Abstract
The human hemochromatosis protein HFE is encoded by the HFE gene and participates in iron regulation. The aim of this study was to detect the most frequent HFE gene mutations in a control population and in β-thalassemia trait (BTT) carriers, and to study their relationship with iron metabolism. Total blood count, hemoglobin electrophoresis at alkaline pH, HbA2 quantification, iron (Fe), total Fe binding capacity and ferritin were assayed. HFE gene mutations were analyzed by real-time PCR. A total of 119 individuals (69 normal and 50 BTT) were examined. In the control group, 9% (6/69) presented a codon 282 heterozygous mutation (C282Y), and 19% a codon 63 mutation (H63D) (13/69, 11 heterozygotes and 2 homozygotes). In the BTT group, 3 carriers (6%) were heterozygous for C282Y, 14 (28%) for H63D, 1 (2%) for a codon 65 mutation and 1 (2%) was H63D and C282Y double heterozygous. Control group Fe metabolism did not show significant differences (p > 0.05) according to whether or not they carried an HFE gene mutation; while the BTT group with and without HFE mutation showed higher Fe and ferritin than the control group (p < 0.05). However, no increases in iron parameters were detected in BTT carriers that simultaneously exhibited an H63D mutation compared to BTT subjects without a mutation. Therefore, the iron metabolism alterations observed in BTT carriers could not be attributed to the presence of HFE gene mutations. It is likely that BTT individuals have other genetic modifiers that affect their iron balance.
1. Introduction
Iron is an essential trace element required as a component of molecules sensing, transporting, and storing oxygen; as well as enzymes involved in oxidation and reduction of substrates during energy production, intermediate metabolism, and the generation of reactive oxygen or nitrogen species for host defense. The impressive advances in our knowledge of iron metabolism have translational implications for the diagnosis and treatment of iron disorders. This large group of pathological condition includes both genetic and acquired disorders, which can be classified as iron deficiency (absolute or functional) and iron overload (primary and secondary). Iron overload may occur in genetic disorders and may be primary, such as the different types of haemochromatosis; or be secondary to increased iron absorption accompanied by hereditary anemia with ineffective erythropoiesis, such as beta-thalassemia [1].
Thalassemia is a hereditary anemia resulting from defects in hemoglobin (Hb) production. Hemolysis and ineffective erythropoiesis together cause the anemia that occurs in thalassemia. Beta (β)-thalassemia, which is caused by a decrease in the production of β-globin chains, affects multiple organs and is associated with considerable morbidity and mortality. More than 300 β-thalassemia alleles have now been characterized, but only about 40 account for 90% or more of all β-thalassemia cases worldwide. The vast majority of β-thalassemia is caused by point mutations and, rarely, by deletions. Patients with β-thalassemia have been typically categorized as minor, major, or intermedia on the basis of α-globin or β-globin chain imbalance, severity of anemia, and clinical picture at presentation. β-thalassemia minor (trait or carrier) represents the heterozygous inheritance of a β-thalassemia mutation, with patients often having clinically asymptomatic microcytic anemia [2].
Tissue iron overload is the most important complication of β-thalassemia and is a major focus of therapeutic management. Blood transfusion is a comprehensive source of iron loading for β-thalassemia patients. Nevertheless, iron overload also occurs in patients who have not received transfusions such as patients suffering from thalassemia intermedia [3]. Hepcidin concentrations are suppressed in β-thalassemia major, intermedia and minor [4,5,6]. This fact allows excessive iron absorption and development of systemic iron overload [4].
Hereditary hemochromatosis (HH) is the most common genetic iron overload disorder among Caucasians. Although multiple mutations can lead to the clinical syndrome, the most common mutations are those in the HFE gene [7]. In 1996, Feder and colleagues used positional cloning to identify HFE, which is linked to the major histocompatibility complex (MHC) on chromosome 6p [8].
The HFE protein is required for normal regulation of hepatic synthesis of hepcidin, the main controller of iron metabolism [1]. Common HFE mutations account for almost 90% of hemochromatosis phenotypes in whites of Western European descent [8].
