Influence of the Catecholamine Syringe Changeover Method on Patients’ Blood Pressure Variability: A Single-Center Retrospective Study
Abstract
1. Introduction
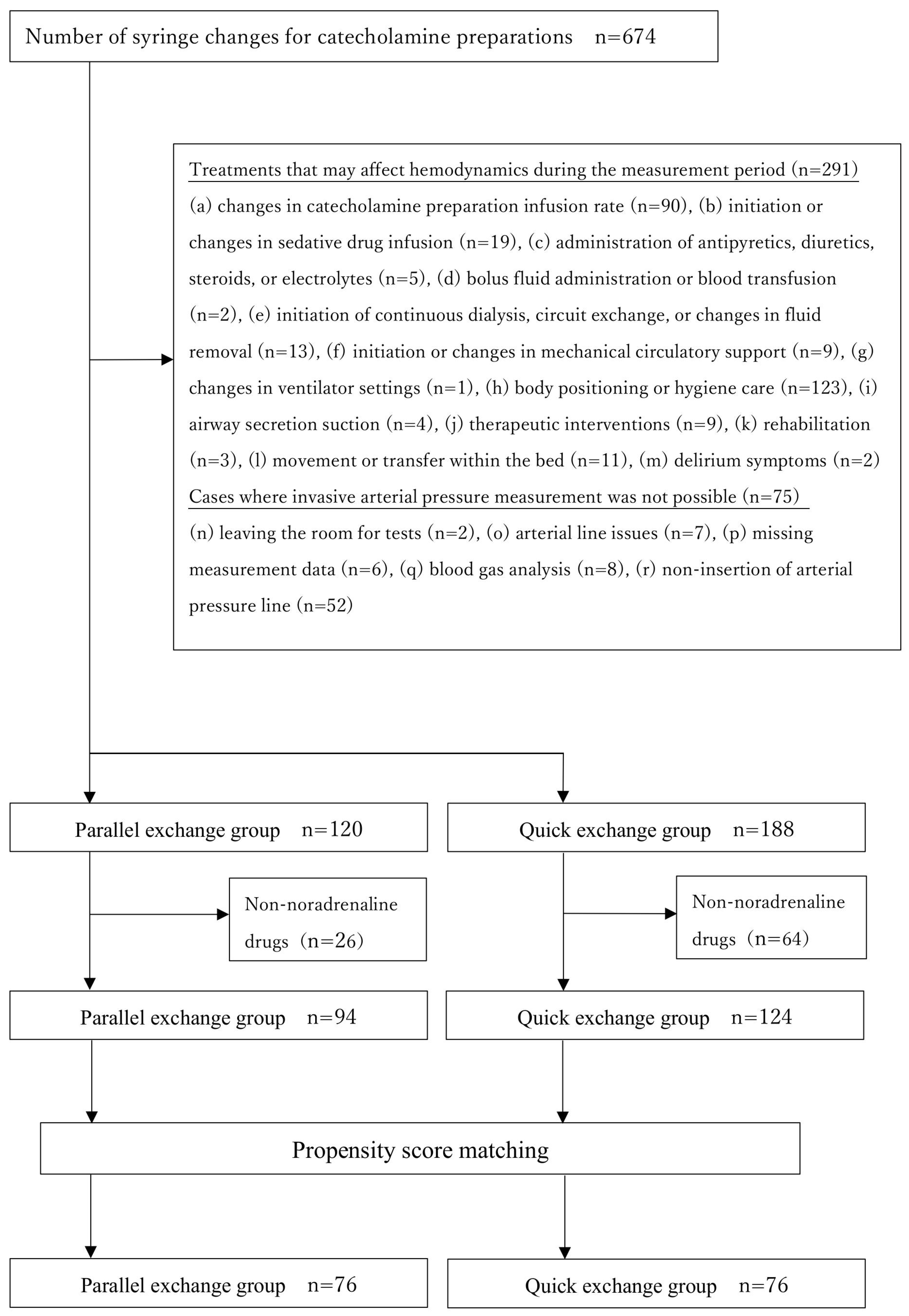
2. Materials and Methods
3. Results
3.1. Unadjusted Comparison Between the Parallel and Quick Exchange Groups
3.2. Comparison Between the Parallel Exchange Group and the Quick Exchange Group After Propensity Score Matching
3.3. Syringe Exchange in Patients with Severe Shock (Sub-Analysis)
3.4. Risk Factors for Syringe Exchange of Catecholamine Drugs
4. Discussion
4.1. Limitations
4.2. Implications for Emergency Nursing
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
References
- Argaud, L.; Cour, M.; Martin, O.; Saint-Denis, M.; Ferry, T.; Goyatton, A.; Robert, D. Changeovers of vasoactive drug infusion pumps: Impact of a quality improvement program. Crit. Care 2007, 11, R133. [Google Scholar] [CrossRef] [PubMed]
- Greau, E.; Lascarrou, J.B.; Le Thuaut, A.; Maquigneau, N.; Alcourt, Y.; Coutolleau, A.; Rousseau, C.; Erragne, V.; Reignier, J. Automatic versus manual changeovers of norepinephrine infusion pumps in critically ill adults: A prospective controlled study. Ann. Intensive Care 2015, 5, 40. [Google Scholar] [CrossRef] [PubMed]
- Elli, S.; Mattiussi, E.; Bambi, S.; Tupputi, S.; Fratello, S.S.; De Nunzio, A.; D’Auria, S.; Rona, R.; Fumagalli, R.; Lucchini, A. Changing the syringe pump: A challenging procedure in critically ill patients. J. Vasc. Access 2020, 21, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Saitoh, S.; Shiromaru, M. Research trends in syringe exchange of catecholamine preparations. J. Jpn. Soc. Emerg. Med. 2013, 16, 551–556. (In Japanese) [Google Scholar]
- Ishikawa, A.; Watanabe, J.; Kuramoto, N. Manual syringe exchange method for catecholamine administration by nurses in critical care units. Jpn. J. Nurs. Art. Sci. 2022, 21, 1–5. (In Japanese) [Google Scholar]
- Tamura, A.; Yamamoto, M.; Sumi, T.; Maruyama, S.; Hamanabe, T.; Saitoh, N.; Abe, S.; Ohta, R.; Sasaki, M.; Kasajima, R.; et al. Evaluation of parallel exchange methods using the communication capability of syringes. J. Hokkaido Assoc. Clin. Eng. Technol. 2020, 30, 126–129. (In Japanese) [Google Scholar]
