Patient Participation During Nursing Bedside Handover: A State-of-the-Art Review
Abstract
1. Introduction
2. Background
2.1. Theoretical Framework
2.2. Rationale and Aim of the Study
3. Materials and Methods
3.1. Determination of the Initial Research Question and Field of Inquiry (Stage 1)
3.2. Determination of the Timeframe (Stage 2)
3.3. Finalization of the Research Question to Reflect the Timeframe (Stage 3)
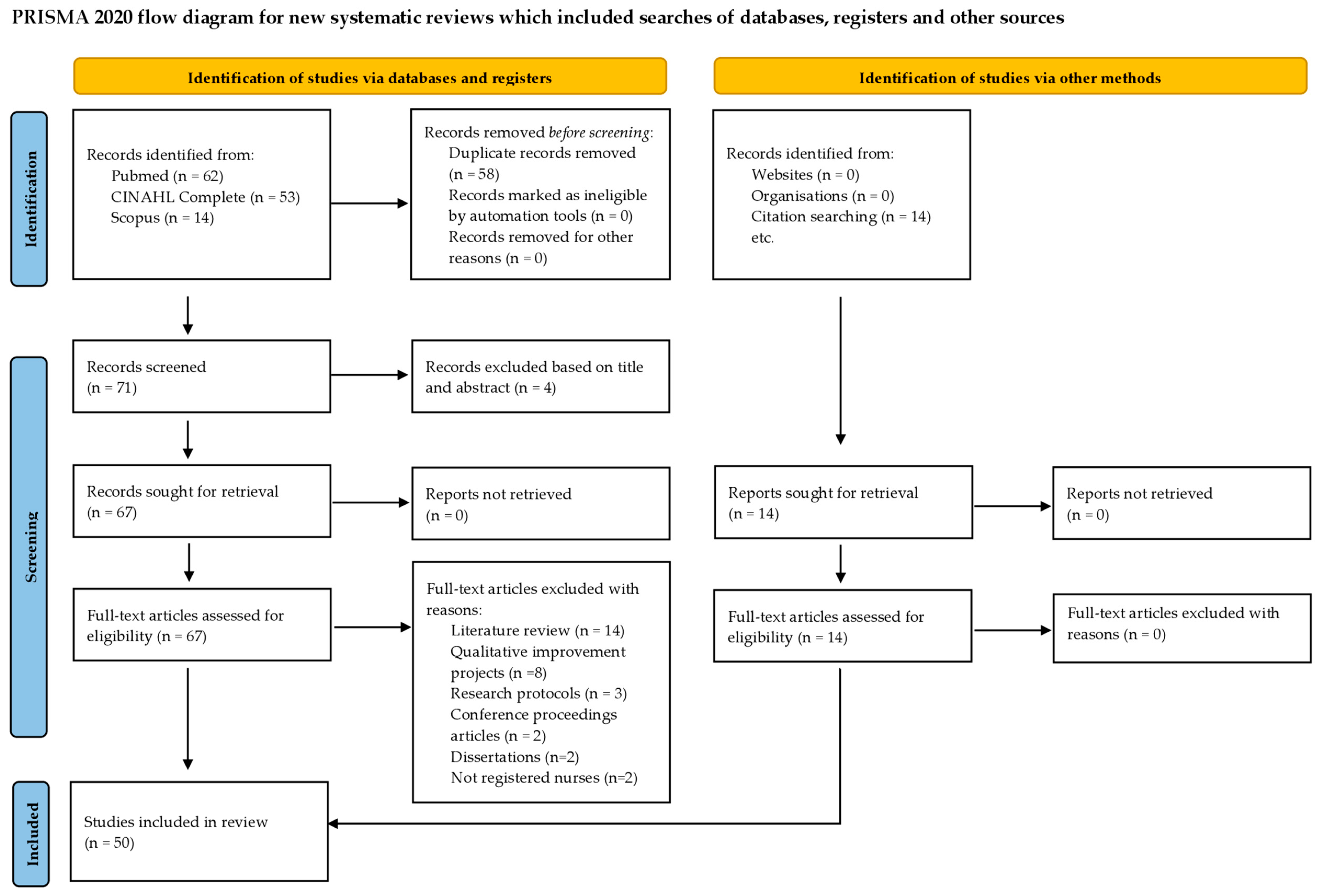
3.4. Development of the Search Strategy to Identify Relevant Articles (Stage 4)
3.5. Analyses (Stage 5)
3.6. Reflexivity (Stage 6)
4. Results
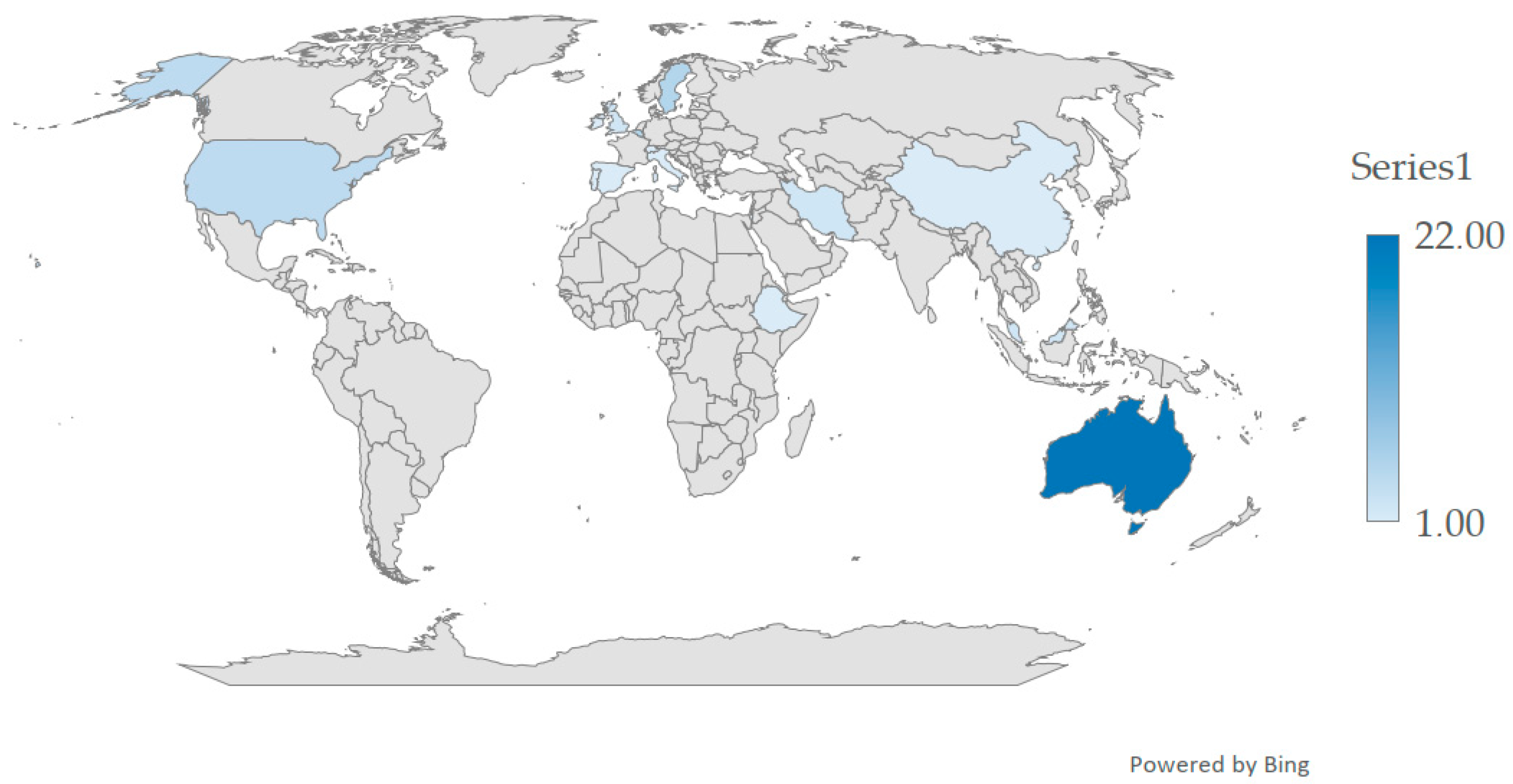
4.1. Studies Characteristics
4.2. Domain of Distinctive Nature and Attributes of Patient Participation During the NBH
4.2.1. Distinctive Nature of Patient Participation
4.2.2. Distinctive Attributes of Patient Participation
4.3. Domain of Nurses’ Practices and Influencing Factors of Patient Participation During the NBH
4.3.1. Nurses’ Practices That Promote and Inhibit Patient Participation
4.3.2. Influencing Factors of Patient Participation
4.4. Domain of Strategies and Impacts of Increasing Patient Participation During the NBH
4.4.1. Strategies for Increasing Patient Participation
4.4.2. Impacts of Increasing Patient Participation
5. Discussion
5.1. Domain of Distinctive Nature and Attributes of Patient Participation During the NBH
5.2. Domain of Nurses’ Practices and Influencing Factors of Patient Participation During the NBH
5.3. Domain of Strategies and Impacts of Increasing Patient Participation During the NBH
5.4. Patient Participation in NBH as a Complex Intervention
5.5. Future Directions in Research
5.6. Study Strengths and Limitations
6. Implications for Comprehensive Care and Health Services
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
Abbreviations
| CINAHL | Cumulative Index to Nursing and Allied Health Literature |
| CROMs | Clinician-Reported Outcomes Measures |
| MAAT | Mixed Methods Appraisal Tools |
| NBH | Nursing Bedside Handover |
| PFPS | Patients for Patient Safety |
| PREMs | Patient-Reported Experience Measures |
| PRISMA | Preferred Reporting Items for Systematic reviews and Meta-Analyses |
| PROMs | Patient-Reported Outcomes measures |
| SANRA | Scale for the Assessment of Narrative Review Articles |
| SotA | State-of-the-art |
| WHO | World Health Organization |
Appendix A
Appendix A.1
| Search Strategy | |
|---|---|
| PubMed | ((“patient participation”[Title/Abstract] OR “patient involvement”[Title/Abstract] OR “patient empowerment”[Title/Abstract] OR “patient engagement”[Title/Abstract] OR “patient-centered”[Title/Abstract]) OR “person-centered”[Title/Abstract])) AND (“bedside handover”[Title/Abstract] OR “bedside handoff”[Title/Abstract] OR “bedside clinical handover”[Title/Abstract] OR “bedside clinical handoff”[Title/Abstract] OR “bedside shift-to-shift handover”[Title/Abstract] OR “bedside shift-to-shift handoff”[Title/Abstract] OR “bedside shift report”[Title/Abstract] OR “Change-of-shift bedside report”[Title/Abstract] OR “change-of-shift bedside handover”[Title/Abstract] OR “change-of-shift bedside handoff”[Title/Abstract] OR “shift report at bedside”[Title/Abstract] OR “bedside sign-in”[Title/Abstract] OR “bedside sign-out”[Title/Abstract] OR “shift report”[Title/Abstract] OR “shift change”[Title/Abstract] OR “nursing handover”[Title/Abstract] OR “nursing handoff”[Title/Abstract])) AND (nurs*[Title/Abstract]) |
| CINAHL Complete | AB (“patient participation” OR “patient involvement” OR “patient empowerment” OR “patient engagement” OR “patient-centered” OR “person-centered”) AND AB (“bedside handover” OR “bedside handoff” OR “bedside clinical handover” OR “bedside clinical handoff” OR “bedside shift-to-shift handover” OR “bedside shift-to-shift handoff” OR “bedside shift report” OR “Change-of-shift bedside report” OR “change-of-shift bedside handover” OR “change-of-shift bedside handoff” OR “shift report at bedside” OR “bedside sign-in” OR “bedside sign-out” OR “shift report” OR “shift change” OR “nursing handover” OR “nursing handoff”) AND AB nurs* |
| Scopus | (ABS (“patient participation” OR “patient involvement” OR “patient empowerment” OR “patient engagement” OR “patient-centered” OR “person-centered”) AND ABS (“bedside handover” OR “bed-side handoff” OR “bedside clinical handover” OR “bedside clinical handoff” OR “bedside shift-two-shift handover” OR “bedside shift-two-shift handoff” OR “bedside shift report” OR “change-off-shift bedside report” OR “change-off-shift bedside handover” OR “change-off-shift bedside handoff” OR “shift report rat bedside” OR “bedside sign-ion” OR “bedside sign-out” OR “shift report” OR “shift change” “nursing handover” OR “nursing handoff”) AND ABS (nursing)) |
