Post-Operative Assessment of Ulnar Nerve Tension Using Shear-Wave Elastography
Abstract
:1. Introduction
2. Material and Methods
2.1. Subjects
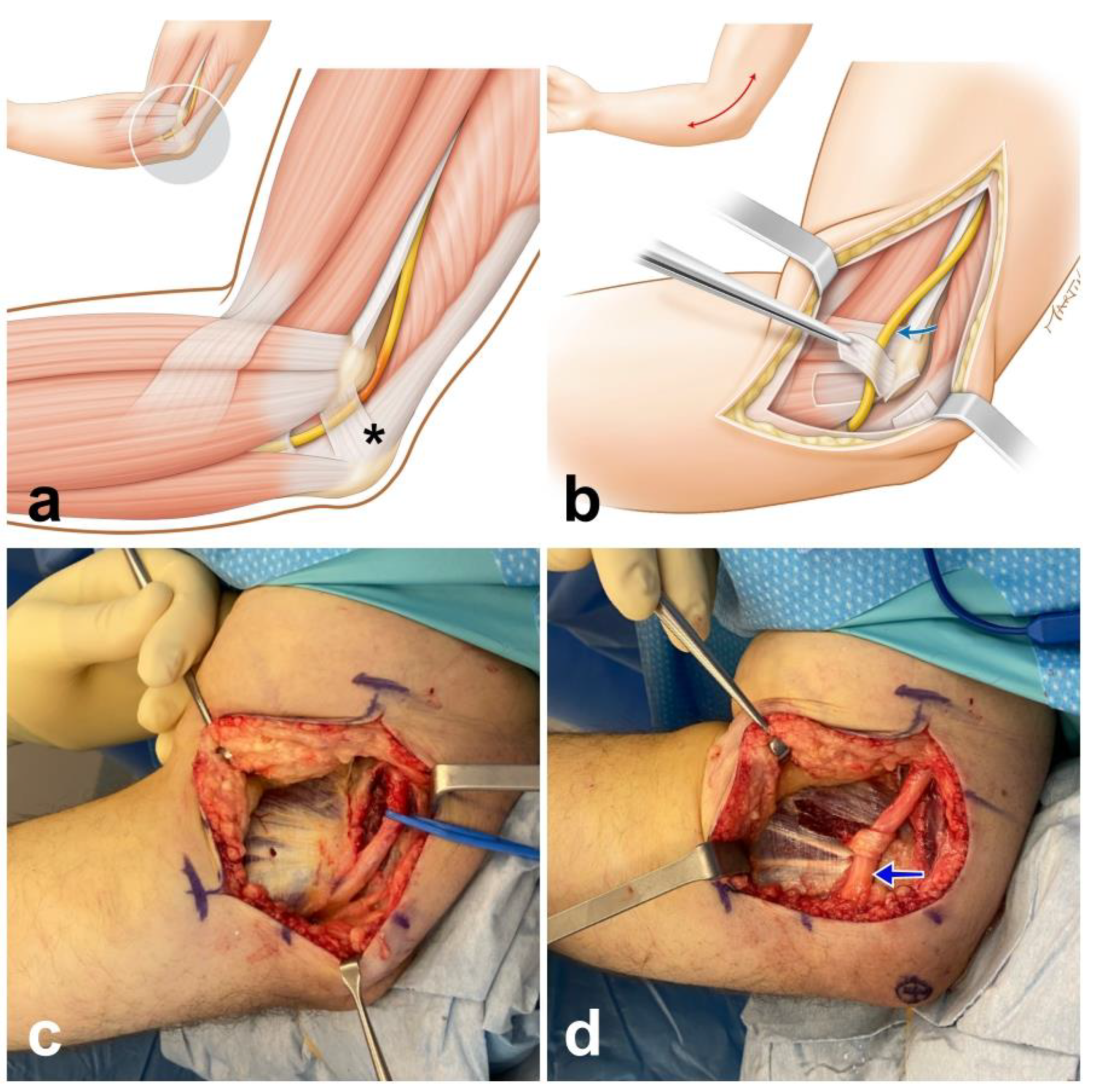
2.2. Operative Procedure
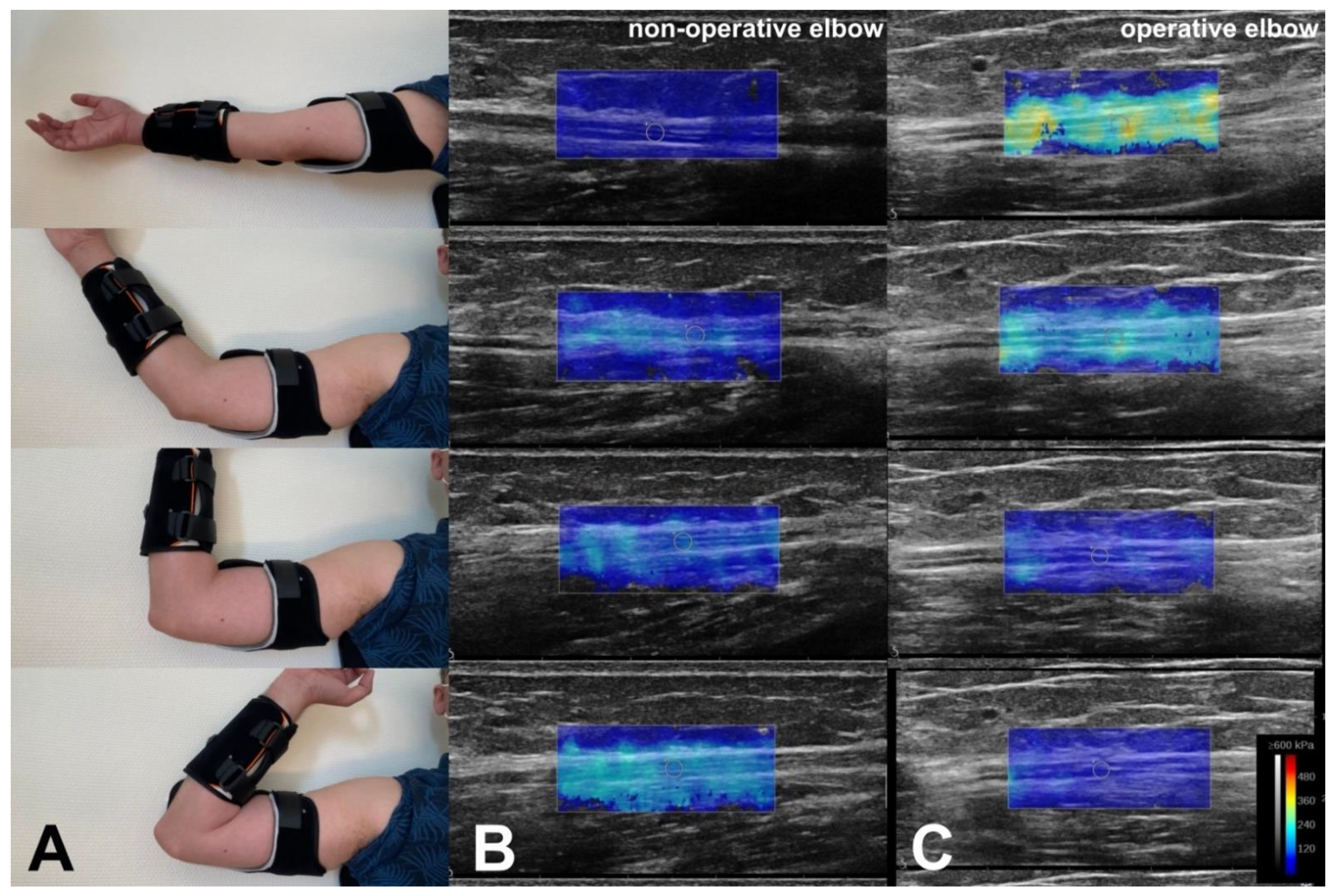
2.3. Ultrasound Protocol
2.4. Statistical Analysis
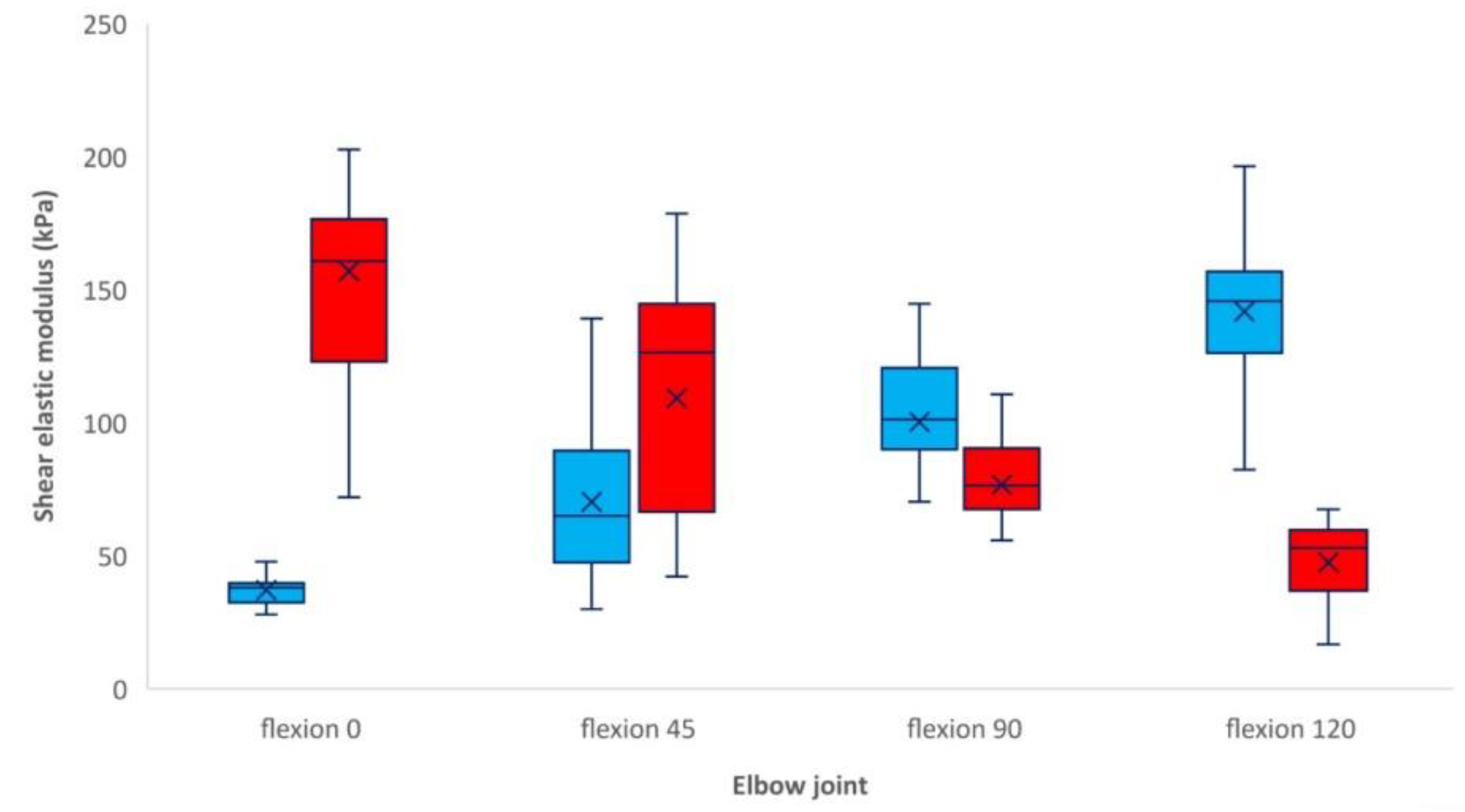
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CSA | cross-sectional area |
| ENMG | electroneuromyography |
| MRI | magnetic resonance imaging |
| SD | standard deviation |
| SW | shear-wave |
| SWE | shear-wave elastography |
References
- Rayegani, S.M.; Raeissadat, S.A.; Kargozar, E.; Rahimi-Dehgolan, S.; Loni, E. Diagnostic value of ultrasonography versus electrodiagnosis in ulnar neuropathy. Med. Devices (Auckl.) 2019, 12, 81–88. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H.; Won, S.J.; Rhee, W.I.; Park, H.J.; Hong, H.M. Diagnostic cutoff value for ultrasonography in the ulnar neuropathy at the elbow. Ann. Rehabil. Med. 2015, 39, 170–175. [Google Scholar] [CrossRef] [Green Version]
- Paluch, Ł.; Noszczyk, B.; Nitek, Ż.; Walecki, J.; Osiak, K.; Pietruski, P. Shear-wave elastography: A new potential method to diagnose ulnar neuropathy at the elbow. Eur. Radiol. 2018, 28, 4932–4939. [Google Scholar] [CrossRef] [Green Version]
- Nakashian, M.N.; Ireland, D.; Kane, P.M. Cubital Tunnel Syndrome: Current Concepts. Curr. Rev. Musculoskelet. Med. 2020, 13, 520–524. [Google Scholar] [CrossRef] [PubMed]
