Topical Ozone as an Adjuvant Therapy in Wound Management: An Integrative Review
Abstract
1. Introduction
2. Material and Methods
2.1. Research Question
2.2. Studies Identification
2.3. Inclusion and Exclusion Criteria
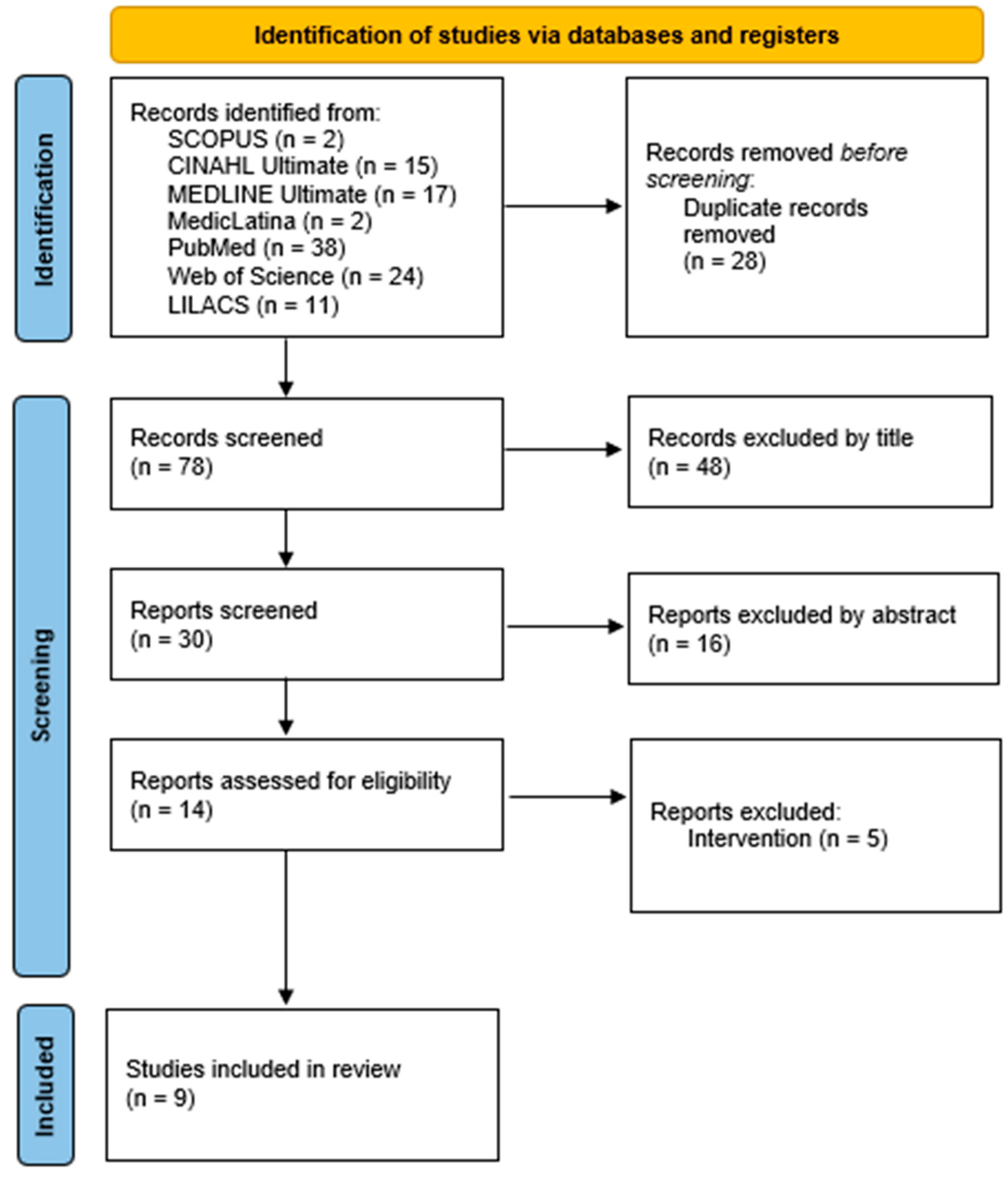
2.4. Study Selection
2.5. Quality Appraisal
2.6. Data Analyses
3. Results
3.1. Quality Appraisal and Assessment of Risk of Bias
3.2. Data Extraction
4. Discussion
4.1. Therapeutic Effects and Clinical Outcomes
4.2. Routes of Administration and Characteristics of Intervention
4.3. Advantages and Clinical Applicability
4.4. Study Limitations and Methodological Variability
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
References
- Blair, M.; Jones, J.; Woessner, A.; Quinn, K. Skin Structure-Function Relationships and the Wound Healing Response to Intrinsic Aging. Adv. Wound Care 2020, 9, 127–143. [Google Scholar] [CrossRef] [PubMed]
- Tottoli, E.; Dorati, R.; Genta, I.; Chiesa, E.; Pisani, S.; Conti, B. Skin Wound Healing Process and New Emerging Technologies for Skin Wound Care and Regeneration. Pharmaceutics 2020, 12, 735. [Google Scholar] [CrossRef]
- Mamun, A.; Shao, C.; Geng, P.; Wang, S.; Xiao, J. Recent advances in molecular mechanisms of skin wound healing and its treatments. Front. Immunol. 2024, 15, 1395479. [Google Scholar] [CrossRef]
- Cunha, J.B.; Dutra, R.A.A.; Salomé, G.M. Elaboration of an algorithm for wound evaluation and treatment. Estima—Braz. J. Enterostomal. Ther. 2018, 16, e2018. [Google Scholar] [CrossRef]
- Peña, O.; Martin, P. Cellular and molecular mechanisms of skin wound healing. Nat. Rev. Mol. Cell Biol. 2024, 25, 599–616. [Google Scholar] [CrossRef]
- Fayne, R.; Borda, L.; Egger, A.; Tomic-Canic, M. The Potential Impact of Social Genomics on Wound Healing. Adv. Wound Care 2020, 9, 325–331. [Google Scholar] [CrossRef]
- Olsson, M.; Järbrink, K.; Divakar, U.; Bajpai, R.; Upton, Z.; Schmidtchen, A.; Car, J. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen. 2018, 27, 114–125. [Google Scholar] [CrossRef]
- Sen, C. Human Wounds and its Burden: Updated 2022 Compendium of Estimates. Adv. Wound Care 2023, 12, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Hashim, N.; Babiker, R.; Dasnadi, S.; Islam, M.; Chaitanya, N.; Mohammed, R.; Farghal, N.S.; Gobara, B.; Rahman, M.M. The impact of ozone on periodontal cell line viability and function. Curr. Issues Mol. Biol. 2025, 47, 72. [Google Scholar] [CrossRef]
- Viebahn-Haensler, R.; Fernández, O. Ozone in Medicine. The Low-Dose Ozone Concept and Its Basic Biochemical Mechanisms of Action in Chronic Inflammatory Diseases. Int. J. Mol. Sci. 2021, 22, 7890. [Google Scholar] [CrossRef] [PubMed]
- Desmet, C.; Préat, V.; Gallez, B. Nanomedicines and gene therapy for the delivery of growth factors to improve perfusion and oxygenation in wound healing. Adv. Drug Deliv. Rev. 2018, 129, 262–284. [Google Scholar] [CrossRef] [PubMed]
