Outcomes of a Risk-Stratified Protocol for Preventing Peristomal Skin Complications in Patients with an Ostomy: A Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting
2.3. Risk Stratification-Based Educational Approach (The Dermamecum Protocol)
2.3.1. Green Path
2.3.2. Yellow Path
2.3.3. Red Path
2.4. Study Procedure
Ethical Considerations
2.5. Eligibility Criteria
2.6. Outcomes
2.7. Measurements
2.8. Sample Size
2.9. Data Analysis
3. Results
3.1. Sample Characteristics
Baseline Assessments
3.2. Early Onset Complications (30 Days)
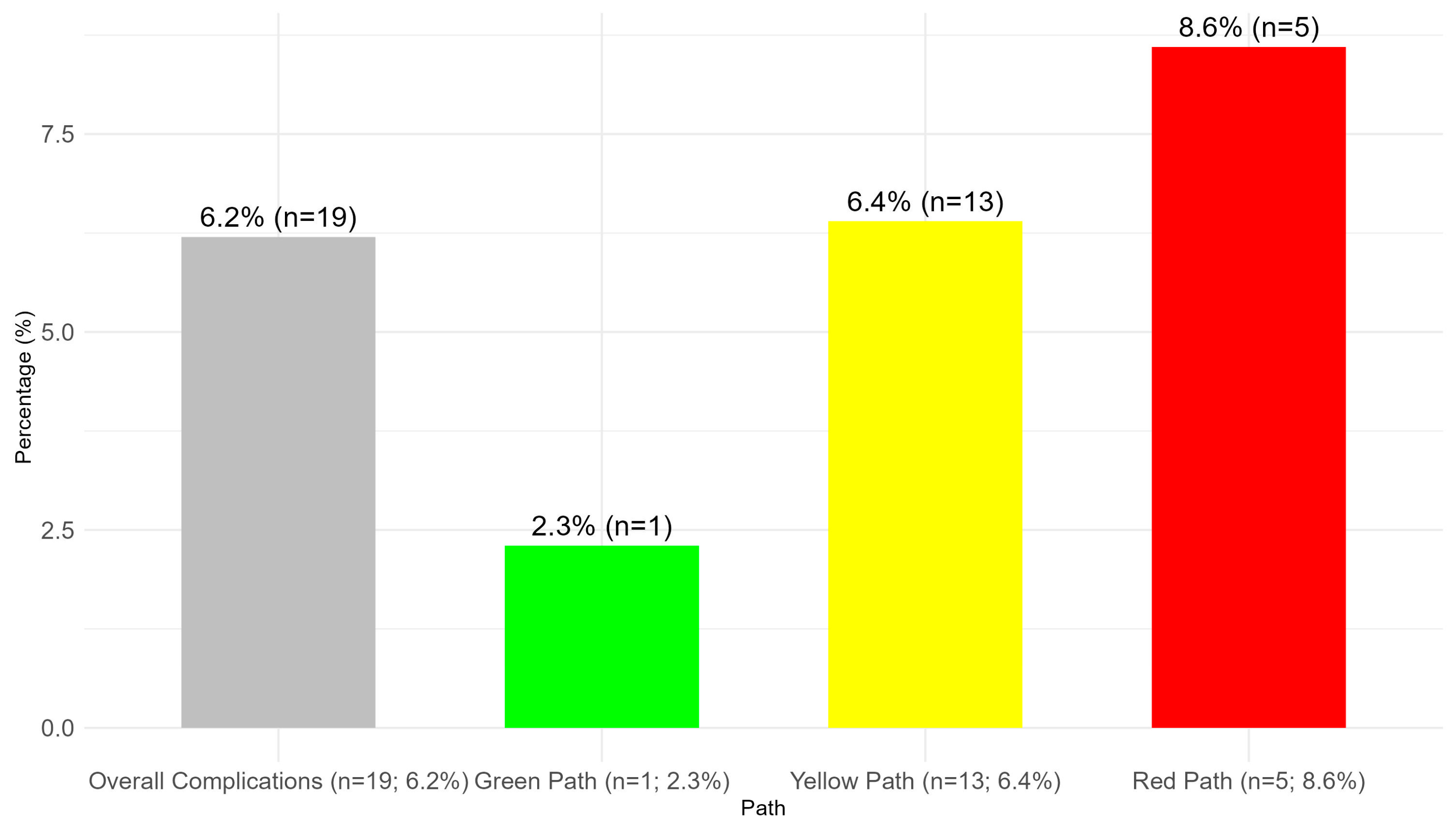
3.3. Late-Onset Complications
3.3.1. PSCs at 60 Days
3.3.2. PSCs at 90 Days
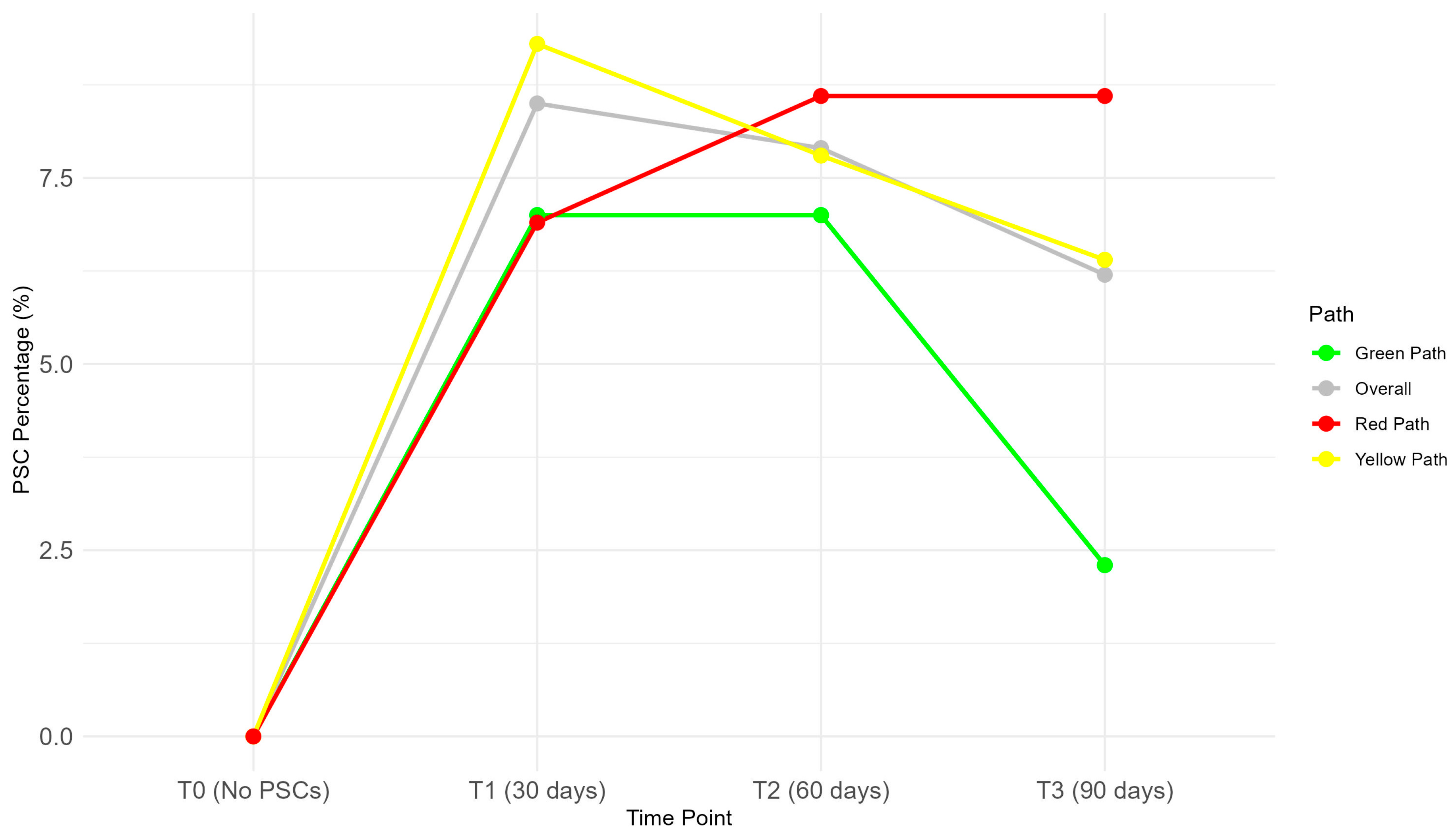
3.3.3. Trends in PSCs over Time
3.4. Self-Care
3.4.1. Self-Care at 30 Days
3.4.2. Self-Care at 60 Days
3.4.3. Self-Care: Trends
3.5. HRQoL
3.5.1. HRQoL at Baseline
3.5.2. HRQoL at 30 Days (T1)
3.5.3. HRQoL at 90 Days (T2)
3.5.4. Trends in HRQoL
3.6. Satisfaction (Assessed at T2)
3.7. Poisson Regression for Temporal Trends in PSCs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
Abbreviations
| PSC | Peristomal skin complication |
| HRQoL | Health-related quality of life |
| IRR | Incidence rate ratio |
| IQR | Interquartile range |
| SD | Standard deviation |
| T0, T1, T2, T3 | Time points (baseline, 30 days, 60 days, 90 days) |
| BMI | Body mass index |
| SF-36 | Short Form-36 Health Survey |
| BH | Benjamini–Hochberg adjustment |
References
- Dellafiore, F.; Caruso, R.; Bonavina, L.; Udugampolage, N.S.; Villa, G.; Russo, S.; Vangone, I.; BaronI, I.; Di Pasquale, C.; Nania, T.; et al. Risk Factors and Pooled Incidence of Intestinal Stoma Complications: Systematic Review and Meta-Analysis. Curr. Med. Res. Opin. 2022, 38, 1103–1113. [Google Scholar] [CrossRef] [PubMed]
- Dellafiore, F.; Manara, D.F.; Arrigoni, C.; Baroni, I.; Di Pasquale, C.; Nania, T.; Caruso, R.; Villa, G. Predictors of Adjustment to Living with an Ostomy: Results of a Cross-Sectional Study. Adv. Skin. Wound Care 2022, 35, 1–6. [Google Scholar] [CrossRef]
- Tsujinaka, S.; Tan, K.-Y.; Miyakura, Y.; Fukano, R.; Oshima, M.; Konishi, F.; Rikiyama, T. Current Management of Intestinal Stomas and Their Complications. J. Anus Rectum Colon. 2020, 4, 25–33. [Google Scholar] [CrossRef]
- Guerra, E.; Denti, F.C.; Di Pasquale, C.; Caroppo, F.; Angileri, L.; Cioni, M.; Parodi, A.; Fortina, A.B.; Ferrucci, S.; Burlando, M. Peristomal Skin Complications: Detailed Analysis of a Web-Based Survey and Predictive Risk Factors. Healthcare 2023, 11, 1823. [Google Scholar] [CrossRef] [PubMed]
- Dellafiore, F.; Conte, G.; Baroni, I.; Pittella, F.; Di Pasquale, C.; Nania, T.; Saracco, C.; Roveron, G.; Caruso, R. Ostomy Adjustment Inventory-23 (OAI-23): Development and Testing of the Italian Version. J. Wound Ostomy Cont. Nurs. 2019, 46, 38–43. [Google Scholar] [CrossRef]
