Impact of Initial Emotional States and Self-Efficacy Changes on Nursing Students’ Practical Skills Performance in Simulation-Based Education
Abstract
1. Introduction
1.1. Simulation Training
1.2. Simulation and Learning Outcomes
1.3. Psychological Benefits of Simulation Training
1.4. Findings on Simulation and Self-Efficacy
1.5. Aim of the Study
2. Material and Methods
2.1. Participants
2.2. Measurements
2.3. Procedure
2.4. Analysis
2.5. Ethics
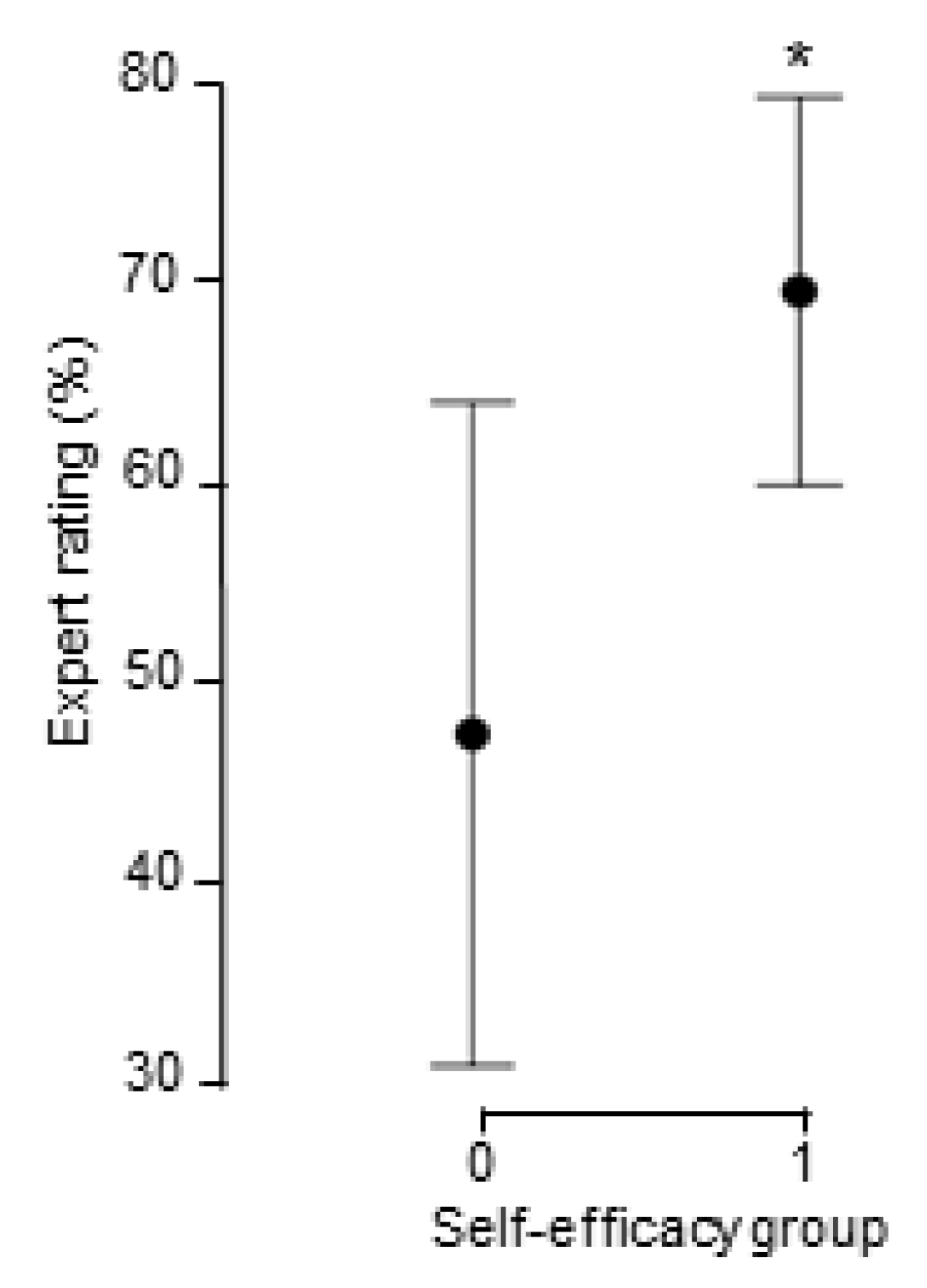
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jeffries, P.R. A framework for designing, implementing, and evaluating: Simulations used as teaching strategies in nursing. Nurs. Educ. Perspect. 2005, 26, 96–103. [Google Scholar]
- Alexander, M.; Durham, C.; Hooper, J.; Jeffries, P.; Goldman, N.; Kardong-Edgren, S.; Kesten, K.; Spector, N.; Tagliareni, E.; Radtke, B.; et al. NCSBN Simulation Guidelines for Prelicensure Nursing Programs. J. Nurs. Regulat. 2015, 6, 39–42. [Google Scholar] [CrossRef]
- Johnston, S.; Parker, C.N.; Fox, A. Impact of audio-visual storytelling in simulation learning experiences of undergraduate nursing students. Nurse Educ. Today 2017, 56, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Welch, T.; Carter, M. Deliberate Practice and Skill Acquisition in Nursing Practice. J. Contin. Educ. Nurs. 2018, 49, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Ward, P.; Hodges, N.J.; Williams, A.M. Deliberate practice and expert performance: Defining the path to excellence. In Skill Acquisition in Sport; Routledge: Abingdon, UK, 2004; pp. 255–282. [Google Scholar]
- Ericsson, K.A.; Whyte, J., IV; Ward, P. Expert performance in nursing: Reviewing research on expertise in nursing within the framework of the expert-performance approach. Adv. Nurs. Sci. 2007, 30, E58–E71. [Google Scholar] [CrossRef]
- Ericsson, K.A. Deliberate practice and acquisition of expert performance: A general overview. Acad. Emerg. Med. 2008, 15, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Exercise of Personal and Collective Efficacy in Changing Societies; Cambridge University Press: Cambridge, UK, 1995. [Google Scholar]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Franklin, A.E.; Lee, C.S. Effectiveness of simulation for improvement in self-efficacy among novice nurses: A meta-analysis. J. Nurs. Educ. 2014, 53, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Medley, C.F.; Claydell, R. Using simulation technology for undergraduate nursing education. J. Nurs. Educ. 2005, 44, 31–34. [Google Scholar] [CrossRef]
- Shin, S.; Park, J.-H.; Kim, J.-H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurs. Educ. Today 2015, 35, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Hegland, P.A.; Aarlie, H.; Strømme, H.; Jamtvedt, G. Simulation-based training for nurses: Systematic review and meta-analysis. Nurs. Educ. Today 2017, 54, 6–20. [Google Scholar] [CrossRef]
