1. Introduction
Supracondylar fracture of the humerus is probably the most common fracture around the elbow in children. The reported incidence is about 3% of all fractures in children and nearly 60% of all elbow fractures. It is most common in children aged 5 to 7 years old, with the non-dominant hand more frequently involved. No substantial difference was observed between boys and girls [
1,
2,
3,
4].
Patients with supracondylar humeral fracture usually present with pain and swelling around the elbow, with or without visible deformity. A subcutaneous hematoma may also be visible. Motion of the elbow is painful and limited. Examination should include assessment of the skin condition (for presence of any open wounds), examination of the whole limb for other fractures, as well as neurologic and vascular examination. Supracondylar fractures are most associated with distal radial fractures. The risk of forearm compartment syndrome is increased in children with a combination of supracondylar and diaphyseal forearm fractures. Neurologic examination is challenging, especially in smaller children, but important. While most neurologic deficits observed at the time of injury are temporary and resolve spontaneously within 3 months, any change in neurologic exam after surgery may indicate nerve injury or entrapment during manipulation and pinning. Vascular status is assessed by palpating the distal radial and ulnar pulse, or in their absence by capillary refill and skin temperature and color examination (sufficient perfusion in the absence of pulse is commonly described as pink pulseless hand) [
3].
There are two main types of pediatric supracondylar fractures, divided according to the direction of displacement of the distal fragment (distal humerus) relative to the proximal fragment (humeral shaft) in the sagittal plane. In extension-type fractures, the distal fragment is displaced posteriorly. Extension-type fractures are the most common subtype; they usually occur because of a fall on an outstretched hand while the elbow is in full extension, and account for almost 98% of all supracondylar fractures. The second type is the flexion type, wherein the distal fragment is displaced anteriorly. Flexion-type fractures usually occur because of a direct blow to the elbow, and they account for approximately 2% of supracondylar fractures [
5,
6,
7,
8].
The diagnosis of supracondylar humeral fracture is usually established using radiography. Two X-rays centered on the elbow are performed: an anterior-posterior (AP) view and a lateral view. On the X-rays, the direction, extent of displacement, and any rotational abnormalities are noted. The fracture is classified into a flexion or extension subtype based on lateral X-ray. The anterior humeral line is the main radiographic line used for diagnosis. This line is drawn along the anterior humeral cortex on a lateral radiograph and then extended down across the capitellum. In a healthy elbow, this line should cross the capitellum in its middle third in any patient older than 4 years, though it may lie in the anterior third of the capitellum in children younger than 4 years of age [
9].
The most used classification to further describe extension-type fractures is the Gartland classification. This classification divides extension-type fractures into three subtypes based on posterior displacement of the distal fragment (on lateral X-ray): type I fractures are non or minimally displaced; type II fractures are displaced, but still have an intact posterior cortex (also commonly referred to as an intact posterior hinge); and type III fractures are completely displaced without any cortical contact between the fragments. The stability of the fracture decreases from type I to type III [
5,
6,
7,
8]. Later, type II fractures were divided into two further subtypes. Type IIa are fractures that do not have a rotational abnormality, and type IIb have some degree of rotational displacement, making them somewhat less stable than type IIa [
10]. Then, type I fractures were divided into type Ia, which was defined as a true undisplaced fracture, and type Ib, which showed a comminution on the medial side and possibly mild extension on lateral X-ray. The authors raised the concern that type Ib fractures left unreduced could lead to unacceptable deformity [
11]. Then again, another subtype was added to the Gartland classification, named type IV [
12]. This subtype is used to describe completely unstable fractures. These unstable extension-type fractures usually do not have any residual periosteal hinge, and are therefore unstable both in flexion and extension. They appear as type III fractures on initial X-rays; however, intraoperatively, following an attempted standard reduction maneuver (elbow flexion), the distal fragment can translate anterior to the humeral shaft, thus transforming into a flexion-type fracture. As manipulation of the fracture is required to recognize this fracture subtype, it usually is established intraoperatively [
9]. Recently, another classification system was proposed by the Pediatric Expert Group of the AO foundation. This classification describes those fractures based on the number of planes in which the displacement occurred: type I—no displacement; type II—displacement in one plane; type III—displacement in two planes; and type IV—rotation with displacement in three planes [
13]. While this is a very comprehensive classification, to date, it has still not been widely undertaken in practice.