- Alenezi, A.; McGrath, I.; Kimpton, A.; Livesay, K. Quality of Life among Ostomy Patients: A Narrative Literature Review. J. Clin. Nurs. 2021, 30, 3111–3123. [Google Scholar] [CrossRef]
- Dellafiore, F.; Pittella, F.; Arrigoni, C.; Baroni, I.; Conte, G.; Di Pasquale, C.; Casole, L.; Villa, G.; Caruso, R. A Multi-Phase Study for the Development of a Self-Efficacy Measuring Scale for Ostomy Care Nursing Management. J. Adv. Nurs. 2020, 76, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Giordano, V.; Nicolotti, M.; Corvese, F.; Vellone, E.; Alvaro, R.; Villa, G. Describing Self-Care and Its Associated Variables in Ostomy Patients. J. Adv. Nurs. 2020, 76, 2982–2992. [Google Scholar] [CrossRef]
- Denti, F.C.; Guerra, E.; Caroppo, F.; Abruzzese, P.; Alessi, F.; Barone, F.; Bernardino, P.; Bergamini, M.; Bernardo, C.; Bosio, G.; et al. Exploring the Impact of a Structured Educational Approach on Peristomal Skin Complications: An Interim Analysis. Healthcare 2024, 12, 1805. [Google Scholar] [CrossRef]
- Burch, J.; Boyles, A.; Maltby, E.; Marsden, J.; Martin, N.; McDermott, B.; Voegeli, D. Keep It Simple: Peristomal Skin Health, Quality of Life and Wellbeing. Br. J. Nurs. 2021, 30, 5–24. [Google Scholar] [CrossRef]
- LeBlanc, K.; Furtado, S.; Mings, D.; Martin, M.; Evans, M.; Eaves, D.; Skountrianos, G. A Cost-Effectiveness Model to Determine Ostomy-Related Costs of Care and Health Outcomes Among People With an Ostomy in Canada Using a Ceramide-Infused Skin Barrier. J. Wound Ostomy Cont. Nurs. 2023, 50, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Taggart, E.; Spencer, K. Maintaining Peristomal Skin Health with Ceramide-Infused Hydrocolloid Skin Barrier. World Counc. Enteros. Ther. J. 2018, 38, S8. [Google Scholar]
- Grove, G.; Houser, T.; Sibbald, G.; Salvadalena, G. Measuring Epidermal Effects of Ostomy Skin Barriers. Skin. Res. Technol. 2019, 25, 179–186. [Google Scholar] [CrossRef]
- Stephen-Haynes, J. The Outcomes of Barrier Protection in Periwound Skin and Stoma Care. Br. J. Nurs. 2014, 23, S26+S28–S30. [Google Scholar] [CrossRef]
- Salvadalena, G.; Colwell, J.C.; Skountrianos, G.; Pittman, J. Lessons Learned About Peristomal Skin Complications: Secondary Analysis of the ADVOCATE Trial. J. Wound Ostomy Continence Nurs. 2020, 47, 357–363. [Google Scholar] [CrossRef]
- Maydick-Youngberg, D. A Descriptive Study to Explore the Effect of Peristomal Skin Complications on Quality of Life of Adults With a Permanent Ostomy. Ostomy Wound Manag. 2017, 63, 10–23. [Google Scholar]
- Cuschieri, S. The STROBE Guidelines. Saudi J. Anaesth. 2019, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Vernon, E. Patient Assessment and Stoma Siting. In Stoma Care Specialist Nursing: A Guide for Clinical Practice; White, M., Perrin, A., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 195–205. ISBN 978-3-031-07798-2. [Google Scholar]
