Robot-Assisted Ankle Rehabilitation Using the Hybrid Assistive Limb for Children after Equinus Surgery: A Report of Two Cases
Abstract
1. Introduction
2. Materials and Methods
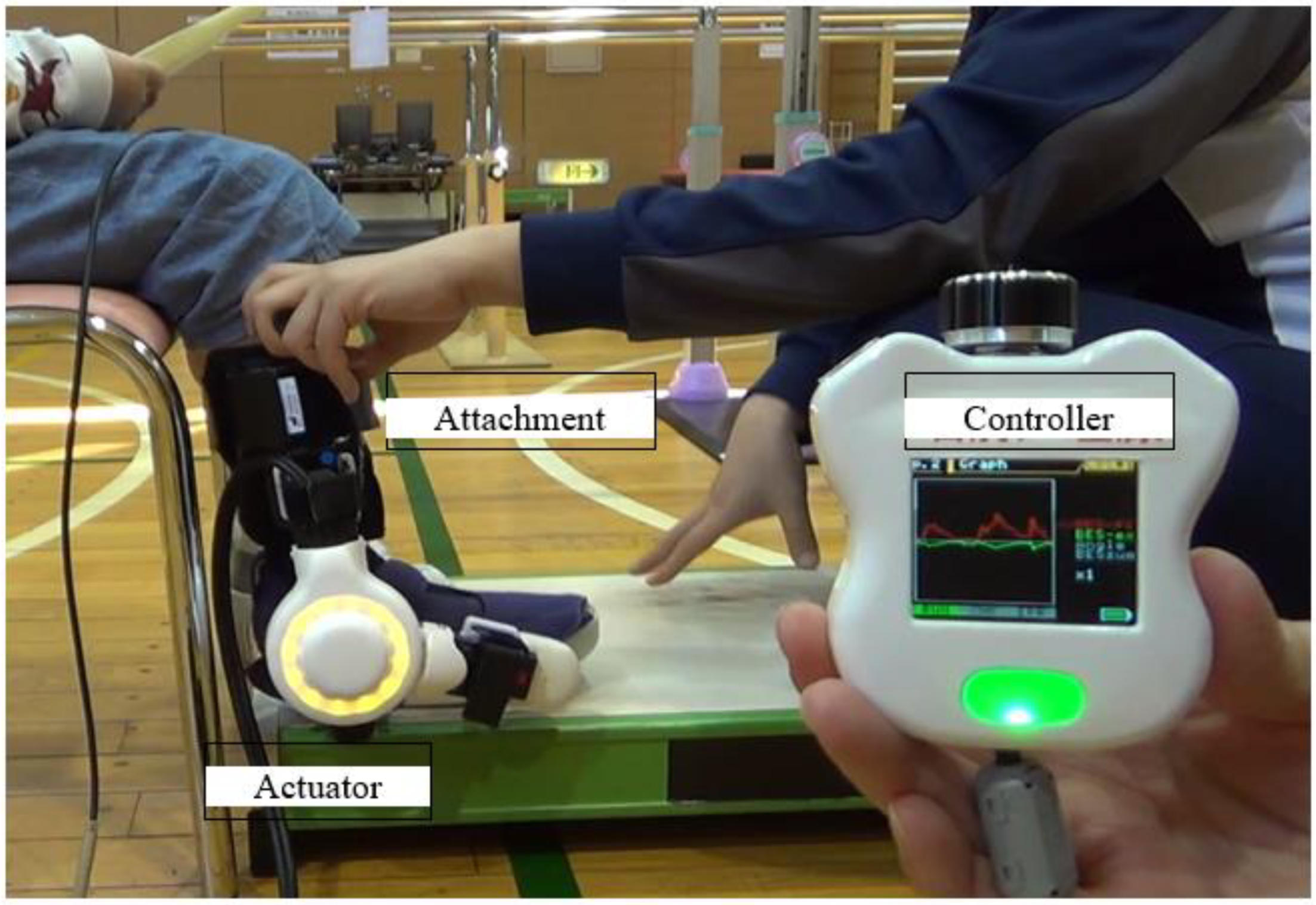
2.1. The Ankle HAL-SJ
2.2. Case Presentation
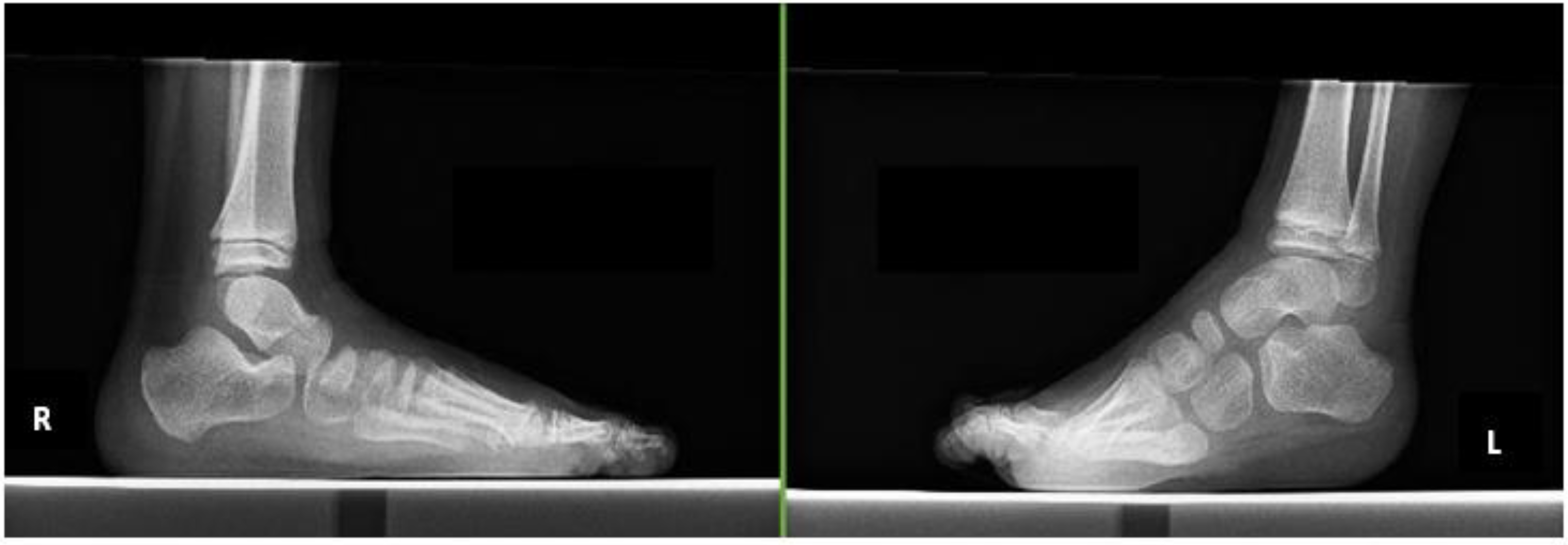
2.2.1. Case 1
2.2.2. Case 2
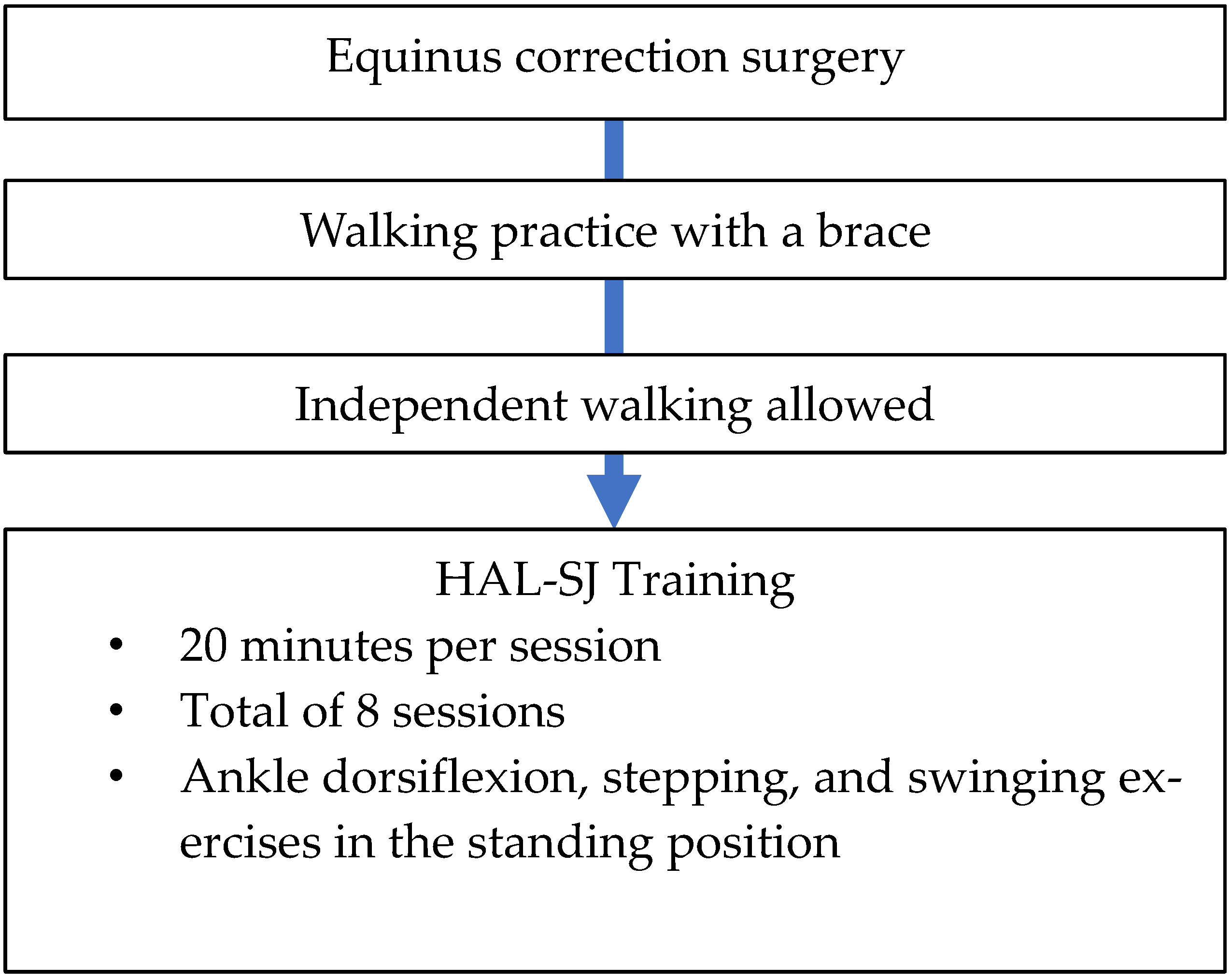
2.3. HAL-SJ Training Protocol
2.4. Outcome Measures
2.4.1. Clinical Assessments
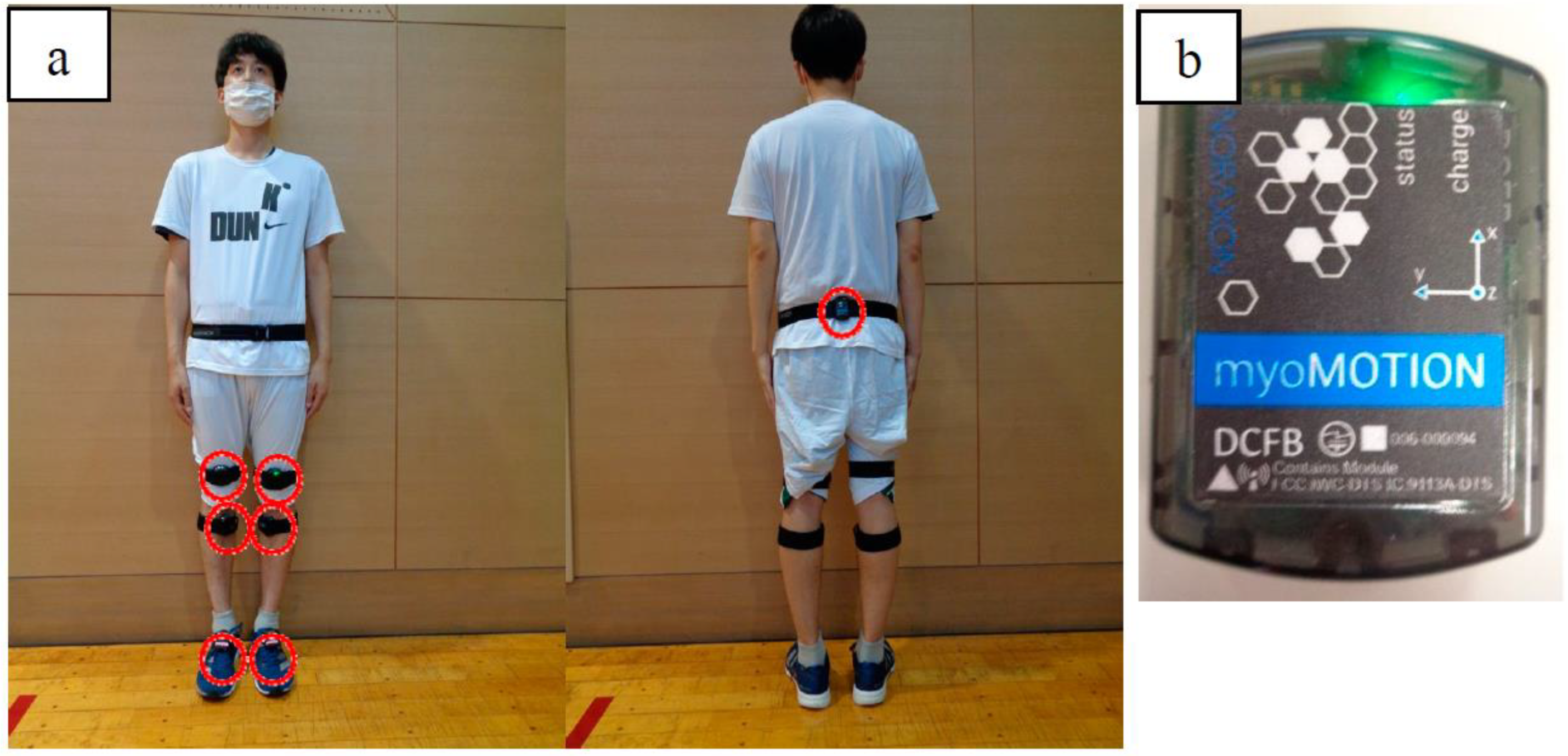
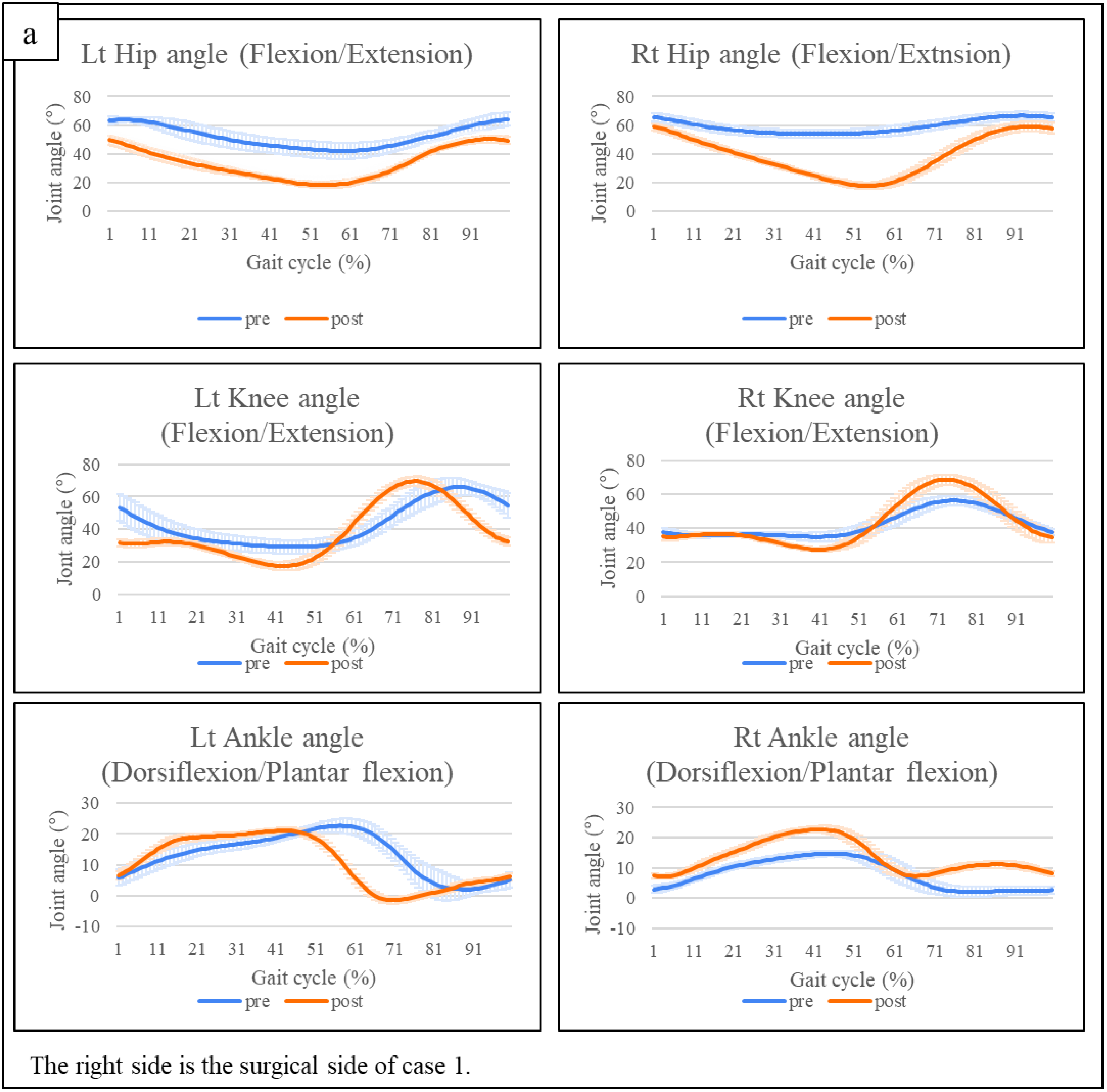
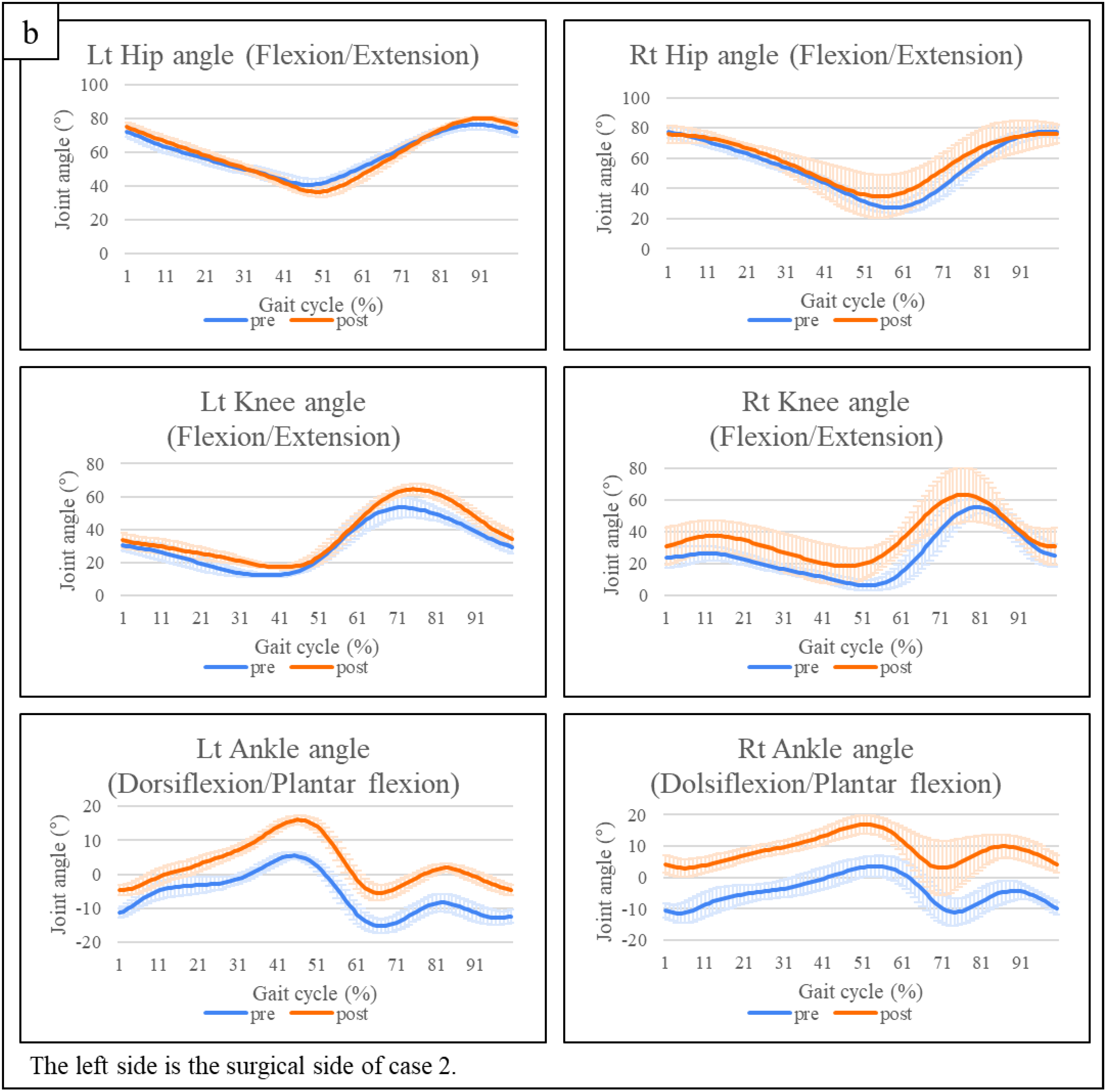
2.4.2. Three-Dimensional Gait Analysis
2.4.3. Co-Contraction of the Medial Gastrocnemius and Tibialis Anterior Muscles
2.5. Ethical Considerations
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lepage, C.; Noreau, L.; Bernard, P.-M. Association between characteristics of locomotion and accomplishment of life habits in children with cerebral palsy. Phys. Ther. 1998, 78, 458–469. [Google Scholar] [CrossRef]
- Graham, H.K.; Fixsen, J.A. Lengthening of the calcanetal tendon in spastic hemiplegia by the white slide technique. J. Bone Jt. Surg. 1988, 70, 472–475. [Google Scholar] [CrossRef]
- Sharrad, W.J.W.; Bernstein, S. Equines deformity in cerebral palsy. J. Bone Jt. Surg. 1972, 54, 272–276. [Google Scholar]
- Graham, H.K.; Selber, P. Musculoskeletal aspects of cerebral palsy. J. Bone Jt. Surg. 2003, 85, 157–166. [Google Scholar] [CrossRef]
