From Triportal to Uniportal Video-Thoracoscopic Lobectomy: The Single Surgeon Learning Curve by CUSUM Chart and Perioperative Outcomes
Abstract
Highlights
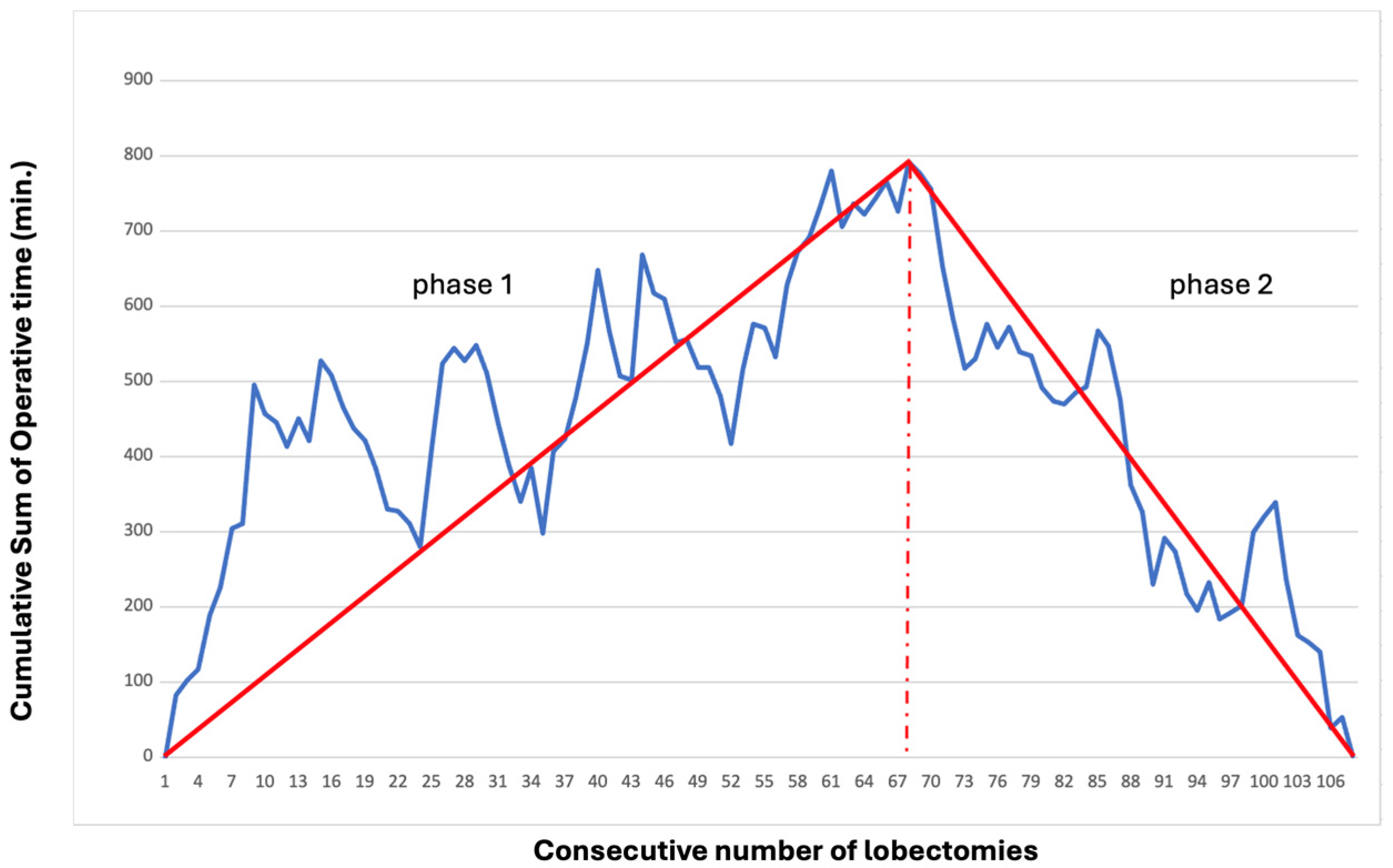
- As U-VATS lobectomy becomes globally prevalent, it suggests a period of skill acquisition for thoracic surgeons. CUSUM analysis of learning curve identified 67 uniportal VATS lobectomies as the inflection point for proficiency, with significant reductions in operative time (188 vs. 170.5 min, p = 0.02), conversions (15% vs. 2.5%, p = 0.04), and complications (42% vs. 22%, p = 0.04).
