Understanding the Neuropsychological Implications of Klinefelter Syndrome in Pediatric Populations: Current Perspectives
Abstract
1. Introduction
2. Neuropsychological Profile
2.1. Executive Dysfunction
2.2. Language Impairments
3. Clinical Challenges
3.1. Psychiatric Disorders
3.2. Social Impairments
3.3. Further Challenges
4. Discussion
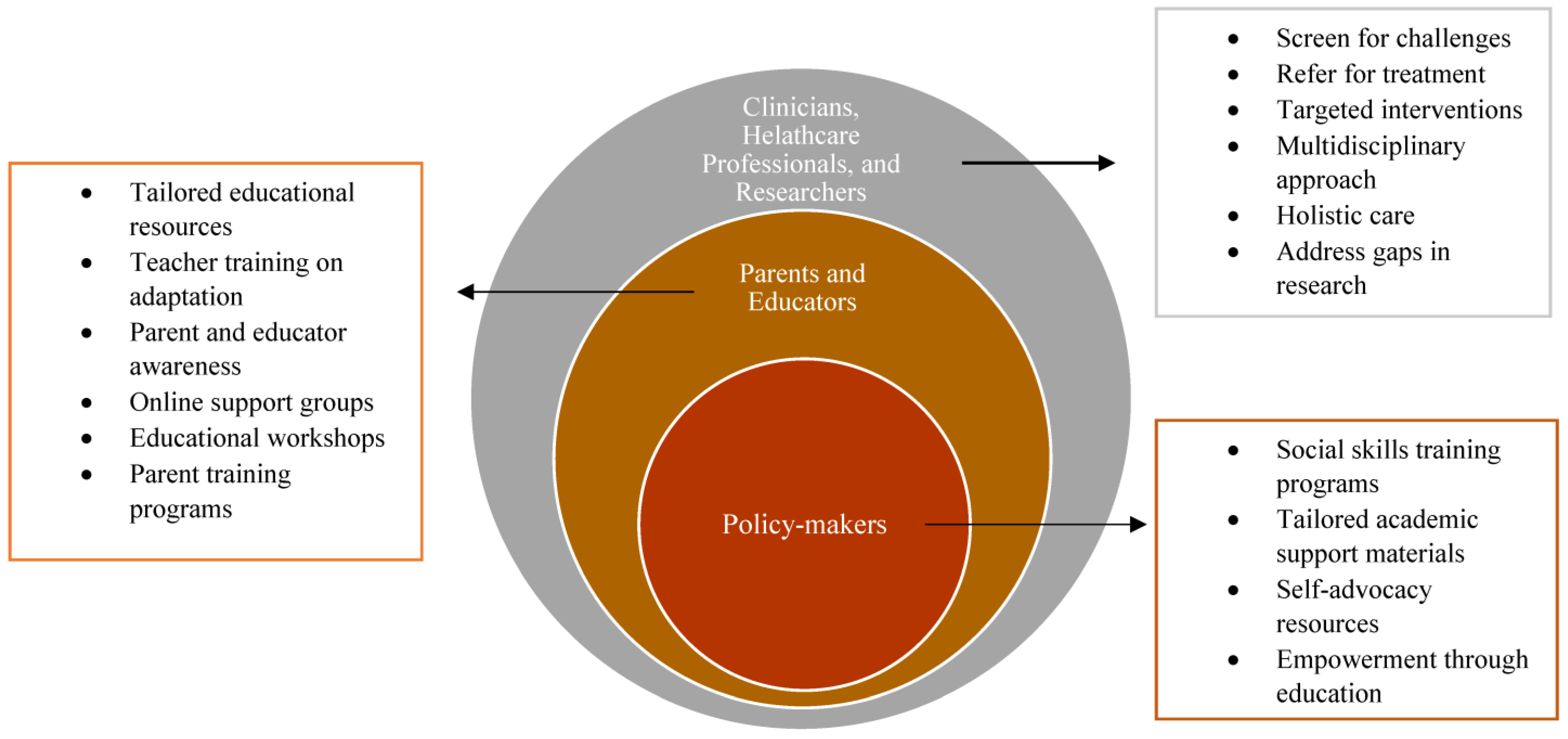
4.1. Clinicians, Healthcare Professionals, and Researchers
4.2. Educators and Parents
4.3. Policymakers
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Butler, G.; Srirangalingam, U.; Faithfull, J.; Sangster, P.; Senniappan, S.; Mitchell, R. Klinefelter syndrome: Going beyond the diagnosis. Arch. Dis. Child. 2023, 108, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Klinefelter, H.; Reifenstein, E.; Albright, F. Syndrome characterized by gynecomastia, aspermatogenesis without a-Leydigism and increased secretion of follicle-stimulating hormone. J. Clin. Endocrinol. 1942, 2, 615–627. [Google Scholar] [CrossRef]
- Barr, M.; Bertram, E. A morphological distinction between neurons of the male and female, and the behavior of the nucleolar satellite during accelerated nucleoprotein synthesis. Nature 1949, 163, 676. [Google Scholar] [CrossRef] [PubMed]
- Marberger, E.; Boccabella, R.; Nelson, W. Oral smear as a method of chromosomal sex detection. Proc. Soc. Exp. Biol. Med. 1955, 89, 488–489. [Google Scholar] [CrossRef] [PubMed]
- Klinger, H.; Ludwig, K. A universal stain for the sex chromatin body. Stain Technol. 1957, 32, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Barr, M.; Plunkett, E. Testicular dysgenesis affecting the seminiferous tubules principally, with chromatin-positive nuclei. Lancet 1956, 271, 853–856. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, J.; Bunge, R.; Boccabella, R. Chromatin test in Klinefelter’s syndrome. J. Clin. Endocrinol. Metab. 1956, 16, 689. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, P.; Strong, J. A case of human intersexuality having a possible XXY sex-determining mechanism. Nature 1959, 183, 302–303. [Google Scholar] [CrossRef] [PubMed]
- King, R.A.; Potter, J.; Motulsky, A. The Genetic Basis of Common Disease, 1st ed.; Oxford University Press: Oxford, UK, 1992. [Google Scholar]
- Paulsen, C.; Gordon, D.; Carpenter, R.; Gandy, H.; Drucker, W. Klinefelter’s syndrome and its variants: A hormonal and chromosomal study. Recent Prog. Horm. Res. 1968, 24, 321–363. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. Executive Functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef] [PubMed]