- Multani, I.; Manji, J.; Hastings-Ison, T.; Khot, A.; Graham, K. Botulinum toxin in the management of children with cerebral palsy. Paediatr. Drugs 2019, 21, 261–281. [Google Scholar] [CrossRef]
- Heinen, F.; Desloovere, K.; Schroeder, A.S.; Berweck, S.; Borggraefe, I.; van Campenhout, A.; Andersen, G.L.; Aydin, R.; Becher, J.G.; Bernert, G.; et al. The updated European Consensus 2009 on the use of Botulinum toxin for children with cerebral palsy. Eur. J. Paediatr. Neurol. 2010, 14, 45–66. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Namara, M.M.; Paton, M.C.; Popat, H.; et al. State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef]
- Kondo, I.; Hosokawa, K.; Iwata, M.; Oda, A.; Nomura, T.; Ikeda, K.; Asagai, Y.; Kohzaki, T.; Nishimura, H. Effectiveness of selective musclerelease surgery for children with cerebral palsy: Longitudinal and stratified analysis. Dev. Med. Child Neurol. 2004, 46, 540–547. [Google Scholar] [CrossRef]
- Takaki, K.; Kusumoto, Y. The relationship between an ankle selective muscle release operation for patients with diplegic cerebral palsy and selective motor control in the lower extremities. J. Jpn. Acad. Health Sci. 2016, 19, 81–85. [Google Scholar]
- Johnston, T.E.; Finson, R.L.; McCarthy, J.J.; Smith, B.T.; Betz, R.R.; Mulcahey, M.J. Use of functional electrical stimulation to augment traditional orthopaedic surgery in children with cerebral palsy. J. Pediatr. Orthop. 2004, 24, 283–291. [Google Scholar] [CrossRef]