- Anzolin, A.; Da Silveira-Kaross, N.; Bertol, C. Ozonated oil in wound healing: What has already been proven? Med. Gas. Res. 2020, 10, 54–59. [Google Scholar] [CrossRef]
- Sidauruk, R.; Yuniati, R.; Handojo, D. The Effectivity of Ozonated VCO on Healing Full Grafted Skin graft Study on Progenitor Cell Endothelial Proliferation and Angiogenesis in Sprague Dawley Mice. Med. Hosp. J. Clin. Med. 2021, 8, 133–138. [Google Scholar] [CrossRef]
- Bai, Q.; Zheng, C.; Sun, N.; Chen, W.; Gao, Q.; Liu, J.; Hu, F.; Zhou, T.; Zhang, Y.; Lu, T. Oxygen-releasing hydrogels promote burn healing under hypoxic conditions. Acta Biomater. 2022, 154, 231–243. [Google Scholar] [CrossRef]
- Pasek, J.; Stanek, A.; Szyluk, K.; Cieślar, G. Ozone Therapy in the Comprehensive Treatment of Leg Ulcers: Case Report. Adv. Skin. Wound Care 2022, 35, 1–5. [Google Scholar] [CrossRef]
- Pasek, J.; Kowalska, A.; Nowak, M. Topical hyperbaric oxygen therapy versus local ozone therapy in healing of venous leg ulcers. Int. J. Environ. Res. Public Health 2023, 20, 1967. [Google Scholar] [CrossRef]
- Pasek, J.; Szajkowski, S.; Cieślar, G. Effect of Treatment of Neuropathic and Ischemic Diabetic Foot Ulcers with the Use of Local Ozone Therapy Procedures—An Observational Single Center Study. Clin. Pract. 2024, 14, 2139–2150. [Google Scholar] [CrossRef]
- Nobre, V.P.C.C.; Gehring Junior, W.; Gamba, M.A.; Oliveira, L.S.S.; Taminato, M. Uso do ozônio no tratamento de feridas: Revisão de escopo. Rev. Feridas 2021, 9, 1773–1778. [Google Scholar] [CrossRef]
- Targino, A.P.L.R.; Reis, E.F.; Ambrozio, L.S.; Santos, S.M.; Carmo, H.O. A aplicabilidade e os benefícios da ozonioterapia no tratamento de feridas: Uma revisão integrativa. In: Ciências Biológicas e da Saúde: Integrando Saberes em Diferentes Contextos. Ed. Cient. 2022, 1, 13–28. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. Checklist for Systematic Reviews and Research Syntheses; The Joanna Briggs Institute: Adelaide, Australia, 2020; Available online: https://jbi.global/ (accessed on 15 March 2025).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Li, L.; Feng, A.; Lu, J.; Liu, H.; Xue, W.; Cui, H. Evaluating the Therapeutic Efficacy of Ozone Liquid Dressing in Healing Wounds Associated with Bullous Pemphigoid. Sci. Rep. 2025, 15, 7205. [Google Scholar] [CrossRef] [PubMed]
- Pasek, J.; Szajkowski, S.; Rokicka, D.; Wróbel, M.; Travagli, V.; Cieślar, G. Impact of Ozone Concentration on the Treatment Effectiveness of Diabetic Foot Syndrome: A Pilot Single-Centre Study. Postepy Dermatol. Alergol. 2024, 41, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Heng, H.; Liu, X.; Geng, H.; Liang, J. Evaluation of the healing potential of short-term ozone therapy for the treatment of diabetic foot ulcers. Front. Endocrinol. 2024, 14, 1304034. [Google Scholar] [CrossRef] [PubMed]
