Comparative Efficacy of Subcutaneous Compared to Intravenous Biologics for Inflammatory Bowel Disease: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Data Sources
2.3. Search Terms
2.3.1. Search Terms for Monoclonal Antibody Therapies
2.3.2. Search Terms for Inflammatory Bowel Diseases
2.3.3. Search Terms for Route of Administration
2.4. Procedure for Selection of Studies
2.5. Eligibility
2.6. Outcomes
2.7. Data Extraction
2.8. Assessing Quality of Included Studies
2.9. Data Synthesis
2.10. Ethics
3. Results
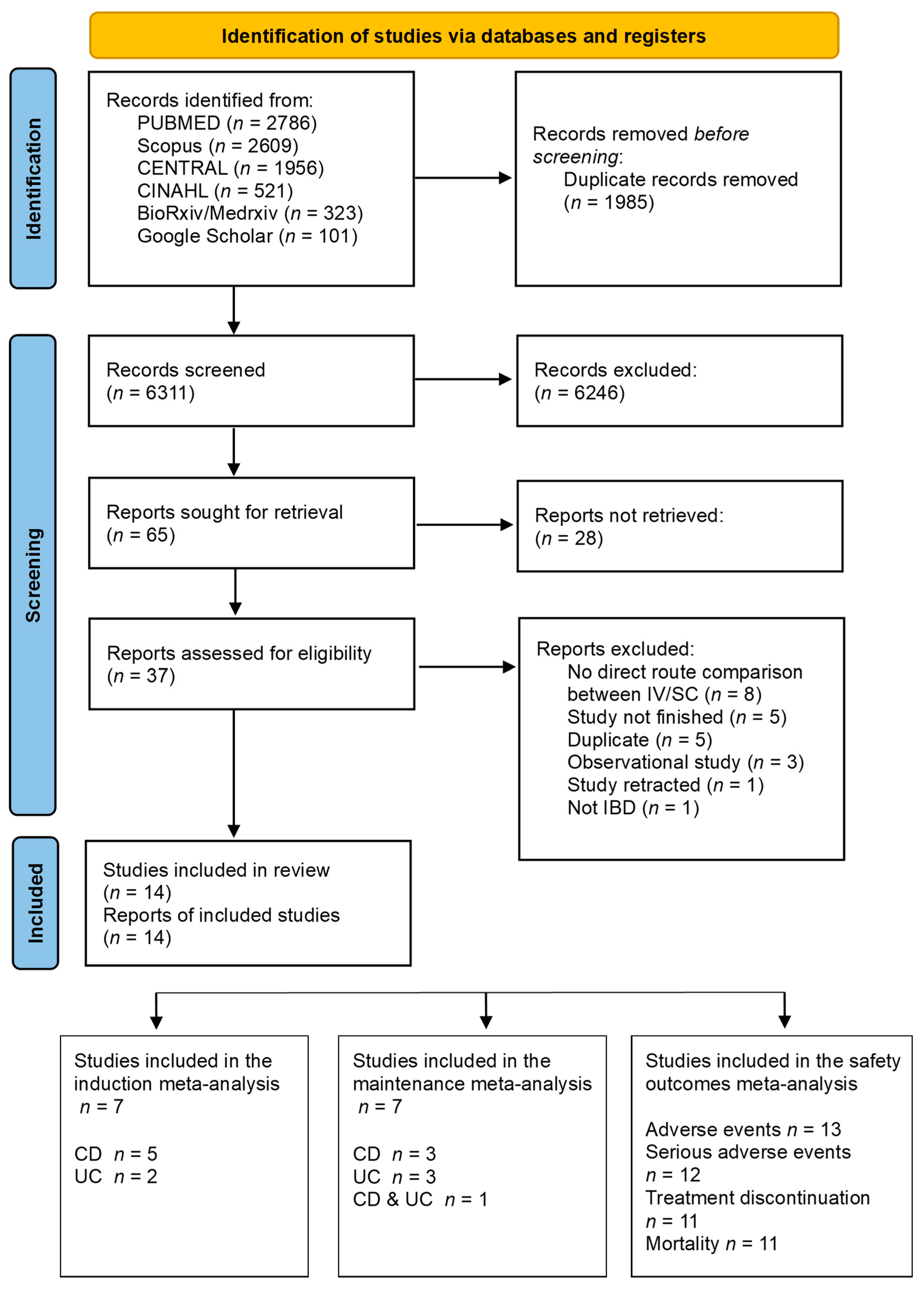
3.1. Search Results
3.2. Characteristics of Included Studies
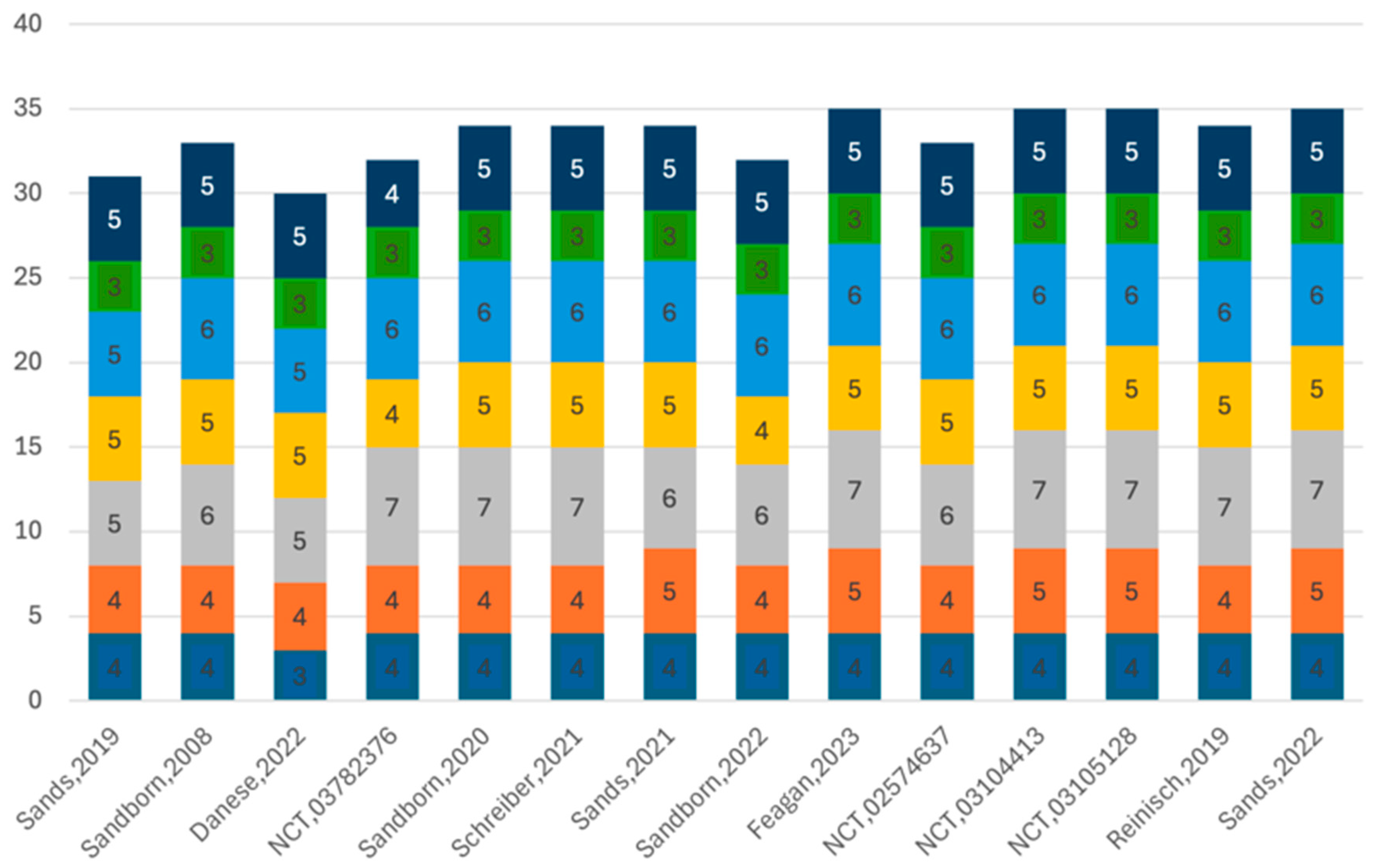
3.3. Assessment of Quality of Included Studies
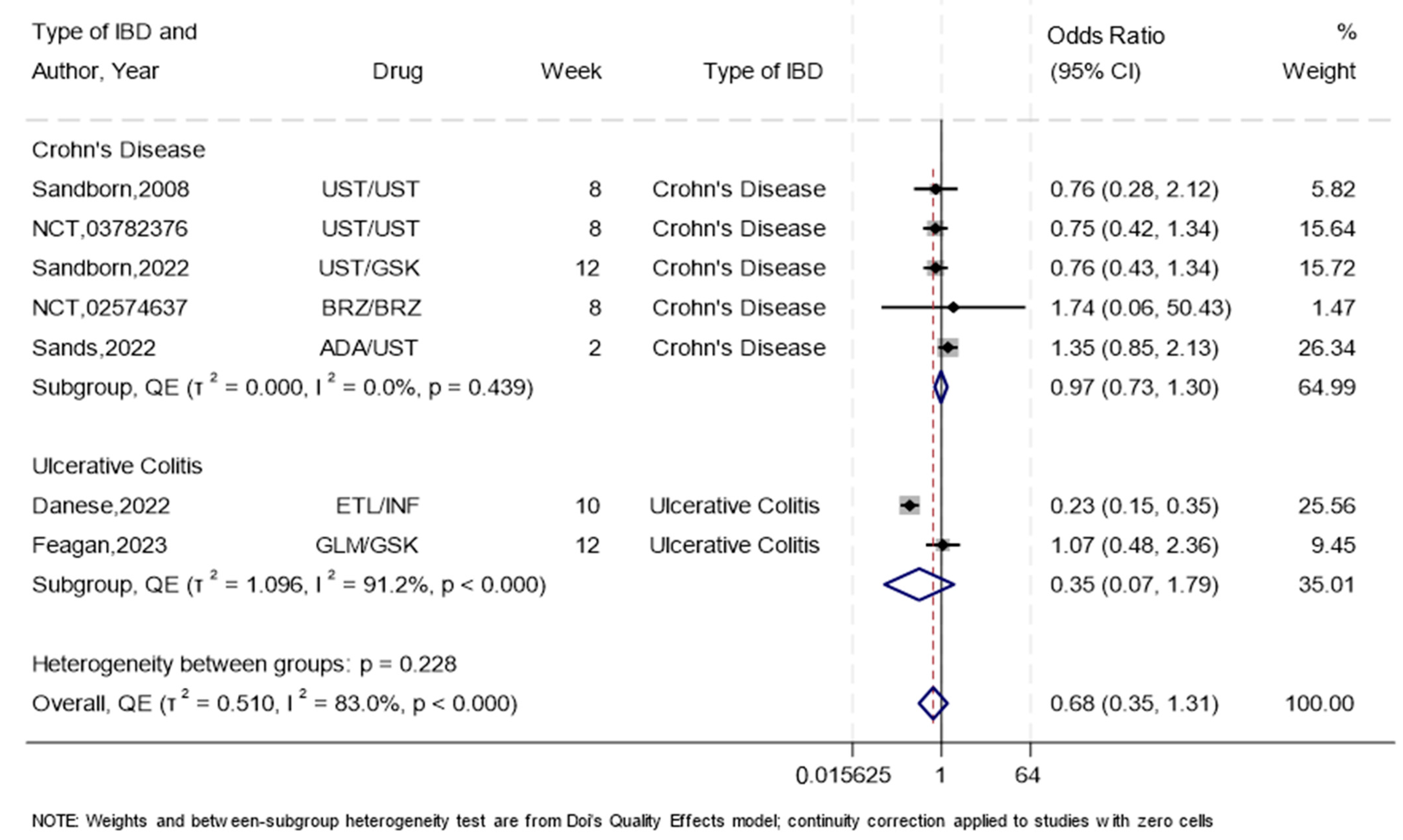
3.4. Induction of Remission
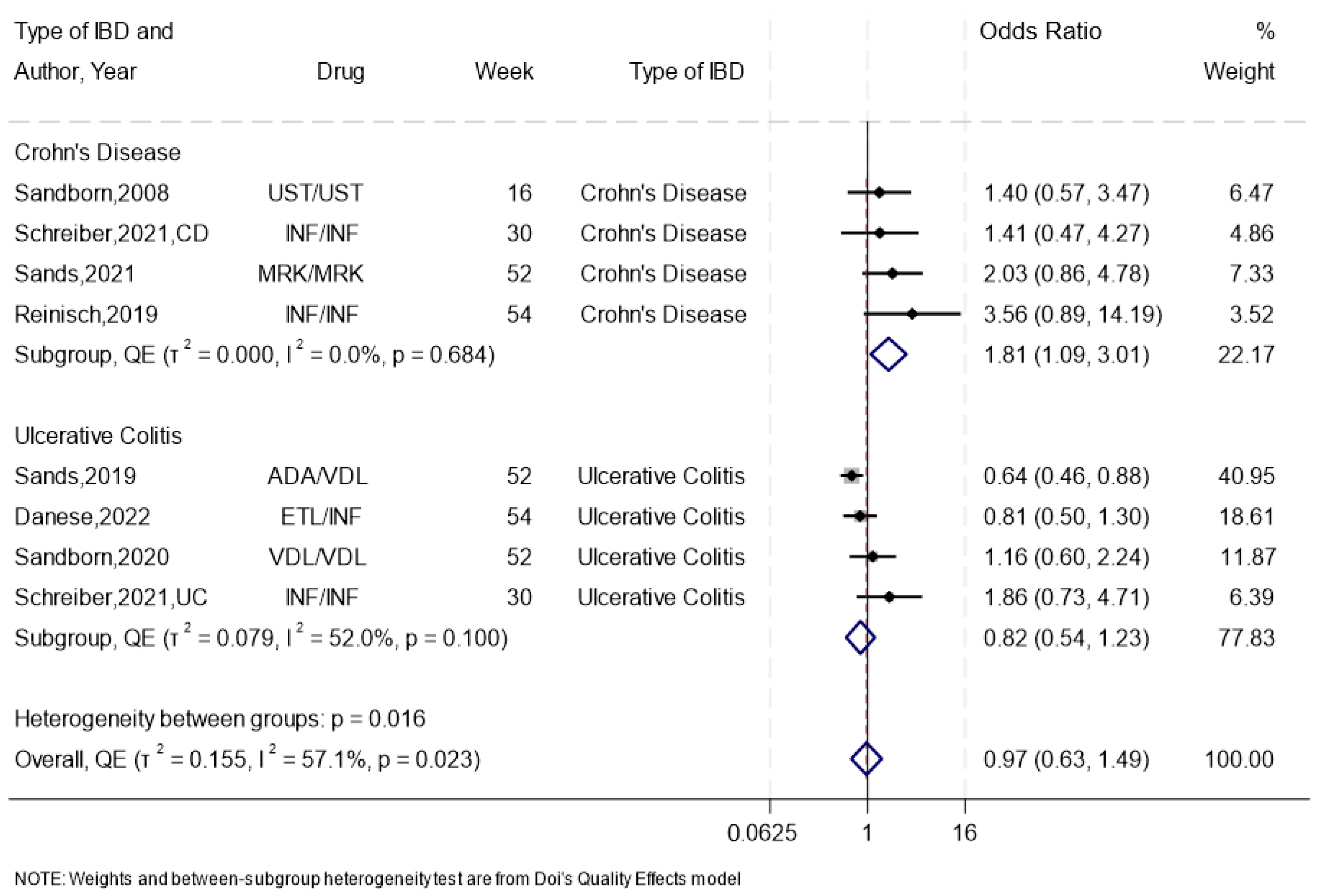
3.5. Maintenance of Remission
3.6. Endoscopic Remission
3.7. Endoscopic Response
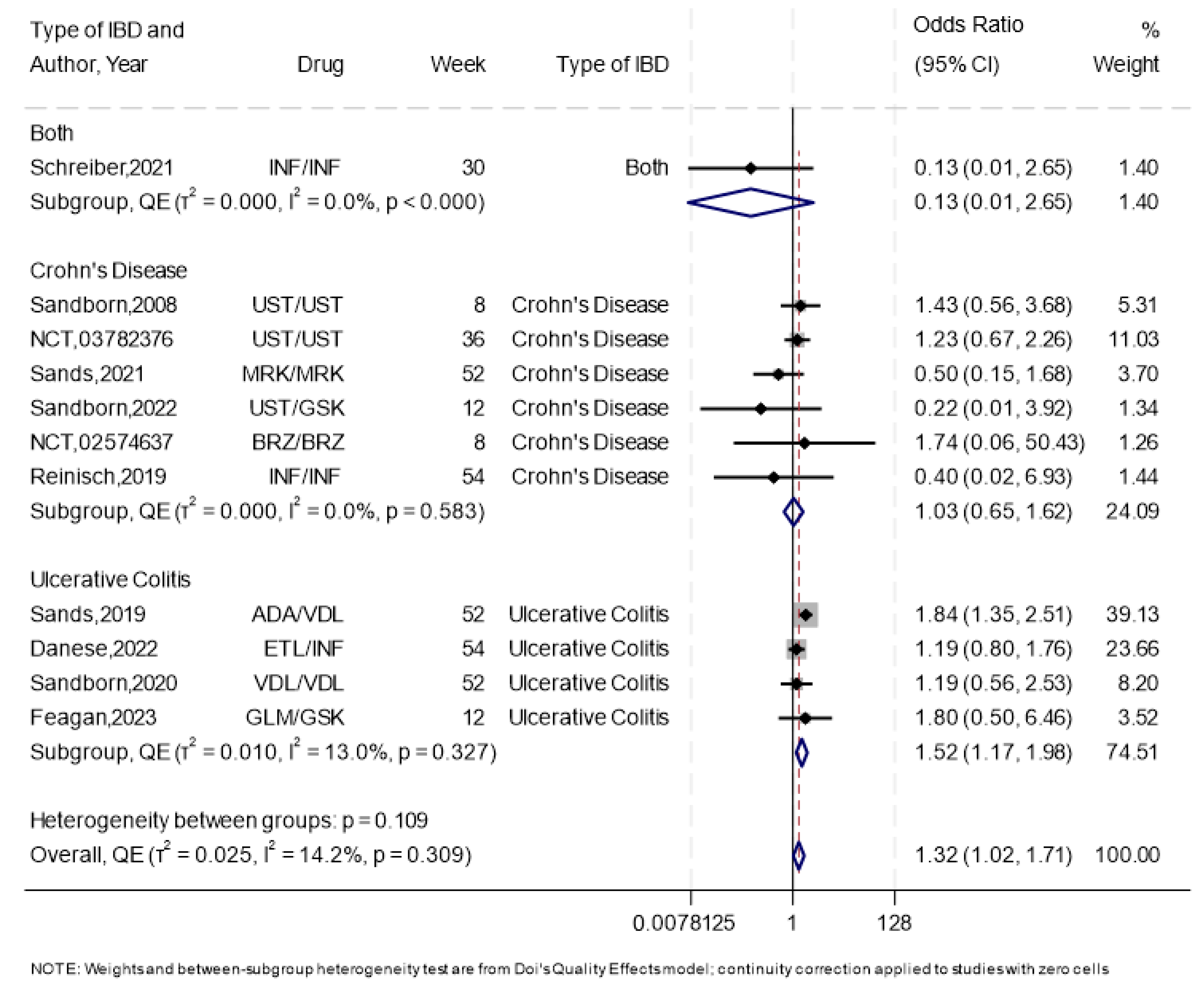
3.8. Any Adverse Events and Serious Adverse Events
3.9. Treatment Discontinuation
3.10. Quality of Life
3.11. Hospitalization
3.12. Mortality
4. Discussion
5. Conclusion
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017, 390, 2769–2778, Erratum in Lancet 2020, 396, e56. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Li, Z.; Liu, S.; Zhang, D. Global, regional and national burden of inflammatory bowel disease in 204 countries and territories from 1990 to 2019: A systematic analysis based on the Global Burden of Disease Study 2019. BMJ Open 2023, 13, e065186. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Radford, S.J.; McGing, J.; Czuber-Dochan, W.; Moran, G. Systematic review: The impact of inflammatory bowel disease-related fatigue on health-related quality of life. Frontline Gastroenterol. 