- Prior experience with triportal VATS does not remove the learning curve; a moving average analysis showed that skill acquisition progressed even after the first 67 procedures.
- Provides a benchmark for surgeons transitioning to uniportal VATS, suggesting about 50–70 cases are needed to achieve competency, aligning with ESTS consensus.
- Supports structured training programs, as even experienced multiportal VATS surgeons require dedicated practice to master uniportal techniques.
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgical Procedure
2.2. Statistical Analysis
3. Results
3.1. CUSUM Analysis
3.2. Perioperative Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CUSUM | Cumulative Sum |
| U-VATS | Uniportal video-thoracoscopy |
| CT | Computed Tomography |
| EBUS-TBNA | Endobronchial Ultrasound Transbronchial Aspiration |
| PET | Positron Emission Tomography |
| SD | Standard Deviation |
| FEV1 | Forced Expiratory Volume in 1 s |
| DLCO | Diffusion Lung Carbon Monoxide |
| IQR | Interquartile |
| ECOG | Eastern Cooperative Oncology Group Performance Status |
| COPD | Chronic Obstructive Pulmonary Disease |
| BMI | Body Mass Index |
| VAS | Visual Analogue Scale |
| LC | Learning Curve |
| NA | Not available |
References
- Gonzalez, D.; Paradela, M.; Garcia, J.; Dela Torre, M. Single-port video- assisted thoracoscopic lobectomy. Interact. Cardiovasc. Thorac. Surg. 2011, 12, 514–515. [Google Scholar] [CrossRef]
- Hansen, H.J.; Petersen, R.H. Video-assisted thoracoscopic lobectomy using a standardized three-port anterior approach—The Copenhagen experience. Ann. Cardiothorac. Surg. 2012, 1, 70–76. [Google Scholar] [CrossRef]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Costa, E.F.; Delgado Roel, M.; Paradela de la Morena, M.; Gonzalez-Rivas, D.; Fernandez-Prado, R.; de la Torre, M. Technique of uniportal VATS major pulmonary resections. J. Thorac. Dis. 2014, 6, S660–S664. [Google Scholar] [CrossRef]
- National Library of Medicine, National Center for Biotechnology Information. Available online: https://pubmed.ncbi.nlm.nih.gov (accessed on 15 January 2025).
- Li, W.H.; Cheng, H.; Gan, X.F.; Li, X.J.; Wang, X.J.; Wu, X.W.; Zhong, H.C.; Wuv, T.C.; Huo, W.W.; Ju, S.L.; et al. Learning curve of uniportal video-assisted thoracoscopic lobectomy: An analysis of the proficiency of 538 cases from a single centre. Interact. Cardiovasc. Thorac. Surg. 2022, 34, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chen, X.; Shen, Y.; Wang, H.; Feng, M.; Tan, L.; D’Amico, T.A. Learning curve for uniportal video-assisted thoracoscopic surgery lobectomy—Results from 120 consecutive patients. J. Thorac. Dis. 2018, 10, 5100–5107. [Google Scholar] [CrossRef]
- Stamenovic, D.; Messerschmidt, A.; Schneider, T. Cumulative sum analysis of the learning curve for uniportal video-assisted thoracoscopic lobectomy and lymphadenectomy. J. Laparoendosc. Adv. Surg. Tech. 2019, 29, 914–920. [Google Scholar] [CrossRef]
