a segurança do paciente. Rev. Bras. Enferm. 2018, 71, 3211–3216. [Google Scholar] [CrossRef]
- Ruskin, K.J.; Bliss, J.P. Alarm fatigue and patient safety. Anesth. Patient Saf. Found. 2019, 34, 1–28. [Google Scholar]
| Reference Number | First Author’s Surname, Year of Publication | Population | Context | Concept (Barriers and Facilitators to the Use of Capnography for Respiratory Monitoring by Nurses in Phase I PACU) |
|---|---|---|---|---|
| [26] | Hutchison et al. (2008) | 54 adult patients following orthopedic surgery, monitored for respiratory depression using capnography by nurses | PACU and general nursing care unit | Barriers:
|
| [27] | McCarter et al. (2008) | 634 adult postoperative patients receiving Patient Controlled-Analgesia (PCA), monitored with capnography by nurses | Postoperative period (Phase I and Phase II) | Facilitators:
|
| [28] | Lakdawala et al. (2017) | 161 adult neuro-surgical patients screened for OSA using STOP-Bang, monitored with capnography by nurses | Preoperative unit, PACU, and neuro-surgery unit | Barriers:
|
| [29] | Jungquist et al. (2019) | 60 adult patients in PACU after spine, neck, hip, or knee surgery, monitored by nurses for opioid-induced respiratory depression | PACU | Barriers:
|
| [30] | Scully (2019) | 314 adult patients diagnosed with OSA, monitored by multidisciplinary team | PACU | Facilitators:
|
| [31] | Atherton et al. (2022) | 176 nurses | PACU | Facilitators:
|
| [21] | Potvin et al. (2022) | 52 adult patients with endotracheal tube or laryngeal mask, monitored by nurses | PACU | Facilitators:
|
| Hutchison et al. (2008) [26] | McCarter et al. (2008) [27] | Lakdawala et al. (2017) [28] | Jungquist et al. (2019) [29] | Scully et al. (2019) [30] | Atherton et al. (2022) [31] | Potvin et al. (2022) [21] | ||
|---|---|---|---|---|---|---|---|---|
| Barriers | High workload | X | ||||||
| Perceived lack of patient adherence | X | X | X | |||||
| Lack of knowledge | X | X | ||||||
| Facilitators | Alarm sound | X | ||||||
| Patient education | X | X | ||||||
| Anticipating patient clinical instability | X | X | X | X | ||||
| Increased nurse confidence | X | X | ||||||
| Perception of enhanced safety | X | X | X | X | X | |||
| Targeted nurse training | X | X | X | X | X | |||
| Continuous improvement in care delivery | X | |||||||
| Effective communication and feedback | X | |||||||
| Promotion of sustainable practices | X | |||||||
| Prior knowledge and exposure | X |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assunção, A.S.L.; Cunha, L.D.M. Barriers and Facilitators to the Use of Capnography for Respiratory Monitoring by Nurses in Phase I Post-Anesthesia Care Unit: A Scoping Review. Nurs. Rep. 2025, 15, 292. https://doi.org/10.3390/nursrep15080292
Assunção ASL, Cunha LDM. Barriers and Facilitators to the Use of Capnography for Respiratory Monitoring by Nurses in Phase I Post-Anesthesia Care Unit: A Scoping Review. Nursing Reports. 2025; 15(8):292. https://doi.org/10.3390/nursrep15080292
Chicago/Turabian StyleAssunção, Adriana Sofia Lucas, and Lara Daniela Matos Cunha. 2025. "Barriers and Facilitators to the Use of Capnography for Respiratory Monitoring by Nurses in Phase I Post-Anesthesia Care Unit: A Scoping Review" Nursing Reports 15, no. 8: 292. https://doi.org/10.3390/nursrep15080292
APA StyleAssunção, A. S. L., & Cunha, L. D. M. (2025). Barriers and Facilitators to the Use of Capnography for Respiratory Monitoring by Nurses in Phase I Post-Anesthesia Care Unit: A Scoping Review. Nursing Reports, 15(8), 292. https://doi.org/10.3390/nursrep15080292