Appendix A.2
| SN | Author(s) and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Score |
|---|---|---|---|---|---|---|---|
| 1. | Dumbala et al. [91] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 2. | Yang et al. [93] | Yes | Yes | Yes | Yes | Yes | 10 e |
| 3. | Ghosh et al. [109] | Yes | Yes | Yes | Yes | Yes | 10 c |
| 4. | Abt et al. [78] | Yes | Yes | Yes | Yes | Yes | 10 e |
| 5. | Ghosh et al. [120] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 c |
| 6. | Cruchinho et al. [84] | Yes | Yes | Yes | Yes | Yes | 10 d |
| 7. | Casey et al. [99] | Yes | Yes | Yes | Cannot tell’ | Cannot tell’ | 8 a |
| 8. | Chien et al. [101] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 9. | Van de Velde et al. [76] | Yes | Yes | Cannot tell’ | Cannot tell’ | Cannot tell’ | 7 a |
| 10. | Lantz et al. [83] | Yes | Yes | Cannot tell’ | Cannot tell’ | Yes | 8 b |
| 11. | Yuen et al. [108] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 12. | Paredes-Garza et al. [85] | Yes | Yes | Cannot tell’ | Cannot tell’ | Yes | 8 a |
| 13. | Dahm et al. [104] | Yes | Yes | Yes | Yes | Cannot tell’ | 9 a |
| 14. | Tobiano et al. [100] | Yes | Yes | Yes | Cannot tell’ | Cannot tell’ | 9 d |
| 15. | Neamti et al. [89] | Yes | Yes | Cannot tell’ | Cannot tell’ | Yes | 8 b |
| 16. | Chien et al. [102] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 17. | Street et al. [98] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 18. | Abbaszade et al. [90] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 b |
| 19. | Olasoji et al. [107] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 20. | Mullen et al. [103] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 21. | Chong et al. [92] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 d |
| 22. | Forde et al. [87] | Yes | Yes | Yes | Yes | Yes | 10 c |
| 23. | Wiklund et al. [81] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 24. | Oxelmark et al. [79] | Yes | Yes | Yes | Yes | Yes | 10 d |
| 25. | Malfait et al. [77] | Yes | Yes | Cannot tell’ | Cannot tell’ | Yes | 8 b |
| 26. | Hada et al. [94] | Yes | Yes | Cannot tell’ | Cannot tell’ | Yes | 8 a |
| 27. | Kullberg et al. [82] | Yes | Yes | Yes | Yes | Yes | 10 d |
| 28. | Olasoji et al. [106] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 d |
| 29. | Malfait et al. [74] | Yes | Yes | Cannot tell’ | Cannot tell’ | Yes | 8 b |
| 30. | Benham-Hutchins et al. [115] | Yes | Yes | Cannot tell’ | Cannot tell’ | Cannot tell’ | 6 a |
| 31. | Malfait et al. [75] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 b |
| 32. | Olasoji et al. [105] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 33. | Malfait et al. [73] | Yes | Yes | Yes | Yes | Cannot tell’ | 9 c |
| 34. | Kullberg et al. [80] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 35. | Benham-Hutchins et al. [116] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 36. | Tobiano et al. [95] | Yes | Yes | Cannot tell’ | Cannot tell’ | Yes | 8 a |
| 37. | Scheidenhelm and Reitz [25] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 b |
| 38. | Khuan and Juni [7] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 39. | Witty et al. [96] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 d |
| 40. | Bruton et al. [118] | Yes | Yes | Yes | Yes | Yes | 10 a |
| 41. | Lupieri et al. [86] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 42. | Eggins and Slade [97] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 43. | Drach-Zahavy and Shilman [88] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 c |
| 44. | Lu et al. [110] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 45. | Bradley and Mott [111] | Yes | Cannot tell’ | Yes | Cannot tell’ | Yes | 8 c |
| 46. | San-Jecklin and Sherman [117] | Yes | Yes | Cannot tell’ | Cannot tell’ | Cannot tell’ | 7 b |
| 47. | Johnson and Cowin [112] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 48. | McMurray et al. [113] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 49. | McMurray et al. [114] | Yes | Yes | Yes | Cannot tell’ | Yes | 9 a |
| 50 | Greaves [119] | Cannot tell’ | Yes | Yes | Cannot tell’ | Cannot tell’ | 7 a |
References
- World Health Organization. Patients for Patient Safety. Available online: https://www.who.int/initiatives/patients-for-patient-safety (accessed on 8 March 2025).
