The Knowledge and Application of Economics in Healthcare in a High-Income Country Today: The Case of Belgium
Abstract
1. Introduction
2. Materials and Methods
2.1. Historical View
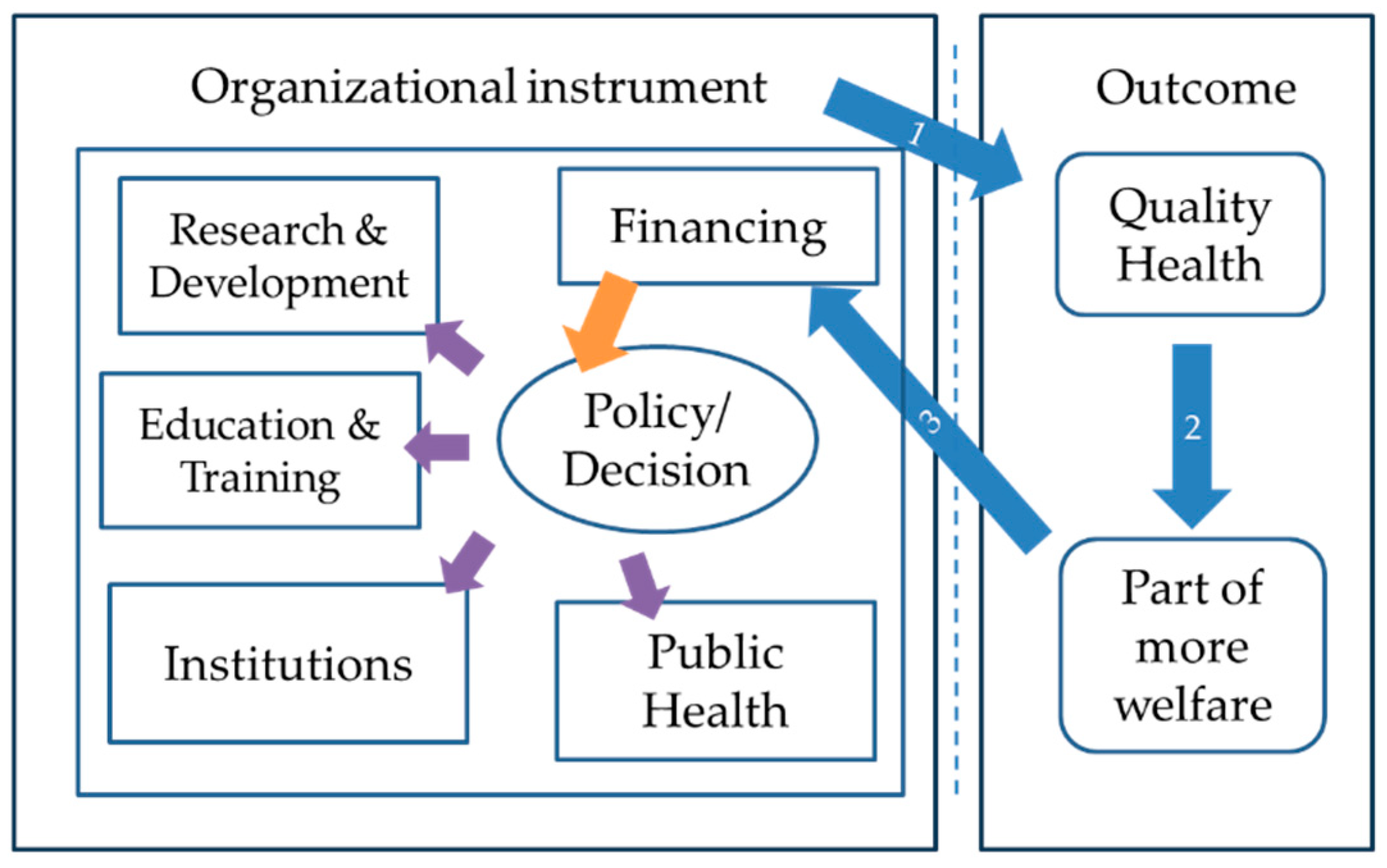
2.2. Healthcare Organization for Application of Health Economics
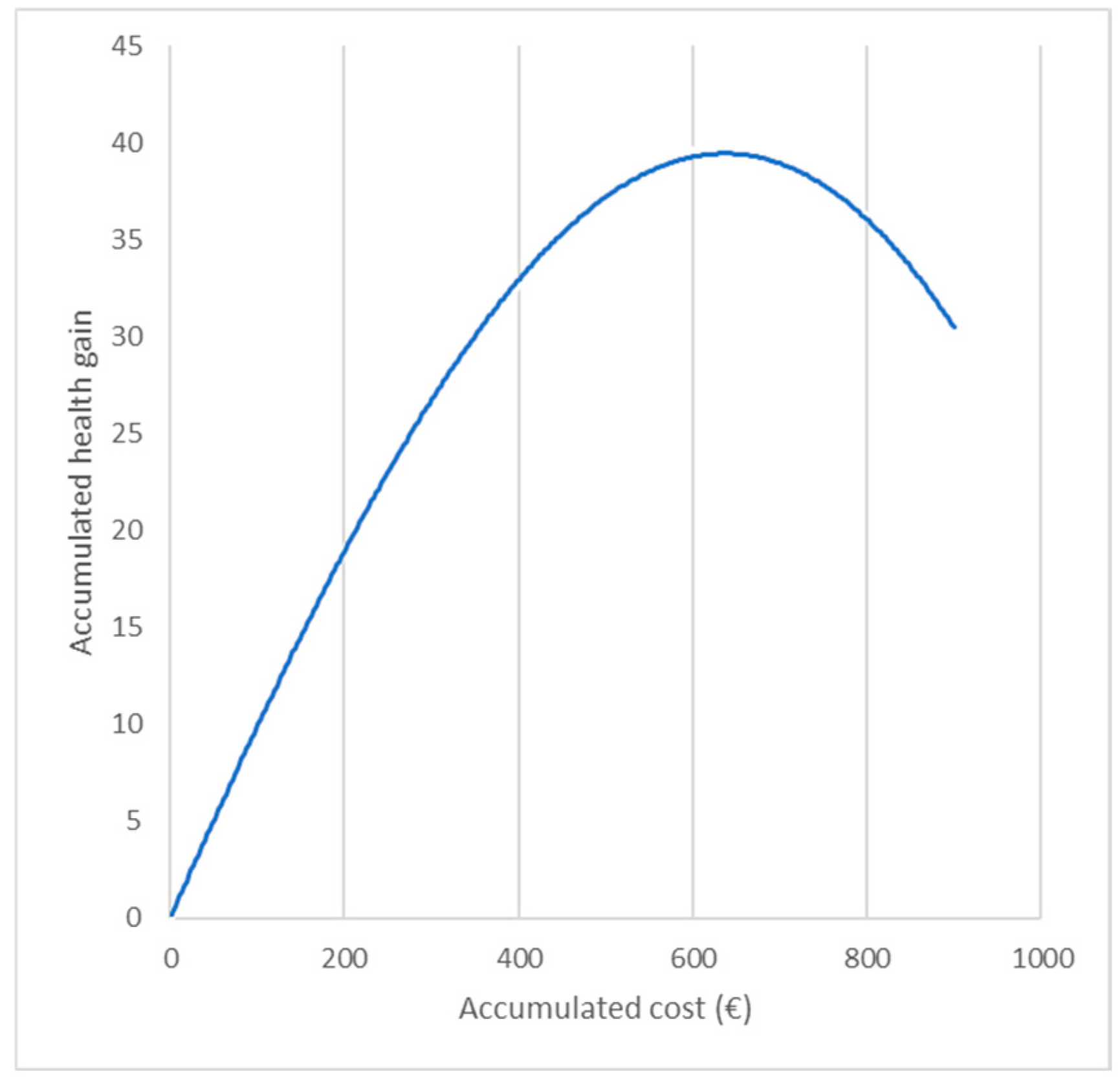
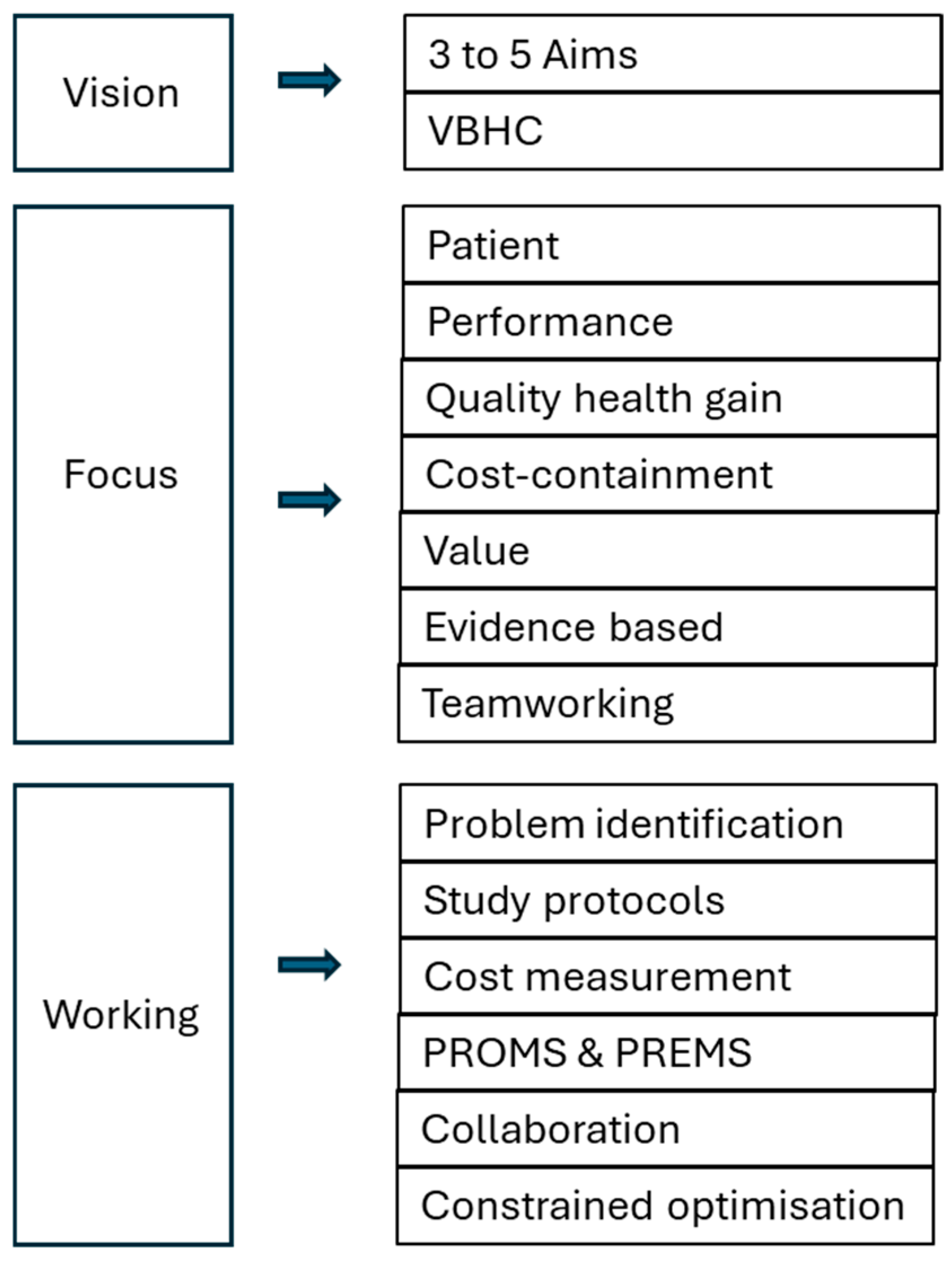
2.3. Where and How Does HE Intervene?
3. Results
3.1. Historical Overview
3.2. The Organization Levels
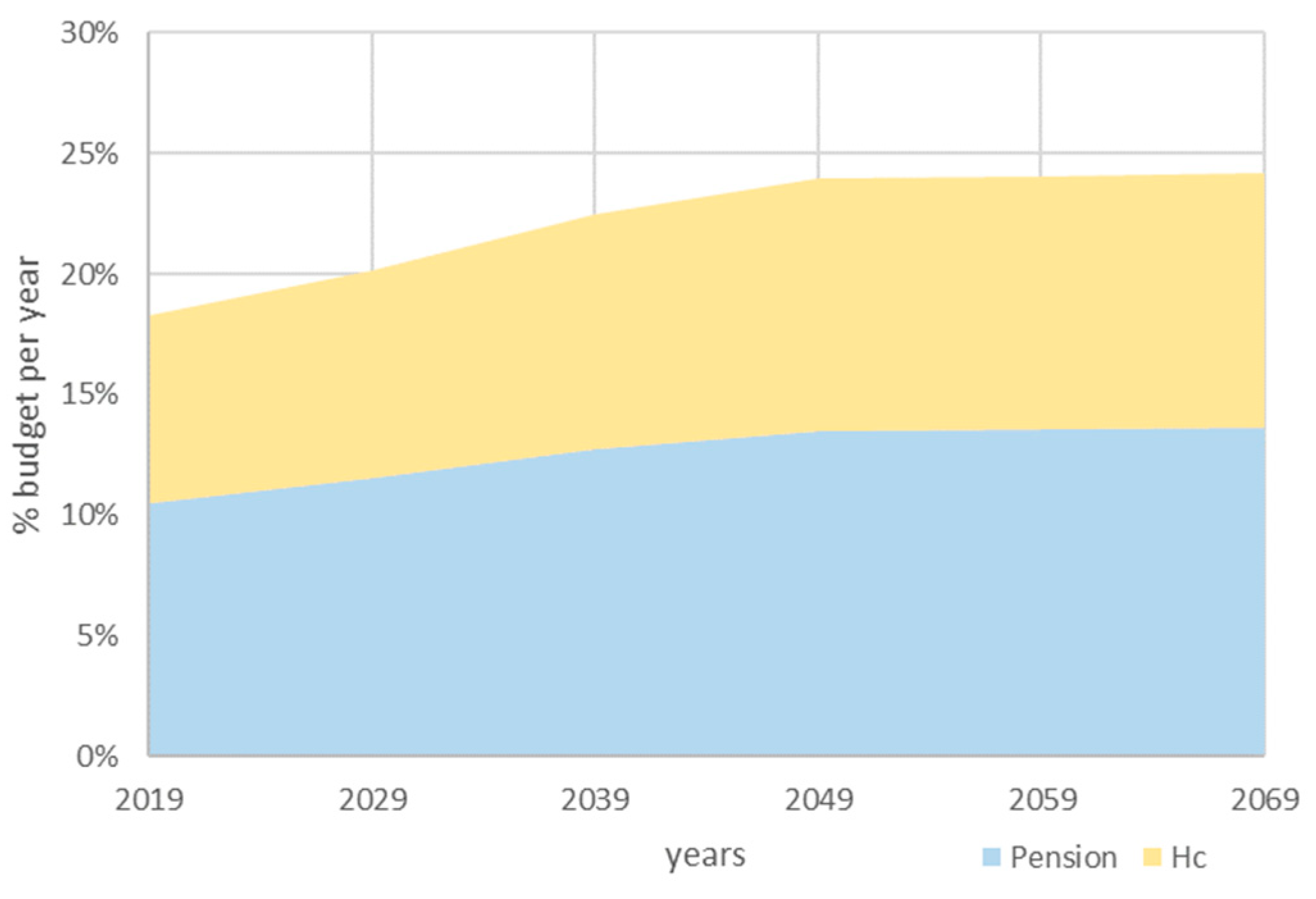
3.3. Challenges to the Sustainability of Healthcare
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
Mutualities and Other Third-Party Payers in Belgium
- Christian mutuality;
- Neutral mutuality health insurance fund;
- Socialist mutualities (Bond Moyson, De Voorzorg);
- Liberal mutuality health insurance fund;
- Independent health insurance funds (Onafhankelijk Ziekenfonds OZ, Securex, Partena, Helan).
Appendix C
- A preliminary care pathway for patients at risk of diabetes and follow-up of patients with diabetes;
- A childhood obesity care pathway;
- A multidisciplinary perinatal (prenatal and postnatal) care pathway for vulnerable women;
- A care pathway around the patient pre- and post-abdominal organ transplantation;
- Investing in psychiatric care with special focus on somatic care and young people with psychiatric problems;
- Reducing readmissions (new hospitalization periods) by rolling out better pulmonary rehabilitation and increasing the quality of life of the patients concerned by improving their functional capabilities;
- Various secondary and tertiary prevention first-line projects, including post-COVID-19 ones.
