Pain Catastrophizing: How Far Have We Come
Abstract
1. Introduction
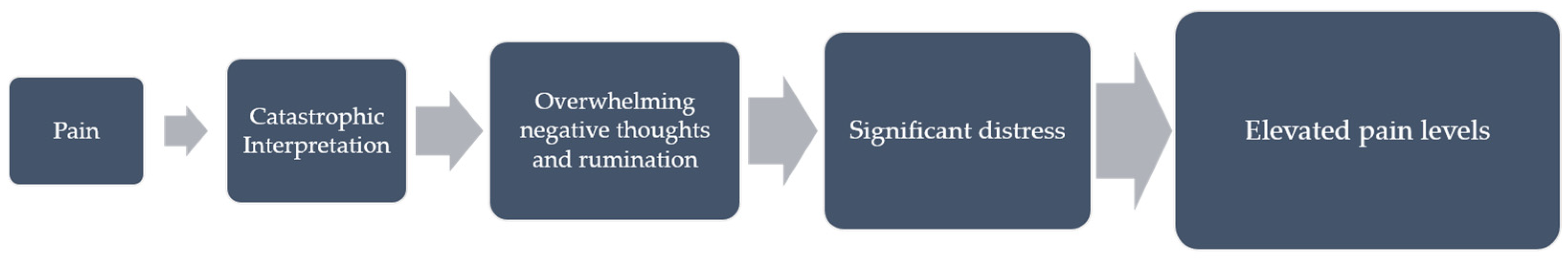
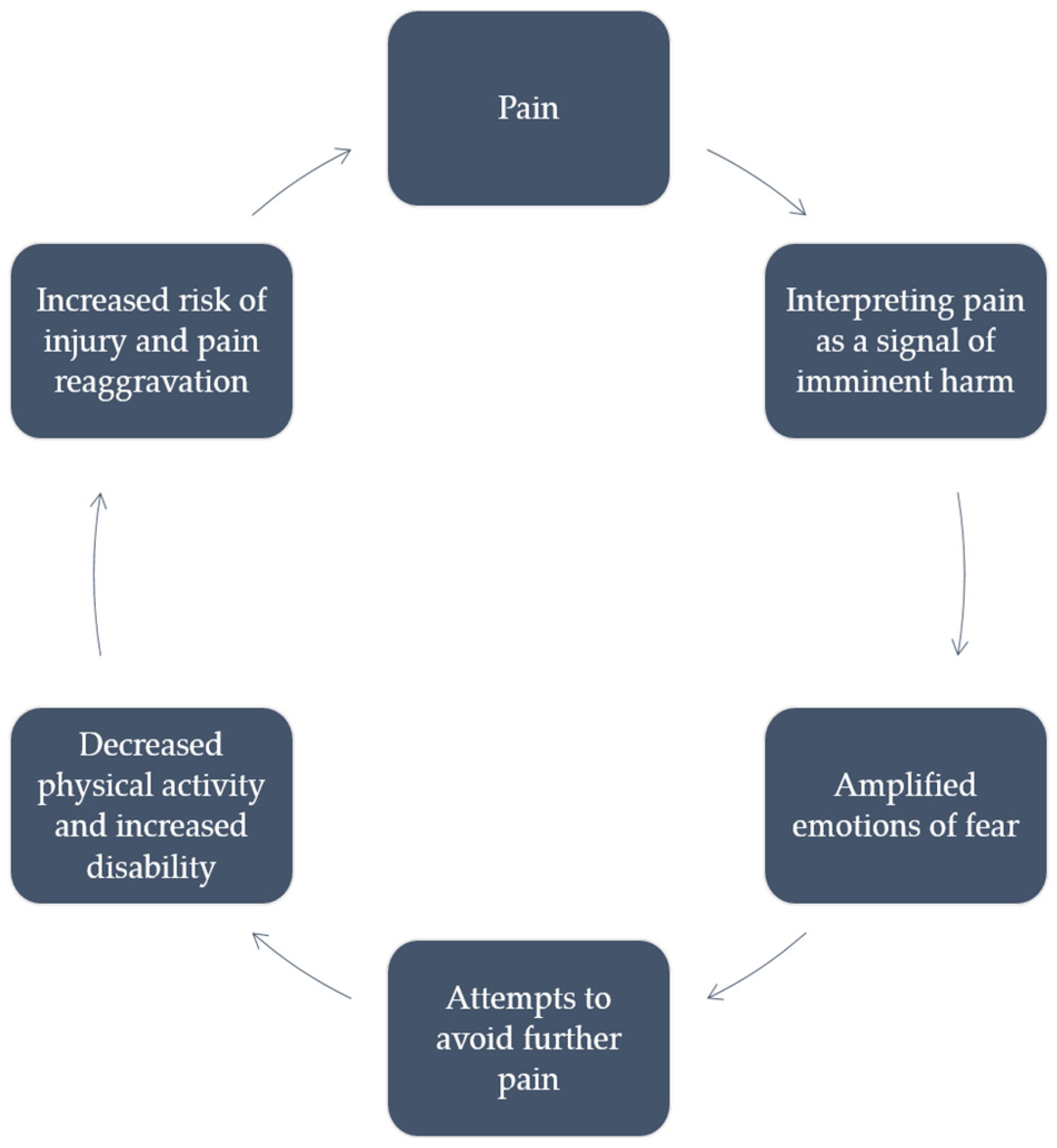
2. Theoretical Foundations of Pain Catastrophizing
3. Assessment Tools for Pain Catastrophizing
4. Prevalence, Demographics, and Cultural Variations of Pain Catastrophizing
5. Influence of Cognitive and Emotional Factors on Pain Perception
6. Clinical Significance of Pain Catastrophizing
| Intervention | Study | Condition | N | Findings |
|---|---|---|---|---|
| Acceptance and Commitment Therapy (ACT) | Lai et al. (2023) [110] | Chronic Pain | 2293 1 | ACT showed significant effects on chronic pain especially when conducted face-to-face, and in the population with chronic headache and fibromyalgia. Considering the size and quality of the meta-analysis, it demonstrated considerable benefits in ACT for patients suffering from chronic pain. |
| Cognitive-Behavioral Therapy (CBT) | Alda et al. (2011) [111] | Fibromyalgia | 169 | CBT was superior to usual care in terms of function and quality of life, as well as in improving the level of pain catastrophizing and pain acceptance. |
| Sun et al. (2020) [112] | Total Knee Replacement | 80 | In comparison to usual care, CBT was more efficient in reducing postoperative pain during activity from the fifth day to the third month, as well as reducing pain catastrophizing in the first three months. | |
| Buhrman et al. (2011) [113] | Chronic Back Pain | 54 | In the group of patients treated with CBT, statistically significant reductions were found in the level of pain catastrophizing and in the quality of life. The study demonstrated no other significant improvements when compared to other treatment. These findings suggest that internet-based CBT could have a supplementary role in chronic back pain treatment. | |
| Mindfulness Based Stress Reduction (MBSR) | Garland et al. (2012) [114] | Irritable Bowel Syndrome | 75 | MBSR was found to significantly improve IBS symptoms, likely by modifying anxiety and catastrophizing related to abdominal sensations. |
| La Cour et al. (2015) [115] | Chronic Pain | 109 | A significant effect of MBSR was found in the self-reported measure of health. Also, significant medium to large size effects were found for lower anxiety and depression, better mental quality of life, feeling in control of the pain, and higher pain acceptance. Small effect sizes were found for pain measures. These findings imply that a standardized MBSR can be clinically useful in management of patients with chronic pain. | |
| Cherkin et al. (2016) [116] | Back Pain | 342 | Treatment with MBSR or CBT, in comparison to usual standards of care, resulted in greater improvement in back pain as well as functional limitations, suggesting that it may be used as an effective therapy of chronic low back pain. | |
| Pain Neuroscience Education (PNE) | Meeus et al. (2010) [117] | Chronic Fatigue Syndrome (CFS) | 48 | PNE was associated with an improved understanding of the neurophysiology of pain and a reduction of the ruminating subscale of the Pain Catastrophizing Scale, implying that PNE could be considered as a possible therapeutic modality in CFS and chronic pain. |
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- International Association for the Study of Pain. Available online: https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/ (accessed on 28 February 2024).
- Darnall, B.D.; Carr, D.B.; Schatman, M.E. Pain psychology and the biopsychosocial model of pain treatment: Ethical imperatives and social responsibility. Pain Med. 2017, 18, 1413–1415. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.H.; Farris, S.G. A meta-analysis of the associations of elements of the fear-avoidance model of chronic pain with negative affect, depression, anxiety, pain-related disability and pain intensity. Eur. J. Pain 2022, 26, 1611–1635. [Google Scholar] [CrossRef] [PubMed]
- Petrini, L.; Arendt-Nielsen, L. Understanding Pain Catastrophizing: Putting Pieces Together. Front. Psychol. 2020, 11, 603420. [Google Scholar] [CrossRef] [PubMed]
- Anagnostopoulos, F.; Paraponiari, A.; Kafetsios, K. The Role of Pain Catastrophizing, Emotional Intelligence, and Pain Intensity in the Quality of Life of Cancer Patients with Chronic Pain. J. Clin. Psychol. Med. Settings 2023, 30, 501–519. [Google Scholar] [CrossRef] [PubMed]
