Abstract
Background/Objectives: Physical activity (PA) during preschool is vital for supporting physiological development, enhancing cognitive abilities and fostering socio-emotional growth. However, consistent disparities in meeting PA guidelines have been observed. This systematic review aims to identify studies that compared preschoolers’ PA, as measured by technological devices, with recommended PA guidelines. Specifically, it examines (i) factors associated with meeting PA guidelines and (ii) the outcomes observed when children meet these guidelines. Methods: The search strategy was designed based on the PICOS framework. Then, a systematic review was conducted using four databases to identify studies that included children from 0 to 6 years old participating in PA sessions recorded through technological devices. PA is compared with guidelines, and correlations were reported. Results: Of the 52 studies reviewed, most found that meeting PA guidelines in preschool-aged children was linked to favourable outcomes across multiple domains. Children who met the guidelines tended to show better motor competence, emotional regulation and cognitive skills, particularly in areas like working memory and social understanding. However, the relationship with body composition and body mass index was inconsistent, suggesting that the benefits of PA in early childhood extend beyond weight-related measures. Conclusions: Meeting PA guidelines in early childhood is strongly associated with cognitive development, emotional regulation, motor skills and social behaviours. However, adherence varies significantly due to a complex mix of individual, familial, socioeconomic and environmental factors.
1. Introduction
Physical activity (PA) is a fundamental component of early childhood development, influencing various physiological, cognitive and socio-emotional dimensions of health []. During the formative years of childhood, habits surrounding PA can lay the foundation for future health behaviours and outcomes. Moreover, PA is of particular interest given the increased prevalence of sedentary lifestyles and related health disorders in children [].
Given the importance of PA, preschool-aged children, typically defined as children between the ages of 3 and 5, represent a critical demographic, as habits ingrained during this period can determine lifelong behaviour patterns []. The concept of the “movement behaviour paradigm” has emerged in recent years. This refers to a holistic framework for understanding how different movement-related behaviours—PA, sedentary behaviour and sleep—interact and collectively influence health and development. This paradigm highlights the importance of taking a holistic approach to fully grasp the collective impact of these behaviours on health and development [,]. While initial studies have examined these relationships in older children and adults, comprehensive investigations focusing specifically on preschool-aged children remain limited [,,].
To understand how much PA preschool-aged children perform, the World Health Organisation (WHO) [] and various national health entities have established guidelines outlining the minimum PA levels recommended for children in this age group. These recommendations have been implemented in countries like the United Kingdom [], the United States [], Australia [], Canada [] and Spain []. Adherence to these guidelines indicates better health outcomes and foundational developmental achievements []. However, while the benefits of PA in older children and adults are extensively studied and well-documented, there is a research gap in the understanding of the holistic impact of meeting these guidelines in preschool-aged children []. This gap is exacerbated by insufficient data on actual activity levels in this demographic and the diverse factors influencing their compliance with these recommended guidelines []. Therefore, it has become crucial to understand the factors affecting adherence to PA guidelines [].
To foster healthy habits among preschoolers, teachers and professionals working with children under five should be aware that the scientific literature has shown that some factors influence children’s adherence to PA guidelines. Among these factors, gender is a critical yet often overlooked factor []. As a social construct, gender intersects with various facets of human behaviour, including health practices []. From toy selection to playgroup participation, boys and girls often experience subtle and explicit nudges towards different pathways, which may influence their activity patterns []. While some studies [,] suggest that boys tend to be more active than girls, engaging in more vigorous or competitive activities, the reasons for these differences and their implications are not fully understood. Are these patterns the result of inherent preferences, societal influences or a combination of both? Furthermore, preschool age is characterised by rapid cognitive development, during which children begin to internalise societal norms and gender roles []. The influence of these internalised beliefs on their PA patterns is exciting.
In addition to gender, parental influence, particularly in education, lifestyle, knowledge and attitudes, significantly shapes preschoolers’ activity levels [,]. According to Chen et al. [], higher parental education often correlates with a higher socioeconomic status, providing more opportunities for preschoolers to participate in organised sports, access play areas and enrol in PA programmes. In this context, Rhodes et al. [] demonstrated that parental attitudes towards PA, influenced by educational experiences, can impact the prioritisation and encouragement of PA among their children. From the preschoolers’ point of view, they often emulate their same-sex parent or the adult in their lives. If the same-sex parent is physically active, the child may be more active []. Therefore, all identified correlations should be analysed through a systematic review to encourage preschoolers to adhere to published guidelines (e.g., WHO, Canadian and Australian guidelines).
Until now, these types of information have been analysed using non-objective tools [,,,,,,]. The scientific literature has established that assessing the amount of PA performed in a valid and reliable way is essential to determine whether or not the daily PA habits align with international guidelines. In this sense, questionnaires have been established as valuable tools [], since they are easy to carry out and can be used to measure the amount of PA performed in different populations []. However, technological devices have introduced the possibility of extracting objective measures, leading to the re-evaluation of traditional assessment methods such as parental reports and observational techniques, which have limitations, such as a lack of precision required for detailed analysis [,].
Specifically, some years ago, the emergence of technologies experienced exponential growth in some scientific fields, where educational settings are not an exception []. Although Global Navigation Satellite Systems (GNSSs) have been used with preschool children [], accelerometers are one of the most widely used technological devices [,,]. Accelerometers are wearable devices that measure the intensity and frequency of movement and offer a promising alternative [] to extract information about PA among preschoolers. Accelerometers provide a more quantifiable and objective perspective, capturing nuances in movement that could be overlooked or misinterpreted in subjective assessments. Their capacity to distinguish between sedentary behaviour, light PA and vigorous PA can provide valuable insights into the quality and quantity of PA in this young age group [,].
In light of these considerations, the need to compare children’s PA levels and PA guideline recommendations and identify those factors that lead children to meet suggestions has become crucial. The rationale is mainly to foster a healthy lifestyle from early childhood, a critical period in a person’s lifespan. In this sense, since objective measures have been introduced, there has been an exponential increase in the number of articles that have analysed the amount of preschoolers’ PA levels through accelerometry [,]. Other authors, instead, have tried to examine associations between accelerometer-derived PA and some outcomes, such as adiposity-related variables in preschool children []. However, regarding guidelines, some authors have been attempting to compare whether children meet a specific PA guideline, such as the WHO, measured through an accelerometer []. However, to the best of the authors’ knowledge, no systematic review has tried to identify related factors when meeting (or not) any PA guideline. For this reason, this systematic review aims to identify studies that compared preschoolers’ PA, as measured by technological devices, with recommended PA guidelines. Specifically, it examines (i) factors associated with meeting PA guidelines and (ii) the outcomes observed when children meet these guidelines. By synthesising existing evidence, the review will address current knowledge gaps and contribute to a more comprehensive understanding of how early adherence to PA guidelines influences developmental trajectories in young children. By exploring the intricacies of accelerometer-derived data, we hope to provide significant evidence that reinforces the importance of early PA, informs public health policies and guides parental and educational practices. The authors of the present systematic review expect it to contribute in two ways. First, the authors expected that this work would contribute to highlighting those correlated factors that science has highlighted, drawing a research path toward what has been performed and what researchers can continue investigating, other factors or whether they influence at the same level in preschoolers with different characteristics. Second, the authors expected to highlight the factors related to education in early childhood that professionals should consider to foster PA from the early years. In addition, these correlated factors could be considered by policymakers to promote preschoolers’ adherence to a healthy lifestyle.
2. Materials and Methods
2.1. Experimental Approach to the Problem
A systematic review was performed using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [] and guidelines for conducting systematic reviews in sports sciences []. The systematic review was registered on PROSPERO (PROSPERO 2025 CRD420251052743).
2.2. Information Sources
A systematic search of four central databases—PubMed, ProQuest, SCOPUS and FECYT (which includes Web of Science, CCC, CIDW, KJD, MEDLINE, RSCI and SCIELO)—was performed to identify studies published before 22 May 2025.
2.3. Search Strategy
The PICO (Patient, Problem or Population–Intervention or Exposure–Comparison, Control or Comparator–Outcome[s]) design was explicitly used to state the question. The search strategy was used in the databases mentioned above. Where possible, the search was limited to scientific studies/journals and language (see exclusion criteria number 6). No lower date limit was applied for publication. The following search terms were used (see Table 1): (preschool OR kindergarten OR “early childhood”) AND (“meet*”) AND (guidelines) AND (“physical activity”) AND (acceleromet* OR pedometer).

