Investigating the Effects of Intraprofessional Learning in Nursing Education: Protocol for a Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
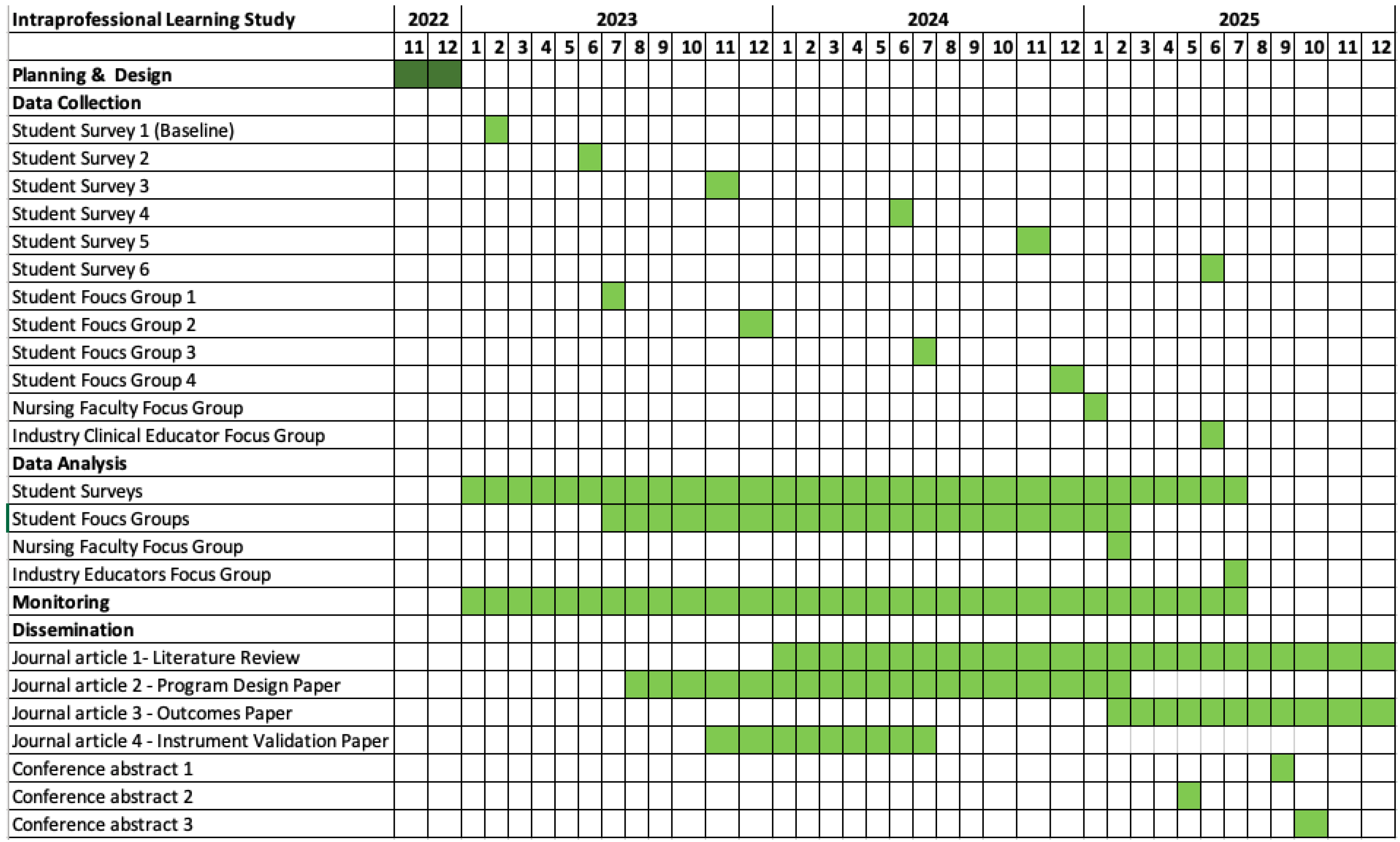
2.1. Design
2.2. Ethics
2.3. Participants and Recruitment Methods
2.4. Recruitment
2.5. Setting
2.6. Intervention
2.7. Data Collection
- Demographic information collected at Time Point 1 [T0].
- The modified KidSIMTM Attitudes Towards Teams in Training Undergoing Designed Educational Simulation Questionnaire (M-ATTITUDES), to suit the IaPL context. All 6 time points [T0–T5].
