Foreign Bodies in Pediatric Otorhinolaryngology: A Review
Abstract
1. Introduction
2. Aural Foreign Bodies
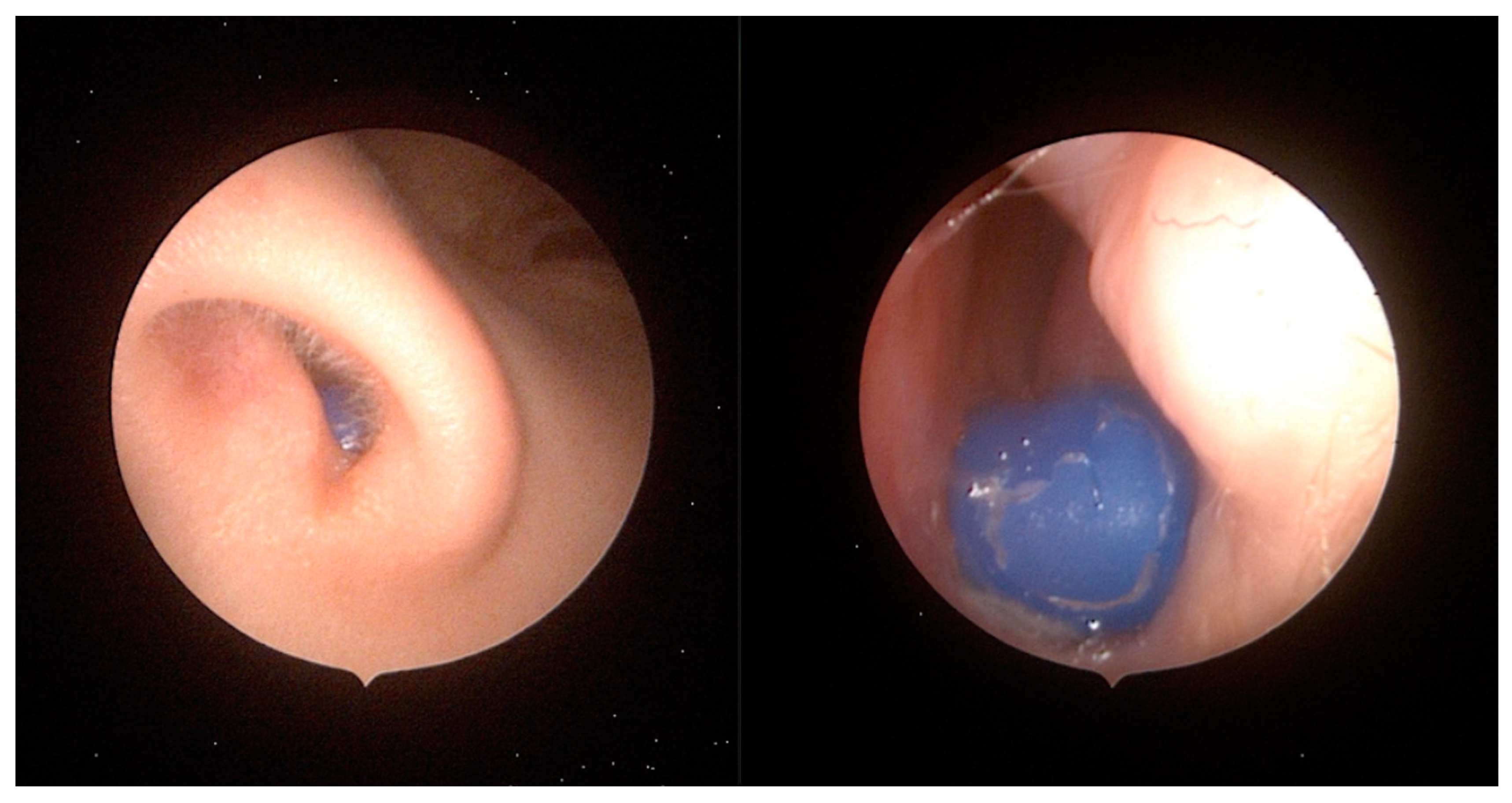
3. Nasal Foreign Bodies
4. Pharyngeal Foreign Bodies
5. Laryngeal Foreign Bodies
6. Tracheobronchial Foreign Bodies
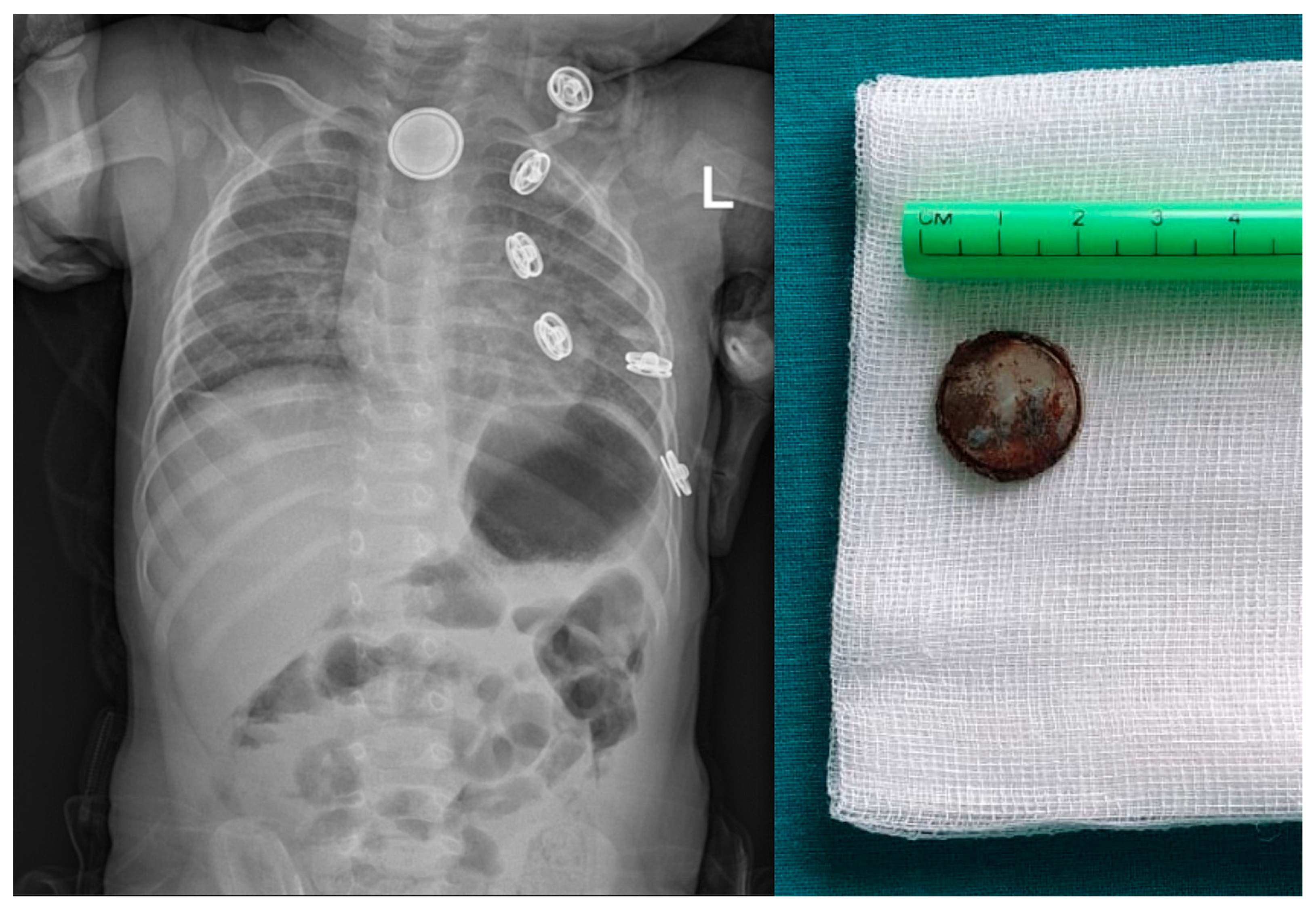
7. Esophageal Foreign Bodies
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hssaine, K.; Belhoucha, B.; Rochdi, Y.; Nouri, H.; Aderdour, L.; Raji, A. Foreign bodies in ENT: Ten-year experience. Pan Afr. Med. J. 2015, 21, 91. [Google Scholar] [CrossRef] [PubMed]
- Hon, S.K.; Izam, T.M.; Koay, C.B.; Razi, A. A prospective evaluation of foreign bodies presenting to the Ear, Nose and Throat Clinic, Hospital Kuala Lumpur. Med. J. Malays. 2001, 56, 463–470. [Google Scholar]
- Mangussi-Gomes, J.; Andrade, J.S.; Matos, R.C.; Kosugi, E.M.; Penido Nde, O. ENT foreign bodies: Profile of the cases seen at a tertiary hospital emergency care unit. Braz. J. Otorhinolaryngol. 2013, 79, 699–703. [Google Scholar] [CrossRef] [PubMed]
- Akenroye, M.I.; Osukoya, A.T. Uncommon, undeclared oesophageal foreign bodies. Niger. J. Clin. Pract. 2012, 15, 244–246. [Google Scholar] [CrossRef] [PubMed]
- Yaroko, A.; Irfan, M. An annual audit of the ear foreign bodies in hospital universiti sains malaysia. Malays. Fam. Physician 2012, 7, 2–5. [Google Scholar]
- Figueiredo, R.R.; Azevedo, A.A.; Kos, A.O.; Tomita, S. Complications of ent foreign bodies: A retrospective study. Braz. J. Otorhinolaryngol. 2008, 74, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Bakhshaee, M.; Hebrani, P.; Shams, M.; Salehi, M.; Ghaffari, A.; Rajati, M. Psychological status in children with ear and nose foreign body insertion. Int. J. Pediatr. Otorhinolaryngol. 2017, 92, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Iseh, K.R.; Yahaya, M. Ear foreign bodies: Observations on the clinical profile in Sokoto, Nigeria. Ann. Afr. Med. 2008, 7, 18–23. [Google Scholar] [CrossRef]
- Schuldt, T.; Großmann, W.; Weiss, N.M.; Ovari, A.; Mlynski, R.; Schraven, S.P. Aural and nasal foreign bodies in children-Epidemiology and correlation with hyperkinetic disorders, developmental disorders and congenital malformations. Int. J. Pediatr. Otorhinolaryngol. 2019, 118, 165–169. [Google Scholar] [CrossRef]
- Perera, H.; Fernando, S.M.; Yasawardena, A.D.K.S.N.; Karunaratne, I. Prevalence of attention deficit hyperactivity disorder (ADHD) in children presenting with self-inserted nasal and aural foreign bodies. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 1362–1364. [Google Scholar] [CrossRef]
- Ngo, A.; Ng, K.C.; Sim, T.P. Otorhinolaryngeal foreign bodies in children presenting to the emergency department. Singapore Med. J. 2005, 46, 172–178. [Google Scholar]
- Endican, S.; Garap, J.P.; Dubey, S.P. Ear, nose and throat foreign bodies in Melanesian children: An analysis of 1037 cases. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 1539–1545. [Google Scholar] [CrossRef]
- Schulze, S.L.; Kerschner, J.; Beste, D. Pediatric external auditory canal foreign bodies: A review of 698 cases. Otolaryngol. Head Neck Surg. 2002, 127, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Bysice, A.; Araslanova, R.; Dzioba, A.; Husein, M. Management of pediatric aural foreign bodies: Towards a universal Otolaryngology referral algorithm. Int. J. Pediatr. Otorhinolaryngol. 2023, 167, 111493. [Google Scholar] [CrossRef] [PubMed]
- Cetinkaya, E.A.; Arslan, I.B.; Cukurova, I. Nasal foreign bodies in children: Types, locations, complications and removal. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 1881–1885. [Google Scholar] [CrossRef]
- Awad, A.H.; ElTaher, M. ENT Foreign Bodies: An Experience. Int. Arch. Otorhinolaryngol. 2018, 22, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Lomate, S.; Ekhar, V.; Chandankhede, V.; Shelkar, R.; Vedi, J. A Prospective Clinical Study of Foreign Bodies in Ear, Nose and Upper Aerodigestive Tract-Our Experience. Indian J. Otolaryngol. Head Neck Surg. 2023, 75, 3461–3466. [Google Scholar] [CrossRef]
- Stoner, M.J.; Dulaurier, M. Pediatric ENT emergencies. Emerg. Med. Clin. N. Am. 2013, 31, 795–808. [Google Scholar] [CrossRef]