- Bender, B.G.; Linden, M.G.; Robinson, A. Neuropsychological impairment in 42 adolescents with sex chromosome abnormalities. Am. J. Med. Genet. Part A 1993, 48, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.L.; Roeltgen, D.P.; Stefanatos, G.; Benecke, R.; Zeger, M.P.; Kushner, H.; Ramos, P.; Elder, F.F.; Zinn, A.R. Cognitive and Motor Development During Childhood in Boys with Klinefelter Syndrome. Am. J. Med. Genet. Part A 2008, 146A, 708–719. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.; Zeger, M.; Kushner, H.; Zinn, A.; Roeltgen, D. An extra X or Y chromosome: Contrasting the cognitive and motor phenotypes in childhood in boys with 47, XYY syndrome or 47, XXY Klinefelter syndrome. Dev. Disabil. Res. Rev. 2009, 15, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Temple, C.M.; Sanfilippo, P.M. Executive skills in Klinefelter’s syndrome. Neuropsychologia 2003, 41, 1547–1559. [Google Scholar] [CrossRef] [PubMed]
- Samango-Sprouse, C.; Stapleton, E.; Chea, S.; Lawson, P.; Sadeghin, T.; Cappello, C.; de Sonneville, L.; van Rijn, S. International investigation of neurocognitive and behavioral phenotype in 47,XXY (Klinefelter syndrome): Predicting individual differences. Am. J. Med. Genet. Part A 2018, 176, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.R.; Wallace, G.L.; Clasen, L.S.; Lenroot, R.K.; Blumenthal, J.D.; White, S.L.; Celano, M.J.; Giedd, J.N. Executive Function in Young Males with Klinefelter (XXY) Syndrome with and without Comorbid Attention-Deficit/Hyperactivity Disorder. J. Int. Neuropsychol. Soc. 2011, 17, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Tran, S.L.; Samango-Sprouse, C.A.; Sadeghin, T.; Powell, S.; Gropman, A.L. Hormonal replacement therapy and its potential influence on working memory and competency/adaptive functioning in 47,XXY (Klinefelter syndrome). Am. J. Med. Genet. Part A 2019, 179, 2374–2381. [Google Scholar] [CrossRef] [PubMed]
- Janusz, J.; Harrison, C.; Boada, C.; Cordeiro, L.; Howell, S.; Tartaglia, N.; Boada, R. Executive function in XXY: Comparison of performance-based measures and rating scales. Am. J. Med. Genet. Part C Semin. Med. Genet. 2020, 184, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Krieger, V.; Amador-Campos, J.A. Assessment of executive function in ADHD adolescents: Contribution of performance tests and rating scales. Child Neuropsychol. 2018, 24, 1063–1087. [Google Scholar] [CrossRef]
- Green, T.; Flash, S.; Shankar, G.; Bade Shrestha, S.; Jo, B.; Klabunde, M.; Hong, D.S.; Reiss, A.L. Effect of sex chromosome number variation on attention-deficit/hyperactivity disorder symptoms, executive function, and processing speed. Dev. Med. Child Neurol. 2022, 64, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Boada, R.; Janusz, J.; Hutaff-Lee, C.; Tartaglia, N. The cognitive phenotype in Klinefelter syndrome: A review of the literature including genetic and hormonal factors. Dev. Disabil. Res. Rev. 2009, 15, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Jahromi, L.B.; Stifter, C.A. Individual Differences in Preschoolers’ Self-Regulation and Theory of Mind. Merrill-Palmer Q. 2008, 54, 125–150. [Google Scholar] [CrossRef]
- Foland-Ross, L.C.; Ghasemi, E.; Lozano Wun, V.; Aye, T.; Kowal, K.; Ross, J.; Reiss, A.L. Executive Dysfunction in Klinefelter Syndrome: Associations with Brain Activation and Testicular Failure. J. Clin. Endocrinol. Metab. 2023, 109, e88–e95. [Google Scholar] [CrossRef] [PubMed]