- Leigh, G.T. High-fidelity patient simulation and nursing students’ self-efficacy: A review of the literature. Int. J. Nurs. Educ. Scholarsh. 2008, 5, 1–17. [Google Scholar] [CrossRef]
- Kavanagh, D.J.; Bower, G.H. Mood and self-efficacy: Impact of joy and sadness on perceived capabilities. Cogn. Ther. Res. 1985, 9, 507–525. [Google Scholar] [CrossRef]
- Totawar, A.K.; Nambudiri, R. Mood and Self-Efficacy: The Moderation of Hedonic and Utilitarian Motivation. Hum. Resour. Dev. Rev. 2013, 13, 314–335. [Google Scholar] [CrossRef]
- Bindarwish, J.; Tenenbaum, G. Metamotivational and contextual effects on performance, self-efficacy, and shifts in affective states. Psychol. Sport Exerc. 2006, 7, 41–56. [Google Scholar] [CrossRef]
- Li, M.; Liu, Y.; Liu, L.; Wang, Z. Proactive personality and innovative work behavior: The mediating effects of affective states and creative self-efficacy in teachers. Curr. Psychol. 2017, 36, 697–706. [Google Scholar] [CrossRef]
- Karabacak, U.; Unver, V.; Ugur, E.; Kocatepe, V.; Ocaktan, N.; Ates, E.; Uslu, Y. Examining the effect of simulation based learning on self-efficacy and performance of first-year nursing students. Nurse Educ. Pract. 2019, 36, 139–143. [Google Scholar] [CrossRef]
- Goldenberg, D.; Andrusyszyn, M.A.; Iwasiw, C. The effect of classroom simulation on nursing students’ self-efficacy related to health teaching. J. Nurs. Educ. 2005, 44, 310–314. [Google Scholar] [CrossRef] [PubMed]
- Pike, T.; O’Donnell, V. The impact of clinical simulation on learner self-efficacy in pre-registration nursing education. Nurs. Educ. Today 2010, 30, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Roh, Y.S.; Lee, W.S.; Chung, H.S.; Park, Y.M. The effects of simulation-based resuscitation training on nurses’ self-efficacy and satisfaction. Nurs. Educ. Today 2013, 33, 123–128. [Google Scholar] [CrossRef]
- Tuttle, R.E. The Impact of Simulation in Nursing Education on the Self-Efficacy and Learner Satisfaction of Nursing Students. Ph.D. Thesis, Capella University, Minneapolis, MT, USA, 2009. [Google Scholar]
- Norman, J. Systematic review of the literature on simulation in nursing education. ABNF J. 2012, 23, 24–28. [Google Scholar]
- Cioffi, J. A study of the use of past experiences in clinical decision making in emergency situations. Int. J. Nurs. Stud. 2001, 38, 591–599. [Google Scholar] [CrossRef]
- Watters, C.; Reedy, G.; Ross, A.; Morgan, N.J.; Handslip, R.; Jaye, P. Does interprofessional simulation increase self-efficacy: A comparative study. BMJ Open 2015, 5, e005472. [Google Scholar] [CrossRef] [PubMed]