- Thompson, O.J.; Powell-Roach, K.; Taylor, J.L.; Terry, E.L.; Booker, S.Q. Pain catastrophizing: A patient-centered approach to assessment. Nursing 2022, 52, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Dugas, M.J.; Giguère Marchal, K.; Cormier, S.; Bouchard, S.; Gouin, J.P.; Shafran, R. Pain catastrophizing and worry about health in generalized anxiety disorder. Clin. Psychol. Psychother. 2023, 30, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Quartana, P.J.; Campbell, C.M.; Edwards, R.R. Pain catastrophizing: A critical review. Expert Rev. Neurother. 2009, 9, 745–758. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.L.; Tripp, D.A. Pain Catastrophizing: Controversies, Misconceptions and Future Directions. J. Pain 2024, 25, 575–587. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Scott, W.; De Paepe, A.L. Knowing What We Are Talking About: The Case of Pain Catastrophizing. J. Pain 2024, 25, 591–594. [Google Scholar] [CrossRef] [PubMed]
- Leung, L. Pain catastrophizing: An updated review. Indian J. Psychol. Med. 2012, 34, 204–217. [Google Scholar] [CrossRef] [PubMed]
- Novak, C.B.; Anastakis, D.J.; Beaton, D.E.; Mackinnon, S.E.; Katz, J. Biomedical and psychosocial factors associated with disability after peripheral nerve injury. J. Bone Joint Surg. Am. 2011, 93, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Pinto, P.R.; McIntyre, T.; Araújo-Soares, V.; Costa, P.; Almeida, A. Differential predictors of acute post-surgical pain intensity after abdominal hysterectomy and major joint arthroplasty. Ann. Behav. Med. 2015, 49, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Shelby, R.A.; Somers, T.J.; Keefe, F.J.; Silva, S.G.; McKee, D.C.; She, L.; Waters, S.J.; Varia, I.; Riordan, Y.B.; Knowles, V.M.; et al. Pain catastrophizing in patients with noncardiac chest pain: Relationships with pain, anxiety, and disability. Psychosom. Med. 2009, 71, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Shim, E.J.; Park, A.; Park, S.P. The relationship between alexithymia and headache impact: The role of somatization and pain catastrophizing. Qual. Life Res. 2018, 27, 2283–2294. [Google Scholar] [CrossRef] [PubMed]
- Craner, J.R.; Sperry, J.A.; Evans, M.M. The Relationship Between Pain Catastrophizing and Outcomes of a 3-Week Comprehensive Pain Rehabilitation Program. Pain Med. 2016, 17, 2026–2035. [Google Scholar] [CrossRef] [PubMed]
- Elvery, N.; Jensen, M.P.; Ehde, D.M.; Day, M.A. Pain Catastrophizing, Mindfulness, and Pain Acceptance. Clin. J. Pain 2017, 33, 485–495. [Google Scholar] [CrossRef]
- Flink, I.K.; Engman, L.; Thomtén, J.; Linton, S.J. The role of catastrophizing in vulvovaginal pain: Impact on pain and partner responses over time. J. Appl. Behav. Res. 2017, 22, e12093. [Google Scholar] [CrossRef]
- Belfer, I.; Schreiber, K.L.; Shaffer, J.R.; Shnol, H.; Blaney, K.; Morando, A.; Englert, D.; Greco, C.; Brufsky, A.; Ahrendt, G.; et al. Persistent Postmastectomy Pain in Breast Cancer Survivors: Analysis of Clinical, Demographic, and Psychosocial Factors. J. Pain 2013, 14, 1185–1195. [Google Scholar] [CrossRef] [PubMed]
- Harrison, A.M.; Silber, E.; McCracken, L.M.; Moss-Morris, R. Beyond a Physical Symptom: The Importance of Psychosocial Factors in Multiple Sclerosis Pain. Eur. J. Neurol. 2015, 22, 1443–1452. [Google Scholar] [CrossRef]
- Shim, E.J.; Song, Y.W.; Park, S.H.; Lee, K.M.; Go, D.J.; Hahm, B.J. Examining the Relationship Between Pain Catastrophizing and Suicide Risk in Patients with Rheumatic Disease: The Mediating Role of Depression, Perceived Social Support, and Perceived Burdensomeness. Int. J. Behav. Med. 2017, 24, 501–512. [Google Scholar] [CrossRef]
- Morasco, B.J.; Lovejoy, T.I.; Turk, D.C.; Crain, A.; Hauser, P.; Dobscha, S.K. Biopsychosocial factors associated with pain in veterans with the hepatitis C virus. J. Behav. Med. 2014, 37, 902–911. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, J.; Barandouzi, Z.A.; Lee, J.; Xu, W.; Feng, B.; Starkweather, A.; Cong, X. Psychosocial and Sensory Factors Contribute to Self-Reported Pain and Quality of Life in Young Adults with Irritable Bowel Syndrome. Pain Manag. Nurs. 2022, 23, 646–654. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zhang, X.; You, B.; Jiang, G.; Chen, H.; Jackson, T. Pain Catastrophizing Dimensions Mediate the Relationship between Chronic Pain Severity and Depression. Pain Manag. Nurs. 2024, 25, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Singh, S.P.; Clement, A.; Calfee, R.P.; Bijsterbosch, J.D.; Cheng, A.L. Improvements in Physical Function and Pain Interference and Changes in Mental Health Among Patients Seeking Musculoskeletal Care. JAMA Netw. Open 2023, 6, e2320520. [Google Scholar] [CrossRef] [PubMed]
- Ellis, A. Reason and Emotion in Psychotherapy; Stuart: New York, NY, USA, 1962. [Google Scholar]
- Beck, A.T.; Emery, C.F. Anxiety Disorders and Phobias: A Cognitive Perspective; Basic Books: New York, NY, USA, 1985. [Google Scholar]
- Sullivan, M.; Thorn, B.; Haythornthwaite, J.A.; Keefe, F.; Martin, M.; Bradley, L.A.; Lefebvre, J.C. Theoretical perspectives on the relation between catastrophizing and pain. Clin. J. Pain 2001, 17, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Gellatly, R.; Beck, A. Catastrophic Thinking: A Transdiagnostic Process Across Psychiatric Disorders. Cogn. Ther. Res. 2016, 40, 441–452. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Crombez, G.; Linton, S.J. The fear-avoidance model of pain. Pain 2016, 157, 1588–1589. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S.; Wisco, B.E.; Lyubomirsky, S. Rethinking rumination. Perspect. Psychol. Sci. 2008, 3, 400–424. [Google Scholar] [CrossRef] [PubMed]