- Shih, M.; Brock, L.; Liu, Y.C.C. Pediatric Aural Foreign Body Extraction: Comparison of Efficacies Among Clinical Settings and Retrieval Methods. Otolaryngol. Head Neck Surg. 2021, 164, 662–666. [Google Scholar] [CrossRef]
- Ansley, J.F.; Cunningham, M.J. Treatment of aural foreign bodies in children. Pediatrics 1998, 101, 638–641. [Google Scholar] [CrossRef]
- Heim, S.W.; Maughan, K.L. Foreign bodies in the ear, nose, and throat. Am. Fam. Physician 2007, 76, 1185–1189. [Google Scholar] [PubMed]
- DiMuzio, J., Jr.; Deschler, D.G. Emergency department management of foreign bodies of the external ear canal in children. Otol. Neurotol. 2002, 23, 473–475. [Google Scholar] [CrossRef] [PubMed]
- Abou-Elfadl, M.; Horra, A.; Abada, R.L.; Mahtar, M.; Roubal, M.; Kadiri, F. Nasal foreign bodies: Results of a study of 260 cases. Eur. Ann. Otorhinolaryngol. Head. Neck Dis. 2015, 132, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Gregori, D.; Salerni, L.; Scarinzi, C.; Morra, B.; Berchialla, P.; Snidero, S.; Corradetti, R.; Passali, D.; Group, E.S. Foreign bodies in the nose causing complications and requiring hospitalization in children 0–14 age: Results from the European survey of foreign bodies injuries study. Rhinology 2008, 46, 28–33. [Google Scholar] [PubMed]
- Figueiredo, R.R.; Azevedo, A.A.; Kos, A.O.; Tomita, S. Nasal foreign bodies: Description of types and complications in 420 cases. Braz. J. Otorhinolaryngol. 2006, 72, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Chan, T.C.; Ufberg, J.; Harrigan, R.A.; Vilke, G.M. Nasal foreign body removal. J. Emerg. Med. 2004, 26, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Tong, M.C.; Ying, S.Y.; van Hasselt, C.A. Nasal foreign bodies in children. Int. J. Pediatr. Otorhinolaryngol. 1996, 35, 207–211. [Google Scholar] [CrossRef]
- Davies, P.H.; Benger, J.R. Foreign bodies in the nose and ear: A review of techniques for removal in the emergency department. J. Accid. Emerg. Med. 2000, 17, 91–94. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Loh, W.S.; Leong, J.L.; Tan, H.K. Hazardous foreign bodies: Complications and management of button batteries in nose. Ann. Otol. Rhinol. Laryngol. 2003, 112, 379–383. [Google Scholar] [CrossRef]
- Kiger, J.R.; Brenkert, T.E.; Losek, J.D. Nasal foreign body removal in children. Pediatr. Emerg. Care 2008, 24, 785–792, quiz 790–792. [Google Scholar] [CrossRef]
- Purohit, N.; Ray, S.; Wilson, T.; Chawla, O.P. The “parent’s kiss”: An effective way to remove paediatric nasal foreign bodies. Ann. R. Coll. Surg. Engl. 2008, 90, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Cook, S.; Burton, M.; Glasziou, P. Efficacy and safety of the “mother’s kiss” technique: A systematic review of case reports and case series. CMAJ 2012, 184, E904–E912. [Google Scholar] [CrossRef] [PubMed]
- Handbook of Non Drug Intervention (HANDI) Project Team; Glasziou, P.; Bennett, J.; Greenberg, P.; Green, S.; Gunn, J.; Hoffman, T.; Pirotta, M. Mother’s kiss for nasal foreign bodies. Aust. Fam. Physician 2013, 42, 288–289. [Google Scholar] [PubMed]
- Navitsky, R.C.; Beamsley, A.; McLaughlin, S. Nasal positive-pressure technique for nasal foreign body removal in children. Am. J. Emerg. Med. 2002, 20, 103–104. [Google Scholar] [CrossRef]
- Lim, C.W.; Park, M.H.; Do, H.J.; Yeom, J.S.; Park, J.S.; Park, E.S.; Seo, J.H.; Park, J.J.; Lim, J.Y.; Park, C.H. Factors Associated with Removal of Impactted Fishbone in Children, Suspected Ingestion. Pediatr. Gastroenterol. Hepatol. Nutr. 2016, 19, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Chawla, A.; Eng, S.P.; Peh, W.C. Clinics in diagnostic imaging (100). Migrated pharyngeal fish bone. Singap. Med. J. 2004, 45, 397–402, quiz 403. [Google Scholar]
- Kay, M.; Wyllie, R. Pediatric foreign bodies and their management. Curr. Gastroenterol. Rep. 2005, 7, 212–218. [Google Scholar] [CrossRef]
- Higo, R.; Matsumoto, Y.; Ichimura, K.; Kaga, K. Foreign bodies in the aerodigestive tract in pediatric patients. Auris Nasus Larynx 2003, 30, 397–401. [Google Scholar] [CrossRef]
- Bloom, D.C.; Christenson, T.E.; Manning, S.C.; Eksteen, E.C.; Perkins, J.A.; Inglis, A.F.; Stool, S.E. Plastic laryngeal foreign bodies in children: A diagnostic challenge. Int. J. Pediatr. Otorhinolaryngol. 2005, 69, 657–662. [Google Scholar] [CrossRef]
