Metronidazole Suspension for Paediatric Use in Developing Countries: Formulation, Quality, and Stability
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Excipients
2.2. Suspension Preparation
2.3. Suspension Quantitative Analysis
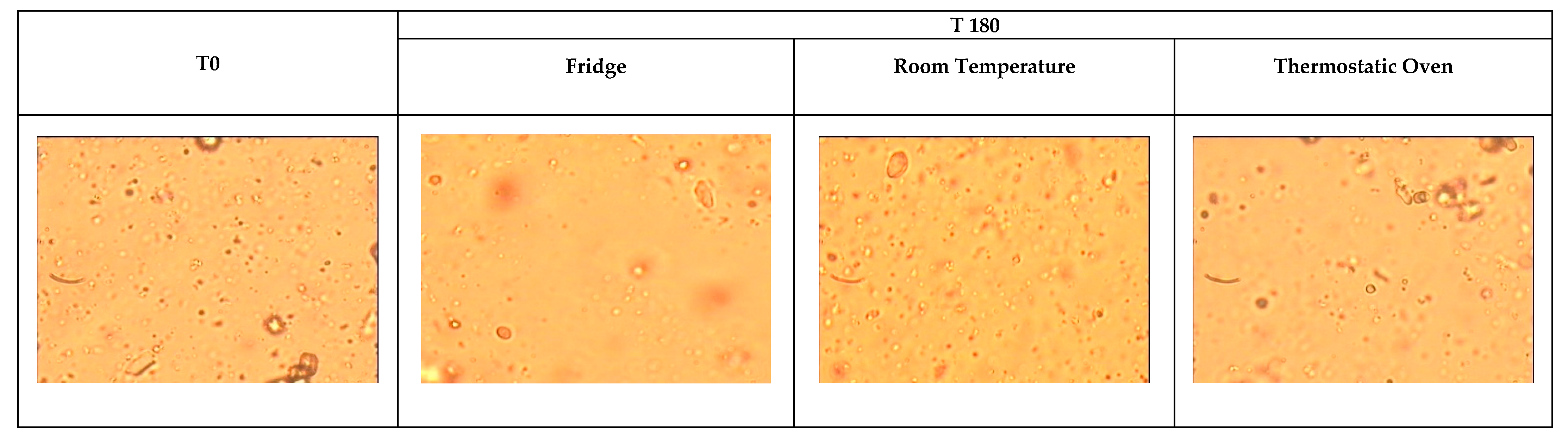
2.4. Evaluation of Suspension Stability
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| A.P.P.A.® | Aid Progress Pharmacist Agreement |
| ADI | Acceptable Daily Intake |
| DCs | Developing Countries |
| EFSA | European Food Safety Authority |
| FDA | Food and Drug Administration |
| GRAS | Generally Recognised As Safe |
| HPLC | High-Performance Liquid Chromatography |
| SD | Standard Deviation |
| T0 | Initial conditions |
| T180 | 180 days of storage |
| UV | Ultraviolet |
| WHO | World Health Organisation |
References
- Lopalco, A.; Denora, N. Paediatric Formulation: Design and Development. Int. J. Mol. Sci. 2020, 21, 7118. [Google Scholar] [CrossRef]
- US Government Accountability Office. Pediatric Drug Research: Studies Conducted Under Best Pharmaceuticals for Children Act: Report to Congressional Committees. 2007. Available online: https://www.gao.gov/assets/gao-07-557.pdf (accessed on 1 April 2025).
- Milne, C.P.; Bruss, J.B. The economics of pediatric formulation development for off-patent drugs. Clin. Ther. 2008, 30, 2133–2145. [Google Scholar] [CrossRef]
- Fadda, H.M.; Weiler, H.; Carvalho, M.; Lee, Y.Z.; Dassouki, H.; AbuBlan, R.; Iurian, S.; Hamid, A.; Şeremet, G.; Li, Z.; et al. Pediatric oral extemporaneous preparations and practices: International Pharmaceutical Federation (FIP) global study. Eur. J. Pharm. Biopharm. 2024, 204, 114483. [Google Scholar] [CrossRef]
- Yuliani, S.H.; Putri, D.C.A.; Virginia, D.M.; Gani, M.R.; Riswanto, F.D.O. Prevalence, Risk, and Challenges of Extemporaneous Preparation for Pediatric Patients in Developing Nations: A Review. Pharmaceutics 2023, 15, 840. [Google Scholar] [CrossRef] [PubMed]
- Commission to the European Parliament and Council. State of Paediatric Medicines in the EU: 10 Years of the EU Pediatric Regulation. 2017. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32006R1901 (accessed on 1 April 2025).
- US Food and Drug Administration. Pediatric Labelling Changes. 2024. Available online: https://www.fda.gov/science-research/pediatrics/pediatric-labeling-changes (accessed on 1 April 2025).
- World Health Organization. WHO Model List of Essential Medicines for Children—9th List. 2023. Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2023.03 (accessed on 1 April 2025).
