The Ongoing Impact of COVID-19 on Pediatric Obesity
Abstract
1. Introduction
2. COVID-19
3. Pediatric Obesity and Related Diseases
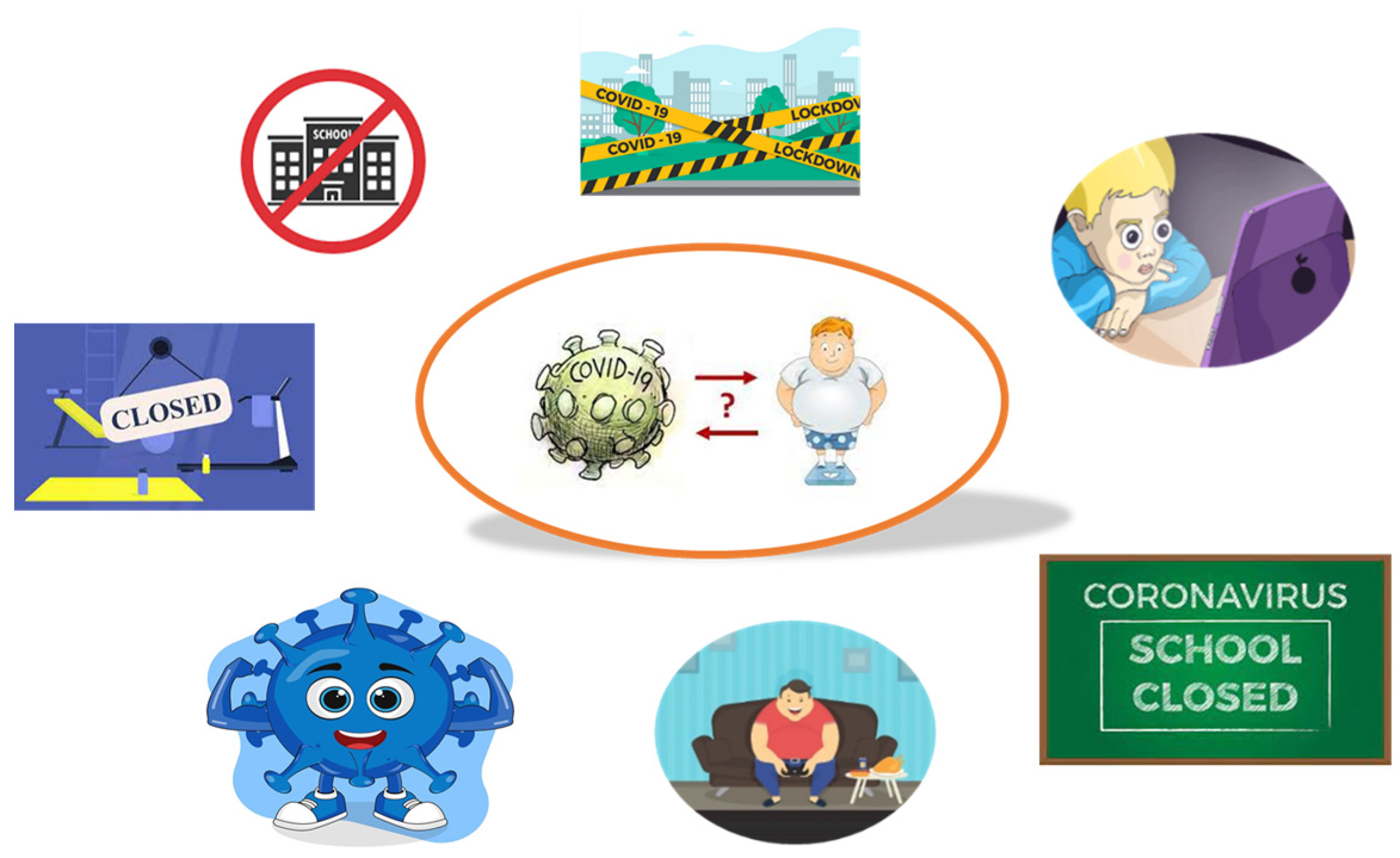
4. Pediatric Obesity in the COVID-19 Era
5. Management of Pediatric Obesity and Strategies for Pediatric Obesity Treatment during the COVID-19 Pandemic
6. Changes in the Prevalence of Pediatric Obesity after COVID-19 Pandemic
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thomas-Eapen, N. Childhood Obesity. Prim. Care 2021, 48, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Bomberg, E.M.; Kyle, T.; Stanford, F.C. Considering pediatric obesity as a US public health emergency. Pediatrics 2023, 152, e2023061501. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Xue, Y. Pediatric obesity: Causes, symptoms, prevention and treatment. Exp. Ther. Med. 2016, 11, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.Y. Association of gut microbiota with obesity in children and adolescents. Clin. Exp. Pediatr. 2022, 66, 148–154. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Childhood Overweight and Obesity. Available online: https://www.who.int/news-room/questions-and-answers/item/noncommunicable-diseases-childhood-overweight-and-obesity (accessed on 18 January 2023).