- Samango-Sprouse, C.A. The mental development in polysomy X Klinefelter syndrome (47,XXY; 48,XXXY): Effects of incomplete X-activation. Semin. Reprod. Med. 2001, 19, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Samango-Sprouse, C.; Law, P. The neurocognitive profile of children with sex chromosome anomalies. In Proceedings of the International Conference of Human Genetics, Vienna, Austria, 15–19 May 2001. [Google Scholar]
- Leonard, M.; Schowalter, J.E.; Landy, G.; Ruddle, F.; Lubs, H. Chromosomal abnormalities in the New Haven newborn study: A prospective study of development of children with sex chromosome anomalies. Birth Defects Orig. Artic. Ser. 1979, 15, 115–160. [Google Scholar]
- Robinson, A.; Lubs, H.A.; Nielsen, J.; Sorensen, K. Early communicative skills of children with Klinefelter syndrome. Birth Defects Orig. Artic. Ser. 1979, 15, 261–266. [Google Scholar] [PubMed]
- Zampini, L.; Burla, T.; Silibello, G.; Dall’Ara, F.; Rigamonti, C.; Lalatta, F.; Vizziello, P. Vocal and gestural productions of 24-month-old children with sex chromosome trisomies. Clin. Linguist. Phon. 2018, 32, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Netley, C.; Rovet, J. Verbal deficits in children with 47, XXY and 47, XXX karyotypes: A descriptive and experimental study. Brain Lang. 1982, 17, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Graham, J.M.J.; Bashir, A.S.; Stark, R.E.; Silbert, A.; Walzer, S. Oral and Written Language Abilities of XXY Boys: Implications for Anticipatory Guidance. Pediatrics 1988, 81, 795–806. [Google Scholar] [CrossRef] [PubMed]
- Melogno, S.; Pinto, M.A.; Orsolini, M.; Tarani, L. Beyond the Literal Meaning of Words in Children with Klinefelter Syndrome: Two Case Studies. Brain Sci. 2018, 8, 171. [Google Scholar] [CrossRef] [PubMed]
- Aksglæde, L.; Skakkebæk, N.E.; Almstrup, K.; Juul, A. Clinical and biological parameters in 166 boys, adolescents and adults with nonmosaic Klinefelter syndrome: A Copenhagen experience. Acta Paediatr. 2011, 100, 793–806. [Google Scholar] [CrossRef] [PubMed]
- Bender, B.G.; Puck, M.H.; Salenblatt, J.A.; Robinson, A. Dyslexia in 47, XXY boys identified at birth. Behav. Genet. 1986, 16, 343–354. [Google Scholar] [CrossRef] [PubMed]
- St John, M.; Ponchard, C.; van Reyk, O.; Mei, C.; Pigdon, L.; Amor, D.J.; Morgan, A.T. Speech and language in children with Klinefelter syndrome. J. Commun. Disord. 2019, 78, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Geschwind, D.; Boone, K.; Miller, B.; Swerdloff, R.S. Neurobehavioral phenotype of Klinefelter syndrome. Ment. Retard. Dev. Disabil. Res. Rev. 2000, 6, 107–116. [Google Scholar] [PubMed]
- Bishop, D.V.; Scerif, G. Klinefelter syndrome as a window on the aetiology of language and communication impairments in children: The neuroligin-neurexin hypothesis. Acta Paediatr. 2011, 100, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Lamonica, D.A.C.; Ribeiro, C.d.C.; Baldin, M.d.S.; Tabaquim, M.d.L.M. Klinefelter syndrome: A speech-language and neuropsychological assessment. Rev. CEFAC 2018, 20, 665–671. [Google Scholar] [CrossRef]