- Schütze, R.; Rees, C.; Smith, A.; Slater, H.; O’Sullivan, P. Metacognition, perseverative thinking, and pain catastrophizing: A moderated-mediation analysis. Eur. J. Pain Lond. Engl. 2020, 24, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Schütze, R.; Rees, C.S.; Smith, A.J.; Slater, H.; Catley, M.; O’Sullivan, P. Assessing beliefs underlying rumination about pain: Development and validation of the pain metacognitions questionnaire. Front. Psychol. 2019, 10, 10. [Google Scholar] [CrossRef]
- Aldrich, S.; Eccleston, C.; Crombez, G. Worrying about Chronic Pain: Vigilance to Threat and Misdirected Problem Solving. Behav. Res. Ther. 2000, 38, 457–470. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.S.; Karoly, P. Fear-Avoidance Model of Chronic Pain. Clin. J. Pain 2012, 28, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, A.T.; Bockow, T.B.; Jensen, M.P. Catastrophizing, pain, and pain interference in individuals with disabilities. Am. J. Phys. Med. Rehabil. 2011, 90, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Slepian, P.M.; Ankawi, B.; France, C.R. Longitudinal analysis supports a fear-avoidance model that incorporates pain resilience alongside pain catastrophizing. Ann. Behav. Med. Publ. Soc. Behav. Med. 2020, 54, 335–345. [Google Scholar] [CrossRef] [PubMed]
- De Deurwaerdère, P.; Di Giovanni, G. Serotonin in Health and Disease. Int. J. Mol. Sci. 2020, 21, 3500. [Google Scholar] [CrossRef]
- Horjales-Araujo, E.; Demontis, D.; Lund, E.K.; Finnerup, N.B.; Børglum, A.D.; Jensen, T.S. Polymorphism in serotonin receptor 3B is associated with pain catastrophizing. PLoS ONE 2013, 8, e78889. [Google Scholar] [CrossRef] [PubMed]
- Soriano, A.; Allen, A.; Malykhina, A.P.; Andy, U.; Harvie, H.; Arya, L. Relationship of Pain Catastrophizing with Urinary Biomarkers in Women with Bladder Pain Syndrome. Female Pelvic Med. Reconstr. Surg. 2021, 27, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Chamessian, A.; Van de Ven, T.; Buchheit, T.; Hsia, H.L.; McDuffie, M.; Gamazon, E.R. Differential expression of systemic inflammatory mediators in amputees with chronic residual limb pain. Pain 2017, 158, 68–74. [Google Scholar] [CrossRef]
- Giordano, R.; Capriotti, C.; Gerra, M.C.; Kappel, A.; Østgaard, S.E.; Dallabona, C.; Arendt-Nielsen, L.; Petersen, K.-S. A potential link between inflammatory profiles, clinical pain, pain catastrophizing and long-term outcomes after total knee arthroplasty surgery. Eur. J. Pain 2024, 1–11. [Google Scholar] [CrossRef]
- Cook, A.D.; Pobjoy, J.; Sarros, S.; Steidl, S.; Dürr, M.; Lacey, D.C.; Hamilton, J.A. Granulocyte-macrophage colony-stimulating factor is a key mediator in inflammatory and arthritic pain. Ann. Rheum. Dis. 2013, 72, 265–270. [Google Scholar] [CrossRef]
- Alves, C.F.D.S.; Caumo, W.; Silvestri, J.M.; Zortea, M.; Santos VS, D.; Cardoso, D.F. Pain catastrophizing is associated with the Val66Met polymorphism of the brain-derived neurotrophic factor in fibromyalgia. Adv. Rheumatol. 2020, 60, 39. [Google Scholar] [CrossRef] [PubMed]
- Arora, V.; Martin, T.J.; Aschenbrenner, C.A.; Hayashida, K.; Kim, S.A.; Parker, R.A. Psychosocial Stress Delays Recovery of Postoperative Pain Following Incisional Surgery in the Rat. Neuroscience 2018, 382, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Jee, H.J.; Zhu, E.; Sun, M.; Liu, W.; Zhang, Q.; Wang, J. Anterior cingulate cortex regulates pain catastrophizing-like behaviors in rats. Mol. Brain 2023, 16, 71. [Google Scholar] [CrossRef]
- Galambos, A.; Szabó, E.; Nagy, Z.; Édes, A.E.; Kocsel, N.; Juhász, G.; Kökönyei, G. A systematic review of structural and functional MRI studies on pain catastrophizing. J. Pain Res. 2019, 12, 1155–1178. [Google Scholar] [CrossRef] [PubMed]
- Malfliet, A.; Coppieters, I.; Van Wilgen, P.; Kregel, J.; De Pauw, R.; Dolphens, M.; Ickmans, K. Brain changes associated with cognitive and emotional factors in chronic pain: A systematic review. Eur. J. Pain 2017, 21, 769–786. [Google Scholar] [CrossRef] [PubMed]
- Blankstein, U.; Chen, J.; Diamant, N.E.; Davis, K.D. Altered Brain Structure in Irritable Bowel Syndrome: Potential Contributions of Pre-Existing and Disease-Driven Factors. Gastroenterology 2010, 138, 1783–1789. [Google Scholar] [CrossRef] [PubMed]
- Seminowicz, D.A.; Shpaner, M.; Keaser, M.L.; Krauthamer, G.M.; Mantegna, J.; Dumas, J.A. Cognitive-behavioral therapy increases prefrontal cortex gray matter in patients with chronic pain. J. Pain 2013, 14, 1573–1584. [Google Scholar] [CrossRef] [PubMed]
