Abstract
Background: Proximal humerus fractures (PHFs) constitute a significant orthopedic challenge, particularly among the elderly, due to osteoporosis and comorbidities. While surgical intervention is often considered for complex fractures, non-surgical treatment (NST) has gained attention, especially during the COVID-19 pandemic, when surgical resources were limited. This study evaluates the functional outcomes of patients over 65 years old who underwent NST for PHFs during the pandemic. Methods: A retrospective analysis was conducted on patients presenting with 3- or 4-part PHFs at the Hospital Marino di Alghero (Italy) between 9 March 2020 and 18 May 2020. Inclusion criteria included age over 65, conservative management, and a minimum 30-month follow-up. Seven patients were evaluated through radiographic imaging and clinical assessments, including the Constant Shoulder Score (CSS), Oxford Shoulder Score (OSS), and Disabilities of the Arm, Shoulder, and Hand Score (DASH). Functional recovery was analyzed over a 48-month period. Results: The average CSS was 69.4 (SD: 22.3), OSS was 34 (SD: 14.6), and DASH was 27.9 (SD: 30.3), indicating moderate functional recovery. One patient required surgical fixation due to excessive displacement. Tuberosity union was observed in 85.7% of cases, and complications were minimal. NST allowed patients to recover shoulder function while avoiding surgical risks, particularly during the pandemic. Conclusions: NST proved to be a viable treatment for elderly patients with PHFs, yielding satisfactory functional outcomes with minimal complications. The pandemic highlighted the importance of conservative approaches in orthopedic management, emphasizing the need for individualized treatment decisions based on patient comorbidities and fracture characteristics.
1. Introduction
Proximal humerus fractures (PHFs) represent a significant burden in orthopedic practice, accounting for approximately 4 to 7% of all fractures [1]. These fractures often occur in people over 65 years old, and their incidence is steadily increasing due to population aging [2,3]; on the other hand, in young adults, this pathologic condition could be due to high-energy traumas or oncologic complications [4]. Fragments’ displacement is common in PHFs, occurring in approximately 51% of PHFs, often involving the surgical neck (77% of cases) [5]. Among osteoporotic fractures, PHFs rank prominently after wrist, lumbar and thoracic vertebral, and proximal femur fractures [6,7].
The mechanisms of PHF differ between elderly and younger individuals. In the elderly, low-energy trauma acting on lower-quality bones is often the cause, while young individuals are more prone to high-energy traumas during sports activities or road accidents [8]. Despite the high incidence of PHFs, a consensus on optimal treatment remains elusive, influenced by various factors. Identification of fracture type, including the number and displacement of fragments, is crucial, but decisions about treatment must also consider patient-specific factors, such as functional demands and comorbidities, in addition to surgeon expertise [9].
The AO classification system provides a comprehensive framework for characterizing PHFs, based on the location of the fracture, involvement of the glenohumeral joint line, and the number of bone fragments [10]. This classification allows for the differentiation of extra-articular two-part fractures, extra-articular three-part fractures, and articular four-part fractures. Another important classification system, the Neer classification, focuses on four main segments of the proximal humerus: the humeral head, the greater tuberosity, the lesser tuberosity, and the humeral shaft. In addition to evaluating fragment displacement, the Neer classification includes six fracture groups, with three-part and four-part fractures comprising approximately 20% of PHFs and representing the most challenging cases to manage [11,12].
About the treatment of these fracture patterns, various approaches are currently available. Surgical options include open reduction internal fixation (ORIF), hemiarthroplasty (HA), and reverse total shoulder arthroplasty (rTSA). However, non-surgical treatment (NST), involving immobilization with a standard sling, cuff and collar, or hanging arm cast, remains a controversial choice for these complex fractures [13]. The optimal treatment modality for these fractures continues to be a topic of debate [14].