Table 1.
Inclusion and exclusion criteria for study selection.
2.4. Selection Process
To identify information from the studies, one author downloaded the information (title, authors, date and database) and transferred it into an Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA), where duplicates were removed. Two authors screened the remaining studies to select those that met all inclusion criteria (Table 1). In the process, a third author should decide if the two authors disagreed on whether an article should be included or excluded.
Moreover, when relevant studies not previously identified were also screened identically and further studies that complied with the inclusion-exclusion criteria were included and labelled as “included from external sources”.
2.5. Data Extraction
The Cochrane Consumers and Communication Review Group’s data extraction template was prepared using an Excel spreadsheet. The spreadsheet assessed inclusion and exclusion requirements for all selected studies. Full-text studies excluded from the analysis were recorded with reasons for exclusion. All records were stored in the spreadsheet. In this process, the authors who decided whether an article should be included or excluded disagreed in two studies. For this reason, the third author agreed that both should be included because they met all the inclusion criteria.
The following information from included articles was extracted: population (e.g., average age, geographic context), PA measured through technological devices, PA duration, technological device’s information, PA guideline used to compare with children’s PA and correlates.
2.6. Quality of Studies
On the one hand, the methodological quality was assessed using the methodological index for non-randomised studies (MINORS) []. The MINORS scale is a list containing eight essential points and is expanded to 12 points when the studies to be treated are comparative. In this case, it was assessed considering nine items (out of 18 points) due to the non-applicability (NA) of three because these items aim to determine studies that include a control group. Each section’s score can be from 0 to 2, depending on the quality obtained for each point. The MINORS checklist asks for the following information (2 = high quality; 1= medium quality; 0 = low quality).
3. Results
3.1. Identification and Selection of Studies
Fifty-two studies met the inclusion criteria (Figure 1). Of these, 37 (71%) were cross-sectional and 15 (29%) longitudinal. Sample sizes varied widely: 18 studies enrolled fewer than 200 participants, 24 included 200–999 and 10 involved more than 1000 children. Most participants were from 3 to 5 years old, although some studies also included infants or 6-year-olds. PA was measured objectively in all studies, with 47 (90%) using accelerometers and the remainder employing pedometers or multi-sensor devices. Most studies (n = 46) benchmarked activity against the WHO 24 h movement guidelines, while others referred to national standards from Canada, Australia or the UK. Although settings ranged across 28 countries, over half of the studies were conducted in high-income contexts. This heterogeneity in methods and populations enabled broad comparison but posed challenges in synthesis.
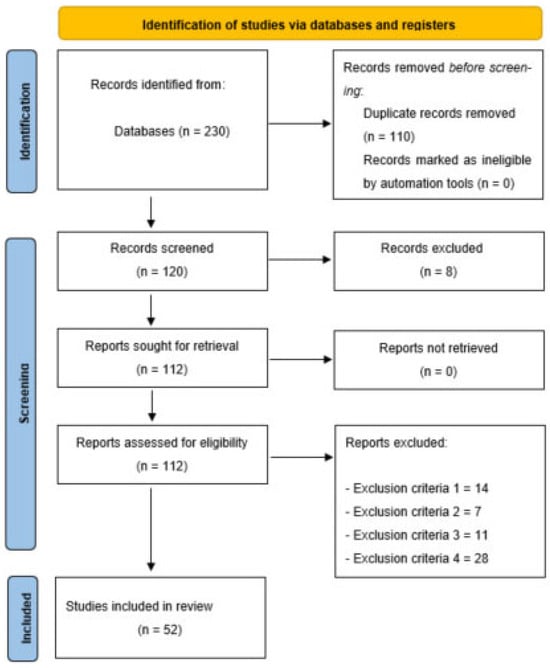
Figure 1.
Flow diagram of this study.
3.2. Quality Assessment
As assessed using the MINORS checklist, study quality was predominantly moderate to high, with total scores ranging from 12 to 18 out of a possible 18. Of the 52 studies, over 80% scored 14 or above, indicating generally sound methodology (see Supplementary Materials, Table S1 [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]). However, consistent weaknesses were observed: more than half of the studies did not report a prospective sample size calculation, and nearly all lacked a control group, limiting causal inference. A few studies also scored lower on follow-up adequacy and dropout reporting. These methodological limitations were not evenly distributed; for example, studies with smaller samples and observational designs tended to have lower quality scores. Notably, no clear pattern emerged linking study quality with reported outcomes. However, studies with higher MINORS scores more consistently reported robust associations between meeting PA guidelines and cognitive or motor development. Item 7 (dropout rate) was marked as ‘N/A’ for cross-sectional studies, as they lack a follow-up phase. For longitudinal studies, dropout rates were assessed, with scores reflecting adherence to the <5% threshold (see Supplementary Materials, Table S1).
3.3. Information on Included Studies
3.3.1. What Influences Children to Meet PA Guidelines?
Several key factors consistently emerged as correlates of preschoolers’ adherence to PA guidelines:
- Gender: Boys were significantly more active than girls in 38 of the 52 studies (73%), especially in moderate-to-vigorous PA (MVPA).
- Age: 21 studies demonstrated that older preschoolers are more likely to adhere to recommendations.
- Parental influence: factors such as maternal PA levels, education and screen-time regulation were significant pred ictors in at least 19 studies, highlighting the household’s role in shaping movement behaviours.
- Environmental factors: Some environmental factors, such as access to outdoor spaces and rural living, were positively linked to PA adherence in 14 studies.
- Race/ethnicity: Other notable influences included race/ethnicity, with minority children in some settings exhibiting higher activity levels than their majority-group peers, though the reasons for this disparity remain underexplored.
- Socioeconomic status (SES) and parental education showed mixed associations. At the same time, higher SES often correlated with more opportunities for structured PA; some studies noted inverse relationships, possibly due to cultural or contextual factors. Time spent outdoors and reduced sedentary behaviour (e.g., limited screen time) were also strongly associated with guideline adherence (see Supplementary Material, Table S2).
3.3.2. What Are the Consequences of Meeting Physical Activity Guidelines?
Meeting PA guidelines was associated with a range of developmental benefits. Enhanced motor skills were reported in 26 studies, particularly in locomotor and ball-control domains, as measured by tools like the Test of Gross Motor Development-2. Cognitive benefits were evident in 11 studies, with stronger executive function—especially working memory and mental flexibility—among children who met guidelines. Emotional and social advantages, such as fewer behavioural problems and increased prosocial behaviour, were identified in 10 studies, with more pronounced effects in boys (see Table S3)
In contrast, the relationship between PA adherence and body composition was inconsistent. Approximately half of the studies assessing BMI or weight status (13 of 26) found no significant association, suggesting that PA’s benefits in early childhood extend beyond weight-related metrics. For example, while motor and cognitive outcomes showed robust links to PA, BMI results varied by subgroup (e.g., a modest association was found only in preschool girls in one study).
Most studies measured activity over at least five consecutive days using accelerometers, allowing detailed tracking of movement intensity. Contextual factors, such as parental reports of play environments, further enriched the findings. Children meeting PA guidelines demonstrated better outcomes across motor, cognitive and emotional domains, though the strength of these associations varied by context and sex (see Supplementary Materials, Table S3).
4. Discussion
This systematic review aims to identify studies that compared preschoolers’ PA, as measured by technological devices, with recommended PA guidelines. Specifically, it examines: (i) factors associated with meeting PA guidelines and (ii) the outcomes observed when children meet these guidelines.
Following this study, the most used PA guidelines are the WHO, Canadian 24 h movement and Australian movement guidelines. A summary of the PA-related recommendations is detailed in Table 2, where similarities can be found, such as at least 30 min of movement in tummy time per day for infants, at least 180 min of PA for toddlers and at least 180 min of PA with one hour of moderate-to-vigorous PA for children older than three years old.

Table 2.
Summary of the most considered PA guidelines.
Following the aim of the systematic review, the included studies have been divided into two groups, which are supposed to be the two main sections in the discussion: (1) what factors influence children to meet PA guidelines and (2) what are the consequences of meeting PA guidelines?