- Berrigan, D.; Arteaga, S.S.; Colón-Ramos, U.; Rosas, L.G.; Monge-Rojas, R.; O’Connor, T.M.; Pérez-Escamilla, R.; Roberts, E.F.S.; Sanchez, B.; Téllez-Rojo, M.M.; et al. Measurement challenges for childhood obesity research within and between Latin America and the United States. Obes. Rev. 2021, 22, e13242. [Google Scholar] [CrossRef] [PubMed]
- Verduci, E.; Bronsky, J.; Embleton, N.; Gerasimidis, K.; Indrio, F.; Köglmeier, J.; de Koning, B.; Lapillonne, A.; Moltu, S.J.; Norsa, L.; et al. Role of dietary factors, food habits, and lifestyle in childhood obesity development: A Position paper from the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on nutrition. J. Pediatr. Gastroenterol. Nutr. 2021, 72, 769–783. [Google Scholar] [CrossRef]
- Mathis, B.J.; Tanaka, K.; Hiramatsu, Y. Factors of Obesity and Metabolically Healthy Obesity in Asia. Medicina 2022, 58, 1271. [Google Scholar] [CrossRef]
- Liberali, R.; Del Castanhel, F.; Kupek, E.; de Assis, M.A.A. de Latent Class Analysis of Lifestyle Risk Factors and Association with Overweight and/or Obesity in Children and Adolescents: Systematic Review. Child. Obes. 2021, 17, 2–15. [Google Scholar] [CrossRef]
- Hunter, K.E.; Johnson, B.J.; Askie, L.; Golley, R.K.; Baur, L.A.; Marschner, I.C.; Taylor, R.W.; Wolfenden, L.; Wood, C.T.; Mihrshahi, S.; et al. Transforming obesity prevention for children (TOPCHILD) collaboration: Protocol for a systematic review with individual participant data meta-analysis of behavioural interventions for the prevention of early childhood obesity. BMJ Open 2022, 12, e048166. [Google Scholar] [CrossRef]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L. Pediatric Obesity-Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- Littlejohn, E. Pediatric Obesity—A Looming Problem for the Pediatric Population. Pediatr. Ann. 2023, 52, e46–e47. [Google Scholar] [CrossRef]
- CDC. Prevalence of Childhood Obesity in the United States. 2021. Available online: https://www.cdc.gov/obesity/data/childhood.html (accessed on 16 January 2024).
- Spinelli, A.; Buoncristiano, M.; Kovacs, V.A.; Yngve, A.; Spiroski, I.; Obreja, G.; Starc, G.; Pérez, N.; Rito, A.; Kunešová, M.; et al. Prevalence of Severe Obesity among Primary School Children in 21 European Countries. Obes. Facts 2019, 12, 244–258. [Google Scholar] [CrossRef]
- Romanelli, R.; Cecchi, N.; Carbone, M.G.; Dinardo, M.; Gaudino, G.; del Giudice, E.M.; Umano, G.R. Pediatric obesity: Prevention is better than care. Ital. J. Pediatr. 2020, 46, 103. [Google Scholar] [CrossRef]
- Appelhans, B.M.; French, S.A.; Martin, M.A.; Lui, K.; Janssen, I. Attenuated efficacy of pediatric obesity treatment during the COVID-19 pandemic. Obesity 2022, 30, 45–49. [Google Scholar] [CrossRef]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in children and adolescents: Epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef] [PubMed]
- Russell, C.D.; Lone, N.I.; Baillie, J.K. Comorbidities, multimorbidity and COVID-19. Nat. Med. 2023, 29, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Delgado, A.M.; Collins, P.Z.; MacArthur, R.D. Consequences of COVID-19 on pediatric obesity and endocrinopathies: A review of the literature. Med. Res. Arch. 2023, 11, 1–13. [Google Scholar] [CrossRef]
- Al-Agailat, L.; Littlejohn, E. Emerging Pediatric Obesity Epidemic with the COVID-19 Pandemic as an Influence. Pediatr. Ann. 2023, 52, e48–e50. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.N.; Yoshida-Montezuma, Y.; Dewart, N.; Jalil, E.; Khattar, J.; De Rubeis, V.; Carsley, S.; Griffith, L.E.; Mbuagbaw, L. Obesity and weight change during the COVID-19 pandemic in children and adults: A systematic review and meta-analysis. Obes. Rev. 2023, 24, e13550. [Google Scholar] [CrossRef]
- De Nucci, S.; Zupo, R.; Castellana, F.; Sila, A.; Triggiani, V.; Lisco, G.; De Pergola, G.; Sardone, R. Public health response to the SARS-CoV-2 pandemic: Concern about ultra-processed food consumption. Foods 2022, 11, 950. [Google Scholar] [CrossRef]
- Fabin-Czepiel, K.; Pieczyńska-Chapuła, K.; Deja, G. “The obesity pandemic” in the COVID-19 pandemic–new treatment for an old problem. Pediatr. Endocrinol. Diabetes Metab. 2023, 29, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Browne, N.T.; Snethen, J.A.; Greenberg, C.S.; Frenn, M.; Kilanowski, J.F.; Gance-Cleveland, B.; Burke, P.J.; Lewandowski, L. When Pandemics Collide: The Impact of COVID-19 on Childhood Obesity. J. Pediatr. Nurs. 2021, 56, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Zachariah, P.; Johnson, C.L.; Halabi, K.C.; Ahn, D.; Sen, A.I.; Fischer, A.; Banker, S.L.; Giordano, M.; Manice, C.S.; Diamond, R.; et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children’s hospital in New York city, New York. JAMA Pediatr. 2020, 174, 202430. [Google Scholar] [CrossRef] [PubMed]
- Weihrauch-Blüher, S.; Huizinga, O.; Joisten, C.; Pflanz, J.; Torbahn, G.; Wiegand, S.; Holzapfel, C.; Hauner, H. Changes in lifestyle and body weight in children and adolescents during the COVID-19 pandemic: A representative survey of parents in Germany. Obes. Facts 2023, 16, 301–312. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus (COVID-19) Dashboard. Available online: http://covid19.who.int (accessed on 16 January 2024).
