Unilateral Triple Canal Repositioning Maneuver: Principles and Design
Abstract
1. Introduction
2. Materials and Methods
- Ampullary segment: the segment of a semicircular canal closest to its ampule.
- Crural segment (called the “non-ampullary arm” in some of the literature): the segment of a semicircular canal closest to its crus (the singular crus for the horizontal canal; the common crus for the anterior and posterior canals).
- Apex (called the “vertex” in some of the literature): the segment of a semicircular canal between its ampullary segment and crural segment.
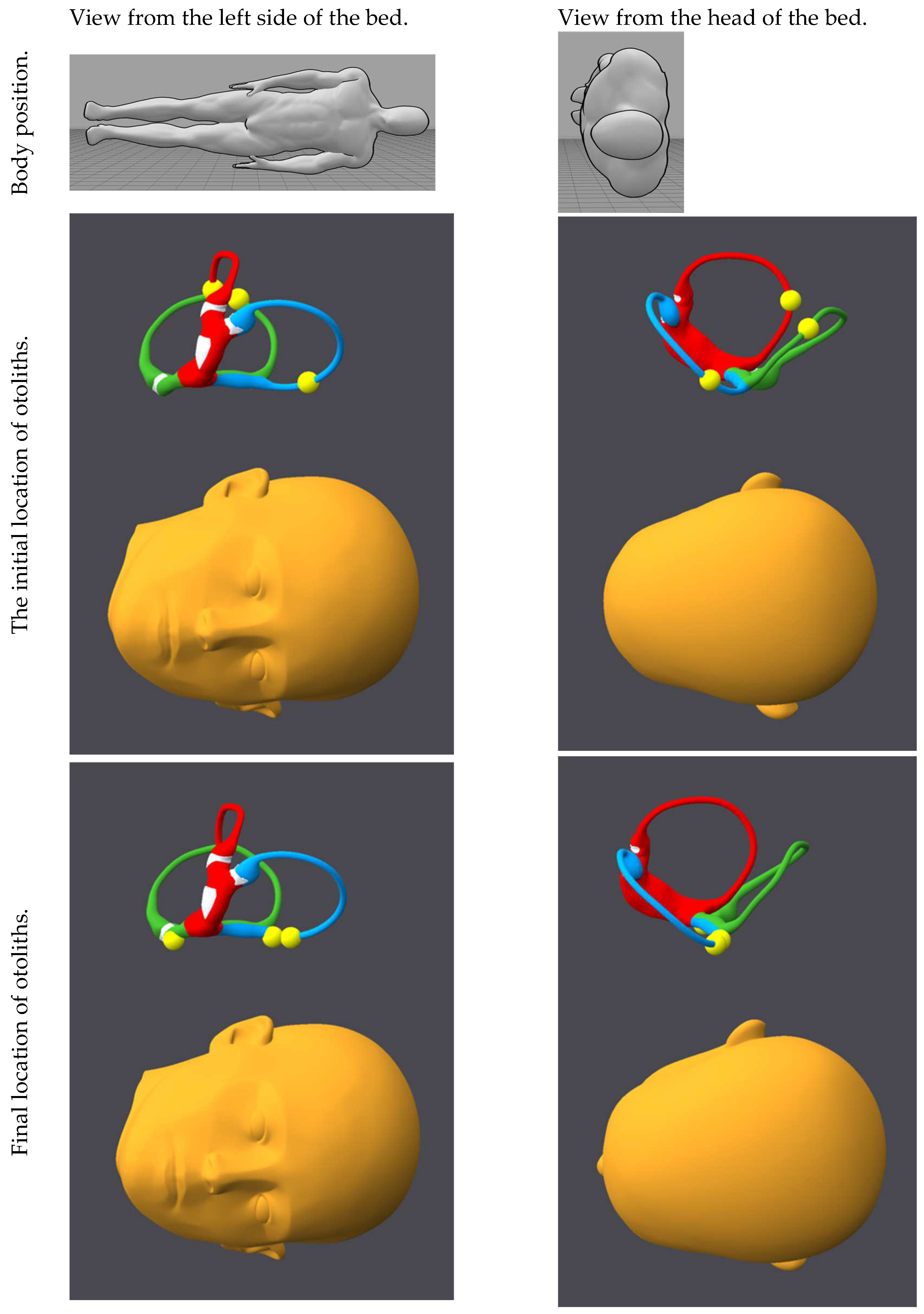
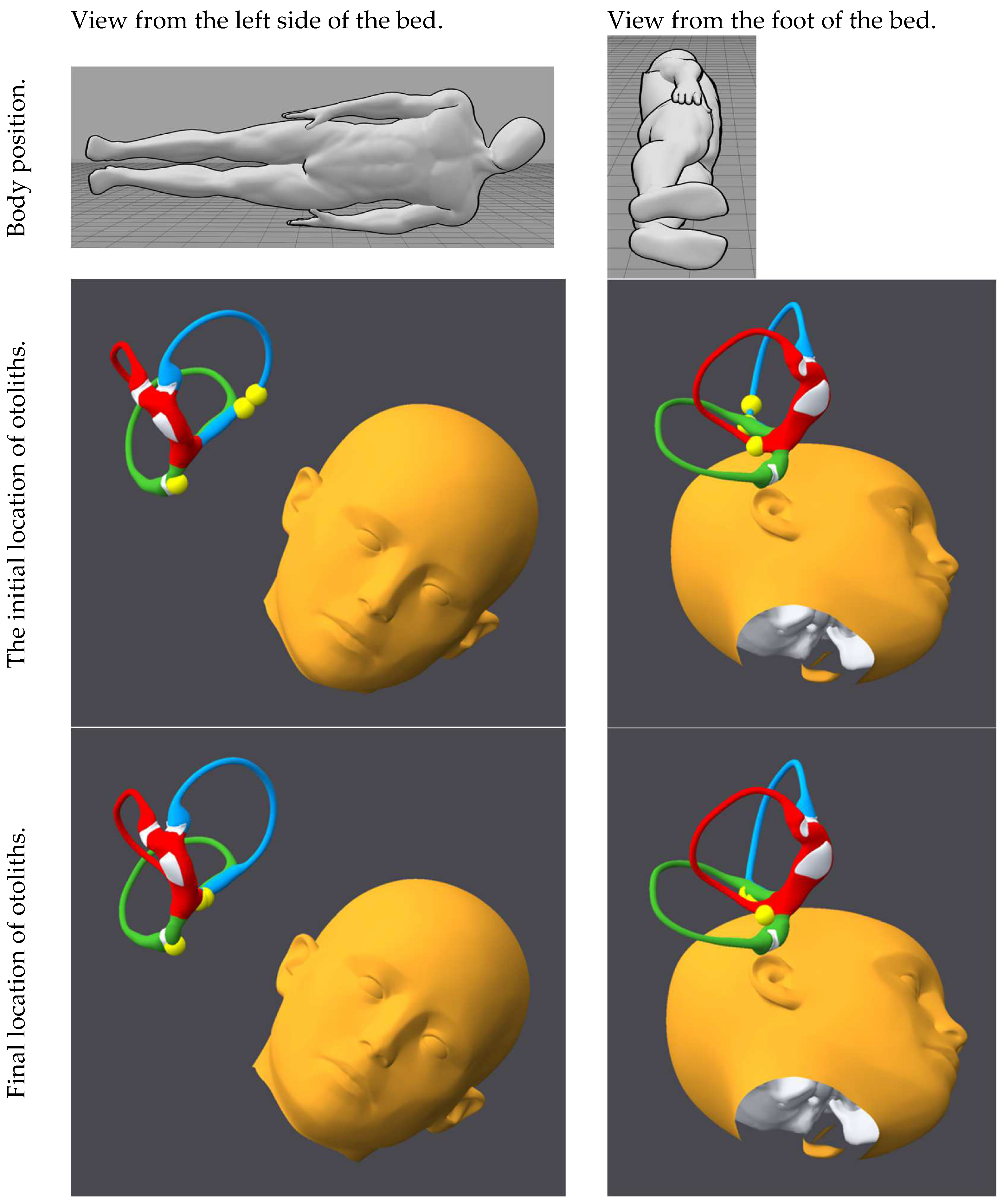
- We assume that the initial conditions are the “worst case scenario” in which the otoliths in each canal are in the ampullary segment (farthest away from the desired location).
