Health-Related Quality of Life (HRQoL) of Patients with Tuberculosis: A Review
Abstract
1. Introduction
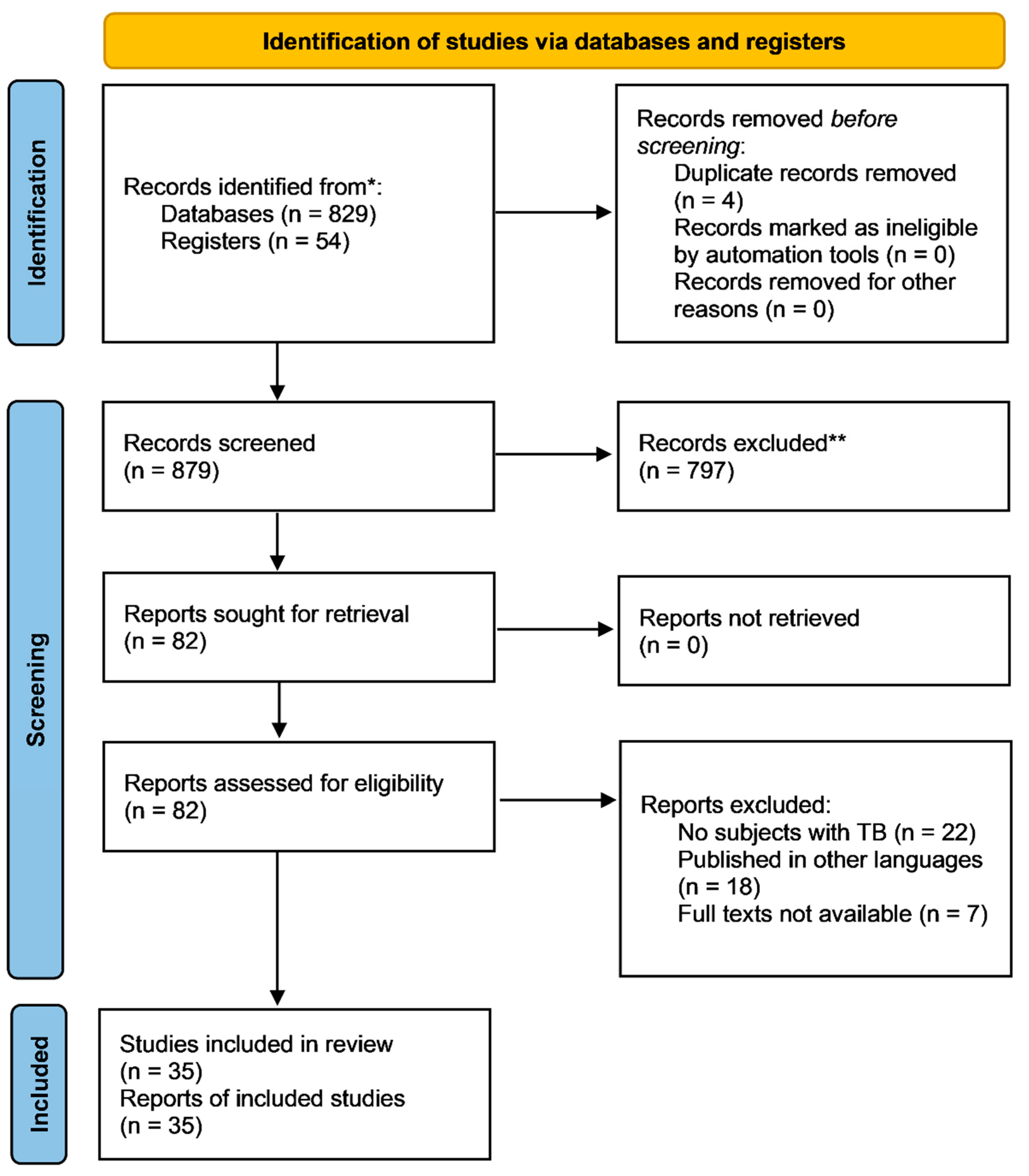
2. Methodology
3. Findings
3.1. Instruments for Describing and Quantifying QoL in TB
3.2. Factors Associated with HRQoL in TB
3.2.1. Active and Latent Tuberculosis (LTBI)
3.2.2. Socio-Demographic (Age, Gender, and Others) and Socio-Economic (Income, Education, Housing, Social Security) Status
3.2.3. QoL in Tuberculosis with HIV Co-Infection
3.2.4. QoL in Tuberculosis with Other Comorbidities
3.3. QoL during and after Treatment
| Study ID (Country) | Study Design | Participants | QoL Instrument Used | QoL Domain Assessed | Findings |
|---|---|---|---|---|---|
| Kastien-Hilka et al., 2016 (South Africa) [80] | Systematic review | TB patients | 1. WHOQOL-BREF2. SGRQ 3. SF-36 4. EQ-5D E 5. BDI 6. STAI-6 7. CES-D | 1. Physical 2. Mental 3. Social health | Although ATT improved all HRQoL domains, the psycho-social domain remained impaired after treatment |
| Bauer et al., 2015 (Canada) [5] | Longitudinal cohort study | 1. TB 2. LTBI 3. Control participants | SF-36 | 1. Physical component summary 2. Mental component summary | TB patients have lower HRQoL scores; Higher decrements in HRQoL are observed soon after starting ATT but improve after two months of ATT |
| Atif et al., 2014 (Malaysia) [19] | Longitudinal study | New smear-positive PTB patients | SF-36 | 1. Physical 2. Mental health | Compromised mental and physical health was observed among TB patients even after the completion of treatment |
| Chung and Li, 2013 [79] | Prospective cohort study | TB patients undergoing treatment | WHOQOL-BREF | 1. Physical 2. Mental 3. Social 4. Environmental | TB affects HRQoL despite effective treatment |
| Aggarwal et al., 2013 (India) [36] | Cohort study | Newly diagnosed PTB patients starting treatment (RNTCP) | WHOQOL-BREF | 1. Physical 2. Psychological 3. Social relationships 4. Environment | For patients treated by the RNTCP, HRQoL assessment may be used as an adjunct outcome measure |
| Ralph et al., 2013 (Indonesia) [55] | Clinical trial | 1. Smear-positive TB 2. Healthy control | SGRQ Indonesian version | 1. Symptoms component 2. Impact components (social functioning, psychological disturbances resulting from airways disease) | PTB treatment can reduce symptoms, improve functional capacity, and improve QoL |
| Balgude and Sontakke, 2012 [51] | NA | 1. Newly diagnosed pulmonary TB 2. Healthy control | WHOQOL-BREF | 1. Physical health 2. Psychological health 3. Social relationships 4. Environment | Even after ATT, physical and psychological domains remain lower in TB patients than in controls |