- Iacopetta, D.; Ceramella, J.; Catalano, A.; Saturnino, C.; Pellegrino, M.; Mariconda, A.; Longo, P.; Sinicropi, M.S.; Aquaro, S. COVID-19 at a glance: An up-to-date overview on variants, drug design and therapies. Viruses 2022, 14, 573. [Google Scholar] [CrossRef] [PubMed]
- Ceramella, J.; Iacopetta, D.; Sinicropi, M.S.; Andreu, I.; Mariconda, A.; Saturnino, C.; Giuzio, F.; Longo, P.; Aquaro, S.; Catalano, A. Drugs for COVID-19: An update. Molecules 2022, 27, 8562. [Google Scholar] [CrossRef] [PubMed]
- Toussi, S.S.; Hammond, J.L.; Gerstenberger, B.S.; Anderson, A.S. Therapeutics for COVID-19. Nat. Microbiol. 2023, 8, 771–786. [Google Scholar] [CrossRef]
- World Health Organization. EG.5 Initial Risk Evaluation. Available online: www.who.int/docs/default-source/coronaviruse/09082023eg.5_ire_final.pdf (accessed on 4 September 2023).
- Dyer, O. COVID-19: Infections climb globally as EG.5 variant gains ground. BMJ 2023, 382, p1900. [Google Scholar] [CrossRef]
- Child, I.; Loza, A.; Doolittle, B. Collateral damage from the COVID-19 pandemic: Pediatric obesity. Populat. Health Manag. 2022, 25, 573–574. [Google Scholar] [CrossRef]
- Valenzise, M.; D’Amico, F.; Cucinotta, U.; Lugarà, C.; Zirilli, G.; Zema, A.; Wasniewska, M.; Pajno, G.B. The lockdown effects on a pediatric obese population in the COVID-19 era. Ital. J. Pediatr. 2021, 47, 209. [Google Scholar] [CrossRef]
- Catalano, A.; Iacopetta, D.; Ceramella, J.; Pellegrino, M.; Giuzio, F.; Marra, M.; Rosano, C.; Saturnino, C.; Sinicropi, M.S.; Aquaro, S. Antibiotic-Resistant ESKAPE Pathogens and COVID-19: The Pandemic beyond the Pandemic. Viruses 2023, 15, 1843. [Google Scholar] [CrossRef]
- Angelini, M.; Teglia, F.; Astolfi, L.; Casolari, G.; Boffetta, P. Decrease of cancer diagnosis during COVID-19 pandemic: A systematic review and meta-analysis. Eur. J. Epidemiol. 2023, 38, 31–38. [Google Scholar] [CrossRef]
- Iacopetta, D.; Ceramella, J.; Baldino, N.; Sinicropi, M.S.; Catalano, A. Targeting breast cancer: An overlook on current strategies. Int. J. Mol. Sci. 2023, 24, 3643. [Google Scholar] [CrossRef]
- Concepcion, J.; Yeager, M.; Alfaro, S.; Newsome, K.; Ibrahim, J.; Bilski, T.; Elkbuli, A. Trends of cancer screenings, diagnoses, and mortalities during the COVID-19 pandemic: Implications and future recommendations. Am. Surg. 2022, 89, 2276–2283. [Google Scholar] [CrossRef]
- Picone, P.; Sanfilippo, T.; Guggino, R.; Scalisi, L.; Monastero, R.; Baschi, R.; Mandalà, V.; San Biagio, L.; Rizzo, M.; Giacomazza, D. Neurological consequences, mental health, physical care, and appropriate nutrition in Long-COVID-19. Cell. Mol. Neurobiol. 2023, 43, 1685–1695. [Google Scholar] [CrossRef]
- Lin, J.E.; Asfour, A.; Sewell, T.B.; Hooe, B.; Pryce, P.; Earley, C.; Shen, M.Y.; Kerner-Rossi, M.; Thakur, K.T.; Vargas, W.S.; et al. Neurological issues in children with COVID-19. Neurosci. Lett. 2021, 743, 135567. [Google Scholar] [CrossRef]
- Llorca-Bofí, V.; Adrados-Pérez, M.; Sánchez-Cazalilla, M.; Torterolo, G.; Arenas-Pijoan, L.; Buil-Reiné, E.; Nicolau-Subires, E.; Albert-Porcar, C.; Ibarra-Pertusa, L.; Puigdevall-Ruestes, M.; et al. Urgent care and suicidal behavior in the child and adolescent population in a psychiatric emergency department in a Spanish province during the two COVID-19 states of alarmAtención urgente y conducta suicida en población infantojuvenil en un servicio de urgencias psiquiátricas de una provincia española durante los 2 estados de alarma por COVID-19. Rev. Psiquiatr. Salud Ment. 2023, 16, 76–83. [Google Scholar] [CrossRef]
- Sheikh, A.; Owais, R.; Ali, E.; Shaikh, A. COVID-19 and early puberty—An unintended consequence of COVID-19 lockdown? Develop. Psychobiol. 2023, 65, e22384. [Google Scholar] [CrossRef]
- Li, L.; Taeihagh, A.; Tan, S.Y. A Scoping review of the impacts of COVID-19 physical distancing measures on vulnerable population groups. Nat. Commun. 2023, 14, 599. [Google Scholar] [CrossRef]
- Catalano, A.; Iacopetta, D.; Ceramella, J.; Maio, A.C.; Basile, G.; Giuzio, F.; Bonomo, M.G.; Aquaro, S.; Walsh, T.J.; Sinicropi, M.S.; et al. Are Nutraceuticals Effective in COVID-19 and Post-COVID Prevention and Treatment? Foods 2022, 11, 2884. [Google Scholar] [CrossRef]
- Oronsky, B.; Larson, C.; Hammond, T.C.; Oronsky, A.; Kesari, S.; Lybeck, M.; Reid, T.R. A Review of Persistent Post-COVID Syndrome (PPCS). Clin. Rev. Allergy Immunol. 2021, 64, 66–74. [Google Scholar] [CrossRef]
- Geetha, T. Novel differentially methylated regions identified by genome-wide DNA methylation analyses contribute to racial disparities in childhood obesity. Genes 2023, 14, 1098. [Google Scholar] [CrossRef]