- Self-efficacy questions to elicit views on knowledge, motivation and confidence for intraprofessional collaborative practice at 5 time points [T0–T5, confidence items only for T0].
- Learning experience questions to elicit views about the intraprofessional teaching approaches at 4 time points [T1–T4].
- For Diploma of Nursing students, there will be a question about whether the IaPL increased their motivation to enroll in a Bachelor of Nursing degree in the future at 5 time points [T1–T5].
- One open-ended question asking for general comments on the IaPL at 5 time points [T1–T5].
Focus Groups
2.8. Instruments
Student Surveys
2.9. Data Analysis
2.10. Risk Management and Safety
2.11. Data Security and Handling
2.12. Confidentiality and Security
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barr, H. Interprofessional Education: Today, Yesterday and Tomorrow. The UK Centre for the Advancement of Interprofessional Education, LTSN for Health Sciences and Practice. 2002. Available online: http://www.health.heacademy.ac.uk/publications/occasionalpaper/occp1 (accessed on 1 March 2023).
- World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010.
- Teheux, L.; Coolen, E.H.; Draaisma, J.M.; de Visser, M.; Scherpbier-de Haan, N.D.; Kuijer-Siebelink, W.; van der Velden, J.A. Intraprofessional workplace learning in postgraduate medical education: A scoping review. BMC Med. Educ. 2021, 21, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Bainbridge, L.; Nasmith, L. Inter and Intra-Professional Collaborative Patient-Centred Care in Postgraduate Medical Education. Members of the FMEC PG Consortium. 2011. Available online: https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=1cf1bf30ac038b7bbaf98b0385111ee25c4aa23c (accessed on 1 March 2023).
- McComas, M.J.; Inglehart, M.R. Dental, dental hygiene, and graduate students’ and faculty perspectives on dental hygienists’ professional role and the potential contribution of a peer teaching program. J. Dent. Educ. 2016, 80, 1049–1061. [Google Scholar] [CrossRef]
- Otsuka, H.; Kondo, K.; Ohara, Y.; Yasuda, M.; Kishimoto, N.; Sunaga, M.; Endo, K.; Arakawa, S.; Kinoshita, A.; Shinada, K. An Inter-and Intraprofessional Education Program in Which Dental Hygiene Students Instruct Medical and Dental Students. J. Dent. Educ. 2016, 80, 1062–1070. [Google Scholar] [CrossRef] [PubMed]
- Jones, V.E.; Karydis, A.; Hottel, T.L. Dental and dental hygiene intraprofessional education: A pilot program and assessment of students’ and patients’ satisfaction. J. Dent. Educ. 2017, 81, 1203–1212. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.C.; Bilich, L.A.; Skuza, N. The benefits and challenges of collaborative learning: Educating dental and dental hygiene students together. J. Dent. Educ. 2018, 82, 1279–1286. [Google Scholar] [CrossRef]
- Flynn, P.M.; Luthra, M.; Blue, C.M. Did Intraprofessional Training with Dental Therapists Affect Dental Students’ Attitudes Toward Caring for the Underserved? J. Dent. Educ. 2017, 81, 162–168. [Google Scholar] [CrossRef]
- Ephrem, H.; Self, K.D.; Blue, C.M. Introducing and Evaluating Intraprofessional Team-Based Care Delivery in a Dental School Clinic: A Pilot Study. J. Dent. Educ. 2018, 82, 980–988. [Google Scholar] [CrossRef]
- Jung, B.; Salvatori, P.; Martin, A. Intraprofessional fieldwork education: Occupational therapy and occupational therapist assistant students learning together. Can. J. Occup. Ther. 2008, 75, 42–50. [Google Scholar] [CrossRef]
- Plack, M.M.; Williams, S.; Miller, D.; Malik, F.; Sniffen, J.; McKenna, R.; Gilner, G. Collaboration between physical therapists and physical therapist assistants: Fostering the development of the preferred relationship within a classroom setting. J. Phys. Ther. Educ. 2006, 20, 3–13. [Google Scholar] [CrossRef]
- Ylitörmänen, T.; Kvist, T.; Turunen, H. Intraprofessional collaboration: A qualitative study of registered nurses’ experiences. Collegian 2023, 30, 17–24. [Google Scholar] [CrossRef]