- In any given position, otoliths should preferably advance toward the crus, or at least remain still, but not retreat toward the ampule. To avoid retreat toward the ampule, the plane of a given canal should be either vertical or oblique but never horizontal. However, if the initial conditions are not the “worst case scenario” mentioned above (for example, the otoliths are initially closer to the crural segment of a canal than to the ampullary segment), then the initial positions will provoke some “retreat” of canaliths toward the apex, but subsequent positions will coax them back toward the crural segment.
- Given the approximately orthogonal dispositions of the canal planes, in any given position, only one canal plane can be vertical, while the other two canal planes will be oblique. If two canals are vertical, then the third is horizontal, which risks permitting otoliths of that canal to retreat toward the ampule.
- Side-lying position, as might be used during a supine roll test or logroll maneuver, with the rostrocaudal axis of the head parallel to the rostrocaudal axis of the trunk and the head’s mid-sagittal plane parallel to the surface of the earth. One could also substitute a position in which the patient is supine but with the head rotated 90° to the side (i.e., with the sagittal plane of the head parallel to the coronal plane of the trunk). For shorthand, we refer to this as the Lempert position in recognition of its use in the Lempert role [49].
- Oblique head-hanging position: position in which the patient is supine, with the neck extended (such that the head is hanging off the edge of the table) and the head turned 45° to one side (i.e., halfway between the sagittal plane and the coronal plane). For shorthand, we refer to this as the Dix–Hallpike position, a commonly used eponymous designation [69].
- The penultimate position of this maneuver does not have an eponymous designation. It is a side-lying position, but with the patient’s neck laterally flexed (away from gravity) by 45° such that the uppermost ear is closer to the shoulder, similar to the penultimate position of the Rahko maneuver [60] or of the modified Epley maneuver [48]. Note that in this position, the common crus is nearly vertical, which helps prevent reflux into the anterior and posterior canals.
3. Results
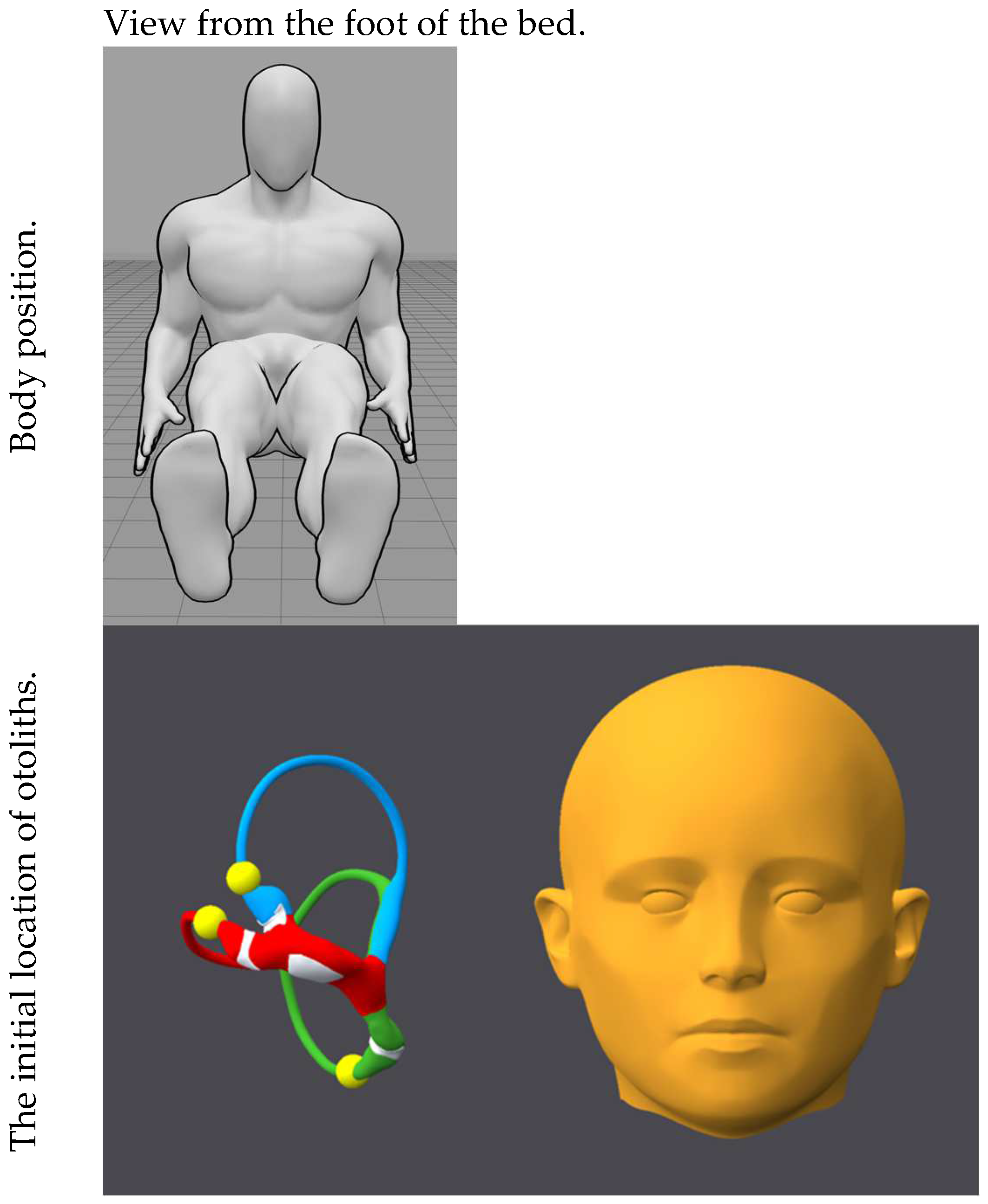
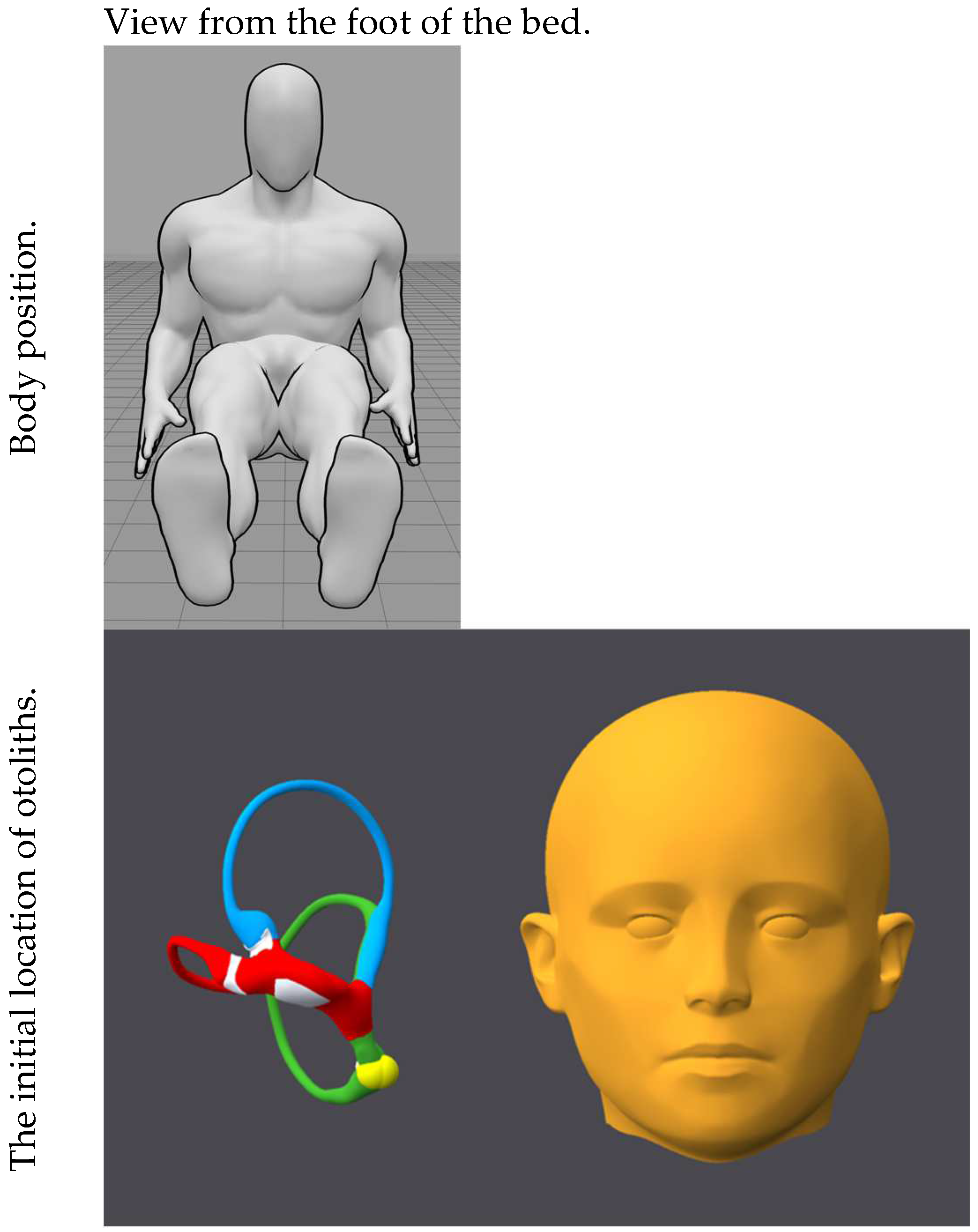
- Neutral seated position.
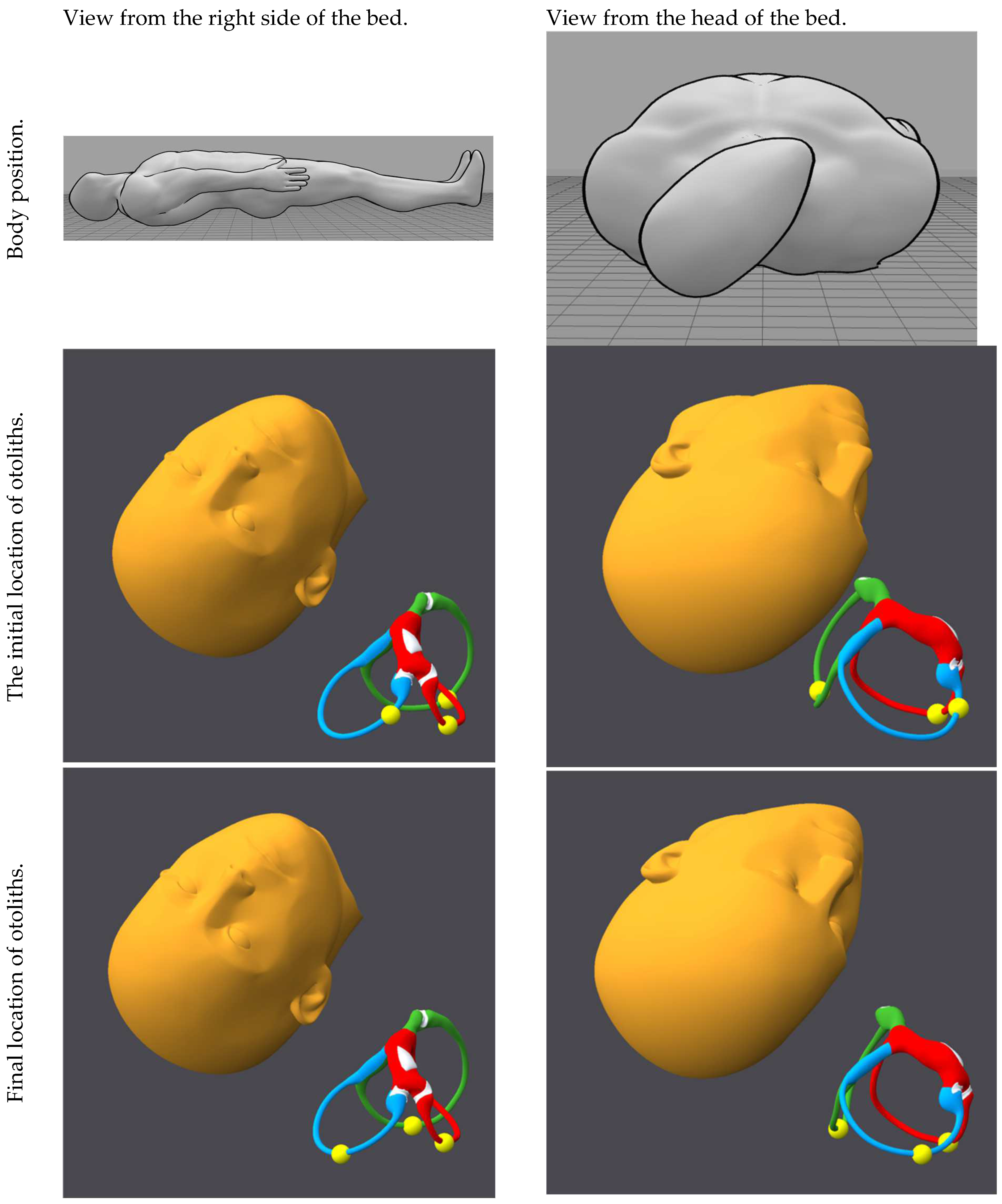
- Side-lying position (Lempert position) on the right side.
- Oblique head-hanging position (Dix–Hallpike position) on the right side.