- Vourdoumpa, A.; Paltoglou, G.; Charmandari, E. The genetic basis of childhood obesity: A systematic review. Nutrients 2023, 15, 1416. [Google Scholar] [CrossRef]
- Richer, L.P.; Tan, Q.; Butler, M.G.; Avedzi, H.M.; DeLorey, D.S.; Peng, Y.; Tun, H.M.; Sharma, A.M.; Ainsley, S.; Orsso, C.E.; et al. Evaluation of autonomic nervous system dysfunction in childhood obesity and Prader–Willi syndrome. Int. J. Mol. Sci. 2023, 24, 8013. [Google Scholar] [CrossRef]
- Salama, M.; Balagopal, B.; Fennoy, I.; Kumar, S. Childhood Obesity, Diabetes. and Cardiovascular Disease Risk. J. Clin. Endocrinol. Metab. 2023, 108, 3051–3066. [Google Scholar] [CrossRef]
- Gunaratne, N.; Deplewski, D. Metabolic consequences of pediatric obesity: A review of pathophysiology, screening, and treatment. Pediatr. Ann. 2023, 52, e62–e67. [Google Scholar] [CrossRef]
- Piester, T.L.; Jagtap, N.; Kalapala, R. Review of paediatric obesity and non-alcoholic fatty liver disease—A focus on emerging non-pharmacologic treatment strategies. Pediatr. Obes. 2023, 18, e13067. [Google Scholar] [CrossRef]
- Pourghazi, F.; Mohammadi, S.; Eslami, M.; Zoshk, M.Y.; Asadi, S.; Ejtahed, H.S.; Qorbani, M. Association between Childhood Obesity and Later Life Kidney Disorders: A Systematic Review. J. Ren. Nutr. 2023, 33, 520–528. [Google Scholar] [CrossRef]
- Jee, Y.H.; Jumani, S.; Mericq, V. The association of accelerated early growth, timing of puberty, and metabolic consequences in children. J. Clin. Endocrinol. Metab. 2023, 108, e663–e670. [Google Scholar] [CrossRef]
- Song, K.; Jung, S.Y.; Yang, J.; Lee, H.S.; Kim, H.-S.; Chae, H.W. Change in prevalence of hypertension among Korean children and adolescents during the Coronavirus Disease 2019 (COVID-19) outbreak: A population-based study. Children 2023, 10, 159. [Google Scholar] [CrossRef]
- Ortiz-Pinto, M.A.; de Miguel-García, S.; Ortiz-Marrón, H.; Ortega-Torres, A.; Cabañas, G.; Gutiérrez–Torres, L.F.; Quiroga–Fernández, C.; Ordobás-Gavin, M.; Galán, I. Childhood obesity and risk of SARS-CoV-2 infection. Int. J. Obes. 2022, 46, 1155–1159. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Ghezzi, M.; Cena, H.; Pascuzzi, M.C.; Regalbuto, C.; Lamberti, R.; Rossi, V.; Manuelli, M.; Bosetti, A.; et al. Pediatric obesity-related asthma: The role of nutrition and nutrients in prevention and treatment. Nutrients 2021, 13, 3708. [Google Scholar] [CrossRef]
- Tsenoli, M.; Smith, J.E.M.; Khan, M.A.B. A community perspective of COVID-19 and obesity in children: Causes and consequences. Obes. Med. 2021, 22, 100327. [Google Scholar] [CrossRef]
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Obesity in children and adolescents during COVID-19 pandemic. Children 2021, 8, 135. [Google Scholar] [CrossRef]
- Tester, J.M.; Rosas, L.G.; Leung, C.W. Food Insecurity and pediatric obesity: A double whammy in the era of COVID-19. Curr. Obes. Rep. 2020, 16, 442–450. [Google Scholar] [CrossRef]
- Patel, B.P.; Sathiyamoorthy, T.; Giruparajah, M.; Toulany, A.; Hamilton, J.K. Weighing in on COVID-19: The impact of the pandemic on children and adolescents with obesity participating in a weight management program. Pediatr. Obes. 2022, 17, e12948. [Google Scholar] [CrossRef]
- Van Lancker, W.; Parolin, Z. COVID-19, school closures, and child poverty: A social crisis in the making. Lancet Public Health 2020, 5, e243–e244. [Google Scholar] [CrossRef]
- Gayatri, M.; Puspitasari, M.D. The impact of COVID-19 pandemic on family well-being: A literature review. Fam. J. 2022, 5, 10664807221131006. [Google Scholar] [CrossRef]
- Kärkkäinen, S.; Mesiäislehto, M.; Sirniö, O.; Karvonen, S.; Kauppinen, T.M. The role of social transfers in mitigating families with children from the economic impact of the COVID-19 pandemic. Int. J. Soc. Welf. 2023, 32, 352–368. [Google Scholar] [CrossRef]
- Murphy, A.L.; Bush, K.R.; Jurasek, J.E. Parent-child/adolescent relationships during the COVID-19 pandemic. In Parenting Across Cultures: Childrearing, Motherhood and Fatherhood in Non-Western Cultures; Springer International Publishing: Cham, Switzerland, 2022; pp. 367–384. [Google Scholar] [CrossRef]
- Treglia, D.; Cutuli, J.J.; Arasteh, K.; Bridgeland, J. Parental and other caregiver loss due to COVID-19 in the United States: Prevalence by race, state, relationship, and child age. J. Commun. Health 2023, 48, 390–397. [Google Scholar] [CrossRef]
- Whaling, K.M.; Der Sarkissian, A.; Larez, N.; Sharkey, J.D.; Allen, M.A.; Nylund-Gibson, K. Child maltreatment prevention service cases are significantly reduced during the COVID-19 pandemic: A longitudinal investigation into unintended consequences of quarantine. Child Maltreatment 2021, 28, 34–41. [Google Scholar] [CrossRef]