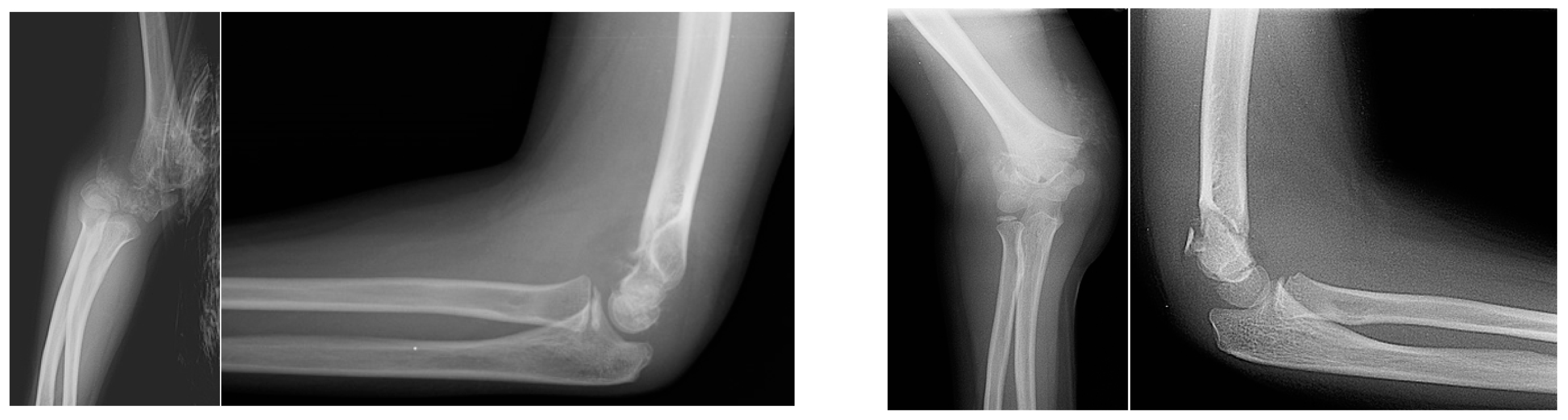
We observed a pediatric supracondylar humeral fracture subtype with sideward translation without any significant sagittal plane displacement on initial radiographs (
Figure 1). This fracture is not clearly described by the most often used Gartland classification system.
The objectives of this study were to describe this fracture subtype, evaluate its incidence, and suggest a modification to the standard operative technique for fracture reduction and fixation of this specific fracture type.
2. Materials and Methods
In this retrospective study, we examined the medical records of all patients who were treated operatively in our institution between the years 2006 and 2014 with the diagnosis of supracondylar fracture of the humerus. All patients younger than 14 years of age with an isolated surgically treated supracondylar humeral fracture were included. Patients with Gartland type I fracture are treated conservatively with a plaster. The management of type IIa fractures is controversial, as these fractures can potentially be treated with manipulation and casting, and then close observation. However, as we cannot be confident about our ability to provide close observation to all our patients, we prefer surgical fixation for those fractures. This is a well-described and common practice [
14]. Type IIb and III fractures, as well as sideward displaced fractures not clearly described by the Gartland classification, are all treated surgically. Thus, by including surgically treated patients only, the patient cohort includes all type II, III fractures and sideward displaced fractures. Multiple trauma patients, open fractures, and floating elbow injuries were excluded.
The data collected from patients’ medical records included age, soft tissue injury, neurovascular injuries, time to surgery, surgical technique used, complications, time to radiologic fracture healing, and time to neurologic recovery.
All images were reviewed by two fellowship trained pediatric orthopedic specialists to provide accurate classification of the fracture subtypes. Fractures were categorized into the sideward displacement group if they met both of the following two criteria: (a) on lateral view, the anterior humeral line crossed the capitellum in the middle or the anterior third; and (b) on anterior-posterior (AP) view, a sideward translation of at least 25% of the width of the distal humeral fragment was observed.
