Evaluating Family Coping Mechanisms in Pediatric Seizure Disorders: From Emergency Room to Long-Term Follow-Up
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Considerations
2.2. Questionnaires and Variables
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Literature Analysis
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alharthi, A.S.; Alzahrani, S.A.; Alharbi, A.A.; Al Thobaiti, L.Y.; Alghamdi, Y.S.; Al Shumrani, K.M.; Alghamdi, M.A.; Alghamdi, N.K.; Alzahrani, S.S.; Alharbi, S.A.; et al. Parents’ Knowledge, Awareness, and Attitude Toward Children with Epilepsy in the Al Baha Region, Saudi Arabia: A Cross-Sectional Study. Cureus 2023, 15, e48057. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singh, R.; Kumari, R.; Prabhakaran, T. Clinical spectrum and neuroimaging findings in children with seizures: A five-year retrospective study. Iran. J. Child Neurol. 2022, 16, 157–166. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jackson, M.C.; Vasquez, A.; Ojo, O.; Fialkow, A.; Hammond, S.; Stredny, C.M.; Antonetty, A.; Loddenkemper, T. Identifying Barriers to Care in the Pediatric Acute Seizure Care Pathway. Int. J. Integr. Care 2022, 22, 28. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Albaradie, R.; Habibullah, H.; Mir, A.; Alshammari, A.K.; Alajmi, M.S.; Alsubaie, F.A.; Alsudairi, R.R.; Bashir, S. The prevalence of seizures in children with developmental delay. Neurosciences 2021, 26, 186–191. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, C.; Hu, Y.; Zhou, J.; Guan, Y.; Wang, M.; Qi, X.; Wang, X.; Zhang, H.; Adilijiang, A.; Li, T.; et al. Retrospective Clinical Analysis of Epilepsy Treatment for Children with Drug-Resistant Epilepsy (A Single-Center Experience). Brain Sci. 2022, 13, 14. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jaygopal, M.; Jain, S.; Malhotra, S.; Purkayastha, A.; Singhal, S. Factors Affecting Stress Levels in Attendants Accompanying Patients to Emergency Department. J. Emergencies Trauma Shock 2022, 15, 116–123. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- León-Campos, Á.; García-Mayor, S.; Martí-García, C.; Morilla-Herrera, J.C.; Morales-Asencio, J.M.; Lupiáñez-Pérez, I.; Pérez-Ardanaz, B.; Cuevas Fernandez-Gallego, M. Quality of Life, Physical and Mental Health, and Economic Evaluation of Family Caregivers of Chronic Dependent Children: INFAPRINT Cohort Study Protocol. Int. J. Environ. Res. Public Health 2023, 20, 5081. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ocansey, P.M.; Kretchy, I.A.; Aryeetey, G.C.; Agyabeng, K.; Nonvignon, J. Anxiety, depression, and stress in caregivers of children and adolescents with mental disorders in Ghana and implications for medication adherence. Ghana Med. J. 2021, 55, 173–182. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Malm-Buatsi, E.; Aston, C.E.; Ryan, J.; Tao, Y.; Palmer, B.W.; Kropp, B.P.; Klein, J.; Wisniewski, A.B.; Frimberger, D. Mental health and parenting characteristics of caregivers of children with spina bifida. J. Pediatr. Urol. 2015, 11, 65.e1–65.e7. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.D.; Hodges, A.; Hajcak, G.; Shankman, S.A. Anxiety sensitivity and the anticipation of predictable and unpredictable threat: Evidence from the startle response and event-related potentials. J. Anxiety Disord. 2015, 33, 62–71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Williams, L.E.; Oler, J.A.; Fox, A.S.; McFarlin, D.R.; Rogers, G.M.; Jesson, M.A.; Davidson, R.J.; Pine, D.S.; Kalin, N.H. Fear of the unknown: Uncertain anticipation reveals amygdala alterations in childhood anxiety disorders. Neuropsychopharmacology 2015, 40, 1428–1435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bendowska, A.; Baum, E. The Significance of Cooperation in Interdisciplinary Health Care Teams as Perceived by Polish Medical Students. Int. J. Environ. Res. Public Health 2023, 20, 954. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lennox-Chhugani, N. Inter-Disciplinary Work in the Context of Integrated Care—A Theoretical and Methodological Framework. Int. J. Integr. Care 2023, 23, 29. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Warren, J.L.; Warren, J.S. The Case for Understanding Interdisciplinary Relationships in Health Care. Ochsner J. 2023, 23, 94–97. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fazel, M.; Townsend, A.; Stewart, H.; Pao, M.; Paz, I.; Walker, J.; Sawyer, S.M.; Sharpe, M. Integrated care to address child and adolescent health in the 21st century: A clinical review. JCPP Adv. 2021, 1, e12045. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ronen, G.M.; Streiner, D.L.; Rosenbaum, P. Health-related quality of life in childhood epilepsy: Moving beyond ‘seizure control with minimal adverse effects’. Health Qual. Life Outcomes 2003, 1, 36. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schillinger, D. Social Determinants, Health Literacy, and Disparities: Intersections and Controversies. Health Lit. Res. Pract. 2021, 5, e234–e243. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coombs, N.C.; Meriwether, W.E.; Caringi, J.; Newcomer, S.R. Barriers to healthcare access among U.S. adults with mental health challenges: A population-based study. SSM Popul. Health 2021, 15, 100847. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Duma, O.O.; Roşu, S.T.; Manole, M.; Petrariu, F.D.; Constantin, B. Disparities in the access to primary healthcare in rural areas from the county of Iasi—Romania. Rev. Med. Chir. Soc. Med. Nat. Iasi 2014, 118, 743–748. [Google Scholar] [PubMed]
- Mosca, I.; Radu, C.; Strilciuc, Ș.; Ungureanu, M.I. A five-year (2017–2021) time series evaluation of patient-reported informal healthcare payments in Romania. J. Med. Life 2023, 16, 387–393. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- George, S.; Daniels, K.; Fioratou, E. A qualitative study into the perceived barriers of accessing healthcare among a vulnerable population involved with a community centre in Romania. Int. J. Equity Health 2018, 17, 41. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Michopoulos, I.; Douzenis, A.; Kalkavoura, C.; Christodoulou, C.; Michalopoulou, P.; Kalemi, G.; Fineti, K.; Patapis, P.; Protopapas, K.; Lykouras, L. Hospital Anxiety and Depression Scale (HADS): Validation in a Greek general hospital sample. Ann. Gen. Psychiatry 2008, 7, 4. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bastianon, C.D.; Klein, E.M.; Tibubos, A.N.; Brähler, E.; Beutel, M.E.; Petrowski, K. Perceived Stress Scale (PSS-10) psychometric properties in migrants and native Germans. BMC Psychiatry 2020, 20, 450. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ríos, M.; Zekri, S.; Alonso-Esteban, Y.; Navarro-Pardo, E. Parental Stress Assessment with the Parenting Stress Index (PSI): A Systematic Review of Its Psychometric Properties. Children 2022, 9, 1649. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schroeder, S.R.; Rojahn, J.; An, X.; Mayo-Ortega, L.; Oyama-Ganiko, R.; Leblanc, J. The Parental Concerns Questionnaire: A Brief Screening Instrument for Potentially Severe Behavior Problems in Infants and Toddlers At-Risk for Developmental Delays. J. Dev. Phys. Disabil. 2014, 26, 237–247. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rozensztrauch, A.; Kołtuniuk, A. The Quality of Life of Children with Epilepsy and the Impact of the Disease on the Family Functioning. Int. J. Environ. Res. Public Health 2022, 19, 2277. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Subki, A.H.; Mukhtar, A.M.; Al-Harbi, R.S.; Alotaibi, A.K.; Mosaad, F.G.; Alsallum, M.S.; Jan, M.M.S. The Impact of Pediatric Epilepsy on Children and Families: A Multicenter Cross-Sectional Study. Clin. Pract. Epidemiol. Ment. Health 2018, 14, 323–333. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Camfield, C.; Breau, L.; Camfield, P. Impact of pediatric epilepsy on the family: A new scale for clinical and research use. Epilepsia 2001, 42, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Nagabushana, D.; Praveen-Kumar, S.; Agadi, J.B. Impact of epilepsy and antiepileptic drugs on health and quality of life in Indian children. Epilepsy Behav. 2019, 93, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Fong, C.Y.; Chang, W.M.; Kong, A.N.; Rithauddin, A.M.; Khoo, T.B.; Ong, L.C. Quality of life in Malaysian children with epilepsy. Epilepsy Behav. 2018, 80, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Wo, S.W.; Lai, P.S.; Ong, L.C.; Low, W.Y.; Lim, K.S.; Tay, C.G.; Wong, C.P.; Ranjini, S. Cross-cultural adaptation of the Malay version of the parent-proxy Health-Related Quality of Life Measure for Children with Epilepsy (CHEQOL-25) in Malaysia. Epilepsy Behav. 