2021, 12, 11–21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rogler, G.; Singh, A.; Kavanaugh, A.; Rubin, D.T. Extraintestinal Manifestations of Inflammatory Bowel Disease: Current Concepts, Treatment, and Implications for Disease Management. Gastroenterology 2021, 161, 1118–1132. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wan, Q.; Zhao, R.; Xia, L.; Wu, Y.; Zhou, Y.; Wang, Y.; Cui, Y.; Shen, X.; Wu, X.T. Inflammatory bowel disease and risk of gastric, small bowel and colorectal cancer: A meta-analysis of 26 observational studies. J. Cancer Res. Clin. Oncol. 2021, 147, 1077–1087. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Wang, S.; Li, J. Treatment of Inflammatory Bowel Disease: A Comprehensive Review. Front. Med. 2021, 8, 765474. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hazel, K.; O’Connor, A. Emerging treatments for inflammatory bowel disease. Ther. Adv. Chronic Dis. 2020, 11, 2040622319899297. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ananthakrishnan, A.N.; Shi, H.Y.; Tang, W.; Law, C.C.; Sung, J.J.; Chan, F.K.; Ng, S.C. Systematic Review and Meta-analysis: Phenotype and Clinical Outcomes of Older-onset Inflammatory Bowel Disease. J. Crohns Colitis 2016, 10, 1224–1236. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Parigi, T.L.; D’Amico, F.; Abreu, M.T.; Dignass, A.; Dotan, I.; Magro, F.; Griffiths, A.M.; Jairath, V.; Iacucci, M.; Mantzaris, G.J.; et al. Difficult-to-treat inflammatory bowel disease: Results from an international consensus meeting. Lancet Gastroenterol. Hepatol. 2023, 8, 853–859. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Gulati, A.; Alipour, O.; Shao, L. Relapse From Deep Remission After Therapeutic De-escalation in Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. J. Crohns Colitis 2020, 14, 1413–1423. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lasa, J.S.; Olivera, P.A.; Danese, S.; Peyrin-Biroulet, L. Efficacy and safety of biologics and small molecule drugs for patients with moderate-to-severe ulcerative colitis: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2022, 7, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Murad, M.H.; Fumery, M.; Sedano, R.; Jairath, V.; Panaccione, R.; Sandborn, W.J.; Ma, C. Comparative efficacy and safety of biologic therapies for moderate-to-severe Crohn’s disease: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 1002–1014. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Breedveld, F.C. Therapeutic monoclonal antibodies. Lancet 2000, 355, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Feagan, B.G.; Sandborn, W.J.; D’Haens, G.; Panés, J.; Kaser, A.; Ferrante, M.; Louis, E.; Franchimont, D.; Dewit, O.; Seidler, U.; et al. Induction therapy with the selective interleukin-23 inhibitor risankizumab in patients with moderate-to-severe Crohn’s disease: A randomised, double-blind, placebo-controlled phase 2 study. Lancet 2017, 389, 1699–1709. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.F.; Zhu, L.L.; Chen, M.; Xu, H.M.; Wang, H.F.; Feng, X.Q.; Zhu, X.P.; Zhou, Q. The optimal choice of medication administration route regarding intravenous, intramuscular, and subcutaneous injection. Patient Prefer. Adherence 2015, 9, 923–942. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xu, Z.; Leu, J.H.; Xu, Y.; Nnane, I.; Liva, S.G.; Wang-Lin, S.X.; Kudgus-Lokken, R.; Vermeulen, A.; Ouellet, D. Development of Therapeutic Proteins for a New Subcutaneous Route of Administration After the Establishment of Intravenous Dosages: A Systematic Review. Clin. Pharmacol. Ther. 2023, 113, 1011–1029. [Google Scholar] [CrossRef] [PubMed]