The incidence of sideward displaced pediatric supracondylar humeral fractures was calculated as a percentage of the total number of fractures. The rate of soft tissue damage (e.g., subcutaneous hematoma, skin dimpling, neurological and vascular deficit on admission) was calculated and compared between the sideward displaced fracture group and all other patients. For statistical analysis, Fisher’s exact test and chi-square tests were used (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY, USA: IBM Corp).
The study was approved by the Institutional Review Board.
Operative Technique
Initially, the standard and well-established technique for the reduction and fixation of pediatric supracondylar humeral fractures is described [
14]. With the patient in a supine position, general anesthetic and prophylactic antibiotics are given. The image intensifier is placed on the fractured side adjacent and parallel to the operating table. It is common practice to use the fluoroscopy unit as a table by placing the fractured elbow in the center of the wide end of the fluoroscopy machine. The fluoroscopy monitor should be positioned on the opposite side of the patient to allow the surgeon a clear view during operation. The arm is prepped and draped (though a semi-sterile technique without drapes and gowns has also been described [
3]). The reduction is achieved via traction with the arm in mild flexion (20–30 degrees) for approximately 60 s. Coronal angulation is corrected by applying varus or valgus force to the forearm. Next the elbow is flexed, while the surgeon applies pressure to the olecranon using a thumb. Reduction is confirmed with an image intensifier. As the images are taken with the elbow in full flexion, the AP view of the humerus is somewhat obstructed by the forearm. In these cases, it is useful to take oblique AP views by internally and externally rotating the elbow to show lateral and medial humeral columns, respectively. A lateral view is obtained by externally rotating the shoulder 90 degrees. The maneuver can be repeated if the reduction is insufficient. After acceptable alignment had been achieved, the fracture is fixed percutaneously with two or three 1.6 mm k-wires (though smaller or larger wires may be required in particularly small or big patients). If the reduction maneuver is unsuccessful, open reduction of the fracture and pinning are performed.
Our modified technique for sideward displaced pediatric supracondylar fractures is described next. It should be noted that the positioning of the patient is a critical part of successful technique application; thus, it is thoroughly described. The patient is positioned supine with the arm extended on a radiolucent arm board (
Figure 2). It is important to make sure that the elbow is clearly visible on imaging before prepping and draping, and the metal attachment piece that holds the arm board to the operating table is not obstructing the view. With some arm boards and small children, it may be necessary to position the patient with the shoulder and head on the arm board to clear all the metal arm board attachments from fluoroscopic view. Due to the innate instability of this type of fracture, we do not recommend performing it in with a semi-sterile technique; instead, proper skin preparation and draping should be carried out. This facilitates switching to an open reduction procedure in the case that closed reduction fails.
If skin dimpling is present on the ulnar side, milking maneuvers should be performed. Skin dimpling is a sign that the distal end of the humeral shaft (the proximal fracture fragment) has pierced the muscle and soft tissues around the fracture site. The milking maneuver is performed by the surgeon’s hand “milking” the soft tissues around the humerus in a proximal to distal fashion. This may be performed for 1–2 min until the humerus is felt to be free and mobile, thus allowing the surgeon to proceed with the reduction maneuver. As there is minimal, if any, posterior or anterior displacement, the fracture reduction is best achieved via axial traction of an extended elbow. While the assistant applies countertraction to the axilla, the surgeon provides traction in extension with one hand, while with the other hand applies directed pressure medially or laterally on the distal fragment, thereby correcting the sideward translation as well as the varus–valgus malalignment (
Figure 3). AP and lateral fluoroscopic views are achieved by rotating the C-arm around the fracture site, with the patient’s arm stabilized in extension. It is useful to place a rolled towel under the elbow, thus making the lateral imaging easier, providing more room for fracture manipulation, and facilitating fracture fixation in the next step.