- Wiesler, E.R.; Chloros, G.D.; Cartwright, M.S.; Shin, H.W.; Walker, F.O. Ultrasound in the diagnosis of ulnar neuropathy at the cubital tunnel. J. Hand Surg. Am. 2006, 31, 1088–1093. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Wang, J.; Yang, X.; Zhong, W.; Ma, Q.; Li, S.; Zhang, W. Use of High-Resolution Ultrasonography in Anterior Subcutaneous Transposition of the Ulnar Nerve for Cubital Tunnel Syndrome. Acta Neurochir. Suppl. 2017, 124, 277–281. [Google Scholar] [PubMed]
- Caliandro, P.; La Torre, G.; Padua, R.; Giannini, F.; Padua, L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst. Rev. 2016, 11, CD006839. [Google Scholar] [CrossRef]
- Bedewi, M.A.; Kotb, M.A.; Aldossary, N.M.; Abodonya, A.M.; Alhariqi, B.A.; Swify, S.M. Shear wave elastography of the ulnar nerve at the forearm. Medicine 2021, 100, e24071. [Google Scholar] [CrossRef]
- Staples, J.R.; Calfee, R. Cubital Tunnel Syndrome: Current Concepts. J. Am. Acad. Orthop. Surg. 2017, 25, e215–e224. [Google Scholar] [CrossRef]
- Kim, S.; Lee, G.Y. Evaluation of the ulnar nerve with shear-wave elastography: A potential sonographic method for the diagnosis of ulnar neuropathy. Ultrasonography 2021, 40, 349–356. [Google Scholar] [CrossRef]
- Rugel, C.L.; Franz, C.K.; Lee, S.S.M. Influence of limb position on assessment of nerve mechanical properties by using shear wave ultrasound elastography. Muscle Nerve 2020, 61, 616–622. [Google Scholar] [CrossRef]
- McGowan, A.J. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J. Bone Joint Surg. Br. 1950, 32, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Wee, T.C.; Simon, N.G. Ultrasound elastography for the evaluation of peripheral nerves: A systematic review. Muscle Nerve 2019, 60, 501–512. [Google Scholar] [CrossRef] [PubMed]