- Mathiasen, R.A.; Cruz, R.M. Asymptomatic near-total airway obstruction by a cylindrical tracheal foreign body. Laryngoscope 2005, 115, 274–277. [Google Scholar] [CrossRef]
- Robinson, P.J. Laryngeal foreign bodies in children: First stop before the right main bronchus. J. Paediatr. Child. Health 2003, 39, 477–479. [Google Scholar] [CrossRef]
- Berkowitz, R.G.; Lim, W.K. Laryngeal foreign bodies in children revisited. Ann. Otol. Rhinol. Laryngol. 2003, 112, 866–868. [Google Scholar] [CrossRef]
- Zaritsky, A.; Nadkarni, V.; Getson, P.; Kuehl, K. CPR in children. Ann. Emerg. Med. 1987, 16, 1107–1111. [Google Scholar] [CrossRef]
- Shubha, A.M.; Das, K. Tracheobronchial foreign bodies in infants. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 1385–1389. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Chu, H.; Tao, Y.; Huang, H.; Peng, L. Lessons Learned From 35 Cases of Laryngeal Foreign Bodies Undergoing Misdiagnosis in Pediatric Population. Ann. Otol. Rhinol. Laryngol. 2017, 126, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.J.; Goo, H.W.; Roh, J.L. Utility of spiral and cine CT scans in pediatric patients suspected of aspirating radiolucent foreign bodies. Otolaryngol. Head Neck Surg. 2008, 138, 576–580. [Google Scholar] [CrossRef]
- Cevik, M.; Gokdemir, M.T.; Boleken, M.E.; Sogut, O.; Kurkcuoglu, C. The characteristics and outcomes of foreign body ingestion and aspiration in children due to lodged foreign body in the aerodigestive tract. Pediatr. Emerg. Care 2013, 29, 53–57, quiz 301. [Google Scholar] [CrossRef] [PubMed]
- Fidkowski, C.W.; Zheng, H.; Firth, P.G. The anesthetic considerations of tracheobronchial foreign bodies in children: A literature review of 12,979 cases. Anesth. Analg. 2010, 111, 1016–1025. [Google Scholar] [CrossRef]
- Sink, J.R.; Kitsko, D.J.; Georg, M.W.; Winger, D.G.; Simons, J.P. Predictors of Foreign Body Aspiration in Children. Otolaryngol. Head Neck Surg. 2016, 155, 501–507. [Google Scholar] [CrossRef]
- Lakhkar, B.B.; Kini, P.; Shenoy, V.; Bhaskaranand, N. Foreign body aspiration: Manipal experience. Indian Pediatr. 2000, 37, 193–195. [Google Scholar]
- Tan, H.K.; Brown, K.; McGill, T.; Kenna, M.A.; Lund, D.P.; Healy, G.B. Airway foreign bodies (FB): A 10-year review. Int. J. Pediatr. Otorhinolaryngol. 2000, 56, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Punnoose, S.E.; Victor, J.; Hazarika, P.; Ss, M. C-MAC(R) video-laryngoscope assisted removal of pediatric upper airway foreign body via apneic technique: Two case reports. SAGE Open Med. Case Rep. 2019, 7, 2050313X18823088. [Google Scholar] [CrossRef] [PubMed]
- Eren, S.; Balci, A.E.; Dikici, B.; Doblan, M.; Eren, M.N. Foreign body aspiration in children: Experience of 1160 cases. Ann. Trop. Paediatr. 2003, 23, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Chapin, M.M.; Rochette, L.M.; Annest, J.L.; Haileyesus, T.; Conner, K.A.; Smith, G.A. Nonfatal choking on food among children 14 years or younger in the United States, 2001–2009. Pediatrics 2013, 132, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Altkorn, R.; Chen, X.; Milkovich, S.; Stool, D.; Rider, G.; Bailey, C.M.; Haas, A.; Riding, K.H.; Pransky, S.M.; Reilly, J.S. Fatal and non-fatal food injuries among children (aged 0–14 years). Int. J. Pediatr. Otorhinolaryngol. 2008, 72, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Gardner, H.G.; Baum, C.C.R.; Dowd, M.D.; Durbin, D.R.; Lichenstein, R.; Quinlan, K.P.; Sege, R.D.; Turner, M.S.; Weiss, J.C.; Smith, G.A.; et al. Prevention of choking among children. Pediatrics 2010, 125, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, W.X.; Cai, Y.R. A time series observation of Chinese children undergoing rigid bronchoscopy for an inhaled foreign body: 3149 cases in 1991–2010. Chin. Med. J. 2015, 128, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Ding, G.; Wu, B.; Vinturache, A.; Cai, C.; Lu, M.; Gu, H.; Palazón-Bru, A. Tracheobronchial foreign body aspiration in children: A retrospective single-center cross-sectional study. Medicine 2020, 99, E20480. [Google Scholar] [CrossRef]
- Shah, R.K.; Patel, A.; Lander, L.; Choi, S.S. Management of foreign bodies obstructing the airway in children. Arch. Otolaryngol. Head Neck Surg. 2010, 136, 373–379. [Google Scholar] [CrossRef][Green Version]