- Feingold, C.E.; Calaluce, M.; Kallen, M.A. Computerized patient model and simulated clinical experiences: Evaluation with baccalaureate nursing students. J. Nurs. Educ. 2004, 43, 156–163. [Google Scholar] [CrossRef]
- Scherer, Y.K.; Bruce, S.A.; Runkawatt, V. A comparison of clinical simulation and case study presentation on nurse practitioner students’ knowledge and confidence in managing a cardiac event. Int. J. Nurs. Educ. Scholarsh. 2007, 4, 22. [Google Scholar] [CrossRef]
- Bandura, A. The Evolution of Social Cognitive Theory; Oxford University Press: Oxford, UK, 2005; pp. 9–35. [Google Scholar]
- Lioce, L.; Meakim, C.H.; Fey, M.K.; Chmil, J.V.; Mariani, B.; Alinier, G. Standards of best practice: Simulation standard IX: Simulation design. Clin. Simul. Nurs. 2015, 11, 309–315. [Google Scholar] [CrossRef]
- Bradley, M.M.; Lang, P.J. Measuring emotion: The self-assessment manikin and the semantic differential. J. Behav. Ther. Exp. Psychiatry 1994, 25, 49–59. [Google Scholar] [CrossRef]
- Backs, R.W.; da Silva, S.P.; Han, K. A comparison of younger and older adults’ self-assessment manikin ratings of affective pictures. Exp. Aging Res. 2005, 31, 421–440. [Google Scholar] [CrossRef] [PubMed]
- Hoeppner, B.B.; Kelly, J.F.; Urbanoski, K.A.; Slaymaker, V. Comparative utility of a single-item versus multiple-item measure of self-efficacy in predicting relapse among young adults. J. Subst. Abus. Treat. 2011, 41, 305–312. [Google Scholar] [CrossRef]
- Gogol, K.; Brunner, M.; Goetz, T.; Martin, R.; Ugen, S.; Keller, U.; Fischbach, A.; Preckel, F. “My Questionnaire is Too Long!” The assessments of motivational-affective constructs with three-item and single-item measures. Contemp. Educ. Psychol. 2014, 39, 188–205. [Google Scholar] [CrossRef]
- Robins, R.W.; Hendin, H.M.; Trzesniewski, K.H. Measuring Global Self-Esteem: Construct Validation of a Single-Item Measure and the Rosenberg Self-Esteem Scale. Pers. Soc. Psychol. Bull. 2001, 27, 151–161. [Google Scholar] [CrossRef]
- Williams, G.; Smith, A. Using Single-Item Measures to Examine the Relationships between Work, Personality, and Well-Being in the Workplace. Psychology 2016, 7, 753–767. [Google Scholar] [CrossRef]
- Diamantopoulos, A.; Sarstedt, M.; Fuchs, C.; Wilczynski, P.; Kaiser, S. Guidelines for choosing between multi-item and single-item scales for construct measurement: A predictive validity perspective. J. Acad. Mark. Sci. 2012, 40, 434–449. [Google Scholar] [CrossRef]