2015, 45, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Verhey, L.H.; Kulik, D.M.; Ronen, G.M.; Rosenbaum, P.; Lach, L.; Streiner, D.L.; Canadian Pediatric Epilepsy Network. Quality of life in childhood epilepsy: What is the level of agreement between youth and their parents? Epilepsy Behav. 2009, 14, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Stevanovic, D.; Tepavcevic, D.K.; Jocic-Jakubi, B.; Jovanovic, M.; Pekmezovic, T.; Lakic, A.; Ronen, G.M. Health-Related Quality of Life Measure for Children with Epilepsy (CHEQOL-25): Preliminary data for the Serbian version. Epilepsy Behav. 2009, 16, 599–602. [Google Scholar] [CrossRef] [PubMed]

| Variables | n = 68 | % |
|---|---|---|
| Age of Child (mean ± SD) | 4.46 years | 2.36 |
| Age of Parent (mean ± SD) | 29.27 years | 4.78 |
| Child Age Range: 0–5 years (%) | 12 | 17.65% |
| Child Age Range: 6–12 years (%) | 36 | 52.94% |
| Child Age Range: 13–18 years (%) | 20 | 29.41% |
| Gender: Male (%) | 38 | 55.88% |
| Gender: Female (%) | 30 | 44.12% |
| Family Income Level: Low (%) | 14 | 20.59% |
| Family Income Level: Middle (%) | 34 | 50.00% |
| Family Income Level: High (%) | 20 | 29.41% |
| Parental Marital Status: Married (%) | 50 | 73.53% |
| Parental Marital Status: Other (%) | 18 | 26.47% |
| Education Level (Parent): High School or Less (%) | 15 | 22.06% |
| Education Level (Parent): College Degree (%) | 35 | 51.47% |
| Education Level (Parent): Advanced Degree (%) | 18 | 26.47% |
| Number of Siblings: None (%) | 22 | 32.35% |
| Number of Siblings: 1 or 2 (%) | 34 | 50.00% |
| Number of Siblings: 3 or more (%) | 12 | 17.65% |
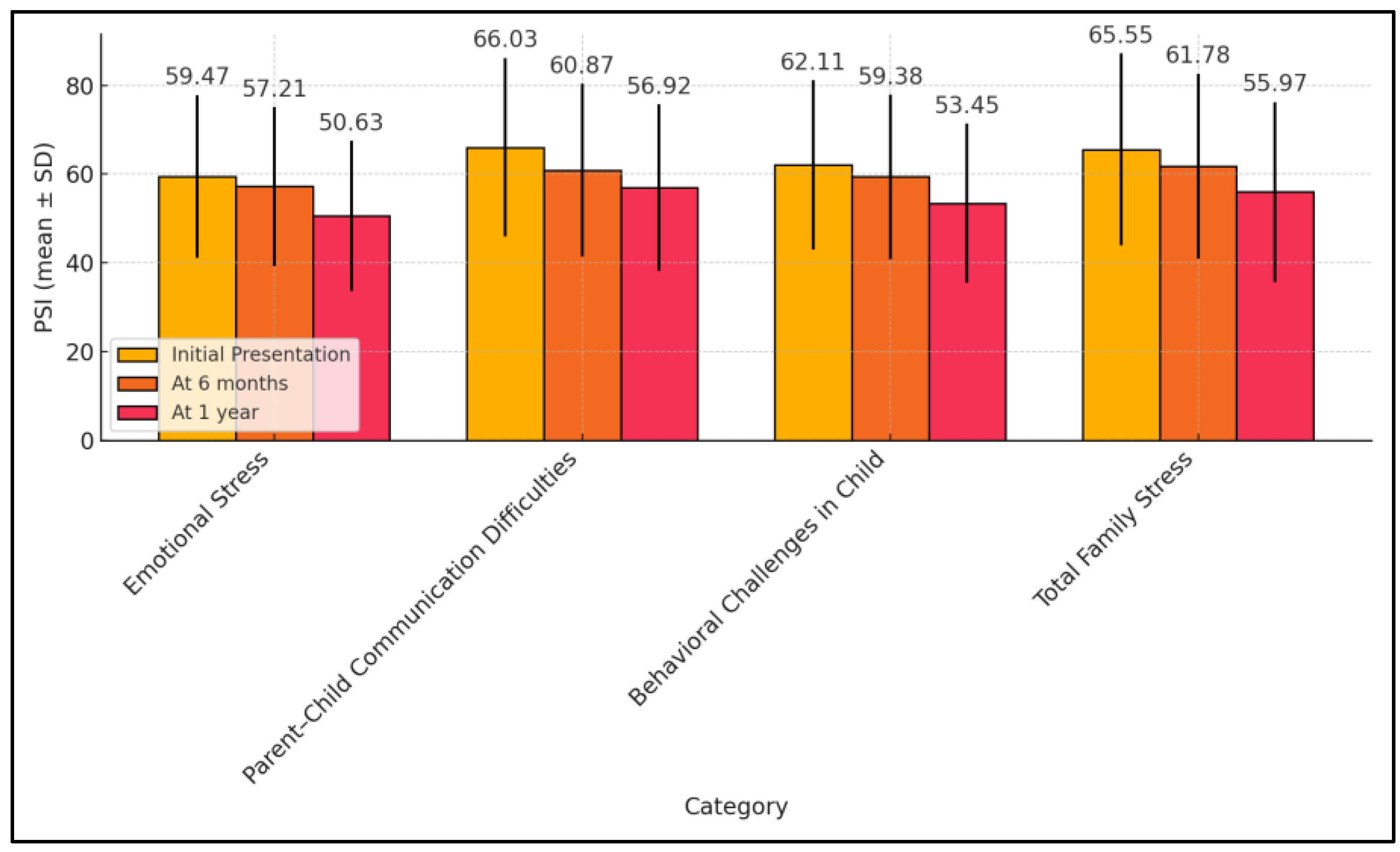
| PSI (Mean ± SD) | Initial Presentation (n = 68) | At 6 Months (n = 68) | At 1 Year (n = 68) | p-Value * |
|---|---|---|---|---|
| Emotional Stress | 59.47 ± 18.32 | 57.21 ± 17.89 | 50.63 ± 16.88 | 0.011 |
| Parent–Child Communication Difficulties | 66.03 ± 20.15 | 60.87 ± 19.46 | 56.92 ± 18.74 | 0.025 |
| Behavioral Challenges in Child | 62.11 ± 19.08 | 59.38 ± 18.55 | 53.45 ± 17.93 | 0.022 |
| Total Family Stress | 65.55 ± 21.65 | 61.78 ± 20.84 | 55.97 ± 20.30 | 0.029 |
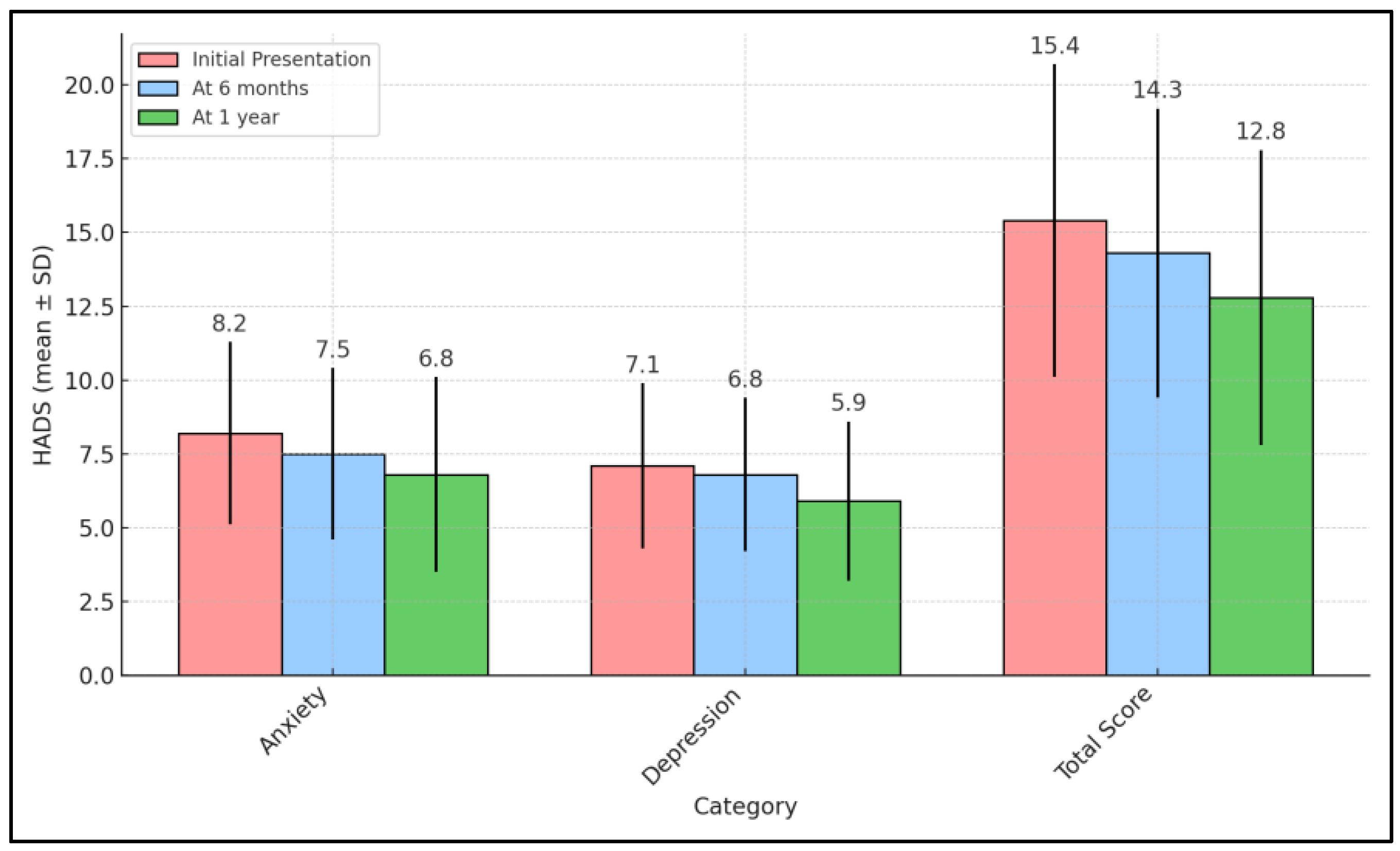