The most prevalent disease-causing HFE mutation in the general population is the 845G polymorphism, which causes a p.Cys282Tyr amino acid substitution (C282Y) in the HFE protein. Homozygosity for this single missense substitution (p.Cys282Tyr) is responsible for between 60 and 100% of cases of HH among European populations [8]. HFE gene sequencing approaches have identified additional HFE mutations with different pathological impacts. These include the amino acid alterations H63D and S65C [9].
Although the causes of iron accumulation in subjects with β-thalassemia are clear, the fact that this accumulation occurs in greater proportions in some patients suggests a possible association between HH and β-thalassemia. The presence of HFE gene mutations in patients affected with β-thalassemia leads to the expression of phenotypic hematological characteristics different from those that would be observed with only primary mutations of the β-globin gene.
The objective of this study was to compare the results of blood testing in a group of subjects with β-thalassemia trait (BTT) and normal individuals with and without common HFE mutations, and to investigate the relationship between HFE mutations and iron metabolism.
2. Materials and Methods
2.1. Subjects
A prospective cross-sectional analytical study was carried out. The population was composed of apparently healthy individuals and patients with BTT, who were diagnosed in the Laboratory of Hematology of the Instituto de Bioquímica Aplicada of the Universidad Nacional de Tucumán (UNT), during the period 2016–2018. All patients and controls signed an informed consent form. The study protocol and the declaration of informed consent were approved by the Comité de Bioética de la Facultad de Medicina of UNT.
2.2. Hematological and Molecular Analysis
A blood sample was collected with EDTA-K2, and a fraction without anticoagulant for serum determinations. Blood count was performed using a Sysmex KX-21N hematological counter (Kobe, Japan). β-thalassemia diagnosis was made by Hb electrophoresis at alkaline pH, and HbA2 quantification through microcolumn chromatography (ByoSystems, Barcelona, Spain). Iron metabolism was assayed by quantifying serum iron (Fe), and total iron binding capacity (TIBC) by a colorimetric method (Wiener lab, Rosario, Argentina). Ferritin was measured by electrochemiluminescence (COBAS, Roche, Basel, Switzerland). Transferrin saturation (SAT) was calculated with the following formula: SAT [%] = (Fe/TIBC) × 100
Isolation of genomic DNA was carried out with the High Pure PCR Template Preparation Kit (Roche Diagnostics) from 200 μL of whole blood anticoagulated with EDTA-K2. Characterization of mutations in the β-globin gene and the HFE gene was carried out using real-time polymerase chain reaction (PCR) with FRET probes (fluorescence resonance energy transfer). PCR, melt curves, and subsequent analysis were performed on the LightCycler 2.0 equipment (Roche). A 587 bp region of the β-globin gene was amplified for β-thalassemia mutations [10]:
- −
- Forward Primer: 5′-GCTGTC ATCACTTAGACCTCA-3′.
- −
- Reverse Primer: 5′-CACAGTGCAGCTCA CTCAG-3′.
Two combinations of hybridization probes were used according to the following scheme [11]: SET A: Mutations: IVSI-110 G → A; Cd39 C → T; SET B: Mutations: IVSI-1 G → A; IVSI-5 G → A; IVSI-6 T → C.
HFE gene mutations were detected with the following pairs of primers and probes [12]:
C282Y mutation, forward primer: CTGGATAACCTTGGCTGTACC, and reverse primer: GGCTCTCATCAGTCACATACC.
H63D/S65C mutations, forward primer: GTCTCCAGGTTCACACTCTC and reverse primer: CCATAATAGTCCAGAAGTCAACAG.
2.3. Statistical Analysis
Statistical analysis was carried out using SPSS 20.0. The results were reported as median and range. Mann–Whitney U tests were used for the comparisons and a significance level of p < 0.05 was adopted.
3. Results
In total, 69 apparently healthy subjects (48 women and 21 men) aged 21–64 years, and 50 BTT carriers (31 women and 19 men) aged 16–79 years were studied. Table 1 shows the HFE gene mutations detected in the population. HFE mutations were present in 28% (19/69, 95% CI = 18–39%) of the control subjects, and in 38% (19/50, 95% CI = 28–54%) of the BTT group (Table 1). No significant difference was observed between control and BTT frequency of HFE mutation (p > 0.05).