| Awaisu et al., 2012 (Malaysia) [50] | Multi-centered non-randomized controlled study | 1. TB-DOTS plus SCI 2. TB-DOTS only | 1. EQ-5D 2. EQ-VAS | 1. Mobility 2. Self-care, 3. Pain or discomfort 4. Anxiety or depression | An integrated TB-tobacco treatment strategy can improve HRQoL among smoker TB patients |
| Guo et al., 2010 (Canada) [22] | Longitudinal study | 1. Active TB patients 2. LTBI patients | SF-36 | 1. PCS 2. Mental component summary (MCS) | Improvements in the baseline HRQoL of high-risk patients can support the outcome of medical treatment |
| Kruijshaar et al., 2010 (UK) [24] | NA | TB patients | SF-36 v2UK versionEQ-5DSTAI-6 CES-D | 1. Physical and general health 2. Vitality and mental health. 3. Anxiety and depression | ATT improved HRQoL but were lower than normal people. |
| Guo et al., 2009 [6] | Systematic review | TB patients | 1. SF-36 2. GQOLI-74 3. QLQ 4. SGRQ 5. SSRS 6. BDQ | 1. PCS 2. MCS | TB has impact on patients’ QoL even after treatment |
| Marra et al., 2008 [11] | NA | 1. Active TB patients 2. LTBI patients | SF-36 v2BDI | 1. Physical 2. Mental 3. Social 4. Emotional | Active TB patients showed improvements in most HRQoL domains |
| Muniyandi et al., 2007 | NA | (TB) patients one year after treatment completion. | SF-36 | 1. Physical 2. Mental 3. Social well-being | HRQoL of TB patients after one year of completion of ATT was normal |
| Pasipanodya et al., 2007b (United States) [86] | NA | PTB or latent tuberculosis infection (LTBI) | SGRQ | 1. Symptoms component 2. Impact components (social functioning, psychological disturbances resulting from airways disease) | PTB has a substantial impact on human health, thus affecting QoL |
| Dion et al., 2004 (Canada) [16] | Cross-sectional study | Pulmonary tuberculosis (PTB) | SF-36v2 SF- 12v2 | 1. PCS 2. MCS | Most cured TB patients have compromised HRQoL |
4. Discussion
4.1. Study Limitations
4.2. Implications for Policy, Practice, and Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- World Health Organization. Ministry of Health of the Russian Federation Moscow Declaration to End TB. First WHO Global Ministerial Conference on Ending TB in the Sustainable Development Era: A Multisectoral Response; Geneva, Switzerland. 2017. Available online: https://www.who.int/tb/features_archive/Moscow_Declaration_to_End_TB_final_ENGLISH.pdf (accessed on 20 March 2021).
- World Health Organization. Global Tuberculosis Report 2018; WHO: Geneva, Switzerland, 2018.
- World Health Organization. Global Tuberculosis Report 2020; WHO: Geneva, Switzerland, 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/336069/9789240013131-eng.pdf (accessed on 1 April 2021).