During the COVID-19 pandemic, there was a notable increase in the adoption of conservative treatments, especially for PHFs [9]. Factors such as the fear of contracting the virus or the limited availability of hospital beds and operating rooms influenced this trend [15]. However, the effectiveness of non-surgical treatment for repairing osteopenic three- and four-part PHFs remains a subject of ongoing debate [9].
This article aims to provide a comprehensive analysis of the impact of the COVID-19 pandemic on PHFs. We will review the evolving epidemiology, changes in fracture patterns, diagnostic challenges, and treatment considerations for PHFs in the context of the pandemic. Furthermore, we will discuss strategies and adaptations implemented in orthopedic practice to ensure timely and appropriate management of PHFs, while ensuring the safety of both patients and healthcare providers. The objective of the study is to evaluate the functional outcome of patients older than 65 years who underwent conservative treatment for PHFs in our department during the spread of COVID-19. Additionally, the secondary endpoint is to identify potential complications associated with NST in these fractures.
2. Materials and Methods
We conducted a retrospective analysis on patients who accessed the Emergency Room of the “Hospital Marino di Alghero” (Sassari, Italy) between 9 March 2020 and 18 May 2020. The study included patients who were diagnosed with a PHF and subsequently treated conservatively (Figure 1). Inclusion criteria consisted of a low-energy 3- or 4-part fracture based on Neer’s shoulder classification, and 11-B or 11-C according to the OTA/AO classification; patients over 65 years old; conservative treatment of the PHF; a minimum follow-up period of 30 months. Cases with a history of injury or illness affecting the ipsilateral shoulder were excluded. We did not collect data related to COVID-19 infection in patients as it was not considered a factor that could positively or negatively affect fracture healing.
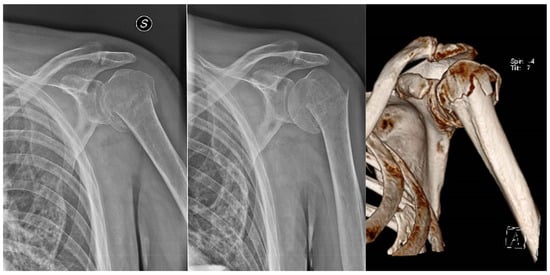
Figure 1.
An 11-C3 fracture according to AO/OTA classification, typically requiring surgical correction.
Demographic data, including age, side of fracture, concomitant injuries, and morbidities, were collected for all patients. Clinical records and radiographs from the time of injury to the present were retrieved for analysis.
In the examined period, we found 11 patients with PHF, but according to the inclusion/exclusion criteria, we removed 4 of them from the cohort: 2 cases did not meet all the inclusion criteria and the other 2 were lost during follow-up. Among the 7 included patients, 3 were women (42.3%) and 4 men (57.7%), with a mean age of 79.8 years SD: 8.77.
The NST protocol involved immobilization in a Gilchrist bandage with the arm against the chest for the initial 30 days. An intermediate radiographic control and orthopedic evaluation were conducted after 7–10 days to monitor for secondary fracture displacement or other possible complications. Subsequent radiographic checks and outpatient visits were scheduled at 1, 3, and 6 months after the injury. Following the removal of the Gilchrist bandage, a 5-week program of daily 1-on-1 rehabilitation sessions with a physiotherapist was implemented to restore function. The rehabilitation protocol included gentle and active-assisted range of motion exercises for the first 2 or 3 weeks, followed by progressive resistive exercises. The final phase of rehabilitation encompassed autonomous rehabilitation with recommended home exercises.
Due to the lockdown measures and restrictions imposed during the spread of COVID-19, some patients encountered difficulties in accessing physiotherapy sessions and adhering to the planned rehabilitation timeline.
In May 2024, all patients were recalled for X-ray control and a follow-up visit 48 months after their injury. The pain was analyzed using the VAS scale, while objective evaluations were performed using three well-known shoulder scores:
Constant Shoulder Score (CSS): This multi-item functional scale assesses pain, activities of daily living (ADL), range of motion (ROM), and strength of the shoulder. The score ranges from 0 to 100 points, with higher scores indicating better shoulder function [16].
