Rare Postoperative Complication of Esophageal Atresia after Open Thoracotomy Repair in Newborn—Lung Torsion: A Case Report
Abstract
1. Introduction
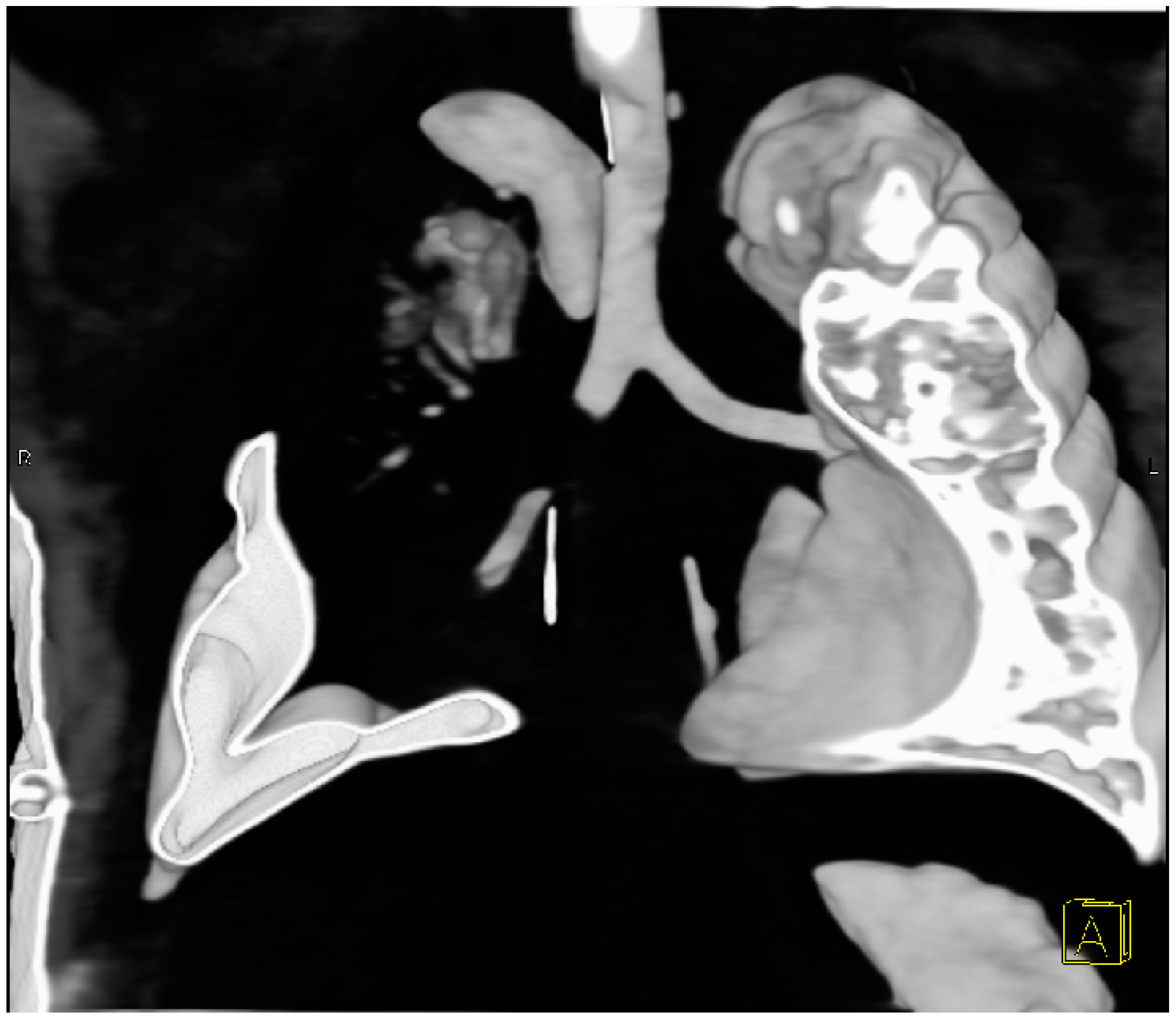
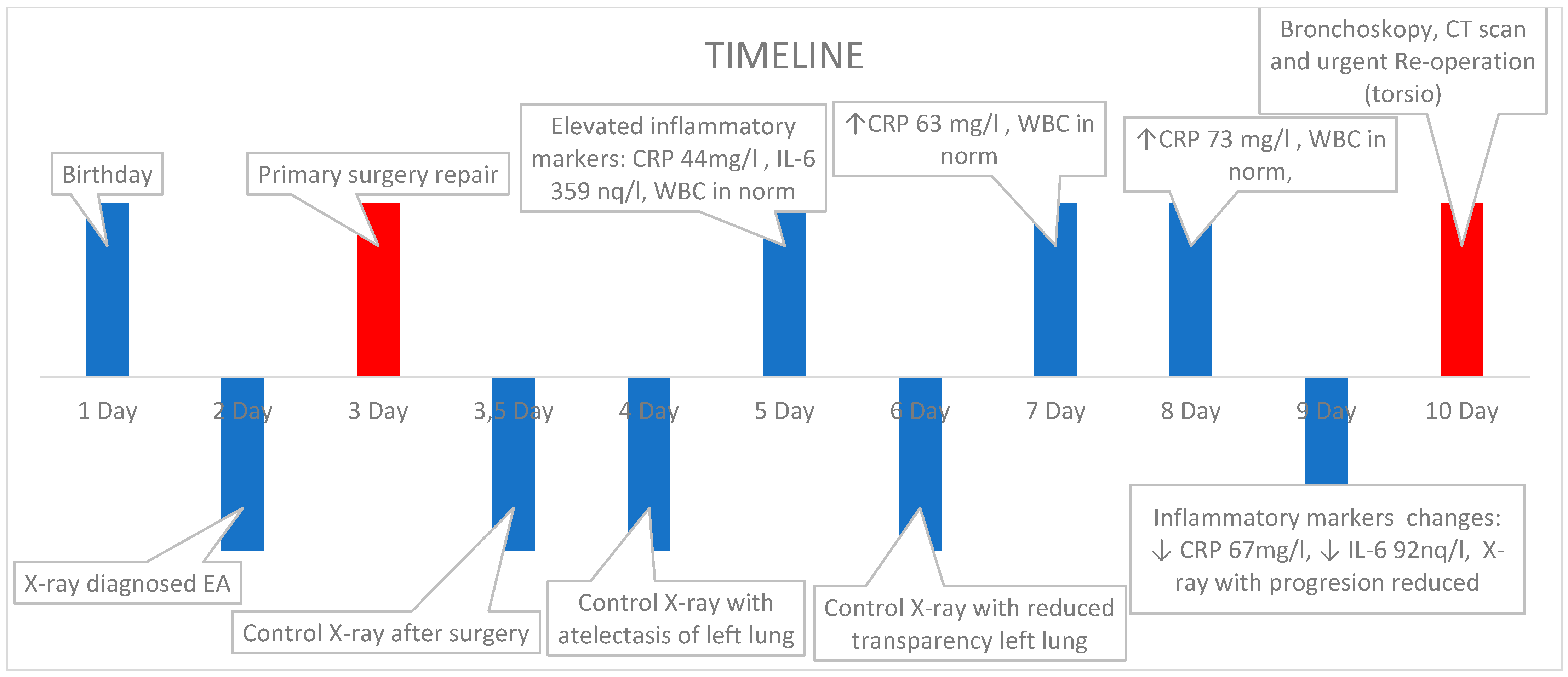
2. Case Presentation
2.1. Clinical History
2.2. Surgical Intervention
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baldwin, D.; Yadav, D. Esophageal Atresia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Kita, Y.; Go, T.; Nii, K.; Matsuura, N.; Yokomise, H. Spontaneous Torsion of the Right Upper Lung Lobe: A Case Report. Surg. Case Rep. 2017, 3, 37. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.; Zamakhshary, M.; Abdallah, M.R.; Miller, S.F.; Langer, J.C.; Wales, P.W.; Dasgupta, R. Lung torsion after tracheoesophageal fistula repair: A Case Report and review of literature. J. Pediatr. Surg. 2007, 42, E5–E9. [Google Scholar] [CrossRef]
- Yang, E.M.; Song, E.S.; In Jang, H.; Jeong, I.S.; Choi, Y.Y. Lung torsion after tracheoesophageal fistula repair in an infant. Korean J. Pediatr. 2013, 56, 186–190. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koziarkiewicz, M.; Taczalska, A.; Piaseczna-Piotrowska, A. Pulmonary torsion as an atypical complication of congenital esophageal atresia repair-a case report and review of literature. Eur. J. Pediatr. Surg. Rep. 2014, 2, 43–45. [Google Scholar] [CrossRef]