- Banerjee, S.; Bandyopadhyay, K.; Taraphdar, P.; Dasgupta, A. Effect of DOTS on quality of life among tuberculosis patients: A follow-up study in a health district of Kolkata. J. Family Med. Prim. Care 2019, 8, 1070–1075. [Google Scholar] [PubMed]
- Bauer, M.; Ahmed, S.; Benedetti, A.; Greenaway, C.; Lalli, M.; Leavens, A.; Menzies, D.; Vadeboncoeur, C.; Vissandjée, B.; Wynne, A.; et al. Health-related quality of life and tuberculosis: A longitudinal cohort study. Health Qual. Life Outcomes 2015, 13, 65. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.; Marra, F.; Marra, C.A. Measuring health-related quality of life in tuberculosis: A systematic review. Health Qual. Life Outcomes 2009, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.; Leavens, A.; Schwartzman, K. A systematic review and meta-analysis of the impact of tuberculosis on health-related quality of life. Qual. Life Res. 2013, 22, 2213–2235. [Google Scholar] [CrossRef] [PubMed]
- Olufemi, A.O.; Chikaodinaka, A.A.; Abimbola, P.; Oluwatoyin, A.T.; Oluwafunmilola, A.; Fasanmi, K.T.; Efosa, E.G. Health-Related Quality of Life (HRQoL) scores vary with treatment and may identify potential defaulters during treatment of tuberculosis. Malawi Med. J. 2018, 30, 283–290. [Google Scholar]
- WHO The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [CrossRef]
- Munro, S.A.; Lewin, S.A.; Smith, H.J.; Engel, M.E.; Fretheim, A.; Volmink, J. Patient adherence to tuberculosis treatment: A systematic review of qualitative research. PLoS Med. 2007, 4, e238. [Google Scholar] [CrossRef]
- Marra, C.A.; Marra, F.; Colley, L.; Moadebi, S.; Elwood, R.K.; Fitzgerald, J.M. Health-related quality of life trajectories among adults with tuberculosis: Differences between latent and active infection. Chest 2008, 133, 396–403. [Google Scholar] [CrossRef]
- Chang, B.; Wu, A.W.; Hansel, N.N.; Diette, G.B. Quality of life in tuberculosis: A review of the English language literature. Qual. Life Res. 2004, 13, 1633–1642. [Google Scholar] [CrossRef]
- Brown, J.; Capocci, S.; Smith, C.; Morris, S.; Abubakar, I.; Lipman, M. Health status and quality of life in tuberculosis. Int. J. Infect. Dis 2015, 32, 68–75. [Google Scholar] [CrossRef]
- Khan, S.; Tangiisuran, B.; Imtiaz, A.; Zainal, H. Health status and quality of life in tuberculosis: Systematic review of study design, instruments, measuring properties and outcomes. Health Sci. J. 2017, 11. Available online: http://www.hsj.gr/medicine/health-status-and-quality-of-life-in-tuberculosis-systematic-review-of-study-design-instruments-measuring-properties-and-outcomes.php?aid=18409 (accessed on 5 April 2021). [CrossRef]
- Chamla, D. The assessment of patients’ health-related quality of life during tuberculosis treatment in Wuhan, China. Int. J. Tuberc. Lung Dis. 2004, 8, 1100–1106. [Google Scholar] [PubMed]
- Dion, M.J.; Tousignant, P.; Bourbeau, J.; Menzies, D.; Schwartzman, K. Feasibility and reliability of health-related quality of life measurements among tuberculosis patients. Qual. Life Res. 2004, 13, 653–665. [Google Scholar] [CrossRef] [PubMed]
- Rajeswari, R.; Muniyandi, M.; Balasubramanian, R.; Narayanan, P.R. Perceptions of tuberculosis patients about their physical, mental and social well-being: A field report from South India. Soc. Sci. Med. 2005, 60, 1845–1853. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0277953604004071 (accessed on 5 April 2021). [CrossRef]
- Ahmad, N.; Javaid, A.; Syed Sulaiman, S.A.; Basit, A.; Afridi, A.K.; Jaber, A.A.S.; Khan, A.H. Effects of multidrug resistant tuberculosis treatment on patients’ health related quality of life: Results from a follow up study. PLoS ONE 2016, 11, e0159560. [Google Scholar] [CrossRef]
- Atif, M.; Sulaiman, S.A.S.; Shafie, A.A.; Asif, M.; Sarfraz, M.K.; Low, H.C.; Babar, Z.-U.-D. Impact of tuberculosis treatment on health-related quality of life of pulmonary tuberculosis patients: A follow-up study. Health Qual. Life Outcomes 2014, 12, 19. [Google Scholar] [CrossRef]
- Dos Santos, A.P.C.; Lazzari, T.K.; Silva, D.R. Health-related quality of life, depression and anxiety in hospitalized patients with Tuberculosis. Tuberc. Respir. Dis. 2017, 80, 69–76. [Google Scholar] [CrossRef]
- Guo, N.; Marra, C.A.; Marra, F.; Moadebi, S.; Elwood, R.K.; FitzGerald, J.M. Health State Utilities in Latent and Active Tuberculosis. Value Health 2008, 11, 1154–1161. Available online: https://linkinghub.elsevier.com/retrieve/pii/S1098301510605979 (accessed on 10 April 2021). [CrossRef]
- Guo, N.; Marra, F.; Fitzgerald, J.M.; Elwood, R.K.; Marra, C.A. Impact of adverse drug reaction and predictivity of quality of life status in tuberculosis. Eur. Respir. J. 2010, 36, 206–208. [Google Scholar] [CrossRef]
- Jaber, A.A.S.; Khan, A.H.; Syed Sulaiman, S.A.; Ahmad, N.; Anaam, M.S. Evaluation of health-related quality of life among tuberculosis patients in two cities in Yemen. PLoS ONE 2016, 11, e0156258. [Google Scholar] [CrossRef]