- Terry, E.L.; Tanner, J.J.; Cardoso, J.S.; Sibille, K.T.; Lai, S.; Deshpande, H. Associations between pain catastrophizing and resting-state functional brain connectivity: Ethnic/race group differences in persons with chronic knee pain. J. Neurosci. Res. 2022, 100, 1047–1062. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.L.; Bishop, S.R.; Pivik, J. The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Bot, A.G.; Becker, S.J.; Bruijnzeel, H.; Mulders, M.A.; Ring, D.; Vranceanu, A.M. Creation of the abbreviated measures of the Pain Catastrophizing Scale and the Short Health Anxiety Inventory: The PCS-4 and SHAI-5. J. Musculoskelet. Pain. 2014, 22, 145–151. [Google Scholar] [CrossRef]
- McWilliams, L.A.; Kowal, J.; Wilson, K.G. Development and evaluation of short forms of the Pain Catastrophizing Scale and the Pain Self-Efficacy Questionnaire. Eur. J. Pain 2015, 19, 1342–1349. [Google Scholar] [CrossRef] [PubMed]
- Franchignoni, F.; Giordano, A.; Ferriero, G.; Monticone, M. Measurement Precision of the Pain Catastrophizing Scale and Its Short Forms in Chronic Low Back Pain. Sci. Rep. 2022, 12, 12042. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Bijttebier, P.; Eccleston, C.; Mascagni, T.; Mertens, G.; Goubert, L.; Verstraeten, K. The child version of the pain catastrophizing scale (PCS-C): A preliminary validation. Pain 2003, 104, 639–646. [Google Scholar] [CrossRef]
- Rosenstiel, A.K.; Keefe, F.J. The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain 1983, 17, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; De Paepe, A.L.; Veirman, E.; Eccleston, C.; Verleysen, G.; Van Ryckeghem, D.M.L. Let’s Talk About Pain Catastrophizing Measures: An Item Content Analysis. PeerJ 2020, 8, e8643. [Google Scholar] [CrossRef] [PubMed]
- Shipton, E.E.; Bate, F.; Garrick, R.; Steketee, C.; Shipton, E.A.; Visser, E.J. Systematic Review of Pain Medicine Content, Teaching, and Assessment in Medical School Curricula Internationally. Pain Ther. 2018, 7, 139–161. [Google Scholar] [CrossRef] [PubMed]
- Ikemoto, T.; Hayashi, K.; Shiro, Y.; Arai, Y.C.; Marcuzzi, A.; Costa, D.; Wrigley, P. A systematic review of cross-cultural validation of the pain catastrophizing scale. Eur. J. Pain 2020, 24, 1228–1241. [Google Scholar] [CrossRef]
- Brouwer, B.; Waardenburg, S.; Jacobs, C.; Overdijk, M.; Leue, C.; Köke, A.; Kuijk, S.V.; van Kleef, M.; Van Zundert, J.; de Meij, N. Biopsychosocial baseline values of 15,000 patients suffering from chronic pain: Dutch DataPain study. Reg. Anesth. Pain Med. 2020, 45, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Day, M.A.; Thorn, B.E. The Relationship of Demographic and Psychosocial Variables to Pain-Related Outcomes in a Rural Chronic Pain Population. Pain 2010, 151, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Blanco, E.I.; Meca, A.; Unger, J.B.; Romero, A.; Szapocznik, J.; Piña-Watson, B.; Cano, M.Á.; Zamboanga, B.L.; Baezconde-Garbanati, L.; Des Rosiers, S.E.; et al. Longitudinal Effects of Latino Parent Cultural Stress, Depressive Symptoms, and Family Functioning on Youth Emotional Well-Being and Health Risk Behaviors. Fam. Process 2017, 56, 981–996. [Google Scholar] [CrossRef] [PubMed]
- Zvolensky, M.J.; Kauffman, B.Y.; Shepherd, J.M.; Viana, A.G.; Bogiaizian, D.; Rogers, A.H.; Bakhshaie, J.; Peraza, N. Pain-Related Anxiety Among Latinx College Students: Relations to Body Vigilance, Worry, Anxious Arousal, and General Depression. J. Racial Ethn. Health Disparities 2020, 7, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Crombez, G. Pain Demands Attention: A Cognitive-Affective Model of the Interruptive Function of Pain. Psychol. Bull. 1999, 125, 356–366. [Google Scholar] [CrossRef] [PubMed]
- Rischer, K.M.; González-Roldán, A.M.; Montoya, P.; Gigl, S.; Anton, F.; van der Meulen, M. Distraction from pain: The role of selective attention and pain catastrophizing. Eur. J. Pain. 2020, 24, 1880–1891. [Google Scholar] [CrossRef] [PubMed]
- Asefi Rad, A.; Wippert, P.M. Insights into pain distraction and the impact of pain catastrophizing on pain perception during different types of distraction tasks. Front. Pain Res. 2024, 5, 1266974. [Google Scholar] [CrossRef] [PubMed]
- Kjøgx, H.; Kasch, H.; Zachariae, R.; Svensson, P.; Jensen, T.S.; Vase, L. Experimental manipulations of pain catastrophizing influence pain levels in patients with chronic pain and healthy volunteers. Pain 2016, 157, 1287–1296. [Google Scholar] [CrossRef] [PubMed]
- Goodin, B.R.; Bulls, H.W. Optimism and the Experience of Pain: Benefits of Seeing the Glass as Half Full. Curr. Pain Headache Rep. 2013, 17, 329. [Google Scholar] [CrossRef]
