Impact of Intracranial Hypertension on Outcome of Severe Traumatic Brain Injury Pediatric Patients: A 15-Year Single Center Experience
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
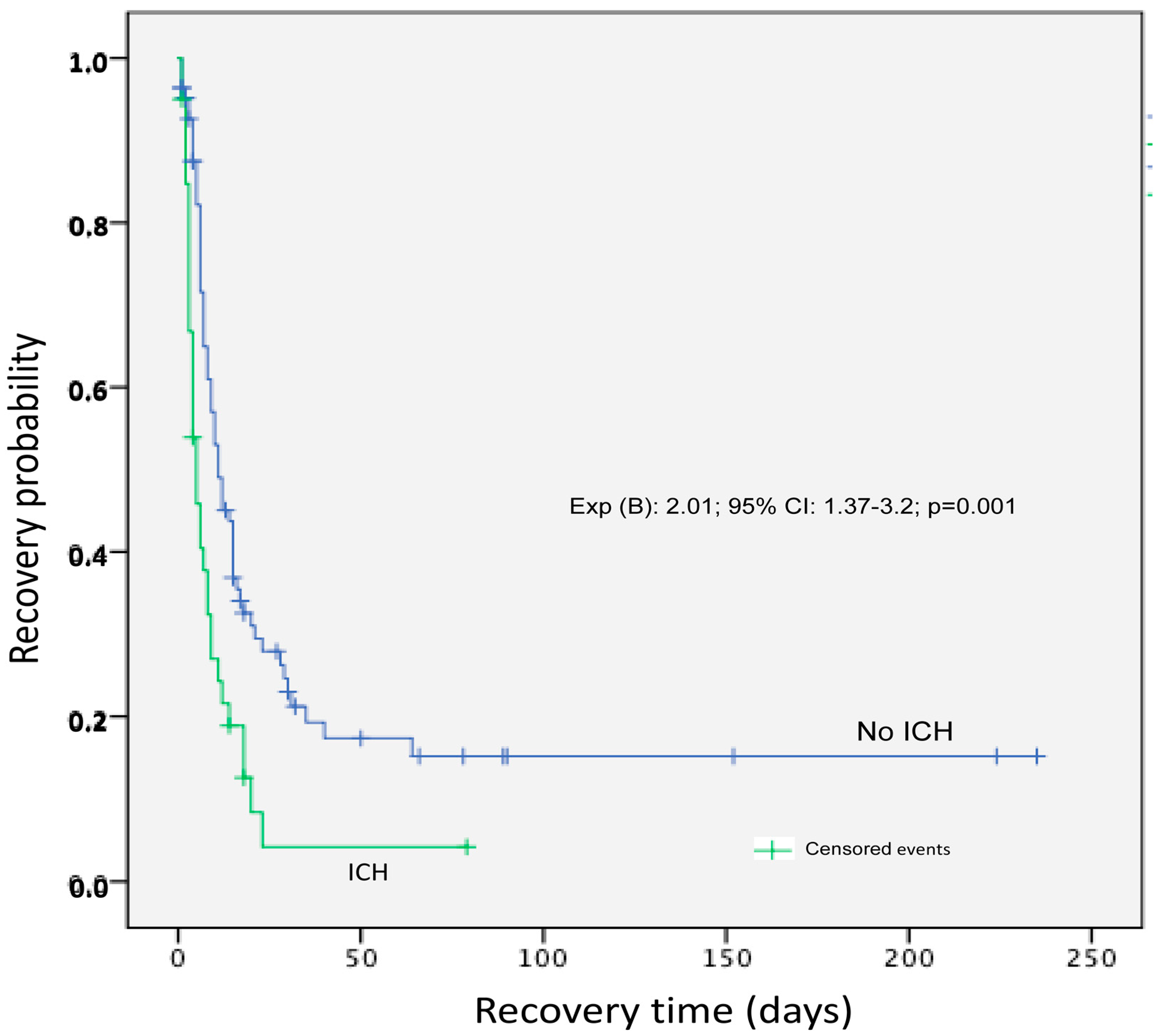
2.2. Primary and Secondary Endpoints of the Study
2.3. Statistical Analyses
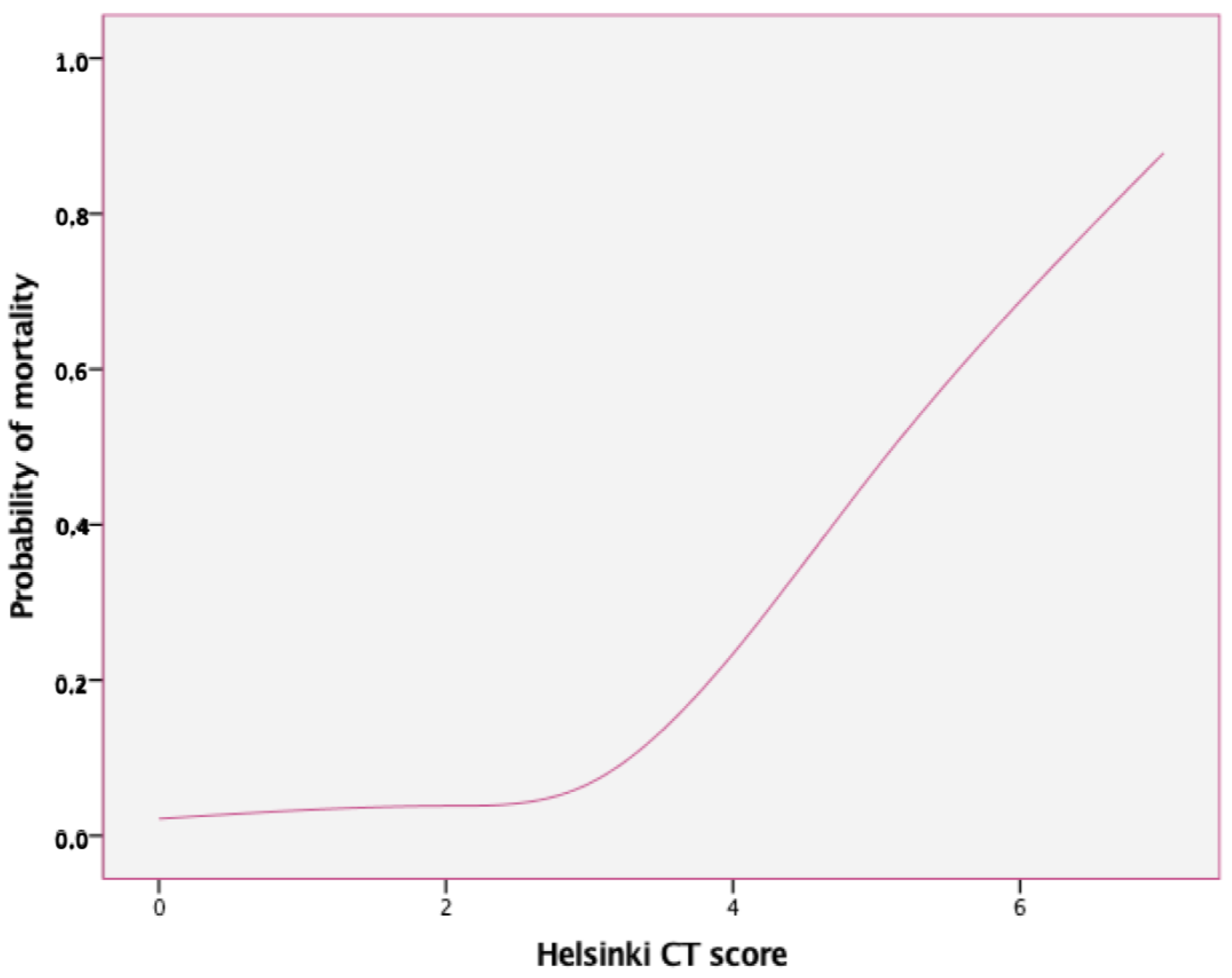
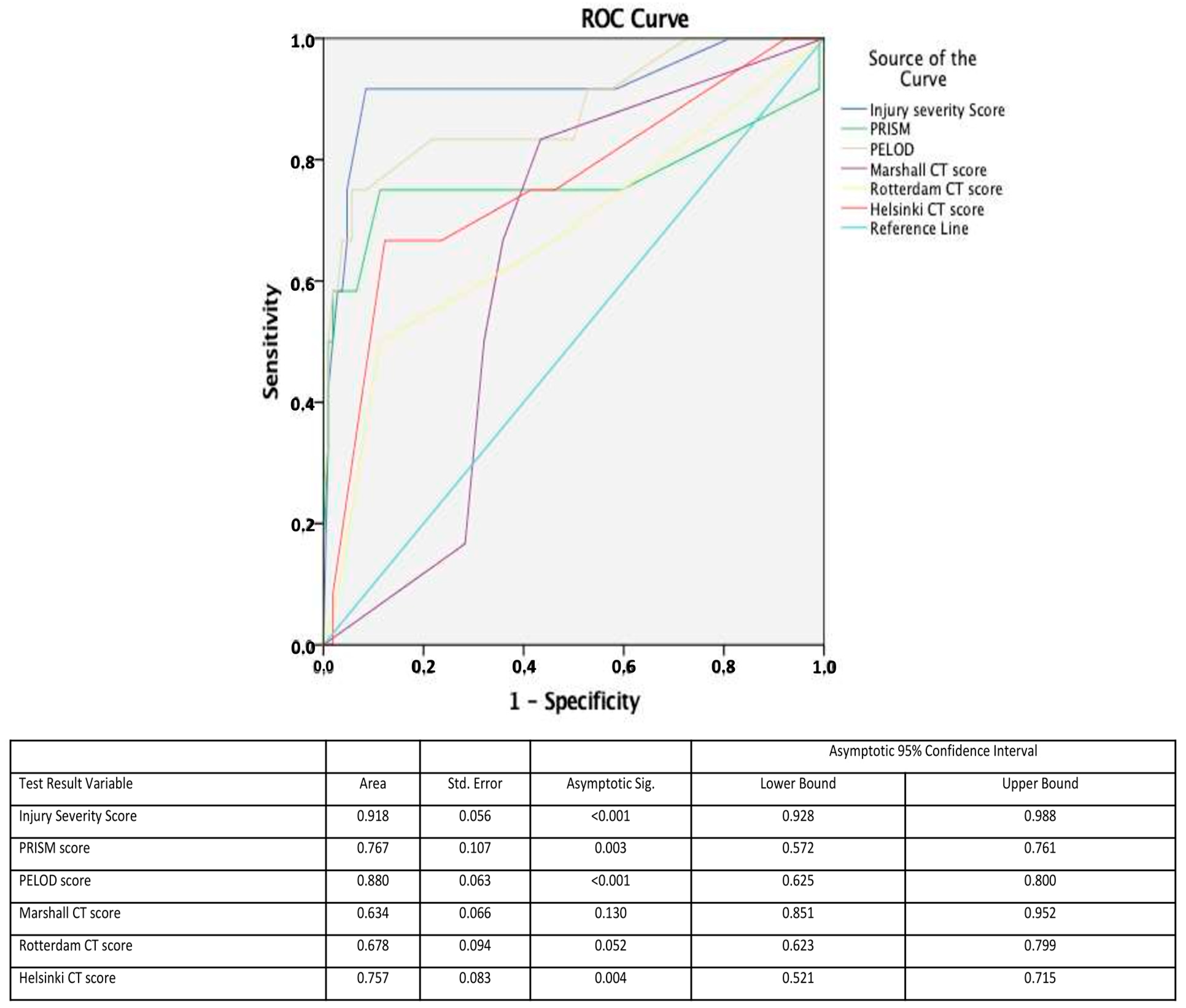
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Han, J.; Yang, S.; Zhang, C.; Zhao, M.; Li, A. Impact of Intracranial Pressure Monitoring on Prognosis of Patients with Severe Traumatic Brain Injury: A PRISMA Systematic Review and Meta-Analysis. Medicine 2016, 95, e2827. [Google Scholar] [CrossRef] [PubMed]
- Young, A.M.H.; Guilfoyle, M.R.; Donnelly, J.; Smielewski, P.; Agarwal, S.; Czosnyka, M.; Hutchinson, P.J. Multimodality neuromonitoring in severe pediatric traumatic brain injury. Pediatr. Res. 2018, 83, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Miles, D.K.; Ponisio, M.R.; Colvin, R.; Limbrick, D.; Greenberg, J.K.; Brancato, C.; Leonard, J.R.; Pineda, J.A. Predictors of intracranial hypertension in children undergoing ICP monitoring after severe traumatic brain injury. Childs Nerv. Syst. 2020, 36, 1453–1460. [Google Scholar] [CrossRef]
- Abraham, P.; Rennert, R.C.; Gabel, B.C.; Sack, J.A.; Karanjia, N.; Warnke, P.; Chen, C.C. ICP management in patients suffering from traumatic brain injury: A systematic review of randomized controlled trials. Acta Neurochir. 2017, 159, 2279–2287. [Google Scholar] [CrossRef] [PubMed]
- Al Saiegh, F.; Philipp, L.; Mouchtouris, N.; Chalouhi, N.; Khanna, O.; Shah, S.O.; Jallo, J. Comparison of Outcomes of Severe Traumatic Brain Injury in 36,929 Patients Treated with or without Intracranial Pressure Monitoring in a Mature Trauma System. World Neurosurg. 2020, 136, e535–e541. [Google Scholar] [CrossRef] [PubMed]
- Robba, C.; Graziano, F.; Rebora, P.; Elli, F.; Giussani, C.; Oddo, M.; Meyfroidt, G.; Helbok, R.; Taccone, F.S.; Prisco, L.; et al. Intracranial pressure monitoring in patients with acute brain injury in the intensive care unit (SYNAPSE-ICU): An international, prospective observational cohort study. Lancet Neurol. 2021, 20, 548–558. [Google Scholar] [CrossRef]