4.1. What Influences Children to Meet PA Guidelines
Efforts to increase PA among children under five must consider various influencing factors, from individual attributes to structural and contextual determinants. Understanding these can help policymakers, educators and caregivers create evidence-based interventions aligned with WHO recommendations.
4.1.1. Gender and Age
As a social construct, gender intersects with various facets of human behaviour, including health practices. From the selection of toys to participation in playgroups, boys and girls are often nudged towards different pathways subtly and explicitly, which may influence their activity patterns []. Numerous studies demonstrated that boys engage in significantly more MVPA than girls [,,,,,,,,,,,,,,,]. The reasons for these differences and their implications are not fully understood. However, some hypotheses could highlight inherent preferences, societal influences, etc. In addition, since this moment in a person’s life is marked by rapid cognitive development, children begin to internalise societal norms and gender roles []. This gender difference is evident across varied cultural contexts, highlighting the persistence of societal and behavioural norms that may favour male participation in active play or structured PA (Leppanen [], Kim [] and Vale []).
Furthermore, children’s age was consistently identified as another significant predictor of PA levels. In this regard, it was found that older preschoolers are more likely to meet PA guidelines than their younger peers, reflecting developmental progressions in motor skill competence and independence [,,,,,]. For these reasons, it is important to involve all children in attractive actives considering that they could be developmentally appropriate and enjoyable [].
4.1.2. Race and Ethnicity
Interestingly, race and ethnic background may influence PA engagement, although the direction of this relationship is context dependent. Minority children in some settings exhibited higher levels of light, moderate and vigorous PA than their majority-group counterparts [,,,]. However, the reasons remain underexplored and may relate to cultural practices, neighbourhood dynamics or targeted interventions.
4.1.3. Parental and Household Influences
SES and household composition further shape children’s PA outcomes. Children from households with low SES, high parity (i.e., later birth order) or single-parent structures tend to have lower PA engagement [,,,].
Regarding the social determinants of health, the child’s caregivers—especially maternal figures—play an essential role in shaping PA behaviours in two ways: maternal PA level and educational level. On the one hand, multiple studies confirm that maternal activity levels and the strength of the social support network surrounding caregivers directly correlate with children’s activity levels [,,,,]. However, when talking about maternal educational level, the findings are not clear. In fact, while in some studies higher maternal education has been associated with increased odds of meeting PA guidelines in some studies [], other research found an inverse relationship, with children of highly educated parents engaging in less activity (Vale []). These contradictory findings point to the complexity of SES as a determinant, with potential moderators such as parental time availability, screen time rules and the value placed on academic vs. physical development.
4.1.4. Environmental and Structural Determinants
Place of residence, including urban vs. rural settings, further modulates PA participation. In South Africa and Tanzania, rural children exhibited higher activity levels than their urban peers, suggesting that access to open play spaces and active transportation may be contributing factors [,]. However, this pattern does not hold uniformly, as research in Mongolia found no urban-rural differences.
Structural factors such as access to safe environments, the presence of community recreation areas and early childhood policies also shape PA engagement. Children in resource-poor preschool environments or underfunded education systems tend to be less physically active [,], underlining the importance of government-level investments and public policy.
4.1.5. Lifestyle Behaviours and Correlates
Additional behavioural factors influence PA adherence. Time spent outdoors is strongly and positively associated with physical activity, and this relationship appears to be mediated by maternal habits and the time children spend watching television [,]. Sedentary behaviour, particularly screen exposure, remains a major barrier to PA participation in preschool-aged children. Conversely, parental life satisfaction or happiness does not show a measurable correlation with children’s PA levels [].
Moreover, the pattern of PA engagement follows a social gradient—children from more advantaged backgrounds are generally more active []. Thus, tackling inequalities in PA requires systemic approaches, such as urban planning to ensure recreational spaces, school policies promoting movement and community-wide initiatives to support families from low-SES backgrounds.
4.1.6. Impact of Sedentary Behaviour on Physical Activity Guideline Adherence
Sedentary time, particularly when structured (e.g., classroom-based activities or screen-based entertainment), may reduce the time available for PA, thus directly affecting adherence to guidelines. In fact, O’Neil et al. [] found that structured preschool environments often prioritise sedentary activities, such as seated learning, which may inadvertently limit opportunities for movement. This suggests that the context in which sedentary behaviour occurs—at home or in educational settings—plays a critical role in shaping PA patterns.
In this way, several studies included in this review highlight sedentary behaviour, particularly excessive screen time, as a significant barrier to meeting PA guidelines [,]. In fact, prolonged screen exposure was consistently associated with reduced MVPA in preschool-aged children, suggesting that sedentary activities may compete with opportunities for active play []. This aligns with findings from De Craemer et al. [], who noted that parental regulation of screen time was a key mediator of PA adherence, with stricter rules linked to higher activity levels.
Moreover, the relationship between sedentary behaviour and PA is not merely a matter of time displacement. Sedentary behaviours may also influence children’s energy levels, motivation or preference for active play. For instance, excessive sedentary time may contribute to reduced physical literacy or motor skill development, critical for sustained PA engagement []. Conversely, interventions that reduce sedentary time, such as incorporating active play zones or movement breaks in preschools, have shown promise in increasing MVPA and overall guideline adherence [].
The limited focus on sedentary behaviour in the reviewed studies highlights a gap in the literature. Hence, future research should prioritise longitudinal designs to clarify whether reducing sedentary time directly enhances PA levels or if other factors, such as parental modelling or environmental access, mediate this relationship. Such insights could inform targeted interventions, such as preschool policies that balance sedentary learning with structured movement opportunities, to optimise adherence to 24 h movement guidelines.
4.2. What Are the Consequences of Meeting Physical Activity Guidelines?
While physical activity is universally recommended for its broad health benefits, its specific impacts on young children remain an area of ongoing research. Findings from the reviewed studies indicate a nuanced picture.
4.2.1. BMI and Physical Health Outcomes
Contrary to common assumptions, the relationship between PA and BMI or weight status in children under five is weak or inconsistent. Most studies found no significant association between PA adherence and body weight or adiposity [,,,,,,,,,,,]. Only one study identified a link between low PA and increased obesity risk in preschool girls []. These findings challenge the notion that early childhood PA alone is sufficient to prevent obesity and suggest that BMI is an inadequate marker of child fitness. For example, Guan [], Lee [] and Kim [] found no statistically significant relationship between PA guideline adherence and BMI z-scores. Chaput [] similarly reported no gender-based adiposity differences despite varying PA levels.
Such discrepancies might be explained by limitations in BMI’s capacity to distinguish fat from lean mass or account for other health dimensions like metabolic fitness. Additionally, dietary patterns, genetic predispositions and environmental exposures (e.g., food insecurity or unsafe play areas) can confound the observed relationships.
4.2.2. Cognitive and Emotional Benefits
More consistent evidence links PA with enhanced emotional and cognitive development in young children. Studies have shown that regular physical activity promotes emotional balance, reduces symptoms of anxiety and depression and supports social-emotional learning [,,]. PA has been positively associated with social cognition, behaviour regulation and general mental well-being in early childhood.
Motor development outcomes—such as motor coordination (MC), locomotor performance and results from assessments like the Test of Gross Motor Development (TGMD-3)—also benefit significantly from higher activity levels [,,,,,]. These findings emphasise that PA is a critical driver of both gross and fine motor skill acquisition, which are foundational for broader developmental competencies.
4.2.3. Language, Learning and Behaviour
Cognitive development in early childhood includes crucial literacy markers like phonological awareness. PA may aid in enhancing phonological working memory and other pre-academic skills []. Children meeting PA recommendations also demonstrated improved working memory and lower incidences of externalising behaviours, such as aggression, disobedience and destructiveness []. These behavioural outcomes suggest that PA contributes to school readiness and emotional regulation.
4.2.4. Environmental Influences on PA Implementation
Despite its benefits, opportunities for PA within institutional settings, such as preschools and classrooms, may be limited. A study by O’Neil et al. [] indicates that structured learning environments and classroom factors may reduce children’s physical activity. Sedentary behaviour promoted by prolonged sitting in early education settings could negate some PA gains, reinforcing the need for health-promoting educational practices [].