| HADS (Mean ± SD) | Initial Presentation (n = 68) | At 6 Months (n = 68) | At 1 Year (n = 68) | p-Value * |
|---|---|---|---|---|
| Anxiety | 8.2 ± 3.1 | 7.5 ± 2.9 | 6.8 ± 3.3 | 0.033 |
| Depression | 7.1 ± 2.8 | 6.8 ± 2.6 | 5.9 ± 2.7 | 0.028 |
| Total Score | 15.4 ± 5.3 | 14.3 ± 4.9 | 12.8 ± 5.0 | 0.017 |
| PCQ (Mean ± SD) | Initial Presentation (n = 68) | At 6 Months (n = 68) | At 1 Year (n = 68) | p-Value * |
|---|---|---|---|---|
| Practical impact | 3.2 ± 1.1 | 2.9 ± 1.0 | 2.5 ± 0.9 | <0.001 |
| Emotional impact | 3.7 ± 1.3 | 3.4 ± 1.2 | 3.0 ± 1.1 | 0.004 |
| Co-parent domain | 2.8 ± 1.2 | 2.5 ± 1.1 | 2.2 ± 1.0 | 0.007 |
| Total score | 9.7 ± 2.6 | 8.8 ± 2.4 | 7.7 ± 2.3 | <0.001 |
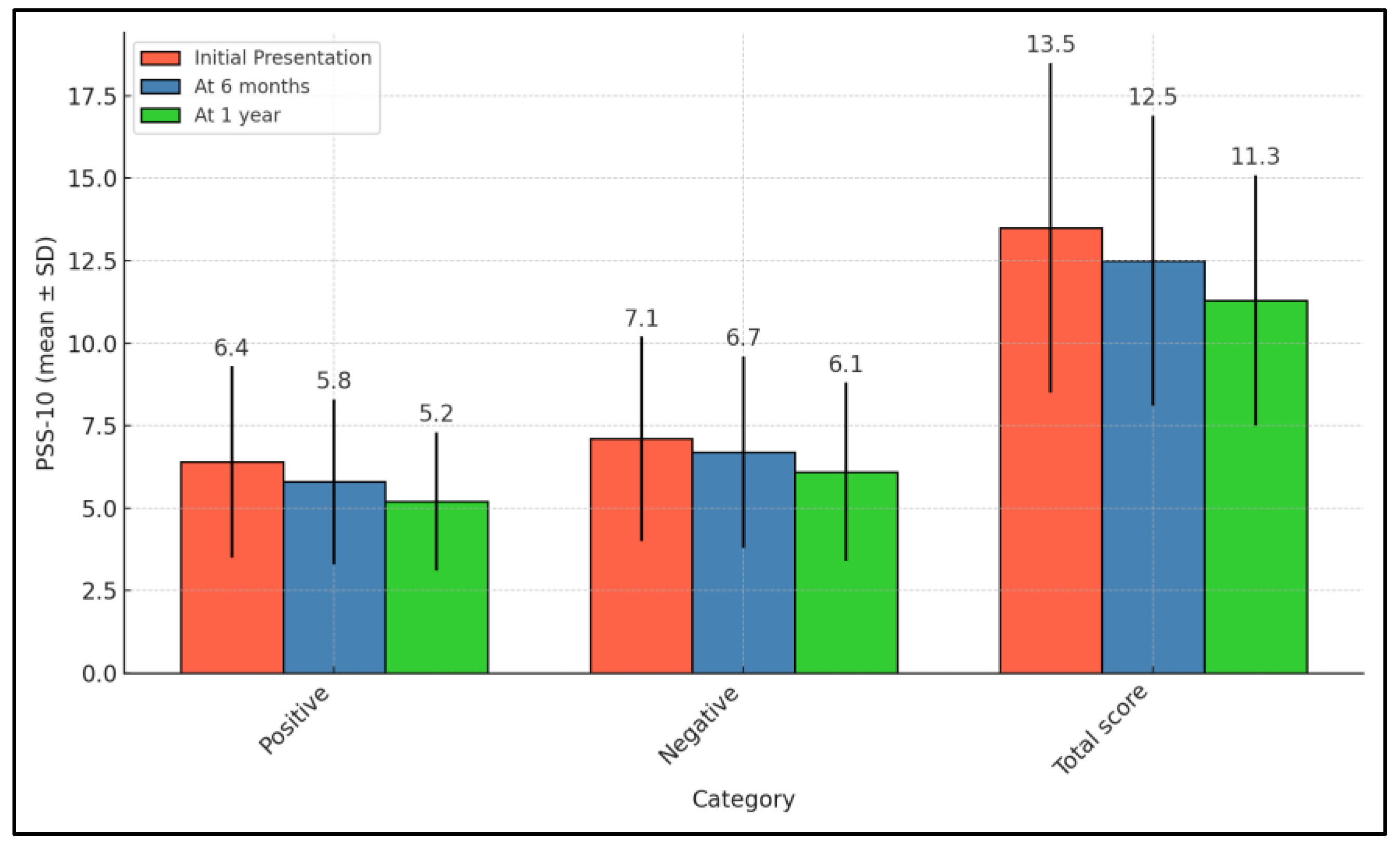
| PSS-10 (Mean ± SD) | Initial Presentation (n = 68) | At 6 Months (n = 68) | At 1 Year (n = 68) | p-Value * |
|---|---|---|---|---|
| Positive | 6.4 ± 2.9 | 5.8 ± 2.5 | 5.2 ± 2.1 | 0.023 |
| Negative | 7.1 ± 3.1 | 6.7 ± 2.9 | 6.1 ± 2.7 | 0.123 |
| Total score | 13.5 ± 5.0 | 12.5 ± 4.4 | 11.3 ± 3.8 | 0.016 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gruescu, A.C.S.; Popoiu, C.; Levai, M.C.; Barata, P.I.; Streian, C.G. Evaluating Family Coping Mechanisms in Pediatric Seizure Disorders: From Emergency Room to Long-Term Follow-Up. Pediatr. Rep. 2024, 16, 657-668. https://doi.org/10.3390/pediatric16030055
Gruescu ACS, Popoiu C, Levai MC, Barata PI, Streian CG. Evaluating Family Coping Mechanisms in Pediatric Seizure Disorders: From Emergency Room to Long-Term Follow-Up. Pediatric Reports. 2024; 16(3):657-668. https://doi.org/10.3390/pediatric16030055
Chicago/Turabian StyleGruescu, Ada Claudia Silvana, Calin Popoiu, Mihaela Codrina Levai, Paula Irina Barata, and Caius Glad Streian. 2024. "Evaluating Family Coping Mechanisms in Pediatric Seizure Disorders: From Emergency Room to Long-Term Follow-Up" Pediatric Reports 16, no. 3: 657-668. https://doi.org/10.3390/pediatric16030055
APA StyleGruescu, A. C. S., Popoiu, C., Levai, M. C., Barata, P. I., & Streian, C. G. (2024). Evaluating Family Coping Mechanisms in Pediatric Seizure Disorders: From Emergency Room to Long-Term Follow-Up. Pediatric Reports, 16(3), 657-668. https://doi.org/10.3390/pediatric16030055