Oxford Shoulder Score (OSS): The OSS is a validated scoring system used to assess the degree of pain and disability caused by shoulder pathology [17]. It provides a total score ranging from 0 (worst outcome) to 48 (best outcome) based on the patient’s subjective assessment of pain and function [17].
Disabilities of Arm, Shoulder, and Hand Score (DASH): The DASH survey was developed as a measure of self-rated upper-extremity disability and symptoms, with scores ranging from 0 (no disability) to 100 (worst outcome) [18].
The primary focus of this study was to evaluate the functional scores of patients during the follow-up period, which reflect their shoulder abilities and recovery. Secondary endpoints included rates of additional surgeries and adverse events.
3. Results
The information about the cohort, the affected arm and the final scores is reported in Table 1 and Table 2.

Table 1.
General information about patients and affected arm.

Table 2.
Scores and range of movement.
All patients included in the study underwent anterior–posterior, scapular Y, and axillary X-ray imaging of the affected shoulder in the Emergency Room. Among the patients, two presented with concomitant traumas: one had fractures of the distal ulna and radius in the same arm, while the other reported a hip fracture and an ipsilateral olecranon fracture.
We also observed in the X-ray imaging that when tuberosities were fractured, the greater tuberosity tended to displace postero-superiorly and the lesser tuberosity displaced medially [19].
During the intermediate radiographic checks, one patient exhibited excessive fracture displacement, necessitating subsequent surgical fixation. In this case, open reduction and internal fixation with an intramedullary nail were performed.
In terms of the evaluation scores, the average CSS was found to be 69.4 (SD: 22.34), indicating moderate shoulder function. The DASH had an average value of 27.9 (SD: 30.26), reflecting relatively low levels of upper-extremity disability and symptoms. The OSS averaged at 34 (SD: 14.56) at 2 years. It is worth noting that Amar Rangan et al., in their study, reported an average OSS value of 40.40 for non-surgically treated patients, which is slightly higher than our recorded OSS value of 34 [20].
Only two patients failed to achieve a minimum shoulder flexion and adduction of 90° at the 2-year follow-up. One patient had no union of the greater tuberosity at the follow-up. He was 93 years old with extremely poor functional demands and multiple comorbidities including ictus and dementia. For these reasons, we decided to not pursue surgical treatment. No other adverse events were reported during the study period.
These findings highlight the functional outcomes of conservative treatment for PHFs in our patient cohort. The CSS, DASH, and OSS scores provide a comprehensive assessment of shoulder function, disability, and pain. While our results demonstrate relatively favorable outcomes, further investigation and comparison with other studies are needed to fully evaluate the effectiveness of conservative treatment for PHFs.
4. Discussion
The optimal treatment for three- and four-part fractures of the proximal humerus in patients with poor bone quality remains a subject of controversy [21]. The COVID-19 pandemic caused an increase in indications for conservative treatment in many fractures, and in particular for those of the proximal humerus [15]. This trend has given us the opportunity to evaluate the outcome of NST in fractures that we would usually have treated surgically.
In our study, we found that NST was associated with a lower rate of adverse events and additional surgery, as well as good functional scores (Figure 2). Nevertheless, other studies such as that of Due et al. reported good outcome after reverse shoulder arthroplasty, while open reduction and internal fixation did not achieve the same results [14].
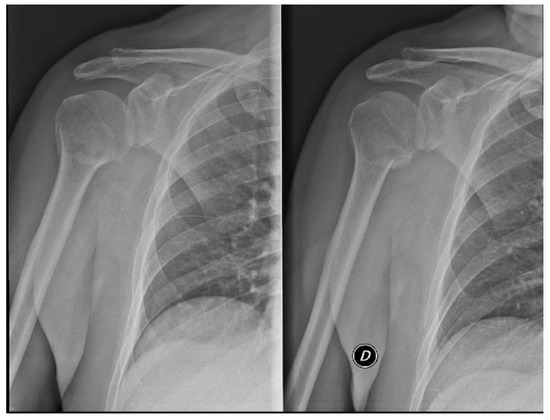
Figure 2.