References
- Skidelsky, R. What’s Wrong with Economics; Yale University Press: New Haven, CT, USA, 2020. [Google Scholar]
- Dasgupta, P. Economics, a Very Short Introduction; Oxford University Press: Oxford, UK, 2007; Volume 156, p. 172. [Google Scholar]
- Barr, N. Economics of the Welfare State, 5th ed.; Oxford university Press: Oxford, UK, 2012; p. 385. [Google Scholar]
- Varian, H. Micro-Economic Analysis, 3rd ed.; W.W. Norton & Company: New York, NY, USA, 1992; p. 506. [Google Scholar]
- Mill, A. Economics 101; Adams Media: Avon, MA, USA, 2016. [Google Scholar]
- Chang, H.-J. Edible Economcs, a Hungry Economist Explains the World; Allen Lane, Penguin Books: London, UK, 2022; p. 192. [Google Scholar]
- Allen, R. Global Economic History, a Very Short Introduction; Oxfor University Press: Oxford, UK, 2011; Volume 282, p. 170. [Google Scholar]
- Pen, J.; van Gemerden, L. Macro-Economie, Wat We Weten en Wat Wij Niet Weten; Aula, Het Spectrum: Utrecht, The Netherlands; Antwerpen, Belgium, 1980. [Google Scholar]
- Folland, S.G.A.; STano, M. The Economics of Health and Health Care, 8th ed.; Alexander, D., Ed.; Pearson: Upper Saddle River, NJ, USA, 2017. [Google Scholar]
- Arrow, K. Uncertainty and welfare economics of medical care. Am. Econ. Rev. 1963, 53, 941–973. [Google Scholar]
- Muurinen, J.M. Demand for health: A generalised Grossman model. J. Health Econ. 1982, 1, 5–28. [Google Scholar] [CrossRef]
- Schut, E.; Varkevisser, M. Economie van de Gezondheidszorg; Bohn Stafleu van Loghum: Houten, The Netherlands, 2016; p. 438. [Google Scholar]
- Standaert, B.; Sauboin, C.; DeAntonio, R.; Marijam, A.; Gomez, J.; Varghese, L.; Zhang, S. How to assess for the full economic value of vaccines? From past to present, drawing lessons for the future. J. Mark. Access. Health Policy 2020, 8, 1719588. [Google Scholar] [CrossRef] [PubMed]
- Maes, J. Uw Sociale Zekerheid in Gevaar; Drukkerij EPO: Berchem, Belgium, 2010. [Google Scholar]
- Deleeck, H. De Architectuur van de Welvaartsstaat Opnieuw Bekeken; ACCO: Leuven, Belgium, 2009. [Google Scholar]
- Culyer, A.J.; Newhouse, J.P. (Eds.) Introduction: The state and scope of health economics. In Handbook of Health Economics; Elsevier Science: Amsterdam, The Netherlands, 2000; p. 890. [Google Scholar]
- Kotsopoulos, N.; Connolly, M.P. Is the gap between micro- and macroeconomic assessments in health care well understood? The case of vaccination and potential remedies. J. Mark. Access. Health Policy 2014, 2, 23897. [Google Scholar] [CrossRef] [PubMed]
- Tulchinsky, T.; Varavikova, E. Health financing: The macroeconomic level. In The New Public Health; Elsevier Inc: Amsterdam, The Netherlands, 2014; pp. 592–607. [Google Scholar]
- Papanicolas, I.; Rajan, D.; Karanikolos, M.; Soucat, A.; Figueras, J. Health System Performance Assessment: A Framework for Policy Analysis; Health Policy Series 57; World Health Organisation: Geneva, Switzerland, 2022. [Google Scholar]
- De Maeseneer, J.; Galle, A. Belgium’s Healthcare System: The Way Forward to Address the Challenges of the 21st Century Comment on “Integration or Fragmentation of Health Care? Examining Policies and Politics in a Belgian Case Study”. Int. J. Health Policy Manag. 2023, 12, 7070. [Google Scholar] [CrossRef]
- Schokkaert, E.; van de Voorde, C. Het Belgisch Systeem van Gezondheidszorg. Meer Bevoegdheden Voor de Gemeenschappen/Gewesten? Of Voor de Ziekenfondsen? Re-Bel Initiative: Brussels, Belgium, 2011. [Google Scholar]
- Bleichrodt, H.; Koopmanschap, M. Economische evaluatie. In Economie van de Gezondheidszorg; Schut, E., Varkevisser, M., Eds.; Bohn Stafleu van Loghum: Houten, The Netherlands, 2016; pp. 324–355. [Google Scholar]
- Baumol, W. The Cost of Disease; Yale University Press: New Haven, CT, USA, 2012; p. 250. [Google Scholar]
- Drummond, M.S.M.; Claxton, K.; Stoddart, G.; Torrance, G. Methods for the Economic Evaluation of Health Care Programmes, 4th ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Annemans, L. Gezondheidseconomie voor Niet-Economen; Academia Press: Gent, Belgium, 2007; p. 102. [Google Scholar]
- Cleemput, I.; Neyt, M.; Van de Sande, S.; Thiry, N. Belgian guidelines for economic evaluations and budget impact analyses: Second edition. In Health Technology Assessment (HTA); Health Care Knowledge Centre (KCE): Brussels, Belgium, 2012. [Google Scholar]
- Standaert, B.; Rappuoli, R. 3. How comprehensive can we be in the economic assessment of vaccines? J. Mark. Access. Health Policy 2017, 5, 1336044. [Google Scholar] [CrossRef] [PubMed]
- MCPake, B.; Normand, C. Health Economics, an International Perspective; Routledge Taylor & Francis Group: London, UK; New York, NY, USA, 2008; p. 285. [Google Scholar]
- Palmer, G.; Ho, M. Health Economics, a Critical & Global Analysis; Palgrave MacMillan: Hampshire, UK, 2008; p. 303. [Google Scholar]
- Sloan, F.; Hsieh, C. Health Economics, 2nd ed.; The MIT Press: Cambridge, MA, USA, 2016; p. 775. [Google Scholar]
- Phelps, C. Health Economics, 6th ed.; Routledge Taylor & Francis Group: New York, NY, USA; London, UK, 2018; p. 481. [Google Scholar]
- Neumann, P.; Sanders, G.; Russell, L.; Siegel, J.; Ganiats, T. Cost-Effectiveness in Health and Medicine; Oxford University Press: New York, NY, USA, 2017; p. 470. [Google Scholar]
- Bhattacharya, J.; Hyde, T.; Tu, P. Health Economics; Bloomsbury Academic: London, UK; New York, NY, USA; Dublin, Ireland, 2022; p. 525. [Google Scholar]
- Griffin, S. The History of Medicine and Organized Healthcare in America. 2020. Available online: https://www.griffinbenefits.com/blog/history-of-healthcare (accessed on 17 February 2024).