- Mooney, J.A.; Rose, J. A Scoping Review of Neuromuscular Electrical Stimulation to Improve Gait in Cerebral Palsy: The Arc of Progress and Future Strategies. Front. Neurol. 2019, 10, 887. [Google Scholar] [CrossRef]
- Borton, D.C.; Walker, K.; Pirpiris, M.; Nattrass, G.R.; Graham, H.K. Isolated calf lengthening in cerebral palsy. J. Bone Jt. Surg. 2001, 83, 364–370. [Google Scholar] [CrossRef]
- Yoshioka, T.; Kubota, S.; Sugaya, H.; Arai, N.; Hyodo, K.; Kanamori, A.; Yamazaki, M. Feasibility and efficacy of knee extension training using a single-joint hybrid assistive limb, versus conventional rehabilitation during the early postoperative period after total knee arthroplasty. J. Rural Med. 2021, 16, 22–28. [Google Scholar] [CrossRef]
- Shimizu, Y.; Kadone, H.; Kubota, S.; Ueno, T.; Sankai, Y.; Hada, Y.; Yamazaki, M. Voluntary elbow extension-flexion using single joint hybrid assistive limb (HAL) for patients of spastic cerebral palsy: Two cases report. Front. Neurol. 2019, 10, 2. [Google Scholar] [CrossRef]
- Kubota, S.; Kadone, H.; Shimizu, Y.; Koda, M.; Noguchi, H.; Takahashi, H.; Watanabe, H.; Hada, Y.; Sankai, Y.; Yamazaki, M. Development of a New Ankle Jt. Hybrid Assistive Limb. Medicina 2022, 58, 395. [Google Scholar] [CrossRef]