- Guglielmo, D.; Hootman, J.M.; Boring, M.A.; Murphy, L.B.; Theis, K.A.; Croft, J.B. Symptoms of Anxiety and Depression Among Adults with Arthritis—United States, 2015–2017. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1081–1087. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.J.G.; Katz, J. Understanding the Co-occurrence of Anxiety Disorders and Chronic Pain: State-of-the-Art. Depress. Anxiety 2009, 26, 888–901. [Google Scholar] [CrossRef] [PubMed]
- Demyttenaere, K.; Bruffaerts, R.; Lee, S.; Posada-Villa, J.; Kovess, V.; Angermeyer, M.C. Mental Disorders Among Persons with Chronic Back or Neck Pain: Results from the World Mental Health Surveys. Pain 2007, 129, 332–342. [Google Scholar] [CrossRef] [PubMed]
- Bair, M.J.; Robinson, R.L.; Katon, W.; Kroenke, K. Depression and pain comorbidity: A literature review. Arch. Intern. Med. 2003, 163, 2433–2445. [Google Scholar] [CrossRef] [PubMed]
- DeVeaugh-Geiss, A.M.; West, S.L.; Miller, W.C.; Sleath, B.; Gaynes, B.N.; Kroenke, K. The Adverse Effects of Comorbid Pain on Depression Outcomes in Primary Care Patients: Results from the ARTIST Trial. Pain Med. 2010, 11, 732–741. [Google Scholar] [CrossRef] [PubMed]
- Hettich, N.; Entringer, T.M.; Kroeger, H.; Schmidt, P.; Tibubos, A.N.; Braehler, E.; Beutel, M.E. Impact of the COVID-19 pandemic on depression, anxiety, loneliness, and satisfaction in the German general population: A longitudinal analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 2481–2490. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Cano, H.J.; Moreno-Murguía, M.B.; Morales-López, O.; Crow-Buchanan, O.; English, J.A.; Lozano-Alcázar, J.; Somilleda-Ventura, S.A. Anxiety, depression, and stress in response to the coronavirus disease-19 pandemic. Cir. Cir. 2020, 88, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Kwon, C.Y.; Lee, B. Prevalence of suicidal behavior in patients with chronic pain: A systematic review and meta-analysis of observational studies. Front. Psychol. 2023, 14, 1217299. [Google Scholar] [CrossRef]
- Brown, L.A.; Lynch, K.G.; Cheatle, M. Pain catastrophizing as a predictor of suicidal ideation in chronic pain patients with an opiate prescription. Psychiatry Res. 2020, 286, 112893. [Google Scholar] [CrossRef]
- Noyman-Veksler, G.; Lerman, S.F.; Joiner, T.E.; Brill, S.; Rudich, Z.; Shalev, H.; Shahar, G. Role of Pain-Based Catastrophizing in Pain, Disability, Distress, and Suicidal Ideation. Psychiatry 2017, 80, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Edwards, R.R.; Smith, M.T.; Kudel, I.; Haythornthwaite, J. Pain-related catastrophizing as a risk factor for suicidal ideation in chronic pain. Pain 2006, 126, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Crawford, A.; Muere, A.; Tripp, D.A.; Nickel, J.C.; Doiron, R.C.; Moldwin, R.; Katz, L. The Chicken or the Egg: Longitudinal Changes in Pain and Catastrophizing in Women with Interstitial Cystitis/Bladder Pain Syndrome. Can. Urol. Assoc. J. 2021, 15, 326–331. [Google Scholar] [CrossRef]
- Doğru, H.Y.; Özsoy, F.; Doğru, S.; Karaman, T.; Şahin, A.; Özsoy, A.Z. Catastrophizing, Depression and Anxiety During Pregnancy: Relation Between Lumbopelvic Pain and Physical/Social Functioning. J. Ration.-Emotive Cogn.-Behav. Ther. 2018, 36, 119–136. [Google Scholar] [CrossRef]
- Harris, J.I.; Usset, T.; Krause, L.; Schill, D.; Reuer, B.; Donahue, R.; Park, C.L. Spiritual/Religious Distress Is Associated with Pain Catastrophizing and Interference in Veterans with Chronic Pain. Pain Med. 2018, 19, 757–763. [Google Scholar] [CrossRef]
- Lackner, J.M.; Quigley, B.M. Pain catastrophizing mediates the relationship between worry and pain suffering in patients with irritable bowel syndrome. Behav. Res. Ther. 2005, 43, 943–957. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi Nasiri, F.S.; Pakdaman, S.; Dehghani, M.; Togha, M. The relationship between pain catastrophizing and headache-related disability: The mediating role of pain intensity. Jpn. Psychol. Res. 2017, 59, 266–274. [Google Scholar] [CrossRef]
- Newman, A.K.; Van Dyke, B.P.; Torres, C.A.; Baxter, J.W.; Eyer, J.C.; Kapoor, S.; Thorn, B.E. The relationship of sociodemographic and psychological variables with chronic pain variables in a low-income population. Pain 2017, 158, 1687–1696. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Yoon, D.M.; Yoon, K.B.; Moon, J.A.; Kim, S.H. Factors Associated with Higher Reported Pain Levels in Patients with Chronic Musculoskeletal Pain: A Cross-Sectional, Correlational Analysis. PLoS ONE 2016, 11, e0163132. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.S.; Davis, M.C.; Yeung, E.W.; Zautra, A.J.; Tennen, H.A. Relations between adaptive and maladaptive pain cognitions and within-day pain exacerbations in individuals with fibromyalgia. J. Behav. Med. 2017, 40, 458–467. [Google Scholar] [CrossRef]