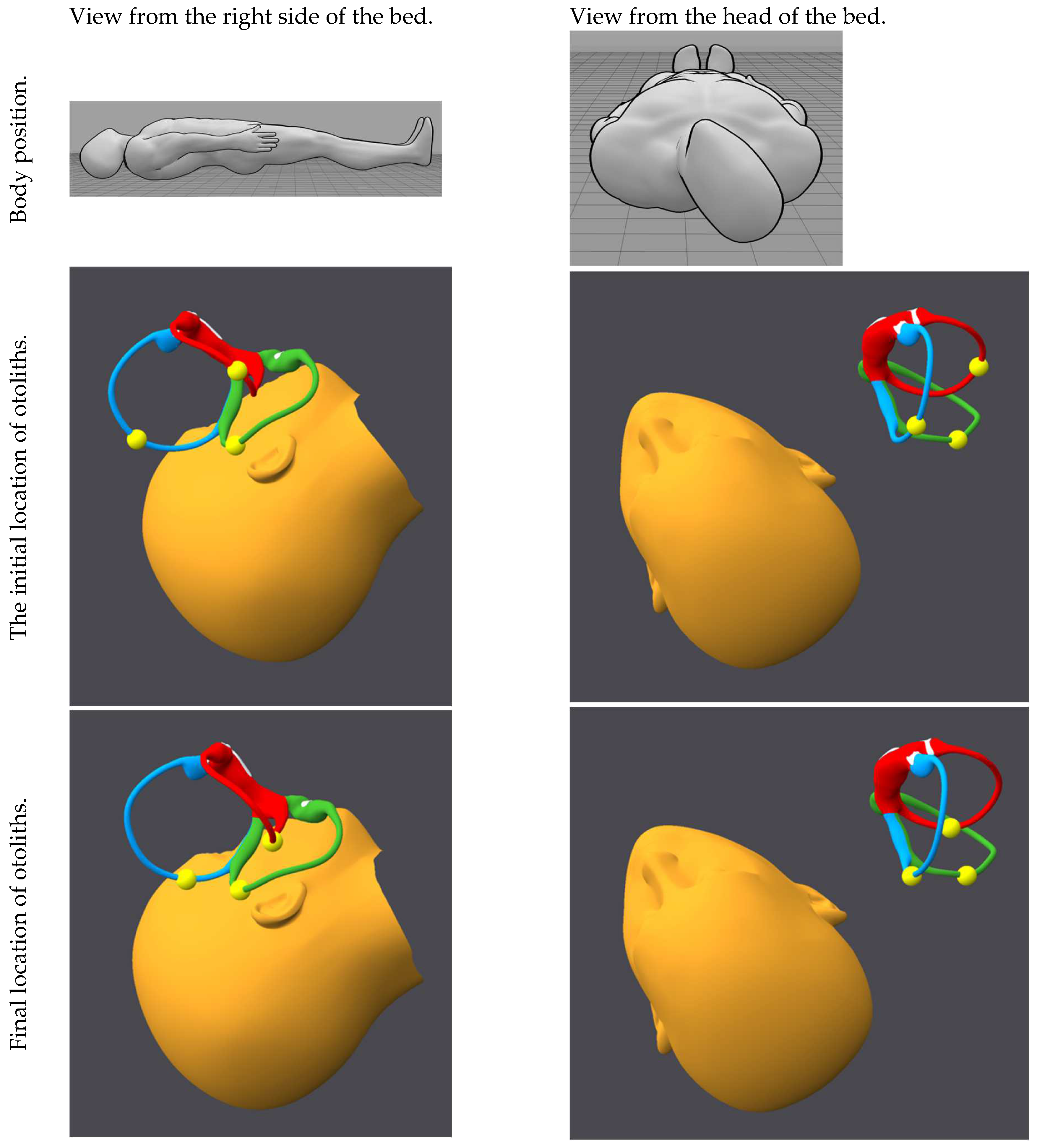
- Midline head-hanging position (Rose position).
- Oblique head-hanging position (Dix–Hallpike position) on the left side.
- Side-lying position (Lempert position) on the left side.
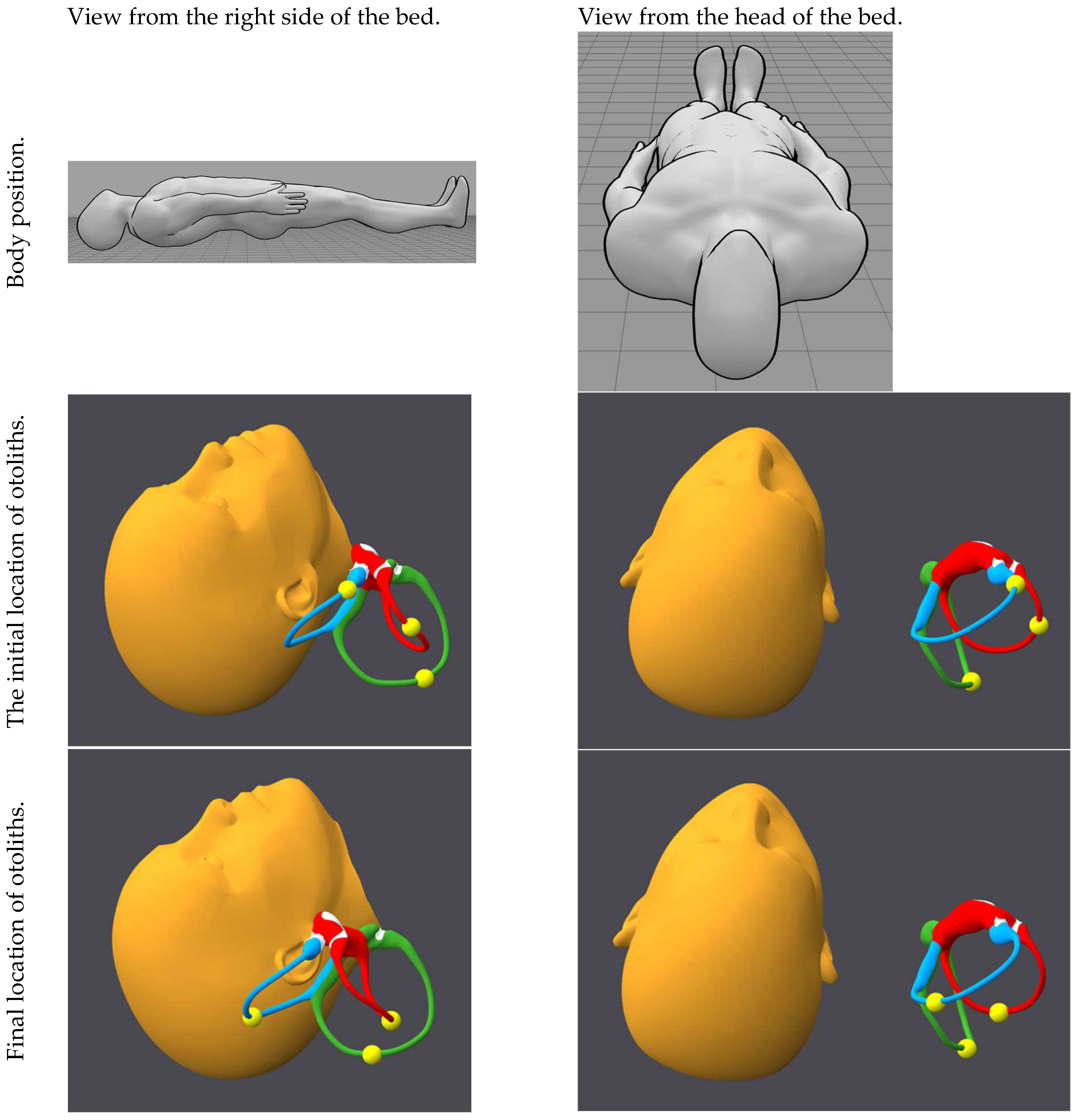
- Lie on the left side with the head angled upward (neck laterally flexed such that the right ear is inclined toward the right shoulder). One reason for including this intermediate position (rather than going directly to the neutral seated position listed below) is that otoliths near the apex of the posterior canal are more likely to be coaxed toward the crus.
- Neutral seated position.
4. Discussion
- For any given canal, its plane is vertically oriented at some point during this maneuver, offering the greatest likelihood for gravity to cause maximum transit of otoliths.
- At other points in the maneuver, that canal plane is oblique, which may enable additional (desirable) progress of the otolith through the canal toward the crural segment but at least will prevent the (undesirable) retreat of otoliths toward the ampule.
- Pausing at each intermediate position (breaking up the total movement) provides an opportunity for otoliths to settle in the most dependent portion of the canal, reducing the likelihood of otolith retreat.