Pinning is carried out with the elbow in almost full extension (0–10 degrees of flexion) (
Figure 4). Our preferred configuration is two lateral and one medial 1.6 mm K-wires. We prefer this configuration, as it has been shown to provide the biggest stability and has been recommended for the most unstable and comminuted fractures [
3] (
Figure 5). First, two lateral wires are inserted under fluoroscopy. Finally, the medial wire is placed. Insertion of the medial wire might be challenging due to medial swelling commonly accompanying this type of fracture. Several techniques have been described for medial wire placement, the most common being the mini-open technique (when small incision is made, exposing the medial epicondyle and making sure the ulnar nerve is not injured during wire insertion) [
10]. Though the medial soft tissues are commonly compromised in this fracture subtype, making an open incision increases the insult to the already compromised soft tissues, thus potentially causing further complications. We prefer to insert the wire percutaneously. The elbow is kept in extension, thus keeping the ulnar nerve posterior to the medial epicondyle (the ulnar nerve has been described to occasionally move anterior to the medial epicondyle in flexion [
14]). The wire is inserted percutaneously and gently, initially by hand next to and slightly anterior to the medial epicondyle under fluoroscopic control in two planes (AP and lateral), while the assistant observes for any motion at the fourth and fifth fingers which signaling irritation of the ulnar nerve. If movement of the fingers is observed, the wire is immediately repositioned. After an acceptable position is confirmed with fluoroscopy, the wire is advanced using a drill, keeping an eye on the 4th and 5th fingers. It should be noted that while we have not observed any iatrogenic injuries to the ulnar nerve resulting from our wire insertion technique in our cohort, due to the limited number of patients in the sideward displacement group, we cannot rule out the possibility that it happened only by chance, as ulnar nerve injuries after medial pinning have been described by other authors [
15,
16].
We routinely perform live imaging of the fracture after fixation on lateral view throughout full range of motion (flexion and extension) to assess the stability of the fracture. If mobility in the distal fragment is noted, the wire configuration is examined to look for wire positioning errors.
Postoperatively, the elbow is fixed in a long arm splint, with the forearm in neutral rotation and elbow at 60–80 degrees of flexion. One week postoperatively, X-rays are performed in clinic to evaluate fracture alignment. Three weeks postoperatively the plaster and the wires are removed in the clinic and an X-ray is performed to assess the union.