- Schokkaert, E. De Gezondheidszorg in Evolutie: Uitdagingen en Keuzes; Koninklijke Vlaamse Academie van België voor Wetenschappen en Kunsten: Brussels, Belgium, 2016. [Google Scholar]
- Bynum, W. The History of Medicine, a Very Whort Introduction; Oxford University Press: Oxford, UK, 2008; Volume 191, p. 169. [Google Scholar]
- Berridge, V. Public Health, a Very Short Introduction; Oxford University Press: Oxford, UK, 2016; Volume 482, p. 138. [Google Scholar]
- Annemans, L.; Crott, R. Economische en sociale aspecten van de Belgische Gezondheidszorg; Belgisch Instituut voor Gezondheidseconomie (BIGE): Brussels, Belgium, 1998; p. 275. [Google Scholar]
- Torfs, K.; Bussels, J.; Kurz, X.; Annemans, L. Inleiding tot de Economische Evaluatie van Gezondheidszorgen; Astra Pharmaceuticals: Brussels, Belgium, 1993; p. 118. [Google Scholar]
- Planbureau, F. Economische Begroting 2024-Economische Vooruitzichten 2025–2029 van Februari 2024; Instituut voor Nationale Rekeningen: Brussels, Belgium, 2024. [Google Scholar]
- Gerkens, S.; Merkur, S. Belgium: Health System Review. Health Syst. Transit. 2020, 22, 1–237. [Google Scholar]
- Samyn, P. Alles Wat je Altijd al Wilde Weten over de Sociale Zekerheid; Federale Overheidsdienst: Brussels, Belgium, 2024. [Google Scholar]
- Riziv, I. Nomenclatuur van de Geneeskundige Verstrekkingen. 2023. Available online: https://www.riziv.fgov.be/nl/nomenclatuur (accessed on 17 February 2024).
- Cremer, H.; Pestieau, P. Social insurance competition between Bismarck and Beveridge. J. Urban Econ. 2003, 54, 181–196. [Google Scholar] [CrossRef]
- Cutler, D. Equality, efficiency, and market fundamentals. The dynamics of international medical-care reform. J. Econ. Lit. 2002, 60, 881–906. [Google Scholar] [CrossRef]
- Schokkaert, E.; Guillaume, J.; van de Voorde, C. Risk adjustment in Belgium: Why and how to introduce socioeconomic variables in health plan payment. In Risk Adjustment, Risk Sharing and Premium Regulation in Health Insurance Markets; McGuire, T., Ed.; Elsevier, Academic Press: Amsterdam, The Netherlands, 2018; pp. 209–234. [Google Scholar]
- Belgium.be. Beschrijving van het Belgische Gezondheidssyteem, naar een Gezond België. Available online: https://www.gezondbelgie.be/nl/hit (accessed on 20 February 2024).
- Bank, B. Analyse MAHA de 2022 avec un premier aperçu pour 2023. In Rapports MAHA; Belfius: Brussels, Belgium, 2023. [Google Scholar]
- Hollingsworth, B.; Parkin, D. Efficiency and productivity change in the English National Health Service: Can data envelopment analysis provide a robust and useful measure? J. Health Serv. Res. Policy 2003, 8, 230–236. [Google Scholar] [CrossRef]
- Plasschaert, B. Efficiency in Flemish Hospitals: A DEA Approach. Master’s Thesis, Faculty of Economy & Business Administration, University of Ghent, Ghent, Belgium, 2018. [Google Scholar]
- Dohmen, P.; van Ineveld, M.; Markus, A.; van der Hagen, L.; van de Klundert, J. Does competition improve hospital performance: A DEA based evaluation from the Netherlands. Eur. J. Health Econ. 2023, 24, 999–1017. [Google Scholar] [CrossRef] [PubMed]
- OECD/European Observatory on Health Systems and Policies. België, Landenprofiel Gezondheid 2017; OECD: Paris, France, 2017. [Google Scholar]
- OECD. Health at a Glance 2021; OECD: Paris, France, 2021. [Google Scholar]
- Ramaekers, D. Key Data in Healthcare General Hospitals; Federal Public Service Health, Food Chain Safety and ENvironment: Brussels, Belgium, 2024; p. 40. [Google Scholar]
- Collin, B. MORSE Report; RIZIV-INAMI: Brussels, Belgium, 2023. [Google Scholar]
- Justaert, M.; Kirsch, A. Meerjarig Begrotingstraject voor de Verzekering voor Geneeskundige Verzorging 2022–2024; RIZIV: Brussels, Belgium, 2022. [Google Scholar]
- Kanavos, P.; Vogelsang, M.; Haig, M.; Kolovou, V. Challenges for health systems seeking to embrace virtual health care for population health. Eur. J. Health Econ. 2022, 23, 1079–1083. [Google Scholar] [CrossRef] [PubMed]
- Varkevisser, M.; Schut, E. Marktordening in de gezondheidszorg. In Economie van de Gezondheidszorg; Schut, E., Varkevisser, M., Eds.; Bohn Stafleu van Loghum: Houten, The Netherlands, 2016; pp. 358–398. [Google Scholar]
- Garrison, L.P., Jr.; Kamal-Bahl, S.; Towse, A. Toward a Broader Concept of Value: Identifying and Defining Elements for an Expanded Cost-Effectiveness Analysis. Value Health 2017, 20, 213–216. [Google Scholar] [CrossRef] [PubMed]
- KCE; IMA; CES-KUL; FPB. Evolutie van de Uitgaven voor Gezondheidszorg; Federaal Kenniscentrum voor Gezondheidszorg: Brussels, Belgium, 2005. [Google Scholar]
- Jeurissen, P.; Maarse, H.; Tanke, M. Betaalbare Zorg; Sdu: Den Haag, The Netherlands, 2018; p. 445. [Google Scholar]
- Van Gompel, J.D.P. Jaarlijks Verslag, Studiecommissie voor de Vergrijzing; Federaal Planbureau: Brussel, Belgium, 2021. [Google Scholar]
- Schut, E.; Varkevisser, M. (Eds.) Productie van gezondheidszorg. In Economie van de Gezondheidszorg; Bohn Stafleu van Loghum: Houten, The Netherlands, 2016; pp. 235–271. [Google Scholar]
- Raworth, K. Doughnut Economics; Penguin Random House: London, UK, 2017; p. 356. [Google Scholar]
- Federaal Kenniscentrum voor de Gezondheidszorg (KCE). 2003. Available online: https://socialsecurity.belgium.be/nl/netwerk/federaal-kenniscentrum-voor-de-gezondheidszorg-kce (accessed on 20 February 2024).