- Mazzocco, M.M.M.; Ross, J.L. Neurogenetic Developmental Disorders: Variation of Manifestation in Childhood, 1st ed.; MIT Press: Cambridge, MA, USA, 2007. [Google Scholar]
- Bender, B.; Harmon, R.; Linden, M.; Robinson, A. Psychosocial adaptation of 39 adolescents with sex chromosome abnormalities. Pediatrics 1995, 96, 302–308. [Google Scholar] [CrossRef] [PubMed]
- DeLisi, L.E.; Friedrich, U.; Wahlstrom, J.; Boccio-Smith, A.; Foreman, A.; Eklund, K.; Crow, T.J. Schizophrenia and Sex Chromosome Anomalies. Schizophr. Bull. 2004, 20, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Bojesen, A.; Juul, S.; Birkebaek, N.; Gravholt, C. Morbidity in Klinefelter syndrome: A Danish Register Study based on hospital discharge diagnoses. J. Clin. Endocrinol. Metab. 2006, 91, 1254–1260. [Google Scholar] [CrossRef] [PubMed]
- Crow, T. Directional asymmetry is the key to the origin of modern Homo sapiens (the Broca-Annett axiom): A reply to Rogers’ review of The Speciation of Modern Homo Sapiens. Laterality 2004, 9, 233–242. [Google Scholar] [CrossRef]
- DeLisi, L.E.; Maurizio, A.M.; Svetina, C.; Ardekani, B.; Szulc, K.; Nierenberg, J.; Leonard, J.; Harvey, P.D. Klinefelter’s syndrome (XXY) as a genetic model for psychotic disorders. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2005, 135B, 15–23. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, S.; Aleman, A.; Swaab, H.; Vink, M.; Sommer, I.; Kahn, R.S. Effects of an extra X chromosome on language lateralization: An fMRI study with Klinefelter men (47,XXY). Schizophr. Res. 2008, 101, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Bruining, H.; Swaab, H.; Kas, M.; van Engeland, H. Psychiatric Characteristics in a Self-Selected Sample of Boys With Klinefelter Syndrome. Pediatrics 2009, 123, e865–e870. [Google Scholar] [CrossRef] [PubMed]
- Ratcliffe, S. Long term outcome in children of sex chromosome abnormalities. Arch. Dis. Child. 1999, 80, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Bender, B.G.; Harmon, R.J.; Linden, M.G.; Bucher-Bartelson, B.; Robinson, A. Psychosocial competence of unselected young adults with sex chromosome abnormalities. Am. J. Med. Genet. 1999, 88, 200–206. [Google Scholar] [CrossRef]
- Boks, M.; de Vette, M.; Sommer, I.; van Rijn, S.; Giltay, J.; Swaab, H.; Kahn, R. Psychiatric morbidity and X-chromosomal origin in Klinefelter sample. Schizophr. Res. 2007, 93, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Turriff, A.; Levy, H.P.; Biesecker, B. Prevalence and psychosocial correlates of depressive symptoms among adolescents and adults with Klinefelter syndrome. Genet. Med. 2011, 13, 966–972. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, S.; de Sonneville, L.; Swaab, H. The nature of social cognitive deficits in children and adults with Klinefelter syndrome (47,XXY). Genes Brain Behav. 2018, 17, e12465. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, L.; Tartaglia, N.; Roeltgen, D.; Ross, J. Social deficits in male children and adolescents with sex chromosome aneuploidy: A comparison of XXY, XYY, and XXYY syndromes. Res. Dev. Disabil. 2012, 33, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- Tartaglia, N.; Cordeiro, L.; Howell, S.; Wilson, R.; Janusz, J. The spectrum of the behavioral phenotype in boys and adolescents 47,XXY (Klinefelter syndrome). Pediatr. Endocrinol. Rev. 2010, 8, 151–159. [Google Scholar]
- van Rijn, S.; Stockmann, L.; Van Buggenhout, G.; van Ravenswaaij-Arts, C.M.A.; Swaab, H. Social cognition and underlying cognitive mechanisms in children with an extra X chromosome: A comparison with autism spectrum disorder: Social cognition and an extra X chromosome. Genes Brain Behav. 2014, 13, 459–467. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, S.; Swaab, H.; Aleman, A.; Kahn, R.S. X Chromosomal effects on social cognitive processing and emotion regulation: A study with Klinefelter men (47,XXY). Schizophr. Res. 2006, 84, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Karampelas, M.; Gardner, J.; Holder, G.; Hardcastle, A.; Webster, A. Retinal dysfunction and high myopia in association with 48,XXYY syndrome. Doc. Ophthalmol. 2013, 127, 245–247. [Google Scholar] [CrossRef] [PubMed]
- Brand, C.; Zitzmann, M.; Eter, N.; Kliesch, S.; Wistuba, J.; Alnawaiseh, M.; Heiduschka, P. Aberrant ocular architecture and function in patients with Klinefelter syndrome. Sci. Rep. 2017, 7, 13130–13138. [Google Scholar] [CrossRef] [PubMed]
- Giambersio, E.; Barile, V.; Giambersio, A.M. Klinefelter’s syndrome and taurodontism. Arch. Ital. Di Urol. Androl. 2019, 91, 130–132. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.M.; DeKlotz, S.; Nadeau, K.J.; Kelsey, M.M.; Zeitler, P.S.; Tartaglia, N.R. High prevalence of cardiometabolic risk features in adolescents with 47,XXY/Klinefelter syndrome. American journal of medical genetics. Part C Semin. Med. Genet. 2020, 184, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, M.; Bongers, R.; Werler, S.; Bogdanova, N.; Wistuba, J.; Kliesch, S.; Tuttelmann, F. Gene expression patterns in relation to the clinical phenotype in Klinefelter syndrome. J. Clin. Endocrinol. Metab. 2015, 100, E518–E523. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, I.N.; Skakkebaek, A.; Andersen, N.H.; Pedersen, L.N.; Hougaard, D.M.; Bojesen, A.; Trolle, C.; Gravholt, C.H. Short QTc interval in males with Klinefelter syndrome-influence of CAG repeat length, body composition, and testosterone replacement therapy. Pacing Clin. Electrophysiol. 2014, 38, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Turriff, A.; Macnamara, E.; Levy, H.P.; Biesecker, B. The impact of living with Klinefelter syndrome: A qualitative exploration of adolescents and adults. J. Genet. Couns. 2017, 26, 728–737. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, S. Salivary testosterone in relation to social cognition and social anxiety in children and adolescents with 47,XXY (Klinefelter syndrome). PLoS ONE 2018, 13, e0200882. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.L.; Kushner, H.; Kowal, K.; Bardsley, M.; Davis, S.; Reiss, A.L.; Tartaglia, N.; Roeltgen, D. Androgen treatment effects on motor function, cognition, and behavior in boys with Klinefelter syndrome. J. Pediatr. 2017, 185, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, L.; Gagliardi, I.; Bigoni, S.; Lupo, S.; Caracciolo, S.; Ferlini, A.; Isidori, A.M.; Zatelli, M.C.; Ambrosio, M.R. Communicating the diagnosis of Klinefelter syndrome to children and adolescents: When, how, and who? J. Community Genet. 2022, 13, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Farley, J.; Huscroft-D’Angelo, J.; Hurly, K.; Aitken, A.; Trout, A. Teacher perspectives on information sharing and parent knowledge of special education. J.-Risk 2022, 24, 1–12. [Google Scholar]
- Bester, N.; Di Vito-Smith, M.; McGarry, T.; Riffkin, M.; Kaehler, S.; Pilot, R.; Bwire, R. The effectiveness of an educational brochure as a risk minimization activity to communicate important rare adverse events to health-care professionals. Adv. Ther. 2016, 33, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Martin, F.; van Rijn, S.; Bierman, M.; Swaab, H. Social management training in males with 47,XXY (Klinefelter syndrome): A pilot study of a neurocognitive-behavioral treatment targeting social, emotional, and behavioral problems. Am. J. Intellect. Dev. Disabil. 2021, 126, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Martin, F.; Swaab, H.; Bierman, M.; van Rijn, S. Effectiveness of social management training on executive functions in males with Klinefelter syndrome (47,XXY). Appl. Neuropsychol. Adult 2023, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Physical, Reproductive, and Endocrine Symptoms | Lannguage Deficits | Executive Dysfunction | Social Impairments |
|---|---|---|---|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tragantzopoulou, P.; Giannouli, V. Understanding the Neuropsychological Implications of Klinefelter Syndrome in Pediatric Populations: Current Perspectives. Pediatr. Rep. 2024, 16, 420-431. https://doi.org/10.3390/pediatric16020036
Tragantzopoulou P, Giannouli V. Understanding the Neuropsychological Implications of Klinefelter Syndrome in Pediatric Populations: Current Perspectives. Pediatric Reports. 2024; 16(2):420-431. https://doi.org/10.3390/pediatric16020036
Chicago/Turabian StyleTragantzopoulou, Panagiota, and Vaitsa Giannouli. 2024. "Understanding the Neuropsychological Implications of Klinefelter Syndrome in Pediatric Populations: Current Perspectives" Pediatric Reports 16, no. 2: 420-431. https://doi.org/10.3390/pediatric16020036
APA StyleTragantzopoulou, P., & Giannouli, V. (2024). Understanding the Neuropsychological Implications of Klinefelter Syndrome in Pediatric Populations: Current Perspectives. Pediatric Reports, 16(2), 420-431. https://doi.org/10.3390/pediatric16020036