- Matsuda, D.; Kubota, S.; Akinaga, Y.; Yasunaga, Y.; Sankai, Y.; Yamazaki, M. Ankle dorsiflexion training with a newly developed Hybrid Assistive Limb for a patient with foot drop caused by common peroneal nerve palsy: A case report. J. Phys. Ther. Sci. 2022, 34, 410–415. [Google Scholar] [CrossRef]
- Thompson, P.; Beath, T.; Bell, J.; Jacobson, G.; Phair, T.; Salbach, N.M.; Wright, F.V. Test-retest reliability of the 10-metre fast walk test and 6-minute walk test in ambulatory school-aged children with cerebral palsy. Dev. Med. Child Neurol. 2008, 50, 370–376. [Google Scholar] [CrossRef]
- Reese, N.; Bandy, W. Range of Motion and Muscle Length Testing, 3rd ed.; Elsevier: St. Louis, MO, USA, 2016. [Google Scholar]
- Bohannon, R.W.; Smith, M.B. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Fowler, E.G.; Staudt, L.A.; Greenberg, M.B.; Oppenheim, W.L. Selective Control Assessment of the Lower Extremity (SCALE): Development, validation, and interrater reliability of a clinical tool for patients with cerebral palsy. Dev. Med. Child Neurol. 2009, 51, 607–614. [Google Scholar] [CrossRef]
- Rosenbaum, P.L.; Walter, S.D.; Hanna, S.E.; Palisano, R.J.; Russell, D.J.; Raina, P.; Wood, E.; Bartlett, D.J.; Galuppi, B.E. Prognosis for Gross Motor Function in Cerebral Palsy Creation of Motor Development Curves. JAMA 2002, 288, 1357–1363. [Google Scholar] [CrossRef]