- Riley, M.R.; Mohr, D.C.; Waddimba, A.C. The reliability and validity of three-item screening measures for burnout: Evidence from group-employed health care practitioners in upstate New York. Stress Health 2018, 34, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Turon, H.; Carey, M.; Boyes, A.; Hobden, B.; Dilworth, S.; Sanson-Fisher, R. Agreement between a single-item measure of anxiety and depression and the Hospital Anxiety and Depression Scale: A cross-sectional study. PLoS ONE 2019, 14, e0210111. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2013. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Chang, Y.-K.; Labban, J.; Gapin, J.; Etnier, J.L. The effects of acute exercise on cognitive performance: A meta-analysis. Brain Res. 2012, 1453, 87–101. [Google Scholar] [CrossRef]
- Cohen, S. Aftereffects of stress on human performance and social behavior: A review of research and theory. Psychol. Bull. 1980, 88, 82–108. [Google Scholar] [CrossRef]
- Dimaggio, G.; MacBeth, A.; Popolo, R.; Salvatore, G.; Perrini, F.; Raouna, A.; Osam, C.S.; Buonocore, L.; Bandiera, A.; Montano, A. The problem of overcontrol: Perfectionism, emotional inhibition, and personality disorders. Compreh. Psychiatry 2018, 83, 71–78. [Google Scholar] [CrossRef]
- Stewart, M.A.; De George-Walker, L. Self-handicapping, perfectionism, locus of control and self-efficacy: A path model. Pers. Individ. Differ. 2014, 66, 160–164. [Google Scholar] [CrossRef]
- Li, J.; Li, X.; Gu, L.; Zhang, R.; Zhao, R.; Cai, Q.; Lu, Y.; Wang, H.; Meng, Q.; Wei, H. Effects of Simulation-Based Deliberate Practice on Nursing Students’ Communication, Empathy, and Self-Efficacy. J. Nurs. Educ. 2019, 58, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Torkshavand, G.; Khatiban, M.; Soltanian, A.R. Simulation-based learning to enhance students’ knowledge and skills in educating older patients. Nurse Educ. Pract. 2020, 42, 102678. [Google Scholar] [CrossRef] [PubMed]
- Klein, G.; Ross, K.G.; Moon, B.M.; Klein, D.E.; Hoffman, R.R.; Hollnagel, E. Macrocognition. IEEE Intell. Syst. 2003, 18, 81–85. [Google Scholar] [CrossRef]
| Scenario | Required Action * | Learning Outcomes | Expert Evaluation Items |
|---|---|---|---|
| Preoperative | Information consultation before operation | Skills: Pre-operation skin care. Post-operation procedure, information about mobilization, elimination, pain, and nausea care | How successful was the student to provide information on skin preparation before the impending surgery? How successful was the student in providing information on the post-operative phase? |
| Postoperative | Observation and nursing measures | Knowledge: Pain evaluation NRS scaleSkills: Intravenous infusion administration for pain and nausea | How successful was the student in assessing the treatment of pain and nausea? How successful was the student in managing pain and nausea intravenous treatment? |
