The Appearance of Osteomyelitis of the Foot and Disseminated Subcutaneous Abscesses During Treatment for Disseminated Tuberculosis Infection in an Immunocompetent Patient: Case Presentation of a Paradoxical Reaction and Literature Review
Abstract
1. Introduction
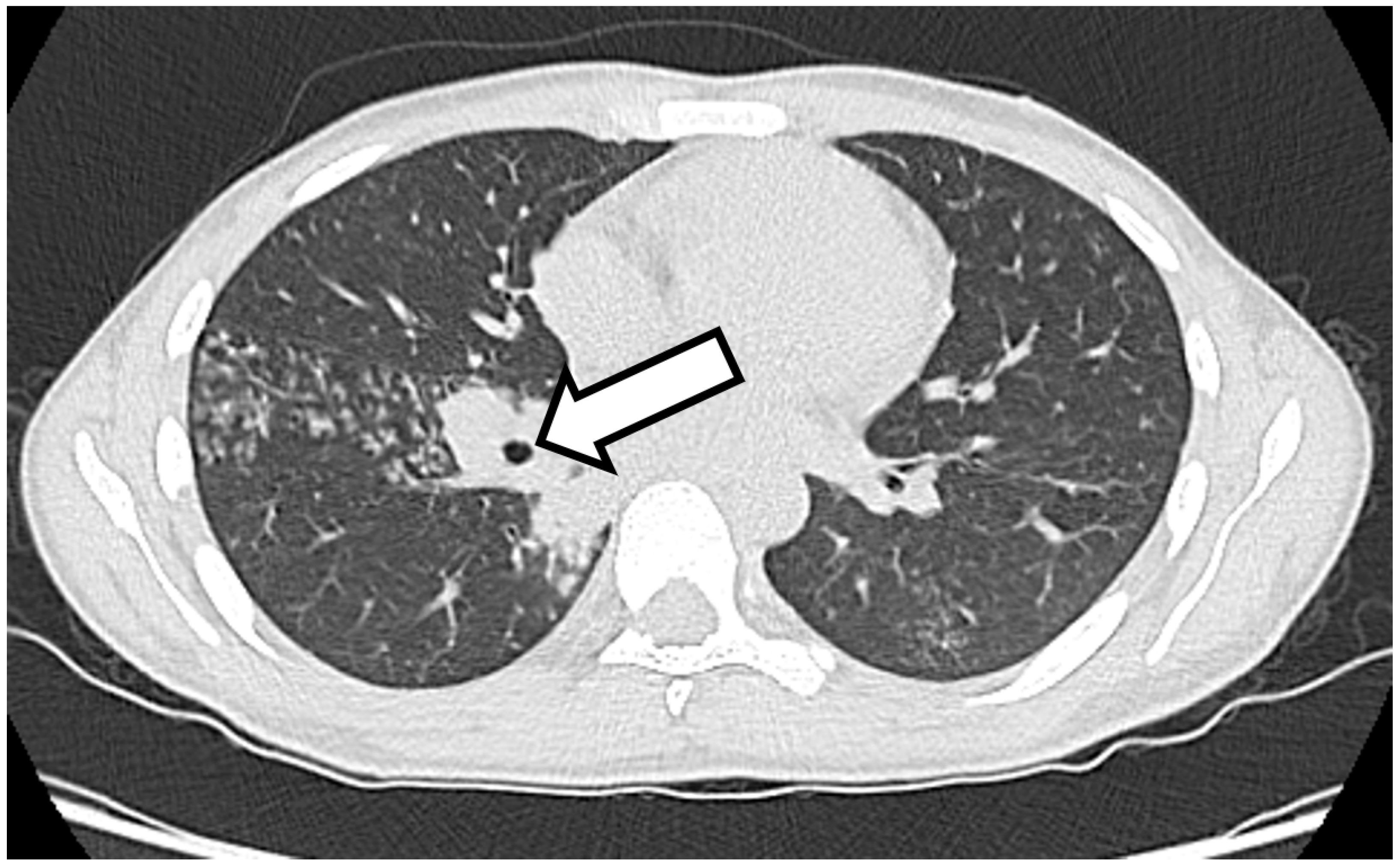
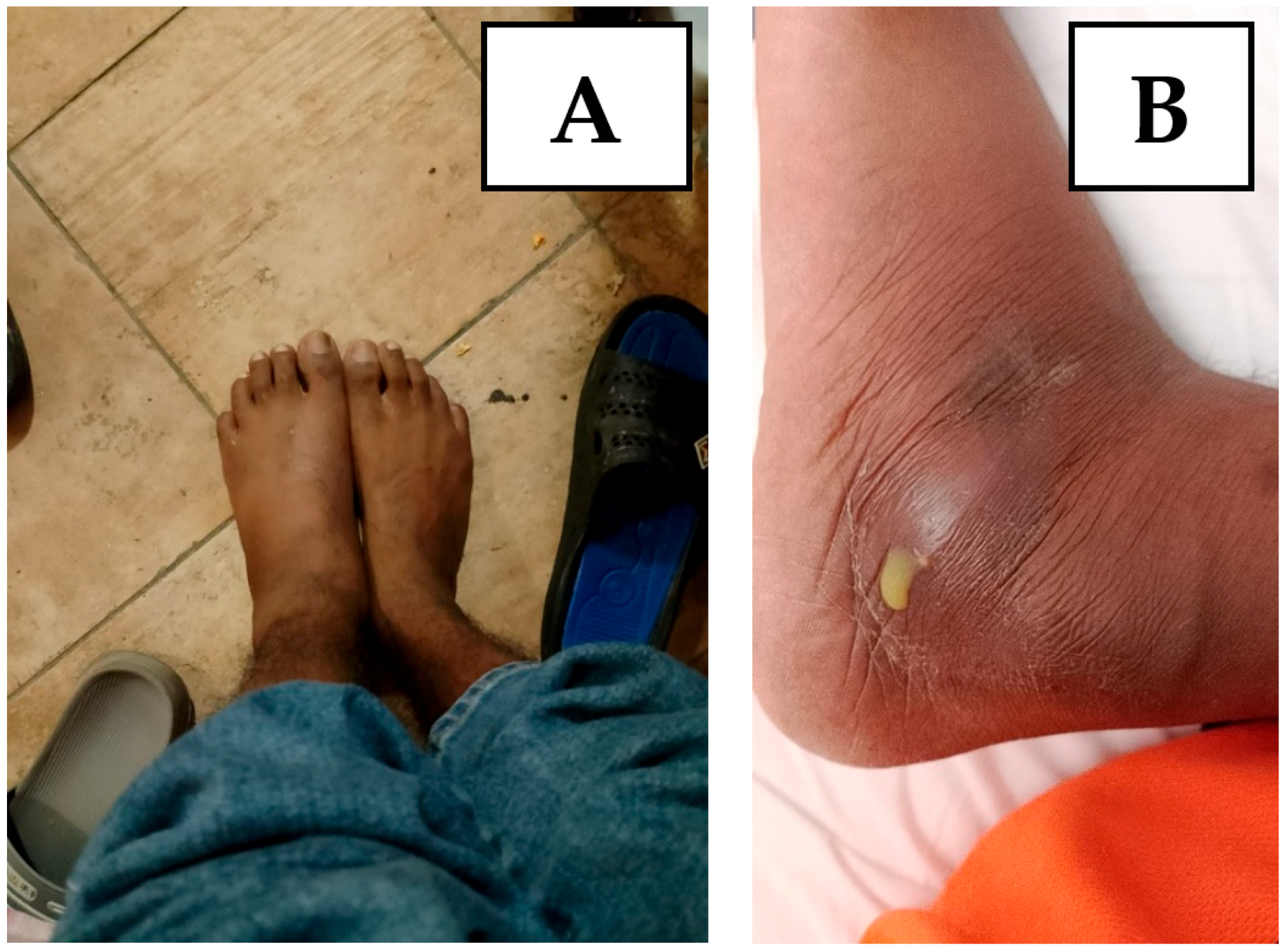
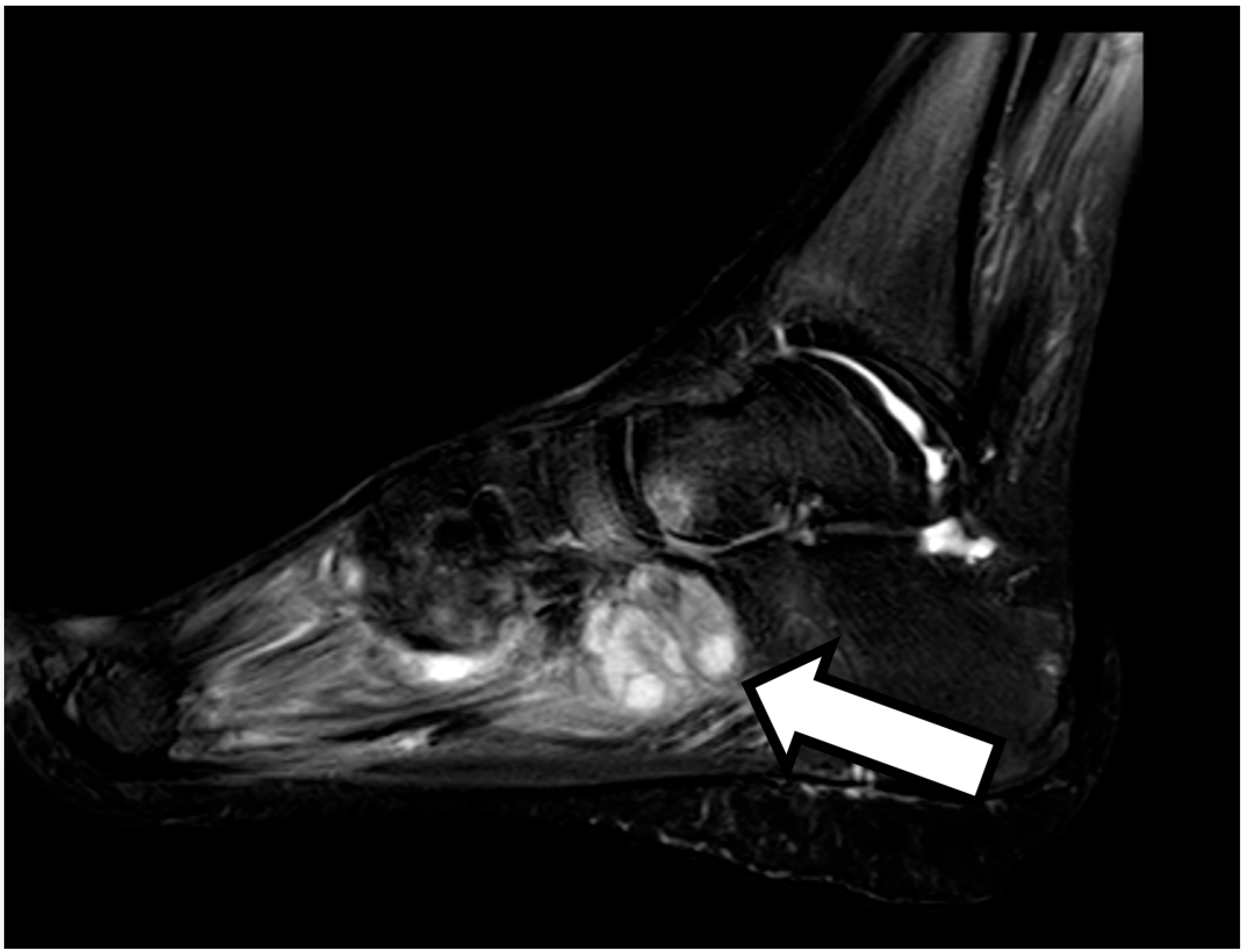
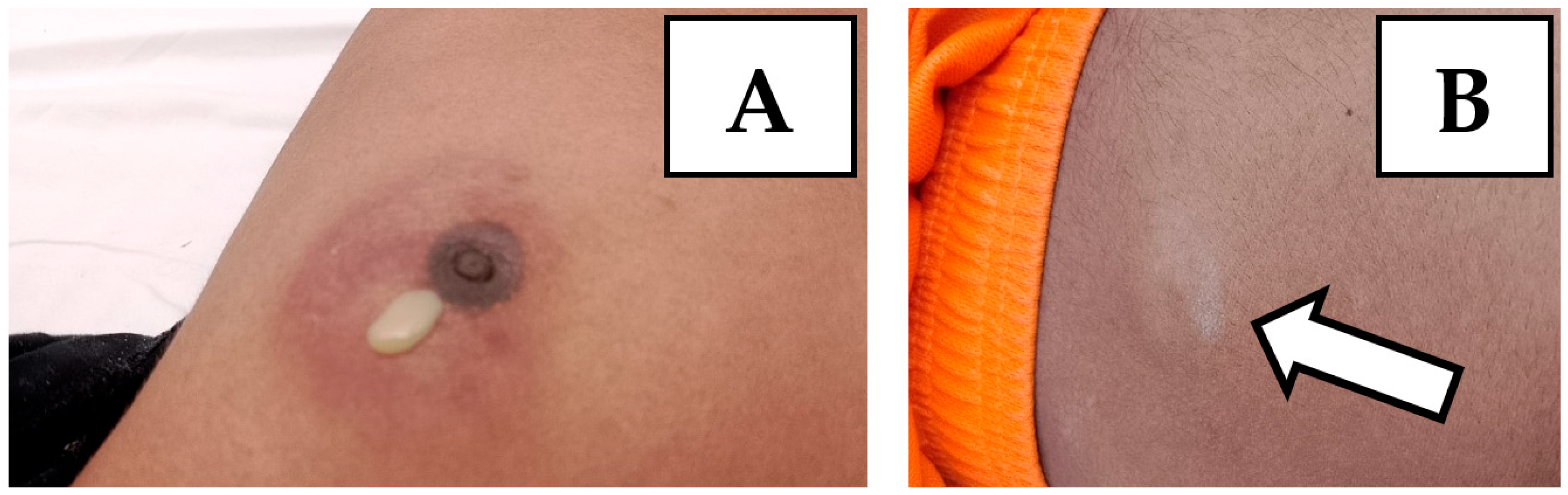
2. Case Presentation
3. Literature Review
4. Discussion and Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azoulay, L.D.; Houist, A.L.; Feredj, E.; Vindrios, W.; Gallien, S. Réaction paradoxale tuberculeuse [Paradoxical tuberculosis reaction]. Rev. Med. Interne 2024, 45, 279–288. (In French) [Google Scholar] [CrossRef] [PubMed]
- Hermans, S.M.; Akkerman, O.W.; Meintjes, G.; Grobusch, M.P. Post-tuberculosis treatment paradoxical reactions. Infection 2024, 52, 2083–2095. [Google Scholar] [CrossRef] [PubMed]
- Done, M.M.; Akkerman, O.W.; Al-Kailany, W.; de Lange, W.C.M.; de Jonge, G.; Kleinnijenhuis, J.; Stienstra, R.; van der Werf, T.S. Corticosteroid therapy for the management of paradoxical inflammatory reaction in patients with pulmonary tuberculosis. Infection 2020, 48, 641–645. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Namale, P.E.; Abdullahi, L.H.; Fine, S.; Kamkuemah, M.; Wilkinson, R.J.; Meintjes, G. Paradoxical TB-IRIS in HIV-infected adults: A systematic review and meta-analysis. Future Microbiol. 2015, 10, 1077–1099. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.; Aljahdali, A.; Ahamed, M.F.; Almarhabi, H. Left hand abscess as a paradoxical reaction during treatment of disseminated tuberculosis in immunocompetent patient: Case report and review of literature. BMC Infect. Dis. 2024, 24, 1186. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Samad, M.; Dallevet, C.A.; Tandjaoui-Lambiotte, Y.; Bourgarit, A.; Jaquet, P. Spectacular Improvement of Paradoxical Reaction in Tuberculosis after Tumor Necrosis Factor-Alpha Antagonist Therapy. Cureus 2023, 15, e50596. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Volpe-Chaves, C.E.; Lacerda, M.L.G.G.; Castilho, S.B.; Fonseca, S.S.O.; Saad, B.A.A.; Franciscato, C.; Tibana, T.K.; Nunes, T.F.; Venturini, J.; Oliveira, S.M.D.V.L.; et al. Vertebral tuberculosis as a paradoxical reaction to the treatment of pulmonary and meningeal tuberculosis in an immunocompetent patient: A case report. Medicine 2020, 99, e20012. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shinga, B.W.; Dièye, A.; Badiane, N.M.D.; Lakhe, N.A.; Diallo, V.M.C.; Mbaye, K.D.; Ka, D.; Badiane, A.S.; Diouf, A.; Déguénonvo, L.F.; et al. Tuberculose intestinale révélée par une occlusion intestinale aigüe au cours d’une réaction paradoxale au traitement anti-tuberculeux chez un patient immunocompétent: À propos d’un cas et revue de la littérature [Intestinal tuberculosis revealed by acute bowel obstruction during paradoxical reaction to antituberculosis treatment in an immunocompetent patient: About a case and literature review]. Pan. Afr. Med. J. 2019, 32, 173. (In French) [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kabra, M.N.; Kunapareddy, T. Paradoxical upgradation response in non-HIV tuberculosis: Report of two cases. Indian J. Med. Microbiol. 2019, 37, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Neki, N.S.; Joshi, N.; Shergill, G.S.; Singh, A.; Meena, N.K.; Kaur, A.; Dhanju, A.S.; Vaid, A.; Kausahal, D. Paradoxical Reaction in an Immunocompetent Internal Medicine Resident Suffering from Tubercular Lymphadenitis. Int. J. Health Sci. Res. 2017, 7, 388–392. [Google Scholar]
- Chaskar, P.; Rana, G.; Anuradha Duggal, N.; Arora, J. Treatment paradox in musculo-skeletal tuberculosis in an immunocompetent adult male; a case report from a tertiary care hospital. J. Clin. Diagn. Res. 2015, 9, DD01–DD02. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Breen, R.A.; Smith, C.J.; Bettinson, H.; Dart, S.; Bannister, B.; Johnson, M.A.; Lipman, M.C. Paradoxical reactions during tuberculosis treatment in patients with and without HIV co-infection. Thorax 2004, 59, 704–707. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rai, D.K.; Kant, S.; Gupta, V.B. Paradoxical reaction in peripheral lymph node tuberculosis: A review for its prevalence, clinical characteristics, and possible treatment. Monaldi Arch. Chest Dis. 2023, 94, 2625. [Google Scholar] [CrossRef] [PubMed]
- Carazo Gallego, B.; Moreno-Pérez, D.; Nuñez Cuadros, E.; Mesa Fernandez, A.; Martin Cantero, M.; Obando Pacheco, P.; Urda Cardona, A. Paradoxical reaction in immunocompetent children with tuberculosis. Int. J. Infect. Dis. 2016, 51, 15–18. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santilli, L.; Canovari, B.; Balducci, M.; Ginevri, F.; Maracci, M.; Polenta, A.; Anzalone, N.; Franca, L.; Mariotti, B.; Sterza, L.; et al. The Appearance of Osteomyelitis of the Foot and Disseminated Subcutaneous Abscesses During Treatment for Disseminated Tuberculosis Infection in an Immunocompetent Patient: Case Presentation of a Paradoxical Reaction and Literature Review. Infect. Dis. Rep. 2025, 17, 46. https://doi.org/10.3390/idr17030046