- In no position is any canal plane parallel with the earth’s surface. This reduces the risk of otolith retreat.
- While there is debate regarding the precise statistics of canals affected by BPPV, there is broad agreement that posterior canal BPPV is the most common variant of BPPV [76]. A patient with posterior canal BPPV will usually complain of symptoms when lying on or when rolling onto the affected side. Thus, if a patient describes symptoms typical of BPPV when lying on or when rolling toward a particular side, then it is reasonable to lateralize treatment (provisionally) to that side.
- BPPV usually (though not invariably) recurs on the same side, so if a patient has a prior documented history of BPPV on a particular side, then it is reasonable to lateralize treatment (provisionally) to that side.
- An ear affected by other diseases [77], such as labyrinthitis [78], vestibular neuritis [79], or Meniere’s disease [80], is more susceptible to developing BPPV. Therefore, if a patient who describes symptoms typical of BPPV also reports a prior history of another otologic disease on a particular side, then it is reasonable to lateralize treatment (provisionally) to that side.
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- von Brevern, M.; Radtke, A.; Lezius, F.; Feldmann, M.; Ziese, T.; Lempert, T.; Neuhauser, H. Epidemiology of benign paroxysmal positional vertigo: A population based study. J. Neurol. Neurosurg. Psychiatry 2007, 78, 710–715. [Google Scholar] [CrossRef] [PubMed]
- Kerber, K.A. Benign paroxysmal positional vertigo: Opportunities squandered. Ann. N. Y. Acad. Sci. 2015, 1343, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Kerber, K.A.; Burke, J.F.; Skolarus, L.E.; Meurer, W.J.; Callaghan, B.C.; Brown, D.L.; Lisabeth, L.D.; McLaughlin, T.J.; Fendrick, A.M.; Morgenstern, L.B. Use of BPPV processes in emergency department dizziness presentations: A population-based study. Otolaryngol. Head Neck Surg. 2013, 148, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Neuhauser, H.K. The epidemiology of dizziness and vertigo. Handb. Clin. Neurol. 2016, 137, 67–82. [Google Scholar] [CrossRef]
- United States Census Bureau. U.S and World Population Clock. Available online: https://www.census.gov/popclock/ (accessed on 30 April 2025).
- Wang, Y.H.; Chan, C.Y.; Liu, Q.H. Benign paroxsymal positional vertigo—Recommendations for treatment in primary care. Ther. Clin. Risk Manag. 2019, 15, 719–725. [Google Scholar] [CrossRef]
- Saishoji, Y.; Yamamoto, N.; Fujiwara, T.; Mori, H.; Taito, S. Epley manoeuvre’s efficacy for benign paroxysmal positional vertigo (BPPV) in primary-care and subspecialty settings: A systematic review and meta-analysis. BMC Prim. Care 2023, 24, 262. [Google Scholar] [CrossRef]
- Kerber, K.A.; Damschroder, L.; McLaughlin, T.; Brown, D.L.; Burke, J.F.; Telian, S.A.; Tsodikov, A.; Fagerlin, A.; An, L.C.; Morgenstern, L.B.; et al. Implementation of Evidence-Based Practice for Benign Paroxysmal Positional Vertigo in the Emergency Department: A Stepped-Wedge Randomized Trial. Ann. Emerg. Med. 2020, 75, 459–470. [Google Scholar] [CrossRef]
- Kerber, K.A.; Forman, J.; Damschroder, L.; Telian, S.A.; Fagerlin, A.; Johnson, P.; Brown, D.L.; An, L.C.; Morgenstern, L.B.; Meurer, W.J. Barriers and facilitators to ED physician use of the test and treatment for BPPV. Neurol. Clin. Pract. 2017, 7, 214–224. [Google Scholar] [CrossRef]
- Del Risco, A.; Cherches, A.; Smith, S.L.; Riska, K.M. Guideline Adherence to Benign Paroxysmal Positional Vertigo Treatment and Management in Primary Care. Otolaryngol. Head Neck Surg. 2023, 169, 865–874. [Google Scholar] [CrossRef]
- Brandt, T.; Daroff, R.B. Physical therapy for benign paroxysmal positional vertigo. Arch. Otolaryngol. 1980, 106, 484–485. [Google Scholar] [CrossRef]
- Yacovino, D.A.; Hain, T.C.; Gualtieri, F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J. Neurol. 2009, 256, 1851–1855. [Google Scholar] [CrossRef] [PubMed]
- Gans, R.E.; Kurtzer, D.; McLeod, H. New Horizontal Canal Benign Paroxysmal Positional Vertigo Treatment: Kurtzer Hybrid Maneuver. Glob. J. Otolaryngol. 2017, 6, 44–48. [Google Scholar] [CrossRef]
- Barreto, R.G.; Yacovino, D.A.; Cherchi, M.; Teixeira, L.J.; Nader, S.N.; Leão, G.F. Universal repositioning maneuver: A new treatment for single canal and multi-canal benign paroxysmal positional vertigo by 3-dimensional model analysis. J. Int. Adv. Otol. 2023, 19, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Young, L.; Badihian, S.; Zee, D.S.; Newman-Toker, D.E.; Kerber, K.A.; Bhandari, A.; Bhandari, R. Benign paroxysmal positional vertigo: A case report in which four wrongs made a right. Clin. Case Rep. 2024, 12, e9529. [Google Scholar] [CrossRef]
- Wu, Y.; Song, N.; Ling, X.; Li, X.; Feng, Y.; Xing, Y.; Gu, P.; Yang, X. Canal switch in benign paroxysmal positional vertigo: Clinical characteristics and possible mechanisms. Front. Neurol. 2022, 13, 1049828. [Google Scholar] [CrossRef]
- Scotto, L.; Califano, L. Canal switch: A possible complication of physical therapeutic manoeuvers for posterior canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol. Ital. 2023, 43, 49–55. [Google Scholar] [CrossRef]
- Foster, C.A.; Zaccaro, K.; Strong, D. Canal conversion and reentry: A risk of Dix-Hallpike during canalith repositioning procedures. Otol. Neurotol. 2012, 33, 199–203. [Google Scholar] [CrossRef]
- Park, S.; Kim, B.G.; Kim, S.H.; Chu, H.; Song, M.Y.; Kim, M. Canal conversion between anterior and posterior semicircular canal in benign paroxysmal positional vertigo. Otol. Neurotol. 2013, 34, 1725–1728. [Google Scholar] [CrossRef]
- Lin, G.C.; Basura, G.J.; Wong, H.T.; Heidenreich, K.D. Canal switch after canalith repositioning procedure for benign paroxysmal positional vertigo. Laryngoscope 2012, 122, 2076–2078. [Google Scholar] [CrossRef]
- Babic, B.B.; Jesic, S.D.; Milovanovic, J.D.; Arsovic, N.A. Unintentional conversion of benign paroxysmal positional vertigo caused by repositioning procedures for canalithiasis: Transitional BPPV. Eur. Arch. Otorhinolaryngol. 2014, 271, 967–973. [Google Scholar] [CrossRef]