- Burns, J.W.; Kubilus, A.; Bruehl, S.; Harden, R.N.; Lofland, K. Do Changes in Cognitive Factors Influence Outcome Following Multidisciplinary Treatment for Chronic Pain? A Cross-Lagged Panel Analysis. J. Consult. Clin. Psychol. 2003, 71, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.M.; McCauley, L.; Bounds, S.C.; Mathur, V.A.; Conn, L.; Simango, M.; Edwards, R.R.; Fontaine, K.R. Changes in Pain Catastrophizing Predict Later Changes in Fibromyalgia Clinical and Experimental Pain Report: Cross-Lagged Panel Analyses of Dispositional and Situational Catastrophizing. Arthritis Res. Ther. 2012, 14, R231. [Google Scholar] [CrossRef] [PubMed]
- Burns, L.C.; Ritvo, S.E.; Ferguson, M.K.; Clarke, H.; Seltzer, Z.; Katz, J. Pain Catastrophizing as a Risk Factor for Chronic Pain after Total Knee Arthroplasty: A Systematic Review. J. Pain Res. 2015, 8, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Arteta, J.; Cobos, B.; Hu, Y.; Jordan, K.; Howard, K. Evaluation of How Depression and Anxiety Mediate the Relationship Between Pain Catastrophizing and Prescription Opioid Misuse in a Chronic Pain Population. Pain Med. 2016, 17, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Riggs, K.R.; Cherrington, A.L.; Kertesz, S.G.; Richman, J.S.; DeRussy, A.J.; Varley, A.L. Higher Pain Catastrophizing and Preoperative Pain is Associated with Increased Risk for Prolonged Postoperative Opioid Use. Pain Physician 2023, 26, E73–E82. [Google Scholar] [PubMed]
- Nazarian, A.; Negus, S.S.; Martin, T.J. Factors mediating pain-related risk for opioid use disorder. Neuropharmacology 2021, 186, 108476. [Google Scholar] [CrossRef] [PubMed]
- Cooperman, N.A.; Hanley, A.W.; Kline, A.; Garland, E.L. A pilot randomized clinical trial of mindfulness-oriented recovery enhancement as an adjunct to methadone treatment for people with opioid use disorder and chronic pain: Impact on illicit drug use, health, and well-being. J. Subst. Abuse Treat. 2021, 127, 108468. [Google Scholar] [CrossRef]
- Garland, E.L.; Hanley, A.W.; Nakamura, Y.; Barrett, J.W.; Baker, A.K.; Reese, S.E. Mindfulness-Oriented Recovery Enhancement vs Supportive Group Therapy for Co-occurring Opioid Misuse and Chronic Pain in Primary Care: A Randomized Clinical Trial. JAMA Intern. Med. 2022, 182, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Davydov, D.M.; Galvez-Sánchez, C.M.; Montoro, C.I.; de Guevara, C.M.L.; Reyes Del Paso, G.A. Personalized behavior management as a replacement for medications for pain control and mood regulation. Sci. Rep. 2021, 11, 20297. [Google Scholar] [CrossRef] [PubMed]
- Suso-Ribera, C.; García-Palacios, A.; Botella, C.; Ribera-Canudas, M.V. Pain Catastrophizing and Its Relationship with Health Outcomes: Does Pain Intensity Matter? Pain Res. Manag. 2017, 2017, 9762864. [Google Scholar] [CrossRef]
- Wheeler, C.H.B.; Williams, A.C.C.; Morley, S.J. Meta-analysis of the psychometric properties of the Pain Catastrophizing Scale and associations with participant characteristics. Pain 2019, 160, 1946–1953. [Google Scholar] [CrossRef] [PubMed]
- Goya Arce, A.B.; Richardson, P.A.; Tran, S.T.; Bhandari, R.P. Comparison of Pain and Psychosocial Correlates Among Hispanic and Non-Hispanic White Youth with Chronic Pain. Pain Rep. 2022, 7, e1020. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Crombez, G. Advancing Psychological Therapies for Chronic Pain. F1000Research 2017, 6, 461. [Google Scholar] [CrossRef] [PubMed]
- Burns, J.W.; Day, M.A.; Thorn, B.E. Is Reduction in Pain Catastrophizing a Therapeutic Mechanism Specific to Cognitive-Behavioral Therapy for Chronic Pain? Transl. Behav. Med. 2012, 2, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Corsi, N.; Colloca, L. Placebo and Nocebo Effects: The Advantage of Measuring Expectations and Psychological Factors. Front. Psychol. 2017, 8, 308. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.A.; Anderson, M.L.; Balderson, B.H.; Cook, A.J.; Sherman, K.J.; Cherkin, D.C. Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: Similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain 2016, 157, 2434–2444. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Calderon, J.; García-Muñoz, C.; Rufo-Barbero, C.; Matias-Soto, J.; Cano-García, F.J. Acceptance and Commitment Therapy for Chronic Pain: An Overview of Systematic Reviews with Meta-Analysis of Randomized Clinical Trials. J. Pain 2024, 25, 595–617. [Google Scholar] [CrossRef] [PubMed]
- Alcon, C.; Bergman, E.; Humphrey, J.; Patel, R.M.; Wang-Price, S. The Relationship between Pain Catastrophizing and Cognitive Function in Chronic Musculoskeletal Pain: A Scoping Review. Pain Res. Manag. 2023, 2023, 5851450. [Google Scholar] [CrossRef] [PubMed]
- Jay, K.; Brandt, M.; Hansen, K.; Sundstrup, E.; Jakobsen, M.D.; Schraefel, M.C. Effect of Individually Tailored Biopsychosocial Workplace Interventions on Chronic Musculoskeletal Pain and Stress Among Laboratory Technicians: Randomized Controlled Trial. Pain Physician 2015, 18, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Angst, F.; Lehmann, S.; Sandor, P.S.; Benz, T. Catastrophizing as a prognostic factor for pain and physical function in the multidisciplinary rehabilitation of fibromyalgia and low back pain. Eur. J. Pain 2022, 26, 1569–1580. [Google Scholar] [CrossRef] [PubMed]