- Martin, L.; Nelson, E.; Rakover, J.; Chose, A. Whole System Measures 2.0: A Compass for Health System Leaders; Institute for healthcare Improevement: Cambridge, MA, USA, 2016. [Google Scholar]
- Porter, M.E.; Olmsted Teisberg, E. Redefining Health Care, Creating Value-Based Competition on Results; Harvard Business School Press Boston, Massachusetts: Boston, MA, USA, 2006. [Google Scholar]
- Moriates, C.; Arora, V.; Shah, N. Understanding Value-Based Healthcare; McGraw-Hill Education: New York, NY, USA, 2015; p. 402. [Google Scholar]
- Nundy, S.; Cooper, L.A.; Mate, K.S. The Quintuple Aim for Health Care Improvement: A New Imperative to Advance Health Equity. JAMA 2022, 327, 521–522. [Google Scholar] [CrossRef]
- Katz, G. Implementing Value-Based Health Care in Europe, Handbook for Pioneers; EIT Health: Munich, Germany, 2020. [Google Scholar]
- Porter, M.E. What is value in health care? N. Engl. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef]
- Sermeus, W.; Vleugels, A. Patiëntgestuurde Organisatie; Kluwer: Alphen aan den Rijn, The Netherlands, 2010. [Google Scholar]
- Klop, G.; Rutte, A. Value-Based Healthcare: Het Antwoord op Onze Toekositge Zorguitdagingen de Zin en Onzin van VBHC Vandaag Met Aanbevelingen voor Morgen; Vintura: Utrecht, The Netherlands, 2021. [Google Scholar]
- Sermeus, W. Management en Beleid in de Gezondheidszorg; Learn, A., Ed.; Acco CV: Leuven, Belgium, 2022. [Google Scholar]
- Blank, R.H.; Burau, V.; Kuhlmann, E. Comparative Health Policy, 5th ed.; Palgrave: London, UK, 2018; p. 370. [Google Scholar]
- Vandenberghe, D. Simulating lifestyle and medical interventions to prevent type-2 diabetes: An economic evaluation for Belgium. Eur. J. Health Econ. 2022, 23, 237–248. [Google Scholar] [CrossRef]
- Standaert, B.; Parez, N.; Tehard, B.; Colin, X.; Detournay, B. Cost-effectiveness analysis of vaccination against rotavirus with RIX4414 in France. Appl. Health Econ. Health Policy 2008, 6, 199–216. [Google Scholar] [CrossRef]
- Darlington, M.; Scarica, R.; Chavez-Pacheco, X.; Segar, L.B.; Durand-Zaleski, I. Decrementally cost-effective health technologies in non-inferiority studies: A systematic review. Front. Pharmacol. 2022, 13, 1025326. [Google Scholar] [CrossRef]
- Sacristan, J.A. How to Assess the Value of Low-Value Care. BMC Health Serv. Res. 2020, 20, 1000. [Google Scholar] [CrossRef]
- Cookson, R.; Griffin, S.; Norheim, O.F.; Culyer, A.J.; Chalkidou, K. Distributional Cost-Effectiveness Analysis Comes of Age. Value Health 2021, 24, 118–120. [Google Scholar] [CrossRef]
- Asaria, M.; Griffin, S.; Cookson, R. Distributional Cost-Effectiveness Analysis: A Tutorial. Med. Decis. Mak. 2016, 36, 8–19. [Google Scholar] [CrossRef]
- Verguet, S.; Kim, J.J.; Jamison, D.T. Extended Cost-Effectiveness Analysis for Health Policy Assessment: A Tutorial. Pharmacoeconomics 2016, 34, 913–923. [Google Scholar] [CrossRef]
- Verguet, S.; Olson, Z.D.; Babigumira, J.B.; Desalegn, D.; Johansson, K.A.; Kruk, M.E.; Levin, C.E.; Nugent, R.A.; Pecenka, C.; Shrime, M.G.; et al. Health gains and financial risk protection afforded by public financing of selected interventions in Ethiopia: An extended cost-effectiveness analysis. Lancet Glob. Health 2015, 3, e288–e296. [Google Scholar] [CrossRef]
- Frazao, T.D.C.; Camilo, D.G.G.; Cabral, E.L.S.; Souza, R.P. Multicriteria decision analysis (MCDA) in health care: A systematic review of the main characteristics and methodological steps. BMC Med. Inform. Decis. Mak. 2018, 18, 90. [Google Scholar] [CrossRef]
- Lahdelma, R.; Salminen, P. Stochastic Multicriteria Acceptability Analysis (SMAA). In Trends in Multiple Criteria Decision Analysis. International Series in Operations Research & Management Science; Ehrgott, M., Figueira, J., Greco, S., Eds.; Springer: Boston, MA, USA, 2010. [Google Scholar]
- Lagravinese, R.; Liberati, P.; Resce, G. Exploring health outcomes by stochastic multicriteira acceptability analysis: Anapplication to Italion regions. Eur. J. Oper. Res. 2019, 274, 1168–1179. [Google Scholar] [CrossRef]
- Mauskopf, J.A.; Paul, J.E.; Grant, D.M.; Stergachis, A. The Role of Cost—Consequence Analysis in Healthcare Decision—Making. PharmacoEconomics 1998, 13, 277–288. [Google Scholar] [CrossRef]
- Jeong, S.; Ohr, S.O.; Cleasby, P.; Barrett, T.; Davey, R.; Deeming, S. A cost-consequence analysis of normalised advance care planning practices among people with chronic diseases in hospital and community settings. BMC Health Serv. Res. 2021, 21, 729. [Google Scholar] [CrossRef]
- Hanquet, G.; Valenciano, M.; Simondon, F.; Moren, A. Vaccine effects and impact of vaccination programmes in post-licensure studies. Vaccine 2013, 31, 5634–5642. [Google Scholar] [CrossRef]
- Standaert, B. The economic value of rotavirus vaccination when optimally implemented in a high-income country. Vaccines 2023, 11, 917. [Google Scholar] [CrossRef]
- Moradpour, J.; Zhang, W.; Grootendorst, P.; Anis, A.H.; Hollis, A. Modeling Tiered Pricing Frameworks: A Simulation Approach. Value Health 2023, 26, 351–358. [Google Scholar] [CrossRef]
- Mauskopf, J.; Earnshaw, S.R.; Brogan, A.; Wolowacz, S.; Brodtkorb, T.-H. Budget-Impact Analysis of Health Care Interventions, a Practical Guide; Adis: Cham, Switzerland, 2017; 224p. [Google Scholar]