- Delaplain, P.T.; Grigorian, A.; Lekawa, M.; Mallicote, M.; Joe, V.; Schubl, S.D.; Kuza, C.M.; Dolich, M.; Nahmias, J. Intracranial pressure monitoring associated with increased mortality in pediatric brain injuries. Pediatr. Surg. Int. 2020, 36, 391–398. [Google Scholar] [CrossRef]
- Pedersen, S.H.; Lilja-Cyron, A.; Astrand, R.; Juhler, M. Monitoring and Measurement of Intracranial Pressure in Pediatric Head Trauma. Front. Neurol. 2020, 10, 1376. [Google Scholar] [CrossRef]
- Chesnut, R.M.; Temkin, N.; Videtta, W.; Petroni, G.; Lujan, S.; Pridgeon, J.; Dikmen, S.; Chaddock, K.; Barber, J.; Machamer, J.; et al. Consensus-Based Management Protocol (CREVICE Protocol) for the Treatment of Severe Traumatic Brain Injury Based on Imaging and Clinical Examination for Use When Intracranial Pressure Monitoring Is Not Employed. J. Neurotrauma 2020, 37, 1291–1299. [Google Scholar] [CrossRef]
- Sarnaik, A.; Ferguson, N.M.; O’Meara, A.M.I.; Agrawal, S.; Deep, A.; Buttram, S.; Bell, M.J.; Wisniewski, S.R.; Luther, J.F.; Hartman, A.L.; et al. Age and Mortality in Pediatric Severe Traumatic Brain Injury: Results from an International Study. Neurocrit. Care 2018, 28, 302–313. [Google Scholar] [CrossRef]
- Appenteng, R.; Nelp, T.; Abdelgadir, J.; Weledji, N.; Haglund, M.; Smith, E.; Obiga, O.; Sakita, F.M.; Miguel, E.A.; Vissoci, C.M.; et al. A systematic review and quality analysis of pediatric traumatic brain injury clinical practice guidelines. PLoS ONE 2018, 13, e0201550. [Google Scholar] [CrossRef] [PubMed]
- Banik, S.; Rath, G.P.; Lamsal, R.; Sinha, S.; Bithal, P.K. Intracranial Pressure Monitoring in Children with Severe Traumatic Brain Injury: A Retrospective Study. J. Pediatr. Neurosci. 2019, 14, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Hubertus, V.; Finger, T.; Drust, R.; Al Hakim, S.; Schaumann, A.; Schulz, M.; Gratopp, A.; Thomale, U.-W. Severe Traumatic Brain Injury in children-paradigm of decompressive craniectomy compared to a historic cohort. Acta Neurochir. 2022, 164, 1421–1434. [Google Scholar] [CrossRef] [PubMed]