- Zhai, R.; Liu, H.; Wang, J.; Shan, L.; Luo, M.; Yao, F. Extensive open lobectomy experience is not a prerequisite for learning uniportal video-assisted thoracic surgery lobectomy. J. Surg. Oncol. 2022, 126, 1104–1113. [Google Scholar] [CrossRef]
- Laven, I.E.W.G.; Daemen, J.H.T.; Franssen, A.J.P.M.; Gronenschild, M.H.M.; Hulsewé, K.W.E.; Vissers, Y.L.J.; de Loos, E.R. Uniportal video-assisted thoracoscopic surgery for lobectomy: The learning curve. Interdiscip. Cardiovasc. Thorac. Surg. 2023, 3, 37. [Google Scholar] [CrossRef]
- Lim, T.O.; Soraya, A.; Ding, L.M.; Morad, Z. Assessing doctors’ competence: Application of CUSUM technique in monitoring doctors’ performance. Int. J. Qual. Health Care 2002, 14, 251–258. [Google Scholar] [CrossRef]
- Fortea-Sanchis, C.; Escrig-Sos, J. Quality Control Techniques in Surgery: Application of Cumulative Sum (CUSUM) Charts. Cir. Esp. 2019, 97, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Bertolaccini, L.; Batirel, H.; Brunelli, A.; Gonzalez-Rivas, D.; Ismail, M.; Ucar, A.M.; Ng, C.S.H.; Scarci, M.; Sihoe, A.D.L.; Ugalde, P.A.; et al. Uniportal video-assisted thoracic surgery lobectomy: A consensus report from the uniportal VATS interest group (UVIG) of the European Society of Thoracic Surgeons (ESTS). Eur. J. Cardio-Thorac. Surg. 2019, 56, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Yang, R.; Shao, F. Comparison of Postoperative Pain and Recovery between Single-Port and Two-Port Thoracoscopic Lobectomy for Lung Cancer. Thorac. Cardiovasc. Surg. 2019, 67, 142–146. [Google Scholar] [CrossRef]
- Hirai, K.; Takeuchi, S.; Usuda, J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: A retrospective comparative study of perioperative clinical outcomes. Eur. J. Cardiothorac. Surg. 2016, 49, 37–41. [Google Scholar] [CrossRef]
- Harris, C.G.; James, R.S.; Tian, D.H.; Yan, T.D.; Doyle, M.P.; Gonzalez-Rivas, D.; Cao, C. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann. Cardiothorac. Surg. 2016, 5, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Dai, Z.; Wei, X.; Pompili, C.; Shi, Q.L.; Xie, T.P.; He, J.-T.; Li, Q. Early Patient-Reported Outcomes After Uniportal vs Multiportal Thoracoscopic Lobectomy. Ann. Thorac. Surg. 2022, 114, 1229–1237. [Google Scholar] [CrossRef]
- Song, Z.; Yuan, Y.; Cheng, C.; Luo, Q.; Cheng, X. The learning curve on uniportal video-assisted thoracoscopic lobectomy with the help of postoperative review of videos. Front. Oncol. 2023, 13, 1085634. [Google Scholar] [CrossRef]
- Igai, H.; Matsuura, N.; Numajiri, K.; Ohsawa, F.; Kamiyoshihara, M. Supervision by an experienced surgeon can reduce the learning curve of uniportal thoracoscopic lobectomy. Transl. Lung Cancer Res. 2023, 12, 207–218. [Google Scholar] [CrossRef]
- Shahoud, J.; Weksler, B.; Williams, B.; Crist, L.; Fernando, H. Initial outcomes with uniportal video-assisted lung resection. Interdiscip. Cardiovasc. Thorac. Surg. 2025, 40, ivaf111. [Google Scholar] [CrossRef] [PubMed]