- Khalilzadeh Ganjalikhani, M.; Tirgari, B.; Roudi Rashtabadi, O.; Shahesmaeili, A. Studying the Effect of Structured Ostomy Care Training on Quality of Life and Anxiety of Patients with Permanent Ostomy. Int. Wound J. 2019, 16, 1383–1390. [Google Scholar] [CrossRef] [PubMed]
- Villa, G.; Vellone, E.; Sciara, S.; Stievano, A.; Proietti, M.G.; Manara, D.F.; Marzo, E.; Pantaleo, G. Two New Tools for Self-care in Ostomy Patients and Their Informal Caregivers: Psychosocial, Clinical, and Operative Aspects. Int. J. Urol. Nurs. 2019, 13, 23–30. [Google Scholar] [CrossRef]
- Jenkinson, C.; Coulter, A.; Wright, L. Short Form 36 (SF36) Health Survey Questionnaire: Normative Data for Adults of Working Age. BMJ 1993, 306, 1437–1440. [Google Scholar] [CrossRef]
- Riegel, B.; Jaarsma, T.; Strömberg, A. A Middle-Range Theory of Self-Care of Chronic Illness. Adv. Nurs. Sci. 2012, 35, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, J.; Alqahtani, I. Self-Care in the Older Adult Population with Chronic Disease: Concept Analysis. Heliyon 2022, 8, e09991. [Google Scholar] [CrossRef]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey. J. Clin. Epidemiol. 1998, 51, 1025–1036. [Google Scholar] [CrossRef] [PubMed]
- Raudenská, P. Single-Item Measures of Happiness and Life Satisfaction: The Issue of Cross-Country Invariance of Popular General Well-Being Measures. Humanit. Soc. Sci. Commun. 2023, 10, 861. [Google Scholar] [CrossRef]
- Kang, H. Sample Size Determination and Power Analysis Using the G*Power Software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef] [PubMed]
- Herson, J.; Wittes, J. The Use of Interim Analysis for Sample Size Adjustment. Drug Inf. J. 1993, 27, 753–760. [Google Scholar] [CrossRef]
- Tutz, G. Poisson Regression. In International Encyclopedia of Statistical Science; Lovric, M., Ed.; Springer: Berlin, Germany, 2011; pp. 1075–1077. ISBN 978-3-642-04897-5. [Google Scholar]
- Rolls, N.; De Fries Jensen, L.; Mthombeni, F.; Vardanega, V.; Håkan-Bloch, J.; Van Hest, N.; Karlsmark, T. Healthcare Resource Use and Associated Costs for Patients with an Ileostomy Experiencing Peristomal Skin Complications. Int. Wound J. 2023, 20, 2540–2550. [Google Scholar] [CrossRef]
- Maglio, A.; Malvone, A.P.; Scaduto, V.; Brambilla, D.; Denti, F.C. The Frequency of Early Stomal, Peristomal and Skin Complications. Br. J. Nurs. 2021, 30, 1272–1276. [Google Scholar] [CrossRef]
- Fellows, J.; Voegeli, D.; Håkan-Bloch, J.; Herschend, N.O.; Størling, Z. Multinational Survey on Living with an Ostomy: Prevalence and Impact of Peristomal Skin Complications. Br. J. Nurs. 2021, 30, S22–S30. [Google Scholar] [CrossRef]
- Steinhagen, E.; Colwell, J.; Cannon, L. Intestinal Stomas—Postoperative Stoma Care and Peristomal Skin Complications. Clin. Colon Rectal surgery 2017, 30, 184–192. [Google Scholar] [CrossRef]