- Araki, T.; Yokota, H.; Morita, A. Pediatric Traumatic Brain Injury: Characteristic Features, Diagnosis, and Management. Neurol. Med. Chir. 2017, 57, 82–93. [Google Scholar] [CrossRef] [PubMed]
- Derakhshanfar, H.; Pourbakhtyaran, E.; Rahimi, S.; Sayyah, S.; Soltantooyeh, Z.; Karbasian, F. Clinical guidelines for traumatic brain injuries in children and boys. Eur. J. Transl. Myol. 2020, 30, 8613. [Google Scholar] [CrossRef]
- Hussain, E. Traumatic Brain Injury in the Pediatric Intensive Care Unit. Pediatr. Ann. 2018, 47, e274–e279. [Google Scholar] [CrossRef]
- Exo, J.; Kochanek, P.M.; Adelson, P.D.; Greene, S.; Clark, R.S.B.; Bayir, H.; Wisniewski, S.R.; Bell, M.J. Intracranial pressure-monitoring systems in children with traumatic brain injury: Combining therapeutic and diagnostic tools. Pediatr. Crit. Care Med. 2011, 12, 560–565. [Google Scholar] [CrossRef]
- Kaur, P.; Sharma, S. Recent Advances in Pathophysiology of Traumatic Brain Injury. Curr. Neuropharmacol. 2018, 16, 1224–1238. [Google Scholar] [CrossRef]
- Harary, M.; Dolmans, R.G.F.; Gormley, W.B. Intracranial Pressure Monitoring-Review and Avenues for Development. Sensors 2018, 18, 465. [Google Scholar] [CrossRef]
- Kochanek, P.M.; Adelson, P.D.; Rosario, B.L.; Hutchison, J.; Miller Ferguson, N.; Ferrazzano, P.; O’Brien, N.; Beca, J.; Sarnaik, A.; LaRovere, K.; et al. Comparison of Intracranial Pressure Measurements Before and After Hypertonic Saline or Mannitol Treatment in Children with Severe Traumatic Brain Injury. JAMA Netw. Open 2022, 5, e220891. [Google Scholar] [CrossRef]
- Kochanek, P.M.; Tasker, R.C.; Bell, M.J.; Adelson, P.D.; Carney, N.; Vavilala, M.S.; Selden, N.R.; Bratton, S.L.; Grant, G.A.; Kissoon, N.; et al. Management of Pediatric Severe Traumatic Brain Injury: 2019 Consensus and Guidelines-Based Algorithm for First and Second Tier Therapies. Pediatr. Crit. Care Med. 2019, 20, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Chesnut, R.; Aguilera, S.; Buki, A.; Bulger, E.; Citerio, G.; Cooper, D.J.; Arrastia, R.D.; Diringer, M.; Figaji, A.; Gao, G.; et al. A management algorithm for adult patients with both brain oxygen and intracranial pressure monitoring: The Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2020, 46, 919–929. [Google Scholar] [CrossRef] [PubMed]
