Abstract
Background/Objectives: An 80-year-old man was admitted to our department after a salvage radical cystectomy for actinic cystitis due to radiotherapy for prostate cancer. He presented with a two-month history of feculent debris in the right stoma and deteriorated general conditions, after a long past medical history of recurrent complicated urinary infections. Methods: Computer tomography (CT) of the abdomen revealed a ureterocolic fistula along the right ureteral pelvic tract. A right percutaneous nephrostomy tube was placed. Due to multiple previous surgeries, several lines of intravenous antibiotic therapies and the overall condition of the patient, a conservative management was preferred. Results: A bovine serum albumin-glutaraldehyde (BioGlue®) adhesive was inoculated into the right ureter through the stoma to close the fistula. After 24 months, the patient remained asymptomatic with negative follow-up imaging. Conclusions: Given the uniqueness of the management of a ureterocolic fistula, this case offers insight into conservative treatment in frail patients not suitable for major surgery.
1. Introduction
Fistulous complications represent a rare event following radical cystectomy (RC), developing in 0.3% to 2.6% of cases. Few cases are described after orthotopic ileal neobladder reconstruction [1] while no data have been reported in the literature regarding management and treatment of a ureterocolic fistula after RC with ureterocutaneostomy (UCS) diversion. A case report showed the use of Bioglue® to close a ureterocutaneous fistula in association with Deflux®, a dextranomer/hyaluronic acid copolymer endoscopically injected, while the Bioglue® was injected to close the fistula from the ureter to the skin [2].
The use of Bioglue® was also assessed by Z. Bahouth et al. in renal mass enucleation in a retrospective comparison series, showing that is feasible and safe [3]. As mentioned, conservative treatment has only anecdotally been reported in the context of ureterocolic fistula, with open revision remaining the standard of care, regardless of the high number of frail patients not eligible for open surgery [4].
2. Case Presentation
2.1. Patient Characteristics and Clinical Findings
An 80-year-old man presented to our department with a two-month history of feculent debris appearing in the urine of the right stoma. About 10 years earlier, the patient underwent radical prostatectomy with regional lymphadenectomy, and the pathology exam showed a prostatic adenocarcinoma Gleason grade 7 (3 + 4) with extracapsular infiltration on the right lobe of the prostate, but with negative resection margins. Pelvic lymph nodes were negative for metastasis. The final pathological stage was pT3a, pN0.
The PSA after 6 months was 0.2 ng/mL, but at the 10th month post operation, he received a cycle of pelvic radiotherapy and androgen deprivation therapy (ADT) due to biochemical recurrence (BCR), with increased PSA at 0.48 ng/mL.
At the 3rd year he became resistant to ADT, had another BCR and started the bipolar androgen therapy (BAT). After 2 years, he received a cycle of stereotactic body radiation treatment (SBRT) on two bone metastases. From 2018 he started to have symptoms of actinic cystitis and recurrent urinary tract infections (UTIs), which responded poorly to intravenous antibiotic therapy. In May 2021 he was admitted to the emergency department for persistent fever, chills and lower abdominal pain. A vesicocutaneous fistula due to a retropubic abscess was diagnosed and surgically drained after bilateral percutaneous nephrostomy (PCN) tube placement. In August 2021, the patient underwent a salvage RC with bilateral UCS diversion with the removal of both PCNs. After a few months, feculent debris appeared in the urine of the right stoma. An abdominal CT scan with intravenous iodinated contrast revealed a ureterocolic fistula involving the cecal part of the colon and the right ureteral pelvic tract, with iodinated contrast leakage into the intestinal lumen (Figure 1).

Figure 1.
Abdominal CT scan reveals the leakage of iodinated contrast into the intestinal lumen consistent with ureterocolic fistula between the right ureteral tract and the cecum.