In brief, factors such as gender, age, parental influence (maternal PA levels, education and screen-time regulation), environmental factors (access to outdoor spaces and rural living), race/ethnicity and SES could be considered when teachers and professionals working with preschool want to fuel their PA level and subsequently, to achieve cognitive development (e.g., executive function, school readiness), emotional regulation (e.g., emotional well-being), motor skills and social behaviors, which have been correlated when preschool children meet PA guidelines.
However, it is important to note and be critical because all studies differ in the design of their protocols. Among them, studies differ in accelerometer branch (e.g., GT3X+ or ActiGraph GT1M), and since different issues such as sampling frequency [,] or the used algorithm [] can affect it is important to highlight. Another example is the validity and reliability of accelerometers. Even though some of them could be validated [], it is not easy because different circumstances in different measurement settings could influence their validity (the type of measured PA, the place where the device has been placed, the minimum effort duration and the minimum speed for avoiding unrealistic data) []. Another additional difficulty could be the cultural influence on the outcomes of the studies of the different PA guidelines used. These reasons led authors to extend the limitations of the present systematic review.
4.3. Limitations
This review presents important insights into the factors influencing PA and its consequences among preschool-aged children. However, several limitations must be acknowledged:
- Most studies included are cross-sectional, limiting the ability to draw causal inferences. While associations between PA and various outcomes are reported, directionality remains unclear.
- More longitudinal, interventional and randomised controlled trials are required to clarify the direction and strength of relationships between PA and child development outcomes. These should utilise objective measurement tools (e.g., accelerometers) and culturally adapted assessment instruments.
- Substantial heterogeneity exists in how studies define and measure PA and guideline adherence. These discrepancies complicate direct comparisons.
- In this way, the methodology of studies that have used technological devices lacks some relevant information, which could be useful due to its impact on the quality of the results obtained during data collection, processing, analysis and reporting []. In this way, the authors encouraged the use of previously published surveys [] to warrant the inclusion of relevant information when using technological devices.
- Numerous studies suffer from limited sample sizes and lack representativeness, often drawing participants from specific schools, geographic locations or socio-demographic strata. This introduces selection bias and undermines the generalizability of findings.
- Studies included in this review span multiple countries and cultural contexts, yet few control for sociocultural variables. Without such contextualization, there is a risk of masking or exaggerating differences between groups.
- Interpreting parental education or SES effects without considering national education systems or social welfare structures may yield misleading conclusions.
- While BMI is commonly used as an outcome, it fails to capture comprehensive aspects of physical health, such as muscle mass, metabolic fitness or physical literacy. Its frequent use may obscure the full benefits of physical activity.
- The systematic review stated that only original studies written in English or Spanish will be included. Future systematic reviews could include original studies written in another language (or without) language restriction.
- Since this systematic review stated that different studies lack of prospective sample size estimation, this calculation is encouraged for future studies.
5. Conclusions
The main purpose of this paper was to identify studies that contrasted suggested PA guidelines with preschoolers’ PA as assessed by technological devices. It specifically looked at (i) what influences children to meet PA guidelines and (ii) what outcomes are observed when children meet these guidelines. To maintain the consistency, the conclusion section has been organised in two parts, answering the stated objectives:
- What Influences Children to Meet PA Guidelines?
Adherence varies significantly due to a complex mix of individual, familial, socioeconomic and environmental factors. Boys consistently engage in more PA than girls, and rural or outdoor-rich environments promote higher activity levels than urban settings. Parental influence—particularly maternal modelling—and socioeconomic status also play critical roles, although findings related to education and income are sometimes contradictory, reflecting cultural and contextual variability.
- What Are the Consequences of Meeting Physical Activity Guidelines?
This review demonstrates that meeting WHO PA guidelines in early childhood is strongly associated with cognitive development, emotional regulation, motor skills and social behaviours. While PA is widely promoted for its role in managing childhood obesity, this review finds limited evidence linking PA with BMI or weight outcomes in young children. Instead, the most consistent benefits of PA lie in non-physical domains such as executive function, school readiness and emotional well-being. These findings highlight the importance of broadening the focus of early PA promotion beyond weight management.
6. Practical Applications
Guidelines are intended for policy-makers responsible for developing national, sub-regional or municipal plans to increase PA in the population through guidance documents, the education sector, the private sector, research and health care providers.
Key areas for improvement include standardising PA measurement tools, prioritising longitudinal and experimental designs to establish causality and expanding culturally sensitive research in low- and middle-income settings. There is also a need to translate evidence into actionable strategies. Interventions like “Active Play Zones” in early education settings—supported by staff training and daily movement breaks—offer practical, scalable solutions. These designated indoor or outdoor spaces with age-appropriate, low-cost materials (e.g., balls, climbing structures, balance tools) encourage varied movement and social interaction. Combined with staff training and short movement breaks throughout the day, these spaces can significantly increase daily physical activity levels, especially in limited outdoor access.
Policies must also address social inequities by improving access to safe play environments and supporting families from disadvantaged backgrounds.
In sum, ensuring that all preschool children meet PA guidelines is a matter of physical health and a foundation for lifelong learning and development. Future efforts must integrate multisectoral, equity-focused approaches that support active, inclusive environments from the earliest stages of life. In this regard, it is encouraged to be informed about the design approaches, design principles and design recommendations (engaging people of all ages and abilities, selecting play space equipment, accessing play space equipment, grouping play space equipment, incorporating risk and challenge, physical play and sensory play, social play, cognitive/dramatic/imaginative play) for a universal design [].