- Yoshida, R.; Tsukamoto, T.; Shobara, T.; Kashiwagi, M.; Ohyama, M. Syringe infusion pump replacement method in patients receiving continuous catecholamine. Nurs. Res. Collect. Nurs. Dep. Kawasaki Munic. Hosp. 2010, 64, 34–36. (In Japanese) [Google Scholar]
- Yoshida, K.; Fukuzaki, M. Verification of the effect of syringe infusion pump operating conditions on infusion volume. Jpn. J. Occup. Med. Traumatol. 2015, 63, 31–35. (In Japanese) [Google Scholar]
- Yamada, N.; Nakanishi, S.; Iwadate, N. A study of syringe exchange methods in catecholamine use—Quick and parallel exchange methods. J. Hokkaido Assoc. Clin. Eng. Technol. 2012, 22, 21–23. (In Japanese) [Google Scholar]
- Poiroux, L.; Le Roy, C.; Ramelet, A.S.; Le Brazic, M.; Messager, L.; Gressent, A.; Alcourt, Y.; Haubertin, C.; Hamel, J.-F.; Piquilloud, L.; et al. Minimising haemodynamic lability during changeover of syringes infusing norepinephrine in adult critical care patients: A multicentre randomised controlled trial. Br. J. Anaesth. 2020, 125, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Lucchini, A.; Elli, S.; Burgazzi, A.; Grilli, L.M.; Pes, C.; Ferrari, K.; Fumagalli, L.; Fiorillo, C.; Giani, M.; Rezoagli, E. Simulated haemodynamic parameters and different infusion set-up affect drug delivery during syringe pump change over: A bench-top study in a laboratory setting. Crit. Care Nurs. 2025, 86, 103861. [Google Scholar] [CrossRef]
- Klem, S.A.; Farrington, J.M.; Leff, R.D. Influence of infusion pump operation and flow rate on hemodynamic stability during epinephrine infusion. Crit. Care Med. 1993, 21, 1213–1217. [Google Scholar] [CrossRef] [PubMed]
- Haneda, S.; Kikuchi, K. Pathogenesis and management of hypertension in the elderly. Nihon Ronen Igakkai Zasshi 1999, 36, 605–612. (In Japanese) [Google Scholar] [CrossRef] [PubMed][Green Version]

| Parallel Exchange (n = 120) | Quick Exchange (n = 188) | p Value | |
|---|---|---|---|
| Age | 70.0 (64.8–83.0) | 68.5 (50.8–80.3) | 0.005 |
| Sex (male, %) | 79 (65.8) | 106 (56.4) | 0.099 |
| Primary disease | |||
| Infection (n, %) | 56 (46.7) | 70 (37.2) | 0.101 |
| Post-cardiac arrest (n, %) | 35 (29.2) | 59 (31.4) | 0.680 |
| Burns (n, %) | 23 (19.2) | 24 (12.8) | 0.128 |
| Hypothermia (n, %) | 6 (5.0) | 10 (5.3) | 0.902 |
| Medical history | |||
| Hypertension (n, %) | 44 (36.7) | 45 (23.9) | 0.009 |
| Diabetes (n, %) | 23 (19.2) | 54 (28.7) | 0.083 |
| Heart disease (n, %) | 21 (17.5) | 68 (36.2) | 0.001 |