3. Results
A total of 263 supracondylar humeral fractures were included in the study. Seventeen cases were classified as isolated sideward displacement according to the aforementioned criteria. The mean age of the included patients was 5.7 years, with an almost equal distribution of male to female patients (55% males). The mean age of the children with sideward displaced fractures was 6.8 years, with a practically similar distribution between boys and girls (8:9). The incidence of solely sideward displaced pediatric supracondylar humeral fractures was 6.46%.
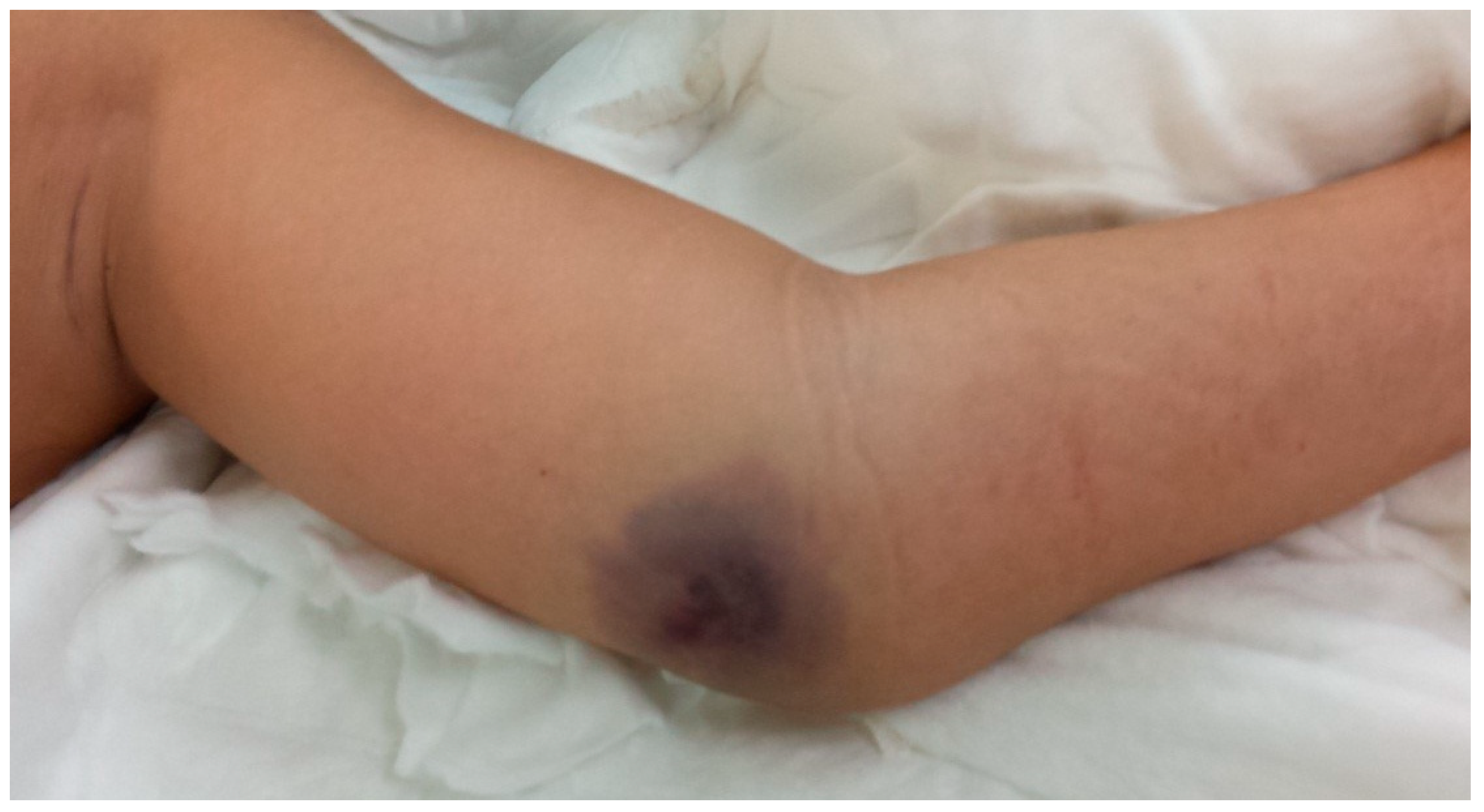
The solely sideward displaced fractures have typical radiological and clinical characteristics. The typical physical findings are medial side subcutaneous hematoma, and often skin dimpling with a palpable bony spike of the proximal fracture fragment on the ulnar side of distal humerus. In addition, gross elbow swelling (signifying the injury’s severity) is commonly observed (
Figure 6).
Subcutaneous hematoma was observed in 76% of sideward displaced fractures and in 19.8% of non-sideward displaced group (
p < 0.00001) (
Table 1). Skin dimpling was recorded in 58.8% of sideward displaced fractures and in 10.6% of overall cases (
p < 0.01). Pulseless pink arm was noted in 5 sideward displaced fractures (29.4%) versus 17 (6.5%) of total cases (15 pulseless pink and 2 pulseless pale)
p < 0.01. We observed a trend of increased incidence of neurological injury in sideward displaced fractures on admission, at 23.5% (3 ulnar nerve and 1 posterior interosseous nerve involvement) compared to only 8% in the overall cohort (12 anterior interosseous nerve, 6 posterior interosseous nerve, and 3 ulnar nerve); however, the difference did not achieve statistical significance (
p = 0.053).
The radiographic features of the fractures include a significant sideward translation in the coronal plane, usually more than 25% of the distal fragment width, with no or minimal posterior displacement in the sagittal plane. Therefore, the anterior humeral line crosses the capitellum at the middle or the anterior third. In our series, all but one distal fragments were displaced to the radial side (
Figure 1).
Intraoperatively, the main feature of the supracondylar humeral fracture with sideward displacement is gross instability, suggesting discontinuity of all cortices as well as a tear of the anterior and posterior periosteum. Elbow flexion during the reduction maneuver fails to control rotation (
Figure 7a) as well as the sideward displacement. Moreover, flexion usually exacerbates the fracture displacement, leading to an anterior translation or flexion of the distal fragment (
Figure 7b).