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pediatric17040079/s1, Table S1: Methodological Quality Assessment of Included Studies Using the MINORS Checklist; Table S2: Factors Influencing Preschool Children’s Adherence to Physical Activity Guidelines; Table S3: The correlations between meeting physical activity guidelines and their effects.
Author Contributions
Conceptualization: M.R.-G.; data curation: M.R.-G.; formal analysis: M.R.-G. and L.P.A.; investigation: M.R.-G. and L.P.A.; methodology: M.R.-G. and L.P.A.; project administration: M.R.-G.; supervision: M.R.-G., U.S.G. and L.P.A.; writing—original draft: U.S.G., R.M.-M. and L.P.A.; writing—review and editing: M.R.-G., U.S.G. and L.P.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chaput, J.-P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO Guidelines on Physical Activity and Sedentary Behaviour for Children and Adolescents Aged 5–17 Years: Summary of the Evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef]
- Rico-González, M.; Holsbrekken, E.; Martín-Moya, R.; Ardigò, L.P. Interventions for Reducing Screen Time of Preschoolers: A Systematic Review of Randomized Controlled Trials. J. Prim. Care Community Health 2025, 16, 21501319241306699. [Google Scholar] [CrossRef]
- Mak, T.C.T.; Chan, D.K.C.; Capio, C.M. Strategies for Teachers to Promote Physical Activity in Early Childhood Education Settings—A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 867. [Google Scholar] [CrossRef]
- Rodrigues, B.; Encantado, J.; Carraca, E.; Martins, J.; Marques, J.; Lopes, L.; Sousa-Sà, E.; Cliff, D.; Mendes, R.; Santos, R. Questionnaires Measuring 24-Hour Movement Behaviors in Childhood and Adolescence: Content Description and Measurement Properties—A Systematic Review. J. Phys. Act. Health 2023, 20, 50–76. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S. Introducing 24-Hour Movement Guidelines for the Early Years: A New Paradigm Gaining Momentum. J. Phys. Act. Health 2020, 17, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Loose, F.; Hudders, L.; Vanwesenbeeck, I.; De Jans, S. Preschoolers and Advertising: A Systematic Literature Review and Future Research Agenda on the Effects of Advertising on Preschool Children. J. Advert. 2023, 52, 439–455. [Google Scholar] [CrossRef]
- Kuhn, M.; Boise, C.; Marvin, C.A.; Knoche, L.L. Challenging Behaviors and Executive Function in Preschool-Aged Children: Relationships and Implications for Practice. Infants Young Child. 2021, 34, 46–65. [Google Scholar] [CrossRef]
- Scarborough, P.; Bhatnagar, P.; Wickramasinghe, K.K.; Allender, S.; Foster, C.; Rayner, M. The Economic Burden of Ill Health Due to Diet, Physical Inactivity, Smoking, Alcohol and Obesity in the UK: An Update to 2006-07 NHS Costs. J. Public Health 2011, 33, 527–535. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P. Physical Activity Guidelines for Americans from the US Department of Health and Human Services. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e005263. [Google Scholar] [CrossRef]
- Eckermann, S.; Willan, A.R. Active Lives South Australia Health Economic Analysis: An Evidence Base for the Potential of Health Promotion Strategies Supporting Physical Activity Guidelines to Reduce Public Health Costs While Improving Wellbeing. Z. Gesundh. Wiss. 2022, 30, 1791–1807. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Leblanc, A.G.; Carson, V.; Choquette, L.; Connor Gorber, S.; Dillman, C.; Duggan, M.; Gordon, M.J.; Hicks, A.; Janssen, I.; et al. Canadian Physical Activity Guidelines for the Early Years (Aged 0–4 Years). Appl. Physiol. Nutr. Metab. 2012, 37, 345–369. [Google Scholar] [CrossRef] [PubMed]
- Arufe-Giráldez, V.; Sanmiguel-Rodríguez, A.; Zagalaz-Sánchez, M.L.; Cachón-Zagalaz, J.; González-Valero, G. Sleep, Physical Activity and Screens in 0–4 Years Spanish Children during the COVID-19 Pandemic: Were the WHO Recommendations Met? J. Hum. Sport. Exerc. 2022, 17, 484–503. [Google Scholar] [CrossRef]
- Aadland, E.; Tjomsland, H.E.; Johannessen, K.; Nilsen, A.K.O.; Resaland, G.K.; Glosvik, Ø.; Lykkebø, O.; Stokke, R.; Andersen, L.B.; Anderssen, S.A.; et al. Active Learning Norwegian Preschool(Er)s (ACTNOW)—Design of a Cluster Randomized Controlled Trial of Staff Professional Development to Promote Physical Activity, Motor Skills, and Cognition in Preschoolers. Front. Psychol. 2020, 11, 1382. [Google Scholar] [CrossRef] [PubMed]
- Kracht, C.L.; Webster, E.K.; Staiano, A.E. A Natural Experiment of State-Level Physical Activity and Screen-Time Policy Changes Early Childhood Education (ECE) Centers and Child Physical Activity. BMC Public Health 2020, 20, 387. [Google Scholar] [CrossRef]
- Martin, N.J. Parent–Teacher Collaboration Is Needed to Enhance Preschoolers’ Physical Activity: What Do We Do Now? Early Child. Educ. J. 2023, 53, 151–159. [Google Scholar] [CrossRef]
- Hu, D.; Zhou, S.; Crowley-McHattan, Z.J.; Liu, Z. Factors That Influence Participation in Physical Activity in School-Aged Children and Adolescents: A Systematic Review from the Social Ecological Model Perspective. Int. J. Environ. Res. Public Health 2021, 18, 3147. [Google Scholar] [CrossRef]
- Tcymbal, A.; Demetriou, Y.; Kelso, A.; Wolbring, L.; Wunsch, K.; Wäsche, H.; Woll, A.; Reimers, A.K. Effects of the Built Environment on Physical Activity: A Systematic Review of Longitudinal Studies Taking Sex/Gender into Account. Environ. Health Prev. Med. 2020, 25, 75. [Google Scholar] [CrossRef]
- Rico-González, M.; Martín-Moya, R.; Mendoza-Muñoz, M.; Carlos-Vivas, J. Preschool Children’s Adherence to the 24-Hour Physical Activity Guidelines: A Systematic Review Comparing Sexes. Health Educ. J. 2024, 83, 695–704. [Google Scholar] [CrossRef]
- Gao, W.; Zhang, Y.; Wu, D.; Dong, Y.; Liu, N.; Wang, H. Compliance with Health-Related Behaviors Guidelines and Its Relationship with Multiple Factors in Preschool Children Aged 3–6 Years: A National Cross-Sectional Survey in China. Int. J. Environ. Res. Public Health 2022, 19, 1262. [Google Scholar] [CrossRef]
- Peral-Suárez, Á.; Cuadrado-Soto, E.; Perea, J.M.; Navia, B.; López-Sobaler, A.M.; Ortega, R.M. Physical Activity Practice and Sports Preferences in a Group of Spanish Schoolchildren Depending on Sex and Parental Care: A Gender Perspective. BMC Pediatr. 2020, 20, 337. [Google Scholar] [CrossRef]
- Zhang, Z.H.; Li, H.J.; Slapsinskaite, A.; Zhang, T.; Zhang, L.; Gui, C.Y. Accelerometer-Measured Physical Activity and Sedentary Behavior in Chinese Children and Adolescents: A Systematic Review and Meta-Analysis. Public Health 2020, 186, 71–77. [Google Scholar] [CrossRef] [PubMed]
- McCabe, P.C. Early Childhood Educators’ Beliefs about Child Behavior and Adult Outcomes Related to Gender and Play. Psychol. Sch. 2022, 59, 51–75. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Guerrero, M.D.; Vanderloo, L.M.; Barbeau, K.; Birken, C.S.; Chaput, J.-P.; Faulkner, G.; Janssen, I.; Madigan, S.; Mâsse, L.C.; et al. Development of a Consensus Statement on the Role of the Family in the Physical Activity, Sedentary, and Sleep Behaviours of Children and Youth. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 74. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, N.; Harris, N.; Downes, M. Preschool Children’s Preferences for Sedentary Activity Relates to Parent’s Restrictive Rules around Active Outdoor Play. BMC Public Health 2019, 19, 946. [Google Scholar] [CrossRef]