- Ratliff, C.R. Early Peristomal Skin Complications Reported by WOC Nurses. J. Wound Ostomy Cont. Nurs. 2010, 37, 505–510. [Google Scholar] [CrossRef]
- D’Ambrosio, F.; Pappalardo, C.; Scardigno, A.; Maida, A.; Ricciardi, R.; Calabrò, G.E. Peristomal Skin Complications in Ileostomy and Colostomy Patients: What We Need to Know from a Public Health Perspective. Int. J. Environ. Res. Public. Health 2022, 20, 79. [Google Scholar] [CrossRef] [PubMed]
- Down, G.; Bain, K.; Andersen, B.D.; Martins, L.; Karlsmark, T.; Jemec, G.; Bain, M.; Nielsen, L.F.; Bechshoeft, C.J.; Hansen, A.S. Clinical Preventive-Based Best Practices to Reduce the Risk of Peristomal Skin Complications—An International Consensus Report. World Counc. Enteros. Ther. J. 2023, 43, 11–19. [Google Scholar] [CrossRef]
- Kennel, K.D.; Barrett, T.; Smith Brown, J.; Tucker, J. Self-Care in Nursing Education. J. Nurs. Educ. 2024, 63, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Aujla, M.; Narasimhan, M. The Cycling of Self-Care through History. Lancet 2023, 402, 2066–2067. [Google Scholar] [CrossRef]
- Yoo, B.H.; Sheldon, B.L.; Podger, R.N. Analyses of Oviposition Times and Intervals in a Wide Range of Layer Flocks under Normal and Continuous Lighting Regimes. Br. Poult. Sci. 1986, 27, 267–287. [Google Scholar] [CrossRef]
- Colomer-Pérez, N.; Paredes-Carbonell, J.J.; Sarabia-Cobo, C.; Useche, S.A.; Gea-Caballero, V. Self-Care and Sense of Coherence: A Salutogenic Model for Health and Care in Nursing Education. Int. J. Environ. Res. Public Health 2022, 19, 9482. [Google Scholar] [CrossRef]
- Marcomini, I.; Iovino, P.; Rasero, L.; Manara, D.F.; Vellone, E.; Villa, G. Self-Care and Quality of Life of Ostomy Patients: A Structural Equation Modeling Analysis. Nurs. Rep. 2024, 14, 3417–3426. [Google Scholar] [CrossRef]
- Mo, J.; Wendel, C.S.; Sloan, J.A.; Sun, V.; Hornbrook, M.C.; Grant, M.; Ercolano, E.; Malkowicz, S.B.; Tallman, N.J.; McCorkle, R.C.; et al. Stoma Location and Ostomy-Related Quality of Life among Cancer Survivors with Ostomies: A Pooled Analysis. Am. J. Surg. 2022, 223, 963–968. [Google Scholar] [CrossRef]
- de Santos, V.L.C.G.; Augusto, F.d.S.; Gomboski, G. Health-Related Quality of Life in Persons With Ostomies Managed in an Outpatient Care Setting. J. Wound Ostomy Continence Nurs. 2016, 43, 158–164. [Google Scholar] [CrossRef]
- Stavropoulou, A.; Vlamakis, D.; Kaba, E.; Kalemikerakis, I.; Polikandrioti, M.; Fasoi, G.; Vasilopoulos, G.; Kelesi, M. “Living with a Stoma”: Exploring the Lived Experience of Patients with Permanent Colostomy. Int. J. Environ. Res. Public. Health 2021, 18, 8512. [Google Scholar] [CrossRef] [PubMed]