Three-part fracture/11-B1.1, managed with non-surgical treatment; result after one month.
Among the patients with displaced PHFs involving the surgical neck, we registered a good outcome after NST, confirmed at the 2-year postoperative outpatient visit, both from a clinical and radiographic point of view.
The correct therapeutic choice for a PHFs remains a challenge for surgeons; in fact, expert surgeons also do not concur on the ideal treatment for this type of fracture [22]. In their study, Jawa et al. demonstrated that among orthopedic surgeons, the agreement with treatment decisions about PHFs was poor. In fact, they calculated the so-called intraclass correlation coefficient (ICC), in which a result under 0.2 indicates poor agreement, founding an ICC of 0.14 [22].
In elderly subjects with poor bone quality and comorbidities, prosthetic replacement can be a viable option [23]; however, surgical interventions expose patients with comorbidities to additional risks, making the conservative approach a viable option that surgeons have to consider in some cases [24].
The COVID-19 pandemic has had a profound impact on healthcare systems worldwide, affecting various aspects of patient care, including the management of fractures. Among these, PHF represents a significant challenge due to its high incidence and potential complexity [15]. Understanding the implications of the pandemic on the presentation, treatment, and outcomes of PHFs is crucial for optimizing patient care during these unprecedented times [15,24].
We need to emphasize that the difficulties stem from the pandemic’s social, economic, and health repercussions rather than the infectious disease itself [15]. PHFs, accounting for a substantial proportion of fractures, have shown a changing pattern in incidence and characteristics during the COVID-19 era. With the implementation of strict public health measures and restrictions on mobility, changes in lifestyle and activity levels resulted in alterations in the mechanisms of injury [24]. Reduced physical activity and an increased emphasis on home-based environments led to a potential shift towards low-energy fractures, particularly among older individuals. Additionally, delayed presentation to healthcare facilities, fear of nosocomial infection, and limited access to elective surgical procedures further complicated the management of PHFs [15].
During the pandemic period, we noticed a double advantage of NST: a lower risk of exposure in an environment with high risks of infection, and an important reduction in hospital costs. In particular, the latter was especially due to not having performed the surgery; thus, all the related expenses such as utilization of the operating room, surgical instruments and medical equipment were spared. Furthermore, the patients’ avoidance of hospitalization also contributed to the cost savings. Considering that this type of episode provides an average hospitalization of three days, as estimated by the Ministry of Economics and Finance of 2014, in our region, it would lead to savings of EUR 2163 only for a hospital stay for every patient [25].
We also noticed that the worst outcome occurred in the patient who did not present an adequate healing of the greater tuberosity (Figure 3). This issue confirms that a complete healing of the greater tuberosity is crucial to restore good function of the limb, particularly because it is the insertion of superior and posterior rotator cuff tendons [26].

Figure 3.
Failure of the greater tuberosity to heal is linked to lower results.
It is crucial to weigh the potential benefits and risks of surgical interventions, especially in elderly patients. Surgeons have to take into account the patient’s overall health status, bone quality, functional demands, and also preferences. Shared decision-making between the patient, the orthopedic surgeon, and the healthcare team is essential in determining the most appropriate treatment approach [27].
The treatment protocol we usually adopt includes four weeks of immobilization, usually in a Desault brace or figure-eight bandage. This duration is meant to stabilize the fracture and reduce the pain. However, the literature stresses early mobilization to prevent joint stiffness and frozen shoulder syndrome. After the first few weeks of immobilization, the introduction of Codman’s pendulum exercises is recommended to maintain passive mobility. Gradually, in later weeks, there is a gradual shift to assisted-active and, subsequently, to active and progressive muscle-strengthening exercises. Rehabilitation plays a role in the restoration of joint mobility and strength of the muscles, with physiotherapy programs aimed at scapulohumeral mobility and strengthening of the rotator cuff and deltoid muscles.