- Berner, K.; Cockcroft, J.; Louw, Q. Kinematics and temporospatial parameters during gait from inertial motion capture in adults with and without HIV: A validity and reliability study. Biomed. Eng. Online 2020, 19, 57. [Google Scholar] [CrossRef]
- Damiano, D.L.; Martellotta, T.L.; Sullivan, D.J.; Granata, K.P.; Abel, M.F. Muscle force production and functional performance in spastic cerebral palsy: Relationship of cocontraction. Arch. Phys. Med. Rehabil. 2000, 81, 895–900. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.W.; Yablon, S.A.; Stokic, D.S. Coactivation of ankle muscles during stance phase of gait in patients with lower limb hypertonia after acquired brain injury. Clin. Neurophysiol. 2012, 123, 1599–1605. [Google Scholar] [CrossRef]
- Cauraugh, J.H.; Naik, S.K.; Hsu, W.H.; Coombes, S.A.; Holt, K.G. Children with cerebral palsy: A systematic review and meta-analysis on gait and electrical stimulation. Clin. Rehabil. 2010, 24, 963–978. [Google Scholar] [CrossRef]
- Park, C.I.; Park, E.S.; Kim, H.W.; Rha, D.-W. Soft Tissue Surgery for Equinus Deformity in Spastic Hemiplegic Cerebral Palsy: Effects on Kinematic and Kinetic Parameters. Yonsei Med. J. 2006, 47, 657–666. [Google Scholar] [CrossRef][Green Version]
- Goodman, M.J.; Menown, J.L.; West, J.M., Jr.; Barr, K.M.; Vander Linden, D.W.; McMulkin, M.L. Secondary gait compensations in individuals without neuromuscular involvement following a unilateral imposed equinus constraint. Gait Posture 2004, 20, 238–244. [Google Scholar] [CrossRef]