- Lai, L.; Liu, Y.; McCracken, L.M.; Li, Y.; Ren, Z. The efficacy of acceptance and commitment therapy for chronic pain: A three-level meta-analysis and a trial sequential analysis of randomized controlled trials. Behav. Res. Ther. 2023, 165, 104308. [Google Scholar] [CrossRef] [PubMed]
- Alda, M.; Luciano, J.V.; Andrés, E.; Serrano-Blanco, A.; Rodero, B.; del Hoyo, Y.L. Effectiveness of Cognitive Behaviour Therapy for the Treatment of Catastrophisation in Patients with Fibromyalgia: A Randomised Controlled Trial. Arthritis Res. Ther. 2011, 13, R173. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.N.; Chen, W.; Zhang, Y.; Zhang, Y.; Feng, S.; Chen, X.Y. Does cognitive behavioral education reduce pain and improve joint function in patients after total knee arthroplasty? A randomized controlled trial. Int. Orthop. 2020, 44, 2027–2035. [Google Scholar] [CrossRef]
- Buhrman, M.; Nilsson-Ihrfeldt, E.; Jannert, M.; Ström, L.; Andersson, G. Guided Internet-Based Cognitive Behavioural Treatment for Chronic Back Pain Reduces Pain Catastrophizing: A Randomized Controlled Trial. J. Rehabil. Med. 2011, 43, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Garland, E.L.; Gaylord, S.A.; Palsson, O.; Faurot, K.; Douglas Mann, J.; Whitehead, W.E. Therapeutic Mechanisms of a Mindfulness-Based Treatment for IBS: Effects on Visceral Sensitivity, Catastrophizing, and Affective Processing of Pain Sensations. J. Behav. Med. 2012, 35, 591–602. [Google Scholar] [CrossRef] [PubMed]
- la Cour, P.; Petersen, M. Effects of mindfulness meditation on chronic pain: A randomized controlled trial. Pain Med. 2015, 16, 641–652. [Google Scholar] [CrossRef] [PubMed]
- Cherkin, D.C.; Sherman, K.J.; Balderson, B.H.; Cook, A.J.; Anderson, M.L.; Hawkes, R.J.; Hansen, K.E.; Turner, J.A. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults with Chronic Low Back Pain: A Randomized Clinical Trial. JAMA 2016, 315, 1240–1249. [Google Scholar] [CrossRef] [PubMed]
- Meeus, M.; Nijs, J.; Van Oosterwijck, J.; Van Alsenoy, V.; Truijen, S. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: A double-blind randomized controlled trial. Arch. Phys. Med. Rehabil. 2010, 91, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Condition | N | Country | Study Design | Findings |
|---|---|---|---|---|---|
| Belfer et al. (2013) [19] | Persistent Postmastectomy Pain (PPMP) | 611 | United States | Cross-Sectional | Catastrophizing was highly correlated with PPMP, especially within the first two years of surgery. Furthermore, catastrophizing along with anxiety, somatization, and sleep was associated with higher pain-related disability in patients. |
| Chen et al. (2022) [23] | Irritable Bowel Syndrome (IBS) | 80 | United States | Cross-Sectional | Psychosocial factors including catastrophizing, such as coping and self-efficacy, were strongly correlated with pain intensity and quality of life in young adults with IBS. |
| Craner et al. (2016) [16] | Chronic Pain Rehabilitation | 648 | United States | Within-Subject | There was a significant association between pain catastrophizing and decreased mental and physical health-related quality of life, higher pain severity, and life interference in patients with chronic pain. Moreover, participation in a comprehensive rehabilitation program significantly decreased pain catastrophizing in patients, which in turn positively affected treatment outcomes. |
| Crawford et al. (2021) [82] | Interstitial Cystitis/Bladder Pain Syndrome | 226 1 | United States and Canada | Prospective Cohort | There was a temporal correlation between catastrophizing and pain, such that early changes in magnification predicted future changes in pain levels, and early changes in pain levels predicted future changes in rumination. |
| Doğru et al. (2018) [83] | Lumbopelvic Pain in Pregnancy | 429 | Turkey | Prospective Cohort | Pain catastrophizing fluctuated during the course of pregnancy, and was significantly correlated with depression, anxiety, physical and social functioning, and mental health. |
| Elvery et al. (2017) [17] | Chronic and Intermittent pain | 260 | Australia | Cross-Sectional | A significant correlation was found between pain catastrophizing and pain intensity, interference, and depression. Pain catastrophizing was shown to have the most robust association among patients with chronic and intermittent pain. |
| Flink et al. (2017) [18] | Vulvovaginal Pain | 510 | Sweden | Prospective Cohort | Catastrophizing was found to be a significant mediator between solicitous partner responses and pain. |