Santilli L, Canovari B, Balducci M, Ginevri F, Maracci M, Polenta A, Anzalone N, Franca L, Mariotti B, Sterza L, et al. The Appearance of Osteomyelitis of the Foot and Disseminated Subcutaneous Abscesses During Treatment for Disseminated Tuberculosis Infection in an Immunocompetent Patient: Case Presentation of a Paradoxical Reaction and Literature Review. Infectious Disease Reports. 2025; 17(3):46. https://doi.org/10.3390/idr17030046
Chicago/Turabian StyleSantilli, Luca, Benedetta Canovari, Maria Balducci, Francesco Ginevri, Monia Maracci, Antonio Polenta, Norma Anzalone, Lucia Franca, Beatrice Mariotti, Lucia Sterza, and et al. 2025. "The Appearance of Osteomyelitis of the Foot and Disseminated Subcutaneous Abscesses During Treatment for Disseminated Tuberculosis Infection in an Immunocompetent Patient: Case Presentation of a Paradoxical Reaction and Literature Review" Infectious Disease Reports 17, no. 3: 46. https://doi.org/10.3390/idr17030046
APA StyleSantilli, L., Canovari, B., Balducci, M., Ginevri, F., Maracci, M., Polenta, A., Anzalone, N., Franca, L., Mariotti, B., Sterza, L., & Barchiesi, F. (2025). The Appearance of Osteomyelitis of the Foot and Disseminated Subcutaneous Abscesses During Treatment for Disseminated Tuberculosis Infection in an Immunocompetent Patient: Case Presentation of a Paradoxical Reaction and Literature Review. Infectious Disease Reports, 17(3), 46. https://doi.org/10.3390/idr17030046