- Stoner, K.L.; Harder, H.; Fallowfield, L.J.; Jenkins, V.A. Intravenous versus Subcutaneous Drug Administration. Which Do Patients Prefer? A Systematic Review. Patient 2014, 8, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Shirley, M. Subcutaneous Infliximab, CT-P13 SC: A Profile of Its Use in the EU. Clin. Drug Investig. 2021, 41, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- De Cock, E.; Pivot, X.; Hauser, N.; Verma, S.; Kritikou, P.; Millar, D.; Knoop, A. A time and motion study of subcutaneous versus intravenous trastuzumab in patients with HER2-positive early breast cancer. Cancer Med. 2016, 5, 389–397. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schreiber, S.; Ben-Horin, S.; Leszczyszyn, J.; Dudkowiak, R.; Lahat, A.; Gawdis-Wojnarska, B.; Pukitis, A.; Horynski, M.; Farkas, K.; Kierkus, J.; et al. Randomized Controlled Trial: Subcutaneous vs. Intravenous Infliximab CT-P13 Maintenance in Inflammatory Bowel Disease. Gastroenterology 2021, 160, 2340–2353. [Google Scholar] [CrossRef] [PubMed]
- Danese, S.; Colombel, J.F.; Lukas, M.; Gisbert, J.P.; D’Haens, G.; Hayee, B.; Panaccione, R.; Kim, H.S.; Reinisch, W.; Tyrrell, H.; et al. Etrolizumab versus infliximab for the treatment of moderately to severely active ulcerative colitis (GARDENIA): A randomised, double-blind, double-dummy, phase 3 study. Lancet Gastroenterol. Hepatol. 2022, 7, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Sandborn, W.J.; Baert, F.; Danese, S.; Krznarić, Ž.; Kobayashi, T.; Yao, X.; Chen, J.; Rosario, M.; Bhatia, S.; Kisfalvi, K.; et al. Efficacy and Safety of Vedolizumab Subcutaneous Formulation in a Randomized Trial of Patients With Ulcerative Colitis. Gastroenterology 2020, 158, 562–572.e512. [Google Scholar] [CrossRef] [PubMed]