Table 1.
Mutations in the HFE gene in β-thalassemia trait and apparently healthy subjects.
Table 2 shows the relationship between ethnicity and β-thalassemia and HFE mutations identified in BTT carriers. Italian origin predominated in the BTT population, followed by Spanish and Arabic. The three origins represented almost 90% of the total population. The rest were of Creole descent, and from France, Bulgaria and Germany. Most of the HFE mutations were detected in Italian-descent individuals.

Table 2.
Relationship between ethnic origin and mutations detected in heterozygous β-thalassemia subjects.
The most frequent β-thalassemia mutation was IVSI-1 (32%, 16/50), followed by IVSI-110 (28%, 14/50), CD39 (20%, 10/50), IVSII-745 (2%, 1/50), and IVSII-1 (2%, 1/50). In eight (16%) BTT subjects, the mutation could not be determined. There were no significant differences (p > 0.05) in the iron parameters according to β-thalassemia mutation type (β0 or β+), except for TIBC which was higher in the β+ group with HFE gene mutation (Table 3).

Table 3.
Influence of the presence of HFE gene mutation on iron metabolism according β-thalassemia mutation type.
In the BTT group, it was observed that transferrin saturation was higher in subjects of Italian and Arab origin compared to those of Spanish origin (p < 0.05) which did not have mutations in the HFE gene (Table 2). In contrast, serum iron, TIBC and ferritin levels did not show significant changes (p > 0.05).
Table 4 displays the hematological study results. As expected, significant differences were detected (p < 0.05) in red blood parameters between BTT male and female groups compared to controls without BTT. Hematocrit and MCHC showed no significant differences (p > 0.05) between the male groups. In those groups without HFE mutation, serum iron saturation and ferritin were higher in the control male group and the BTT female group than the control female group (p < 0.05). In those groups with HFE mutation, only ferritin showed a significant difference in the BTT female group compared to the control female group (p < 0.05). Iron parameters did not differ in BTT carriers based the presence or absence of HFE mutation (p > 0.05).

Table 4.
Hematological parameters according to HFE gene mutation presence in the study groups.
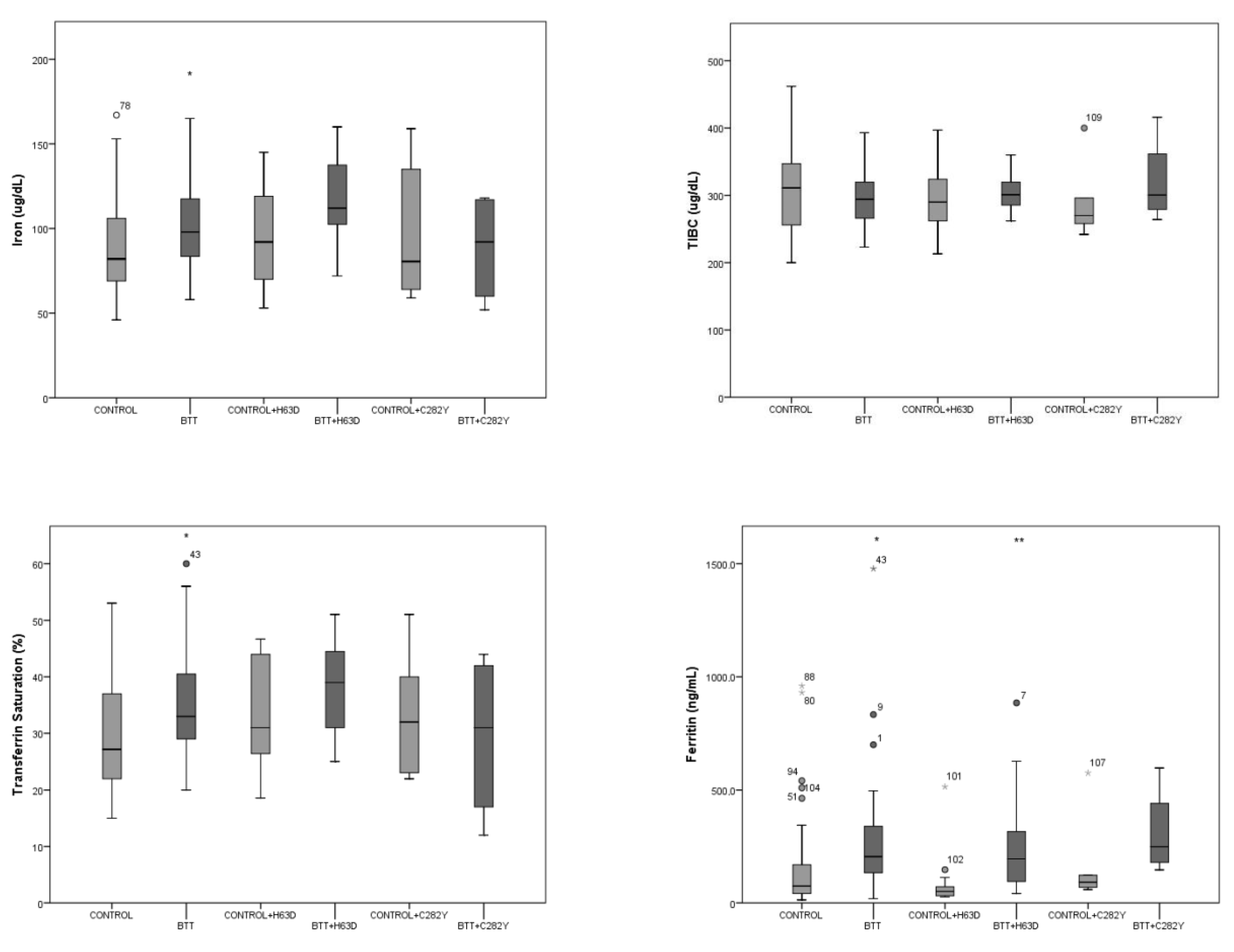