- Baker, R. Measuring Walking A Handbook of Clinical Gait Analysis; Mac Keith Press: Gosport, UK, 2013. [Google Scholar]
- Kuo, A.D. The six determinants of gait and the inverted pendulum analogy: A dynamic walking perspective. Hum. Mov. Sci. 2007, 26, 617–656. [Google Scholar] [CrossRef]
- Inoue, T.; Sato, Y.; Shimizu, K.; Tashiro, H.; Yokoi, Y.; Kozuka, N. Effects of cane use on walking parameters and lower limb muscle activity in adults with spastic cerebral palsy: A cross-sectional study. J. Phys. Ther. 2021, 33, 544–548. [Google Scholar] [CrossRef]


| Case 1 | Case 2 | |||||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||
| 10-m walk test | Speed | m/s | 0.59 | 1.05 | 0.71 | 0.82 |
| Stride length | m/s | 0.19 | 0.38 | 0.32 | 0.33 | |
| Cadence | steps/min | 192.40 | 163.18 | 131.54 | 147.06 | |
| ROM | DKE | ° | 0 | 5 | 10 | 15 |
| MAS | Dorsiflexion | 0 | 0 | 0 | 0 | |
| Plantar flexion | 0 | 0 | 0 | 0 | ||
| SCALE | 10 | 12 | 12 | 12 | ||
| GMFM | Standing | % | 79.48 | 82.05 | 94.87 | 94.87 |
| Walking, running, and jumping | % | 54.16 | 55.55 | 76.39 | 91.67 | |
| Kinematic Parameters | Case 1 | Case 2 | ||||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||
| Stance phase | ||||||
| Maximum hip extension angle | ° | Rt | −53.75 | −17.71 | −27.23 | −34.72 |
| Lt | −42.03 | −18.44 | −41.23 | −36.57 | ||
| Maximum knee extension angle | ° | Rt | −34.91 | −27.61 | −6.62 | −18.62 |