- Dispenza, F.; De Stefano, A.; Costantino, C.; Rando, D.; Giglione, M.; Stagno, R.; Bennici, E. Canal switch and re-entry phenomenon in benign paroxysmal positional vertigo: Difference between immediate and delayed occurrence. Acta Otorhinolaryngol. Ital. 2015, 35, 116–120. [Google Scholar] [PubMed]
- Lee, G.; Lee, S.G.; Park, H.S.; Kim, B.J.; Choi, S.J.; Choi, J.W. Clinical characteristics and associated factors of canal switch in benign paroxysmal positional vertigo. J. Vestib. Res. Equilib. Orientat. 2019, 29, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Anagnostou, E.; Stamboulis, E.; Kararizou, E. Canal conversion after repositioning procedures: Comparison of Semont and Epley maneuver. J. Neurol. 2014, 261, 866–869. [Google Scholar] [CrossRef]
- Shim, D.B.; Song, C.E.; Jung, E.J.; Ko, K.M.; Park, J.W.; Song, M.H. Benign paroxysmal positional vertigo with simultaneous involvement of multiple semicircular canals. Korean J. Audiol. 2014, 18, 126–130. [Google Scholar] [CrossRef]
- Zanotti, E.; Yacovino, D.A. Benign Paroxysmal Positional Vertigo: Canal Switching Affecting All Canals During a Single Session. Otol. Neurotol. 2021, 42, e110. [Google Scholar] [CrossRef]
- Obrist, D.; Hegemann, S. Fluid-particle dynamics in canalithiasis. J. R. Soc. Interface 2008, 5, 1215–1229. [Google Scholar] [CrossRef]
- Aran-Tapia, I.; Soto-Varela, A.; Perez-Munuzuri, V.; Santos-Perez, S.; Aran, I.; Munuzuri, A.P. Numerical Simulations of the Epley Maneuver With Clinical Implications. Ear Hear. 2024, 45, 1033–1044. [Google Scholar] [CrossRef]
- Joshi, A.; Babu, D.; Prakash, A.H.; Chandrashekara, C.V. Simulation of endolymph flow for response of cupula. Vibroengineering Procedia 2020, 31, 86–90. [Google Scholar] [CrossRef]
- Boselli, F.; Obrist, D.; Kleiser, L. Vortical flow in the utricle and the ampulla: A computational study on the fluid dynamics of the vestibular system. Biomech. Model. Mechanobiol. 2013, 12, 335–348. [Google Scholar] [CrossRef]
- Rajguru, S.M.; Ifediba, M.A.; Rabbitt, R.D. Three-dimensional biomechanical model of benign paroxysmal positional vertigo. Ann. Biomed. Eng. 2004, 32, 831–846. [Google Scholar] [CrossRef]
- Bhandari, A.; Kingma, H.; Bhandari, R. BPPV Simulation: A Powerful Tool to Understand and Optimize the Diagnostics and Treatment of all Possible Variants of BPPV. Front. Neurol. 2021, 12, 632286. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Domínguez, I.; Fernández-Seara, M.A.; Perez-Fernandez, N.; Burguete, J. Systematic Method for Morphological Reconstruction of the Semicircular Canals Using a Fully Automatic Skeletonization Process. Appl. Sci. 2019, 9, 4904. [Google Scholar] [CrossRef]
- Iversen, M.M.; Rabbitt, R.D. Wave Mechanics of the Vestibular Semicircular Canals. Biophys. J. 2017, 113, 1133–1149. [Google Scholar] [CrossRef]
- Bradshaw, A.P.; Curthoys, I.S.; Todd, M.J.; Magnussen, J.S.; Taubman, D.S.; Aw, S.T.; Halmagyi, G.M. A mathematical model of human semicircular canal geometry: A new basis for interpreting vestibular physiology. J. Assoc. Res. Otolaryngol. 2010, 11, 145–159. [Google Scholar] [CrossRef]
- Blanks, R.H.; Curthoys, I.S.; Markham, C.H. Planar relationships of the semicircular canals in man. Acta Otolaryngol. 1975, 80, 185–196. [Google Scholar] [CrossRef]
- Bertholon, P.; Bronstein, A.M.; Davies, R.A.; Rudge, P.; Thilo, K.V. Positional down beating nystagmus in 50 patients: Cerebellar disorders and possible anterior semicircular canalithiasis. J. Neurol. Neurosurg. Psychiatry 2002, 72, 366–372. [Google Scholar] [CrossRef]
- Della Santina, C.C.; Potyagaylo, V.; Migliaccio, A.A.; Minor, L.B.; Carey, J.P. Orientation of human semicircular canals measured by three-dimensional multiplanar CT reconstruction. J. Assoc. Res. Otolaryngol. 2005, 6, 191–206. [Google Scholar] [CrossRef]
- Ifediba, M.A.; Rajguru, S.M.; Hullar, T.E.; Rabbitt, R.D. The role of 3-canal biomechanics in angular motion transduction by the human vestibular labyrinth. Ann. Biomed. Eng. 2007, 35, 1247–1263. [Google Scholar] [CrossRef] [PubMed]
- Teixido, M.; Woods, O.; Kung, B.; Seyyedi, M. A 3D benign paroxysmal positional vertigo model for study of otolith disease. World J. Otorhinolaryngol. Head Neck Surg. 2016, 2, 1–6. [Google Scholar] [CrossRef]
- Traboulsi, H.; Teixido, M. BPPV Viewer: A downloadable 3D BPPV model for study of otolith disease. World J. Otorhinolaryngol.—Head Neck Surg. 2021, 7, 34–39. [Google Scholar] [CrossRef]
- Epley, J.M. The canalith repositioning procedure: For treatment of benign paroxysmal positional vertigo. Otolaryngol. Head Neck Surg. 1992, 107, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Semont, A.; Freyss, G.; Vitte, E. Curing the BPPV with a liberatory maneuver. Adv. Otorhinolaryngol. 1988, 42, 290–293. [Google Scholar] [CrossRef] [PubMed]
- Strupp, M.; Goldschagg, N.; Vinck, A.S.; Bayer, O.; Vandenbroeck, S.; Salerni, L.; Hennig, A.; Obrist, D.; Mandala, M. BPPV: Comparison of the SemontPLUS With the Semont Maneuver: A Prospective Randomized Trial. Front. Neurol. 2021, 12, 652573. [Google Scholar] [CrossRef]
- Strupp, M.; Mandala, M.; Vinck, A.S.; Van Breda, L.; Salerni, L.; Gerb, J.; Bayer, O.; Mavrodiev, V.; Goldschagg, N. The Semont-Plus Maneuver or the Epley Maneuver in Posterior Canal Benign Paroxysmal Positional Vertigo: A Randomized Clinical Study. JAMA Neurol. 2023, 80, 798–804. [Google Scholar] [CrossRef]
- Foster, C.A.; Ponnapan, A.; Zaccaro, K.; Strong, D. A Comparison of Two Home Exercises for Benign Positional Vertigo: Half Somersault versus Epley Maneuver. Audiol. Neurotol. Extra 2012, 2, 16–23. [Google Scholar] [CrossRef]
- Roberts, R.A.; Gans, R.E.; Montaudo, R.L. Efficacy of a new treatment maneuver for posterior canal benign paroxysmal positional vertigo. J. Am. Acad. Audiol. 2006, 17, 598–604. [Google Scholar] [CrossRef]
- Gan, Z.; Zhou, S.; Yang, H.; He, F.; Wei, D.; Bai, Y.; Wang, Y.; Wang, Y.; Fu, W.; Han, J. Self-Treatment of Posterior Canal Benign Paroxysmal Positional Vertigo: A Preliminary Study. Front. Med. 2021, 8, 654637. [Google Scholar] [CrossRef]
- Lempert, T.; Tiel-Wilck, K. A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope 1996, 106, 476–478. [Google Scholar] [CrossRef]