- Kruijshaar, M.E.; Lipman, M.; Essink-Bot, M.-L.; Lozewicz, S.; Creer, D.; Dart, S.; Maguire, H.; Abubakar, I. Health status of UK patients with active tuberculosis. Int. J. Tuberc. Lung Dis. 2010, 14, 296–302. [Google Scholar] [PubMed]
- Kisaka, S.M.B.; Rutebemberwa, E.; Kasasa, S.; Ocen, F.; Nankya-Mutyoba, J. Does health-related quality of life among adults with pulmonary tuberculosis improve across the treatment period? A hospital-based cross sectional study in Mbale Region, Eastern Uganda. BMC Res. Notes 2016, 9, 467. [Google Scholar] [CrossRef] [PubMed]
- Roba, A.A.; Dasa, T.T.; Weldegebreal, F.; Asfaw, A.; Mitiku, H.; Teklemariam, Z.; Naganuri, M.; Geddugol, B.J.; Mesfin, F.; Befikadu, H.; et al. Tuberculosis patients are physically challenged and socially isolated: A mixed methods case-control study of health related quality of life in Eastern Ethiopia. PLoS ONE 2018, 13, e0204697. [Google Scholar] [CrossRef] [PubMed]
- Shahdadi, H.; Salarzaee, M.; Balouchi, A. Quality of life of diabetic patients with smear positive PTB in southeastern Iran: A cross-sectional study in a poor region of Iran. Indian J. Tuberc. 2018, 65, 159–163. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0019570717301385 (accessed on 25 May 2021). [CrossRef]
- Sineke, T.; Evans, D.; Schnippel, K.; van Aswegen, H.; Berhanu, R.; Musakwa, N.; Lönnmark, E.; Long, L.; Rosen, S. The impact of adverse events on health-related quality of life among patients receiving treatment for drug-resistant tuberculosis in Johannesburg, South Africa. Health Qual. Life Outcomes 2019, 17, 94. [Google Scholar] [CrossRef]
- Ramkumar, S.; Vijayalakshmi, S.; Seetharaman, N.; Pajanivel, R.; Lokeshmaran, A. Health-related quality of life among tuberculosis patients under revised national tuberculosis control programme in rural and urban Puducherry. Indian J. Tuberc. 2017, 64, 14–19. [Google Scholar] [CrossRef]
- Unalan, D.; Soyuer, F.; Ozturk, A. Comparison of SF-36 and WHOQOL-100 life quality scales in early period tuberculosis subjects. J. Pak. Med. Assoc. 2012, 62, 1161–1167. [Google Scholar]
- Unalan, D.; Soyuer, F.; Ceyhan, O.; Basturk, M.; Ozturk, A. Is the quality of life different in patients with active and inactive tuberculosis? Indian J. Tuberc. 2008, 55, 127–137. [Google Scholar]
- Jørstad, M.D.; Aẞmus, J.; Marijani, M.; Sviland, L.; Mustafa, T. Diagnostic delay in extrapulmonary tuberculosis and impact on patient morbidity: A study from Zanzibar. PLoS ONE 2018, 13, e0203593. [Google Scholar] [CrossRef]
- Kastien-Hilka, T.; Rosenkranz, B.; Sinanovic, E.; Bennett, B.; Schwenkglenks, M. Health-related quality of life in South African patients with pulmonary tuberculosis. PLoS ONE 2017, 12, e0174605. [Google Scholar] [CrossRef]
- Kittikraisak, W.; Kingkaew, P.; Teerawattananon, Y.; Yothasamut, J.; Natesuwan, S.; Manosuthi, W.; Chongsuvivatwong, V.; Whitehead, S.J. Health related quality of life among patients with tuberculosis and HIV in Thailand. PLoS ONE 2012, 7, e29775. [Google Scholar] [CrossRef] [PubMed]
- Saleem, S.; Malik, A.A.; Ghulam, A.; Ahmed, J.; Hussain, H. Health-related quality of life among pulmonary tuberculosis patients in Pakistan. Qual. Life Res. 2018, 27, 3137–3143. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.N.; Gupta, D.; Janmeja, A.K.; Jindal, S.K. Assessment of health-related quality of life in patients with pulmonary tuberculosis under programme conditions. Int. J. Tuberc. Lung Dis. 2013, 17, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.-S.; Lan, Y.-L.; Yang, M.-C. Psychometric testing of the short version of the world health organization quality of life (WHOQOL-BREF) questionnaire among pulmonary tuberculosis patients in Taiwan. BMC Public Health 2012, 12, 630. [Google Scholar] [CrossRef] [PubMed]
- Dar, S.A.; Shah, N.N.; Wani, Z.A.; Nazir, D. A prospective study on quality of life in patients with pulmonary tuberculosis at a tertiary care hospital in Kashmir, Northern India. Indian J. Tuberc. 2019, 66, 118–122. [Google Scholar] [CrossRef]
- Sharma, R.; Yadav, R.; Sharma, M.; Saini, V.; Koushal, V. Quality of life of multi drug resistant tuberculosis patients: A study of north India. Acta Med. Iran. 2014, 52, 448–453. [Google Scholar]
- Dhuria, M.; Sharma, N.; Singh, N.P.; Jiloha, R.C.; Saha, R.; Ingle, G.K. A study of the impact of tuberculosis on the quality of life and the effect after treatment with DOTS. Asia Pac. J. Public Health 2009, 21, 312–320. [Google Scholar] [CrossRef]
- Laxmeshwar, C.; Stewart, A.G.; Dalal, A.; Kumar, A.M.V.; Kalaiselvi, S.; Das, M.; Gawde, N.; Thi, S.S.; Isaakidis, P. Beyond “cure” and “treatment success”: Quality of life of patients with multidrug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 2019, 23, 73–81. [Google Scholar] [CrossRef]