| Type of exchanged drug | 0.071 | ||
| Noradrenaline (n, %) | 94 (78.3) | 124 (66.0) | |
| Dobutamine (n, %) | 11 (9.2) | 37 (19.7) | |
| Vasopressin (n, %) | 9 (7.5) | 20 (10.6) | |
| Adrenaline (n, %) | 4 (3.3) | 2 (1.1) | |
| Dopamine (n, %) | 0 (0.0) | 2 (1.1) | |
| Milrinone (n, %) | 0 (0.0) | 1 (0.5) | |
| Normal saline solution to boost catecholamine (n, %) | 2 (1.7) | 2 (1.1) | |
| Number of catecholamines used (single, %) | 63 (52.5) | 57 (30.3) | 0.024 |
| Total flow rate of the exchange route at the time of exchange (mL/h) | 5.6 (3.6–9.1) | 6.4 (4.1–8.25) | 0.249 |
| Infusion rate of the exchanged drug (mL/h) | 4.15 (2.1–6.1) | 4.1 (2.5–5.6) | 0.825 |
| Dosage of the exchanged drug (γ) | 0.2 (0.1–0.3) | 0.2 (0.1–0.5) | 0.064 |
| The coefficient of variation in mean blood pressure during the 30 min before syringe exchange | 0.029 (0.019–0.050) | 0.030 (0.017–0.049) | 0.517 |
| The time of exchange (Night, %) | 68 (56.7) | 96 (51.1) | 0.337 |
| Parallel Exchange (n = 120) | Quick Exchange (n = 188) | p Value | ||
|---|---|---|---|---|
| Coefficient of variation | ||||
| After 5 min | SBP | 0.026 (0.013–0.050) | 0.024 (0.012–0.046) | 0.542 |
| DBP | 0.021 (0.009–0.042) | 0.022 (0.009–0.041) | 0.901 | |
| MBP | 0.024 (0.011–0.049) | 0.023 (0.010–0.043) | 0.473 | |
| After 10 min | SBP | 0.037 (0.021–0.067) | 0.037 (0.020–0.061) | 0.674 |
| DBP | 0.031 (0.017–0.055) | 0.034 (0.017–0.053) | 0.880 | |
| MBP | 0.035 (0.019–0.059) | 0.034 (0.018–0.059) | 0.589 | |
| After 15 min | SBP | 0.040 (0.026–0.071) | 0.043 (0.024–0.071) | 0.661 |
| DBP | 0.038 (0.024–0.057) | 0.036 (0.020–0.064) | 0.631 | |
| MBP | 0.040 (0.024–0.064) | 0.039 (0.022–0.067) | 0.472 | |
| Absolute value of the change | ||||
| After 5 min | SBP | −1.0 (−6.0–6.0) | −3.0 (−8.0–2.0) | 0.050 |
| DBP | −1.0 (−3.0–2.0) | −1.0 (−3.0–2.0) | 0.978 | |
| MBP | −0.7 (−4.3–3.3) | −1.3 (−4.4–1.3) | 0.209 | |
| After 10 min | SBP | 0.0 (−7.0–5.0) | −2.5 (−7.0–4.0) | 0.303 |
| DBP | 0.0 (−3.0–2.0) | 0.0 (−3.0–3.0) | 0.761 | |
| MBP | 0.0 (−4.8–3.0) | −0.7 (−4.4–2.7) | 0.683 | |
| After 15 min | SBP | −2.0 (−8.0–3.0) | −2.0 (−8.0–4.3) | 0.680 |
| DBP | −1.0 (−3.3–1.0) | 0.0 (−3.0–3.0) | 0.194 | |
| MBP | −1.3 (−5.0–2.3) | −1.2 (−4.7–3.0) | 0.538 | |
| Parallel Exchange (n = 76) | Quick Exchange (n = 76) | p Value | ||
|---|---|---|---|---|