- Cianfarani, S.; Pampanini, V. The impact of stress on health in childhood and adolescence in the era of the COVID-19 pandemic. Horm. Res. Paediatr. 2023, 96, 83–87. [Google Scholar] [CrossRef]
- Nutsugbodo, R.Y.; Mensah, C.; Amissah, E.F.; Baah, N.G. COVID-19, parental job losses, online learning anxiety, and social support of hospitality and tourism students. J. Hosp. Tour. Educ. 2023, 35, 251–264. [Google Scholar] [CrossRef]
- Jenssen, B.P.; Kelly, M.K.; Shu, D.; Dalembert, G.; McPeak, K.E.; Powell, M.; Mayne, S.L.; Fiks, A.G. Trends and persistent disparities in child obesity during the COVID-19 pandemic. Child. Obes. 2023; in press. [Google Scholar] [CrossRef]
- Dubnov-Raz, G.; Maor, S.; Ziv-Baran, T. Pediatric obesity and body weight following the COVID-19 pandemic. Child Care Health Dev. 2022, 48, 881–885. [Google Scholar] [CrossRef]
- Shalitin, S.; Phillip, M.; Yackobovitch-Gavan, M. Changes in body mass index in children and adolescents in Israel during the COVID-19 pandemic. Int. J. Obes. 2022, 46, 1160–1167. [Google Scholar] [CrossRef]
- Maggio, A.B.R.; Gal-Dudding, C.; Martin, X.; Chamay-Weber, C. Evaluation of the impact of the COVID-19 lockdown on BMI in children and adolescents with or without obesity. BMC Pediatr. 2022, 22, 509. [Google Scholar] [CrossRef]
- Hu, P.; Samuels, S.; Maciejewski, K.R.; Li, F.; Aloe, C.; Name, M.V.; Savoye, M.; Sharifi, M. Changes in weight-related health behaviors and social determinants of health among youth with overweight/obesity during the COVID-19 Pandemic. Child. Obes. 2021; in press. [Google Scholar] [CrossRef]
- Mayne, S.L.; Kelleher, S.; Hannan, C.; Kelly, M.K.; Powell, M.; Dalembert, G.; McPeak, K.; Jenssen, B.P.; Fiks, A.G. Neighborhood greenspace and changes in pediatric obesity during COVID-19. Am. J. Prev. Med. 2023, 64, 33–41. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, M.; Yu, J.; Pei, Z.; Sun, C.; He, J.; Qian, T.; Luo, F.; Zhang, S.; Xu, Z. Nationwide trends of pediatric obesity and BMI z-Score From 2017–2021 in China: Comparable findings from real-world mobile- and hospital-based data. Front. Endocrinol. 2022, 13, 859245. [Google Scholar] [CrossRef]
- Hu, J.; Liu, J.; Wang, J.; Shen, M.; Ge, W.; Shen, H.; Zhang, T.; Yang, H.; Yin, J. Unfavorable progression of obesity in children and adolescents due to COVID-19 pandemic: A school-based survey in China. Obesity 2021, 29, 1907–1915. [Google Scholar] [CrossRef]
- O’Brien, K.; Agostino, J.; Ciszek, K.; Douglas, K.A. Parents’ perceptions of their child’s weight among children in their first year of primary school: A mixed-methods analysis of an Australian cross-sectional (complete enumeration) study. Int. J. Obes. 2022, 46, 992–1001. [Google Scholar] [CrossRef]
- Neshteruk, C.D.; Zizzi, A.; Suarez, L.; Erickson, E.; Kraus, W.E.; Li, J.S.; Skinner, A.C.; Story, M.; Zucker, N.; Armstrong, S.C. Weight-related behaviors of children with obesity during the COVID-19 pandemic. Child. Obes. 2021, 17, 371–378. [Google Scholar] [CrossRef]
- Miller, A.; Bochner, R.; Sohler, N.; Calixte, R.; Chan, C.; Umpaichitra, V.; Shalmiyev, E.; Novikova, N.; Desai, N.; Seigel, W.; et al. Modified body mass index z-scores in children in New York City during the COVID-19 pandemic. Pediatr. Obes. 2022, 17, e12958. [Google Scholar] [CrossRef]
- Pujia, R.; Ferro, Y.; Maurotti, S.; Khoory, J.; Gazzaruso, C.; Pujia, A.; Montalcini, T.; Mazza, E. The effects of COVID-19 on the eating habits of children and adolescents in Italy: A pilot survey study. Nutrients 2021, 13, 2641. [Google Scholar] [CrossRef]
- Salman, H.; İssi Irlayici, F.; Akçam, M. The COVID-19 pandemic and the prevalence of childhood obesity in Turkiye. J. Pediatr. Gastroenterol. Nutr. 2023, 76, e15–e19. [Google Scholar] [CrossRef]
- Fäldt, A.; Nejat, S.; Edvinsson Sollander, S.; Durbeej, N.; Holmgren, A. Increased incidence of overweight and obesity among preschool Swedish children during the COVID-19 pandemic. Eur. J. Public Health 2023, 33, 127–131. [Google Scholar] [CrossRef]
- de Lima, J.B.; Salazar, L.; Fernandes, A.; Teixeira, C.; Marques, L.; Afonso, C. Long COVID in children and adolescents: A retrospective study in a pediatric cohort. Pediatr. Infect. Dis. J. 2023, 42, e109–e111. [Google Scholar] [CrossRef]
- Catalano, A. COVID-19: Could irisin become the handyman myokine of the 21st century? Coronaviruses 2020, 1, 32–41. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. American Academy of Pediatrics Raises Concern about Children’s Nu-Trition and Physical Activity during Pandemic. Available online: https://www.aap.org/en/news-room/news-releases/aap/2020/american-academy-of-pediatrics-raises-concern-about-childrens-nutrition-and-physical-activity-during-pandemic/ (accessed on 17 January 2024).