- Sandborn, W.J.; Feagan, B.G.; Fedorak, R.N.; Scherl, E.; Fleisher, M.R.; Katz, S.; Johanns, J.; Blank, M.; Rutgeerts, P.; Ustekinumab Crohn’s Disease Study Group. A randomized trial of Ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with moderate-to-severe Crohn’s disease. Gastroenterology 2008, 135, 1130–1141. [Google Scholar] [CrossRef] [PubMed]
- Feagan, B.G.; Sands, B.E.; Sandborn, W.J.; Germinaro, M.; Vetter, M.; Shao, J.; Sheng, S.; Johanns, J.; Panés, J.; VEGA Study Group. Guselkumab plus golimumab combination therapy versus guselkumab or golimumab monotherapy in patients with ulcerative colitis (VEGA): A randomised, double-blind, controlled, phase 2, proof-of-concept trial. Lancet Gastroenterol. Hepatol. 2023, 8, 307–320. [Google Scholar] [CrossRef] [PubMed]
- Sandborn, W.J.; D’Haens, G.R.; Reinisch, W.; Panés, J.; Chan, D.; Gonzalez, S.; Weisel, K.; Germinaro, M.; Frustaci, M.E.; Yang, Z.; et al. Guselkumab for the Treatment of Crohn’s Disease: Induction Results From the Phase 2 GALAXI-1 Study. Gastroenterology 2022, 162, 1650–1664.e165, Erratum in Gastroenterology 2023, 165, 1588. https://doi.org/10.1053/j.gastro.2023.09.010. [Google Scholar] [CrossRef] [PubMed]
- NCT02574637. Evaluation of Efficacy and Safety of Brazikumab (MEDI2070) in Participants with Active, Moderate to Severe Crohn’s Disease. ClinicalTrials.gov2021 [Updated 5 May 2021]. Available online: https://clinicaltrials.gov/study/NCT02574637 (accessed on 24 June 2024).