- Eckhoff, D.O.; Diaz, D.A.; Anderson, M. Using simulation to teach intraprofessional telehealth communication. Clin. Simul. Nurs. 2022, 67, 39–48. [Google Scholar] [CrossRef]
- Wesemann, D.; Posey, K.; Wilson, C. Clinical Simulation to Evaluate Students’ Intraprofessional Telehealth Skills between Multiple University Campuses. Clin. Simul. Nurs. 2021, 54, 35–39. [Google Scholar] [CrossRef]
- Limoges, J.; Jagos, K.; Lankshear, S.; Madorin, S.; Witmer, D. Getting to the root of it: How do faculty address professional boundaries, role expansion, and intra-professional collaboration? J. Nurs. Educ. Pract. 2018, 8, 113–121. [Google Scholar] [CrossRef]
- Boothby, J.; Gropelli, T.; Succheralli, L. An innovative teaching model using intraprofessional simulations. Nurs. Educ. Perspect. 2019, 40, 184–185. [Google Scholar] [CrossRef]
- Berger, J.D.; Kuszajewski, M.; Borghese, C.; Muckler, V.C. A quality improvement project using high-fidelity simulation training to improve clinical knowledge among critical care transport nurses. Clin. Simul. Nurs. 2018, 14, 54–60. [Google Scholar] [CrossRef]
- Moore, J.; Jairath, N.; Montejo, L.; O’Brien, S.; Want, D. Using a Telehealth Simulation to Prepare Nursing Students for Intraprofessional Collaboration. Clin. Simul. Nurs. 2023, 78, 1–6. [Google Scholar] [CrossRef]
- Butcher, D.L.; MacKinnon, K.; Bruce, A.; Gordon, C.; Koning, C. Experiences of pre-licensure or pre-registration health professional students and their educators in working with intra-professional teams: A qualitative systematic review. JBI Evid. Synth. 2017, 15, 1011–1056. [Google Scholar] [CrossRef]
- Ferrillo, H.; Watson, S.M. Using an Intraprofessional Global Immersion to Foster Role Formation in Nursing Students. J. Nurs. Educ. 2019, 58, 294–297. [Google Scholar] [CrossRef]
- Lankshear, S.; Rush, J.; Weeres, A.; Martin, D. Enhancing role clarity for the practical nurse. J. Nurs. Adm. 2016, 46, 300–307. [Google Scholar] [CrossRef]
- Yamashita, T.; Osawa, S.; Ota, K.; Minami, T.; Morisaki, Y.; Takahashi, Y.; Itatani, T.; Hara, S.; Tamai, T.; Fujiu, M. Interdisciplinary groups perform better than intradisciplinary groups in online group discussion activities. Med. Educ. Online 2021, 26, 1886649. [Google Scholar] [CrossRef]
- Leonard, B.; Shuhaibar, E.L.; Chen, R. Nursing student perceptions of intraprofessional team education using high-fidelity simulation. J. Nurs. Educ. 2010, 49, 628–631. [Google Scholar] [CrossRef] [PubMed]
- Barr, H.; Koppel, I.; Reeves, S.; Hammick, M.; Freeth, D.S. Effective Interprofessional Education: Argument, Assumption and Evidence (Promoting Partnership for Health); John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Freeth, D.; Reeves, S. Learning to work together: Using the presage, process, product (3P) model to highlight decisions and possibilities. J. Interprofessional Care 2004, 18, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Knight, E.P.; Prettyman, A.V. Rural telehealth team education for baccalaureate and nurse practitioner students. J. Nurs. Educ. 2020, 59, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, A.; Ball, S.; Connelly, S.; Hercinger, M.; Hanks, J.; Potthoff, M.; Banzhaf, S.; McCafferty, K. Intraprofessional simulation’s impact on advanced practice and baccalaureate student self-efficacy. Clin. Simul. Nurs. 2018, 16, 33–39. [Google Scholar] [CrossRef]
- George, T.P.; Murphy, P.F.; DeCristofaro, C.; Hucks, J.M. Student perceptions regarding collaborative intraprofessional nursing education. Nurse Educ. 2019, 44, 226–230. [Google Scholar] [CrossRef]
- Koutoukidis, G.P. The Role of Intra-Professional Education in Vocational and Higher Education; University of Canberra: Canberra, Australia, 2020. [Google Scholar]
- International Nursing Association for Clinical and Simulation Learning. Healthcare Simulation Standards of Best Practice. 2021. Available online: https://www.inacsl.org/healthcare-simulation-standards (accessed on 1 March 2023).