| Lt | −29.99 | −17.55 | −12.72 | −17.42 | ||
| Swing phase | ||||||
| Maximum hip flexion angle | ° | Rt | 66.47 | 59.04 | 77.78 | 76.16 |
| Lt | 64.12 | 50.21 | 76.43 | 80.26 | ||
| Maximum knee flexion angle | ° | Rt | 56.19 | 68.59 | 55.50 | 50.01 |
| Lt | 65.83 | 69.62 | 53.16 | 50.71 | ||
| Maximum ankle dorsiflexion angle | ° | Rt | 4.35 | 11.20 | −4.26 | 9.90 |
| Lt | 6.12 | 6.11 | −8.50 | 1.82 | ||
| Case 1 | Case 2 | ||||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||
| Ankle joint dorsiflexion | Rt | 0.45 ± 0.31 | 0.88 ± 0.40 | 0.33 ± 0.15 | 0.57 ± 0.24 |
| Lt | 0.58 ± 0.33 | 0.81 ± 0.23 | Error | 0.74 ± 0.27 | |
| Ankle joint plantar flexion | Rt | 0.98 ± 0.58 | 0.26 ± 0.12 | 0.24 ± 0.21 | 0.21 ± 0.17 |
| Lt | 0.38 ± 0.15 | 0.36 ± 0.16 | Error | 0.34 ± 0.27 | |
| COI value during walking | |||||
| Double stance 1 | Rt | 0.86 ± 0.32 | 0.91 ± 0.20 | 0.50 ± 0.17 | 0.54 ± 0.13 |
| Lt | 0.89 ± 0.43 | 0.58 ± 0.18 | 0.78 ± 0.30 | 0.78 ± 0.21 | |
| Left stance phase/right swing phase | Rt | 0.57 ± 0.21 | 0.65 ± 0.13 | 0.71 ± 0.20 | 0.48 ± 0.15 |
| Lt | 0.57 ± 0.24 | 0.50 ± 0.06 | 0.68 ± 0.21 | 0.43 ± 0.06 | |
| Double stance 2 | Rt | 0.76 ± 0.25 | 0.63 ± 0.24 | 0.68 ± 0.16 | 0.59 ± 0.29 |
| Lt | 0.53 ± 0.14 | 0.55 ± 0.09 | 0.63 ± 0.15 | 0.55 ± 0.11 | |
| Left swing phase/right stance phase | Rt | 0.77 ± 0.19 | 0.48 ± 0.09 | 0.53 ± 0.23 | 0.43 ± 0.16 |