- Alam, H.B.; Vercruysse, G.; Martin, M.; Brown, C.V.R.; Brasel, K.; Moore, E.E.; Sava, J.; Ciesla, D.; Inaba, K. Western Trauma Association Critical Decisions in Trauma Committee Western Trauma Association critical decisions in trauma: Management of intracranial hypertension in patients with severe traumatic brain injuries. J. Trauma Acute Care Surg. 2020, 88, 345–351. [Google Scholar] [CrossRef] [PubMed]
- O’Lynnger, T.M.; Shannon, C.N.; Le, T.M.; Greeno, A.; Chung, D.; Lamb, F.S.; Wellons, J.C. Standardizing ICU management of pediatric traumatic brain injury is associated with improved outcomes at discharge. J. Neurosurg. Pediatr. 2016, 17, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, M.S.; Hansen, G.; Piantino, J. Pediatric neurocritical care in the 21st century: From empiricism to evidence. Curr. Opin. Crit. Care 2016, 22, 106–112. [Google Scholar] [CrossRef]
- Changa, A.R.; Czeisler, B.M.; Lord, A.S. Management of Elevated Intracranial Pressure: A Review. Curr. Neurol. Neurosci. Rep. 2019, 19, 99. [Google Scholar] [CrossRef]
- Lang, S.S.; Kumar, N.K.; Zhao, C.; Zhang, D.Y.; Tucker, A.M.; Storm, P.B.; Heuer, G.G.; Gajjar, A.A.; Kim, C.T.; Huh, J.W.; et al. Invasive brain tissue oxygen and intracranial pressure (ICP) monitoring versus ICP-only monitoring in pediatric severe traumatic brain injury. J. Neurosurg. Pediatr. 2022, 1, 1–11. [Google Scholar] [CrossRef]
- Dhar, R.; Sandler, R.H.; Manwaring, K.; Kostick, N.; Mansy, H.A. Noninvasive detection of elevated ICP using spontaneous tympanic membrane pulsation. Sci. Rep. 2021, 11, 21957. [Google Scholar] [CrossRef]
- Bailey, B.M.; Liesemer, K.; Statler, K.D.; Riva-Cambrin, J.; Bratton, S.L. Monitoring and prediction of intracranial hypertension in pediatric traumatic brain injury: Clinical factors and initial head computed tomography. J. Trauma Acute Care Surg. 2012, 72, 263–270. [Google Scholar] [CrossRef]
- Alkhoury, F.; Kyriakides, T.C. Intracranial Pressure Monitoring in Children with Severe Traumatic Brain Injury: National Trauma Data Bank-Based Review of Outcomes. JAMA Surg. 2014, 149, 544–548. [Google Scholar] [CrossRef]