- Maalouf, M.F.; Wang, A.; Robitaille, S.; Liberman, A.S.; Fiore, J.F.; Feldman, L.S.; Lee, L. Patient Perspective on Adapting to Bowel Dysfunction after Rectal Cancer Surgery. Colorectal Dis. 2024, 26, 1701–1710. [Google Scholar] [CrossRef] [PubMed]
- Maalouf, M.F.; Robitaille, S.; Penta, R.; Pook, M.; Liberman, A.S.; Fiore, J.F.; Feldman, L.S.; Lee, L. Understanding the Impact of Bowel Dysfunction on Quality of Life After Rectal Cancer Surgery from the Patient’s Perspective. Dis. Colon. Rectum 2023, 66, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, L.; Zhu, L. The Impact of Stoma Management Education on the Self-Care Abilities of Individuals with an Intestinal Stoma. Gastrointest. Nurs. 2023, 21, S14–S21. [Google Scholar] [CrossRef]
- Simpson, E.; Pourshahidi, K.; Davis, J.; Slevin, M.; Lawther, R.; O’Connor, G.; Porrett, T.; Marley, J.; Gill, C. Living with and without an Intestinal Stoma: Factors That Promote Psychological Well-being and Self-care: A Cross-sectional Study. Nurs. Open 2023, 10, 7811–7825. [Google Scholar] [CrossRef]
- Chan, M.S.; Moore, Z.; Patton, D.; McNamara, D.; O’Connor, T.; Avsar, P. A Systematic Review of Patient Risk Factors for Complications Following Stoma Formation among Adults Undergoing Colorectal Surgery. Int. J. Colorectal Dis. 2023, 38, 238. [Google Scholar] [CrossRef]
- Slocum, T.A.; Joslyn, P.R.; Nichols, B.; Pinkelman, S.E. Revisiting an Analysis of Threats to Internal Validity in Multiple Baseline Designs. Perspect. Behav. Sci. 2022, 45, 681–694. [Google Scholar] [CrossRef]
- Kim, S. Overview of Clinical Study Designs. Clin. Exp. Emerg. Med. 2024, 11, 33–42. [Google Scholar] [CrossRef]
- Althubaiti, A. Sample Size Determination: A Practical Guide for Health Researchers. J. Gen. Fam. Med. 2023, 24, 72–78. [Google Scholar] [CrossRef]
- Murad, M.H.; Katabi, A.; Benkhadra, R.; Montori, V.M. External Validity, Generalisability, Applicability and Directness: A Brief Primer. BMJ Evid.-Based Med. 2018, 23, 17–19. [Google Scholar] [CrossRef]
- Piedmont, R.L. Social Desirability Bias. In Encyclopedia of Quality of Life and Well-Being Research; Maggino, F., Ed.; Springer International Publishing: Cham, Switzerland, 2023; p. 6526. ISBN 978-3-031-17298-4. [Google Scholar]
- Lu, H.; Cole, S.R.; Howe, C.J.; Westreich, D. Toward a Clearer Definition of Selection Bias When Estimating Causal Effects. Epidemiology 2022, 33, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Arrigoni, C.; Grugnetti, A.M.; Caruso, R. Nursing Students’ Clinical Competencies: A Survey on Clinical Education Objectives. Ann. Ig. Med. Prev. E Comunità 2017, 29, 179–188. [Google Scholar] [CrossRef]
- Averitt, A.J.; Ryan, P.B.; Weng, C.; Perotte, A. A Conceptual Framework for External Validity. J. Biomed. Inform. 2021, 121, 103870. [Google Scholar] [CrossRef] [PubMed]


| Time Point | Clinical Assessment | PSC ¶ | Self-Care | HRQoL | Satisfaction |
|---|---|---|---|---|---|