With the described surgical technique, all sideward displaced fractures were acceptably reduced using closed manipulation, with the anterior humeral line crossing in the middle third of the capitellum without any coronal translation or angulation found upon final radiographs. No open reduction was necessary in any case. The achieved fixation was stable based on real-time live imaging through the full range of motion performed at the end of the operation. No secondary displacement on one week’s and three weeks’ follow-up radiographs was noted. None of the patients needed re-operation. All fractures healed radiologically in three weeks, and pins were removed at this stage. No limitation in range of motion (compared to other side) or neurovascular compromise (all neurologic injuries resolved without intervention) was observed upon final follow-up 6 months after surgery.
4. Discussion
The most common complications of supracondylar fractures are elbow deformities, particularly cubitus varus and cubitus valgus. Their incidence is reported to be up to 50% [
1]. The consensus opinion today is that those deformities are a result of malunion rather than growth imbalance after fracture union. Therefore, due to the high incidence of reported residual deformities, pediatric humeral fractures require accurate and timely management [
1]. The oft-used Gartland classification describes extension-type supracondylar humeral fractures radiologically by the severity of posterior displacement on the sagittal plane. The clinical significance of the different subtypes is ranked by decreasing stability from type I to type III. Leitch et al. added the type IV fracture to the Gartland classification; these are described as type III fractures that exhibit instability both in flexion as well as in extension [
11]. Multidirectional instability could be identified during surgery under fluoroscopy by elbow flexion (the distal fragment moves into flexion) and extension (the distal fragment moves into extension). Due to this instability, the standard techniques for lower type fractures are not suitable, as they involve flexion of the elbow. Different techniques were proposed for type IV fractures, though a substantial proportion of those fractures still require open reduction [
14].
Pediatric supracondylar fractures with sideward displacement do not clearly fit under any currently described Gartland subtype. While they can be considered as a subtype of flexion-type injury [
17], the key feature of flexion-type supracondylar fractures is instability in flexion. In our cohort, the incidence of the sideward displaced fracture was three times higher than the reported incidence of flexion-type fractures. Additionally, while treating those fractures, we noted instability both in flexion and in extension. Although these fractures exhibit multidirectional instability in a manner somewhat similar to type IV fractures, they cannot be clearly considered as such, as there is no posterior displacement on the initial lateral radiograph.
Supracondylar fractures with isolated sideward displacement have distinct radiological and clinical characteristics. The mechanism of injury suggests laterally directed shearing force on an extended elbow. Radiologically, they are characterized by significant sideward displacement in the coronal plane with no or minimal displacement in the sagittal plane. In all but one of our cases, the distal fragment was displaced radially. It was grossly unstable, indicating disruption of all cortices as well as the anterior and posterior periosteum. The distinct radiological characteristics of this fracture provide substantial clues to the treating surgeon that they should expect multidirectional instability. Therefore, the operating room can be properly organized to address this fracture with the described modified technique; this contrasts with type IV fractures that do not have clear signs of multidirectional instability upon initial X-ray.
Litario et al. [
18] in their recent work analyzed predictors for open reduction in the treatment of supracondylar fractures of the humerus in children, concluding that coronal displacement was one of the two most significant preoperative factors for conversion to open reduction. This statement supports our observations regarding complexity of the described fracture pattern.
The suggested operative technique facilitates successful closed reduction and a percutaneous pinning technique. Due to the fracture’s gross rotational instability, positioning the patient supine with the arm on an arm table allows for rotation of the C-arm around the elbow, thus providing better control over fracture reduction and avoiding the need to rotate the arm to achieve a lateral fluoroscopic view. Consequently, rotational deformity can be corrected and reduction maintained throughout the procedure until stable fixation is achieved. The use of a short radiolucent arm board is ideal, though any radiolucent arm board can be used. As most arm boards are fixed to the operating table with metal screws, we recommend taking one fluoroscopic AP image of the elbow before preparation and draping to make sure no metal object is obstructing the view.
While the supine position is most often used for supracondylar humeral fracture reduction, both supine and prone positioning of the patient has been used. A recent systematic review showed comparable results for closed reduction and pinning in both positions [
19]. However, as sideward displaced fractures may require switching to open reduction, we do not recommend using prone positioning for this fracture subtype. The supine position facilitates easy conversion to the open reduction technique, as the recommended open approach is anterior [
14].