- Darenskaya, M.A.; Tokmakova, S.I.; Bondarenko, O.V.; Ziablitskaia, K.V.; Lunitsyna, Y.V.; Mokrenko, E.V.; Goncharov, I.S.; Gaidarova, T.A.; Klyushnikov, O.V.; Suslikova, M.I.; et al. Effectiveness of Combined Application of Cryosurgical Method and Local Ozone Therapy in Patients with Oral Leukoplakia. Biomed. Res. Ther. 2023, 10, 5491–5499. [Google Scholar] [CrossRef]
- Marinova, P. Ruptured Ulcerated and Inflamed Gout Tophi with Deep Soft Tissue Infection of Left Foot—When Rheumatology Meets Surgery: A Case Report Treated with Local Ozone Therapy. Rheumatology 2023, 31, 108–119. [Google Scholar] [CrossRef]
- Buric, J.; Berjano, P.; Damilano, M. Severe Spinal Surgery Infection and Local Ozone Therapy as Complementary Treatment: A Case Report. Int. J. Spine Surg. 2019, 13, 371–376. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Mendes, K.D.S.; Silveira, R.C.C.P.; Galvão, C.M. Integrative review: Research method for the incorporation of evidence in health and nursing. Texto Contexto Enferm. 2008, 17, 758–764. [Google Scholar] [CrossRef]
- Souza, M.T.; Silva, M.D.; Carvalho, R. Integrative review: What is it? How to do it? Einstein 2010, 8, 102–106. [Google Scholar] [CrossRef]
- Torraco, R.J. Writing integrative literature reviews: Using the past and present to explore the future. Hum. Resour. Dev. Rev. 2016, 15, 404–428. [Google Scholar] [CrossRef]
- Roth, A.; Elkashif, A.; Selvamani, V.; Stucky, R.; Seleem, M.; Ziaie, B.; Rahimi, R. Wearable and flexible ozone generating system for treatment of infected dermal wounds. Front. Bioeng. Biotechnol. 2020, 8, 458. [Google Scholar] [CrossRef]
- Baggio, A.; Bizelli, V.; Delamura, I.; Viotto, A.; Veras, A.; Teixeira, G.; Faverani, L.P.; Bassi, A.P.F. Systemic ozone therapy as an adjunctive treatment in guided bone regeneration: A histomorphometrical and immunohistochemical study in rats. Clin. Oral. Investig. 2024, 28, 556. [Google Scholar] [CrossRef] [PubMed]
- Pires, J.; Karam, A.; Garcia, V.; Ribeiro, F.; Pontes, A.; Andrade, C.; Zuza, E.C. Effect of systemic ozone therapy as a biomodulator of tissue regeneration and inflammatory response in rats. Rev. Odontol. UNESP 2021, 50, e20210046. [Google Scholar] [CrossRef]
- Cascini, F.; Franzini, M.; Andreoli, A.; Manzotti, A.; Cadeddu, C.; Quaranta, G.; Gentili, A.; Ricciardi, W. Use of oxygen-ozone therapy to improve the effectiveness of antibiotic treatment on infected arthroplasty: Protocol for a superiority, open-label, multicentre, randomised, parallel trial. BMJ Open 2024, 14, e076739. [Google Scholar] [CrossRef] [PubMed]
- Roth, A.; Krishnakumar, A.; McCain, R.; Maruthamuthu, M.; McIntosh, M.; Chen, Y.; Cox, A.D.; Jannasch, A.S.H.; Nguyen, J.; Seleem, M.N.; et al. Biocompatibility and safety assessment of combined topical ozone and antibiotics for treatment of infected wounds. ACS Biomater. Sci. Eng. 2023, 9, 3606–3617. [Google Scholar] [CrossRef]