2.2. Treatment
The patient was elected for a surgical repair and a right PCN was immediately placed, with leakage of fecal material. The initial plan was to perform a right hemicolectomy with right ureteral exeresis, with or without homolateral nephrectomy. After a multidisciplinary assessment based on the patient’s performance status and life expectancy, a minimally invasive endoscopy treatment was proposed. Firstly, under deep sedation, iodinated contrast was injected through both the PCN and the right stoma; the combined pyelography confirmed the presence of a ureterocecal fistula at the L3–L4 spinal level (Figure 2). A 5 mL syringe of commercial purified bovine serum albumin (BSA) and glutaraldehyde surgical adhesive (BioGlue®, CryoLife, Inc., Atlanta, GA, USA) was aseptically injected from the right stoma through a dual lumen catheter in the right ureter under X-ray image acquisition (Figure 3). From the right PCN, air was injected to avoid the ascent of the BioGlue® adhesive agent into the renal pelvis, maintaining the BioGlue at the communication point between the right ureter and the bowel.
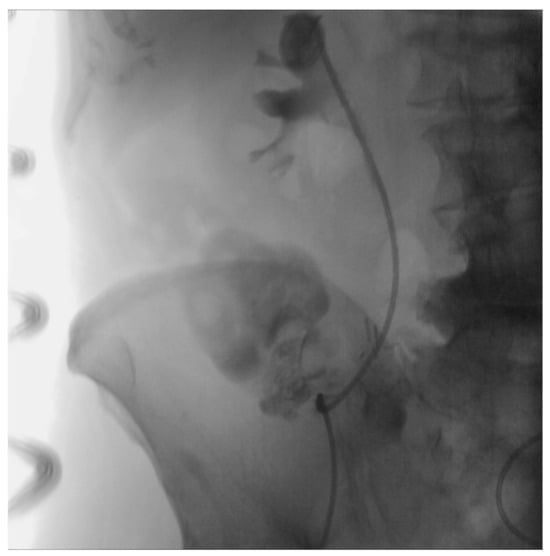
Figure 2.
Retrograde pyelography confirms the presence of a ureterocolic fistula at the L3–L4 spinal level.
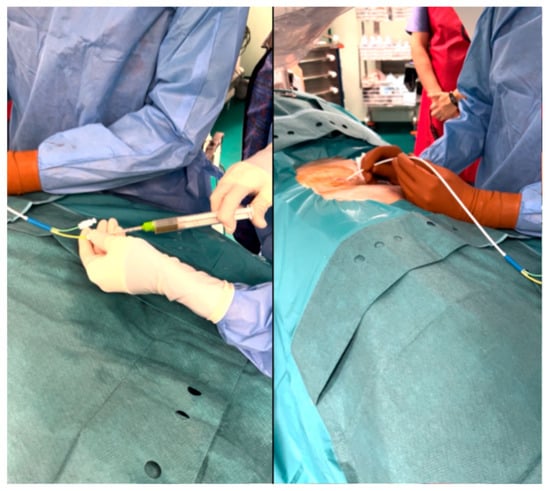
Figure 3.
BioGlue® endoscopic injection from the right stoma through a dual lumen catheter in the right ureter.
2.3. Outcome and Follow-Up
Following the procedure, the patient underwent a 48 h course of large-spectrum antibiotic therapy and was then discharged without complications. After 1 month, he had a complete resolution of stooling from the right stoma, with clear urine drainage from the right PCN and left stoma. At 5-, 12- and 24-month follow-up he remained asymptomatic with a silent right stoma and negative imaging (Figure 4). The patient is currently under the care of a dedicated nephrologist to monitor his renal function. He replaces the right PCN and the left ureteral catheter every three months at our center.