- Jiaqiang, S.; Jingwu, S.; Yanming, H.; Qiuping, L.; Yinfeng, W.; Xianguang, L.; Guanglun, W.; Demin, H. Rigid bronchoscopy for inhaled pen caps in children. J. Pediatr. Surg. 2009, 44, 1708–1711. [Google Scholar] [CrossRef]
- Yang, X.J.; Zhang, J.; Chu, P.; Guo, Y.L.; Tai, J.; Zhang, Y.M.; Tang, L.X.; Ni, X. Pneumomediastinum Secondary to Foreign Body Aspiration: Clinical Features and Treatment Explorement in 39 Pediatric Patients. Chin. Med. J. 2016, 129, 2691–2696. [Google Scholar] [CrossRef]
- Sultan, T.A.; van As, A.B. Review of tracheobronchial foreign body aspiration in the South African paediatric age group. J. Thorac. Dis. 2016, 8, 3787–3796. [Google Scholar] [CrossRef]
- Boufersaoui, A.; Smati, L.; Benhalla, K.N.; Boukari, R.; Smail, S.; Anik, K.; Aouameur, R.; Chaouche, H.; Baghriche, M. Foreign body aspiration in children: Experience from 2624 patients. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 1683–1688. [Google Scholar] [CrossRef]
- Antón-Pacheco, J.L.; Martín-Alelú, R.; López, M.; Morante, R.; Merino-Mateo, L.; Barrero, S.; Castilla, R.; Cano, I.; Garcia, A.; Gómez, A. Foreign body aspiration in children: Treatment timing and related complications. Int. J. Pediatr. Otorhinolaryngol. 2021, 144, 110690. [Google Scholar] [CrossRef] [PubMed]
- Na’ara, S.; Vainer, I.; Amit, M.; Gordin, A. Foreign Body Aspiration in Infants and Older Children: A Comparative Study. Ear Nose Throat J. 2020, 99, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Linnaus, M.; Notrica, D. Airway foreign bodies in pediatric patients: Anatomic location of foreign body affects complications and outcomes. Pediatr. Surg. Int. 2017, 33, 59–64. [Google Scholar] [CrossRef]
- Tang, L.F.; Xu, Y.C.; Wang, Y.S.; Wang, C.F.; Zhu, G.H.; Bao, X.E.; Lu, M.P.; Chen, L.X.; Chen, Z.M. Airway foreign body removal by flexible bronchoscopy: Experience with 1027 children during 2000–2008. World J. Pediatr. 2009, 5, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Johnson, D.G.; Matlak, M.E. Bronchoscopic removal of aspirated foreign bodies in children. J. Pediatr. Surg. 1994, 29, 682–684. [Google Scholar] [CrossRef]
- Rodriguez, H.; Passali, G.C.; Gregori, D.; Chinski, A.; Tiscornia, C.; Botto, H.; Nieto, M.; Zanetta, A.; Passali, D.; Cuestas, G. Management of foreign bodies in the airway and oesophagus. Int. J. Pediatr. Otorhinolaryngol. 2012, 76 (Suppl. S1), S84–S91. [Google Scholar] [CrossRef]
- Even, L.; Heno, N.; Talmon, Y.; Samet, E.; Zonis, Z.; Kugelman, A. Diagnostic evaluation of foreign body aspiration in children: A prospective study. J. Pediatr. Surg. 2005, 40, 1122–1127. [Google Scholar] [CrossRef]
- Ayed, A.K.; Jafar, A.M.; Owayed, A. Foreign body aspiration in children: Diagnosis and treatment. Pediatr. Surg. Int. 2003, 19, 485–488. [Google Scholar] [CrossRef]
- Paksu, S.; Paksu, M.S.; Kilic, M.; Guner, S.N.; Baysal, K.; Sancak, R.; Ozturk, F. Foreign body aspiration in childhood: Evaluation of diagnostic parameters. Pediatr. Emerg. Care 2012, 28, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Louie, M.C.; Bradin, S. Foreign body ingestion and aspiration. Pediatr. Rev. 2009, 30, 295–301. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chung, M.K.; Jeong, H.S.; Ahn, K.M.; Park, S.H.; Cho, J.K.; Son, Y.I.; Baek, C.H. Pulmonary recovery after rigid bronchoscopic retrieval of airway foreign body. Laryngoscope 2007, 117, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Fahy, J.V.; Dickey, B.F. Airway mucus function and dysfunction. N. Engl. J. Med. 2010, 363, 2233–2247. [Google Scholar] [CrossRef]
- Rance, A.; Mittaine, M.; Michelet, M.; Martin Blondel, A.; Labouret, G. Delayed diagnosis of foreign body aspiration in children. Arch. Pediatr. 2022, 29, 424–428. [Google Scholar] [CrossRef]
- Wu, Y.; Dai, J.; Wang, G.; Li, Y.; Li, H.; Wu, C.; Wei, G. Delayed diagnosis and surgical treatment of bronchial foreign body in children. J. Pediatr. Surg. 2020, 55, 1860–1865. [Google Scholar] [CrossRef] [PubMed]
- Orji, F.T.; Akpeh, J.O. Tracheobronchial foreign body aspiration in children: How reliable are clinical and radiological signs in the diagnosis? Clin. Otolaryngol. 2010, 35, 479–485. [Google Scholar] [CrossRef]