There have been various studies comparing the effectiveness of conservative versus surgical treatment for fractures of the proximal humerus. In a multicenter randomized trial (PROFHER trial), Rangan et al. demonstrated that in elderly patients with non-displaced or moderately displaced fractures, conservative management leads to the same functional outcomes as with surgery but with fewer complications [20]. Another study by Launonen et al. in 2019 again confirmed that in patients over 65 years of age, the quality of life and long-term shoulder function are not significantly varied in conservative and surgical treatment [5]. A 2021 Cochrane review conducted by Handoll et al. noted that surgery is not necessarily guaranteed to lead to functional improvement compared to conservative management and that complications such as stiffness, chronic pain, infections, and implant failure are more frequent in surgically treated patients [21].
The study has several limitations: first of all, the cohort of patients is small and comprehensive for a limited period of time. This is because we focused our attention on the spread of COVID-19. We acknowledge that the small sample size limits the generalizability of our findings. However, given the unique circumstances of the COVID-19 pandemic and the limited availability of comparable cases, we believe that our study still provides valuable insights on proximal humerus fractures. Moreover, we recognize that the lack of a control group is a limitation, but due to the limited and peculiar time frame analyzed, it was not feasible to include one. Due to the small sample, it was also not possible to perform a significant statistical analysis.
On the other hand, a boon of the study is that we recalled all patients who underwent both a clinical examination and a radiographic check. Moreover, the time frame analyzed is also very narrow, but it allows us to analyze only the pandemic period, in which surgical indications were very limited.
5. Conclusions
Overall, our study supports the importance of considering conservative treatment as a valuable option for three- and four-part fractures of the proximal humerus in patients with poor bone quality, particularly in the elderly population with comorbidities. NST demonstrated favorable outcomes with lower rates of adverse events and additional surgeries. This approach can provide a valuable alternative for elderly patients with comorbidities who may be at higher risk for surgical complications.
Conservative treatment of proximal humerus fractures remains an effective therapeutic option in many situations, particularly in elderly patients and those with minimally displaced fractures. Treatment selection should be personalized, considering fracture morphology, the patient’s general condition, and long-term functional expectations. A well-structured protocol, including early mobilization and appropriate rehabilitation, is essential to optimize functional recovery and minimize the risk of joint stiffness.
Further research is needed to compare the long-term outcomes of conservative and surgical treatments in this specific patient population. Randomized controlled trials with larger sample sizes and longer follow-up periods will provide more robust evidence for guiding treatment decisions in patients with poor bone quality and complex proximal humerus fractures.
Author Contributions
Conceptualization, G.C., A.Z. and C.C.; methodology, G.C., A.Z. and C.C.; software, A.Z. and C.C.; validation, G.C., A.Z., G.M., F.Q. and C.C.; formal analysis, G.C., A.Z. and C.C.; investigation, G.C. and A.Z.; data curation, G.C. and A.Z.; writing—original draft preparation, G.C., A.Z. and C.C.; writing—review and editing, G.C., A.Z. and C.C.; visualization, C.C.; supervision, G.M. and F.Q. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were waived for this study because it is a retrospective case series, whose data are totally anonymized.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author(s).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PHF | Proximal humerus fracture |