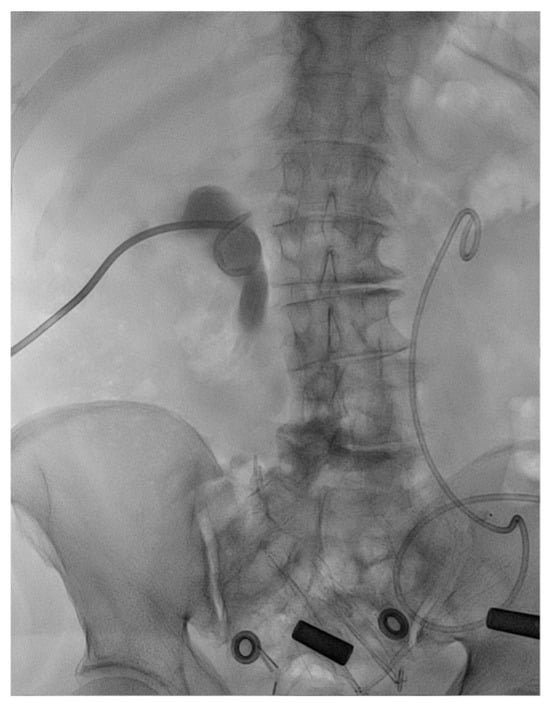
Figure 4.
Retrograde pyelography at 24 months after BioGlue® injection without evidence of residual fistula.
3. Discussion
Given the low incidence of fistula formation after RC, management strategies and outcomes are poorly defined in the literature. Typically, a patient with an abnormal connection between the urinary and the digestive tract presents with pneumaturia, fecaluria and recurrent UTIs; however, the diagnosis in patients with urinary diversion is often not as straightforward [5]. Diagnosis can be challenging, and it is usually confirmed by a contrast-enhanced abdomino-pelvic CT scan [5]. Conservative management based on oral antibiotics, continuous urine drainage, and a low-residue diet could be an option in asymptomatic patients with small fistulas [6]; however, laparotomic surgical revision remains the standard of care for urinary diversion-enteric fistulas. This consists of resection of the affected bowel tract and reconstitution of the bowel transit [4].
The aetiology of the ureterocolic fistula system seems to be multifactorial: it may be secondary to prior surgical intervention, radiation therapy, Crohn’s disease [7], diverticulitis [8], or obstructing ureteral calculi [9]. In our case, we attributed the fistula to multiple causes: first, to the patient’s previous abdominal surgery (radical prostatectomy) followed by a salvage pelvic radiotherapy; second, to the large inflammatory state of the tissues due to recurrent complicated UTIs.
During the last few years, several tissue sealants have been developed to improve homeostasis. BioGlue® is a bovine serum albumin-glutaraldehyde surgical adhesive agent [10]; it is a well-known sealant agent and has widely been used in vascular and cardiac surgery [11]. A previous case report has explored conservative management strategies using tissue adhesives. For example, BioGlue® has been successfully used to occlude uretero-cutaneous fistulas in renal transplant recipients, with complete resolution of leakage and no subsequent infections reported [2].
A similar application of BioGlue® outside the field of urology has been reported in the management of rectovaginal fistulas. In one case, a 45-year-old patient was successfully treated with BioGlue®, leading to complete resolution of symptoms. Additionally, other reports have demonstrated the potential efficacy of BioGlue® in the treatment of anal fistulas, suggesting a broader utility of this tissue adhesive across various types of fistulous disease [12,13].
In urology, it was used for tumor bed closure after partial nephrectomy, during which BioGlue® application was shown to be a feasible and safe technique that can shorten ischemia time and potentially reduce the transfusion rate [3,14]. In our scenario, BioGlue® was endoscopically injected through the stoma to occlude the ureteral lumen in the tract where the fistula is located to effectively close the ureterocecal fistula. The renal pelvis was free of the glue due to the air that was inflated through the PCN during the procedure. Renal function was preserved. The continuous drainage of urine was assessed through the permanently placed PCN.
4. Conclusions
We demonstrate for the first time the feasibility, safety and long-term outcomes of the use of BioGlue® to treat a ureterocolic fistula developed after RC with UCS diversion. This approach offers a noninvasive treatment without resorting to laparotomy and surgical repair, with clear benefits for the patient. Although the use of BioGlue® may not be suitable for all situations, it offers a valuable treatment alternative for selected patients with multiple comorbidities.