The most described reduction maneuver and pinning technique consists of axial traction followed by maximum elbow flexion. Pinning is carried out with the elbow in full flexion [
13,
20]. The goal of the flexion maneuver is to correct posterior displacement in extension-type fractures. In the sideward displaced fracture, due to the minimal, if any, posterior displacement, there is no need for elbow flexion. In our experience, repeated attempts to reduce the fracture by flexing the elbow led to recurrent failed attempts, displacement of the distal fragment into flexion, and exacerbated rotational malalignment, thereby further compromising the fracture’s stability. Reduction of the fracture is better achieved via axial traction of the extended elbow, with medially or laterally directed pressure on the distal fracture fragment thus correcting the coronal translation and varus–valgus malalignment (
Figure 3). The use of a rolled towel under the elbow facilitates control of the reduction in flexion and extension as well as intraoperative lateral imaging.
There is no consensus on the ideal fixation configuration for supracondylar fractures. Though it has been shown that cross pinning (medial pin + lateral pin) provides maximal stability, a three lateral pin configuration has been widely accepted as a viable alternative for unstable fractures (type III and IV). Yet, as lateral configuration cannot provide full stability to the medial humeral column, a cross pin configuration is still used mostly for fractures with medial comminution, very proximal fractures, or obliquely oriented fractures wherein lateral wires cannot provide substantial medial purchase. For stable fractures, notably type II, a two lateral pin configuration is usually acceptable [
1,
3]. As fractures with sideward translation are very unstable and commonly display some degree of comminution, we prefer to fix them with two lateral wires and one medial wire (as a protocol for all fractures of this type). However, if no medial comminution is present, it may be reasonable to use a three lateral pin configuration, thereby reducing the risk of iatrogenic injury to the ulnar nerve.
The timing for fixation of supracondylar fractures is not clearly defined, though it is clearly related to the amount of soft tissue injury. Type II fractures are not urgent, though if treatment is delayed for a week, a callus can already be seen around the fracture, making reduction substantially harder. In our institution, we aim to fix all type II fractures within 48 h. For type III fractures, it has been reported that delays up to 21 h can be safely tolerated [
21]. Yet, most authors recommend fixing these fractures within 12 h, as long as the skin is intact and without tenting, the swelling is mild, and neurovascular examination is normal [
1,
3]. When soft tissue injury is observed, urgent treatment is warranted, especially as soft tissue injury has been linked with further neurovascular compromise and deterioration, even with an initially normal vascular and neurologic exam [
22,
23]. In sideward displaced supracondylar fractures, we also observed substantial soft tissue injury. Medial hematoma and skin tenting were quite common in these patients. Thus, those fractures warrant urgent surgical treatment. Early recognition of this fracture subtype by the treating surgeon allows for the arrangement of the suitable operative room setup, as well as the application of an appropriate reduction and surgical technique. Consequently, the chance of secondary periosteal and soft tissue injury during reduction maneuvers can be reduced, and the need for open reductions can be diminished.
Postoperative care of sideward displaced fractures is similar to standard care for any other supracondylar fracture. After pinning, the arm is fixed with a long arm plaster. Although in many institutions, the common practice uses a circular plaster, we prefer to use a backslab. As the stability to the fracture is provided by the pins, the backslab is used to provide some level of stability to the elbow, without the need for very rigid fixation. As further treatment is performed in an outpatient setting, backslab removal is much easier and quicker than the removal of circumferential plaster, without compromising the quality of treatment. Due to the swelling of the soft tissues around the elbow, we usually fix the elbow in 60–80 degrees of flexion and neutral rotation. The wires are removed 3 weeks postoperatively in clinic. Despite the high fracture instability indicating substantial periosteal stripping, we have not observed any delay in fracture union. After wire removal, the patients are allowed a range of motion as tolerated, though they are instructed to refrain from contact sports and high impact activities for an additional 3 weeks.
There are several limitations to this study. First, this is a retrospective case series study describing our experience with a modified surgical technique. Thus, no comparison with another group was performed. However, due to the high success rate with our closed reduction technique compared to the literature, we did not feel it would be ethical to use previously described techniques. Secondly, the number of patients with sideward displaced fractures was limited, as this is not a common fracture subtype. Further studies collecting appropriate functional scores and long-term radiographic assessments are recommended.