- Eppich, W.; Cheng, A. Promoting Excellence and Reflective Learning in Simulation (PEARLS): Development and rationale for a blended approach to health care simulation debriefing. Simul. Healthc. 2015, 10, 106–115. [Google Scholar] [CrossRef]
- Sigalet, E.; Donnon, T.; Grant, V. Undergraduate students’ perceptions of and attitudes toward a simulation-based interprofessional curriculum: The KidSIM ATTITUDES questionnaire. Simul. Healthc. 2012, 7, 353–358. [Google Scholar] [CrossRef]
- AlBalawi, I.; Alqahtani, J.S.; Al Ghamdi, S.S.; Aldhahir, A.M.; Alnasser, M.; Alqahtani, A.S.; AlRabeeah, S.M.; Alkhathami, M.; Almaqati, T.N.; AlDraiwiesh, I.A. Health Sciences Students’ Attitude, Perception, and Experience of Using Educational Simulation in Saudi Arabia: A Cross-Sectional Study. Nurs. Rep. 2022, 12, 620–628. [Google Scholar] [CrossRef]
- El-Gamal, S.; de Beer, J.; Sunari, D. Exploring the Effect of Trauma Care Simulation on Undergraduate Critical Care Nursing Students’ Attitude at a College of Nursing, in Jeddah—An Intervention Study. J. Educ. Pract. 2017, 8, 154–162. [Google Scholar]
- James, L.S.; Williams, M.L.; Camel, S.P.; Slagle, P. Nursing student’s attitudes toward teams in an undergraduate interprofessional mass casualty simulation. In Nursing Forum; Wiley Online Library: Hoboken, NJ, USA, 2021. [Google Scholar]
- Sanko, J.S.; Shekhter, I.; Mckay, M.; Gattamorta, K.; Birnbach, D.J. Interprofessional Simulation Olympics as a platform to assess team work knowledge acquisition. BMJ Simul. Technol. Enhanc. Learn. 2015, 1, 49. [Google Scholar] [CrossRef]
- Seale, J.; Ikram, S.; Whittingham, L.; Butchers, C. Combining medical, physiotherapy and nursing undergraduates in high-fidelity simulation: Determining students’ perceptions. BMJ Simul. Technol. Enhanc. Learn. 2019, 5, 108. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, C.A.; Lewis, J. Perceptions of interprofessional clinical simulation among medical and nursing students: A pilot study. J. Interprofessional Care 2015, 29, 504–506. [Google Scholar] [CrossRef] [PubMed]