| Baseline (T0) | Yes | Yes * | No | Yes | No |
| T1 (30 days) | Yes | Yes | Yes | Yes | No |
| T2 (60 days) | Yes | Yes | Yes | Yes | Yes |
| T3 (90 days) | Yes | Yes | No | Yes | No |
| Overall (n = 305) | Green Path (n = 43; 14.1% of the Total) | Yellow Path (n = 204; 66.9% of the Total) | Red Path (n = 58; 19.0% of the Total) | p ¥ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |||
| Pre-operative information | ||||||||||
| Sex | ||||||||||
| Male | 173 | 56.7 | 9 | 20.9 | 131 | 64.2 | 33 | 56.9 | <0.001 | |
| Female | 132 | 43.3 | 34 | 79.1 | 73 | 35.8 | 25 | 43.1 | ||
| Age | ||||||||||
| Years (mean; SD) | 65.75 | 14.11 | 68.91 | 13.68 | 65.22 | 14.20 | 65.29 | 14.06 | 0.251 | |
| BMI | ||||||||||
| Underweight | 33 | 10.8 | 2 | 4.7 | 21 | 10.3 | 10 | 17.2 | <0.001 | |
| Normal | 158 | 51.8 | 35 | 81.4 | 107 | 52.5 | 16 | 27.6 | ||
| Overweight | 83 | 27.2 | 5 | 11.6 | 57 | 27.9 | 21 | 36.2 | ||
| Obese | 31 | 10.2 | 1 | 2.3 | 19 | 9.3 | 11 | 19.0 | ||
| Comorbidity | ||||||||||
| Diabetes | 41 | 13.4 | 3 | 7.0 | 34 | 16.7 | 4 | 6.9 | 0.003 | |
| IBD | 21 | 6.9 | 2 | 4.7 | 8 | 3.9 | 11 | 19.0 | ||
| Hematologic disorders | 25 | 8.2 | 2 | 4.7 | 21 | 10.3 | 2 | 3.4 | ||
| Cardiovascular disorders | 116 | 38.0 | 15 | 34.9 | 83 | 40.7 | 18 | 31.0 | ||
| Psoriasis | 1 | 0.3 | 0 | 0 | 0 | 0 | 1 | 1.7 | ||
| Atopic dermatitis | 8 | 2.6 | 2 | 4.7 | 4 | 2.0 | 2 | 3.4 | ||
| Allergic dermatitis | 22 | 7.2 | 2 | 4.7 | 15 | 7.4 | 5 | 8.6 | ||
| Any | 166 | 54.4 | 22 | 51.2 | 112 | 54.9 | 32 | 55.2 | 0.898 | |
| Previous treatment | ||||||||||
| Neoadjuvant Chemotherapy | 67 | 22.0 | 6 | 14 | 56 | 27.5 | 5 | 8.6 | 0.004 | |
| Radiotherapy | 44 | 14.4 | 3 | 7.0 | 35 | 17.2 | 6 | 10.3 | 0.139 | |
| Any previous surgeries | ||||||||||
| Yes | 88 | 28.9 | 13 | 30.2 | 57 | 27.9 | 18 | 31.6 | 0.849 | |
| Type of stoma that was planned | ||||||||||
| Colostomy | 123 | 40.3 | 20 | 46.5 | 84 | 41.2 | 19 | 32.8 | 0.009 | |
| Ileostomy | 121 | 39.7 | 10 | 23.3 | 78 | 38.2 | 33 | 56.9 | ||
| Urostomy | 61 | 20.0 | 13 | 30.2 | 42 | 20.6 | 6 | 10.3 | ||
| A stoma siting was scheduled | ||||||||||
| Yes | 240 | 79.5 | 39 | 90.7 | 162 | 79.8 | 39 | 69.6 | 0.036 | |
| Job types | ||||||||||
| Sedentary | 20 | 6.6 | 8 | 18.6 | 8 | 3.9 | 4 | 6.9 | 0.009 | |
| Semi-sedentary | 92 | 30.2 | 12 | 27.9 | 67 | 32.8 | 13 | 22.4 | ||
| Non-sedentary | 79 | 25.9 | 7 | 16.3 | 58 | 28.4 | 14 | 24.1 | ||
| Not working | 114 | 37.4 | 16 | 37.2 | 71 | 34.8 | 27 | 46.6 | ||
| Sport activity | ||||||||||
| Never | 170 | 55.7 | 25 | 58.1 | 107 | 52.5 | 38 | 65.5 | 0.194 | |
| Rarely | 83 | 27.2 | 11 | 25.6 | 57 | 27.9 | 15 | 25.9 | ||
| Often | 38 | 12.5 | 7 | 16.3 | 29 | 14.2 | 2 | 3.4 | ||
| Always | 14 | 4.6 | 0 | 0 | 11 | 5.4 | 3 | 5.2 | ||
| Post-operative (15 days)– Dermamecum baseline | ||||||||||
| Scheduled stoma site implemented | ||||||||||