- Viebahn-Hänsler, R.; León Fernández, O.S.; Fahmy, Z. Concept—Guidelines and Treatment Strategies. Ozone Sci. Eng. 2012, 34, 408–424. [Google Scholar] [CrossRef]
| Database | Search Strategy | Results Retrieved |
|---|---|---|
| SCOPUS | ((adult) AND (“ozone”) AND (“wounds”) AND (“therapeutic effects” OR “therapeutic efficacy”)) | 2 |
| CINAHL Ultimate | ((adults OR aged OR elderly) AND (“ozone therapy”) AND (“therapeutic effect” OR “therapeutic efficacy”) AND (“wounds” OR “chronic wounds”)) | 15 |
| MEDLINE Ultimate | (“Ozone”[MeSH] OR “ozone therapy”) AND (“Wound Healing”[MeSH] OR “Skin Ulcer”[MeSH]) AND (“Topical Administration”[MeSH] OR “topical ozone”) | 17 |
| MedicLatina | (“ozonoterapia” OR “ozono tópico”) AND (“feridas” OR “úlceras”) AND (“terapia adjuvante” OR “tratamento complementar”) | 2 |
| PubMed | (“Ozone”[MeSH Terms] OR “ozonated oil” OR “ozonated water” OR “ozone gas”) AND (“Wound Healing”[MeSH Terms] OR “chronic wounds” OR “diabetic foot ulcer”) AND (“Topical Administration”[MeSH] OR “adjuvant therapy” OR “complementary therapy”) | 38 |
| Web of Science | TS=(“ozone” AND “wound healing” AND (“topical” OR “adjuvant” OR “complementary therapy”)) | 24 |
| LILACS | (“ozônio” OR “ozonioterapia”) AND (“feridas” OR “úlceras crônicas”) AND (“terapia adjuvante” OR “cuidados complementares”) [DeCS terms applied] | 11 |
| Paper | Study Design | JBI Tool |
|---|---|---|
| Li, L. et al. (2025) [22]—Evaluating the therapeutic efficacy of ozone liquid dressing in healing wounds associated with bullous pemphigoid | Experimental study | JBI Critical Appraisal Checklist for Randomized Controlled Trials |
| Pasek, J. et al. (2024) [23]—Impact of ozone concentration on the treatment effectiveness of diabetic foot syndrome: a pilot single-centre study | Quasi-Experimental Study | JBI Critical Appraisal Checklist for Quasi-Experimental Studies |
| Pasek, J. et al. (2024) [17]—Effect of Treatment of Neuropathic and Ischemic Diabetic Foot Ulcers with the Use of Local Ozone Therapy Procedures | Observational study | JBI Critical Appraisal Checklist for Analytical Observational Studies |
| Sun et al. (2024) [24]—Evaluation of the healing potential of short-term ozone therapy for the treatment of diabetic foot ulcers | Retrospective cohort study | JBI Critical Appraisal Checklist for Analytical Cohort Studies |
| Pasek, J. et al. (2023) [16]—Topical Hyperbaric Oxygen Therapy Versus Local Ozone Therapy in Healing of Venous Leg Ulcers | Randomized Controlled Trials | JBI Critical Appraisal Checklist for Randomized Controlled Trials |
| Darenskaya, M.A. et al. (2023) [25]—Effectiveness of Combined Application of Cryosurgical Method and Local Ozone Therapy in Patients with Oral Leukoplakia | Experimental study | JBI Critical Appraisal Checklist for Experimental Studies |
