Open Reduction and Internal Fixation of a Volar Displaced Salter–Harris III Mallet Fracture in a Pediatric Patient: A Case Report
Abstract
1. Introduction
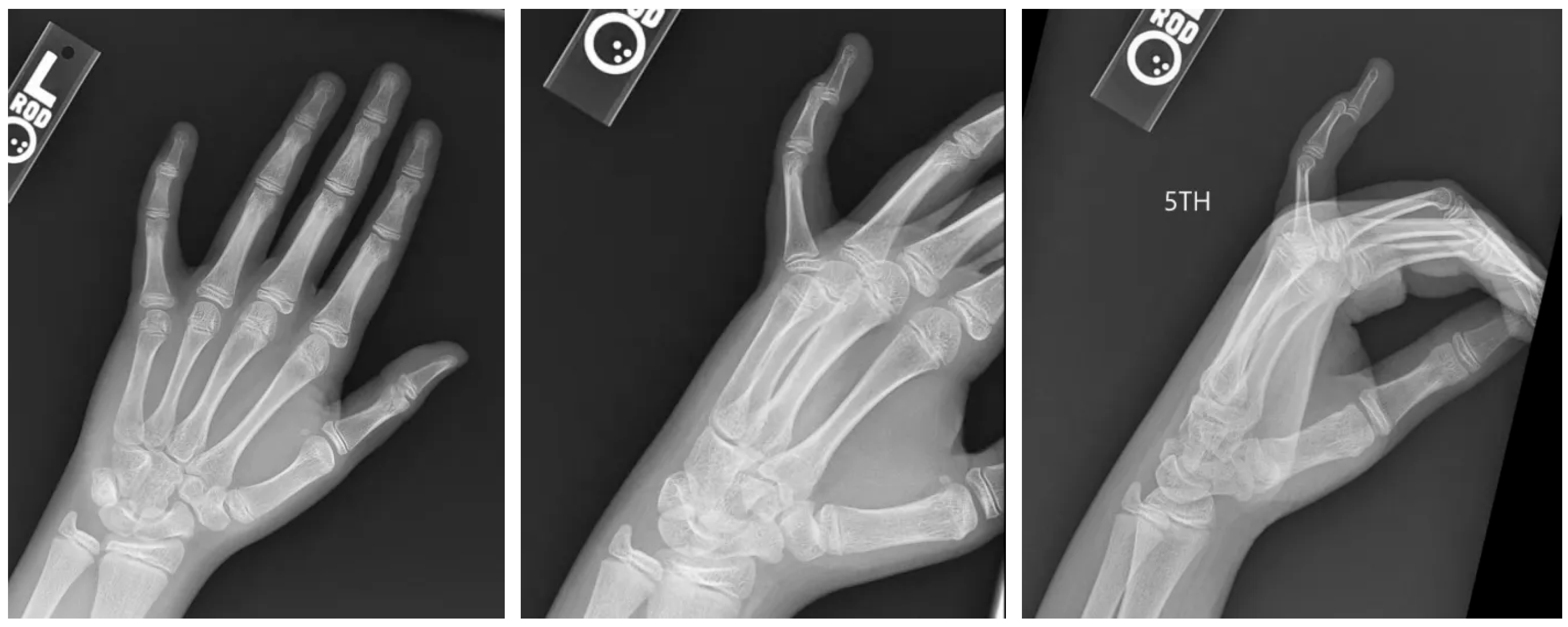
2. Case Presentation
2.1. Surgery
2.2. Follow-Up
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sivakumar, B.S.; Graham, D.J.; Ledgard, J.P.; Lawson, R.D. Acute Mallet Finger Injuries—A Review. J. Hand Surg. 2023, 48, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Wada, T.; Oda, T. Mallet fingers with bone avulsion and DIP joint subluxation. J. Hand Surg. Eur. Vol. 2015, 40, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Annarumma, G.; Spinelli, A.; Massa, B.; Serio, A.; Vecchiato, M.; Demeco, A.; Brugin, E.; Sirico, F.; Giada, F.; et al. Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation. Pediatr. Rep. 2022, 14, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Lamaris, G.A.; Matthew, M.K. The Diagnosis and Management of Mallet Finger Injuries. Hand 2017, 12, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.A.; Friedrich, J.B. Management of Finger Joint Dislocation and Fracture-Dislocations in Athletes. Clin. Sports Med. 2020, 39, 423–442. [Google Scholar] [CrossRef] [PubMed]
- Botero, S.S.; Diaz, J.J.H.; Benaïda, A.; Collon, S.; Facca, S.; Liverneaux, P.A. Review of Acute Traumatic Closed Mallet Finger Injuries in Adults. Arch. Plast. Surg. 2016, 43, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Kreutz-Rodrigues, L.; Gibreel, W.; Moran, S.L.; Carlsen, B.T.; Bakri, K. Frequency, Pattern, and Treatment of Hand Fractures in Children and Adolescents: A 27-Year Review of 4356 Pediatric Hand Fractures. Hand 2022, 17, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Caine, D.; Meyers, R.; Nguyen, J.; Schöffl, V.; Maffulli, N. Primary Periphyseal Stress Injuries in Young Athletes: A Systematic Review. Sports Med. 2022, 52, 741–772. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Naito, K.; Sugiyama, Y.; Obayashi, O.; Kaneko, K. Bony mallet finger without epiphyseal plate injury in childhood. Int. J. Surg. Case Rep. 2015, 14, 172–174. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Salter, R.B.; Harris, W.R. Injuries Involving the Epiphyseal Plate. J. Bone Jt. Surg. 1963, 45, 587–662. Available online: https://journals.lww.com/jbjsjournal/fulltext/1963/45030/injuries_involving_the_epiphyseal_plate.19.aspx (accessed on 15 June 2025). [CrossRef]
- Zlotolow, D.A.; Kozin, S.H. Hand and Wrist Injuries in the Pediatric Athlete. Clin. Sports Med. 2020, 39, 457–479. [Google Scholar] [CrossRef] [PubMed]