| Yes | 221 | 72.5 | 36 | 83.7 | 150 | 73.5 | 35 | 60.3 | 0.029 | |
| Diet | ||||||||||
| Low residue | 108 | 35.4 | 22 | 51.2 | 74 | 36.3 | 12 | 20.7 | 0.027 | |
| For ileostomy | 102 | 33.4 | 10 | 23.3 | 67 | 32.8 | 25 | 43.1 | ||
| No special diet | 57 | 18.7 | 7 | 16.3 | 41 | 20.1 | 9 | 15.5 | ||
| Other | 38 | 12.5 | 4 | 9.3 | 22 | 10.8 | 12 | 20.7 | ||
| Abdomen profile | ||||||||||
| Regular | 189 | 62.0 | 39 | 90.7 | 135 | 66.2 | 15 | 25.9 | <0.001 | |
| Extroflexed | 68 | 22.3 | 4 | 9.3 | 39 | 19.1 | 25 | 43.1 | ||
| Introflexed | 48 | 15.7 | 0 | 0 | 30 | 14.7 | 18 | 31.0 | ||
| Physical form of the stoma post-surgery | ||||||||||
| Extroflexed | 95 | 31.1 | 10 | 23.3 | 69 | 33.7 | 16 | 27.6 | 0.478 | |
| Normal | 81 | 26.6 | 14 | 32.6 | 48 | 23.4 | 19 | 32.8 | ||
| Low | 51 | 16.7 | 6 | 14.0 | 39 | 19.0 | 6 | 10.3 | ||
| Flat | 36 | 11.8 | 5 | 11.6 | 23 | 11.2 | 8 | 13.8 | ||
| Introflexed | 39 | 12.8 | 8 | 18.6 | 24 | 11.7 | 7 | 12.1 | ||
| Missing data | 3 | 1.0 | 0 | 0 | 1 | 0.5 | 2 | 3.4 | ||
| Post-surgical herniation and prolapse complications | ||||||||||
| Incisional hernia | 7 | 2.3 | 2 | 4.7 | 3 | 1.5 | 2 | 3.4 | 0.424 | |
| Prolapse | 5 | 1.6 | 0 | 0 | 3 | 1.5 | 2 | 3.4 | ||
| Hernia | 1 | 0.3 | 0 | 0 | 1 | 0.5 | 0 | 0 | ||
| Device | ||||||||||
| Single-piece device | 149 | 48.9 | 24 | 55.8 | 97 | 47.5 | 28 | 48.3 | 0.629 | |
| Two-piece device | 153 | 50.2 | 19 | 44.2 | 106 | 52.0 | 28 | 48.3 | ||
| Missing data | 3 | 1.0 | 0 | 0 | 1 | 0.5 | 2 | 3.4 | ||
| Device baseplate | ||||||||||
| Flat | 109 | 35.7 | 15 | 34.9 | 71 | 34.8 | 23 | 41.1 | 0.120 | |
| Traditional convex | 183 | 60.0 | 24 | 55.8 | 126 | 61.8 | 33 | 58.9 | ||
| Deep convex | 10 | 3.3 | 4 | 9.3 | 6 | 2.9 | 0 | 0 | ||
| Missing data | 3 | 1.0 | 0 | 0 | 1 | 0.5 | 2 | 3.4 | ||
| Baseplate material | ||||||||||
| Hydrocolloid | 230 | 75.4 | 28 | 65.1 | 155 | 76.0 | 47 | 81.0 | 0.093 | |
| Hydrocolloid plus nonwoven textile | 72 | 23.6 | 15 | 34.9 | 48 | 23.5 | 9 | 15.5 | ||
| Missing data | 3 | 1.0 | 0 | 0 | 1 | 0.5 | 2 | 3.4 | ||
| Caregiver support | ||||||||||
| Full | 91 | 29.8 | 13 | 30.2 | 59 | 28.9 | 19 | 32.8 | 0.719 | |
| Partial | 82 | 26.9 | 8 | 18.6 | 59 | 28.9 | 15 | 25.9 | ||
| Supervisory | 42 | 13.8 | 6 | 14.0 | 27 | 13.2 | 9 | 15.5 | ||
| None | 87 | 28.5 | 16 | 37.2 | 58 | 28.4 | 13 | 22.4 | ||
| Missing data | 3 | 1.0 | 0 | 0 | 1 | 0.5 | 2 | 3.4 | ||
| Ostomy care products | ||||||||||
| Pasta with alcohol | 38 | 12.6 | 7 | 16.3 | 25 | 12.3 | 6 | 10.7 | 0.810 | |
| Alcohol-free paste | 107 | 35.4 | 16 | 37.2 | 66 | 32.5 | 25 | 44.6 | ||
| Protective film | 168 | 55.6 | 23 | 53.5 | 111 | 54.7 | 34 | 60.7 | ||
| Remover utilization | 261 | 86.4 | 36 | 83.7 | 176 | 86.7 | 49 | 87.5 | ||
| Belt | 38 | 12.6 | 4 | 9.3 | 29 | 14.3 | 5 | 8.9 | ||