- Chen, C.; Sellberg, F.; Ahlqvist, V.H.; Neovius, M.; Christiansen, F.; Berglind, D. Associations of Participation in Organized Sports and Physical Activity in Preschool Children: A Cross-Sectional Study. BMC Pediatr. 2020, 20, 328. [Google Scholar] [CrossRef]
- Reimers, A.K.; Schmidt, S.C.E.; Demetriou, Y.; Marzi, I.; Woll, A. Parental and Peer Support and Modelling in Relation to Domain-Specific Physical Activity Participation in Boys and Girls from Germany. PLoS ONE 2019, 14, e0223928. [Google Scholar] [CrossRef]
- Vanderloo, L.M.; Maguire, J.L.; Keown-Stoneman, C.D.G.; Parkin, P.C.; Borkhoff, C.M.; Tremblay, M.S.; Anderson, L.N.; Birken, C.S.; TARGet Kids! Collaboration. Associations Between Meeting the 24-Hour Movement Guidelines and Cardiometabolic Risk in Young Children. Pediatr. Exerc. Sci. 2021, 33, 112–119. [Google Scholar] [CrossRef]
- Chia, M.Y.H.; Tay, L.Y.; Chua, T.B.K. Quality of Life and Meeting 24-h WHO Guidelines Among Preschool Children in Singapore. Early Child. Educ. J. 2020, 48, 313–323. [Google Scholar] [CrossRef]
- Pyper, E.; Harrington, D.; Manson, H. The Impact of Different Types of Parental Support Behaviours on Child Physical Activity, Healthy Eating, and Screen Time: A Cross-Sectional Study. BMC Public Health 2016, 16, 568. [Google Scholar] [CrossRef]
- Prioreschi, A.; Micklesfield, L.K. Compliance with Physical Activity and Sedentary Behavior Guidelines and Associations with Abdominal Adiposity in a Sample of Infants and Toddlers From Soweto, South Africa. J. Phys. Act. Health 2019, 16, 872–879. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Schary, D.P.; Cardinal, B.J. Adherence to Active Play and Electronic Media Guidelines in Preschool Children: Gender and Parental Education Considerations. Matern. Child. Health J. 2013, 17, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Huang, W.Y.; Lau, P.W.C.; Wong, S.H.-S.; Sit, C.H.-P. Movement Behaviors and Mental Health of Caregivers of Preschoolers in China during the COVID-19 Pandemic. Prev. Med. 2022, 155, 106913. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, J.; Arundell, L.; Hnatiuk, J.A. Associations between the Neighbourhood Social Environment and Preschool Children’s Physical Activity and Screen Time. BMC Public Health 2022, 22, 1065. [Google Scholar] [CrossRef] [PubMed]
- Fjørtoft, I.; Pedersen, A.V.; Sigmundsson, H.; Vereijken, B. Measuring Physical Fitness in Children Who Are 5 to 12 Years Old with a Test Battery That Is Functional and Easy to Administer. Phys. Ther. 2011, 91, 1087–1095. [Google Scholar] [CrossRef]
- Wendel-Vos, G.C.W.; Schuit, A.J.; Saris, W.H.M.; Kromhout, D. Reproducibility and Relative Validity of the Short Questionnaire to Assess Health-Enhancing Physical Activity. J. Clin. Epidemiol. 2003, 56, 1163–1169. [Google Scholar] [CrossRef]
- Janssen, X.; Martin, A.; Hughes, A.R.; Hill, C.M.; Kotronoulas, G.; Hesketh, K.R. Associations of Screen Time, Sedentary Time and Physical Activity with Sleep in under 5s: A Systematic Review and Meta-Analysis. Sleep. Med. Rev. 2020, 49, 101226. [Google Scholar] [CrossRef]
- Petersen, T.L.; Møller, L.B.; Brønd, J.C.; Jepsen, R.; Grøntved, A. Association between Parent and Child Physical Activity: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 67. [Google Scholar] [CrossRef]
- Lettink, A.; Altenburg, T.M.; Arts, J.; Van Hees, V.T.; Chinapaw, M.J.M. Systematic Review of Accelerometer-Based Methods for 24-h Physical Behavior Assessment in Young Children (0–5 Years Old). Int. J. Behav. Nutr. Phys. Act. 2022, 19, 116. [Google Scholar] [CrossRef]
- Rico-González, M.; Pino-Ortega, J.; Martínez-Bello, V. Creating a Mark of Reference About the Use of Positioning Technology in Preschool-Aged Children Based on a Systematic Review. J. Res. Child. Educ. 2024, 38, 616–631. [Google Scholar] [CrossRef]
- Dobell, A.; Pringle, A.; Faghy, M.A.; Roscoe, C.M.P. Fundamental Movement Skills and Accelerometer-Measured Physical Activity Levels during Early Childhood: A Systematic Review. Children 2020, 7, 224. [Google Scholar] [CrossRef]
- Herbert, J.; Matłosz, P.; Lenik, J.; Szybisty, A.; Baran, J.; Przednowek, K.; Wyszyńska, J. Objectively Assessed Physical Activity of Preschool-Aged Children from Urban Areas. Int. J. Environ. Res. Public Health 2020, 17, 1375. [Google Scholar] [CrossRef]
- Wiersma, R.; Haverkamp, B.F.; Van Beek, J.H.; Riemersma, A.M.J.; Boezen, H.M.; Smidt, N.; Corpeleijn, E.; Hartman, E. Unravelling the Association between Accelerometer-derived Physical Activity and Adiposity among Preschool Children: A Systematic Review and Meta-analyses. Obes. Rev. 2020, 21, e12936. [Google Scholar] [CrossRef] [PubMed]
- Bourke, M.; Haddara, A.; Loh, A.; Carson, V.; Breau, B.; Tucker, P. Adherence to the World Health Organization’s Physical Activity Recommendation in Preschool-Aged Children: A Systematic Review and Meta-Analysis of Accelerometer Studies. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 52. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Rico-González, M.; Pino-Ortega, J.; Clemente, F.M.; Los Arcos, A. Guidelines for Performing Systematic Reviews in Sports Science. Biol. Sport. 2022, 39, 463–471. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Original Article Methodological Index for Non-Randomized Studies (Minors). ANZ J. Surg. 2003, 73, 712–716. [Google Scholar]
- Christian, H.; Murray, K.; Trost, S.G.; Schipperijn, J.; Trapp, G.; Maitland, C.; Divitini, M. Meeting the Australian 24-Hour Movement Guidelines for the Early Years Is Associated with Better Social-Emotional Development in Preschool Boys. Prev. Med. Rep. 2022, 27, 101770. [Google Scholar] [CrossRef]
- De Lucena Martins, C.M.; Lemos, L.F.G.B.P.; De Souza Filho, A.N.; Bezerra, T.A.; Soares, I.A.A.; Mota, J.G.; Bandeira, P.F.R.; Mota, J.A.P.S.; Tassitano, R.M.; Duncan, M.J. Adherence to 24-hour Movement Guidelines in low-income Brazilian Preschoolers and Associations with Demographic Correlates. Am. J. Hum. Biol. 2021, 33, e23519. [Google Scholar] [CrossRef]
- Nicolai Ré, A.H.; Okely, A.D.; Logan, S.W.; da Silva, M.M.L.M.; Cattuzzo, M.T.; Stodden, D.F. Relationship between Meeting Physical Activity Guidelines and Motor Competence among Low-Income School Youth. J. Sci. Med. Sport. 2020, 23, 591–595. [Google Scholar] [CrossRef]
- McNeill, J.; Howard, S.J.; Vella, S.A.; Cliff, D.P. Compliance with the 24-Hour Movement Guidelines for the Early Years: Cross-Sectional and Longitudinal Associations with Executive Function and Psychosocial Health in Preschool Children. J. Sci. Med. Sport. 2020, 23, 846–853. [Google Scholar] [CrossRef]
- Kracht, C.L.; Webster, E.K.; Staiano, A.E. Relationship between the 24-Hour Movement Guidelines and Fundamental Motor Skills in Preschoolers. J. Sci. Med. Sport. 2020, 23, 1185–1190. [Google Scholar] [CrossRef]
- Meredith-Jones, K.; Galland, B.; Haszard, J.; Gray, A.; Sayers, R.; Hanna, M.; Taylor, B.; Taylor, R. Do Young Children Consistently Meet 24-h Sleep and Activity Guidelines? A Longitudinal Analysis Using Actigraphy. Int. J. Obes. 2019, 43, 2555–2564. [Google Scholar] [CrossRef]
- O’Neill, J.R.; Pfeiffer, K.A.; Dowda, M.; Pate, R.R. In-School and Out-of-School Physical Activity in Preschool Children. J. Phys. Act. Health 2016, 13, 606–610. [Google Scholar] [CrossRef] [PubMed]