| Marinova, P.G. (2023) [26]—Ruptured Ulcerated and Inflamed Gout Tophi with Deep Soft Tissue Infection of Left Foot—Case Treated with Local Ozone Therapy | Case report | JBI Critical Appraisal Checklist for Case Reports |
| Pasek, J. et al. (2022) [15]—Ozone Therapy in the Comprehensive Treatment of Leg Ulcers: Case Report | Case report | JBI Critical Appraisal Checklist for Case Reports |
| Buric et al. (2019) [27]—Severe spinal surgery infection and local ozone therapy as complementary treatment: A case report | Case report | JBI Critical Appraisal Checklist for Case Reports |
| Paper | Score Obtained | Maximum Score | Percentage (%) | Justification |
|---|---|---|---|---|
| Li et al. (2025) [22] | 8 | 10 | 80% | Well-structured study, but with some shortcomings in detailing the randomization and allocation criteria. |
| Pasek et al. (2024) [23] | 7 | 10 | 70% | Minor flaws in the description of how participants were allocated to different ozone concentrations. |
| Pasek et al. (2024) [17] | 6 | 10 | 60% | Some issues regarding control of selection and confounding bias. |
| Sun et al. (2024) [24] | 8 | 10 | 80% | Retrospective study with reasonable control group and appropriate statistical analysis; limitations in randomization and blinding |
| Pasek et al. (2023) [16] | 9 | 10 | 90% | Well-conducted study, although with limitations in bias control. |
| Darenskaya et al. (2023) [25] | 8 | 10 | 80% | Good outcomes, but some limitations in randomization and bias control. |
| Marinova (2023) [26] | 6 | 10 | 60% | Interesting application but limited due to single-case study design. |
| Pasek et al. (2022) [15] | 7 | 10 | 70% | Limited conclusions due to case study format. |
| Buric et al. (2019) [27] | 7 | 10 | 70% | Positive clinical outcomes, but limited generalizability due to being a single case report |
| Study | Author | Year | Country | Aim of the Study |
|---|---|---|---|---|
| S1 | Li et al. [22] | 2025 | China | To evaluate the therapeutic efficacy of liquid ozone dressings in patients with bullous pemphigoid |
| S2 | Pasek et al. [23] | 2024 | Poland | To assess the impact of ozone concentration on the effectiveness of diabetic foot syndrome treatment |
| S3 | Pasek et al. [17] | 2024 | Poland | To evaluate the healing of neuropathic and ischemic diabetic ulcers with local ozone |
| S4 | Sun et al. [24] | 2024 | China | To evaluate the clinical outcomes and inflammatory biomarkers in diabetic foot ulcers treated with short-term topical ozone therapy |
| S5 | Pasek et al. [16] | 2023 | Poland | To compare the therapeutic efficacy of topical hyperbaric oxygen therapy versus ozone therapy in venous ulcers |
| S6 | Darenskaya et al. [25] | 2023 | Russia | To evaluate the efficacy of cryosurgery combined with ozone in oral leukoplakia |
| S7 | Marinova [26] | 2023 | Bulgaria | To report the treatment of an ulcerated and infected gouty tophus with ozone |