- World Health Organization. Strategic Objective 4: Patient and Family Engagement. In Global Patient Safety Action Plan 2021–2030: Towards Eliminating Avoidable Harm in Health Care; WHO: Geneva, Switzerland, 2021; pp. 40–47. [Google Scholar]
- Gomes, P.; Ribeiro, S.; Silva, M.; Cruchinho, P.; Nunes, E.; Nascimento, C.; Lucas, P. Cross-Cultural Validation of the Portuguese Version of the Quality of Oncology Nursing Care Scale. Cancers 2024, 16, 859. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.; Gaspar, F.; Potra, T.; Lucas, P. Translation, Adaptation, and Validation of the Self-Efficacy Scale for Clinical Nurse Leaders for the Portuguese Culture. Int. J. Environ. Res. Public Health 2022, 19, 8590. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Communication During Patient Hand-Overs; World Health Organization: Geneva, Switzerland, 2007; Volume 1. [Google Scholar]
- Cruchinho, P.; Teixeira, G.; Lucas, P.; Gaspar, F. Evaluating the Methodological Approaches of Cross-Cultural Adaptation of the Bedside Handover Attitudes and Behaviours Questionnaire into Portuguese. J. Healthc. Leadersh. 2023, 15, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Khuan, L.; Juni, M.H. Nurses’ Opinions of Patient Involvement in Relation to Patient-Centered Care during Bedside Handovers. Asian Nurs. Res. 2017, 11, 216–222. [Google Scholar] [CrossRef]
- Burston, S.; Chaboyer, W.; Gillespie, B.; Carroll, R. The Effect of a Transforming Care Initiative on Patient Outcomes in Acute Surgical Units: A Time Series Study. J. Adv. Nurs. 2015, 71, 417–429. [Google Scholar] [CrossRef]
- Givens, S.E.; Skully, C.; Bromley, G. Psychiatric Inpatient Bedside Handoff: Implementation of a Quality Improvement Project and Nurses’ Responses. J. Psychosoc. Nurs. Ment. Health Serv. 2016, 54, 33–37. [Google Scholar] [CrossRef]
- Patton, L.J.; Tidwell, J.D.; Falder-Saeed, K.L.; Young, V.B.; Lewis, B.D.; Binder, J.F. Ensuring Safe Transfer of Pediatric Patients: A Quality Improvement Project to Standardize Handoff Communication. J. Pediatr. Nurs. 2017, 34, 44–52. [Google Scholar] [CrossRef]
- Tobiano, G.; Chaboyer, W.; McMurray, A. Family Members’ Perceptions of the Nursing Bedside Handover. J. Clin. Nurs. 2013, 22, 192–200. [Google Scholar] [CrossRef]
- Baldwin, K.M.; Spears, M.J. Improving the Patient Experience and Decreasing Patient Anxiety with Using Bedside Report. Clin. Nurse Spec. 2019, 33, 82–89. [Google Scholar] [CrossRef]
- Campbell, D.; Dontje, K. Implementing Bedside Handoff in the Emergency Department: A Practice Improvement Project. J. Emerg. Nurs. 2019, 45, 149–154. [Google Scholar] [CrossRef]
- Fucik, S. Standardized Bedside Handoff: One Organization’s Journey. J. Pediatr. Nurs. 2019, 44, 133–136. [Google Scholar] [CrossRef]
- Mørk, A.; Krupp, A.; Hankwitz, J.; Malec, A. Using Kotter’s Change Framework to Implement and Sustain Multiple Complementary ICU Initiatives. J. Nurs. Care Qual. 2018, 33, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Elgin, K.W.; Poston, R.D. Optimizing Registered Nurse Bedside Shift Report: Innovative Application of Simulation Methods. J. Nurses Prof. Dev. 2019, 35, E6–E14. [Google Scholar] [CrossRef] [PubMed]
- Spinks, J.; Chaboyer, W.; Bucknall, T.; Tobiano, G.; Whitty, J.A. Patient and Nurse Preferences for Nurse Handover-Using Preferences to Inform Policy: A Discrete Choice Experiment Protocol. BMJ Open 2015, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.; Heisler, S.; Fahey, L.; McGinnis, J.; Whiffen, T.L. Nurse Knowledge Exchangeplus: Human-Centered Implementation for Spread and Sustainability. Jt. Comm. J. Qual. Patient Saf. 2015, 41, 303–312. [Google Scholar] [CrossRef]
- Bressan, V.; Cadorin, L.; Stevanin, S.; Palese, A. Patients Experiences of Bedside Handover: Findings from a Meta-synthesis. Scand. J. Caring Sci. 2019, 33, 556–568. [Google Scholar] [CrossRef]
- Grimshaw, J.; Hatch, D.; Willard, M.; Abraham, S. A Qualitative Study of the Change-of-Shift Report at the Patients’ Bedside. Health Care Manag. 2016, 35, 294–304. [Google Scholar] [CrossRef]
- Mako, T.; Svanäng, P.; Bjerså, K. Patients’ Perceptions of the Meaning of Good Care in Surgical Care: A Grounded Theory Study. BMC Nurs. 2016, 15, 47. [Google Scholar] [CrossRef]
- Tidwell, T.; Edwards, J.; Snider, E.; Lindsey, C.; Reed, A.; Scroggins, I.; Zarski, C.; Brigance, J. A Nursing Pilot Study on Bedside Reporting to Promote Best Practice and Patient/Family-Centered Care. J. Neurosci. Nurs. 2011, 43, E1–E5. [Google Scholar] [CrossRef]
- Tobiano, G.; Bucknall, T.; Sladdin, I.; Whitty, J.A.; Chaboyer, W. Patient Participation in Nursing Bedside Handover: A Systematic Mixed-Methods Review. Int. J. Nurs. Stud. 2018, 77, 243–258. [Google Scholar] [CrossRef]
- Groves, P.S.; Manges, K.A.; Scott-Cawiezell, J. Handing off Safety at the Bedside. Clin. Nurs. Res. 2016, 25, 473–493. [Google Scholar] [CrossRef] [PubMed]
- Scheidenhelm, S.; Reitz, O.E. Hardwiring Bedside Shift Report. JONA J. Nurs. Adm. 2017, 47, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Laws, D.; Amato, S. Incorporating Bedside Reporting into Change-of-Shift Report. Rehabil. Nurs. 2010, 35, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Karmila, R.; Handiyani, H.; Rachmi, S.F. Factors Relating to Nurse Satisfaction with Communication during the Bedside Handover. Enferm. Clin. 2019, 29, 640–647. [Google Scholar] [CrossRef]
- Manges, K.A.; Groves, P.S. Exploring the Hidden Functions of Nursing Bedside Shift Report: A Performance, Ritual, and Sensemaking Opportunity. J. Nurs. Care Qual. 2019, 34, 256–262. [Google Scholar] [CrossRef]
- Boshart, B.; Knowlton, M.; Whichello, R. Reimplementing Bedside Shift Report at a Community Hospital. Nurs. Manag. 2016, 47, 52–55. [Google Scholar] [CrossRef]
- Redley, B.; Waugh, R. Mixed Methods Evaluation of a Quality Improvement and Audit Tool for Nurse-to-Nurse Bedside Clinical Handover in Ward Settings. Appl. Nurs. Res. 2018, 40, 80–89. [Google Scholar] [CrossRef]
- McAllen, E.R.; Stephens, K.; Swanson-Biearman, B.; Kerr, K.; Whiteman, K. Moving Shift Report to the Bedside: An Evidence-Based Quality Improvement Project. Online J. Issues Nurs. 2018, 23, 1–12. [Google Scholar] [CrossRef]
- Miller, K.B.; Hamza, A.; Metersky, K.; Gaffney, D.M. Nursing Transfer of Accountability at the Bedside: Partnering with Patients to Pilot a New Initiative in Ontario Community Hospitals. Patient Exp. J. 2018, 5, 90–96. [Google Scholar] [CrossRef]
- Pacenko, C.d.L.; Figueiredo, K.C.; Nunes, E.; Cruchinho, P.; Lucas, P. Mapping Strategies for Strengthening Safety Culture: A Scoping Review. Healthcare 2024, 12, 1194. [Google Scholar] [CrossRef]
- Maher, A.; Hsu, H.; Ebrahim, M.E.B.M.; Vukasovic, M.; Coggins, A. Implementation of Bedside Handover That Includes Patients or Carers in Hospital Settings: A Systematic Review. J. Eval. Clin. Pract. 2025, 31, e14223. [Google Scholar] [CrossRef]
- Daicampi, C.; Veronese, M.; Cesaro, E. Impact of Bedside Handover on Patient Perceptions and Hospital Organizational Outcomes: A Systematic Review. J. Nurs. Manag. 2025, 2025, 3803491. [Google Scholar] [CrossRef]
- Paredes-Garza, F.; López-Mases, P.; Lázaro, E.; Marín-Maicas, P. Effect of on Patient Safety of Bedside Handoff Performed in Intensive Care Units. Systematic Review. An. Sist. Sanit. Navar. 2022, 45, e0996. [Google Scholar] [CrossRef] [PubMed]
- Clari, M.; Conti, A.; Chiarini, D.; Martin, B.; Dimonte, V.; Campagna, S. Barriers to and Facilitators of Bedside Nursing Handover. J. Nurs. Care Qual. 2021, 36, E51–E58. [Google Scholar] [CrossRef] [PubMed]
- McCloskey, R.M.; Furlong, K.E.; Hansen, L. Patient, Family and Nurse Experiences with Patient Presence during Handovers in Acute Care Hospital Settings: A Systematic Review of Qualitative Evidence. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 754–792. [Google Scholar] [CrossRef] [PubMed]
- Bressan, V.; Cadorin, L.; Pellegrinet, D.; Bulfone, G.; Stevanin, S.; Palese, A. Bedside Shift Handover Implementation Quantitative Evidence: Findings from a Scoping Review. J. Nurs. Manag. 2019, 27, 815–832. [Google Scholar] [CrossRef]
- Forde, M.F.; Coffey, A.; Hegarty, J. The Factors to Be Considered When Evaluating Bedside Handover. J. Nurs. Manag. 2018, 26, 757–768. [Google Scholar] [CrossRef]