- Guan, H.; Zhang, Z.; Wang, B.; Okely, A.D.; Tong, M.; Wu, J.; Zhang, T. Proportion of Kindergarten Children Meeting the WHO Guidelines on Physical Activity, Sedentary Behaviour and Sleep and Associations with Adiposity in Urban Beijing. BMC Pediatr. 2020, 20, 70. [Google Scholar] [CrossRef] [PubMed]
- Leppänen, M.H.; Ray, C.; Wennman, H.; Alexandrou, C.; Sääksjärvi, K.; Koivusilta, L.; Erkkola, M.; Roos, E. Compliance with the 24-h Movement Guidelines and the Relationship with Anthropometry in Finnish Preschoolers: The DAGIS Study. BMC Public Health 2019, 19, 1618. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Bernard, J.Y.; Padmapriya, N.; Yao, J.; Goh, C.; Tan, K.H.; Yap, F.; Chong, Y.-S.; Shek, L.; Godfrey, K.M.; et al. Socio-Demographic and Maternal Predictors of Adherence to 24-Hour Movement Guidelines in Singaporean Children. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 70. [Google Scholar] [CrossRef]
- Santos, R.; Zhang, Z.; Pereira, J.R.; Sousa-Sá, E.; Cliff, D.P.; Okely, A.D. Compliance with the Australian 24-Hour Movement Guidelines for the Early Years: Associations with Weight Status. BMC Public Health 2017, 17, 867. [Google Scholar] [CrossRef]
- Cliff, D.P.; McNeill, J.; Vella, S.A.; Howard, S.J.; Santos, R.; Batterham, M.; Melhuish, E.; Okely, A.D.; De Rosnay, M. Adherence to 24-Hour Movement Guidelines for the Early Years and Associations with Social-Cognitive Development among Australian Preschool Children. BMC Public Health 2017, 17, 857. [Google Scholar] [CrossRef]
- Draper, C.; Tomaz, S.A.; Cook, C.J.; Jugdav, S.S.; Ramsammy, C.; Besharati, S.; Van Heerden, A.; Vilakazi, K.; Cockcroft, K.; Howard, S.J.; et al. Understanding the Influence of 24-Hour Movement Behaviours on the Health and Development of Preschool Children from Low-Income South African Settings: The SUNRISE Pilot Study. S. Afr. J. Sports Med. 2020, 32, 1–7. [Google Scholar] [CrossRef]
- Khalsa, A.S.; Kharofa, R.; Ollberding, N.J.; Bishop, L.; Copeland, K.A. Attainment of ‘5-2-1-0’ Obesity Recommendations in Preschool-Aged Children. Prev. Med. Rep. 2017, 8, 79–87. [Google Scholar] [CrossRef]
- Hall, C.J.S.; Eyre, E.L.J.; Oxford, S.W.; Duncan, M.J. Relationships between Motor Competence, Physical Activity, and Obesity in British Preschool Aged Children. J. Funct. Morphol. Kinesiol. 2018, 3, 57. [Google Scholar] [CrossRef]
- Breau, B.; Brandes, B.; Wright, M.N.; Buck, C.; Vallis, L.A.; Brandes, M. Association of Individual Motor Abilities and Accelerometer-Derived Physical Activity Measures in Preschool-Aged Children. J. Meas. Phys. Behav. 2021, 4, 227–235. [Google Scholar] [CrossRef]
- Feng, J.; Huang, W.Y.; Reilly, J.J.; Wong, S.H.-S. Compliance with the WHO 24-h Movement Guidelines and Associations with Body Weight Status among Preschool Children in Hong Kong. Appl. Physiol. Nutr. Metab. 2021, 46, 1273–1278. [Google Scholar] [CrossRef]
- Kambas, A.; Venetsanou, F.; Avloniti, A.; Giannakidou, D.M.; Gourgoulis, V.; Draganidis, D.; Chatzinikolaou, A.; Fatouros, I.; Michalopoulou, M. Pedometer Determined Physical Activity and Obesity Prevalence of Greek Children Aged 4–6 Years. Ann. Hum. Biol. 2015, 42, 233–238. [Google Scholar] [CrossRef]
- Armstrong, B.; Covington, L.B.; Hager, E.R.; Black, M.M. Objective Sleep and Physical Activity Using 24-Hour Ankle-Worn Accelerometry among Toddlers from Low-Income Families. Sleep Health 2019, 5, 459–465. [Google Scholar] [CrossRef]
- Berglind, D.; Ljung, R.; Tynelius, P.; Brooke, H.L. Cross-sectional and Prospective Associations of Meeting 24-h Movement Guidelines with Overweight and Obesity in Preschool Children. Pediatr. Obes. 2018, 13, 442–449. [Google Scholar] [CrossRef]
- Carson, V.; Ezeugwu, V.E.; Tamana, S.K.; Chikuma, J.; Lefebvre, D.L.; Azad, M.B.; Moraes, T.J.; Subbarao, P.; Becker, A.B.; Turvey, S.E.; et al. Associations between Meeting the Canadian 24-Hour Movement Guidelines for the Early Years and Behavioral and Emotional Problems among 3-Year-Olds. J. Sci. Med. Sport. 2019, 22, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Colley, R.C.; Aubert, S.; Carson, V.; Janssen, I.; Roberts, K.C.; Tremblay, M.S. Proportion of Preschool-Aged Children Meeting the Canadian 24-Hour Movement Guidelines and Associations with Adiposity: Results from the Canadian Health Measures Survey. BMC Public Health 2017, 17, 829. [Google Scholar] [CrossRef] [PubMed]
- De Craemer, M.; Verbestel, V.; Cardon, G.; Androutsos, O.; Manios, Y.; Chastin, S. Correlates of Meeting the Physical Activity, Sedentary Behavior, and Sleep Guidelines for the Early Years among Belgian Preschool Children: The ToyBox-Study. Int. J. Environ. Res. Public Health 2020, 17, 7006. [Google Scholar] [CrossRef] [PubMed]
- Slaton, A.; Kowalski, A.J.; Zemanick, A.; Pulling Kuhn, A.; Hager, E.R.; Black, M.M. Motor Competence and Attainment of Global Physical Activity Guidelines among a Statewide Sample of Preschoolers. Int. J. Environ. Res. Public Health 2020, 17, 8546. [Google Scholar] [CrossRef]
- Lee, S.T.; Wong, J.E.; Chan, G.K.L.; Poh, B.K. Association between Compliance with Movement Behavior Guidelines and Obesity among Malaysian Preschoolers. Int. J. Environ. Res. Public Health 2021, 18, 4611. [Google Scholar] [CrossRef]
- Jago, R.; Sebire, S.J.; Wood, L.; Pool, L.; Zahra, J.; Thompson, J.L.; Lawlor, D.A. Associations between Objectively Assessed Child and Parental Physical Activity: A Cross-Sectional Study of Families with 5–6 Year Old Children. BMC Public Health 2014, 14, 655. [Google Scholar] [CrossRef]
- Li, F.; Yin, L.; Sun, M.; Gao, Z. Examining Relationships among Chinese Preschool Children’s Meeting 24-Hour Movement Guidelines and Fundamental Movement Skills. J. Clin. Med. 2022, 11, 5623. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Ma, J.; Harada, K.; Lee, S.; Gu, Y. Associations between Adherence to Combinations of 24-h Movement Guidelines and Overweight and Obesity in Japanese Preschool Children. Int. J. Environ. Res. Public Health 2020, 17, 9320. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.V.; Pham, T.N.D.; Nguyen, C.L.D.; Nguyen, T.T.D.; Okely, A.D.; Tang, H.K. Prevalence of Physical Activity, Screen Time, and Sleep, and Associations with Adiposity and Motor Development among Preschool-Age Children in Vietnam: The SUNRISE Vietnam Pilot Study. Indian. J. Pediatr. 2022, 89, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Larouche, R.; Garriguet, D.; Tremblay, M.S. Outdoor Time, Physical Activity and Sedentary Time among Young Children: The 2012–2013 Canadian Health Measures Survey. Can. J. Public. Health 2016, 107, e500–e506. [Google Scholar] [CrossRef]
- Lee, E.-Y.; Hesketh, K.D.; Hunter, S.; Kuzik, N.; Rhodes, R.E.; Rinaldi, C.M.; Spence, J.C.; Carson, V. Meeting New Canadian 24-Hour Movement Guidelines for the Early Years and Associations with Adiposity among Toddlers Living in Edmonton, Canada. BMC Public Health 2017, 17, 840. [Google Scholar] [CrossRef]
- Kracht, C.L.; Webster, E.K.; Staiano, A.E. Sociodemographic Differences in Young Children Meeting 24-Hour Movement Guidelines. J. Phys. Act. Health 2019, 16, 908–915. [Google Scholar] [CrossRef]
- Engberg, E.; Ray, C.; Määttä, S.; Figueiredo, R.A.O.; Leppänen, M.H.; Pajulahti, R.; Koivusilta, L.; Korkalo, L.; Nissinen, K.; Vepsäläinen, H.; et al. Parental Happiness Associates with the Co-Occurrence of Preschool-Aged Children’s Healthy Energy Balance-Related Behaviors. J. Happiness Stud. 2022, 23, 1493–1507. [Google Scholar] [CrossRef]
- Vale, S.; Ricardo, N.; Soares-Miranda, L.; Santos, R.; Moreira, C.; Mota, J. Parental Education and Physical Activity in Pre-school Children. Child 2014, 40, 446–452. [Google Scholar] [CrossRef]