| Mobilization | Help the patient out of bed, walk a few steps and back into bed again | Knowledge: Pain prevention increasing patient activity Skills: Patient assistance through mobilization | How successful was the student at preventing pain when the patient was getting out of bed? How well did the student collaborate so that the patient finds the best way to get to the bedside? |
| Sepsis | Observation and nursing measures | Knowledge: Observation for suspicion of infection and sepsis development Skills: Blood culture orders and physician consultation | How well did the student control the identity and the blood transfusion form? How successfully did the student perform safe blood management using the right equipment? |
| Minimum | Maximum | Mean (M) | Standard Deviation (SD) | |
|---|---|---|---|---|
| SAM Mood | 2 | 9 | 5.55 | 1.68 |
| SAM Activation | 2 | 9 | 6.66 | 1.65 |
| SAM Control | 1 | 8 | 4.69 | 1.83 |
| SE pre | 20 | 90 | 58.07 | 16.61 |
| SE post | 10 | 90 | 61.64 | 21.18 |
| SE change | −50 | 50 | 6.20 | 27.98 |
| Expert score 1 | 0 | 100 | 55.56 | 27.64 |
| Expert score 2 | 0 | 90 | 59.26 | 28.81 |
| Expert average | 5 | 90 | 57.41 | 26.54 |
| 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|
| 1. SAM Mood | −0.353 | 0.451 * | 0.417 * | 0.196 | 0.098 | −0.223 |
| 2. SAM Activation | −0.602 ** | −0.337 | −0.066 | 0.228 | 0.332 * | |
| 3. SAM Control | 0.396 * | −0.079 | −0.288 | −0.627 ** | ||
| 4. SE pre | 0.686 ** | −0.241 | −0.073 | |||
| 5. SE post | 0.261 | 0.639 ** | ||||
| 6. Expert Average | 0.541 ** | |||||
| 7. SE change |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lugo, R.G.; Hjelmeland, I.; Hansen, M.T.; Haug, E.; Sütterlin, S.; Grønlien, H.K. Impact of Initial Emotional States and Self-Efficacy Changes on Nursing Students’ Practical Skills Performance in Simulation-Based Education. Nurs. Rep. 2021, 11, 267-278. https://doi.org/10.3390/nursrep11020026
Lugo RG, Hjelmeland I, Hansen MT, Haug E, Sütterlin S, Grønlien HK. Impact of Initial Emotional States and Self-Efficacy Changes on Nursing Students’ Practical Skills Performance in Simulation-Based Education. Nursing Reports. 2021; 11(2):267-278. https://doi.org/10.3390/nursrep11020026
Chicago/Turabian StyleLugo, Ricardo Gregorio, Inger Hjelmeland, Mette Tindvik Hansen, Erna Haug, Stefan Sütterlin, and Heidi Kristine Grønlien. 2021. "Impact of Initial Emotional States and Self-Efficacy Changes on Nursing Students’ Practical Skills Performance in Simulation-Based Education" Nursing Reports 11, no. 2: 267-278. https://doi.org/10.3390/nursrep11020026
APA StyleLugo, R. G., Hjelmeland, I., Hansen, M. T., Haug, E., Sütterlin, S., & Grønlien, H. K. (2021). Impact of Initial Emotional States and Self-Efficacy Changes on Nursing Students’ Practical Skills Performance in Simulation-Based Education. Nursing Reports, 11(2), 267-278. https://doi.org/10.3390/nursrep11020026