- Casalini, A.G.; Majori, M.; Anghinolfi, M.; Burlone, E.; D’Ippolito, R.; Toschi, M.; Pisi, G.; Barantani, D.; Ghasempour, D.; Monica, M. Foreign body aspiration in adults and in children: Advantages and consequences of a dedicated protocol in our 30-year experience. J. Bronchol. Interv. Pulmonol. 2013, 20, 313–321. [Google Scholar] [CrossRef]
- Foltran, F.; Ballali, S.; Passali, F.M.; Kern, E.; Morra, B.; Passali, G.C.; Berchialla, P.; Lauriello, M.; Gregori, D. Foreign bodies in the airways: A meta-analysis of published papers. Int. J. Pediatr. Otorhinolaryngol. 2012, 76 (Suppl. S1), S12–S19. [Google Scholar] [CrossRef]
- Ciftci, A.O.; Bingol-Kologlu, M.; Senocak, M.E.; Tanyel, F.C.; Buyukpamukcu, N. Bronchoscopy for evaluation of foreign body aspiration in children. J. Pediatr. Surg. 2003, 38, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Heyer, C.M.; Bollmeier, M.E.; Rossler, L.; Nuesslein, T.G.; Stephan, V.; Bauer, T.T.; Rieger, C.H.L. Evaluation of clinical, radiologic, and laboratory prebronchoscopy findings in children with suspected foreign body aspiration. J. Pediatr. Surg. 2006, 41, 1882–1888. [Google Scholar] [CrossRef] [PubMed]
- Mu, L.C.; Sun, D.Q.; He, P. Radiological diagnosis of aspirated foreign bodies in children: Review of 343 cases. J. Laryngol. Otol. 1990, 104, 778–782. [Google Scholar] [CrossRef] [PubMed]
- Tokar, B.; Ozkan, R.; Ilhan, H. Tracheobronchial foreign bodies in children: Importance of accurate history and plain chest radiography in delayed presentation. Clin. Radiol. 2004, 59, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Hitter, A.; Hullo, E.; Durand, C.; Righini, C.A. Diagnostic value of various investigations in children with suspected foreign body aspiration: Review. Eur. Ann. Otorhinolaryngol. Head. Neck Dis. 2011, 128, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Mortellaro, V.E.; Iqbal, C.; Fu, R.; Curtis, H.; Fike, F.B.; St Peter, S.D. Predictors of radiolucent foreign body aspiration. J. Pediatr. Surg. 2013, 48, 1867–1870. [Google Scholar] [CrossRef] [PubMed]
- Sahin, A.; Meteroglu, F.; Eren, S.; Celik, Y. Inhalation of foreign bodies in children: Experience of 22 years. J. Trauma. Acute Care Surg. 2013, 74, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Avraham, S.; Aviram, M.; Farkash Novik, E.; Hoch, S.E.; Pozailov, S.; Levin, M.; Raviv, I.; Goldbart, A.; Dizitzer, Y.; Golan-Tripto, I. Comparison of chest X-ray interpretation by pediatric pulmonologists, pediatric radiologists, and pediatric residents in children with suspected foreign body aspiration-a retrospective cohort study. Eur. J. Pediatr. 2023, 182, 3101–3109. [Google Scholar] [CrossRef]
- Lee, E.Y.; Greenberg, S.B.; Boiselle, P.M. Multidetector computed tomography of pediatric large airway diseases: State-of-the-art. Radiol. Clin. N. Am. 2011, 49, 869–893. [Google Scholar] [CrossRef]
- Yang, C.; Hua, R.; Xu, K.; Hua, X.; Ma, P.; Zheng, J.N.; Li, S.D.; Li, J.S.; Rong, Y.T.; Hu, C.F. The role of 3D computed tomography (CT) imaging in the diagnosis of foreign body aspiration in children. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 265–273. [Google Scholar]
- El Khoury, P.; Makhoul, M.; El Hadi, C.; Haber, C.; Rassi, S. CT Scan in Children Suspected of Foreign Body Aspiration: A Systematic Review and Meta-analysis. Otolaryngol. Head Neck Surg. 2024, 170, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Martinot, A.; Closset, M.; Marquette, C.H.; Hue, V.; Deschildre, A.; Ramon, P.; Remy, J.; Leclerc, F. Indications for flexible versus rigid bronchoscopy in children with suspected foreign-body aspiration. Am. J. Respir. Crit. Care Med. 1997, 155, 1676–1679. [Google Scholar] [CrossRef] [PubMed]
- Divisi, D.; Di Tommaso, S.; Garramone, M.; Di Francescantonio, W.; Crisci, R.M.; Costa, A.M.; Gravina, G.L.; Crisci, R. Foreign bodies aspirated in children: Role of bronchoscopy. Thorac. Cardiovasc. Surg. 2007, 55, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Avital, A.; Godfrey, S.; Gross, M.; Kerem, E.; Springer, C. Suspected foreign body inhalation in children: What are the indications for bronchoscopy? J. Pediatr. 2009, 155, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Korlacki, W.; Korecka, K.; Dzielicki, J. Foreign body aspiration in children: Diagnostic and therapeutic role of bronchoscopy. Pediatr. Surg. Int. 2011, 27, 833–837. [Google Scholar] [CrossRef] [PubMed]
