Preschool Hearing Screening: Nineteen Years of the Coração Delta Project in Campo Maior, Portugal
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
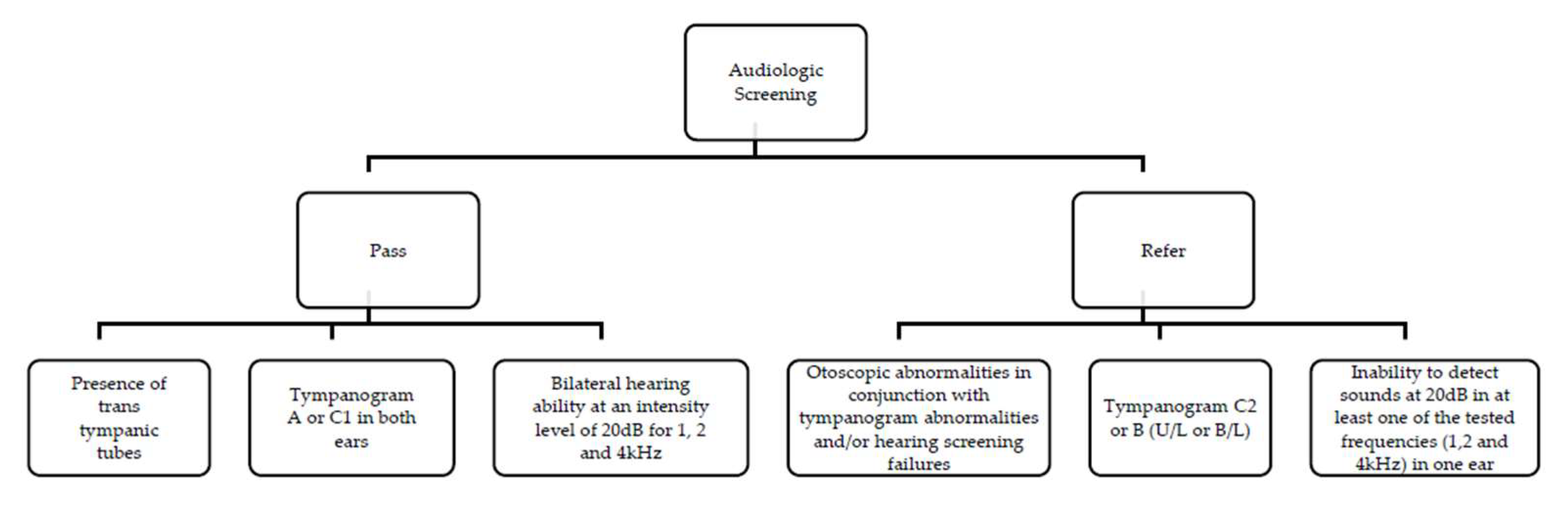
2.2. Procedure
- –
- The presence of transtympanic tubes, accompanied by a recommendation to continue consulting their otorhinolaryngologist (ENT).
- –
- A tympanogram results classified as type A or C1 in both ears.
- –
- Bilateral hearing ability at an intensity level of 20 dB for frequencies of 1, 2, and 4 kHz.
- –
- Observed alterations during otoscopy, in conjunction with tympanogram abnormalities and/or hearing screening failures.
- –
- A tympanogram results classified as type C2 or B in one or both ears.
- –
- Inability to detect sounds at 20 dB in at least one of the tested frequencies in one ear.