| ORIF | open reduction internal fixation |
| HA | hemiarthroplasty |
| rTSA | reverse total shoulder arthroplasty |
| NST | non-surgical treatment |
| CSS | Constant Shoulder Score |
| OSS | Oxford Shoulder Score |
| DASH | Disabilities of Arm, Shoulder, and Hand Score |
| ICC | intraclass correlation coefficient |
References
- Passaretti, D.; Candela, V.; Sessa, P.; Gumina, S. Epidemiology of proximal humeral fractures: Detailed survey of 711 patients in a metropolitan area. J. Shoulder Elb. Surg. 2017, 26, 2117–2124. [Google Scholar] [CrossRef]
- Tarallo, L.; Micheloni, G.M.; Giorgini, A.; Lombardi, M.; Limone, B.; Catani, F.; Porcellini, G. Anatomically reduced fixation should always be considered when treating B and C proximal epiphyseal humeral fractures. J. Orthop. Traumatol. 2022, 23, 51. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Corbacho, B.; Duarte, A.; Keding, A.; Handoll, H.; Chuang, L.H.; Torgerson, D.; Brealey, S.; Jefferson, L.; Hewitt, C.; Rangan, A. Cost effectiveness of surgical versus non-surgical treatment of adults withdisplaced fractures of the proximal humerus: Economic evaluation alongside the PROFHER trial. Bone Jt. J. 2016, 98-B, 152–159. [Google Scholar] [CrossRef]
- Ellerbrock, M.; Theil, C.; Gosheger, G.; Deventer, N.; Klingebiel, S.; Rickert, C.; Schneider, K.N. Function and return to sports after proximal humeral replacement in patients with primary bone sarcoma. J. Orthop. Traumatol. 2022, 23, 59. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Launonen, A.P.; Fjalestad, T.; Laitinen, M.K.; Lähdeoja, T.; Ekholm, C.; Wagle, T.; Mattila, V.M.; NITEP-group. Nordic Innovative Trials to Evaluate osteoPorotic Fractures (NITEP) Collaboration: The Nordic DeltaCon Trial protocol-non-operative treatment versus reversed total shoulder arthroplasty in patients 65 years of age and older with a displaced proximal humerus fracture: A prospective, randomised controlled trial. BMJ Open 2019, 9, e024916. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Launonen, A.P.; Lepola, V.; Saranko, A.; Flinkkilä, T.; Laitinen, M.; Mattila, V.M. Epidemiology of proximal humerus fractures. Arch. Osteoporos. 2015, 10, 209. [Google Scholar] [CrossRef] [PubMed]
- Warriner, A.H.; Patkar, N.M.; Curtis, J.R.; Delzell, E.; Gary, L.; Kilgore, M.; Saag, K. Which fractures are most attributable to osteoporosis? J. Clin. Epidemiol. 2011, 64, 46–53. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Calvo, E.; Morcillo, D.; Foruria, A.M.; Redondo-Santamaría, E.; Osorio-Picorne, F.; Caeiro, J.R.; in representation of the GEIOS-SECOT Outpatient Osteoporotic Fracture Study Group. Nondisplaced proximal humeral fractures: High incidence among outpatient-treated osteoporotic fractures and severe impact on upper extremity function and patient subjective health perception. J. Shoulder Elb. Surg. 2011, 20, 795–801. [Google Scholar] [CrossRef]
- Maier, D.; Jaeger, M.; Izadpanah, K.; Strohm, P.C.; Suedkamp, N.P. Proximal humeral fracture treatment in adults. J. Bone Jt. Surg. Am. 2014, 96, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.E.; Nazarian, S.; Koch, P. Classification AO des fractures. Tome I. Les os Longs; Springer: Berlin, Germany, 1987; pp. 11–20. [Google Scholar]
- Carofino, B.C.; Leopold, S.S. Classifications in brief: The Neer classification for proximal humerus fractures. Clin. Orthop. Relat. Res. 2013, 471, 39–43. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Naranja, R.J., Jr.; Iannotti, J.P. Displaced three- and four-part proximal humerus fractures: Evaluation and management. J. Am. Acad. Orthop. Surg. 2000, 8, 373–382. [Google Scholar] [CrossRef]