- Vale, S.; Trost, S.; Ruiz, J.J.; Rêgo, C.; Moreira, P.; Mota, J. Physical Activity Guidelines and Preschooler’s Obesity Status. Int. J. Obes. 2013, 37, 1352–1355. [Google Scholar] [CrossRef]
- Vale, S.; Trost, S.G.; Duncan, M.J.; Mota, J. Step Based Physical Activity Guidelines for Preschool-Aged Children. Prev. Med. 2015, 70, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Abdeta, C.; Cliff, D.; Kariippanon, K.; Deksisa, A.; Garoma, S.; Tesfaye, D.; Chong, K.H.; Antczak, D.; Okely, A.D. Adherence to the WHO Physical Activity, Screen Time and Sleep Guidelines and Associations with Socio-Demographic Factors among Ethiopian Preschool Children: The SUNRISE Study. J. Act. Sedentary Sleep Behav. 2024, 3, 22. [Google Scholar] [CrossRef]
- Christian, H.E.; Adams, E.K.; Moore, H.L.; Nathan, A.; Murray, K.; Schipperijn, J.; Trost, S.G. Developmental Trends in Young Children’s Device-Measured Physical Activity and Sedentary Behaviour. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 97. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Li, F.; Liu, P.; Yin, Z.; Yang, Z.; Pi, L.; Gao, Z. Examining the Relationship between Meeting 24-Hour Movement Behaviour Guidelines and Mental Health in Chinese Preschool Children. Front. Pediatr. 2024, 12, 1337158. [Google Scholar] [CrossRef]
- Palmer, S.A.; Stevens, Z.; Palmer, K.K.; Chinn, K.M.; Farquhar, J.M.; Robinson, L.E. Exploring If Playground Quality Predicts Head Start Preschoolers’ School Day Physical Activity. Int. J. Early Child. 2025, 57, 51–70. [Google Scholar] [CrossRef]
- Kolehmainen, N.; Thornton, C.; Craw, O.; Pearce, M.S.; Kudlek, L.; Nazarpour, K.; Cutler, L.; Van Sluijs, E.; Rapley, T. Physical Activity in Young Children across Developmental and Health States: The ActiveCHILD Study. eClinicalMedicine 2023, 60, 102008. [Google Scholar] [CrossRef]
- Yu, C.C.W.; Zhang, B.; Lo, S.; Sun, F. Physical Activity, Sedentary Behaviour, and Sleep Habits in Kindergarten Children in Hong Kong. HK J. Paediatr. 2023, 28, 219–227. [Google Scholar]
- Ré, A.H.N.; Cattuzzo, M.T.; Stodden, D.; Santos, G.D.; Tertuliano, A.L.O.; Monteiro, C.B.D.M.; Coledam, D.H.C.; Okely, A.D. Physical Development and Sociocultural Context Influences on Children’s Physical Activity. Rev. Paul. Pediatr. 2025, 43, e2024113. [Google Scholar] [CrossRef]
- Mwase-Vuma, T.W.; Janssen, X.; Chong, K.H.; Okely, A.D.; Tremblay, M.S.; Draper, C.E.; Webster, E.K.; Florindo, A.A.; Staiano, A.E.; Nguyen, B.; et al. Prevalence and Correlates of Adherence to the Global Total Physical Activity Guideline Based on Step Counting Among 3- to 4-Year-Olds: Evidence from SUNRISE Pilot Studies From 17 Countries. J. Phys. Act. Health 2024, 21, 1–8. [Google Scholar] [CrossRef]
- Byambaa, A.; Dechinjamts, O.; Jambaldorj, B.; Jones, R.A.; Chong, K.H.; Okely, A.D. Prevalence and Health Associations of Meeting the World Health Organization Guidelines for Physical Activity, Sedentary Behavior, and Sleep in Preschool-Aged Children: The SUNRISE Mongolia Pilot and Feasibility Study. J. Phys. Act. Health 2024, 21, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Christian, H.; Nathan, A.; Trost, S.G.; Schipperijn, J.; Boruff, B.; Adams, E.K.; George, P.; Moore, H.L.; Henry, A. Profile of the PLAY Spaces & Environments for Children’s Physical Activity, Sedentary Behaviour and Sleep (PLAYCE) Cohort Study, Western Australia. J. Act. Sedentary Sleep Behav. 2025, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Zhang, L.; Hu, T.; Ma, J.; Li, X.; Zhang, X.; Kim, H. The Cross-Sectional and Longitudinal Associations Between Adherence to 24-Hour Movement Behavior Guidelines and Bone Health in Young Children. Healthcare 2024, 12, 2173. [Google Scholar] [CrossRef] [PubMed]
- Nusurupia, J.J.; Germana, L.H.; Wickramasinghe, P.; Tang, H.K.; Munambah, N.; Hossain, M.S.; Bang, P.; Hongyan, G.; Florindo, A.A.; Draper, C.E.; et al. Urban Versus Rural Differences in Meeting 24-h Movement Behaviour Guidelines Among 3–4-Year-Olds: An Analysis of SUNRISE Pilot Study Data From 10 Low- and Middle-Income Countries. Child Care Health Dev. 2024, 50, e70008. [Google Scholar] [CrossRef]
- Strong, W.B.; Malina, R.M.; Blimkie, C.J.R.; Daniels, S.R.; Dishman, R.K.; Gutin, B.; Hergenroeder, A.C.; Must, A.; Nixon, P.A.; Pivarnik, J.M.; et al. Evidence Based Physical Activity for School-Age Youth. J. Pediatr. 2005, 146, 732–737. [Google Scholar] [CrossRef]
- Munambah, N.; Gretschel, P.; Muchirahondo, F.C.; Chiwaridzo, M.; Chikwanha, T.M.; Kariippanon, K.E.; Chong, K.H.; Cross, P.L.; Draper, C.E.; Okely, A.D. 24 Hour Movement Behaviours and the Health and Development of Pre-School Children from Zimbabwean Settings: The SUNRISE Pilot Study. SA J. Sports Med. 2021, 33, v33i1a10864. [Google Scholar] [CrossRef]
- Iguacel, I.; Fernández-Alvira, J.M.; Bammann, K.; Chadjigeorgiou, C.; De Henauw, S.; Heidinger-Felső, R.; Lissner, L.; Michels, N.; Page, A.; Reisch, L.A.; et al. Social Vulnerability as a Predictor of Physical Activity and Screen Time in European Children. Int. J. Public Health 2018, 63, 283–295. [Google Scholar] [CrossRef]
- Sigmundová, D.; Vorlíček, M.; Voráčová, J.; Dygrýn, J.; Sigmund, E. Parental Impact on Adherence of Young Children to 24-h Movement Behaviour Guidelines: The Czech FAMIly Physical Activity, Sedentary Behaviour and Sleep Study. Eur. J. Public Health 2025, 35, 295–301. [Google Scholar] [CrossRef]
- Ball, K.; Carver, A.; Downing, K.; Jackson, M.; O’Rourke, K. Addressing the Social Determinants of Inequities in Physical Activity and Sedentary Behaviours. Health Promot. Int. 2015, 30, ii8–ii19. [Google Scholar] [CrossRef]
- Taylor, R.W.; Haszard, J.J.; Healey, D.; Meredith-Jones, K.A.; Taylor, B.J.; Galland, B.C. Adherence to 24-h Movement Behavior Guidelines and Psychosocial Functioning in Young Children: A Longitudinal Analysis. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 110. [Google Scholar] [CrossRef]
- Di Maglie, A.; Marsigliante, S.; My, G.; Colazzo, S.; Muscella, A. Effects of a Physical Activity Intervention on Schoolchildren Fitness. Physiol. Rep. 2022, 10, e15115. [Google Scholar] [CrossRef]
- Gómez-Carmona, C.D.; Rojas-Valverde, D.; Rico-González, M.; Ibáñez, S.J.; Pino-Ortega, J. What Is the Most Suitable Sampling Frequency to Register Accelerometry-Based Workload? A Case Study in Soccer. Proc. Inst. Mech. Eng. Part. P J. Sports Eng. Technol. 2020, 235, 114–121. [Google Scholar] [CrossRef]
- Rico-González, M.; Arcos, A.L.; Rojas-Valverde, D.; Clemente, F.M.; Pino-Ortega, J. A Survey to Assess the Quality of the Data Obtained by Radio-Frequency Technologies and Microelectromechanical Systems to Measure External Workload and Collective Behavior Variables in Team Sports. Sensors 2020, 20, 2271. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.M.; Summerbell, C.; Hobbs, M.; Hesketh, K.R.; Saxena, S.; Muir, C.; Hillier-Brown, F.C. A Systematic Review of the Validity, Reliability, and Feasibility of Measurement Tools Used to Assess the Physical Activity and Sedentary Behaviour of Pre-School Aged Children. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 141. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.; Boyle, B.; Lynch, H. Designing Public Playgrounds for Inclusion: A Scoping Review of Grey Literature Guidelines for Universal Design. Child. Geogr. 2023, 21, 422–441. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).