2.3. Statistical Analysis
3. Results
3.1. Screening Results
3.2. Medical Referral
3.3. Association of Medical Otoscopy Findings with Tympanogram Types
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davidse, N.J.; de Jong, M.T.; Bus, A.G.; Huijbregts, S.C.J.; Swaab, H. Cognitive and Environmental Predictors of Early Literacy Skills. Read Writ. 2011, 24, 395–412. [Google Scholar] [CrossRef] [PubMed]
- Rayner, K.; Foorman, B.R.; Perfetti, C.A.; Pesetsky, D.; Seidenberg, M.S. How Psychological Science Informs the Teaching of Reading. Psychol. Sci. Public Interest 2001, 2, 31–74. [Google Scholar] [CrossRef] [PubMed]
- Hand, E.D.; Lonigan, C.J.; Puranik, C.S. Prediction of kindergarten and first-grade reading skills: Unique contributions of preschool writing and early-literacy skills. Read Writ. 2024, 37, 25–48. [Google Scholar] [CrossRef]
- Share, D.L. Blueprint for a universal theory of learning to read: The Combinatorial Model. Bluepr. A Univers. Theory Learn. Read Comb. Model 2025, 60, 2. [Google Scholar] [CrossRef]
- Furgoni, A.; Martin, C.D.; Stoehr, A. A cross linguistic study on orthographic influence during auditory word recognition. Sci. Rep. 2025, 15, 8374. [Google Scholar] [CrossRef] [PubMed]
- Ehri, L.C. Development of Sight Word Reading: Phases and Findings. In The Science of Reading: A Handbook; Snowling, M.J., Hulme, C., Eds.; Blackwell Publishing: Singapore, 2007; pp. 135–154. [Google Scholar]
- Boothroyd, A. Speech Perception in the Classroom. In Handbook of Acoustic Accessibility—Best Practices for Listening, Learning, and Literacy in the Classroom; Smaldino, J.J., Flexer, C., Eds.; Thieme: New York, NY, USA; Stuttgart, Germany, 2012; pp. 18–33. [Google Scholar]
- Klatte, M.; Bergström, K.; Lachmann, T. Does noise affect learning? A short review on noise effects on cognitive performance in children. Front Psychol. 2013, 4, 578. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gordon, K.R.; Grieco-Calub, T.M. Children build their vocabularies in noisy environments: The necessity of a cross-disciplinary approach to understand word learning. Wiley Interdiscip. Rev. Cogn. Sci. 2024, 15, e1671. [Google Scholar] [CrossRef] [PubMed]
- McFadden, B.; Pittman, A. Effect of minimal hearing loss on children’s ability to multitask in quiet and in noise. Lang. Speech Hear. Serv. Sch. 2008, 39, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Porter, H.; Bess, F.H. Children with Unilateral Hearing Loss. In Comprehensive Handbook of Pediatric Audiology; Seewald, R., Tharpe, A.M., Eds.; University of Western Ontario: London, ON, Canada; Plural Publishing, Inc.: San Diego, CA, USA, 2011; pp. 175–192. [Google Scholar]
- Tharpe, A.M. Permanent Minimal and Mild Bilateral Hearing Loss in Children: Implications and Outcomes. In Comprehensive Handbook of Pediatric Audiology; Seewald, R., Tharpe, A.M., Eds.; University of Western Ontario: London, ON, Canada; Plural Publishing, Inc.: San Diego, CA, USA, 2011; pp. 193–202. [Google Scholar]
- World Health Organization. Hearing Screening: Considerations for Implementation; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- American Speech-Language-Hearing Association. Panel on Audiologic Assessment. In Guidelines for Audiologic Screening; The Association: Rockville, MD, USA, 1997. [Google Scholar]
- Skarżyński, H.; Piotrowska, A. Screening for Pre-School and School-Age Hearing Problems: European Consensus Statement. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 120–121. [Google Scholar] [CrossRef] [PubMed]