- Anshasi, H.; Almayasi, Z.A. Perceptions of Patients and Nurses about Bedside Nursing Handover: A Qualitative Systematic Review and Meta-Synthesis. Nurs. Res. Pract. 2024, 2024, 1–18. [Google Scholar] [CrossRef]
- Anderson, J.; Malone, L.; Shanahan, K.; Manning, J. Nursing Bedside Clinical Handover: An Integrated Review of Issues and Tools. J. Clin. Nurs. 2015, 24, 662–671. [Google Scholar] [CrossRef]
- Chaboyer, W.; McMurray, A.; Wallis, M. Standard Operating Protocol for Implementing Bedside Handover in Nursing; Griffith University: South Brisbane, Australia, 2008. [Google Scholar]
- Van de Velde, E.; Vandewiele, H.; Van Hecke, A.; Eeckloo, K.; Malfait, S. Bedside Handovers in Mental Health Care: An Explorative Review. Arch. Psychiatr. Nurs. 2024, 51, 10–16. [Google Scholar] [CrossRef]
- Tobiano, G.; Jerofke-Owen, T.; Marshall, A.P. Promoting Patient Engagement: A Scoping Review of Actions That Align with the Interactive Care Model. Scand. J. Caring Sci. 2021, 35, 722–741. [Google Scholar] [CrossRef] [PubMed]
- Hada, A.; Coyer, F. Shift-to-shift Nursing Handover Interventions Associated with Improved Inpatient Outcomes—Falls, Pressure Injuries and Medication Administration Errors: An Integrative Review. Nurs. Health Sci. 2021, 23, 337–351. [Google Scholar] [CrossRef] [PubMed]
- Bressan, V.; Mio, M.; Palese, A. Nursing Handovers and Patient Safety: Findings from an Umbrella Review. J. Adv. Nurs. 2020, 76, 927–938. [Google Scholar] [CrossRef] [PubMed]
- Sherman, J.; Sand-Jecklin, K.; Johnson, J. Investigating Bedside Nursing Report: A Synthesis of the Literature. Medsurg Nurs. 2013, 22, 308–312, 318. [Google Scholar]
- Buus, N.; Hoeck, B.; Hamilton, B.E. Nurses’ Shift Reports: A Systematic Literature Search and Critical Review of Qualitative Field Studies. J. Clin. Nurs. 2017, 26, 2891–2906. [Google Scholar] [CrossRef]
- Corry, M.; Clarke, M.; While, A.E.; Lalor, J. Developing Complex Interventions for Nursing: A Critical Review of Key Guidelines. J. Clin. Nurs. 2013, 22, 2366–2386. [Google Scholar] [CrossRef]
- May, C.; Finch, T.; Mair, F.; Ballini, L.; Dowrick, C.; Eccles, M.; Gask, L.; MacFarlane, A.; Murray, E.; Rapley, T.; et al. Understanding the Implementation of Complex Interventions in Health Care: The Normalization Process Model. BMC Health Serv. Res. 2007, 7, 148. [Google Scholar] [CrossRef]
- Tobiano, G.; Bucknall, T.; Sladdin, I.; Whitty, J.A.; Chaboyer, W. Reprint of: Patient Participation in Nursing Bedside Handover: A Systematic Mixed-Methods Review. Int. J. Nurs. Stud. 2019, 97, 63–77. [Google Scholar] [CrossRef]
- Colin, R. Desk-Based Research. In Real World Research; John Wiley & Sons: Hoboken, NJ, USA, 2024; p. 110. [Google Scholar]
- de Chirico, M. Material Driven Design vs. Crise: Material Activism for a Harvest Society. In For Nature/with Nature: New Sustainable Design Scenarios; Gambardella, C., Ed.; Springer: Cham, Switzerland, 2024; pp. 390–391. [Google Scholar]
- Brites, I.S.G.; Silva, L.M.; Barbosa, J.L.V.; Rigo, S.J.; Correia, S.D.; Leithardt, V.R.Q. Machine Learning and IoT Applied to Cardiovascular Diseases Identification through Heart Sounds: A Literature Review. In Information Technology and Systems: Proceedings of ICITS 20222; Rocha, Á., Ferraz, C., Porras, Á.M., Delgado, E.J., Eds.; Springer: Cham, Switzerland, 2021; p. 359. [Google Scholar]
- Buchholz, S.W.; Dickins, K.A. Literature Review and Synthesis Tipology. In Literature Review and Synthesis: A Guide for Nurses and Other Healthcare Professionals; Springer Publishing Company: New York, NY, USA, 2023; p. 51. [Google Scholar]
- Barry, E.S.; Merkebu, J.; Varpio, L. Understanding State-of-the-Art Literature Reviews. J. Grad. Med. Educ. 2022, 14, 659–662. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Barry, E.S.; Merkebu, J.; Varpio, L. How to Conduct a State-of-the-Art Literature Review. J. Grad. Med. Educ. 2022, 14, 663–665. [Google Scholar] [CrossRef] [PubMed]
- Cruchinho, P.; Teixeira, G.; Lucas, P.; Gaspar, F. Influencing Factors of Nurses’ Practice during the Bedside Handover: A Qualitative Evidence Synthesis Protocol. J. Pers. Med. 2023, 13, 267. [Google Scholar] [CrossRef] [PubMed]
- Houser, J. The Sucessful Literature Review. In Nursing Research: Reading, Using, and Creating Evidence; Jones & Bartlett Publishers: Burlington, MA, USA, 2023; p. 111. [Google Scholar]
- Harris, D. Managing the Literature. In Literature Review and Research Design: A Guide to Effective Research Practice; Routledge: Oxon, UK, 2020; p. 93. [Google Scholar]
- Subirana, M.; Solá, I.; Garcia, J.M.; Gich, I.; Urrútia, G. A Nursing Qualitative Systematic Review Required MEDLINE and CINAHL for Study Identification. J. Clin. Epidemiol. 2005, 58, 20–25. [Google Scholar] [CrossRef] [PubMed]
- National Library of Medicine. What Is PubMed? Available online: https://www.nlm.nih.gov/oet/ed/pubmed/mesh/mod00/01-000.html (accessed on 29 March 2025).
- Tobiano, G.; Marshall, A.P.; Chaboyer, W. Comparing Perceptions of Patient Nonparticipation in Nursing Care: A Secondary Analysis. J. Nurs. Scholarsh. 2021, 53, 449–457. [Google Scholar] [CrossRef]
- Schandl, A.; Falk, A.-C.; Frank, C. Patient Participation in the Intensive Care Unit. Intensive Crit. Care Nurs. 2017, 42, 105–109. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan: A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. Mixed Methods Appraisal Tool (MMAT) Version 2018 User Guide; McGill University: Montreal, QC, Canada, 2018. [Google Scholar]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Improving the Content Validity of the Mixed Methods Appraisal Tool: A Modified e-Delphi Study. J. Clin. Epidemiol. 2019, 111, 49–59.e1. [Google Scholar] [CrossRef]
- Souto, R.Q.; Khanassov, V.; Hong, Q.N.; Bush, P.L.; Vedel, I.; Pluye, P. Systematic Mixed Studies Reviews: Updating Results on the Reliability and Efficiency of the Mixed Methods Appraisal Tool. Int. J. Nurs. Stud. 2015, 52, 500–501. [Google Scholar] [CrossRef]
- Kim, H.S. Introduction. In The Essence of Nursing Practice: Philosophy and Perspective; Springer Publishing Company: New York, NY, USA, 2015; p. 11. [Google Scholar]
- Rundio, A.; Scott, L. Leadership and DNP-Educated Nurse Executive. In Role Development for Doctoral Advanced Nursing Practice; Dreher, H.M., Glasgow, M.E.S., Eds.; Spinger Publishing: New York, NY, USA, 2011; p. 247. [Google Scholar]
- Malfait, S.; Van Hecke, A.; Van Biesen, W.; Eeckloo, K. Do Bedside Handovers Reduce Handover Duration? An Observational Study with Implications for Evidence-Based Practice. Worldviews Evid.-Based Nurs. 2018, 15, 432–439. [Google Scholar] [CrossRef]
- Malfait, S.; Eeckloo, K.; Van Biesen, W.; Van Hecke, A. The Effectiveness of Bedside Handovers: A Multilevel, Longitudinal Study of Effects on Nurses and Patients. J. Adv. Nurs. 2019, 75, 1690–1701. [Google Scholar] [CrossRef]
- Malfait, S.; Eeckloo, K.; Van Biesen, W.; Deryckere, M.; Lust, E.; Van Hecke, A. Compliance with a Structured Bedside Handover Protocol: An Observational, Multicentred Study. Int. J. Nurs. Stud. 2018, 84, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Van de Velde, E.; Van Hecke, A.; Eeckloo, K.; Malfait, S. Implementing Bedside Handovers in Mental Health Care: Insights from an Experience-Based Co-Design. Patient Educ. Couns. 2024, 119, 108051. [Google Scholar] [CrossRef] [PubMed]
- Malfait, S.; Van Hecke, A.; Van Biesen, W.; Eeckloo, K. Is Privacy a Problem during Bedside Handovers? A Practice-Oriented Discussion Paper. Nurs. Ethics 2019, 26, 2288–2297. [Google Scholar] [CrossRef] [PubMed]
- Abt, M.; Schneider, P.; Martin, L.; Delmas, P.; Ortoleva Bucher, C. I-PASS-Structured Bedside Nursing Handovers: A Type-1 Effectiveness: Implementation Hybrid Pilot Study. J. Adv. Nurs. 2025; early view. [Google Scholar] [CrossRef]
- Oxelmark, L.; Whitty, J.A.; Ulin, K.; Chaboyer, W.; Oliveira Gonçalves, A.S.; Ringdal, M. Patients Prefer Clinical Handover at the Bedside; Nurses Do Not: Evidence from a Discrete Choice Experiment. Int. J. Nurs. Stud. 2020, 105, 103444. [Google Scholar] [CrossRef]
- Kullberg, A.; Sharp, L.; Dahl, O.; Brandberg, Y.; Bergenmar, M. Nurse Perceptions of Person-Centered Handovers in the Oncological Inpatient Setting: A Qualitative Study. Int. J. Nurs. Stud. 2018, 86, 44–51. [Google Scholar] [CrossRef]
- Wiklund, I.; Sahar, Z.; Papadopolou, M.; Löfgren, M. Parental Experience of Bedside Handover during Childbirth: A Qualitative Interview Study. Sex. Reprod. Healthc. 2020, 24, 100496. [Google Scholar] [CrossRef]