- Yao, S.; Song, J.; Li, S.; Cao, C.; Fang, L.; Wang, C.; Xu, G. Helsinki Computed Tomography Scoring System Can Independently Predict Long-Term Outcome in Traumatic Brain Injury. World Neurosurg. 2017, 101, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Kochanek, P.M.; Carney, N.; Adelson, P.D.; Ashwal, S.; Bell, M.J.; Bratton, S.; Carson, S.; Chesnut, R.M.; Ghajar, J.; Goldstein, B.; et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents--second edition. Pediatr. Crit. Care Med. 2012, 13 (Suppl. 1), S1–S82. [Google Scholar] [CrossRef] [PubMed]
- Adelson, P.D.; Bratton, S.L.; Carney, N.A.; Chesnut, R.M.; du Coudray, H.E.M.; Goldstein, B.; Kochanek, P.M.; Miller, H.C.; Partington, M.D.; Selden, N.R.; et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 5. Indications for intracranial pressure monitoring in pediatric patients with severe traumatic brain injury. Pediatr. Crit. Care Med. 2003, 4 (Suppl. 3), S19–S24. [Google Scholar] [PubMed]
- Anania, P.; Battaglini, D.; Miller, J.P.; Balestrino, A.; Prior, A.; D’Andrea, A.; Badaloni, F.; Pelosi, P.; Robba, C.; Zona, G.; et al. Escalation therapy in severe traumatic brain injury: How long is intracranial pressure monitoring necessary? Neurosurg. Rev. 2020, 44, 2415–2423. [Google Scholar] [CrossRef]
- Yuan, Q.; Wu, X.; Sun, Y.; Yu, J.; Li, Z.; Du, Z.; Mao, Y.; Zhou, L.; Hu, J. Impact of intracranial pressure monitoring on mortality in patients with traumatic brain injury: A systematic review and meta-analysis. J. Neurosurg. 2015, 122, 574–587. [Google Scholar] [CrossRef]
- Hawryluk, G.W.J.; Aguilera, S.; Buki, A.; Bulger, E.; Citerio, G.; Cooper, D.J.; Arrastia, R.D.; Diringer, M.; Figaji, A.; Gao, G.; et al. A management algorithm for patients with intracranial pressure monitoring: The Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2019, 45, 1783–1794. [Google Scholar] [CrossRef]
- García-Lira, J.R.; Zapata-Vázquez, R.E.; Alonzo-Vazquez, F.; Rodríguez-Ruz, S.G.; Medina-Moreno, M.R.; Torres-Escalante, J.L. Monitoring Intracranial Pressure in Severe Traumatic Brain Injury. Available online: https://pubmed.ncbi.nlm.nih.gov/27296717/ (accessed on 8 February 2021).