- Singh, S.K.; Agrawal, A.; Tiwari, K.K. Improvement in quality of life in pulmonary tuberculosis patients: A prospective study. Trop. Dr. 2017, 47, 97–100. [Google Scholar] [CrossRef]
- Dhuria, M.; Sharma, N.; Ingle, G. Impact of tuberculosis on the quality of life. Indian J. Community Med. 2008, 33, 58–59. [Google Scholar] [CrossRef]
- Hansel, N.N.; Wu, A.W.; Chang, B.; Diette, G.B. Quality of life in tuberculosis: Patient and provider perspectives. Qual. Life Res. 2004, 13, 639–652. [Google Scholar] [CrossRef] [PubMed]
- Kastien-Hilka, T.; Rosenkranz, B.; Bennett, B.; Sinanovic, E.; Schwenkglenks, M. How to evaluate health-related quality of life and its association with medication adherence in pulmonary tuberculosis—Designing a prospective observational study in South Africa. Front. Pharmacol. 2016, 7, 125. [Google Scholar] [CrossRef]
- Masumoto, S.; Yamamoto, T.; Ohkado, A.; Yoshimatsu, S.; Querri, A.G.; Kamiya, Y. Factors associated with health-related quality of life among pulmonary tuberculosis patients in Manila, the Philippines. Qual. Life Res. 2014, 23, 1523–1533. [Google Scholar] [CrossRef] [PubMed]
- Peddireddy, V. Quality of life, psychological interventions and treatment outcome in tuberculosis patients: The Indian Scenario. Front. Psychol. 2016, 7, 1664. [Google Scholar] [CrossRef] [PubMed]
- Adeyeye, O.O.; Ogunleye, O.O.; Coker, A.; Kuyinu, Y.; Bamisile, R.T.; Ekrikpo, U.; Onadeko, B. Factors influencing quality of life and predictors of low quality of life scores in patients on treatment for pulmonary tuberculosis: A cross sectional study. J. Public Health Afr. 2014, 5, 366. [Google Scholar] [CrossRef]
- Aggarwal, A.N. Health-related quality of life: A neglected aspect of pulmonary tuberculosis. Lung India 2010, 27, 1–3. [Google Scholar] [CrossRef]
- Awaisu, A.; Haniki Nik Mohamed, M.; Noordin, N.M.; Muttalif, A.R.; Aziz, N.A.; Syed Sulaiman, S.A.; Mahayiddin, A.A. Impact of connecting tuberculosis directly observed therapy short-course with smoking cessation on health-related quality of life. Tob. Induc. Dis. 2012, 10, 2. [Google Scholar] [CrossRef]
- Balgude, A.; Sontakke, S. Study of impact of antitubercular therapy on quality of life. Indian J. Med. Sci. 2012, 66, 71–77. [Google Scholar]
- Deribew, A.; Deribe, K.; Reda, A.A.; Tesfaye, M.; Hailmichael, Y.; Maja, T.; Colebunders, R. Change in quality of life: A follow up study among patients with HIV infection with and without TB in Ethiopia. BMC Public Health 2013, 13, 408. [Google Scholar] [CrossRef]
- Dias, A.A.L.; de Oliveira, D.M.F.; Turato, E.R.; de Figueiredo, R.M. Life experiences of patients who have completed tuberculosis treatment: A qualitative investigation in southeast Brazil. BMC Public Health 2013, 13, 595. [Google Scholar] [CrossRef]
- Louw, J.; Peltzer, K.; Naidoo, P.; Matseke, G.; Mchunu, G.; Tutshana, B. Quality of life among tuberculosis (TB), TB retreatment and/or TB-HIV co-infected primary public health care patients in three districts in South Africa. Health Qual. Life Outcomes 2012, 10, 77. [Google Scholar] [CrossRef] [PubMed]
- Ralph, A.P.; Kenangalem, E.; Waramori, G.; Pontororing, G.J.; Tjitra, E.; Maguire, G.P.; Kelly, P.M.; Anstey, N.M. High morbidity during treatment and residual pulmonary disability in pulmonary tuberculosis: Under-recognised phenomena. PLoS ONE 2013, 8, e80302. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, V.K.; Rajpal, S. Health related quality of life (HRQL) scoring (DR-12 score) in tuberculosis--additional evaluative tool under DOTS. J. Commun. Dis. 2005, 37, 261–268. [Google Scholar] [PubMed]
- Dion, M.-J.; Tousignant, P.; Bourbeau, J.; Menzies, D.; Schwartzman, K. Measurement of health preferences among patients with tuberculous infection and disease. Med. Decis. Making 2002, 22, S102–S114. [Google Scholar] [CrossRef]
- Marra, C.A.; Marra, F.; Cox, V.C.; Palepu, A.; Fitzgerald, J.M. Factors influencing quality of life in patients with active tuberculosis. Health Qual. Life Outcomes 2004, 2, 58. [Google Scholar] [CrossRef]
- Shedrawy, J.; Jansson, L.; Röhl, I.; Kulane, A.; Bruchfeld, J.; Lönnroth, K. Quality of life of patients on treatment for latent tuberculosis infection: A mixed-method study in Stockholm, Sweden. Health Qual. Life Outcomes 2019, 17, 158. [Google Scholar] [CrossRef]
- Wang, Y.; Lii, J.; Lu, F. Measuring and assessing the quality of life of patients with pulmonary tuberculosis. Zhonghua Jie He He Hu Xi Za Zhi 1998, 21, 720–723. [Google Scholar]
- Shedrawy, J.; Jansson, L.; Bruchfeld, J.; Lönnroth, K. Health-related quality of life among persons treated for tuberculosis in a European setting. Int. J. Tuberc. Lung Dis. 2020, 24, 461–463. [Google Scholar] [CrossRef]
- Duyan, V.; Kurt, B.; Aktas, Z.; Duyan, G.C.; Kulkul, D.O. Relationship between quality of life and characteristics of patients hospitalised with tuberculosis. Int. J. Tuberc. Lung Dis. 2005, 9, 1361–1366. [Google Scholar]