- Ghabri, S.; Mauskopf, J. The use of budget impact analysis in the economic evaluation of new medicines in Australia, England, France and the United States: Relationship to cost-effectiveness analysis and methodological challenges. Eur. J. Health Econ. 2018, 19, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.H.; O’Brien, B.J. The death of cost-minimization analysis? Health Econ. 2001, 10, 179–184. [Google Scholar] [CrossRef]
- Duenas, A. Cost-Minimization Analysis. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; p. 516. [Google Scholar]
- Brent, R.J. Cost-Benefit Analysis versus Cost-Effectiveness Analysis from a Societal Perspective in Healthcare. Int. J. Environ. Res. Public Health 2023, 20, 4637. [Google Scholar] [CrossRef]
- Johannesson, M.; Jonsson, B. Economic evaluation in health care: Is there a role for cost-benefit analysis? Health Policy 1991, 17, 1–23. [Google Scholar] [CrossRef]
- Crown, W.; Buyukkaramikli, N.; Thokala, P.; Morton, A.; Sir, M.Y.; Marshall, D.A.; Tosh, J.; Padula, W.V.; Ijzerman, M.J.; Wong, P.K.; et al. Constrained Optimization Methods in Health Services Research-An Introduction: Report 1 of the ISPOR Optimization Methods Emerging Good Practices Task Force. Value Health 2017, 20, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Demarteau, N.; Breuer, T.; Standaert, B. Selecting a mix of prevention strategies against cervical cancer for maximum efficiency with an optimization program. Pharmacoeconomics 2012, 30, 337–353. [Google Scholar] [CrossRef]
- Kapoor, R.; Standaert, B.; Pezalla, E.J.; Demarteau, N.; Sutton, K.; Tichy, E.; Bungey, G.; Arnetorp, S.; Bergenheim, K.; Darroch-Thompson, D.; et al. Identification of an Optimal COVID-19 Booster Allocation Strategy to Minimize Hospital Bed-Days with a Fixed Healthcare Budget. Vaccines 2023, 11, 377. [Google Scholar] [CrossRef] [PubMed]
- Varghese, L.; Puteh, S.E.W.; Schecroun, N.; Jahis, R.; Van Vlaenderen, I.; Standaert, B.A. Applying a Constrained Optimization Portfolio Model to Aid Prioritization of Public Health Interventions in Malaysia. Value Health Reg. Issues 2020, 21, 172–180. [Google Scholar] [CrossRef]
- Standaert, B.; Schecroun, N.; Ethgen, O.; Topachevskyi, O.; Morioka, Y.; Van Vlaenderen, I. Optimising the introduction of multiple childhood vaccines in Japan: A model proposing the introduction sequence achieving the highest health gains. Health Policy 2017, 121, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Dort, T.; Schecroun, N.; Standaert, B. Improving the Hospital Quality of Care during Winter Periods by Optimizing Budget Allocation Between Rotavirus Vaccination and Bed Expansion. Appl. Health Econ. Health Policy 2018, 16, 123–132. [Google Scholar] [CrossRef]
- Reyes-Santias, F.; Cordova-Arevalo, O.; Rivo-Lopez, E. Using flexible regression models for calculating hospital’s production functions. BMC Health Serv. Res. 2020, 20, 641. [Google Scholar] [CrossRef]
- Thusini, S.; Milenova, M.; Nahabedian, N.; Grey, B.; Soukup, T.; Chua, K.-C.; Henderson, C. Correction: The development of the concept of return-on-investment from large-scale quality improvement programmes in healthcare: An integrative systematic literature review. BMC Health Serv. Res. 2022, 22, 1567. [Google Scholar] [CrossRef] [PubMed]
- Thusini, S.; Milenova, M.; Nahabedian, N.; Grey, B.; Soukup, T.; Chua, K.-C.; Henderson, C. The development of the concept of return-on-investment from large-scale quality improvement programmes in healthcare: An integrative systematic literature review. BMC Health Serv. Res. 2022, 22, 1492. [Google Scholar]
- Hollingsworth, B.; Peacock, S. Efficiency Measurement in Health and Health Care, 1st ed.; Routledge International Studies in Health Economics; Routledge: London, Uk, 2008; 172p. [Google Scholar]
- van der Schans, S.; Schöttler, M.H.; van der Schans, J.; Connolly, M.P.; Postma, M.J.; Boersma, C. Investing in the Prevention of Communicable Disease Outbreaks: Fiscal Health Modelling-The Tool of Choice for Assessing Public Finance Sustainability. Vaccines 2023, 11, 823. [Google Scholar] [CrossRef]
- Connolly, M.P.; Kotsopoulos, N.; Postma, M.J.; Bhatt, A. The Fiscal Consequences Attributed to Changes in Morbidity and Mortality Linked to Investments in Health Care: A Government Perspective Analytic Framework. Value Health 2017, 20, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Kotsopoulos, N.; Haitsma, G.; Connolly, M.P.; Standaert, B. Estimating the money flow in the economy attributed to rotavirus disease and vaccination in the Netherlands using a Social Accounting Matrix (SAM) framework. Expert Rev. Pharmacoecon. Outcomes Res. 2019, 20, 603–612. [Google Scholar] [CrossRef] [PubMed]
- Standaert, B.; Sauboin, C.; Leclerc, Q.J.; Connolly, M.P. Comparing the Analysis and Results of a Modified Social Accounting Matrix Framework with Conventional Methods of Reporting Indirect Non-Medical Costs. Pharmacoeconomics 2021, 39, 257–269. [Google Scholar] [CrossRef]
- Kraay, A.; McKenzie, D. Do poverty traps exist? Assessing the evidence. J. Econ. Perspect. 2014, 28, 127–148. [Google Scholar] [CrossRef]
- Matsuyama, K. Poverty traps. In Economic Growth; Durlauf, S.N., Blume, L.E., Eds.; Palgrave Macmillan UK: London, UK, 2010; pp. 215–221. [Google Scholar]