- Chetwood, J.D.; Tran, Y.; Subramanian, S.; Smith, P.J.; Iborra, M.; Buisson, A.; Paramsothy, S.; Leong, R.W. Intravenous Versus Subcutaneous Infliximab in Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. J. Crohn’s Colitis 2024, 18, 1440–1449. [Google Scholar] [CrossRef] [PubMed]
- Peyrin-Biroulet, L.; Bossuyt, P.; Bettenworth, D.; Loftus, E.V., Jr.; Anjie, S.I.; D’Haens, G.; Saruta, M.; Arkkila, P.; Park, H.; Choi, D.; et al. Comparative Efficacy of Subcutaneous and Intravenous Infliximab and Vedolizumab for Maintenance Treatment of TNF-naive Adult Patients with Inflammatory Bowel Disease: A Systematic Literature Review and Network Meta-analysis. Dig. Dis. Sci. 2024, 69, 1808–1825. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gajendran, M.; Loganathan, P.; Catinella, A.P.; Hashash, J.G. A comprehensive review and update on Crohn’s disease. Dis. Mon. 2018, 64, 20–57. [Google Scholar] [CrossRef] [PubMed]
- Sandborn, W.J.; Sands, B.E.; Uddin, S.; Qasim Khan, R.M.; Sagar Mukherjee, R. Clinical Trial Design in Ulcerative Colitis: Interpreting Evolving Endpoints Based on Post Hoc Analyses of the Vedolizumab Phase 3 Trials GEMINI 1 and VISIBLE 1. Crohns Colitis 360 2024, 6, otad076. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Viscido, A.; Valvano, M.; Stefanelli, G.; Capannolo, A.; Castellini, C.; Onori, E.; Ciccone, A.; Vernia, F.; Latella, G. Systematic review and meta-analysis: The advantage of endoscopic Mayo score 0 over 1 in patients with ulcerative colitis. BMC Gastroenterol. 2022, 22, 92. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sharara, A.I.; Malaeb, M.; Lenfant, M.; Ferrante, M. Assessment of Endoscopic Disease Activity in Ulcerative Colitis: Is Simplicity the Ultimate Sophistication? Inflamm. Intest. Dis. 2022, 7, 7–12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vuitton, L.; Marteau, P.; Sandborn, W.J.; Levesque, B.G.; Feagan, B.; Vermeire, S.; Danese, S.; D’Haens, G.; Lowenberg, M.; Khanna, R.; et al. IOIBD technical review on endoscopic indices for Crohn’s disease clinical trials. Gut 2016, 65, 1447–1455. [Google Scholar] [CrossRef] [PubMed]
- Stone, J.C.; Glass, K.; Clark, J.; Ritskes-Hoitinga, M.; Munn, Z.; Tugwell, P.; Doi, S.A.R. The MethodologicAl STandards for Epidemiological Research (MASTER) scale demonstrated a unified framework for bias assessment. J. Clin. Epidemiol. 2021, 134, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Doi, S.A.; Thalib, L. A quality-effects model for meta-analysis. Epidemiology 2008, 19, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Hedeker, D.; Gibbons, R.D. A random-effects ordinal regression model for multilevel analysis. Biometrics 1994, 50, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022): Cochrane; Wiley: Hoboken, NJ, USA, 2022; Available online: www.training.cochrane.org/handbook (accessed on 24 June 2024).
- Thompson, S.G. Systematic Review: Why sources of heterogeneity in meta-analysis should be investigated. BMJ 1994, 309, 1351. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- NCT03104413. A Study to Assess the Efficacy and Safety of Risankizumab in Participants with Moderately to Severely Active Crohn’s Disease Who Failed Prior Biologic Treatment. ClinicalTrial.gov2022. Available online: https://clinicaltrials.gov/study/NCT03104413 (accessed on 15 June 2024).
- NCT03105128. A Study of the Efficacy and Safety of Risankizumab in Participants with Moderately to Severely Active Crohn’s Disease. ClinicalTrial.gov2022. Available online: https://clinicaltrials.gov/study/NCT03105128 (accessed on 10 July 2024).
- NCT03782376. A Study to Evaluate Efficacy and Safety of Ustekinumab Re-Induction Therapy in Participants with Moderately to Severely Active Crohn’s Disease (POWER). ClinicalTrial.gov2018. Available online: https://clinicaltrials.gov/study/NCT03782376 (accessed on 15 July 2024).