- Bourdages-Pageau, E.; Vieira, A.; Lacasse, Y.; Figueroa, P.U. Outcomes of Uniportal vs Multiportal Video-Assisted Thoracoscopic Lobectomy. Semin. Thorac. Cardiovasc. Surg. 2020, 32, 145–151. [Google Scholar] [CrossRef]
- Grossi, S.; Cattoni, M.; Rotolo, N.; Imperatori, A. Video-assisted thoracoscopic surgery simulation and training: A comprehensive literature review. BMC Med. Educ. 2023, 27, 535. [Google Scholar] [CrossRef] [PubMed]
- Woodall, W.H.; Rakovich, G.; Steiner, S.H. An overview and critique of the use of cumulative sum methods with surgical learning curve data. Stat. Med. 2021, 40, 1400–1413. [Google Scholar] [CrossRef] [PubMed]

| Characteristics of Patients | Patients (n = 107) | Phase 1 (n = 67) | Phase 2 (n = 40) | p-Value |
|---|---|---|---|---|
| Age, median (IQR) | 69 (62–75) | 70 (62–75) | 68 (2–75) | 0.37 |
| Male, n (%) | 67 (63) | 43 (64) | 24 (60) | 0.88 |
| Smokers/former smokers, n (%) | 70 (65) | 43 (64) | 27 (67) | 0.71 |
| BMI, mean (SD) kg/m2 | 25.8 (4.38) | 25.5 (4.19) | 26 (4.77) | 0.43 |
| FEV1, median (IQR) | 103 (90–118.8) | 103 (90–117) | 104.5 (94–119) | 0.74 |
| DLCO, %, median (IQR) | 85 (72.5–96) | 85 (75–96) | 88 (71–99.5) | 0.61 |
| Performance status (ECOG), 0, n (%) | 91 (85) | 56 (84) | 35 (87) | 0.65 |
| Comorbidities, n (%) | ||||
| COPD | 24 (22) | 17 (25) | 7 (17) | 0.34 |
| Hypertension | 69 (64) | 43 (64) | 26 (65) | 0.9 |
| Diabetes | 21 (20) | 13 (19) | 8 (20) | 0.9 |
| Dyslipideamia | 41 (38) | 27 (40) | 14 (35) | 0.6 |
| Heart failure | 18 (17) | 13 (19) | 5 (12) | 0.3 |
| Tumor characteristics | ||||
| Adenocarcinoma, n (%) | 79 (74) | 47 (70) | 32 (80) | 0.3 |
| Squamous, n (%) | 13 (12) | 8 (12) | 5 (12) | 0.9 |
| Carcinoid, n (%) | 7 (6) | 5 (7) | 2 (5) | 0.7 |
| Other cancer, n (%) | 8 (7) | 7 (10) | 1 (2) | 0.2 |
| Tumor size, median (IQR) mm | 23 (16–33) | 23 (16–33) | 25 (16–34) | 0.6 |
| Tumor site, n (%) | ||||
| Right upper lobe | 29 (27) | 19 (28) | 10 (25) | 0.7 |
| Middle lobe | 4 (4) | 2 (3) | 2 (5) | 0.6 |
| Right lower lobe | 25 (23) | 18 (27) | 7 (17) | 0.3 |
| Left upper lobe | 28 (26) | 17 (25) | 11 (27) | 0.8 |
| Left lower lobe | 18 (17) | 9 (13) | 9 (22) | 0.2 |
| Bilobectomy | 3 (3) | 2 (3) | 1 (2) | 0.9 |
| Stage, n (%) | ||||
| I | 70 (65) | 43 (64) | 27 (67) | 0.7 |
| II | 21 (20) | 14 (21) | 7 (17) | 0.7 |
| IIIa | 12 (11) | 8 (12) | 4 (10) | 0.7 |
| Perioperative Outcomes | Patients (n = 107) | Group A (n = 67) | Group B (n = 40) | p-Value |
|---|---|---|---|---|
| Surgery time, median (DS) min | 184 (151–226) | 188 (151–236) | 170.5 (134–202) | 0.02 |
| Conversion to thoracotomy, n (%) | 11 (10) | 10 (15) | 1 (2) | 0.04 |
| Length of stay, median (IQR) days | 6 (5–9) | 6 (5–9.5) | 5 (4–8) | 0.04 |
| Chest drainage time, median (IQR) days | 4 (3–5.5) | 4 (3–6.5) | 3 (3–5) | 0.19 |
| Complications, n (%) | 37 (35) | 28 (42) | 9 (22) | 0.04 |