Figure 1 shows levels of serum iron (Fe), TIBC, transferrin saturation (TS) and ferritin in control and BTT groups according HFE mutation type. Iron metabolism analysis in the apparently healthy group did not reveal significant differences (p > 0.05) according to presence or absence of HFE gene mutation. The BTT group demonstrated higher Fe, ST and ferritin than controls (p < 0.05). The BTT group with H63D mutation only exhibited an increase in ferritin compared to controls with the same mutation (p < 0.05). Only one male BTT carrier without an HFE gene mutation showed ferritin higher than 1000 ng/mL. The only BTT patient with the C282Y/H63D genotype and the two control H63D homozygotes were females and did not show alterations in iron metabolism. Comparisons according to the type of mutation (C282Y or H63D) with respect to sex could not be made due to insufficient numbers of subjects in each group.
Figure 1.
Iron parameters according the presence of HFE mutation in the groups under study. Abbreviations: TIBC, total iron binding capacity. * p < 0.05 compared to control; ** p < 0.05 compared control + H63D. The number case is included in outliers.
4. Discussion
β-thalassemia trait is characterized by ineffective erythropoiesis, which can induce excess iron absorption and cause iron overload. The interaction of β-thalassemia with hemochromatosis, which is caused in most cases by mutations in the HFE gene, can further exacerbate iron overload. Previous work has described an increase in iron, transferrin and/or ferritin levels in β thalassemia carriers that also had an H63D mutation, compared to those that did not carry this mutation [13,14,15,16]. However, other publications showed that the simultaneous presence of β-thalassemia and an HFE gene mutation did not modify serum ferritin levels [17,18,19,20].
Iron metabolism analysis revealed that β-thalassemia carriers had higher Fe, ST and ferritin than apparently healthy subjects. When comparing β-thalassemia subjects with an H63D mutation to controls with same mutation, an increase in ferritin level was observed in the first group. Recent publications have found an increase in ferritin levels in β-thalassemia major individuals with an H63D mutation [21,22]. In present work, this rise could not be attributed to the presence of the HFE gene mutation, since it was shown that BTT carriers displayed higher ferritin levels than healthy subjects. Another study previously described this effect in both BTT women and men [23,24]. Increased iron storage in BTT, as reflected by significantly higher concentrations of ferritin, would be a consequence of higher iron absorption [23].