- Vannucchi, P.; Giannoni, B. Terapia della vertigine parossistica posizionale del canale semicircolare laterale, Tecniche a confronto [Treatment of lateral canal BPPV, comparison of techniques]. In VII Giornata di Vestibologia Pratica, ‘La Terapia Fisica delle Vertigini Periferiche’ [Practical Vestibulology, ‘Physical Therapy for Peripheral Vertigo’]; Nuti, D., Passali, D., Eds.; CSS Formenti: Milano, Italy, 1998. [Google Scholar]
- Vannucchi, P.; Libonati, G.; Gufoni, M.; Asprella Libonati, G. The Physical Treatment of Lateral Semicircular Canal Canalolithiasis. Audiol. Med. 2005, 3, 52–56. [Google Scholar] [CrossRef]
- Gufoni, M.; Mastrosimone, L.; Di Nasso, F. Repositioning maneuver in benign paroxysmal vertigo of horizontal semicircular canal. Acta Otorhinolaryngol. Ital. 1998, 18, 363–367. [Google Scholar]
- Ramos, B.F.; Cal, R.; Brock, C.M.; Mangabeira Albernaz, P.L.; Zuma, E.M.F. Zuma Modified Maneuver as a Treatment to Geotropic Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo. Int. Arch. Otorhinolaryngol. 2021, 25, e255–e257. [Google Scholar] [CrossRef] [PubMed]
- Ciniglio Appiani, G.; Catania, G.; Gagliardi, M.; Cuiuli, G. Repositioning maneuver for the treatment of the apogeotropic variant of horizontal canal benign paroxysmal positional vertigo. Otol. Neurotol. 2005, 26, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Zuma e Maia, F. New Treatment Strategy for Apogeotropic Horizontal Canal Benign Paroxysmal Positional Vertigo. Audiol. Res. 2016, 6, 163. [Google Scholar] [CrossRef]
- Kim, Y.K.; Shin, J.E.; Chung, J.W. The effect of canalith repositioning for anterior semicircular canal canalithiasis. ORL J. Otorhinolaryngol. Relat. Spec. 2005, 67, 56–60. [Google Scholar] [CrossRef]
- Mosca, F.; Morano, M. Benign paroxysmal positional vertigo, incidence and treatment. Ann. Otolaryngol. Chir. Cervicofac. 2001, 118, 95–101. [Google Scholar]
- Bhandari, A.; Bhandari, R.; Kingma, H.; Strupp, M. Diagnostic and Therapeutic Maneuvers for Anterior Canal BPPV Canalithiasis: Three-Dimensional Simulations. Front. Neurol. 2021, 12, 740599. [Google Scholar] [CrossRef]
- Honrubia, V.; Baloh, R.W.; Harris, M.R.; Jacobson, K.M. Paroxysmal positional vertigo syndrome. Am. J. Otol. 1999, 20, 465–470. [Google Scholar]
- Rahko, T. The test and treatment methods of benign paroxysmal positional vertigo and an addition to the management of vertigo due to the superior vestibular canal (BPPV-SC). Clin. Otolaryngol. Allied Sci. 2002, 27, 392–395. [Google Scholar] [CrossRef]
- Garaycochea, O.; Perez-Fernandez, N.; Manrique-Huarte, R. A novel maneuver for diagnosis and treatment of torsional-vertical down beating positioning nystagmus: Anterior canal and apogeotropic posterior canal BPPV. Braz. J. Otorhinolaryngol. 2022, 88, 708–716. [Google Scholar] [CrossRef]
- Casani, A.P.; Cerchiai, N.; Dallan, I.; Sellari-Franceschini, S. Anterior canal lithiasis: Diagnosis and treatment. Otolaryngol. Head Neck Surg. 2011, 144, 412–418. [Google Scholar] [CrossRef]
- Bhandari, R.; Bhandari, A.; Kingma, H.; Berg, R.V. Large Variability of Head Angulation During the Epley Maneuver: Use of a Head-Mounted Guidance System with Visual Feedback to Improve Outcomes. J. Int. Adv. Otol. 2023, 19, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Boselli, F.; Kleiser, L.; Bockisch, C.J.; Hegemann, S.C.; Obrist, D. Quantitative analysis of benign paroxysmal positional vertigo fatigue under canalithiasis conditions. J. Biomech. 2014, 47, 1853–1860. [Google Scholar] [CrossRef]
- Peng, Y.; Qi, J. A Dynamic Model of Otolith for Determinants of a BPPV Reposition Maneuver with Its Simulation. J. Phys. Conf. Ser. 2020, 1631, 012044. [Google Scholar] [CrossRef]
- Bhandari, A.; Bhandari, R.; Kingma, H.; Zuma, E.M.F.; Strupp, M. Three-dimensional simulations of six treatment maneuvers for horizontal canal benign paroxysmal positional vertigo canalithiasis. Eur. J. Neurol. Off. J. Eur. Fed. Neurol. Soc. 2021, 28, 4178–4183. [Google Scholar] [CrossRef]
- Mandala, M.; Pepponi, E.; Santoro, G.P.; Cambi, J.; Casani, A.; Faralli, M.; Giannoni, B.; Gufoni, M.; Marcelli, V.; Trabalzini, F.; et al. Double-blind randomized trial on the efficacy of the Gufoni maneuver for treatment of lateral canal BPPV. Laryngoscope 2013, 123, 1782–1786. [Google Scholar] [CrossRef]
- Hain, T.C.; Squires, T.M.; Stone, H.A. Clinical implications of a mathematical model of benign paroxysmal positional vertigo. Ann. N. Y. Acad. Sci. 2005, 1039, 384–394. [Google Scholar] [CrossRef]
- Dix, M.R.; Hallpike, C.S. The pathology symptomatology and diagnosis of certain common disorders of the vestibular system. Proc. R. Soc. Med. 1952, 45, 341–354. [Google Scholar] [CrossRef]
- Bickham, W.S. Misconception, in America, as to the Rose position. J. Am. Med. Assoc. 1931, 96, 2185–2187. [Google Scholar] [CrossRef]
- Rose, E. Vorschlag zur Proposal to facilitate operations on the upper jaw. In Erleichterung der Operationen am Oberkiefer; Julius Sittenfeld: Berlin, Germany, 1874. [Google Scholar]
- Greene, A.K.; Kreuter, M.; Mulliken, J.B. Professor Edmund Rose: His position in surgery. Plast. Reconstr. Surg. 2003, 111, 383–386. [Google Scholar] [CrossRef]
- Oas, J.G. Benign paroxysmal positional vertigo: A clinician’s perspective. Ann. N. Y. Acad. Sci. 2001, 942, 201–209. [Google Scholar] [CrossRef]
- Harmat, K.; Tamas, L.T.; Schubert, M.C.; Gerlinger, I.; Komoly, S.; Buki, B. Prevalence of and Theoretical Explanation for Type 2 Benign Paroxysmal Positional Vertigo. J. Neurol. Phys. Ther. 2022, 46, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Fife, T.D. Positional dizziness. Continuum 2012, 18, 1060–1085. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.H.; Ban, J.H.; Lee, K.C.; Kim, S.M. Benign paroxysmal positional vertigo secondary to inner ear disease. Otolaryngol. Head Neck Surg. 2010, 143, 413–417. [Google Scholar] [CrossRef]
- Baloh, R.W.; Honrubia, V.; Jacobson, K. Benign positional vertigo: Clinical and oculographic features in 240 cases. Neurology 1987, 37, 371–378. [Google Scholar] [CrossRef]
- Balatsouras, D.G.; Koukoutsis, G.; Ganelis, P.; Economou, N.C.; Moukos, A.; Aspris, A.; Katotomichelakis, M. Benign paroxysmal positional vertigo secondary to vestibular neuritis. Eur. Arch. Otorhinolaryngol. 2014, 271, 919–924. [Google Scholar] [CrossRef]
- Kutlubaev, M.A.; Xu, Y.; Hornibrook, J. Benign paroxysmal positional vertigo in Meniere’s disease: Systematic review and meta-analysis of frequency and clinical characteristics. J. Neurol. 2019, 268, 1608–1614. [Google Scholar] [CrossRef]