- Kullberg, A.; Sharp, L.; Johansson, H.; Brandberg, Y.; Bergenmar, M. Improved Patient Satisfaction 2 Years after Introducing Person-centred Handover in an Oncological Inpatient Care Setting. J. Clin. Nurs. 2019, 28, 3262–3270. [Google Scholar] [CrossRef]
- Lantz, A.H.; Gunningberg, L.; Eriksson, G.; Eldh, A.C.; Wenemark, M.; Pöder, U. Evaluation of Patient Participation in Relation to the Implementation of a Person-centered Nursing Shift Handover. Worldviews Evid.-Based Nurs. 2023, 20, 330–338. [Google Scholar] [CrossRef]
- Cruchinho, P.; López-Franco, M.; Teixeira, G.; Lucas, P.; Gaspar, F. Translation and Validation for the Portuguese Population of the Bedside Handover Attitudes and Behaviors Questionnaire. Risk Manag. Healthc. Policy 2025, 18, 185–203. [Google Scholar] [CrossRef]
- Paredes-Garza, F.; Lázaro, E.; Vázquez, N. Nursing Bedside Handover in an Intensive Care Unit with a Mixed Structure: Nursing Professionals’ Perception. J. Nurs. Manag. 2022, 30, 4314–4321. [Google Scholar] [CrossRef] [PubMed]
- Lupieri, G.; Creatti, C.; Palese, A. Cardio-Thoracic Surgical Patients’ Experience on Bedside Nursing Handovers: Findings from a Qualitative Study. Intensive Crit. Care Nurs. 2016, 35, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Forde, M.F.; Coffey, A.; Hegarty, J. Bedside Handover at the Change of Nursing Shift: A Mixed-Methods Study. J. Clin. Nurs. 2020, 29, 3731–3742. [Google Scholar] [CrossRef] [PubMed]
- Drach-Zahavy, A.; Shilman, O. Patients’ Participation during a Nursing Handover: The Role of Handover Characteristics and Patients’ Personal Traits. J. Adv. Nurs. 2015, 71, 136–147. [Google Scholar] [CrossRef]
- Nemati, S.M.; Fathi, M.; Nouri, B.; Valiee, S. Effects of an Specific Methodology (I Pass the Baton) on Quality of Handoff Information among Nurses: A Comparative Study. J. Healthc. Qual. Res. 2022, 37, 268–274. [Google Scholar] [CrossRef]
- Abbaszade, A.; Assarroudi, A.; Armat, M.R.; Stewart, J.J.; Rakhshani, M.H.; Sefidi, N.; Sahebkar, M. Evaluation of the Impact of Handoff Based on the SBAR Technique on Quality of Nursing Care. J. Nurs. Care Qual. 2021, 36, E38–E43. [Google Scholar] [CrossRef]
- Dumbala, G.; Belay, Y.; Yimam, E.; Abebe, Y. Clinical Handover Experience among Nurses Working in Ethiopia: Phenomenological Qualitative Study. BMC Nurs. 2025, 24, 540. [Google Scholar] [CrossRef]
- Chong, D.W.Q.; Iqbal, A.R.; Kaur Jaj, B.; Zainab, A.; Nordin, A.; Abd Majid, N.D.; Jusoh, A. Perceptions of Nurses on Inter-Shift Handover: A Descriptive Study in Hospital Kuala Lumpur, Malaysia. Med. J. Malays. 2020, 75, 691–697. [Google Scholar]
- Yang, H.; Li, Z.; Feng, A.; Li, S.; Xu, L. A Pilot Study on the Application of ISOBAR Combined with Case Teaching Method in Pediatric Resident Nurses’ Clinical Handover. BMC Med. Educ. 2025, 25, 547. [Google Scholar] [CrossRef]
- Hada, A.; Jack, L.; Coyer, F. Using a Knowledge Translation Framework to Identify Barriers and Supports to Effective Nursing Handover: A Focus Group Study. Heliyon 2019, 5, e01960. [Google Scholar] [CrossRef]
- Tobiano, G.; Whitty, J.A.; Bucknall, T.; Chaboyer, W. Nurses’ Perceived Barriers to Bedside Handover and Their Implication for Clinical Practice. Worldviews Evid.-Based Nurs. 2017, 14, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Whitty, J.A.; Spinks, J.; Bucknall, T.; Tobiano, G.; Chaboyer, W. Patient and Nurse Preferences for Implementation of Bedside Handover: Do They Agree? Findings from a Discrete Choice Experiment. Health Expect. 2017, 20, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Eggins, S.; Slade, D. Contrasting Discourse Styles and Barriers to Patient Participation in Bedside Nursing Handovers. Commun. Med. 2017, 13, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Street, M.; Dempster, J.; Berry, D.; Gray, E.; Mapes, J.; Liskaser, R.; Papageorgiou, S.; Considine, J. Enhancing Active Patient Participation in Nursing Handover: A Mixed Methods Study. J. Clin. Nurs. 2022, 31, 1016–1029. [Google Scholar] [CrossRef]
- Casey, P.; Yuen, E.; Liskaser, R.; Blencowe, P.; Boyd, L.; Abdelrazek, M.; Wang, Z.; Considine, J. Utility of a Digital App to Enhance Patient-Nurse Communications and Patient Involvement in Bedside Handover: Patient and Nurse Perceptions. Aust. Health Rev. 2024, 48, 673–681. [Google Scholar] [CrossRef]
- Tobiano, G.; Marshall, A.P.; Gardiner, T.; Jenkinson, K.; Shapiro, M.; Ireland, M. Development and Psychometric Testing of the Patient Participation in Bedside Handover Survey. Health Expect. 2022, 25, 2492–2502. [Google Scholar] [CrossRef]
- Chien, L.J.; Slade, D.; Goncharov, L.; Taylor, J.; Dahm, M.R.; Brady, B.; McMahon, J.; Raine, S.E.; Thornton, A. Implementing a Ward-level Intervention to Improve Nursing Handover Communication with a Focus on Bedside Handover: A Qualitative Study. J. Clin. Nurs. 2024, 33, 2688–2706. [Google Scholar] [CrossRef]
- Chien, L.J.; Slade, D.; Dahm, M.R.; Brady, B.; Roberts, E.; Goncharov, L.; Taylor, J.; Eggins, S.; Thornton, A. Improving Patient-centred Care through a Tailored Intervention Addressing Nursing Clinical Handover Communication in Its Organizational and Cultural Context. J. Adv. Nurs. 2022, 78, 1413–1430. [Google Scholar] [CrossRef]
- Mullen, A.; Harman, K.; Flanagan, K.; O’Brien, B.; Isobel, S. Involving Mental Health Consumers in Nursing Handover: A Qualitative Study of Nursing Views of the Practice and Its Implementation. Int. J. Ment. Health Nurs. 2020, 29, 1157–1167. [Google Scholar] [CrossRef]
- Dahm, M.R.; Slade, D.; Brady, B.; Goncharov, L.; Chien, L. Tracing Interpersonal Discursive Features in Australian Nursing Bedside Handovers: Approachability Features, Patient Engagement and Insights for ESP Training and Working with Internationally Trained Nurses. Engl. Specif. Purp. 2022, 66, 17–32. [Google Scholar] [CrossRef]
- Olasoji, M.; Plummer, V.; Reed, F.; Jacob, S.; Shaw, L.; Shanti, M.; Cross, W. Views of Mental Health Consumers about Being Involved in Nursing Handover on Acute Inpatient Units. Int. J. Ment. Health Nurs. 2018, 27, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Olasoji, M.; Cross, W.; Reed, F.; Wang, W.; Jacob, S.; Plummer, V. Mental Health Nurses’ Attitudes towards Consumer Involvement in Nursing Handover Pre and Post an Educational Implementation. Int. J. Ment. Health Nurs. 2019, 28, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Olasoji, M.; Plummer, V.; Shanti, M.; Reed, F.; Cross, W. The Benefits of Consumer Involvement in Nursing Handover on Acute Inpatient Unit: Post-implementation Views. Int. J. Ment. Health Nurs. 2020, 29, 786–795. [Google Scholar] [CrossRef] [PubMed]
- Yuen, E.Y.N.; Street, M.; Abdelrazek, M.; Blencowe, P.; Etienne, G.; Liskaser, R.; Choudhary, N.; Considine, J. Evaluating the Efficacy of a Digital App to Enhance Patient-centred Nursing Handover: A Simulation Study. J. Clin. Nurs. 2023, 32, 7626–7637. [Google Scholar] [CrossRef]
- Ghosh, M.; Nosaka, K.; Saunders, R.; Gallagher, O.; Towell-Barnard, A.; Ghosh, D.; Gent, L.; Coventry, L. Patient Perception of Involvement in Nursing Bedside Handover: A Cross-sectional Study. J. Adv. Nurs. 2025, 81, 8666–8689. [Google Scholar] [CrossRef]
- Lu, S.; Kerr, D.; Mckinlay, L. Bedside Nursing Handover: Patients’ Opinions. Int. J. Nurs. Pract. 2014, 20, 451–459. [Google Scholar] [CrossRef]
- Bradley, S.; Mott, S. Adopting a Patient-Centred Approach: An Investigation into the Introduction of Bedside Handover to Three Rural Hospitals. J. Clin. Nurs. 2014, 23, 1927–1936. [Google Scholar] [CrossRef]
- Johnson, M.; Cowin, L.S. Nurses Discuss Bedside Handover and Using Written Handover Sheets. J. Nurs. Manag. 2013, 21, 121–129. [Google Scholar] [CrossRef]
- McMurray, A.; Chaboyer, W.; Wallis, M.; Johnson, J.; Gehrke, T. Patients’ Perspectives of Bedside Nursing Handover. Collegian 2011, 18, 19–26. [Google Scholar] [CrossRef]
- McMurray, A.; Chaboyer, W.; Wallis, M.; Fetherston, C. Implementing Bedside Handover: Strategies for Change Management. J. Clin. Nurs. 2010, 19, 2580–2589. [Google Scholar] [CrossRef]
- Benham-Hutchins, M.; Brown, S.A.; Donovan, E.E.; Guevara, H.; Johnson, A.H. Spanish-Speaking Hispanic Patients’ Information-Sharing Preferences during Hospitalization: An Exploratory Pilot Study. J. Particip. Med. 2018, 10, e10782. [Google Scholar] [CrossRef] [PubMed]