| Lt | 0.50 ± 0.16 | 0.33 ± 0.07 | 0.54 ± 0.12 | 0.49 ± 0.09 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takahashi, K.; Mutsuzaki, H.; Yoshikawa, K.; Yamamoto, S.; Koseki, K.; Takeuchi, R.; Mataki, Y.; Iwasaki, N. Robot-Assisted Ankle Rehabilitation Using the Hybrid Assistive Limb for Children after Equinus Surgery: A Report of Two Cases. Pediatr. Rep. 2022, 14, 338-351. https://doi.org/10.3390/pediatric14030041
Takahashi K, Mutsuzaki H, Yoshikawa K, Yamamoto S, Koseki K, Takeuchi R, Mataki Y, Iwasaki N. Robot-Assisted Ankle Rehabilitation Using the Hybrid Assistive Limb for Children after Equinus Surgery: A Report of Two Cases. Pediatric Reports. 2022; 14(3):338-351. https://doi.org/10.3390/pediatric14030041
Chicago/Turabian StyleTakahashi, Kazushi, Hirotaka Mutsuzaki, Kenichi Yoshikawa, Satoshi Yamamoto, Kazunori Koseki, Ryoko Takeuchi, Yuki Mataki, and Nobuaki Iwasaki. 2022. "Robot-Assisted Ankle Rehabilitation Using the Hybrid Assistive Limb for Children after Equinus Surgery: A Report of Two Cases" Pediatric Reports 14, no. 3: 338-351. https://doi.org/10.3390/pediatric14030041
APA StyleTakahashi, K., Mutsuzaki, H., Yoshikawa, K., Yamamoto, S., Koseki, K., Takeuchi, R., Mataki, Y., & Iwasaki, N. (2022). Robot-Assisted Ankle Rehabilitation Using the Hybrid Assistive Limb for Children after Equinus Surgery: A Report of Two Cases. Pediatric Reports, 14(3), 338-351. https://doi.org/10.3390/pediatric14030041