- Zielhuis, G.A.; Rach, G.H.; Broek, P.V.D. The Occurrence of Otitis Media with Effusion in Dutch Pre-School Children. Clin. Otolaryngol. Allied Sci. 1990, 15, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, R.M.; Shin, J.J.; Schwartz, S.R.; Coggins, R.; Gagnon, L.; Hackell, J.M.; Hoelting, D.; Hunter, L.L.; Kummer, A.W.; Payne, S.C.; et al. Clinical Practice Guideline: Otitis Media with Effusion (Update). Otolaryngol.-Head Neck Surg. Off. J. Am. Acad. Otolaryngol.-Head Neck Surg. 2016, 154 (Suppl. S1), S1–S41. [Google Scholar] [CrossRef] [PubMed]
- Vanneste, P.; Page, C. Otitis media with effusion in children: Pathophysiology, diagnosis, and treatment. A review. J. Otol. 2019, 14, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Mackey, A.R.; Persson, A.; Uhlén, I. Pre-school hearing screening is necessary to detect childhood hearing loss after the newborn period: A study exploring risk factors, additional disabilities, and referral pathways. Int. J. Audiol. 2025, 64, 80–88. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Audiology. Clinical Practice Guidelines: Childhood Hearing Screening; American Academy of Audiology: Reston, VA, USA, 2011. [Google Scholar]
- Hunter, L.L.; Blankenship, C.M. Middle ear measurement. In Comprehensive Handbook of Pediatric Audiology; Tharpe, A.M., Seewald, R., Eds.; Plural Publishing: San Diego, CA, USA, 2017; pp. 449–473. [Google Scholar]
- Dows, M.; Northern, J. Hearing in Children; Williams&Wilkins: London, UK, 2014. [Google Scholar]
- Dahlgren, G.; Whitehead, M. Concepts and Principles for Tackling Social Inequities in Health: Levelling Up Part I and Part II; WHO Regional Office for Europe: Copenhagen, Denmark, 2006. [Google Scholar]
- Entidade Reguladora da Saúde. Direito à proteção da saúde–O Serviço Nacional de Saúde–Universalidade; Entidade Reguladora da Saúde (ERS): Porto, Portugal, 2021. [Google Scholar]
- Furtado, C.; Pereira, J. Equidade e Acesso aos Cuidados de Saúde-Documento de Trabalho; Escola Nacional de Saúde Pública, Universidade Nova de Lisboa: Lisbon, Portugal, 2010. [Google Scholar]
- Coração Delta—Associação de Solidariedade Social. Coração Delta—Associação de Solidariedade Social. Available online: https://www.coracaodelta.com (accessed on 2 June 2025).
- Instituto Nacional de Estatística. Available online: https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=ine_main (accessed on 2 June 2025).
- Pilka, E.; Jedrzejczak, W.W.; Kochanek, K.; Pastucha, M.; Skarzynski, H. Assessment of the Hearing Status of School-Age Children from Rural and Urban Areas of Mid-Eastern Poland. Int. J. Environ. Res. Public Health 2021, 18, 4299. [Google Scholar] [CrossRef] [PubMed]
- Anwar, K. Otitis media with effusion: Accuracy of tympanometry in detecting fluid in the middle ears of children at myringotomies. Pak. J. Med. Sci. 2016, 32, 466–470. [Google Scholar] [CrossRef] [PubMed]
- Fiellau-Nikolajsen, M. Tympanometry and middle ear effusion: A cohort-study in three-year-old children. Int. J. Pediatr. Otorhinolaryngol. 1980, 2, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Robler, S.K.; Platt, A.; Jenson, C.D.; Inglis, S.M.; Hofstetter, P.; Ross, A.A.; Wang, N.-Y.; Labrique, A.; Gallo, J.J.; Egger, J.R.; et al. Changing the Paradigm for School Hearing Screening Globally: Evaluation of Screening Protocols From Two Randomized Trials in Rural Alaska. Ear Hear. 2023, 44, 877–893. [Google Scholar] [CrossRef] [PubMed]