- Reinisch, W.; Jang, B.I.; Borzan, V.; Lahat, A.; Pukitis, A.; Osipenko, M.; Mostovoy, Y.; Schreiber, S.; Ben-Horin, S.; Lee, S.J.; et al. DOP62 A novel formulation of CT-P13 (infliximab biosimilar) for subcutaneous administration: 1-year result from a Phase I open-label randomised controlled trial in patients with active Crohn’s disease. J. Crohn’s Colitis 2019, 13 (Suppl. S1), S066–S067. [Google Scholar] [CrossRef]
- Sands, B.E.; Irving, P.M.; Hoops, T.; Izanec, J.L.; Gao, L.L.; Gasink, C.; Greenspan, A.; Allez, M.; Danese, S.; Hanauer, S.B.; et al. Ustekinumab versus adalimumab for induction and maintenance therapy in biologic-naive patients with moderately to severely active Crohn’s disease: A multicentre, randomised, double-blind, parallel-group, phase 3b trial. Lancet 2022, 399, 2200–2211. [Google Scholar] [CrossRef] [PubMed]
- Sands, B.E.; Peyrin-Biroulet, L.; Kierkus, J.; Higgins, P.D.R.; Fischer, M.; Jairath, V.; Hirai, F.; D’Haens, G.; Belin, R.M.; Miller, D.; et al. Efficacy and Safety of Mirikizumab in a Randomized Phase 2 Study of Patients With Crohn’s Disease. Gastroenterology 2021, 162, 495–508. [Google Scholar] [CrossRef] [PubMed]
- Sands, B.E.; Peyrin-Biroulet, L.; Loftus, E.V., Jr.; Danese, S.; Colombel, J.F.; Törüner, M.; Jonaitis, L.; Abhyankar, B.; Chen, J.; Rogers, R.; et al. Vedolizumab versus Adalimumab for Moderate-to-Severe Ulcerative Colitis. N. Engl. J. Med. 2019, 381, 1215–1226. [Google Scholar] [CrossRef] [PubMed]
- Feuerstein, J.D.; Ho, E.Y.; Shmidt, E.; Singh, H.; Falck-Ytter, Y.; Sultan, S.; Terdiman, J.P.; American Gastroenterological Asso-ciation Institute Clinical Guidelines Committee. AGA Clinical Practice Guidelines on the Medical Management of Moderate to Severe Luminal and Perianal Fistulizing Crohn’s Disease. Gastroenterology 2021, 160, 2496–2508. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, G.R.; Loftus, E.V.; Isaacs, K.L.; Regueiro, M.D.; Gerson, L.B.; Sands, B.E. ACG Clinical Guideline: Management of Crohn’s Disease in Adults. Am. J. Gastroenterol. 2018, 113, 481–517, Erratum in Am. J. Gastroenterol. 2018, 113, 1101. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.; Bonovas, S.; Doherty, G.; Kucharzik, T.; Gisbert, J.P.; Raine, T.; Adamina, M.; Armuzzi, A.; Bachmann, O.; Bager, P.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Medical Treatment. J. Crohns Colitis 2020, 14, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Motaghi, E.; Ghasemi-Pirbaluti, M.; Zabihi, M. Etrolizumab versus infliximab in the treatment of induction phase of ulcerative colitis: A systematic review and indirect comparison. Pharmacol. Res. 2019, 139, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Kawalec, P.; Pilc, A. An indirect comparison of infliximab versus adalimumab or golimumab for active ulcerative colitis. Arch. Med. Sci. 2016, 12, 1097–1109. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Raine, T.; Bonovas, S.; Burisch, J.; Kucharzik, T.; Adamina, M.; Annese, V.; Bachmann, O.; Bettenworth, D.; Chaparro, M.; Czuber-Dochan, W.; et al. ECCO Guidelines on Therapeutics in Ulcerative Colitis: Medical Treatment. J. Crohns Colitis 2022, 16, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.T.; Ananthakrishnan, A.N.; Siegel, C.A.; Sauer, B.G.; Long, M.D. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am. J. Gastroenterol. 2019, 114, 384–413. [Google Scholar] [CrossRef] [PubMed]
- Moćko, P.; Kawalec, P.; Pilc, A. Safety Profile of Biologic Drugs in the Therapy of Ulcerative Colitis: A Systematic Review and Network Meta-Analysis. Pharmacotherapy 2016, 36, 870–879. [Google Scholar] [CrossRef] [PubMed]
- Annese, V.; Duricova, D.; Gower-Rousseau, C.; Jess, T.; Langholz, E. Impact of New Treatments on Hospitalisation, Surgery, Infection, and Mortality in IBD: A Focus Paper by the Epidemiology Committee of ECCO. J. Crohns Colitis 2016, 10, 216–225. [Google Scholar] [CrossRef] [PubMed]
- D’Haens, G.; Panaccione, R.; Baert, F.; Bossuyt, P.; Colombel, J.F.; Danese, S.; Dubinsky, M.; Feagan, B.G.; Hisamatsu, T.; Lim, A.; et al. Risankizumab as induction therapy for Crohn’s disease: Results from the phase 3 ADVANCE and MOTIVATE induction trials. Lancet 2022, 399, 2015–2030. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Type of IBD | Specific Biologic | SC/IV Sample Size | Gender | Age Mean (SD) | Phase of Remission | Follow-Up Period (Months) | Mechanism of Action |
|---|---|---|---|---|---|---|---|---|