- Benham-Hutchins, M.; Staggers, N.; Mackert, M.; Johnson, A.H.; DeBronkart, D. “I Want to Know Everything”: A Qualitative Study of Perspectives from Patients with Chronic Diseases on Sharing Health Information during Hospitalization. BMC Health Serv. Res. 2017, 17, 529. [Google Scholar] [CrossRef] [PubMed]
- Sand-Jecklin, K.; Sherman, J. Incorporating Bedside Report into Nursing Handoff: Evaluation of Change in Practice. J. Nurs. Care Qual. 2013, 28, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Bruton, J.; Norton, C.; Smyth, N.; Ward, H.; Day, S. Nurse Handover: Patient and Staff Experiences. Br. J. Nurs. 2016, 25, 386–393. [Google Scholar] [CrossRef]
- Greaves, C. Patients’ Perceptions of Bedside Handover. Nurs. Stand. 1999, 14, 32–35. [Google Scholar] [CrossRef]
- Ghosh, M.; O’Connell, B.; Nguyen, H.T.; Coventry, L.; Towell-Barnard, A.; Gallagher, O.; Gullick, K.; Gent, L.; Saunders, R. Patient and Family Involvement in Nursing Bedside Handover: A Qualitative Descriptive Study of Consumer Perceptions of Nursing Care. Nurs. Reports 2025, 15, 51. [Google Scholar] [CrossRef]
- Chen, C. Knowledge Domains Analysis. In Turning Points: The Nature of Creativity; Springer: Philadelfia, PA, USA, 2011; p. 139. [Google Scholar]
- Slade, D.; Murray, K.A.; Pun, J.K.H.; Eggins, S. Nurses’ Perceptions of Mandatory Bedside Clinical Handovers: An Australian Hospital Study. J. Nurs. Manag. 2019, 27, 161–171. [Google Scholar] [CrossRef]
- Pun, J. Using a Simulation-Based Approach to Promote Structured and Interactive Nursing Clinical Handover: A Pre- and Post-Evaluation Pilot Study in Bilingual Hong Kong. BMC Nurs. 2023, 22, 38. [Google Scholar] [CrossRef]
- Pun, J.; Chan, E.A.; Man, M.; Eggins, S.; Slade, D. Pre- and Post Evaluations of the Effects of the Connect, Ask, Respond and Empathise (CARE) Protocol on Nursing Handover: A Case Study of a Bilingual Hospital in Hong Kong. J. Clin. Nurs. 2019, 28, 3001–3011. [Google Scholar] [CrossRef]
- Slade, D.; Pun, J.; Murray, K.A.; Eggins, S. Benefits of Health Care Communication Training for Nurses Conducting Bedside Handovers: An Australian Hospital Case Study. J. Contin. Educ. Nurs. 2018, 49, 329–336. [Google Scholar] [CrossRef]
- Arruum, D.; Setyowati, S.; Novieastari, E.; Hamid, A.Y.S. Nursing Theories as the Basis for the Handover Development: A Systematic Review. Enfermería Clínica 2021, 31, 576–579. [Google Scholar] [CrossRef]
- Avalos, J.; Roy, D.; Asan, O.; Zhang, Y. The Influential Factors on Nurses’ Situation Awareness in Inpatient Settings: A Literature Review. Hum. Factors Healthc. 2021, 1, 100006. [Google Scholar] [CrossRef]
- O’keefe, W.S.; Schimdt, L.L.; Hamamek, L.P.; Castro, D.; Pickering, S.P. Defining Situation Awareness. In A Pratical Guide to Crew Resource Management for Healthcare Teams; Cambridge Scholars Publishing: Newcastle, UK, 2022; p. 23. [Google Scholar]
- Stanton, N.A.; Stewart, R.; Harris, D.; Houghton, R.J.; Baber, C.; McMaster, R.; Salmon, P.; Hoyle, G.; Walker, G.; Young, M.S.; et al. Distributed Situation Awareness in Dynamic Systems: Theoretical Development and Application of an Ergonomics Methodology. Ergonomics 2006, 49, 1288–1311. [Google Scholar] [CrossRef]
- Clark, J.R.; Stanton, N.A.; Revell, K.M.A. Review of Handover Tools and Tecniques in High-Risk Shift Work Domains. In Human–Automation Interaction Design: Developing a Vehicle Automation Assistant; CRC Press: Boca Raton, FL, USA, 2022; pp. 37–56. [Google Scholar]
- Fore, A.M.; Sculli, G.L. A Concept Analysis of Situational Awareness in Nursing. J. Adv. Nurs. 2013, 69, 2613–2621. [Google Scholar] [CrossRef]
- Sitterding, M.C.; Broome, M.E.; Everett, L.Q.; Ebright, P. Understanding Situation Awareness in Nursing Work. Adv. Nurs. Sci. 2012, 35, 77–92. [Google Scholar] [CrossRef]
- Eisenberg, E.M. The Social Construction of Healthcare Teams. In Improving Healthcare Team Communication: Building on Lessons from Aviation and Aerospace; Nemeth, C.P., Ed.; Ashgate: Hampshire, UK, 2008; p. 16. [Google Scholar]
- Kalisch, B.J.; Landstrom, G.L.; Hinshaw, A.S. Missed Nursing Care: A Concept Analysis. J. Adv. Nurs. 2009, 65, 1509–1517. [Google Scholar] [CrossRef]
- Pezzolesi, C.; Manser, T.; Schifano, F.Z.; Kostrzewski, A.; Pickles, J.; Nicholls, H.; Fishman, D.; Arshad, M.; Dhillon, S. Does Clinical Handover Promote Situation Awareness? Implications for Person-Centered Healthcare. Int. J. Pers. Cent. Med. 2012, 2, 294–300. [Google Scholar]
- O’keefe, W.S.; Schimdt, L.L.; Hamamek, L.P.; Castro, D.; Pickering, S.P. Exchancing Information during Handovers. In A Pratical Guide to Crew Resource Management for Healthcare Teams; Cambridge Scholars Publishing: Newcastle, UK, 2022; pp. 51–61. [Google Scholar]
- Orasanu, J.; Fisher, U. Improving Healthcare Communication: Lessons from the Flightdeck. In Improving Healthcare Team Communication: Building on Lessons from Aviation and Aerospace; Nemeth, C.P., Ed.; CRC Press: Boca Raton, FL, USA, 2008; p. 32. [Google Scholar]
- Galatzan, B.J.; Carrington, J.M. Communicating Data, Information, and Knowledge in the Nursing Handoff. CIN Comput. Inform. Nurs. 2021, 40, 21–27. [Google Scholar] [CrossRef]
- Riegel, B.; Jaarsma, T.; Lee, C.S.; Strömberg, A. Integrating Symptoms Into the Middle-Range Theory of Self-Care of Chronic Illness. Adv. Nurs. Sci. 2019, 42, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Riegel, B.; Jaarsma, T.; Strömberg, A. A Middle-Range Theory of Self-Care of Chronic Illness. Adv. Nurs. Sci. 2012, 35, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Baird, M.; Bristow, S.; Moses, A. Self-Management and Empowerment. In Chronic Care Nursing: A Framework for Practice; Deravin-Malone, L., Anderson, J., Eds.; Cambridge University Press: Cambridge, UK, 2016; pp. 80–97. [Google Scholar]
- Pollack, A.H.; Mishra, S.R.; Apodaca, C.; Khelifi, M.; Haldar, S.; Pratt, W. Different Roles with Different Goals: Designing to Support Shared Situational Awareness between Patients and Clinicians in the Hospital. J. Am. Med. Inform. Assoc. 2021, 28, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Nagels, M.; Abel, M.-H.; Tali, F. Focus on the Agency of Learners to Innovate in Pedagogy. In The Future of Innovation and Technology in Education: Policies and Practices for Teaching and Learning Excellence; Visvizi, A., Lytras, M.D., Linda, D., Eds.; Esmerald Publishing: Bingley, UK, 2019; p. 30. [Google Scholar]
- Poitras, M.-E.; Chouinard, M.-C.; Gallagher, F.; Fortin, M. Nursing Activities for Patients with Chronic Disease in Primary Care Settings. Nurs. Res. 2018, 67, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Giddens, J.F. Concept-Based Instruction for the Classroom. In Mastering Concept-Based Teaching and Competency Assessment: A Guide for Nurse Educators; Elsevier: Columbia, MO, USA, 2024; p. 109. [Google Scholar]
- de Lange, S.; Heyns, T.; Filmalter, C. A Concept Analysis of Person-Centred Handover Practices: The Meaning in Emergency Departments. Int. Emerg. Nurs. 2024, 74, 101446. [Google Scholar] [CrossRef] [PubMed]
- Schuster, P.M.; Nycolyn, L. Communication and Patient Safety: Understanding the Connection. In Communication for Nurses: How to Prevent Harmful Events and Promote Patient Safety; F.A. Davis Company: Philadelfia, PA, USA, 2010; pp. 3–10. [Google Scholar]
- Bårdsgjerde, E.K.; Kvangarsnes, M.; Landstad, B.J.; Hole, T.; Magne, N. A Comprehensive Model for Patient Participation. In Towards Sustainable Good Health and Well-Being The Role of Health Literacy; Hole, T., Kvangarsnes, M., Landstad, B.J., Bårdsgjerde, E.K., Magne, N., Tippett-Spirto, S.E., Eds.; Springer: Cham, Switzerland, 2025. [Google Scholar]
- Bårdsgjerde, E.K.; Landstad, B.J.; Hole, T.; Nylenna, M.; Gjeilo, K.H.; Kvangarsnes, M. Nurses’ Perceptions of Patient Participation in the Myocardial Infarction Pathway. Nurs. Open 2020, 7, 1606–1615. [Google Scholar] [CrossRef]
- Thompson, A.G.H. The Meaning of Patient Involvement and Participation in Health Care Consultations: A Taxonomy. Soc. Sci. Med. 2007, 64, 1297–1310. [Google Scholar] [CrossRef]
- American Nurses Association. Code of Ethics for Nurses: With Interpretative Statements; American Nurses Association: Silver Spring, MD, USA, 2015. [Google Scholar]
- International Council of Nurses. The ICN Code of Ethics for Nurses: Revised 2021; International Council of Nurses: Geneva, Switzerland, 2021; ISBN 978-92-95099-94-4. [Google Scholar]