As with other studies, our comparison between β0 and β+ carriers with or without HFE gene mutation did not detect significant differences in parameters related to iron, except TIBC, which was significantly increased in the β+ group with HFE mutation [19,20].
On the other hand, the presence of HFE gene mutation in the control population did not increase iron parameters. This fact has already been observed by other authors [25,26]. However, there are authors that affirm the opposite [27,28]. Jackson et al. detected significant differences in serum iron, TIBC and transferrin saturation between blood donors with and without HFE mutation; but H63D heterozygotes and C282Y heterozygous females did not show significant differences in ferritin levels when compared with wild type donors. In the present work, the analysis of iron probably did not exhibit significant differences because most of the participants heterozygous for the H63D mutation were female. Serum iron and ferritin are influenced by age, sex, diet and disease, as well as by biological variation among individuals and by methodological differences [29].
The spectrum of β-thalassemia mutations was different to that previously reported for Tucumán [11]. In our study, the IVSI-110 mutation was the most frequent, whereas the CD39 mutation was most prevalent in the first molecular study conducted in the region. IVSI-110 was present mainly in Italian-origin carriers. The frequency of IVSI-110 in Italy varies among the different geographical regions, appearing in some places with a greater or similar frequency as CD39 [30,31]. Additionally, the Arab contribution to IVSI-110’s origin in the Tucumán population cannot be discounted, since it is the most prevalent in Syria and Lebanon [32,33]. In addition, ethnicity was an important factor in the analysis of HFE genotype/phenotype relationships. Thus, in both Italian- and Arab-origin BTT individuals, it was shown that transferrin saturation was increased compared to Spanish-origin individuals in whom HFE mutation was not detected. In a Spanish study, the C282Y heterozygote, H63D heterozygote and homozygote, and H63D/S65C compound heterozygote genotypes were associated with increased transferrin saturation relative to wild type in the general population [26].
Other studies have shown that HFE gene mutations are common among β-thalassemia carriers compared with normal controls [34,35]. This was not confirmed in present work since there was no significant increase in HFE mutation frequency in the BTT group. The presence of the C282Y/H63D genotype was related to iron overload [36], but the only BTT patient with this genotype did not display iron elevation. Jaing et al. found that β-thalassemia carriers who are homozygous for the H63D variant have higher serum ferritin levels than carriers without the variant [37]. However, in the present study there was no iron metabolism disturbance in H63D homozygotes. This effect could be a consequence of the low penetrance of this genotype, and that other cofactors that contribute to iron overload would be usually present, such as iron intake, alcohol intake, tobacco use, and male gender [7,26].
A limitation of our study is that other mutations that could increase iron deposits were not analyzed in current work, such as mutations in hemojuvelin, hepcidin, transferrin receptor 2 and ferroportin genes [38]. Additionally, acquired factors such as dietary habits, blood donations, pregnancies, menopause, and malabsorption syndromes, among others, could influence the iron metabolism results [20].
5. Conclusions
There is a wide spectrum of phenotypes in β-thalassemia, and there are population-specific genetic modifiers that influence them. These include mutations in the HFE gene [37]. In BTT subjects of Italian and Arab origin, only a significant increase in transferrin saturation was detected, compared to subjects of Spanish origin. Remarkably, in the latter, mutations in the HFE gene were not identified. On the other hand, the present work detected no increase in iron parameters in β-thalassemia carriers that simultaneously exhibited HFE mutation compared to those BTT subjects without HFE mutation. In addition, apparently healthy subjects with HFE mutation did not show differences in iron status. However, BTT individuals displayed higher ferritin levels than controls in both groups, with and without HFE mutation. Because of this, there may be other genetic modifiers present in β-thalassemia individuals that could aggravate their ferric balance.