| S8 | Pasek et al. [15] | 2022 | Poland | To report a case of chronic ulcer treated with ozone |
| S9 | Buric et al. [27] | 2019 | Italy | To report a post-surgical infection treated with ozone as adjunctive therapy |
| Study | Methodology and Sample Size | Type of Wound | Ozone Intervention | Main Results |
|---|---|---|---|---|
| S1 | Experimental study with control group (n = 120) | Bullous pemphigoid | Ozonated water; daily application; up to 14 days | Higher healing rate; reduced pain and infection |
| S2 | Quasi-Experimental Study (n = 50) | Diabetic foot | O3 at 30 µg/mL (group 1) and 60 µg/mL (group 2); 30 sessions of 30 min | Greater wound area and pain reduction in group 2 |
| S3 | Observational study (n = 90) | Neuropathic and ischemic diabetic ulcers | Local O3; number of sessions not specified | Significant wound reduction; higher efficacy in neuropathic ulcers |
| S4 | Retrospective cohort study (n = 89) | Diabetic foot ulcers | Short-term topical ozone therapy (gaseous ozone); evaluated over 12 weeks | Improved healing rate, reduced inflammation (↓ CRP, IL-6, TNF-α), ↑ VEGF and SOD; fewer reinfections and reoperations |
| S5 | Randomized Controlled Trials (n = 114) | Venous ulcer | 30 sessions of local ozone | Reduction of ulcer area and pain; less effective than oxygen therapy |
| S6 | Experimental study (n = 33) | Verrucous oral leukoplakia | Ozonated olive oil after cryosurgery; 14 days | Pain and edema reduction; increased epithelialization |
| S7 | Case report | Ulcerated and infected gouty tophus | Ozonated olive oil with vitamin E | Progressive improvement in infection and healing |
| S8 | Case report | Chronic ulcer post-orthopedic surgery | 30 sessions of local ozone | Complete healing; pain relief and improved quality of life |
| S9 | Case report | Spinal surgical infection | Ozone gas injected twice/week for 3 weeks | Total wound healing; no recurrence after 1 year |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinto, C.B.; Pinto, A.; Barroso, M.; Coelho, T.; Costa, S. Topical Ozone as an Adjuvant Therapy in Wound Management: An Integrative Review. Nurs. Rep. 2025, 15, 414. https://doi.org/10.3390/nursrep15120414
Pinto CB, Pinto A, Barroso M, Coelho T, Costa S. Topical Ozone as an Adjuvant Therapy in Wound Management: An Integrative Review. Nursing Reports. 2025; 15(12):414. https://doi.org/10.3390/nursrep15120414
Chicago/Turabian StylePinto, Cristina Barroso, Adelino Pinto, Manuela Barroso, Telma Coelho, and Sandra Costa. 2025. "Topical Ozone as an Adjuvant Therapy in Wound Management: An Integrative Review" Nursing Reports 15, no. 12: 414. https://doi.org/10.3390/nursrep15120414
APA StylePinto, C. B., Pinto, A., Barroso, M., Coelho, T., & Costa, S. (2025). Topical Ozone as an Adjuvant Therapy in Wound Management: An Integrative Review. Nursing Reports, 15(12), 414. https://doi.org/10.3390/nursrep15120414