- Jankowska-Polanska, B.K.; Kamińska, M.; Uchmanowicz, I.; Rycombel, A. Quality of life and health behaviours of patients with tuberculosis—Sex differences. Pneumonol. Alergol. Pol. 2015, 83, 256–265. [Google Scholar] [CrossRef]
- Louw, J.S.; Mabaso, M.; Peltzer, K. Change in health-related quality of life among pulmonary tuberculosis patients at primary health care settings in South Africa: A prospective cohort study. PLoS ONE 2016, 11, e0151892. [Google Scholar] [CrossRef]
- Miller, T.L.; McNabb, S.J.N.; Hilsenrath, P.; Pasipanodya, J.; Weis, S.E. Personal and societal health quality lost to tuberculosis. PLoS ONE 2009, 4, e5080. [Google Scholar] [CrossRef] [PubMed]
- Pasipanodya, J.G.; Miller, T.L.; Vecino, M.; Munguia, G.; Bae, S.; Drewyer, G.; Weis, S.E. Using the St. George respiratory questionnaire to ascertain health quality in persons with treated pulmonary tuberculosis. Chest 2007, 132, 1591–1598. [Google Scholar] [CrossRef] [PubMed]
- Rajeswari, R.; Balasubramanian, R.; Muniyandi, M.; Geetharamani, S.; Thresa, X.; Venkatesan, P. Socio-economic impact of tuberculosis on patients and family in India. Int. J. Tuberc. Lung Dis. 1999, 3, 869–877. [Google Scholar] [PubMed]
- Deribew, A.; Tesfaye, M.; Hailmichael, Y.; Negussu, N.; Daba, S.; Wogi, A.; Belachew, T.; Apers, L.; Colebunders, R. Tuberculosis and HIV co-infection: Its impact on quality of life. Health Qual. Life Outcomes 2009, 7, 105. [Google Scholar] [CrossRef]
- Dowdy, D.W.; Israel, G.; Vellozo, V.; Saraceni, V.; Cohn, S.; Cavalcante, S.; Chaisson, R.E.; Golub, J.E.; Durovni, B. Quality of life among people treated for tuberculosis and human immunodeficiency virus in Rio de Janeiro, Brazil. Int. J. Tuberc. Lung Dis. 2013, 17, 345–347. [Google Scholar] [CrossRef]
- Hailu, T.; Yitayal, M.; Yazachew, L. Health-related quality of life and associated factors among adult HIV mono-infected and TB/HIV co-infected patients in public health facilities in Northeast Ethiopia: A comparative cross-sectional study. Patient Prefer. Adherence 2020, 14, 1873–1887. [Google Scholar] [CrossRef]
- Jha, D.K.; Jha, J.; Jha, A.K.; Achappa, B.; Holla, R. Quality of life among HIV-tuberculosis co-infected patients. Perspect. Clin. Res. 2019, 10, 125–129. [Google Scholar] [CrossRef]
- Mthiyane, T.; Pym, A.; Dheda, K.; Rustomjee, R.; Reddy, T.; Manie, S. Longitudinal assessment of health related quality of life of HIV infected patients treated for tuberculosis and HIV in a high burden setting. Qual. Life Res. 2016, 25, 3067–3076. [Google Scholar] [CrossRef]
- de Souza Neves, L.A.; Canini, S.R.M.; Reis, R.K.; Santos, C.B.D.; Gir, E. Aids and tuberculosis: Coinfection from the perspective of the quality of life of patients. Evista Esc. Enferm. USP 2012, 46, 704–710. [Google Scholar]
- Opollo, V.; Sun, X.; Lando, R.; Miyahara, S.; Torres, T.S.; Hosseinipour, M.C.; Bisson, G.P.; Kumwenda, J.; Gupta, A.; Nyirenda, M.; et al. The effect of TB treatment on health-related quality of life for people with advanced HIV. Int. J. Tuberc. Lung Dis. 2020, 24, 910–915. [Google Scholar] [CrossRef] [PubMed]
- Babikako, H.M.; Neuhauser, D.; Katamba, A.; Mupere, E. Feasibility, reliability and validity of health-related quality of life questionnaire among adult pulmonary tuberculosis patients in urban Uganda: Cross-sectional study. Health Qual. Life Outcomes 2010, 8, 93. [Google Scholar] [CrossRef]
- Edwards, T.; White, L.V.; Lee, N.; Castro, M.C.; Saludar, N.R.; Faguer, B.N.; Fuente, N.D.; Mayoga, F.; Ariyoshi, K.; Garfin, A.M.C.G.; et al. Effects of comorbidities on quality of life in Filipino people with tuberculosis. Int. J. Tuberc. Lung Dis. 2020, 24, 712–719. [Google Scholar] [CrossRef]
- Yeung, M.W.; Khoo, E.; Brode, S.K.; Jamieson, F.B.; Kamiya, H.; Kwong, J.C.; Macdonald, L.; Marras, T.K.; Morimoto, K.; Sander, B. Health-related quality of life, comorbidities and mortality in pulmonary nontuberculous mycobacterial infections: A systematic review. Respirology 2016, 21, 1015–1025. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.N. Quality of life with tuberculosis. J. Clin. Tuberc. Other Mycobact. Dis. 2019, 17, 100121. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.-S.; Li, C.-R. Can DOTS improve quality of life among patients with pulmonary tuberculosis? Int. J. Tuberc. Lung Dis. 2013, 17, 425–426. [Google Scholar] [CrossRef]
- Kastien-Hilka, T.; Abulfathi, A.; Rosenkranz, B.; Bennett, B.; Schwenkglenks, M.; Sinanovic, E. Health-related quality of life and its association with medication adherence in active pulmonary tuberculosis—A systematic review of global literature with focus on South Africa. Health Qual. Life Outcomes 2016, 14, 42. [Google Scholar] [CrossRef]
- Datta, S.; Gilman, R.H.; Montoya, R.; Quevedo Cruz, L.; Valencia, T.; Huff, D.; Saunders, M.J.; Evans, C.A. Quality of life, tuberculosis and treatment outcome; a case-control and nested cohort study. Eur. Respir. J. 2020, 56, 1900495. [Google Scholar] [CrossRef]