- Brodie, K.D.; David, A.P.; Kriss, H.; Chan, D.K. Outcomes of an Early Childhood Hearing Screening Program in a Low-Income Setting. JAMA Otolaryngol. Head Neck Surg. 2022, 148, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Lü, J.; Huang, Z.; Yang, T.; Li, Y.; Mei, L.; Xiang, M.; Chai, Y.; Li, X.; Li, L.; Yao, G.; et al. Screening for delayed-onset hearing loss in preschool children who previously passed the newborn hearing screening. Int. J. Pediatr. Otorhinolaryngol. 2011, 75, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
| N | % | |
|---|---|---|
| Children passed screening | 758 | 71.0 |
| Children referred to ENT | 310 | 29.0 |
| –With unilateral changes | 137 | 12.7 |
| –With bilateral changes | 173 | 16.3 |
| Tympanogram alterations | ||
| –Unilateral | 104 | 9.7 |
| –Bilateral | 81 | 7.6 |
| –Type B tympanogram in both ears | 81 | 7.6 |
| Tympanostomy tubes present | 12 | 1.2 |
| Frequency | Right Ear | Left Ear |
|---|---|---|
| 1 kHz | 58 (50.9%) | 50 (44.6%) |
| 2 kHz | 34 (29.8%) | 35 (31.5%) |
| 4 kHz | 45 (39.5%) | 43 (38.7%) |
| N | % | |
|---|---|---|
| U/L Tympanogram | 104 | 9.7 |
| U/L Hearing Screening | 9 | 0.8 |
| U/L Tympanogram + Hearing Screening | 24 | 2.2 |
| B/L Tympanogram | 81 | 7.6 |
| B/L Hearing Screening | 3 | 0.3 |
| B/L Tympanogram + Hearing Screening (U/L) | 31 | 2.9 |
| B/L Tympanogram + Hearing Screening (B/L) | 51 | 4.8 |
| B/L Hearing Screening + Tympanogram (U/L) | 7 | 0.7 |
| N | % | |
|---|---|---|
| ENT Consultation | 123 | 56.7 |
| Monitoring | 30 | 13.8 |
| Medication | 20 | 9.2 |
| Discharge | 19 | 8.8 |
| Other Consultation(s) | 16 | 7.4 |
| Wax Removal | 5 | 2.3 |
| Speech Therapy | 4 | 1.8 |
| Total | 217 | 100.0 |
| Medical Otoscopy | Type A (N = 42) | Type C1 (N = 60) | Type C2 (N = 159) | Type B (N = 173) |
|---|---|---|---|---|
| Normal | 36 (86.4%) | 50 (83.3%) | 85 (53.5%) | 33 (19.1%) |
| Otitis Media with Effusion | 2 (4.8%) | 3 (5.0%) | 13 (8.2%) | 91 (52.6%) |
| Acute Otitis Media | 1 (2.4%) | 0 (0.0%) | 3 (1.9%) | 8 (4.6%) |
| Tympanic Depression | 0 (0.0%) | 3 (5.0%) | 23 (14.5%) | 11 (6.4%) |
| Cerumen | 2 (4.8%) | 2 (3.3%) | 11 (6.9%) | 22 (12.7%) |
| Tympanosclerosis | 0 (0.0%) | 0 (0.0%) | 2 (1.3%) | 0 (0.0%) |
| Tympanic Perforation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (0.6%) |
| Eustachian Tube Dysfunction | 1 (2.4%) | 2 (3.3%) | 19 (11.9%) | 7 (4.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reis, C.; Monteiro, L.; Monteiro, C.; Pereira, J.; Teixeira, J.; Mendes, J.; Pereira, M.; Barrocas, M.; Gomes, D.; Serrano, M. Preschool Hearing Screening: Nineteen Years of the Coração Delta Project in Campo Maior, Portugal. Audiol. Res. 2025, 15, 104. https://doi.org/10.3390/audiolres15040104
Reis C, Monteiro L, Monteiro C, Pereira J, Teixeira J, Mendes J, Pereira M, Barrocas M, Gomes D, Serrano M. Preschool Hearing Screening: Nineteen Years of the Coração Delta Project in Campo Maior, Portugal. Audiology Research. 2025; 15(4):104. https://doi.org/10.3390/audiolres15040104
Chicago/Turabian StyleReis, Cláudia, Luísa Monteiro, Conceição Monteiro, Joana Pereira, Joana Teixeira, João Mendes, Mariana Pereira, Magda Barrocas, Dionísia Gomes, and Margarida Serrano. 2025. "Preschool Hearing Screening: Nineteen Years of the Coração Delta Project in Campo Maior, Portugal" Audiology Research 15, no. 4: 104. https://doi.org/10.3390/audiolres15040104
APA StyleReis, C., Monteiro, L., Monteiro, C., Pereira, J., Teixeira, J., Mendes, J., Pereira, M., Barrocas, M., Gomes, D., & Serrano, M. (2025). Preschool Hearing Screening: Nineteen Years of the Coração Delta Project in Campo Maior, Portugal. Audiology Research, 15(4), 104. https://doi.org/10.3390/audiolres15040104