Author Contributions
Conceptualization and methodology, M.E.M., B.A.I. and S.S.L.; formal analysis (sample collection, DNA extraction, beta-thalassemia diagnosis and HFE genotyping), N.S.A.A., C.H., M.M.T. and M.E.L.A.; data curation, M.E.M., N.S.A.A. and S.S.L.; writing—original draft preparation, M.E.M. and S.S.L.; writing—review and editing, S.S.L. and B.A.I.; supervision, project administration and funding acquisition, M.E.M., B.A.I. and S.S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Consejo de Investigaciones de la Universidad Nacional de Tucumán (CIUNT 26/D520) and Alberto J. Roemmers Foundation.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Comité de Bioética de la Facultad de Medicina of Universidad Nacional de Tucumán, Argentina.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, S.S.L., upon reasonable request.
Acknowledgments
The authors thank biochemist specialist Guillermo Vechetti and Laboratorio Tucumán for the use of its molecular biology equipment.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Camaschella, C.; Pagani, A. Advances in understanding iron metabolism and its crosstalk with erythropoiesis. Br. J. Haematol. 2018, 182, 481–494. [Google Scholar] [CrossRef]
- Taher, A.T.; Weatherall, D.J.; Cappellini, M.D. Thalassaemia. Lancet 2018, 391, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Ribeil, J.A.; Arlet, J.B.; Dussiot, M.; Moura, I.C.; Courtois, G.; Hermine, O. Ineffective erythropoiesis in β- thalassemia. Sci. World J. 2013, 394295. [Google Scholar]
- Jones, E.; Pasricha, S.R.; Allen, A.; Evans, P.; Fisher, C.A.; Wray, K.; Premawardhena, A.; Bandara, D.; Perera, A.; Webster, C.; et al. Hepcidin is suppressed by erythropoiesis in hemoglobin E β-thalassemia and β-thalassemia trait. Blood 2015, 125, 873–880. [Google Scholar] [CrossRef] [PubMed]
- El Beshlawy, A.; Alaraby, I.; Abdel Kader, M.S.; Ahmed, D.H.; Abdelrahman, H.E. Study of serum hepcidin in hereditary hemolytic anemias. Hemoglobin 2012, 36, 555–570. [Google Scholar] [CrossRef]
- Nemeth, E. Hepcidin in beta-thalassemia. Ann. N. Y. Acad. Sci. 2010, 1202, 31–35. [Google Scholar] [CrossRef]
- Powell, L.W.; Seckington, R.C.; Deugnier, Y. Haemochromatosis. Lancet 2016, 388, 706–716. [Google Scholar] [CrossRef] [PubMed]
- Feder, J.N.; Gnirke, A.; Thomas, W.; Tsuchihashi, Z.; Ruddy, D.A.; Basava, A.; Dormishian, F.; Domingo, R., Jr.; Ellis, M.C.; Fullan, A.; et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat. Genet. 1996, 13, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Hollerer, I.; Bachmann, A.; Muckenthaler, M.U. Pathophysiological consequences and benefits of HFE mutations: 20 years of research. Haematologica 2017, 102, 809–817. [Google Scholar] [CrossRef]
- Vrettou, C.; Traeger-Synodinos, J.; Tzetis, M.; Malamis, G.; Kanavakis, E. Rapid screening of multiple beta-globin gene mutations by real-time PCR on the LightCycler: Application to carrier screening and prenatal diagnosis of thalassemia syndromes. Clin. Chem. 2003, 49, 769–776. [Google Scholar] [CrossRef]