- Inkeroinen, S.; Virtanen, H.; Stolt, M.; Leino-Kilpi, H. Patients’ Right to Know: A Scoping Review. J. Clin. Nurs. 2023, 32, 4311–4324. [Google Scholar] [CrossRef]
- Waldron, J. Participation: The Right of Rights. Proc. Aristot. Soc. 1998, 98, 307–337. [Google Scholar] [CrossRef]
- Sidani, S. Phases of Intervention Evaluation Research. In Health Intervention Research: Understanding Research Design and Methods; Sage Publications: London, UK, 2015; p. 36. [Google Scholar]
- Kim, H.S. Conceptual Domains in Practice: A Framework for Theoretical Analysis. In The Nature Theoretical Thinking on Nursing; Springer Publishing Company: New York, NY, USA, 2010; pp. 73–74. [Google Scholar]
- Sun, L.; Liu, H.; Tan, M. Clinical Handover at the Bedside: An Evidence-Based Quality Implementation Project. Int. J. Evid. Based. Healthc. 2016, 14, 186–187. [Google Scholar] [CrossRef]
- Sidani, S.; Braden, C.J. Overview of Designing Interventions. In Design, Evaluation, and Translation of Nursing Interventions; Wiley: Oxford, UK, 2011; pp. 21–22, 25. ISBN 9780813820323. [Google Scholar]
- Alrajhi, A.; Sormunen, T.; Alsubhi, H. Factors Affecting Bedside Handover between Nurses in Critical Care Area. J. Nurs. Health. Sci. 2018, 7, 53–64. [Google Scholar]
- Malfait, S.; Eeckloo, K.; Van Biesen, W.; Van Hecke, A. Barriers and Facilitators for the Use of Nursing Bedside Handovers: Implications for Evidence-based Practice. Worldviews Evid.-Based Nurs. 2019, 16, 289–298. [Google Scholar] [CrossRef]
- Cho, S.; Lee, J.L.; Kim, K.S.; Kim, E.M. Systematic Review of Quality Improvement Projects Related to Intershift Nursing Handover. J. Nurs. Care Qual. 2022, 37, E8–E14. [Google Scholar] [CrossRef] [PubMed]
- Costa, D. Cross-Cutting Patient Safety Topics/Practices. In Making Healthcare Safer III: A Critical Analysis of Existing and Emerging Patient Safety Practices; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2020; pp. 17–83. [Google Scholar]
- American Academy of Pediatrics; American College of Emergency Physicians. Emergency Nurses Association Handoffs: Transitions of Care for Children in the Emergency Department. Pediatrics 2016, 138, e20162680. [Google Scholar] [CrossRef]
- Sorensen, L.J.; Stanton, N.A. Keeping It Together: The Role of Transactional Situation Awareness in Team Performance. Int. J. Ind. Ergon. 2016, 53, 267–273. [Google Scholar] [CrossRef]
- Webster, K.L.W.; Keebler, J.R.; Chaparro, A.; Greilich, P.; Fagerlund, A.; Lazzara, E.H. Handoffs and Teamwork: A Framework for Care Transition Communication. Jt. Comm. J. Qual. Patient Saf. 2022, 48, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Riesenberg, L.A. Shift-to-Shift Handoff Research: Where Do We Go from Here? J. Grad. Med. Educ. 2012, 4, 4–8. [Google Scholar] [CrossRef]
- Thomas, L.; Donohue-Porter, P. Blending Evidence and Innovation: Improving Intershift Handoffs in a Multihospital Setting. J. Nurs. Care Qual. 2012, 27, 116–124. [Google Scholar] [CrossRef]
- Street, M.; Eustace, P.; Livingston, P.M.; Craike, M.J.; Kent, B.; Patterson, D. Communication at the Bedside to Enhance Patient Care: A Survey of Nurses’ Experience and Perspective of Handover. Int. J. Nurs. Pract. 2011, 17, 133–140. [Google Scholar] [CrossRef]
- Moyo, P.; Anderson, J.; Francis, K.; Biles, J. Exploring the Experiences and Perceptions of the Utilisation of Structured Clinical Handover Frameworks by Nurses Working in Acute Care Settings: A Scoping Review. J. Clin. Nurs. 2024, 33, 4297–4313. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Pocket Guide TeamSTEPPS® 2.0: Team Strategies & Tools to Enhance Performance and Patient Safety; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2013. [Google Scholar]
- Brown-Deveaux, D.; Kaplan, S.; Gabbe, L.; Mansfield, L. Transformational Leadership Meets Innovative Strategy: How Nurse Leaders and Clinical Nurses Redesigned Bedside Handover to Improve Nursing Practice. Nurse Lead. 2022, 20, 290–296. [Google Scholar] [CrossRef]
- Eggins, S.; Slade, D. Resource: Communicating Effectively in Bedside Nursing Handovers. In Effective Communication in Clinical Handover: From Research to Practice; Eggins, S., Slade, D., Geddes, F., Eds.; De Gruyter: Sidney, Australia, 2016; pp. 115–125. [Google Scholar]
- de Lange, S.; Heyns, T.; Filmalter, C. Clinical Practice Guidelines for Person-Centred Handover Practices in Emergency Departments: A Scoping Review. BMJ Open 2024, 14, e082677. [Google Scholar] [CrossRef]
- Gregory, S.; Tan, D.; Tilrico, M.; Edwardson, N.; Gamm, L. Bedside Shift Reports: What Does the Evidence Say? J. Nurs. Adm. 2014, 44, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Sidani, S.; Braden, C.J. Overview of Interventions. In Nursing and Health Interventions: Design, Evaluation and Implementation; Wiley-Blackwell: Hoboken, NJ, USA, 2021; pp. 20–27. [Google Scholar]
- Kelly, T. Glossary. In Electronic Health Records for Quality Nursing & Health Care; DEStech publications: Lancaster, PA, USA, 2016; p. 439. [Google Scholar]
- Lorenzi, N.M. Introduction. In Transforming Health Care Through Information; Lorenzy, N.M., Ash, J.S., Einbinder, J., McPhee, W., Einbinder, L., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; p. 17. [Google Scholar]
- Kodama, Y.; Fukahori, H. Nurse Managers’ Attributes to Promote Change in Their Wards: A Qualitative Study. Nurs. Open 2017, 4, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.; Fischer, S.; Walpola, R.L.; Chauhan, A.; Babalola, T.; Mears, S.; Le-Dao, H. Where Do Models for Change Management, Improvement and Implementation Meet? A Systematic Review of the Applications of Change Management Models in Healthcare. J. Healthc. Leadersh. 2021, 13, 85–108. [Google Scholar] [CrossRef] [PubMed]
- American Nurses Association. Scope of Practice of Nursing Administration. In Nursing Administration: Scope and Standards of Practice; American Nurses Association: Silver Spring, MD, USA, 2016; pp. 1–3. [Google Scholar]
- Storm, M.; Coulter, A. Patient-Centred Care in the Nordic Countries. In Researching Patient Safety and Quality in Healthcare: A Nordic Perpective; Aase, K., Schibevaag, L., Eds.; CRC Press: New York, NY, USA, 2017; pp. 27–42. [Google Scholar]
- Organisation for Economic Co-operation and Development. Measuring What Matters: The Patient-Reported Indicator Surveys: Patient-Reported Indicators for Assessing Health System Performance; OECD: Paris, France, 2019. [Google Scholar]
- Benson, T. Why PROMS and PREMs Matter. In Patient-Reported Outcomes and Experience: Measuring What We Want; Springer: Cham, Switzerland, 2022; p. 7. [Google Scholar]
- Cappelleri, J.C.; Zou, K.H.; Bushmakin, A.G.; Alvir, J.M.J.; Alemayehu, D.; Symonds, T. Introduction. In Patient-Reported Outcomes: Measurement, Implementation and Interpretation; CRC Press: New York, NY, USA, 2014; pp. 1–20. [Google Scholar]
- EIT Health. Implementing Value-Based Healthcare in Europe: Handbook for Pioneers; EIT Health: Munich, Germany, 2020. [Google Scholar]
- Petersson, I.F.; Grahn, B.; Stigmar, K. Clinician-Reported Outcomes Measures:Experiences from Multicenter Follow-up and an Overview o Commonly Used Measures in Vocational Rehabilitation and Disability Evaluation. In Handbook of Vocational Rehabilitation and Disability Evaluation: Aplication and Implementation of ICF; Escorpizo, R., Brage, S., Hima, D., Stucki, G., Eds.; Springer: Berlin/Heidelberg, Germany, 2014; p. 455. [Google Scholar]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process Evaluation of Complex Interventions: Medical Research Council Guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef]
- Effective Practice and Organisation of Care. Patient-Mediated Interventions. In EPOC Taxonomy; Effective Practice and Organisation of Care: London, UK, 2015; p. 11. [Google Scholar]
- Tobiano, G.; Latimer, S.; Manias, E.; Marshall, A.P.; Rattray, M.; Jenkinson, K.; Teasdale, T.; Wren, K.; Chaboyer, W. Co-Design of an Intervention to Improve Patient Participation in Discharge Medication Communication. Int. J. Qual. Health. Care 2024, 36, mzae013. [Google Scholar] [CrossRef]
- Slattery, P.; Saeri, A.K.; Bragge, P. Research Co-Design in Health: A Rapid Overview of Reviews. Health Res. Policy Syst. 2020, 18, 17. [Google Scholar] [CrossRef]