- Faro, A.; Wood, R.E.; Schechter, M.S.; Leong, A.B.; Wittkugel, E.; Abode, K.; Chimel, J.F.; Daines, C.; Davis, S.; Eber, E. Official American Thoracic Society technical standards: Flexible airway endoscopy in children. Am. J. Respir. Crit. Care Med. 2015, 191, 1066–1080. [Google Scholar] [CrossRef] [PubMed]
- Sersar, S.I.; Rizk, W.H.; Bilal, M.; El Diasty, M.M.; Eltantawy, T.A.; Abdelhakam, B.B.; Elgamal, A.L.; Bieh, A.A. Inhaled foreign bodies: Presentation, management and value of history and plain chest radiography in delayed presentation. Otolaryngol. Head Neck Surg. 2006, 134, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Wu, L.; Jin, Z.; Chen, X.; Chen, C.; Liu, J.; Jiang, A.; Fu, Y.; Shu, Q. Residual airway foreign bodies in children who underwent rigid bronchoscopy. Int. J. Pediatr. Otorhinolaryngol. 2019, 118, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Tan, G.X.; Boss, E.F.; Rhee, D.S. Bronchoscopy for Pediatric Airway Foreign Body: Thirty-Day Adverse Outcomes in the ACS NSQIP-P. Otolaryngol. Head Neck Surg. 2019, 160, 326–331. [Google Scholar] [CrossRef]
- Pawar, D.K. Dislodgement of bronchial foreign body during retrieval in children. Paediatr. Anaesth. 2000, 10, 333–335. [Google Scholar] [CrossRef]
- Swanson, K.L.; Prakash, U.B.; Midthun, D.E.; Edell, E.S.; Utz, J.P.; McDougall, J.C.; Brutinel, W.M. Flexible bronchoscopic management of airway foreign bodies in children. Chest 2002, 121, 1695–1700. [Google Scholar] [CrossRef] [PubMed]
- Dikensoy, O.; Usalan, C.; Filiz, A. Foreign body aspiration: Clinical utility of flexible bronchoscopy. Postgrad. Med. J. 2002, 78, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Figueroa, J.L.; Gochicoa-Rangel, L.G.; Ramirez-San Juan, D.H.; Vargas, M.H. Foreign body removal by flexible fiberoptic bronchoscopy in infants and children. Pediatr. Pulmonol. 2005, 40, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Keil, O.; Schwerk, N. Foreign body aspiration in children-being safe and flexible. Curr. Opin. Anaesthesiol. 2023, 36, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chen, Y.; Zhong, C.; Zeng, Y.; Luo, W.; Li, S. The efficacy and safety of airway foreign body removal by balloon catheter via flexible bronchoscope in children—A retrospective analysis. Int. J. Pediatr. Otorhinolaryngol. 2016, 82, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Kendigelen, P. Anesthetic consideration of tracheobronchial foreign body aspiration in children. J. Thorac. Dis. 2016, 8, 3803–3807. [Google Scholar] [CrossRef]
- Saquib Mallick, M.; Rauf Khan, A.; Al-Bassam, A. Late presentation of tracheobronchial foreign body aspiration in children. J. Trop. Pediatr. 2005, 51, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Okonkwo, O.C.; Simons, A.; Nichani, J.; North West ENTRC. Paediatric airway foreign body—The human factors influencing patient safety in our hospitals. Int. J. Pediatr. Otorhinolaryngol. 2016, 91, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.C.; Closson, F.T. Updates in pediatric gastrointestinal foreign bodies. Pediatr. Clin. N. Am. 2013, 60, 1221–1239. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.P.; Hawes, D.; Taylor, T.M. Foreign body ingestion in children: Case series, review of the literature and guidelines on minimising accidental ingestions. J. Fam. Health Care 2010, 20, 200–204. [Google Scholar]
- McKinney, O.W.; Heaton, P.A.; Gamble, J.; Paul, S.P. Recognition and management of foreign body ingestion and aspiration. Nurs. Stand. 2017, 31, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Yalcin, S.; Karnak, I.; Ciftci, A.O.; Senocak, M.E.; Tanyel, F.C.; Buyukpamukcu, N. Foreign body ingestion in children: An analysis of pediatric surgical practice. Pediatr. Surg. Int. 2007, 23, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Tokar, B.; Cevik, A.A.; Ilhan, H. Ingested gastrointestinal foreign bodies: Predisposing factors for complications in children having surgical or endoscopic removal. Pediatr. Surg. Int. 2007, 23, 135–139. [Google Scholar] [CrossRef]