- Lazarte, S.S.; Mónaco, M.E.; Haro, A.C.; Jiménez, C.L.; Ledesma Achem, M.E.; Issé, B.A. Molecular characterization and phenotypical study of β-thalassemia in Tucumán, Argentina. Hemoglobin 2014, 38, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Moysés, C.B.; Moreira, E.S.; Asprino, P.F.; Guimarães, G.S.; Alberto, F.L. Simultaneous detection of the C282Y, H63D and S65C mutations in the hemochromatosis gene using quenched-FRET real-time PCR. Braz. J. Med. Biol. Res. 2008, 41, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Melis, M.A.; Cau, M.; Deidda, F.; Barella, S.; Cao, A.; Galanello, R. H63D mutation in the HFE gene increases iron overload in β-thalassemia carriers. Haematologica. 2002, 87, 242–245. [Google Scholar]
- Martins, R.; Picanço, I.; Fonseca, A.; Ferreira, L.; Rodrigues, O.; Coelho, M.; Seixas, T.; Miranda, A.; Nunes, B.; Costa, L.; et al. The role of HFE mutations on iron metabolism in beta-thalassemia carriers. J. Hum. Genet. 2004, 49, 651–655. [Google Scholar] [CrossRef]
- Nadkarni, A.H.; Singh, A.A.; Colaco, S.; Hariharan, P.; Colah, R.B.; Ghosh, K. Effect of the hemochromatosis mutations on iron overload among the indian β thalassemia carriers. J. Clin. Lab. Anal. 2016, 31, e22054. [Google Scholar] [CrossRef]
- AlFadhli, S.; Salem, M.; Shome, D.K.; Mahdi, N.; Nizam, R. The effects of HFE polymorphisms on biochemical parameters of iron status in Arab beta-thalassemia patients. Indian J. Hematol. Blood Transfus. 2017, 33, 545–551. [Google Scholar] [CrossRef]
- Jazayeri, M.; Bakayev, V.; Adibi, P.; Haghighi Rad, H.F.; Zakeri, H.; Kalantar, E.; Zali, M.R. Frequency of HFE gene mutations in Iranian beta thalassaemia minor patients. Eur. J. Haematol. 2003, 71, 408–411. [Google Scholar] [CrossRef] [PubMed]
- Mellouli, F.; El Borgi, W.; Kaabi, H.; Ben Hassen, E.; Sassi, R.; Hmida, H.; Cherif, G.; Maamar, M.; Zouari, B.; Boukef, K.; et al. HFE gene mutations in Tunisian major β-thalassemia and iron overload. Transfus. Clin. Et Biol. 2006, 13, 353–357. [Google Scholar]
- Estevão, I.F.; Peitl Junior, P.; Bonini-Domingos, C.R. Serum ferritin and transferrin saturation levels in β0 and β+ thalassemia patients. Genet Mol. Res. 2011, 10, 632–639. [Google Scholar] [CrossRef]
- López-Escribano, H.; Ferragut, J.F.; Parera, M.M.; Guix, P.; Castro, J.A.; Ramon, M.M.; Picornell, A. Effect of co-inheritance of β-thalassemia and hemochromatosis mutations on iron overload. Hemoglobin 2012, 36, 85–92. [Google Scholar] [CrossRef]
- Enein, A.A.; El Dessouky, N.A.; Mohamed, K.S.; Botros, S.K.A.; Abd El Gawad, M.F.; Hamdy, M.; Dyaa, N. Frequency of hereditary hemochromatosis (HFE) gene mutations in egyptian beta thalassemia patients and its relation to iron overload. Maced. J. Med. Sci. 2016, 4, 226–231. [Google Scholar] [CrossRef]
- Soltanpour, M.S.; Kambiz Davari, K. The correlation of cardiac and hepatic hemosiderosis as measured by T2*MRI technique with ferritin levels and hemochromatosis gene mutations in Iranian patients with beta thalassemia major. Oman Med. J. 2018, 33, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Fucharoen, S.; Winichagoon, P.; Sirankapracha, P.; Zeder, C.; Gowachirapant, S.; Judprasong, K.; Tanno, T.; Miller, J.L.; Hurrell, R.F. Iron metabolism in heterozygotes for hemoglobin E (HbE), alpha-thalassemia 1, or beta-thalassemia and in compound heterozygotes for HbE/beta-thalassemia. Am. J. Clin Nutr. 2008, 88, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Mehta, B.C.; Pandya, B.G. Iron status of beta thalassemia carriers. Am. J. Hematol. 1987, 24, 137–141. [Google Scholar] [CrossRef]