- Saccone, D.; Migheli, M. Free to escape? Economic freedoms, growth and poverty traps. Rev. Dev. Econ. 2022, 26, 1518–1554. [Google Scholar] [CrossRef]
- Terlinden, A.; Aissaoui, A.; Ethgen, O. Insurance-based risk-sharing agreements. J. Pharm. Policy Pract. 2015, 8, P22. [Google Scholar] [CrossRef]
- Kim, A.E.; Choi, D.H.; Chang, J.; Kim, S.H. Performance-Based Risk-Sharing Arrangements (PBRSA): Is it a Solution to Increase Bang for the Buck for Pharmaceutical Reimbursement Strategy for Our Nation and Around the World? Clin. Drug Investig. 2020, 40, 1107–1113. [Google Scholar] [CrossRef]
- Garrison, L.P., Jr.; Towse, A.; Briggs, A.; de Pouvourville, G.; Grueger, J.; Mohr, P.E.; Severens, J.H.; Siviero, P.; Sleeper, M. Performance-based risk-sharing arrangements-good practices for design, implementation, and evaluation: Report of the ISPOR good practices for performance-based risk-sharing arrangements task force. Value Health 2013, 16, 703–719. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, F.R.; Santos, S.; Silva, C.; Sousa, G. Risk-sharing agreements, present and future. Ecancermedicalscience 2018, 12, 823. [Google Scholar] [CrossRef] [PubMed]
- Rutten, M.; Reed, G. A comparative analysis of some policy options to reduce rationing in the UK’s NHS: Lessons from a general equilibrium model incorporating positive health effects. J. Health Econ. 2009, 28, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Breeze, P.R.; Squires, H.; Ennis, K.; Meier, P.; Hayes, K.; Lomax, N.; Shiell, A.; Kee, F.; de Vocht, F.; O’flaherty, M.; et al. Guidance on the use of complex systems models for economic evaluations of public health interventions. Health Econ. 2023, 32, 1603–1625. [Google Scholar] [CrossRef] [PubMed]
- Hafner, M.; Yerushalmi, E.; Andersson, F.L.; Burtea, T. Partially different? The importance of general equilibrium in health economic evaluations: An application to nocturia. Health Econ. 2023, 32, 654–674. [Google Scholar] [CrossRef]
- Sielska, A.; Nojszewska, E. Production function for modeling hospital activities. The case of Polish county hospitals. PLoS ONE 2022, 17, e0268350. [Google Scholar] [CrossRef]
| Market | Planned | |
|---|---|---|
| Value | Budget | Finance |
| Incremental CEA | BIA | FHM cohort |
| Decremental CEA | Cost minimisation | FHM-SAM |
| Distributional CEA | CBA | Poverty trap avoidance |
| Extended CEA | CO | RSA |
| MCDA/SMAA | Portfolio management | Macro-economics |
| Cost–consequence analysis | Cobb–Douglas function | Production functions |
| Cost–impact analysis | ROI and SROI | |
| Tiered and volume pricing | DEA | |
| Overall | Planned-Driven | Market-Driven | |
|---|---|---|---|
| What? | Finance | Budget | Value |
| Definition | Reimbursable and registered medical activities | Action plan, time schedule, goals, budget scheme | Value-based pricing |
| How much? | 70% | 10% | 20% |
| Methods? | Fiscal health modelling Macro-economics | Budget impact + constrained optimization Cobb–Douglas function DEA | Cost-effectiveness analysis Cost–impact analysis |
| Influencer? | Hospital network | Europe—OECD | PPF to PPP |
| Logic? | Constrained budget | More for more | |
| Who? | NSSO insurance payers | Producers | |
| Level | Application | Activity | Type of Economic Approach | Method |
|---|---|---|---|---|
| Macro or Strategic | Financial | Defining the annual growth rate; nomenclatura; BFM | Financial economy | FHM; macro-economy; production function |
| Contribution | OOP + social | Financial + market economy | FHM; SAM | |
| Budgeting | Plan, scheme, target (quantified) | Budget economy | CO; portfolio; Cobb–Douglas; DEA | |
| Meso or Offer/Supply | Network Regions | Hospitalisations; health subregions; population health | Budget economy | Cost–consequence; DEA; CO |
| Offer Limitations | Grants/regional taxations | Financial economy | Modeling + simulations | |
| Mutualities/Insurance | Regulated competition | Market economy | FHM | |
| Micro or Tactical | Demand/Offer | Elasticities | Market economy | Budget/outcome; CO |
| HTA | Pricing | Market economy | CEA-BIA; CBA; RSA; CIA; FHM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Market Access Society. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Standaert, B.; Vandenberghe, D.; Connolly, M.P.; Hellings, J. The Knowledge and Application of Economics in Healthcare in a High-Income Country Today: The Case of Belgium. J. Mark. Access Health Policy 2024, 12, 264-279. https://doi.org/10.3390/jmahp12030021
Standaert B, Vandenberghe D, Connolly MP, Hellings J. The Knowledge and Application of Economics in Healthcare in a High-Income Country Today: The Case of Belgium. Journal of Market Access & Health Policy. 2024; 12(3):264-279. https://doi.org/10.3390/jmahp12030021
Chicago/Turabian StyleStandaert, Baudouin, Désirée Vandenberghe, Mark P. Connolly, and Johan Hellings. 2024. "The Knowledge and Application of Economics in Healthcare in a High-Income Country Today: The Case of Belgium" Journal of Market Access & Health Policy 12, no. 3: 264-279. https://doi.org/10.3390/jmahp12030021
APA StyleStandaert, B., Vandenberghe, D., Connolly, M. P., & Hellings, J. (2024). The Knowledge and Application of Economics in Healthcare in a High-Income Country Today: The Case of Belgium. Journal of Market Access & Health Policy, 12(3), 264-279. https://doi.org/10.3390/jmahp12030021