- Orman, S.; Mohamadi, A.; Serino, J.; Murphy, J.; Hanna, P.; Weaver, M.J.; Dyer, G.; Nazarian, A.; von Keudell, A. Comparison of surgical and non-surgical treatments for 3- and 4-part proximal humerus fractures: A network meta-analysis. Shoulder Elb. 2020, 12, 99–108. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Du, S.; Ye, J.; Chen, H.; Li, X.; Lin, Q. Interventions for Treating 3- or 4-part proximal humeral fractures in elderly patient: A network meta-analysis of randomized controlled trials. Int. J. Surg. 2017, 48, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Maniscalco, P.; Ciatti, C.; Gattoni, S.; Quattrini, F.; Pagliarello, C.P.; Patane’, A.C.; Capelli, P.; Banchini, F.; Rivera, F.; Sanna, F.; et al. Proximal humerus fractures in COVID-19 lockdown: The experience of three orthopedics and traumatology departments in the first ten weeks of the Italian epidemic. Acta Biomed. 2021, 92, e2021104. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vrotsou, K.; Ávila, M.; Machón, M.; Mateo-Abad, M.; Pardo, Y.; Garin, O.; Zaror, C.; González, N.; Escobar, A.; Cuéllar, R. Constant-Murley Score: Systematic review and standardized evaluation in different shoulder pathologies. Qual. Life Res. 2018, 27, 2217–2226. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Younis, F.; Sultan, J.; Dix, S.; Hughes, P.J. The range of the Oxford Shoulder Score in the asymptomatic population: A marker for post-operative improvement. Ann. R. Coll. Surg. Engl. 2011, 93, 629–633. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gummesson, C.; Atroshi, I.; Ekdahl, C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet. Disord. 2003, 4, 11. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sanchez-Sotelo, J. Proximal humerus fractures. Clin. Anat. 2006, 19, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Rangan, A.; Handoll, H.; Brealey, S.; Jefferson, L.; Keding, A.; Martin, B.C.; Goodchild, L.; Chuang, L.H.; Hewitt, C.; Torgerson, D.; et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: The PROFHER randomized clinical trial. JAMA 2015, 313, 1037–1047. [Google Scholar] [CrossRef] [PubMed]
- Handoll, H.H.; Brorson, S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst. Rev. 2022, 6, CD000434. [Google Scholar] [CrossRef] [PubMed]
- Jawa, A.; Yi, P.H.; Boykin, R.E.; Gardner, M.J.; Gerber, C.; Lorich, D.G.; Walch, G.; Warner, J.J. Treatment of proximal humerus fractures: Comparison of shoulder and trauma surgeons. Am. J. Orthop. 2015, 44, 77–81. [Google Scholar] [PubMed]
- Troiano, E.; Peri, G.; Calò, I.; Colasanti, G.B.; Mondanelli, N.; Giannotti, S. A novel “7 sutures and 8 knots” surgical technique in reverse shoulder arthroplasty for proximal humeral fractures: Tuberosity healing improves short-term clinical results. J. Orthop. Traumatol. 2023, 24, 18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maniscalco, P.; Quattrini, F.; Ciatti, C.; Gattoni, S.; Pagliarello, C.P.; Burgio, V.; Di Stefano, G.; Cauteruccio, M.; Giovanelli, M.; Magro, A.; et al. The Italian Covid-19 Phase 2 in Piacenza: Results of the first semester of 2020 and future prospective of new orthopedics surgical procedures. Acta Biomed. 2020, 91, e2020159. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ministero dell’Economia e delle Finanze. Libro Verde Sulla Spesa Sanitaria; Alcuni Esempi Settoriali: Rome, Italy, 2007. Available online: http://www.mef.gov.it/ministero/commissioni/ctfp/documenti/Libro_verde_spesa_pubblica.pdf (accessed on 22 March 2023).
- Mostowfi Zadeh, D.; Abdelghafour, K.; Assiotis, A. Proximal Humerus Fracture/Dislocation: Look for the Greater Tuberosity. Cureus 2023, 15, e33795. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- COVIDSurg Collaborative, Machine learning risk prediction of mortality for patients undergoing surgery with perioperative SARS-CoV-2: The COVIDSurg mortality score. Br. J. Surg. 2021, 108, 1274–1292. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).