| Coefficient of variation | ||||
| After 5 min | SBP | 0.027 (0.013–0.049) | 0.035 (0.017–0.055) | 0.268 |
| DBP | 0.018 (0.009–0.042) | 0.027 (0.010–0.046) | 0.152 | |
| MBP | 0.024 (0.011–0.044) | 0.032 (0.011–0.046) | 0.360 | |
| After 10 min | SBP | 0.041 (0.022–0.064) | 0.048 (0.024–0.073) | 0.354 |
| DBP | 0.033 (0.015–0.050) | 0.037 (0.021–0.054) | 0.398 | |
| MBP | 0.036 (0.019–0.057) | 0.040 (0.020–0.064) | 0.454 | |
| After 15 min | SBP | 0.042 (0.026–0.073) | 0.054 (0.028–0.079) | 0.560 |
| DBP | 0.040 (0.024–0.056) | 0.041 (0.026–0.063) | 0.799 | |
| MBP | 0.041 (0.024–0.065) | 0.046 (0.026–0.073) | 0.737 | |
| Absolute value of the change | ||||
| After 5 min | SBP | −1.0 (−8.0–5.3) | −3.0 (−10.0–4.3) | 0.398 |
| DBP | −1.0 (−3.3–1.3) | 0.0 (−3.0–2.3) | 0.459 | |
| MBP | −1.0 (−5.0–2.7) | −1.2 (−5.8–2.2) | 0.892 | |
| After 10 min | SBP | −1.0 (−9.0–4.0) | −1.5 (−8.3–4.0) | 0.867 |
| DBP | 0.0 (−3.0–1.0) | 0.0 (−3.0–3.0) | 0.226 | |
| MBP | 0.0 (−5.0–2.0) | −0.3 (−4.8–3.8) | 0.538 | |
| After 15 min | SBP | −2.0 (−6.0–4.0) | −2.5 (−8.0–5.0) | 0.839 |
| DBP | −1.0 (−4.0–1.3) | 0.0 (−3.0–3.0) | 0.411 | |
| MBP | −1.3 (−4.4–2.6) | −1.2 (−4.8–3.4) | 0.818 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niitsu, Y.; Tsuchida, T.; Sato, R.; Shintaku, J.; Iwasa, K. Influence of the Catecholamine Syringe Changeover Method on Patients’ Blood Pressure Variability: A Single-Center Retrospective Study. Nurs. Rep. 2025, 15, 345. https://doi.org/10.3390/nursrep15100345
Niitsu Y, Tsuchida T, Sato R, Shintaku J, Iwasa K. Influence of the Catecholamine Syringe Changeover Method on Patients’ Blood Pressure Variability: A Single-Center Retrospective Study. Nursing Reports. 2025; 15(10):345. https://doi.org/10.3390/nursrep15100345
Chicago/Turabian StyleNiitsu, Yuta, Takumi Tsuchida, Ryuta Sato, Juna Shintaku, and Koichi Iwasa. 2025. "Influence of the Catecholamine Syringe Changeover Method on Patients’ Blood Pressure Variability: A Single-Center Retrospective Study" Nursing Reports 15, no. 10: 345. https://doi.org/10.3390/nursrep15100345
APA StyleNiitsu, Y., Tsuchida, T., Sato, R., Shintaku, J., & Iwasa, K. (2025). Influence of the Catecholamine Syringe Changeover Method on Patients’ Blood Pressure Variability: A Single-Center Retrospective Study. Nursing Reports, 15(10), 345. https://doi.org/10.3390/nursrep15100345