- Petersen, R.; Pedroso, M.S. Economic benefits of promoting safe walking and biking to school: Creating momentum for community improvements. Am. J. Prevent. Med. 2021, 60, e41–e43. [Google Scholar] [CrossRef]
- Abuga, K.; Nyamweya, N. Alcohol-Based Hand Sanitizers in COVID-19 Prevention: A Multidimensional Perspective. Pharmacy 2021, 9, 64. [Google Scholar] [CrossRef]
- Iacopetta, D.; Catalano, A.; Ceramella, J.; Saturnino, C.; Salvagno, L.; Ielo, I.; Drommi, D.; Scali, E.; Plutino, M.R.; Rosace, G.; et al. The different facets of triclocarban: A review. Molecules 2021, 26, 2811. [Google Scholar] [CrossRef]
- Sinicropi, M.S.; Iacopetta, D.; Ceramella, J.; Catalano, A.; Mariconda, A.; Pellegrino, M.; Saturnino, C.; Longo, P.; Aquaro, S. Triclosan: A small molecule with controversial roles. Antibiotics 2022, 11, 735. [Google Scholar] [CrossRef]
- Khan, A.; Ahsan, A.; Farooq, M.A.; Naveed, M.; Li, H. Role of polycyclic aromatic hydrocarbons as EDCs in metabolic disorders. In Endocrine Disrupting Chemicals-induced Metabolic Disorders and Treatment Strategies; Springer: Cham, Switzerland, 2021; pp. 323–341. [Google Scholar]
- Amato, A.A.; Wheeler, H.B.; Blumberg, B. Obesity and endocrine-disrupting chemicals. Endocr. Connect. 2021, 10, R87–R105. [Google Scholar] [CrossRef]
- Braun, J.M. Early-life exposure to EDCs: Role in childhood obesity and neurodevelopment. Nat. Rev. Endocrinol. 2017, 13, 161–173. [Google Scholar] [CrossRef]
- Woo Baidal, J.A.; Chang, J.; Hulse, E.; Turetsky, R.; Parkinson, K.; Rausch, J.C. Zooming towards a telehealth solution for vulnerable children with obesity during Coronovirus Disease 2019. Obesity 2020, 28, 1184–1186. [Google Scholar] [CrossRef]
- Paruthi, S. Telemedicine in Pediatric Sleep. Sleep Med. Clin. 2020, 15, e1–e7. [Google Scholar] [CrossRef]
- O’Hara, V.M.; Johnston, S.V.; Browne, N.T. The Paediatric weight management office visit via telemedicine: Pre- to Post-COVID-19 pandemic. Pediatr. Obes. 2020, 15, e12694. [Google Scholar] [CrossRef]
- Wang-Selfridge, A.A.; Dennis, J.F. Management of obesity using telemedicine during the COVID-19 pandemic. Mo Med. 2021, 118, 442–445. [Google Scholar]
- Umano, G.R.; Di Sessa, A.; Guarino, S.; Gaudino, G.; Marzuillo, P.; Miraglia Del Giudice, E. Telemedicine in the COVID-19 era: Taking care of children with obesity and diabetes mellitus. World J. Diabetes 2021, 12, 651–657. [Google Scholar] [CrossRef]
- Shah, A.C.; Badawy, S.M. Telemedicine in Pediatrics: Systematic Review of Randomized Controlled Trials. JMIR Pediatr. Parent 2021, 4, e22696. [Google Scholar] [CrossRef]
- Vandoni, M.; Codella, R.; Pippi, R.; Carnevale Pellino, V.; Lovecchio, N.; Marin, L.; Silvestri, D.; Gatti, A.; Magenes, V.C.; Regalbuto, C.; et al. Combatting sedentary behaviors by delivering remote physical exercise in children and adolescents with obesity in the COVID-19 era: A narrative review. Nutrients 2021, 13, 4459. [Google Scholar] [CrossRef]
- Pecoraro, P.; Gallè, F.; Muscariello, E.; Di Mauro, V.; Daniele, O.; Forte, S.; Ricchiuti, R.; Liguori, G.; Valerio, G. A telehealth intervention for ensuring continuity of care of pediatric obesity during the COVID-19 lockdown in Italy. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3502–3507. [Google Scholar] [CrossRef]
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Edwards, K.; Ofori, A.; Kukreja, S.; Schneider, B.; Messiah, S.E. Telehealth utilization among multi-ethnic patients with obesity during the COVID-19 pandemic. J. Telemed. Telecare 2023, 29, 530–539. [Google Scholar] [CrossRef]
- Chaves, E.; Reddy, S.D.; Cadieux, A.; Tomasula, J.; Reynolds, K. The continued impact of the COVID-19 pandemic on pediatric obesity: A commentary on the return to a healthy new “normal”. Int. J. Environ. Res. Public Health 2022, 19, 5597. [Google Scholar] [CrossRef]
- Sanyaolu, A.; Okorie, C.; Qi, X.; Locke, J.; Rehman, S. Childhood and adolescent obesity in the United States: A public health concern. Glob. Pediatr. Health 2019, 6, 2333794x19891305. [Google Scholar] [CrossRef]
- Ajibewa, T.A.; Beemer, L.R.; Sonneville, K.R.; Miller, A.L.; Toledo-Corral, C.; Robinson, L.E.; Hasson, R.E. Psychological stress and lowered physical activity enjoyment in adolescents with overweight/obesity. Am. J. Health Promot. 2021, 35, 766–774. [Google Scholar] [CrossRef]
- Oikarinen, N.; Jokelainen, T.; Heikkilä, L.; Nurkkala, M.; Hukkanen, J.; Salonurmi, T.; Savolainen, M.J.; Teeriniemi, A.M. Low eating self-efficacy is associated with unfavorable eating behavior tendencies among individuals with overweight and obesity. Sci. Rep. 2023, 13, 7730. [Google Scholar] [CrossRef]