| Harris et al. (2017) [84] | Chronic Pain | 436 | United States | Cross-Sectional | Pain catastrophizing was related to spiritual distress directly, as well as through its relationship with depression. Pain interference was also associated with spiritual distress; however, only through its relationship with depression. |
| Harrison et al. (2015) [20] | Multiple Sclerosis Pain | 612 | United Kingdom | Cross-Sectional | Psychological factors, including catastrophizing, as well as distress, negative beliefs about pain, and avoidance of activity, were associated with worse pain intensity and outcomes. |
| Ikemoto et al. (2017) [61] | Knee Osteoarthritis | 77 | Japan | Cross-Sectional | In female patients with knee osteoarthritis, pain catastrophizing has been highly correlated to pain severity and quality of life. |
| Kjøgx et al. (2016) [69] | Chronic Headache | 44 | Denmark | Randomized Controlled Trial | Hypnotic suggestions significantly affected pain catastrophizing, as well as the levels of pain intensity and pain unpleasantness, with changes in pain catastrophizing being predictors of the changes in pain. |
| Lackner et al. (2005) [85] | Irritable Bowel Syndrome (IBS) | 186 | United States | Cross-Sectional | Worry was strongly associated with the emotionally unpleasant aspects of pain, especially suffering, and pain catastrophizing was found to be the mediating factor between the two. |
| Morasco et al. (2014) [22] | Hepatitis C | 116 | United States | Cross-Sectional | Pain catastrophizing and social support were associated with pain intensity, whereas age, pain severity, prescription opioid use, and chronic pain self-efficacy were associated with the level of pain interference. |
| Mortazavi Nasiri et al. (2017) [86] | Migraine | 178 | Iran | Descriptive-Correlational | There was a positive correlation between disability and catastrophizing, with pain intensity as a mediating factor. A high frequency of maladaptive coping strategies such as catastrophizing was found in the population of migraine patients with headache-related disability. |
| Newman et al. (2017) [87] | Chronic Pain | 290 | United States | Cross-Sectional | Depression and catastrophizing were mediating factors for age and various pain outcomes, and catastrophizing mediated the effects of literacy and poverty. |
| Novak et al. (2011) [12] | Peripheral Neve Injury | 158 | Canada | Cross-Sectional | Disability due to pain was predicted by various factors including pain catastrophizing. |
| Noyman-Veksler et al. (2017) [80] | Chronic Pain | 428/165 2 | Israel | Cross-Sectional | Pain catastrophizing was predictive of pain, and distress was predictive of pain-related disability. Pain catastrophizing was also associated with depression and suicidal ideation. |
| Park et al. (2016) [88] | Chronic Musculoskeletal Pain | 357 | Korea | Cross-Sectional | Pain catastrophizing, as well as older age and insomnia, were significantly associated with higher pain levels |
| Pinto et al. (2014) [13] | Acute Postoperative Pain | 252 | Portugal | Prospective Cohort | Pain catastrophizing was found to be a significant predictor for acute postoperative pain. |
| Shelby et al. (2009) [14] | Noncardiac Chest Pain | 97 | United States | Cross-Sectional | Through relationship with pain catastrophizing, chest pain and anxiety were found to indirectly influence physical disability. Chest pain also showed a significant indirect relationship with psychosocial disability through pain catastrophizing. |
| Shim et al. (2017) [21] | Rheumatic Disease | 360 | Korea | Cross-Sectional | Magnification element of pain catastrophizing had a significant indirect relationship with suicide risk through perceived burdensomeness, depression, and perceived social support. |
| Shim et al. (2018) [15] | Headache | 247 | Korea | Cross-Sectional | Pain catastrophizing was found to be the only significant mediator through which alexithymia was associated with headache-related outcomes. |
| Taylor et al. (2017) [89] | Fibromyalgia | 220 | United States | Within-Subject | Catastrophizing and coping efficacy were associated with end-of-day pain in patients with fibromyalgia. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simic, K.; Savic, B.; Knezevic, N.N. Pain Catastrophizing: How Far Have We Come. Neurol. Int. 2024, 16, 483-501. https://doi.org/10.3390/neurolint16030036
Simic K, Savic B, Knezevic NN. Pain Catastrophizing: How Far Have We Come. Neurology International. 2024; 16(3):483-501. https://doi.org/10.3390/neurolint16030036
Chicago/Turabian StyleSimic, Katarina, Boris Savic, and Nebojsa Nick Knezevic. 2024. "Pain Catastrophizing: How Far Have We Come" Neurology International 16, no. 3: 483-501. https://doi.org/10.3390/neurolint16030036
APA StyleSimic, K., Savic, B., & Knezevic, N. N. (2024). Pain Catastrophizing: How Far Have We Come. Neurology International, 16(3), 483-501. https://doi.org/10.3390/neurolint16030036