| Rings | 23 | 7.6 | 1 | 2.3 | 14 | 6.9 | 8 | 14.3 | ||
| Powder | 49 | 16.2 | 8 | 18.6 | 33 | 16.3 | 8 | 14.3 | ||
| Extenders | 11 | 3.6 | 2 | 4.7 | 6 | 3.0 | 3 | 5.4 | ||
| Hygiene | ||||||||||
| Neutral pH soap | 176 | 58.3 | 20 | 46.5 | 122 | 60.1 | 34 | 60.7 | 0.640 | |
| Acid pH soap | 81 | 26.8 | 15 | 34.9 | 54 | 26.6 | 12 | 21.4 | ||
| Basic pH soap | 19 | 3.3 | 1 | 2.3 | 8 | 3.9 | 1 | 1.7 | ||
| Non-woven gauze | 145 | 48.0 | 27 | 62.8 | 93 | 45.8 | 25 | 44.6 | ||
| Wet wipes | 54 | 17.9 | 11 | 25.6 | 33 | 16.3 | 10 | 17.9 | ||
| Predictor | Coefficient | Standard Error | z-Value | Incidence Rate Ratio (IRR) | p |
|---|---|---|---|---|---|
| Intercept | 0.031 | 0.075 | 0.412 | 1.031 | 0.681 |
| Time (T1) | 0.217 | 0.085 | 2.553 | 1.243 | 0.011 |
| Time (T2) | 0.312 | 0.089 | 3.506 | 1.366 | <0.001 |
| Time (T3) | 0.201 | 0.082 | 2.451 | 1.223 | 0.014 |
| Path (Green) | −0.453 | 0.104 | −4.356 | 0.636 | <0.001 |
| Path (Yellow) | −0.112 | 0.098 | −1.143 | 0.894 | 0.253 |
| Sex (Male) | 0.089 | 0.067 | 1.331 | 1.093 | 0.183 |
| Age | 0.021 | 0.005 | 4.200 | 1.021 | <0.001 |
| BMI (Overweight) | 0.157 | 0.072 | 2.181 | 1.170 | 0.029 |
| BMI (Obese) | 0.251 | 0.085 | 2.953 | 1.285 | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denti, F.C.; Guerra, E.; Caroppo, F.; Abruzzese, P.; Alessi, F.; Barone, F.; Bernardino, P.; Bergamini, M.; Bernardo, M.C.; Bosio, G.; et al. Outcomes of a Risk-Stratified Protocol for Preventing Peristomal Skin Complications in Patients with an Ostomy: A Cohort Study. Nurs. Rep. 2025, 15, 179. https://doi.org/10.3390/nursrep15050179
Denti FC, Guerra E, Caroppo F, Abruzzese P, Alessi F, Barone F, Bernardino P, Bergamini M, Bernardo MC, Bosio G, et al. Outcomes of a Risk-Stratified Protocol for Preventing Peristomal Skin Complications in Patients with an Ostomy: A Cohort Study. Nursing Reports. 2025; 15(5):179. https://doi.org/10.3390/nursrep15050179
Chicago/Turabian StyleDenti, Francesco Carlo, Eliana Guerra, Francesca Caroppo, Pietro Abruzzese, Fabrizio Alessi, Filippo Barone, Pasqualina Bernardino, Massimiliano Bergamini, Maria Cristina Bernardo, Gloria Bosio, and et al. 2025. "Outcomes of a Risk-Stratified Protocol for Preventing Peristomal Skin Complications in Patients with an Ostomy: A Cohort Study" Nursing Reports 15, no. 5: 179. https://doi.org/10.3390/nursrep15050179
APA StyleDenti, F. C., Guerra, E., Caroppo, F., Abruzzese, P., Alessi, F., Barone, F., Bernardino, P., Bergamini, M., Bernardo, M. C., Bosio, G., Carp, P., Cecconello, M., Cerchier, A., Croci, F., Detti, R., Dimitrova, M. M., Di Pasquale, C., D'Ippolito, M. R., Ditta, S., ... Caruso, R. (2025). Outcomes of a Risk-Stratified Protocol for Preventing Peristomal Skin Complications in Patients with an Ostomy: A Cohort Study. Nursing Reports, 15(5), 179. https://doi.org/10.3390/nursrep15050179