- Cornelson, S.M.; Sclocco, R.; Kettner, N.W. Ulnar nerve instability in the cubital tunnel of asymptomatic volunteers. J. Ultrasound 2019, 22, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Terayama, Y.; Uchiyama, S.; Ueda, K.; Iwakura, N.; Ikegami, S.; Kato, Y.; Kato, H. Optimal Measurement Level and Ulnar Nerve Cross-Sectional Area Cutoff Threshold for Identifying Ulnar Neuropathy at the Elbow by MRI and Ultrasonography. J. Hand Surg. Am. 2018, 43, 529–536. [Google Scholar] [CrossRef]
- Yoon, J.S.; Hong, S.J.; Kim, B.J.; Kim, S.J.; Kim, J.M.; Walker, F.O.; Cartwright, M.S. Ulnar nerve and cubital tunnel ultrasound in ulnar neuropathy at the elbow. Arch. Phys. Med. Rehabil. 2008, 89, 887–889. [Google Scholar] [CrossRef]
- Paluch, Ł.; Noszczyk, B.H.; Walecki, J.; Osiak, K.; Kiciński, M.; Pietruski, P. Shear-wave elastography in the diagnosis of ulnar tunnel syndrome. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, 1593–1599. [Google Scholar] [CrossRef]
- Chen, I.J.; Chang, K.V.; Wu, W.T.; Özçakar, L. Ultrasound Parameters Other Than the Direct Measurement of Ulnar Nerve Size for Diagnosing Cubital Tunnel Syndrome: A Systemic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2019, 100, 1114–1130. [Google Scholar] [CrossRef]
- Wright, T.W.; Glowczewskie, F., Jr.; Cowin, D.; Wheeler, D.L. Ulnar nerve excursion and strain at the elbow and wrist associated with upper extremity motion. J. Hand Surg. Am. 2001, 26, 655–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grewal, R.; Varitimidis, S.E.; Vardakas, D.G.; Fu, F.H.; Sotereanos, D.G. Ulnar nerve elongation and excursion in the cubital tunnel after decompression and anterior transposition. J. Hand Surg. Br. 2000, 25, 457–460. [Google Scholar] [CrossRef]