- Arana, A.; Hauser, B.; Hachimi-Idrissi, S.; Vandenplas, Y. Management of ingested foreign bodies in childhood and review of the literature. Eur. J. Pediatr. 2001, 160, 468–472. [Google Scholar] [CrossRef]
- Louie, J.P.; Alpern, E.R.; Windreich, R.M. Witnessed and unwitnessed esophageal foreign bodies in children. Pediatr. Emerg. Care 2005, 21, 582–585. [Google Scholar] [CrossRef] [PubMed]
- Sink, J.R.; Kitsko, D.J.; Mehta, D.K.; Georg, M.W.; Simons, J.P. Diagnosis of Pediatric Foreign Body Ingestion: Clinical Presentation, Physical Examination, and Radiologic Findings. Ann. Otol. Rhinol. Laryngol. 2016, 125, 342–350. [Google Scholar] [CrossRef]
- Little, D.C.; Shah, S.R.; St Peter, S.D.; Calkins, C.M.; Morrow, S.E.; Murphy, J.P.; Sharp, R.J.; Andrews, W.S.; Holcomb, G.W., III; Ostlie, D.J. Esophageal foreign bodies in the pediatric population: Our first 500 cases. J. Pediatr. Surg. 2006, 41, 914–918. [Google Scholar] [CrossRef]
- Denney, W.; Ahmad, N.; Dillard, B.; Nowicki, M.J. Children will eat the strangest things: A 10-year retrospective analysis of foreign body and caustic ingestions from a single academic center. Pediatr. Emerg. Care 2012, 28, 731–734. [Google Scholar] [CrossRef]
- Popel, J.; El-Hakim, H.; El-Matary, W. Esophageal foreign body extraction in children: Flexible versus rigid endoscopy. Surg. Endosc. 2011, 25, 919–922. [Google Scholar] [CrossRef] [PubMed]
- Russell, R.; Lucas, A.; Johnson, J.; Yannam, G.; Griffin, R.; Beierle, E.; Anderson, S.; Chen, M.; Harmon, C. Extraction of esophageal foreign bodies in children: Rigid versus flexible endoscopy. Pediatr. Surg. Int. 2014, 30, 417–422. [Google Scholar] [CrossRef]
- DeRowe, A.; Massick, D.; Beste, D.J. Clinical characteristics of aero-digestive foreign bodies in neurologically impaired children. Int. J. Pediatr. Otorhinolaryngol. 2002, 62, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Berdan, E.A.; Sato, T.T. Pediatric Airway and Esophageal Foreign Bodies. Surg. Clin. N. Am. 2017, 97, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Luk, W.H.; Fan, W.C.; Chan, R.Y.; Chan, S.W.; Tse, K.H.; Chan, J.C. Foreign body ingestion: Comparison of diagnostic accuracy of computed tomography versus endoscopy. J. Laryngol. Otol. 2009, 123, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Gregori, D.; Scarinzi, C.; Morra, B.; Salerni, L.; Berchialla, P.; Snidero, S.; Corradetti, R.; Pasali, D.; Group, E.S. Ingested foreign bodies causing complications and requiring hospitalization in European children: Results from the ESFBI study. Pediatr. Int. 2010, 52, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Telford, J.J. Management of ingested foreign bodies. Can. J. Gastroenterol. 2005, 19, 599–601. [Google Scholar] [CrossRef]
- Loh, K.S.; Tan, L.K.; Smith, J.D.; Yeoh, K.H.; Dong, F. Complications of foreign bodies in the esophagus. Otolaryngol. Head Neck Surg. 2000, 123, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Gurevich, Y.; Sahn, B.; Weinstein, T. Foreign body ingestion in pediatric patients. Curr. Opin. Pediatr. 2018, 30, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Birk, M.; Bauerfeind, P.; Deprez, P.H.; Hafner, M.; Hartmann, D.; Hassan, C.; Hucl, T.; Lesur, G.; Aabakken, L.; Meining, A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.C.; Hsiao, T.Y.; Hsu, W.C. Comparison of rigid and flexible endoscopy for removing esophageal foreign bodies in an emergency. J. Formos. Med. Assoc. 2016, 115, 639–644. [Google Scholar] [CrossRef][Green Version]
- Jayachandra, S.; Eslick, G.D. A systematic review of paediatric foreign body ingestion: Presentation, complications, and management. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 311–317. [Google Scholar] [CrossRef]
- Litovitz, T.; Whitaker, N.; Clark, L.; White, N.C.; Marsolek, M. Emerging battery-ingestion hazard: Clinical implications. Pediatrics 2010, 125, 1168–1177. [Google Scholar] [CrossRef] [PubMed]
- Buttazzoni, E.; Gregori, D.; Paoli, B.; Soriani, N.; Baldas, S.; Rodriguez, H.; Lorenzoni, G.; Susy Safe Working, G. Symptoms associated with button batteries injuries in children: An epidemiological review. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 2200–2207. [Google Scholar] [CrossRef] [PubMed]