- Alla, S.R.; Deal, N.D.; Dempsey, I.J. Current Concepts: Mallet Finger. Hand 2014, 9, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Tisano, B.; Zynda, A.J.; Ellis, H.B.; Wilson, P.L. Epidemiology of Pediatric Gymnastics Injuries Reported in US Emergency Departments: Sex- and Age-Based Injury Patterns. Orthop. J. Sports Med. 2022, 10, 23259671221102478. [Google Scholar] [CrossRef] [PubMed]
- de Boeck, H.; Jaecken, R. Treatment of Chronic Mallet Finger Deformity in Children by Tenodermodesis. J. Pediatr. Orthop. 1992, 12, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.C.Y.; Chong, A.K.S. Pediatric Hand and Wrist Fractures. Clin. Plast. Surg. 2019, 46, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Khera, B.; Chang, C.; Bhat, W. An overview of mallet finger injuries. Acta Biomed. Atenei Parm. 2021, 92, e2021246. [Google Scholar] [CrossRef]
- Prucz, R.B.; Friedrich, J.B. Finger Joint Injuries. Clin. Sports Med. 2015, 34, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, N.; Bosley, J.; Stacy, G.S. Conventional Radiographic Evaluation of Athletic Injuries to the Hand. Radiol. Clin. N. Am. 2013, 51, 239–255. [Google Scholar] [CrossRef] [PubMed]
- Chiang, Y.S.; Hsu, C.E.; Shaw, L.; Chang, C.Y.; Wang, W.C.; Chiu, Y.C. Smile incision and reverse shotgun approach in distal interphalangeal joint arthrodesis. BMC Musculoskelet. Disord. 2024, 25, 895. [Google Scholar] [CrossRef] [PubMed]
- Mahi, G.; Ansong, E.; Gan, E.; Dehbozorgi, S.; Chong, H.H. Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis. Hand 2024. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baur, A.; Anthony, T.; Lustig, K.; Lee, M.L. Open Reduction and Internal Fixation of a Volar Displaced Salter–Harris III Mallet Fracture in a Pediatric Patient: A Case Report. Pediatr. Rep. 2025, 17, 82. https://doi.org/10.3390/pediatric17040082
Baur A, Anthony T, Lustig K, Lee ML. Open Reduction and Internal Fixation of a Volar Displaced Salter–Harris III Mallet Fracture in a Pediatric Patient: A Case Report. Pediatric Reports. 2025; 17(4):82. https://doi.org/10.3390/pediatric17040082
Chicago/Turabian StyleBaur, Alexander, Taylor Anthony, Keith Lustig, and Michael L. Lee. 2025. "Open Reduction and Internal Fixation of a Volar Displaced Salter–Harris III Mallet Fracture in a Pediatric Patient: A Case Report" Pediatric Reports 17, no. 4: 82. https://doi.org/10.3390/pediatric17040082
APA StyleBaur, A., Anthony, T., Lustig, K., & Lee, M. L. (2025). Open Reduction and Internal Fixation of a Volar Displaced Salter–Harris III Mallet Fracture in a Pediatric Patient: A Case Report. Pediatric Reports, 17(4), 82. https://doi.org/10.3390/pediatric17040082