- Syed, M.K.; Al Faqeeh, A.A.; Othman, A.; Almas, T.; Khedro, T.; Alsufyani, R.; Almubarak, D.; Al Faqeh, R.; Syed, S.; Syed, S.K. Management of early post-operative complications of esophageal atresia with tracheoesophageal fistula: A retrospective study. Cureus 2020, 12, e11904. [Google Scholar] [CrossRef] [PubMed]
- Van Hoorn, C.E.; Costerus, S.A.; Lau, J.; Wijnen, R.M.H.; Vlot, J.; Tibboel, D.; de Graaff, J.C. Perioperative management of esophageal atresia/tracheo-esophageal fistula: An analysis of data of 101 consecutive patients. Paediatr. Anaesth. 2019, 29, 1024–1032. [Google Scholar] [CrossRef] [PubMed]
- Apostolakis, E.; Koletsis, E.N.; Panagopoulos, N.; Prokakis, C.; Dougenis, D. Fatal stroke after completion pneumonectomy for torsion of left upper lobe following left lower lobectomy. J. Cardiothorac. Surg. 2006, 1, 25. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Xie, D.; Wang, H.; He, W.; Zhou, Y.; Hernández-Arenas, L.A.; Jiang, G. predictors of survival in lung torsion: A systematic review and pooled analysis. J. Thorac. Cardiovasc. Surg. 2016, 152, 737–745.e3. [Google Scholar] [CrossRef]
- Thomas, P.A. The lung torsion dilemma: Detorsion without resection or resection without detorsion? J. Thorac. Cardiovasc. Surg. 2016, 152, 746. [Google Scholar] [CrossRef]
- Jalota Sahota, R.; Anjum, F. Lung Torsion. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]


| Authors | Year | Approach and Type of Execution | Reoperation Time after Primary Surgery |