- Salehitali, S.; Noorian, K.; Hafizi, M.; Dehkordi, A.H. Quality of life and its effective factors in tuberculosis patients receiving directly observed treatment short-course (DOTS). J. Clin. Tuberc. Other Mycobact. Dis. 2019, 15, 100093. [Google Scholar] [CrossRef]
- Valadares, R.M.C.; da Silva Carvalho, W.; de Miranda, S.S. Association of adverse drug reaction to anti-tuberculosis medication with quality of life in patients in a tertiary referral hospital. Rev. Soc. Bras. Med. Trop. 2019, 53, e20190207. [Google Scholar] [CrossRef]
- Alene, K.A.; Clements, A.C.A.; McBryde, E.S.; Jaramillo, E.; Lönnroth, K.; Shaweno, D.; Gulliver, A.; Viney, K. Mental health disorders, social stressors, and health-related quality of life in patients with multidrug-resistant tuberculosis: A systematic review and meta-analysis. J. Infect. 2018, 77, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Vo, N.X.; Xuan Doan, T.B.; Kha Vo, D.N.; Tran, T.K.; Vo, T.Q. Assessing quality of life for multidrug-resistant and extensively drug-resistant tuberculosis patients. J. Pak. Med. Assoc. 2019, 69 (Suppl. 2), S137–S157. [Google Scholar] [PubMed]
- Pasipanodya, J.G.; Miller, T.L.; Vecino, M.; Munguia, G.; Garmon, R.; Bae, S.; Drewyer, G.; Weis, S.E. Pulmonary impairment after tuberculosis. Chest 2007, 131, 1817–1824. [Google Scholar] [CrossRef] [PubMed]
- Atif, M.; Toghrayee, Z.; Sulaiman, S.S.; Shafie, A.A.; Low, H.C.; Babar, Z.U.D. Missing data analysis in longitudinal studies: Findings from a quality of life study in Malaysian Tuberculosis Patients. Value Health 2014, 17, A778. [Google Scholar] [CrossRef][Green Version]
| Study ID (Country) | Study Design | Participants | QoL Instrument Used | QoL Domain Assessed | Findings |
|---|---|---|---|---|---|
| Shedrawy et al., 2019 (Sweden) [59] | Cross-sectional study | LTBI | 1. EQ-5D-3 L 2. RHS-15 | 1. Physical, 2. Psycho-social 3. Pain | No HRQoL decrements were detected in LTBI patients |
| Bauer et al., 2015 (Canada) [5] | Longitudinal cohort study | 1. Diagnosed and treated for TB disease 2. LTBI 3. Persons screened but not treated for TB disease or LTBI | SF-36 | Eight domain scores and mental and physical component summary | HRQoL decrements detected in TB patients |
| Bauer et al., 2013 [7] | Systematic review and meta-analysis | 1. Active TB 2. LTBI 3. Healthy controls treatment | 1. SF-36 2. GHQ–12 3. HAD 4. MACL 5. SIP 6. SRI (BDI) 7. EQ 5D 8. WHOQOL-BREF 9. WHOQOL-HIV | 1. Physical 2. Psychological 3. Social 4. Environment | Poorer HRQoL was reported in subjects with active TB than in persons treated for LTBI |
| Kruijshaar et al., 2010 (UK) [24] | Prospective study | Pulmonary TB patients | 1. SF-36 2. EQ-5D | 1. Physical 2. Psychological | TB patients had diminished HRQoL scores |
| Guo et al., 2009 [6] | Systematic review and meta-analysis | 1. Active TB 2. LTBI, regardless of the treatment status | 1. SF 36 2. HUI, 3. EQ-5D 4. VAS 5. QLQ 6. GHQ-12 7. BDQ 8. SSRS | 1. Physical 2. Mental 3. Social well-being 4. Functioning | 1. HRQoL decrements in TB patients 2. Among patients in both active and LTBI, mental well-being was more severely disrupted than physical health |
| Marra et al., 2008 [11] | NA | 1. Active TB 2. LTBI | 1. SF-36 2. DI | 1. Physical component summary 2. Mental component summary 3. Depression | HRQoL decrements detected at the completion of therapy in TB patients |
| Unalan et al., 2008 [31] | NA | 1. Active TB 2. Inactive tuberculosis | 1. SF 36 2. BDI | 1. Physical component summary (PCS) 2. Mental component summary 3. Social functionality | QoL decrements detected in active TB patients |
| Guo et al., 2008 (Canada) [21] | NA | 1. Active TB 2. LTBI | 1. SF-36 2. HUI2/3 3. VAS | Eight domain scores | For active TB and LTBI, health state utility values did not generate identical utility scores |
| Marra et al., 2004 (Canada) [58] | Multi-site study | Active TB patients | Focus groups and individual interviews | 1. Physical functioning and 2. Emotional/mental well-being | QoL decrements detected in active TB patients |
| Dion et al., 2002 (Canada) [57] | NR | 1. Active TB 2. Previous active TB patients | 1. VAS 2. Standard gamble (SG) | 1. Physical component summary (PCS) 2. Mental component summary (MCS) | QoL decrements detected in active TB patients |
| Study ID (Country) | Study Design | Participants | QoL Instrument Used | QoL Domain Assessed | Findings |
|---|---|---|---|---|---|
| Opollo et al., 2020 (Brazil, Haiti, India, Kenya, Malawi, Peru, South Africa, Uganda, Zambia, and Zimbabwe) [74] | Open-label trial | TB patient with advanced HIV infection | Questionnaire | 1. Psycho- logical 2. Economic 3. Socio-cultural 4. Spiritual | HRQoL was found to improve over time, with no difference between arms |