- Zhou, J.; Li, J.; Ye, T.; Zeng, Y. Ultrasound measurements versus invasive intracranial pressure measurement method in patients with brain injury: A retrospective study. BMC Med. Imaging 2019, 19, 53. [Google Scholar] [CrossRef]
- Reisner, A.; Chern, J.J.; Walson, K.; Tillman, N.; Petrillo-Albarano, T.; Sribnick, E.A.; Blackwell, L.S.; Suskin, Z.D.; Kuan, C.-Y.; Vats, A. Introduction of severe traumatic brain injury care protocol is associated with reduction in mortality for pediatric patients: A case study of Children’s Healthcare of Atlanta’s neurotrauma program. J. Neurosurg. Pediatr. 2018, 22, 165–172. [Google Scholar] [CrossRef]
- Ma, R.; Rowland, D.; Judge, A.; Calisto, A.; Jayamohan, J.; Johnson, D.; Richards, P.; Magdum, S.; Wall, S. Complications following intracranial pressure monitoring in children: A 6-year single-center experience. J. Neurosurg. Pediatr. 2018, 21, 278–283. [Google Scholar] [CrossRef]
- Manfiotto, M.; Beccaria, K.; Rolland, A.; Paternoster, G.; Plas, B.; Boetto, S.; Vinchon, M.; Mottolese, C.; Beuriat, P.-A.; Szathmari, A.; et al. Decompressive Craniectomy in Children with Severe Traumatic Brain Injury: A Multicenter Retrospective Study and Literature Review. World Neurosurg. 2019, 129, e56–e62. [Google Scholar] [CrossRef]
- Güresir, E.; Schuss, P.; Seifert, V.; Vatter, H. Decompressive craniectomy in children: Single-center series and systematic review. Neurosurgery 2012, 70, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Bruns, N.; Kamp, O.; Lange, K.; Lefering, R.; Felderhoff-Müser, U.; Dudda, M.; Dohna-Schwake, C.; Dgu, T. Mortality and Outcomes after Decompressive Craniectomy in Children with Severe Traumatic Brain Injury. 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.08.05.21261248v1 (accessed on 8 February 2021).
- Cooper, D.J.; Rosenfeld, J.V.; Murray, L.; Arabi, Y.M.; Davies, A.R.; Ponsford, J.; Seppelt, I.; Reilly, P.; Wiegers, E.; Wolfe, R.; et al. Patient Outcomes at Twelve Months after Early Decompressive Craniectomy for Diffuse Traumatic Brain Injury in the Randomized DECRA Clinical Trial. J. Neurotrauma 2020, 37, 810–816. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Wang, Z.; Su, Z.; Qiu, S.; Xu, J.; Zhou, Y.; Yan, A.; Yin, R.; Lu, B.; Nie, X.; et al. Effects of Intracranial Pressure Monitoring on Mortality in Patients with Severe Traumatic Brain Injury: A Meta-Analysis. PLoS ONE 2016, 11, e0168901. [Google Scholar] [CrossRef] [PubMed]
- Muisyo, T.; Bernardo, E.O.; Camazine, M.; Colvin, R.; Thomas, K.A.; Borgman, M.A.; Spinella, P.C. Mortality prediction in pediatric trauma. J. Pediatr. Surg. 2019, 54, 1613–1616. [Google Scholar] [CrossRef]
- Gonçalves, J.-P.; Severo, M.; Rocha, C.; Jardim, J.; Mota, T.; Ribeiro, A. Performance of PRISM III and PELOD-2 scores in a pediatric intensive care unit. Eur. J. Pediatr. 2015, 174, 1305–1310. [Google Scholar] [CrossRef]
- Brown, J.B.; Gestring, M.L.; Leeper, C.M.; Sperry, J.L.; Peitzman, A.B.; Billiar, T.R.; Gaines, B.A. The value of the Injury Severity Score in pediatric trauma: Time for a new definition of severe injury? J. Trauma Acute Care Surg. 2017, 82, 995–1001. [Google Scholar] [CrossRef]
- Meshcheryakov, S.V.; Semenova, Z.B.; Lukianov, V.I.; Sorokina, E.G.; Karaseva, O.V. Prognosis of Severe Traumatic Brain Injury Outcomes in Children. Acta Neurochir. Suppl. 2018, 126, 11–16. [Google Scholar] [CrossRef]
- Garg, K.; Sharma, R.; Gupta, D.; Sinha, S.; Satyarthee, G.D.; Agarwal, D.; Kale, S.S.; Sharma, B.S.; Mahapatra, A.K. Outcome Predictors in Pediatric Head Trauma: A Study of Clinicoradiological Factors. J. Pediatr. Neurosci. 2017, 12, 149–153. [Google Scholar] [CrossRef]
- Nikova, A.S.; Sioutas, G.; Kotopoulos, K.; Ganchev, D.; Chatzipaulou, V.; Birbilis, T. The Clock Is Ticking-Brain Atrophy in Case of Acute Trauma? Korean J. Neurotrauma 2019, 15, 117–125. [Google Scholar] [CrossRef]