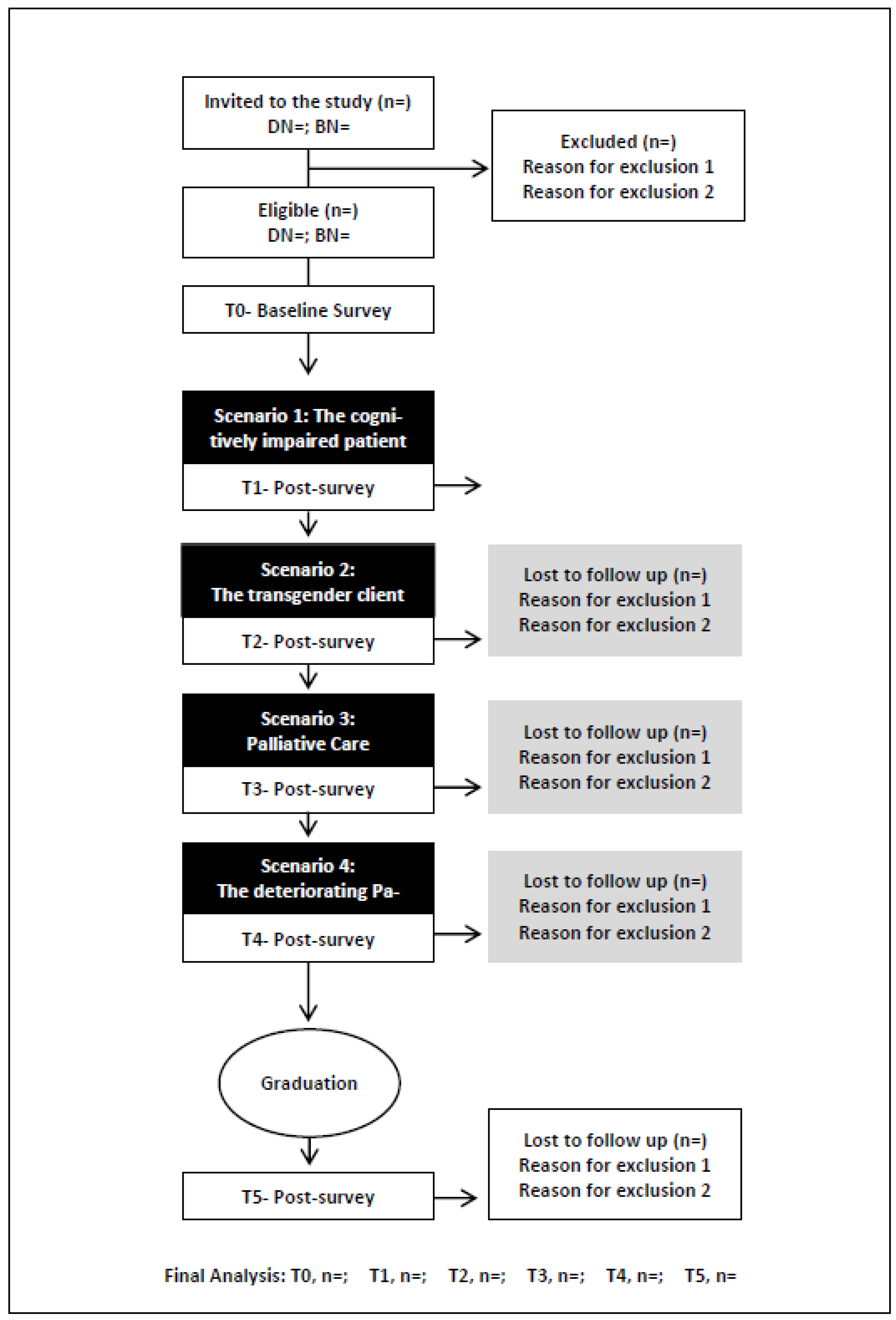
| Time | Timing | IaPL Intervention | Course | Year | Sem | Type of Data |
|---|---|---|---|---|---|---|
| T0 | 02/2023 | Pre-test | BN | 2 | 1 | Survey 1
|
| DN | 1 | 1 | ||||
| T1 | 06/2023 | Aged Care—The Cognitively Impaired Patient | BN | 2 | 1 | Survey 2
|
| DN | 1 | 1 | ||||
| T2 | 11/2023 | Mental Health—The Transgender Client | BN | 2 | 2 | Survey 3
|
| DN | 1 | 2 | ||||
| T3 | 06/2024 | Complex Care—Palliative Care | BN | 3 | 1 | Survey 4
|
| DN | 2 | 1 | ||||
| T4 | 11/2024 | Acute Care—The Deteriorating Patient | BN | 3 | 2 | Survey 5
|
| DN | 2 | 2 | ||||
| T5 | 06/2025 | Final Post-test 6 months post-graduation | BN | N/A | N/A | Survey 6
|
| DN | N/A | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiegaldie, D.; Weerasekara, I.; Shaw, L. Investigating the Effects of Intraprofessional Learning in Nursing Education: Protocol for a Longitudinal Study. Nurs. Rep. 2023, 13, 740-750. https://doi.org/10.3390/nursrep13020065
Kiegaldie D, Weerasekara I, Shaw L. Investigating the Effects of Intraprofessional Learning in Nursing Education: Protocol for a Longitudinal Study. Nursing Reports. 2023; 13(2):740-750. https://doi.org/10.3390/nursrep13020065
Chicago/Turabian StyleKiegaldie, Debra, Ishanka Weerasekara, and Louise Shaw. 2023. "Investigating the Effects of Intraprofessional Learning in Nursing Education: Protocol for a Longitudinal Study" Nursing Reports 13, no. 2: 740-750. https://doi.org/10.3390/nursrep13020065
APA StyleKiegaldie, D., Weerasekara, I., & Shaw, L. (2023). Investigating the Effects of Intraprofessional Learning in Nursing Education: Protocol for a Longitudinal Study. Nursing Reports, 13(2), 740-750. https://doi.org/10.3390/nursrep13020065