- Bombard, Y.; Baker, G.R.; Orlando, E.; Fancott, C.; Bhatia, P.; Casalino, S.; Onate, K.; Denis, J.-L.; Pomey, M.-P. Engaging Patients to Improve Quality of Care: A Systematic Review. Implement. Sci. 2018, 13, 98. [Google Scholar] [CrossRef]
- Castro, E.M.; Malfait, S.; Van Regenmortel, T.; Van Hecke, A.; Sermeus, W.; Vanhaecht, K. Co-Design for Implementing Patient Participation in Hospital Services: A Discussion Paper. Patient Educ. Couns. 2018, 101, 1302–1305. [Google Scholar] [CrossRef]
- Van Citters, A. Experience-Based Co-Design of Health Care Services; Institute for Healthcare Improvement: Cambridge, MA, USA, 2017. [Google Scholar]
- Bay, B.; Benveniste, S.; Beuscart-Zephir, M.-C.; Duclos, A.; Janalhiac, M.-P.; Jégau, G.; Lewkowicz, M.; Pingaud, H.; Vigouroux, N. Co-Design: Methodologies and Future Use. In Co-Design in Living Labs for Healthcare and Independent Living: Concepts, Methods and Tools; Picard, R., Ed.; Wiley: London, UK, 2017; p. 57. [Google Scholar]
- Bonaconsa, C.; van den Bergh, D.; Charani, E.; Phillips, T.; Spogter, A.; Mohamed, A.; Peters, D.; Joubert, I.; Mendelson, M. Co-Design of a Nurse Handover Tool to Optimise Infection Control and Antimicrobial Stewardship in a Low Resource Setting Intensive Care Unit: A Nurse Led Collaboration. Wellcome Open Res. 2024, 9, 583. [Google Scholar] [CrossRef]
- Farrington, C.J. Co-Designing Healthcare Systems: Between Transformation and Tokenism. J. R. Soc. Med. 2016, 109, 368–371. [Google Scholar] [CrossRef]
- Davies, K.; Khrog, C.; Buykx, P. Authentic Co-Design in Social Work Research: Principles and Practices. In Handbook of Research Methods in Social Work; Alston, M., Buykx, P., Foote, W., Betts, D., Eds.; Edward Elgar: Cheltenham, UK, 2025; pp. 218–219. [Google Scholar]
- Yusrawati; Kamil, H.; Tahlil, T. The Effectiveness of Bedside Handover Training to Improve Knowledge, Attitudes, and Skills among Nurses. Enfermería Clínica 2022, 32, S11–S14. [Google Scholar] [CrossRef]
- Choi, J.Y.; Byun, M.; Kim, E.J. Educational Interventions for Improving Nursing Shift Handovers: A Systematic Review. Nurse Educ. Pract. 2024, 74, 103846. [Google Scholar] [CrossRef] [PubMed]
- Chapman, H.M. Maintaining a Safe Environment. In Applying the Roper-Logan-Tierney Model in Practice, 3rd ed.; Holland, K., Jenkins, J., Eds.; Elsevier: Edimburg, UK, 2019; p. 71. [Google Scholar]
- López-Domingo, B.; Rodríguez-Martín, B. Factors Associated with the Provision of Individualized Care during Hospitalization: A Systematic Review. J. Nurs. Manag. 2021, 29, 113–132. [Google Scholar] [CrossRef]
- Yan, L.; Liu, L.; Wang, F.; Zhao, F.; Hu, X. Barriers and Facilitators to Feeling Safe for Inpatients: A Model Based on a Qualitative Meta-Synthesis. Front. Public Health. 2024, 12, 1308258. [Google Scholar] [CrossRef]
- Whittam, S. Maintaining a Safe Environment. In Applying the Roper-Logan-Tierney Model in Practice, 2nd ed.; Holland, K., Jenkins, J., Solom, J., Whittam, S., Eds.; Churchill Livingstone Elsevier: Philadelfia, PA, USA, 2008; p. 46. [Google Scholar]
- Hannawa, A.F. SACCIA Safe Communication: Five Core Competencies for Safe and High-Quality Care. J. Patient Saf. Risk Manag. 2018, 23, 99–107. [Google Scholar] [CrossRef]
- White-Trevino, K.; Dearmon, V. Transitioning Nurse Handoff to the Bedside: Engaging Staff and Patients. Nurs. Adm. Q. 2018, 42, 261–268. [Google Scholar] [CrossRef]
- Smeulers, M.; Vermeulen, H. Best of Both Worlds: Combining Evidence with Local Context to Develop a Nursing Shift Handover Blueprint. Int. J. Qual. Health Care 2016, 28, 749–757. [Google Scholar] [CrossRef]
- Ferlie, E.B. Organizational Interventions. In Knowledge Translation in Health Care:Moving from Evidence to Practice; Straus, S.E., Tetroe, J., Graham, I.D., Eds.; Wiley Blackwell: Toronto, ON, Canada, 2013; p. 2012. [Google Scholar]
- Hagl, C.; Kanitz, R.; Gonzalez, K.; Hoegl, M. Change Management Interventions: Taking Stock and Moving Forward. Hum. Resour. Manag. Rev. 2024, 34, 101000. [Google Scholar] [CrossRef]
- Voehl, F.; Harrington, J. Sustainable Change Life Cycle. In Change Management: Manage the Change Or It Will Manage You; CRC Press: Boca Raton, FL, USA, 2017; p. 101. [Google Scholar]
- Bellot, J. Organizational Climate and Culture. In Leadership and Nursing Care Management; Huber, D.L., Joseph, M.L., Eds.; Elsevier: Columbia, MO, USA, 2022; p. 60. [Google Scholar]
- Safdari, A.; Rassouli, M.; Jafarizadeh, R.; Khademi, F.; Barasteh, S. Causes of Missed Nursing Care during COVID-19 Pandemic: A Qualitative Study in Iran. Front. Public Health. 2022, 10, 758156. [Google Scholar] [CrossRef]
- Australian Commission on Safety and Quality in Health Care. Implementing the Comprehensive Care Standard: Deliver Comprehensive Care; Australian Commission on Safety and Quality in Health Care: Sidney, Australia, 2020. [Google Scholar]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA: A Scale for the Quality Assessment of Narrative Review Articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed]
| Domain of Knowledge | Description |
|---|---|
| Domain of Distinctive Nature and Attributes of Patient Participation during the NBH | Distinctive Nature of Patient Participation Patient participation in NBH has been used not only as a practice for informing patients within the context of nursing care safety but also as a means of patient empowerment, supporting the development of self-management skills in preparation for discharge. |
| Distinctive Attributes of Patient Participation NBH is characterized by attributes grounded in the recognition that patients have an active role, while respecting confidentiality and privacy. Patient participation challenges nurses to manage sensitive information appropriately. | |
| Domain of Nurses’ Practices and Influencing Factors of Patient Participation during the NBH | Nurses’ Practices that Promote or Inhibit Patient Participation NBH involves a variety of nursing practices with different levels of patient involvement and participation. Nurses may demonstrate behaviors that either promote or inhibit patient participation, depending on whether they are starting or ending their shift, influencing the behaviors adopted by patients who are able and willing to participate. |
| Influencing Factors of Patient Participation Patient participation in NBH is influenced by contextual factors (e.g., organizational handover policies), patient-related factors (e.g., clinical condition or being asleep during NBH), and nurse-related factors (e.g., limited use of therapeutic communication skills). | |
| Domain of Strategies and Impacts of Increasing Patient Participation during the NBH | Strategies for Increasing Patient Participation NBH implementation strategies, such as the use of co-design approaches to interventions, the adoption of handover protocols to standardize nurses’ performance during handover, active support from nurse managers in change processes, and nurses’ training, are associated with increased patient participation. |
| Impacts of Increasing Patient Participation Enhanced patient participation in NBH affects nurses’ perceptions of individualized care provided to patients, including safety and protection, reduces patient anxiety, improves patient satisfaction with information exchange, and positively influences perceived quality of care. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruchinho, P.; Teixeira, G.; Lucas, P.; Gaspar, F.; López-Franco, M.D. Patient Participation During Nursing Bedside Handover: A State-of-the-Art Review. Nurs. Rep. 2025, 15, 438. https://doi.org/10.3390/nursrep15120438
Cruchinho P, Teixeira G, Lucas P, Gaspar F, López-Franco MD. Patient Participation During Nursing Bedside Handover: A State-of-the-Art Review. Nursing Reports. 2025; 15(12):438. https://doi.org/10.3390/nursrep15120438
Chicago/Turabian StyleCruchinho, Paulo, Gisela Teixeira, Pedro Lucas, Filomena Gaspar, and María Dolores López-Franco. 2025. "Patient Participation During Nursing Bedside Handover: A State-of-the-Art Review" Nursing Reports 15, no. 12: 438. https://doi.org/10.3390/nursrep15120438
APA StyleCruchinho, P., Teixeira, G., Lucas, P., Gaspar, F., & López-Franco, M. D. (2025). Patient Participation During Nursing Bedside Handover: A State-of-the-Art Review. Nursing Reports, 15(12), 438. https://doi.org/10.3390/nursrep15120438