- Mikkonen, E.D.; Skrifvars, M.B.; Reinikainen, M.; Bendel, S.; Laitio, R.; Hoppu, S.; Ala-Kokko, T.; Karppinen, A.; Raj, R. Validation of prognostic models in intensive care unit-treated pediatric traumatic brain injury patients. J. Neurosurg. Pediatr. 2019, 24, 330–337. [Google Scholar] [CrossRef]
- Cooper, S.; Bendinelli, C.; Bivard, A.; Parsons, M.; Balogh, Z.J. Abnormalities on Perfusion CT and Intervention for Intracranial Hypertension in Severe Traumatic Brain Injury. J. Clin. Med. 2020, 9, 2000. [Google Scholar] [CrossRef] [PubMed]
- Shan, Y.; Li, Y.; Xu, X.; Feng, J.; Wu, X.; Gao, G. Evaluation of Intracranial Hypertension in Traumatic Brain Injury Patient: A Noninvasive Approach Based on Cranial Computed Tomography Features. J. Clin. Med. 2021, 10, 2524. [Google Scholar] [CrossRef] [PubMed]
- Gudigar, A.; Raghavendra, U.; Hegde, A.; Menon, G.R.; Molinari, F.; Ciaccio, E.J.; Acharya, U.R. Automated Detection and Screening of Traumatic Brain Injury (TBI) Using Computed Tomography Images: A Comprehensive Review and Future Perspectives. Int. J. Env. Res. Public Health 2021, 18, 6499. [Google Scholar] [CrossRef]
- Thelin, E.P.; Nelson, D.W.; Vehviläinen, J.; Nyström, H.; Kivisaari, R.; Siironen, J.; Svensson, M.; Skrifvars, M.B.; Bellander, B.-M.; Raj, R. Evaluation of novel computerized tomography scoring systems in human traumatic brain injury: An observational, multicenter study. PLoS Med. 2017, 14, e1002368. [Google Scholar] [CrossRef]
- Raj, R.; Siironen, J.; Skrifvars, M.B.; Hernesniemi, J.; Kivisaari, R. Predicting outcome in traumatic brain injury: Development of a novel computerized tomography classification system (Helsinki computerized tomography score). Neurosurgery 2014, 75, 632–646, discussion 646–647. [Google Scholar] [CrossRef]
- Khaki, D.; Hietanen, V.; Corell, A.; Hergès, H.O.; Ljungqvist, J. Selection of CT variables and prognostic models for outcome prediction in patients with traumatic brain injury. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 94. [Google Scholar] [CrossRef]
- Yap, K.E.; Islam, A.A.; Ihwan, A.; Baan, J.A.B.; Hamid, F. Comparison of Helsinki CT and Rotterdam CT Scoring Systems as Prognostic Factors of Brain Injury. Nusant. Med. Sci. J. 2021, 6, 33–43. [Google Scholar] [CrossRef]
- Liesemer, K.; Riva-Cambrin, J.; Bennett, K.S.; Bratton, S.L.; Tran, H.; Metzger, R.R.; Bennett, T.D. Use of Rotterdam CT Scores for Mortality Risk Stratification in Children with Traumatic Brain Injury. Pediatr. Crit. Care Med. 2014, 15, 554–562. [Google Scholar] [CrossRef]


| Variable | ICP Monitoring (n = 78) | No ICP Monitoring (n = 40) | p-Value |
|---|---|---|---|
| Sex, n (%) | NS | ||
| Males | 55 (70.5) | 31 (77.5) | |
| Females | 23 (29.5) | 9 (22.5) | |
| Age (mean, SD) | 10.1 (5.5) | 8.2 (5) | 0.001 |
| Severity of illness measures | |||
| GCS score, median (IQR) | 8 (3–8) | 9.5 (8–15) | 0.001 |
| ISS score, median (IQR) | 14 (10–20) | 7.5 (5–14) | 0.003 |
| PRISM score, median (IQR) | 11 (2–21) | 2 (0–11) | 0.013 |
| PELOD score, median (IQR) | 11 (6–12) | 2 (0–11) | 0.001 |
| Imaging findings | |||
| Marshall CT, n (%) | NS | ||
| I + II | 43 (55) | 28 (70) | |
| III + IV | 13 (17) | 1 (2.5) | |
| V + VI | 22 (28) | 11 (27.5) | |
| Rotterdam CT, n (%) | 0.001 | ||
| 1 | 35 (45) | 25 (62.5) | |
| 2 | 26 (33) | 13 (32.5) | |
| 3 | 13 (17) | 2 (5) | |
| 4 | 4 (5) | 0 (0) | |
| Helsinki CT score (median, IQR) | 2 (0–5) | 0 (0–2) | 0.001 |
| Hospital Outcomes | |||
| PICU LOS, median (IQR) | 10 (5–18) | 5 (2–11) | 0.001 |
| MV days, median (IQR) | 7 (4–12) | 2 (0–4) | 0.001 |
| Glasgow Outcome Score, n (%) | 0.002 | ||
| Good Outcome/Moderate disability | 60 (77) | 37 (92.5) | |
| Severe disability/Vegetative State | 7 (9) | 2 (5) | |
| Death | 11 (14) | 1 (2.5) |
| Variable | ICH (n = 43) | No ICH (n = 75) | p-Value | Survivors (n = 106) | Non-Survivors (n = 12) | p-Value |
|---|---|---|---|---|---|---|
| Sex, n (%) | NS | NS | ||||
| Males | 29 (67.5) | 57 (76) | 77 (72.6) | 9 (75) | ||