- Litovitz, T.; Whitaker, N.; Clark, L. Preventing battery ingestions: An analysis of 8648 cases. Pediatrics 2010, 125, 1178–1183. [Google Scholar] [CrossRef] [PubMed]
- Pugmire, B.S.; Lin, T.K.; Pentiuk, S.; de Alarcon, A.; Hart, C.K.; Trout, A.T. Imaging button battery ingestions and insertions in children: A 15-year single-center review. Pediatr. Radiol. 2017, 47, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.P.; Paul, R. Magnets and Button Batteries: Two Dangerous Foreign Body Ingestions. J. Coll. Physicians Surg. Pak. 2017, 27, 119–120. [Google Scholar] [PubMed]
- Lee, J.H.; Lee, J.H.; Shim, J.O.; Lee, J.H.; Eun, B.L.; Yoo, K.H. Foreign Body Ingestion in Children: Should Button Batteries in the Stomach Be Urgently Removed? Pediatr. Gastroenterol. Hepatol. Nutr. 2016, 19, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, J.M.; Burrows, S.A.; Saunders, M.W. Lodged oesophageal button battery masquerading as a coin: An unusual cause of bilateral vocal cord paralysis. Emerg. Med. J. 2007, 24, e15. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, Y.M.; Muensterer, O.; Wendling-Keim, D. The use of honey in button battery ingestions: A systematic review. Front. Pediatr. 2023, 11, 1259780. [Google Scholar] [CrossRef] [PubMed]
- Mubarak, A.; Benninga, M.A.; Broekaert, I.; Dolinsek, J.; Homan, M.; Mas, E.; Miele, E.; Pienar, C.; Thapar, N.; Thomson, M.; et al. Diagnosis, Management, and Prevention of Button Battery Ingestion in Childhood: A European Society for Paediatric Gastroenterology Hepatology and Nutrition Position Paper. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 129–136. [Google Scholar] [CrossRef]
- Gyawali, B.R.; Guragain, R.; Gyawali, D.R. Role of Honey and Acetic Acid in Mitigating the Effects of Button Battery in Esophageal Mucosa: A Cadaveric Animal Model Experimental Study. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 5759–5765. [Google Scholar] [CrossRef]
- Sethia, R.; Gibbs, H.; Jacobs, I.N.; Reilly, J.S.; Rhoades, K.; Jatana, K.R. Current management of button battery injuries. Laryngoscope Investig. Otolaryngol. 2021, 6, 549–563. [Google Scholar] [CrossRef] [PubMed]
- Jatana, K.R.; Barron, C.L.; Jacobs, I.N. Initial clinical application of tissue pH neutralization after esophageal button battery removal in children. Laryngoscope 2019, 129, 1772–1776. [Google Scholar] [CrossRef] [PubMed]
- Kramer, R.E.; Lerner, D.G.; Lin, T.; Manfredi, M.; Shah, M.; Stephen, T.C.; Gibbons, T.E.; Pali, H.; Sahn, B.; McOmber, M.; et al. Management of ingested foreign bodies in children: A clinical report of the NASPGHAN Endoscopy Committee. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 562–574. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, A.; Hansen, N.F.; Schiodt, O.M. Fatal aortoesophageal fistula caused by button battery ingestion in a 1-year-old child. Am. J. Emerg. Med. 2010, 28, 984.e5–984.e6. [Google Scholar] [CrossRef] [PubMed]
- Virgilis, D.; Weinberger, J.M.; Fisher, D.; Goldberg, S.; Picard, E.; Kerem, E. Vocal cord paralysis secondary to impacted esophageal foreign bodies in young children. Pediatrics 2001, 107, E101. [Google Scholar] [CrossRef]
- Soerdjbalie-Maikoe, V.; van Rijn, R.R. A case of fatal coin battery ingestion in a 2-year-old child. Forensic Sci. Int. 2010, 198, e19–e22. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paladin, I.; Mizdrak, I.; Gabelica, M.; Golec Parčina, N.; Mimica, I.; Batinović, F. Foreign Bodies in Pediatric Otorhinolaryngology: A Review. Pediatr. Rep. 2024, 16, 504-518. https://doi.org/10.3390/pediatric16020042
Paladin I, Mizdrak I, Gabelica M, Golec Parčina N, Mimica I, Batinović F. Foreign Bodies in Pediatric Otorhinolaryngology: A Review. Pediatric Reports. 2024; 16(2):504-518. https://doi.org/10.3390/pediatric16020042
Chicago/Turabian StylePaladin, Ivan, Ivan Mizdrak, Mirko Gabelica, Nikolina Golec Parčina, Ivan Mimica, and Franko Batinović. 2024. "Foreign Bodies in Pediatric Otorhinolaryngology: A Review" Pediatric Reports 16, no. 2: 504-518. https://doi.org/10.3390/pediatric16020042
APA StylePaladin, I., Mizdrak, I., Gabelica, M., Golec Parčina, N., Mimica, I., & Batinović, F. (2024). Foreign Bodies in Pediatric Otorhinolaryngology: A Review. Pediatric Reports, 16(2), 504-518. https://doi.org/10.3390/pediatric16020042