| Hailu et al., 2020 (Ethiopia) [70] | Cross-sectional study | 1. HIV mono-infected 2. TB and HIV co-infected patients | WHOQOL-HIV-BREF | 1. Physical 2. Psychological 3. Level of independence 4. Social relationships 5. Environmental 6. Spiritual health | Poor HRQoL reported in TB/HIV co-infected patients in all domains compared with HIV mono-infected patients |
| Jha et al., 2019 (India) [71] | Cross-sectional study | 1. HIV-TB co-infected patients 2. HIV patients | 1. WHOQOL-HIV BREF 2. Beck’s Depression Inventory Scale | 1. Physical health 2. Psychological well-being 3. Social relationship 4. Environmental health 5. Level of independence 6. Spiritual health | HIV-TB co-infected patients had a poorer QoL than only HIV patients |
| Mthiyane et al., 2016 (South Africa) [72] | Longitudinal study | HIV-TB co-infected patients | FAHI | 1. Physical well-being 2. Functional 3. Global well-being 4. Emotional well-being 5. Cognitive functioning | Improvement in QoL consistent with a decrease in adverse events and signs and symptoms of TB |
| Deribew et al., 2013 (Ethiopia) [52] | Prospective study | 1. HIV-infected patients without TB 2. TB/HIV co-infected patients | 1. WHOQOL-HIV-BREF 2. Kessler-10 scale | 1. Physical health 2. Psychological well-being 3. Social relationships 4. Environmental health 5. Level of independence 6. Spiritual health | Integrating mental health services into the TB/HIV programs can improve QoL |
| Dowdy et al., 2013 (Brazil) [69] | Cross-sectional study | 1. HIV patients 2. TB patients 3. TB/HIV co-infected patients | 1. Medical Outcomes Study HIV Health Survey (MOS-HIV) 2. Visual Analog Scale (VAS) | 1. Physical health summary 2. Mental health summary 3. Visual Analog Scale | Among patients receiving treatment, those with HIV, active TB, and both conditions were found to have similar QoL |
| Louw et al., 2012 (Sout Africa) [54] | Cross-sectional study | 1. TB patients 2. TB re-treatment patients 3. TB-HIV co-infected patients | Social Functioning (SF)-12 Health | 1. Physical health Component 2. Mental health Component | TB and HIV weaken patient’s physical functioning and, thereby, impair QoL |
| Kittikraisak et al., 2012 (Thailand) [34] | Cross-sectional survey | 1. TB patients 2. HIV-infected TB patients 3. HIV patients | 1. EuroQol (EQ-5D) and 2. EuroQol Visual Analog Scale (EQ-VAS) | 1. Mobility 2. Self-care 3. Usual activities 4. Pain or discomfort 5. Anxiety or depression | Patients with TB and HIV had impaired QoL |
| Neves et al., 2012 (Brazil) [73] | Cross-sectional study | 1. HIV/TB co-infection patients 2. HIV-positive individuals without TB | WHOQOL-HIV-BREF | 1. Physical 2. Psychological 3. Level of independence 4. Social relations | TB and HIV can alter biopsycho-social factors, which can impair QoL |
| Study ID (Country) | Study Design | Participants | QoL Instrument Used | QoL Domain Assessed | Findings |
|---|---|---|---|---|---|
| Edwards et al., 2020 (Philippines) [76] | Cross-sectional survey | TB patients with comorbidity with undernutrition, diabetes (DM), and anemia. | WHOQOL-BREF questionnaire | 1. Physical 2. Psychological 3. Social 4. Environmental | Food insecurity and nutritional status denote modifiable risk factors for poor QoL that may be improved through interventions |
| Yeung et al., 2016 [77] | Systematic reviews and meta-analyses | Populations with and without nontuberculous mycobacterial (NTM) disease | 1. SF-362. SGRQ(St. George’s Respiratory Questionnaire 3. Visual analog scores (VAS) | 1. Physical 2. Anxiety or depression 3. Pain or discomfort | Pulmonary NTM had worse health outcomes, thus impairing HRQoL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yasobant, S.; Nazli Khatib, M.; Syed, Z.Q.; Gaidhane, A.M.; Shah, H.; Narkhede, K.; Bhavsar, P.; Patel, J.; Sinha, A.; Puwar, T.; et al. Health-Related Quality of Life (HRQoL) of Patients with Tuberculosis: A Review. Infect. Dis. Rep. 2022, 14, 509-524. https://doi.org/10.3390/idr14040055
Yasobant S, Nazli Khatib M, Syed ZQ, Gaidhane AM, Shah H, Narkhede K, Bhavsar P, Patel J, Sinha A, Puwar T, et al. Health-Related Quality of Life (HRQoL) of Patients with Tuberculosis: A Review. Infectious Disease Reports. 2022; 14(4):509-524. https://doi.org/10.3390/idr14040055
Chicago/Turabian StyleYasobant, Sandul, Mahalaqua Nazli Khatib, Zahiruddin Quazi Syed, Abhay M. Gaidhane, Harsh Shah, Kiran Narkhede, Priya Bhavsar, Jay Patel, Anish Sinha, Tapasvi Puwar, and et al. 2022. "Health-Related Quality of Life (HRQoL) of Patients with Tuberculosis: A Review" Infectious Disease Reports 14, no. 4: 509-524. https://doi.org/10.3390/idr14040055
APA StyleYasobant, S., Nazli Khatib, M., Syed, Z. Q., Gaidhane, A. M., Shah, H., Narkhede, K., Bhavsar, P., Patel, J., Sinha, A., Puwar, T., Saha, S., & Saxena, D. (2022). Health-Related Quality of Life (HRQoL) of Patients with Tuberculosis: A Review. Infectious Disease Reports, 14(4), 509-524. https://doi.org/10.3390/idr14040055