| Pulmonary complications, n (%) | 14 (13) | 12 (18) | 2 (5) | 0.05 |
| Prolonged air leak | 10 (9) | 8 (12) | 2 (5) | 0.3 |
| Pneumonia | 1 (1) | 1 (1) | 0 (0) | 1 |
| Not pulmonary complications, n (%) | 25 (23) | 19 (28) | 6 (15) | 0.1 |
| Atrial fibrillation | 11 (10) | 9 (13) | 2 (5) | 0.2 |
| Anemia | 9 (8) | 6 (9) | 3 (7) | 1 |
| Urinary tract infections | 4 (4) | 3 (4) | 1 (2) | 1 |
| Fever | 8 (7) | 6 (9) | 2 (5) | 0.7 |
| Postop. pain, VAS score, median (IQR) | ||||
| VAS I GPO | 3 (1–5) | 3 (1–5) | 2 (2–3) | 0.07 |
| VAS II GPO | 2 (1–4) | 3 (1–4) | 2 (0–2) | 0.001 |
| VAS III GPO | 2 (0–3) | 2 (1–3) | 1 (0–2) | 0.52 |
| VAS at discharget home | 0 (0–1) | 0 (0–1) | 0 (0–0) | 0.002 |
| Increase in pain treatment, n (%) | 35 (33) | 26 (39) | 9 (22) | 0.08 |
| 30 days mortality, n (%) | 1 (1) | 0 (0) | 1 (2) | 0.2 |
| Authors | n° of U-VATS | Surgeon | Cut-Off Value | Decrease in Time Among LC Phases p-Value |
|---|---|---|---|---|
| Li [6], 2022 | 538 | 1 | 52 | 0.001 |
| Liu [7], 2018 | 120 | 1 | 44 | 0.001 |
| Stamenovic [8] 2019 | 52 | 1 | 28 | 0.002 |
| Zhai [9] 2022 | 103 | 1 | 33 | 0.002 |
| Laven [10] 2023 | 324 | 4 | 14–26 | NA |
| Cerretani[*]2025 | 107 | 1 | 67 | 0.003 |
| Causes of Conversion | 1st Phase of Learning Curve 67 Patients | 2nd Phase of Proficiency 40 Patients | p-Value |
|---|---|---|---|
| Conversion to thoracotomy, n (%) | 10 (15) | 1 (2.5) | 0.04 |
| Vascular accident, n | 4 | none | |
| Technical difficulty, n | 4 | none | |
| Bronchial accident, n | 2 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerretani, G.; Nardecchia, E.; Asteggiano, E.; Colombo, A.; Di Natale, D.; Filipponi, L.; Rotolo, N. From Triportal to Uniportal Video-Thoracoscopic Lobectomy: The Single Surgeon Learning Curve by CUSUM Chart and Perioperative Outcomes. Surg. Tech. Dev. 2025, 14, 34. https://doi.org/10.3390/std14040034
Cerretani G, Nardecchia E, Asteggiano E, Colombo A, Di Natale D, Filipponi L, Rotolo N. From Triportal to Uniportal Video-Thoracoscopic Lobectomy: The Single Surgeon Learning Curve by CUSUM Chart and Perioperative Outcomes. Surgical Techniques Development. 2025; 14(4):34. https://doi.org/10.3390/std14040034
Chicago/Turabian StyleCerretani, Giorgia, Elisa Nardecchia, Elena Asteggiano, Alberto Colombo, Davide Di Natale, Luca Filipponi, and Nicola Rotolo. 2025. "From Triportal to Uniportal Video-Thoracoscopic Lobectomy: The Single Surgeon Learning Curve by CUSUM Chart and Perioperative Outcomes" Surgical Techniques Development 14, no. 4: 34. https://doi.org/10.3390/std14040034
APA StyleCerretani, G., Nardecchia, E., Asteggiano, E., Colombo, A., Di Natale, D., Filipponi, L., & Rotolo, N. (2025). From Triportal to Uniportal Video-Thoracoscopic Lobectomy: The Single Surgeon Learning Curve by CUSUM Chart and Perioperative Outcomes. Surgical Techniques Development, 14(4), 34. https://doi.org/10.3390/std14040034