Author Contributions
Conceptualization, C.R., R.M. and R.B.; resources: G.R., G.A. and N.L.; writing—original draft preparation, C.R. and P.S.; writing—review and editing, G.R., A.S., F.M. and R.B; supervision, R.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
All data generated during this report are included in this published article. Further enquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
RC, radical cystectomy; UCS, ureterocutaneostomy; UTI, urinary tract infection; PCN, percutaneous nephrostomy.
References
- Smith, Z.L.; Johnson, S.C.; Golan, S.; McGinnis, J.R.; Steinberg, G.D.; Smith, N.D. Fistulous Complications following Radical Cystectomy for Bladder Cancer: Analysis of a Large Modern Cohort. J. Urol. 2018, 199, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Mastromichalis, M.H.; Frazzini, P.; Newall, P.M. Successful endoscopic management of a chronic transplant ureterocutaneous fistula. Urology 2011, 78, 952–953. [Google Scholar] [PubMed]
- Bahouth, Z.; Moskovitz, B.; Halachmi, S.; Nativ, O. Bovine serum albumin-glutaraldehyde (BioGlue®) tissue adhesive versus standard renorrhaphy following renal mass enucleation: A retrospective comparison. Ther. Adv. Urol. 2017, 9, 67–72. [Google Scholar] [PubMed]
- Msezane, L.; Reynolds, W.S.; Mhapsekar, R.; Gerber, G.; Steinberg, G. Open surgical repair of ureteral strictures and fistulas following radical cystectomy and urinary diversion. J. Urol. 2008, 179, 1428–1431. [Google Scholar] [CrossRef]
- Scozzari, G.; Arezzo, A.; Morino, M. Enterovesical fistulas: Diagnosis and management. Tech. Coloproctol. 2010, 14, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.S.; Klein, E.A. Conservative management of an ileal neobladder-enteric fistula. Urology 1999, 54, 366. [Google Scholar] [CrossRef] [PubMed]
- El Khader, K.; Karmouni, T.; Guillé, F.; Lobel, B. Ureteroileal fistula: An unusual complication of Crohn’s disease. Acta Gastroenterol. Belg. 2000, 63, 312–313. [Google Scholar] [PubMed]
- Leicht, W.; Thomas, C.; Thüroff, J.; Roos, F. Colovesical fistula caused by diverticulitis of the sigmoid colon: Diagnosis and treatment. Urologe A 2012, 51, 971–974. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.K.; Chang, S.D.; Roche, C.J.; Duddalwar, V.A.; Rowley, V.A.; McLoughlin, M.G. Spontaneous ureterocolic fistula secondary to calculous pyohydroureteronephrosis. Br. J. Radiol. 2005, 78, 954–955. [Google Scholar] [CrossRef] [PubMed]
- Bioglue CryoLife Inc. BioGlue Surgical Adhesive; Medical Information; IFU for BioGlue Surgical Adhesive (USA). Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/p010003b.pdf (accessed on 2 February 2020).
- Mitrev, Z.; Belostotskii, V.; Hristov, N. Suture line reinforcement using suction-assisted bioglue application during surgery for acute aortic dissection. Interact. Cardiovasc. Thorac. Surg. 2007, 6, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Garcia, S.; Dissanaike, S. Case report: Treatment of rectovaginal fistula with Bioglue(®). Int. J. Surg. Case Rep. 2012, 3, 327–329. [Google Scholar] [CrossRef] [PubMed]
- Van Koperen, P.J.; Bemelman, W.A.; Gerhards, M.F.; Janssen, L.W.; van Tets, W.F.; van Dalsen, A.D.; Slors, J.F.M. The anal fistula plug treatment compared with the mucosal advancement flap for cryptoglandular high transsphincteric perianal fistula: A double-blinded multicenter randomized trial. Dis. Colon. Rectum. 2011, 54, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Hidas, G.; Kastin, A.; Mullerad, M.; Shental, J.; Moskovitz, B.; Nativ, O. Sutureless nephron-sparing surgery: Use of albumin glutaraldehyde tissue adhesive (BioGlue). Urology 2006, 67, 697–700; discussion 700. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).