- Tomaz, A.; Gananca, M.M.; Gananca, C.F.; Gananca, F.F.; Caovilla, H.H.; Harker, L. Benign paroxysmal positional vertigo: Concomitant involvement of different semicircular canals. Ann. Otol. Rhinol. Laryngol. 2009, 118, 113–117. [Google Scholar] [CrossRef]

| Maneuver | Number of Positions | Posterior Canal (PC) | Lateral Canal (LC) | Anterior Canal (AC) | |||
|---|---|---|---|---|---|---|---|
| PC Success | PC Failure | LC Success | LC Failure | AC Success | AC Failure | ||
| Maneuvers intended to treat unilateral posterior canal | |||||||
| Epley. Excellent efficacy for all canals. | 3 | 10 Otoliths usually reflux into AC before resolving. | 0 | 10 | 0 | 9 | 1 Occasionally, otoliths fail to exit the ampulla. |
| Semont. Good efficacy for PC. Occasionally treats LC. | 2 | 3 | 7 Usually, in position 2, otoliths reflux into AC and then remain there. Sometimes, in position 1, otoliths reach the apex, but then in position 2, they retreat. | 1 | 9 In position 1, otoliths reach the apex, but then in position 2, they usually retreat. | 0 | 10 In position 1, the AC plane remains horizontal, so otoliths remain stationary, not even advancing toward the apex. |
| Semont plus. Very good efficacy for PC. Occasionally treats AC. | 2 | 8 | 2 Sometimes (1) refluxes into AC. Sometimes (1) retreats from the apex. | 0 | 10 Retreats from apex. | 3 | 7 Retreats from the apex or does not reach the apex. |
| Foster. Very good efficacy for PC. Good efficacy for AC. Rarely treats LC. | 5 | 8 May (7) transiently reflux into AC. | 2 | 1 | 9 Retreats from apex. | 6 | 4 Does not progress from the ampulla. |
| Gans. Modest efficacy for PC. Very good efficacy for LC. Good efficacy for AC. | 3 | 2 | 8 Retreats from apex. | 10 | 0 | 8 Otoliths sometimes (1) reflux into PC and then resolve. | 2 Otoliths sometimes (1) reflux into PC and then remain there. |
| Modified Epley. Excellent efficacy for PC and LC. Good efficacy for AC. | 4 | 10 | 0 | 10 | 0 | 6 | 4 Does not exit the ampulla. |
| Maneuvers intended to treat bilateral posterior canals | |||||||
| Brandt–Daroff. Excellent efficacy for LC. Occasionally treats AC. | 3 | 0 | 10 | 10 | 0 | 2 | 8 Usually retreats from the apex. |
| Maneuvers intended to treat unilateral lateral canal (geotropic or apogeotropic) | |||||||
| Lempert roll. Excellent efficacy for LC. | 4 | 0 | 10 | 10 | 0 | 0 | 10 In position 2, otoliths from AC often (7) reflux into PC and then remain there. |
| Vannucchi–Asprella. Poor efficacy for all canals. | 3 | 1 Sometimes (1) refluxes into AC, then resolves. | 9 Approaches but then retreats from the apex. | 1 | 9 In some instances (7), otoliths fail to exit the ampulla. | 1 | 9 |
| Maneuvers intended to treat unilateral lateral canal, geotropic variant | |||||||
| Gufoni–Appiani, geotropic. Excellent efficacy for LC. Rarely treats AC. | 2 | 0 | 10 | 10 | 0 | 2 Rarely do otoliths escape the AC cupula during the first position. | 8 |
| Modified Zuma. Excellent efficacy for LC. Modest efficacy for AC. | 5 | 0 | 10 | 10 | 0 | 3 | 7 Sometimes (4) otoliths reach the common crus but reflux into the PC. |
| Maneuvers intended to treat unilateral lateral canal, apogeotropic variant | |||||||
| Gufoni–Appiani, apogeotropic. Modest efficacy for LC alone. | 3 | 0 | 10 | 5 | 5 | 0 | 10 |
| Zuma. Excellent efficacy for LC alone. Rarely treats AC. | 5 | 0 | 10 | 10 | 0 | 1 | 9 Sometimes (5) in position 2, AC refluxes into PC and remains there. |
| Maneuvers intended to treat bilateral lateral canals | |||||||
| Kurtzer hybrid. Poor efficacy overall. | 6 | 1 | 9 Otoliths sometimes alternate PC and AC, mutually refluxing | 1 | 9 Often, otolith remains in the ampulla. | 0 | 10 Otoliths sometimes alternate PC and AC, mutually refluxing |
| Maneuvers intended to treat unilateral anterior canal | |||||||
| Kim. Excellent efficacy for AC, modest efficacy for LC. | 4 | 0 | 10 | 7 | 3 | 10 | 0 |
| Reverse Semont. Excellent efficacy for AC. Rarely treats LC. | 2 | 0 | 10 | 1 | 9 | 10 | 0 |
| Reverse Epley. No efficacy. | 3 | 0 | 10 | 0 | 10 | 0 | 10 |
| Rahko. Good efficacy for AC alone. | 3 | 0 | 10 | 0 | 10 | 7 | 3 Sometimes, otoliths fail to exit the ampulla. |
| Garaycochea. Very good efficacy for AC alone. | 6 | 0 | 10 | 0 | 10 | 8 | 2 |
| Maneuvers intended to treat bilateral anterior canals | |||||||
| Yacovino. Good efficacy for AC alone. | 2 | 0 | 10 | 0 | 10 | 7 | 3 Sometimes (2) otoliths reflux from AC to PC and remain there. Sometimes (1) otoliths fail to exit the ampulla. |
| Maneuvers intended to treat multiple canals | |||||||
| Barreto. Excellent efficacy for AC, moderate efficacy for PC, and no efficacy for LC. | 2 | 7 Sometimes (2) refluxes into AC before resolving | 3 Sometimes (3) otoliths do not exit the ampulla. | 0 | 10 | 10 | 0 |
| Position | Right Anterior Canal | Right Posterior Canal | Right Horizontal Canal |
|---|---|---|---|
| 1. Neutral (seated). |
|
|
|
| 2: Right Lempert (side-lying). Acts predominantly on the right horizontal canal. |
|
|
|
| 3: Right Dix–Hallpike. Acts predominantly on the right posterior canal. |
|
|
|
| 4: Rose position. |
|
|
|
| 5: Left Dix–Hallpike. Acts predominantly on the right anterior canal. |
|
|
|
| 6: Left Lempert (side-lying). Acts predominantly on the right horizontal canal. |
|
|
|
| 7: Left lateral decubitus, with neck laterally flexed by 45° such that the upper ear is closer to the shoulder. |
|
|
|
| 8: Neutral (seated). |
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cherchi, M. Unilateral Triple Canal Repositioning Maneuver: Principles and Design. Audiol. Res. 2025, 15, 55. https://doi.org/10.3390/audiolres15030055
Cherchi M. Unilateral Triple Canal Repositioning Maneuver: Principles and Design. Audiology Research. 2025; 15(3):55. https://doi.org/10.3390/audiolres15030055
Chicago/Turabian StyleCherchi, Marcello. 2025. "Unilateral Triple Canal Repositioning Maneuver: Principles and Design" Audiology Research 15, no. 3: 55. https://doi.org/10.3390/audiolres15030055
APA StyleCherchi, M. (2025). Unilateral Triple Canal Repositioning Maneuver: Principles and Design. Audiology Research, 15(3), 55. https://doi.org/10.3390/audiolres15030055