- Terzis, J.; Faibisoff, B.; Williams, B. The nerve gap: Suture under tension vs. graft. Plast. Reconstr. Surg. 1975, 56, 166–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hentz, V.R.; Rosen, J.M.; Xiao, S.J.; McGill, K.C.; Abraham, G. The nerve gap dilemma: A comparison of nerves repaired end to end under tension with nerve grafts in a primate model. J. Hand Surg. Am. 1993, 18, 417–425. [Google Scholar] [CrossRef]
- Sunderland, I.R.; Brenner, M.J.; Singham, J.; Rickman, S.R.; Hunter, D.A.; Mackinnon, S.E. Effect of tension on nerve regeneration in rat sciatic nerve transection model. Ann. Plast. Surg. 2004, 53, 382–387. [Google Scholar] [CrossRef] [PubMed]
| Case | Sex | Age (y) | Operated Side | Grade (McGowan) | Motor Ulnar Nerve Conduction Velocity (m/s) Amplitude (µV) | Time between Surgery and SWE (Months) | Distance Ulnar Nerve/Medial Epicondyle after Transposition (cm) | Shear Elastic Modulus of the Ulnar Nerve (kPa) Non-Operated Side. Elbow Flexion: 0° 45° 90° 120° | Shear Elastic Modulus of the Ulnar Nerve (kPa) Operated Side. Elbow Flexion: 0° 45° 90° 120° |
|---|---|---|---|---|---|---|---|---|---|
| 1 | male | 78 | R | 2 | 26 3.9 | 12 | 1.2 | 38.2 30 41.3 82.3 | 116.2 86.5 66.6 38.9 |
| 2 | male | 41 | L | 2 | 35.2 6.9 | 7 | 1.0 | 27.9 38.8 96.8 146.0 | 150.1 137.0 91.1 58.5 |
| 3 | female | 25 | L | 2 | 23 14.4 | 9 | 1.1 | 29.9 92.9 123.2 140.7 | 260.7 178.6 80.6 60.9 |
| 4 | male | 43 | R | 1 | 40 6.8 | 18 | 1.0 | 37.1 86.1 105.5 145.7 | 165.7 143.3 87.9 52.8 |