| Reinisch, 2019 [45] (CT-P13 SC 1.6 study Part 1) | Crohn’s Disease | SC: Infliximab: 120, 180, 240 mg IV: Infliximab: 5 mg/kg | SC:31 IV:13 | - | - | Maintenance | 12.5 | TNF-alpha Inhibitor |
| Schreiber, 2021 [20] (CT-P13 SC 1.6 study Part 2) | Crohn’s Disease and Ulcerative Colitis | SC: Infliximab: 120, 240 mg IV: Infliximab: 5 mg/kg | SC:66 IV:65 | SC:30 F, 36 M IV: 30 F, 35 M | SC:33 IV:36 | Maintenance | 12.5 | TNF-alpha Inhibitor |
| Sands, 2019 [48] | Ulcerative Colitis | SC: Adalimumab: 40, 80 mg IV: Vedolizumab: 300 mg | SC:386 IV:385 | SC:170 F, 216 M IV:151 F, 234 M | SC:40.5 (13.4) IV:40.8 (13.7) | Maintenance | 12 | TNF-alpha Inhibitor and Anti-integrin Antibody |
| Sands, 2022 [46] | Crohn’s Disease | SC: Adalimumab: 40, 80, 160 mg IV: Ustekinumab: 6 mg/kg | SC:195 IV:191 | SC:100 F, 95 M IV:101 F, 90 M | SC:37·4 12·99) IV:37·0 (13·23) | Induction | 12 | TNF-alpha Inhibitor and IL-12/IL-23 Inhibitor |
| Sandborn, 2008 [23] | Crohn’s Disease | SC: Ustekinumab: 90 mg IV: Ustekinumab: 4.5 mg/kg | SC:65 IV:66 | SC:27 F, 38 M IV:34 F, 32 M | SC:37 (13) IV:43 (12) | Induction and Maintenance | 6 | IL-12/IL-23 Inhibitor |
| NCT03782376 [44] | Crohn’s Disease | SC: Ustekinumab: 90 mg IV: Ustekinumab: 6 mg/kg | SC:107 IV:108 | SC:62 F, 45 M IV:62 F, 46 M | SC:40 (13.07) IV:41.8 (13.63) | Induction | 8 | IL-12/IL-23 Inhibitor |
| Sandborn, 2020 [22] | Ulcerative Colitis | SC: Vedolizumab: 108 mg IV: Vedolizumab: 300 mg | SC:106 IV:54 | SC:41 F, 65 M SC:23 F, 31 M | SC:38.1 (13.1) IV:41.6 (14.1) | Maintenance | 12 | Anti-integrin Antibody |
| Danses, 2022 [21] | Ulcerative Colitis | SC: Etrolizumab: 105 mg IV: Infliximab: 5 mg/kg | SC:199 IV:198 | SC:81 F, 118 M IV:66 F, 132 M | SC:40.0 (15.2) IV:39.5 (13.4) | Induction and Maintenance | 12.5 | Integrin Inhibitor and TNF-alpha Inhibitor |
| Sandborn, 2022 [25] | Crohn’s Disease | SC: Ustekinumab: 90 mg IV: Guselkumab: 200, 600, 1200 mg | SC:63 IV:185 | SC:22 F, 41 M IV:80 F, 105 M | SC:36.1 (12.02) IV:39.6 (13.86) | Induction | 11.7–12.2 | IL-12/IL-23 Inhibitor |
| Feagan, 2023 [24] | Ulcerative Colitis | SC: Golimumab: 100, 200 mg IV: Guselkumab: 200 mg | SC:72 IV:71 | SC:30 F, 42 M IV:31 F, 40 M | SC:38.1 (10.47) IV:39.1 (13.67) | Induction | 11.5 | TNF-alpha Inhibitor and IL-23 Inhibitor |
| Sands, 2021 [47] | Crohn’s Disease | SC: Mirikizumab: 300 mg IV: Mirikizumab: 1000 mg | SC:46 IV:41 | - | - | Maintenance | 12 | IL-23 Inhibitor |
| NCT02574637 [26] | Crohn’s Disease | SC: Brazikumab: 35, 70, 105, 210 mg IV: Brazikumab: 700 mg | SC:10 IV:5 | SC:5 F, 5 M IV:3 F, 2 M | SC:40.14 (13.30) IV:37.2 (13.29) | Induction | 6.4 | IL-23 Inhibitor |
| NCT03104413 [42] | Crohn’s Disease | SC: Risankizumab: 180, 360 mg IV: Risankizumab: 1200 mg | SC:83 IV:453 | - | - | Adverse Events | 10.1 | IL-23 Inhibitor |
| NCT03105128 [43] | Crohn’s Disease | SC: Risankizumab: 180, 360 mg IV: Risankizumab: 1200 mg | SC:135 IV:812 | - | - | Adverse Events | 10.1 | IL-23 Inhibitor |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alwisi, N.; Ismail, R.; Al-Kuwari, H.; Al-Ansari, K.H.; Al-Matwi, M.A.; Aweer, N.A.; Al-Marri, W.N.; Al-Kubaisi, Y.; Al-Mohannadi, M.; Hamran, S.; et al. Comparative Efficacy of Subcutaneous Compared to Intravenous Biologics for Inflammatory Bowel Disease: Systematic Review and Meta-Analysis. Gastroenterol. Insights 2025, 16, 12. https://doi.org/10.3390/gastroent16020012
Alwisi N, Ismail R, Al-Kuwari H, Al-Ansari KH, Al-Matwi MA, Aweer NA, Al-Marri WN, Al-Kubaisi Y, Al-Mohannadi M, Hamran S, et al. Comparative Efficacy of Subcutaneous Compared to Intravenous Biologics for Inflammatory Bowel Disease: Systematic Review and Meta-Analysis. Gastroenterology Insights. 2025; 16(2):12. https://doi.org/10.3390/gastroent16020012
Chicago/Turabian StyleAlwisi, Nouran, Rana Ismail, Hissa Al-Kuwari, Khalifa H. Al-Ansari, Mohammed A. Al-Matwi, Noor A. Aweer, Wejdan N. Al-Marri, Yousif Al-Kubaisi, Muneera Al-Mohannadi, Shahd Hamran, and et al. 2025. "Comparative Efficacy of Subcutaneous Compared to Intravenous Biologics for Inflammatory Bowel Disease: Systematic Review and Meta-Analysis" Gastroenterology Insights 16, no. 2: 12. https://doi.org/10.3390/gastroent16020012
APA StyleAlwisi, N., Ismail, R., Al-Kuwari, H., Al-Ansari, K. H., Al-Matwi, M. A., Aweer, N. A., Al-Marri, W. N., Al-Kubaisi, Y., Al-Mohannadi, M., Hamran, S., Farooqui, H. H., & Chivese, T. (2025). Comparative Efficacy of Subcutaneous Compared to Intravenous Biologics for Inflammatory Bowel Disease: Systematic Review and Meta-Analysis. Gastroenterology Insights, 16(2), 12. https://doi.org/10.3390/gastroent16020012