|---|---|---|---|
| Oliveira et al. [3] | 2007 | Transpleural, detorsion 90° | 7 days |
| Yang et al. [4] | 2013 | Transpleural, detorsion 180° | 3 days |
| Segmentectomy RML | 10 days | ||
| Koziarkiewicz et al. [5] | 2014 | Transpleural, detorsion 180° | 8 days |
| Segmentectomy RML | 5 months | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gryboś, S.; Karaffová, V.; Klapačová, K. Rare Postoperative Complication of Esophageal Atresia after Open Thoracotomy Repair in Newborn—Lung Torsion: A Case Report. Pediatr. Rep. 2024, 16, 717-723. https://doi.org/10.3390/pediatric16030060
Gryboś S, Karaffová V, Klapačová K. Rare Postoperative Complication of Esophageal Atresia after Open Thoracotomy Repair in Newborn—Lung Torsion: A Case Report. Pediatric Reports. 2024; 16(3):717-723. https://doi.org/10.3390/pediatric16030060
Chicago/Turabian StyleGryboś, Szymon, Viera Karaffová, and Katarina Klapačová. 2024. "Rare Postoperative Complication of Esophageal Atresia after Open Thoracotomy Repair in Newborn—Lung Torsion: A Case Report" Pediatric Reports 16, no. 3: 717-723. https://doi.org/10.3390/pediatric16030060
APA StyleGryboś, S., Karaffová, V., & Klapačová, K. (2024). Rare Postoperative Complication of Esophageal Atresia after Open Thoracotomy Repair in Newborn—Lung Torsion: A Case Report. Pediatric Reports, 16(3), 717-723. https://doi.org/10.3390/pediatric16030060