- Kang, N.R.; Kwack, Y.S. An Update on mental health problems and cognitive behavioral therapy in pediatric obesity. Pediatr. Gastroenterol. Hepatol. Nutr. 2020, 23, 15. [Google Scholar] [CrossRef]
- Tronieri, J.S.; Wadden, T.A.; Leonard, S.M.; Berkowitz, R.I. A pilot study of acceptance-based behavioural weight loss for adolescents with obesity. Behav. Cogn. Psychother. 2019, 47, 686–696. [Google Scholar] [CrossRef]
- Vasile, C.M.; Padovani, P.; Rujinski, S.D.; Nicolosu, D.; Toma, C.; Turcu, A.A.; Cioboata, R. The increase in childhood obesity and its association with hypertension during pandemics. J. Clin. Med. 2023, 12, 5909. [Google Scholar] [CrossRef]
- Taghizadeh, S.; Hashemi, M.G.; Zarnag, R.K.; Fayyazishishavan, E.; Gholami, M.; Farhangi, M.A.; Gojani, L.J. Barriers and facilitators of childhood obesity prevention policies: A systematic review and meta-synthesis. Front. Pediatr. 2023, 10, 1054133. [Google Scholar] [CrossRef]
- Herouvi, D.; Paltoglou, G.; Soldatou, A.; Kalpia, C.; Karanasios, S.; Karavanaki, K. Lifestyle and pharmacological interventions and treatment indications for the management of obesity in children and adolescents. Children 2023, 10, 1230. [Google Scholar] [CrossRef]
- Freeney Wright, T.; Rivero, C.M.; Barlow, S.E. Updates in the treatment of pediatric obesity. Curr. Treat. Opt. Pediatr. 2023, 9, 93–105. [Google Scholar] [CrossRef]
- Kao, T.S.A.; Ling, J.; Vu, C.; Hawn, R.; Christodoulos, H. Motivational interviewing in pediatric obesity: A meta-analysis of the effects on behavioral outcomes. Ann. Behav. Med. 2023, 57, 605–619. [Google Scholar] [CrossRef]
- Lin, C.A.; Vosburgh, K.L.; Roy, D.; Duffy, V.B. Usability testing an mHealth program with tailored motivational messages for early adolescents. Nutrients 2023, 15, 574. [Google Scholar] [CrossRef]
- Griffiths, L.A.; Douglas, S.M.; Raynor, H.A. The role of structure in dietary approaches for the treatment of pediatric overweight and obesity: A critical review. Obes. Rev. 2021, 22, e13266. [Google Scholar] [CrossRef]
- Barnett, T.A.; Kelly, A.S.; Young, D.R.; Perry, C.K.; Pratt, C.A.; Edwards, N.M.; Rao, G.; Vos, M.B. Sedentary behaviors in today’s youth: Approaches to the prevention and management of childhood obesity: A scientific statement from the American Heart Association. Circulation 2018, 138, e142–e159. [Google Scholar] [CrossRef]
- Zarkogianni, K.; Chatzidaki, E.; Polychronaki, N.; Kalafatis, E.; Nicolaides, N.C.; Voutetakis, A.; Chioti, V.; Kitani, R.-A.; Mitsis, K.; Perakis, Κ.; et al. The ENDORSE feasibility study: Exploring the use of M-Health, artificial intelligence and serious games for the management of childhood obesity. Nutrients 2023, 15, 1451. [Google Scholar] [CrossRef]
- Cuda, S.; Censani, M. Progress in pediatric obesity: New and advanced therapies. Curr. Opin. Pediatr. 2022, 34, 407–413. [Google Scholar] [CrossRef]
- Griggs, C.L.; Perez, N.P., Jr.; Goldstone, R.N.; Kelleher, C.M.; Chang, D.C.; Stanford, F.C.; Pratt, J.S. National trends in the use of metabolic and bariatric surgery among pediatric patients with severe obesity. JAMA Pediatr. 2018, 172, 1191–1192. [Google Scholar] [CrossRef] [PubMed]
- Singhal, R.; Wiggins, T.; Super, J.; Alqahtani, A.; Nadler, E.P.; Ludwig, C.; Tahrani, A.; Mahawar, K.; GENEVA Collaborative. 30-Day morbidity and mortality of bariatric metabolic surgery in adolescence during the COVID-19 pandemic—The GENEVA study. Pediatr. Obes. 2021, 16, e12832. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, A.; Elahmedi, M.; Alqahtani, Y.A.; Al-Darwish, A. Endoscopic sleeve gastroplasty in 109 consecutive children and adolescents with obesity: Two-year outcomes of a new modality. Am. J. Gastroenterol. 2019, 114, 1857–1862. [Google Scholar] [CrossRef]
- Azcona-Sanjulian, M.C. Telomere length and pediatric obesity: A review. Genes 2021, 12, 946. [Google Scholar] [CrossRef]
- Piątkowska-Chmiel, I.; Krawiec, P.; Ziętara, K.J.; Pawłowski, P.; Samardakiewicz, M.; Pac-Kożuchowska, E.; Herbet, M. The impact of chronic stress related to COVID-19 on eating behaviors and the risk of obesity in children and adolescents. Nutrients 2023, 16, 54. [Google Scholar] [CrossRef]
- Choi, J.E.; Lee, H.A.; Park, S.W.; Lee, J.W.; Lee, J.H.; Park, H.; Kim, H.S. Increase of prevalence of obesity and metabolic syndrome in children and adolescents in Korea during the COVID-19 pandemic: A cross-sectional study using the KNHANES. Children 2023, 10, 1105. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, M.D. Investigating the effects of the COVID-19 pandemic on pediatric body mass index, and health status in an inner-city, low-income setting. J. Pediatr. Health Care 2023, 37, 193–199. [Google Scholar] [CrossRef]