| 5 | female | 53 | R | 2 | 37 8.1 | 3 | 0.49 | 54.6 56 70.2 157.4 | 72 56.1 29 49.6 |
| 6 | female | 68 | R | 2 | 11 5.2 | 2 | 1.23 | 38 65 88.1 140.7 | 178.5 126.4 55.7 26.9 |
| 7 | female | 53 | L | 2 | 40 9.8 | 16 | 0.65 | 47.8 139.1 144.7 156.3 | 202.6 146.1 110.7 67.5 |
| 8 | male | 40 | L | 3 | ---- | 3 | 2.13 | 39.9 35.2 95.4 111.6 | 115.8 62.1 72.5 53 |
| 9 | male | 56 | L | 3 | ---- | 3 | 1.2 | 35 79.6 122.4 173.5 | 160.7 70.7 70.2 62.4 |
| 10 | female | 69 | R | 1 | 40 5.1 | 3 | 1.33 | 20.6 36.5 57.5 108.5 | 129.7 100.7 50.5 16.6 |
| 11 | male | 49 | L | 1 | 32 6.5 | 12 | 2.04 | 39.4 92.8 115.2 196.3 | 174.5 151.5 102.8 34.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durand, S.; Raffoul, W.; Christen, T.; Pedrazzi, N. Post-Operative Assessment of Ulnar Nerve Tension Using Shear-Wave Elastography. Neurol. Int. 2021, 13, 469-476. https://doi.org/10.3390/neurolint13030046
Durand S, Raffoul W, Christen T, Pedrazzi N. Post-Operative Assessment of Ulnar Nerve Tension Using Shear-Wave Elastography. Neurology International. 2021; 13(3):469-476. https://doi.org/10.3390/neurolint13030046
Chicago/Turabian StyleDurand, Sebastien, Wassim Raffoul, Thierry Christen, and Nadine Pedrazzi. 2021. "Post-Operative Assessment of Ulnar Nerve Tension Using Shear-Wave Elastography" Neurology International 13, no. 3: 469-476. https://doi.org/10.3390/neurolint13030046
APA StyleDurand, S., Raffoul, W., Christen, T., & Pedrazzi, N. (2021). Post-Operative Assessment of Ulnar Nerve Tension Using Shear-Wave Elastography. Neurology International, 13(3), 469-476. https://doi.org/10.3390/neurolint13030046