- Adams, P.C.; Reboussin, D.M.; Barton, J.C.; McLaren, C.E.; Eckfeldt, J.H.; McLaren, G.D.; Sholinsky, P.; Walker, A.P.; Gordeuk, V.R. Hemochromatosis and Iron Overload Screening (HEIRS) Study Research Investigators. Hemochromatosis and iron-overload screening in a racially diverse population. N. Engl. J. Med. 2005, 352, 1769–1778. [Google Scholar] [CrossRef]
- Aranda, N.; Viteri, F.E.; Montserrat, C.; Arija, V. Effects of C282Y, H63D, and S65C HFE gene mutations, diet, and life-style factors on iron status in a general Mediterranean population from Tarragona, Spain. Ann. Hematol. 2010, 89, 767–773. [Google Scholar] [CrossRef]
- Kaczorowska-Hac, B.; Luszczyk, M.; Antosiewicz, J.; Ziolkowski, W.; Adamkiewicz-Drozynska, E.; Mysliwiec, M.; Milosz, E.; Kaczor, J.J. HFE gene mutations and iron status in 100 healthy polish children. J. Pediatr. Hematol. Oncol. 2017, 39, e240–e243. [Google Scholar] [CrossRef]
- Jackson, H.A.; Carter, K.; Darke, C.; Guttridge, M.G.; Ravine, D.; Hutton, R.D.; Napier, J.A.; Worwood, M. HFE mutations, iron deficiency and overload in 10,500 blood donors. Br. J. Haematol. 2001, 114, 474–484. [Google Scholar] [CrossRef] [PubMed]
- Worwood, M. Iron deficiency anaemia and iron overload. In Dacie and Lewis Practical Haematology, 10th ed.; Meloni, D., Oberle, K., Saltzberg, D., Eds.; Churchil Livingstone Elsevier: Philadelphia, PA, USA, 2006; pp. 131–160. [Google Scholar]
- Rosatelli, M.C.; Tuveri, T.; Scalas, M.T.; Leoni, G.B.; Sardu, R.; Faà, V.; Meloni, A.; Pischedda, M.A.; Demurtas, M.; Monni, G.; et al. Molecular screening and fetal diagnosis of beta-thalassemia in the Italian population. Hum. Genet. 1992, 89, 585–589. [Google Scholar]
- Rigoli, L.; Meo, A.; Miceli, M.R.; Alessio, K.; Caruso, R.A.; La Rosa, M.A.; Salpietro, D.C.; Ricca, M.; Barberi, I. Molecular analysis of beta-thalassaemia patients in a high incidence area of southern Italy. Clin. Lab. Haematol. 2001, 23, 373–378. [Google Scholar] [CrossRef]
- Murad, H.; Moassas, F.; Ghoury, I.; Mukhalalaty, Y. Haplotype Analysis of Three Common β-Thalassemia Mutations in Syrian Patients. Hemoglobin 2018, 42, 302–305. [Google Scholar] [CrossRef]
- Makhoul, N.J.; Wells, R.S.; Kaspar, H.; Shbaklo, H.; Taher, A.; Chakar, N.; Zalloua, P.A. Genetic heterogeneity of Beta thalassemia in Lebanon reflects historic and recent population migration. Ann. Hum. Genet. 2005, 69, 55–66. [Google Scholar] [CrossRef]
- Madani, H.A.; Afify, R.A.; Abd El-Aal, A.A.; Salama, N.; Ramy, N. Role of HFE gene mutations on developing iron overload in beta-thalassaemia carriers in Egypt. East Mediterr. Health J. 2011, 17, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, T.M.; Souza, F.P.; Jardim, A.C.; Cordeiro, J.A.; Pinho, J.R.; Sitnik, R.; Estevão, I.F.; Bonini-Domingos, C.R.; Rahal, P. HFE gene mutations in Brazilian thalassemic patients. Braz. J. Med. Biol. Res. 2006, 39, 1575–1580. [Google Scholar] [CrossRef]
- Beutler, E. The significance of the 187G (H63D) mutation in hemochromatosis. Am. J. Hum. Genet. 1997, 61, 762–764. [Google Scholar] [CrossRef] [PubMed]
- Jaing, T.H.; Chang, T.Y.; Chen, S.H.; Lin, C.W.; Wen, Y.C.; Chiu, C.C. Molecular genetics of β-thalassemia: A narrative review. Medicine 2021, 100, e27522. [Google Scholar] [CrossRef]
- Kawabata, H. The mechanisms of systemic iron homeostasis and etiology, diagnosis, and treatment of hereditary hemochromatosis. Int. J. Hematol. 2018, 107, 31–43. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).