- Chang, T.-H.; Chen, Y.-C.; Chen, W.-Y.; Chen, C.-Y.; Hsu, W.-Y.; Chou, Y.; Chang, Y.-H. Weight Gain Associated with COVID-19 lockdown in children and adolescents: A systematic review and meta-analysis. Nutrients 2021, 13, 3668. [Google Scholar] [CrossRef]
- Vogel, M.; Geserick, M.; Gausche, R.; Beger, C.; Poulain, T.; Meigen, C.; Körner, A.; Keller, E.; Kiess, W.; Pfäffle, R. Age- and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int. J. Obes. 2022, 46, 144–152. [Google Scholar] [CrossRef]
- Koebnick, C.; Sidell, M.A.; Li, X.; Resnicow, K.; Kunani, P.; Young, D.R.; Woolford, S.J. Disparities in weight changes during the COVID-19 pandemic-related lockdown in youths. Obesity 2023, 31, 789–801. [Google Scholar] [CrossRef]
- Long, X.; Li, X.Y.; Jiang, H.; Shen, L.D.; Zhang, L.F.; Pu, Z.; Gao, X.; Li, M. Impact of the COVID-19 kindergarten closure on overweight and obesity among 3-to 7-year-old children. World J. Pediatr. 2023, 19, 469–477. [Google Scholar] [CrossRef]
- Pinheiro, F.; Viana, V.; Rêgo, C. Weight trends in children and adolescents during the COVID-19 pandemic and its relationship with psychological distress. Port. J. Pediatr. 2023, 54, 21–31. [Google Scholar]
- Woolford, S.J.; Sidell, M.; Li, X.; Else, V.; Young, D.R.; Resnicow, K.; Koebnick, C. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA 2021, 326, 1434–1436. [Google Scholar] [CrossRef]
- Warhadpande, M.; Sainz, K.; Jacobson, M.S. Effects of the COVID-19 pandemic on pediatric and adolescent ASCVD risk factors. Curr. Atheroscler. Rep. 2023, 25, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Chung, A.; Tully, L.; Czernin, S.; Thompson, R.; Mansoor, A.; Gortmaker, S.L. Reducing risk of childhood obesity in the wake of COVID-19. BMJ 2021, 374, n1716. [Google Scholar] [CrossRef] [PubMed]
- Jenssen, B.P.; Kelly, M.K.; Powell, M.; Bouchelle, Z.; Mayne, S.L.; Fiks, A.G. COVID-19 and changes in child obesity. Pediatrics 2021, 147, e2021050123. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity among Adults: United States, 2017–2018. Available online: https://www.cdc.gov/nchs/products/databriefs/db360.htm (accessed on 16 January 2024).
- Ogden, C.L.; Carroll, M.D.; Fakhouri, T.H.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of obesity among youths by household income and education level of head of household—United States 2011–2014. MMWR. Morb. Mortal. Wkly. Rep. 2018, 67, 186–189. [Google Scholar] [CrossRef]
- Dietz, W.H. The COVID-19 lockdown increased obesity disparities; will the increases in type 2 diabetes continue? Obesity 2023, 31, 699–702. [Google Scholar] [CrossRef]
- Ban, C.Y.; Shin, H.; Eum, S.; Yon, H.; Lee, S.W.; Choi, Y.S.; Shin, Y.H.; Shin, J.U.; Koyanagi, A.; Jacob, L. 17-year trends of body mass index, overweight, and obesity among adolescents from 2005 to 2021, including the COVID-19 pandemic: A Korean national representative study. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 1565–1575. [Google Scholar] [CrossRef] [PubMed]
- Takaya, J.; Higashino, H.; Takaya, R.; Sakaguchi, H.; Tanoue, J.; Higashide, T.; Moriguchi, H.; Nakao, M.; Takai, Y. Effect of the COVID-19 pandemic lockdown on the physique of school-age children in Japan. Ann. Pediatr. Endocrinol. Metab. 2023, 28, 124–130. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iacopetta, D.; Catalano, A.; Ceramella, J.; Pellegrino, M.; Marra, M.; Scali, E.; Sinicropi, M.S.; Aquaro, S. The Ongoing Impact of COVID-19 on Pediatric Obesity. Pediatr. Rep. 2024, 16, 135-150. https://doi.org/10.3390/pediatric16010013
Iacopetta D, Catalano A, Ceramella J, Pellegrino M, Marra M, Scali E, Sinicropi MS, Aquaro S. The Ongoing Impact of COVID-19 on Pediatric Obesity. Pediatric Reports. 2024; 16(1):135-150. https://doi.org/10.3390/pediatric16010013
Chicago/Turabian StyleIacopetta, Domenico, Alessia Catalano, Jessica Ceramella, Michele Pellegrino, Maria Marra, Elisabetta Scali, Maria Stefania Sinicropi, and Stefano Aquaro. 2024. "The Ongoing Impact of COVID-19 on Pediatric Obesity" Pediatric Reports 16, no. 1: 135-150. https://doi.org/10.3390/pediatric16010013
APA StyleIacopetta, D., Catalano, A., Ceramella, J., Pellegrino, M., Marra, M., Scali, E., Sinicropi, M. S., & Aquaro, S. (2024). The Ongoing Impact of COVID-19 on Pediatric Obesity. Pediatric Reports, 16(1), 135-150. https://doi.org/10.3390/pediatric16010013