| Females | 14 (32.5) | 18 (24) | 29 (27.4) | 3 (25) | ||
| Age (mean, SD) | 10 (5.8) | 9 (5.2) | NS | 9 (5.5) | 7.5 (4) | NS |
| Severity of illness measures | ||||||
| GCS score, median (IQR) | 7 (3–8) | 9.5 (8–13) | 0.001 | 8 (8–12) | 3 (3–8) | 0.001 |
| ISS score, median (IQR) | 16 (14–30) | 10 (5–14) | 0.001 | 10 (5–14) | 40 (20–75) | 0.001 |
| PRISM score, median (IQR) | 12.5 (2.0–22) | 2 (1–11) | 0.001 | 2 (2–11) | 25 (12–35) | 0.001 |
| PELOD score, median (IQR) | 11.5 (8–16) | 6 (2–11) | 0.001 | 6 (2–11) | 21 (12–32) | 0.001 |
| Imaging findings | ||||||
| Marshall CT, n (%) | NS | NS | ||||
| I + II | 21 (49) | 50 (66.7) | 67 (63) | 4 (33) | ||
| III + IV | 8 (18.5) | 6 (8) | 8 (8) | 6 (50) | ||
| V + VI | 14 (32.5) | 19 (25.3) | 31 (29) | 2 (17) | ||
| Rotterdam CT, n (%) | 0.001 | 0.030 | ||||
| 1 | 13 (30.3) | 47 (62.7) | 56 (52.8) | 4 (33) | ||
| 2 | 17 (39.5) | 22 (29.3) | 37 (35) | 2 (17) | ||
| 3 | 11 (25.6) | 4 (5.3) | 10 (9.4) | 5 (42) | ||
| 4 | 2 (4.6) | 2 (2.7) | 3 (2.8) | 1 (8) | ||
| Helsinki CT score (median, IQR) | 2 (0–5) | 0 (0–2) | 0.001 | 0 (0–2) | 5 (0–5) | 0.001 |
| Hospital Outcomes | ||||||
| PICU LOS, median (IQR) | 10 (4–20) | 5 (4–13) | 0.015 | 8 (4–15) | 4 (2–15) | NS |
| MV days, median (IQR) | 7 (4–16) | 3 (3–8) | 0.005 | 4 (1–8) | 5 (2–14) | NS |
| GOS, n (%) | 0.005 | 0.001 | ||||
| Good Outcome/ Moderate disability | 27 (63) | 70 (93.3) | 97 (91.5) | 0 (0) | ||
| Severe disability/ Vegetative State | 6 (14) | 3 (4) | 9 (8.5) | 0 (0) | ||
| Death | 10 (23) | 2 (2.7) | 0 (0) | 12 (100) |
| Intracranial Hypertension | Unfavorable Outcome | |||||
|---|---|---|---|---|---|---|
| p-Value | Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | |
| Age (1 year) | 0.678 | 0.981 | 0.89–1.07 | 0.587 | 1.051 | 0.88–1.25 |
| Female Sex | 0.447 | 0.677 | 0.25–1.85 | 0.189 | 4.166 | 0.5–35 |
| GCS | 0.359 | 1.155 | 0.85–1.57 | 0.677 | 0.878 | 0.48–1.6 |
| ISS | 0.039 | 0.958 | 0.89–0.98 | 0.001 | 0.842 | 0.76–0.94 |
| PRISM score (>20) | 0.650 | 0.984 | 0.91–1.05 | 0.120 | 1.122 | 0.97–1.3 |
| PELOD score (>20) | 0.806 | 0.994 | 0.95–1.04 | 0.009 | 0.736 | 0.58–0.93 |
| Marshall CT score | 0.491 | 0.896 | 0.65–1.22 | 0.301 | 0.735 | 0.41–1.3 |
| Rotterdam CT score | 0.563 | 1.38 | 0.46–4.15 | 0.121 | 5.761 | 0.63–52.8 |
| Helsinki CT score | 0.048 | 0.711 | 0.5–0.91 | 0.141 | 0.645 | 0.36–1.16 |
| Intracranial Hypertension | - | - | - | 0.297 | 2.597 | 0.43–15.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsitsipanis, C.; Miliaraki, M.; Ntotsikas, K.; Baldounis, D.; Kokkinakis, E.; Briassoulis, G.; Venihaki, M.; Vakis, A.; Ilia, S. Impact of Intracranial Hypertension on Outcome of Severe Traumatic Brain Injury Pediatric Patients: A 15-Year Single Center Experience. Pediatr. Rep. 2022, 14, 352-365. https://doi.org/10.3390/pediatric14030042
Tsitsipanis C, Miliaraki M, Ntotsikas K, Baldounis D, Kokkinakis E, Briassoulis G, Venihaki M, Vakis A, Ilia S. Impact of Intracranial Hypertension on Outcome of Severe Traumatic Brain Injury Pediatric Patients: A 15-Year Single Center Experience. Pediatric Reports. 2022; 14(3):352-365. https://doi.org/10.3390/pediatric14030042
Chicago/Turabian StyleTsitsipanis, Christos, Marianna Miliaraki, Konstantinos Ntotsikas, Dimitrios Baldounis, Emmanouil Kokkinakis, George Briassoulis, Maria Venihaki, Antonios Vakis, and Stavroula Ilia. 2022. "Impact of Intracranial Hypertension on Outcome of Severe Traumatic Brain Injury Pediatric Patients: A 15-Year Single Center Experience" Pediatric Reports 14, no. 3: 352-365. https://doi.org/10.3390/pediatric14030042
APA StyleTsitsipanis, C., Miliaraki, M., Ntotsikas, K., Baldounis, D., Kokkinakis, E., Briassoulis, G., Venihaki, M., Vakis, A., & Ilia, S. (2022). Impact of Intracranial Hypertension on Outcome of Severe Traumatic Brain Injury Pediatric Patients: A 15-Year Single Center Experience. Pediatric Reports, 14(3), 352-365. https://doi.org/10.3390/pediatric14030042