- Orubu, E.S.F.; Duncan, J.; Tuleu, C.; Turner, M.A.; Nunn, A. WHO essential medicines for children 2011–2019: Age-appropriateness of enteral formulations. Arch. Dis. Child. 2022, 107, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.; Masini, T.; Huttner, B.D.; Moja, L.; Penazzato, M.; Cappello, B. Assessing the Appropriateness of Formulations on the WHO Model List of Essential Medicines for Children: Development of a Paediatric Quality Target Product Profile Tool. Pharmaceutics 2022, 14, 473. [Google Scholar] [CrossRef]
- Nunn, T.; Williams, J. Formulation of medicines for children. Br. J. Clin. Pharmacol. 2005, 59, 674–676. [Google Scholar] [CrossRef] [PubMed]
- Baratta, F.; Zingarelli, C.; Felismè, F.; Lamy, E.; Cajuste, R.; Saint-Jean, P.H.; Ambreck, E.; Di Lascio, G.; Brusa, P. Spironolactone suspension for paediatric use: Formulation, quality and stability. Pharm. Pract. 2024, 22, 2987. [Google Scholar] [CrossRef]
- McElhiney, L.F. Case Report: The Quest for a Palatable Compounded Metronidazole (Base) Suspension. Int. J. Pharm. Compd. 2021, 25, 24–28. [Google Scholar]
- Mennella, J.A.; Reed, D.R.; Mathew, P.S.; Roberts, K.M.; Mansfield, C.J. “A spoonful of sugar helps the medicine go down”: Bitter masking by sucrose among children and adults. Chem. Senses 2015, 40, 17–25. [Google Scholar] [CrossRef]
- Mennella, J.A.; Bobowski, N.K. The sweetness and bitterness of childhood: Insights from basic research on taste preferences. Physiol. Behav. 2015, 152 Pt B, 502–507. [Google Scholar] [CrossRef]
- Mennella, J.A.; Pepino, M.Y.; Reed, D.R. Genetic and environmental determinants of bitter perception and sweet preferences. Pediatrics 2005, 115, e216-22. [Google Scholar] [CrossRef] [PubMed]
- Lipchock, S.V.; Reed, D.R.; Mennella, J.A. Relationship between bitter-taste receptor genotype and solid medication formulation usage among young children: A retrospective analysis. Clin. Ther. 2012, 34, 728–733. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baratta, F.; Germano, A.; Di Lascio, G.; Petieau, R.; Brusa, P. Establishment of galenic laboratories in developing countries to produce high quality medicines: Results of Aid Progress Pharmacist Agreement (A.P.P.A.®) Project. Croat. Med. J. 2014, 55, 662–668. [Google Scholar] [CrossRef]
- Baratta, F.; Di Lascio, G.; Tarditi, F.; Petieau, R.; Brusa, P. Galenic formulations to fight the phenomenon of counterfeiting in developing Countries. J. Drug Deliv. Sci. Technol. 2016, 32, 313–315. [Google Scholar] [CrossRef]
- Baratta, F.; Germano, A.; Brusa, P. Diffusion of counterfeit drugs in developing countries and stability of galenics stored for months under different conditions of temperature and relative humidity. Croat. Med. J. 2012, 53, 173–184. [Google Scholar] [CrossRef]
- A.P.P.A.®. Non-Profit Association Website. Available online: https://www.progettoappa.it/ (accessed on 1 April 2025).
- Moss, D.M.; Priest, J.W.; Hamlin, K.; Derado, G.; Herbein, J.; Petri, W.A., Jr.; Lammie, P.J. Longitudinal evaluation of enteric protozoa in Haitian children by stool exam and multiplex serologic assay. Am. J. Trop. Med. Hyg. 2014, 90, 653–660. [Google Scholar] [CrossRef]
- Michel, D.; Raymond, L.; Apply, A.; Daphenide St Louis, D.; Balthazard-Accou, K.; Millien, M.F.; Emmanuel, E. Contribution to the Diagnostic Study of Intestinal Parasitosis, Haiti. Eur. Sci. J. 2021, 17, 64. [Google Scholar] [CrossRef]
- European Directorate for the Quality of Medicines and HealthCare. European Pharmacopoeia, 11th ed.; Council of Europe: Geneva, Switzerland, 2023. [Google Scholar]
- Moffat, A.C.; Osselton, D.M.; Widdop, B. Clarke’s Analysis of Drugs and Poisons, 4th ed.; Pharmaceutical Press: London, UK, 2011. [Google Scholar]
- Haque, R.; Mondal, D.; Duggal, P.; Kabir, M.; Roy, S.; Farr, B.M.; Sack, R.B.; Petri, W.A., Jr. Entamoeba histolytica infection in children and protection from subsequent amebiasis. Infect. Immun. 2006, 74, 904–909. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- US Food and Drug Administration. Drugs@FDA: FDA-Approved Drugs. Available online: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=216755 (accessed on 30 May 2025).
- Drugs.com. Likmez: Package Insert/Prescribing Info. Available online: https://www.drugs.com/pro/likmez.html#s-34089-3 (accessed on 30 May 2025).
- Medicines.ie. Flagyl-S 200mg/5mL Oral Suspension Information. 2024. Available online: https://www.medicines.ie/medicines/flagyl-s-200mg-5ml-oral-suspension-32159/patient-info (accessed on 30 May 2025).
- Jarouche, M.; Ibrahim, M.; Pearson, J.; Low, M.; Rowe, J. Stability of Metronidazole Free-Base Oral Suspensions Formulated with United States Pharmacopeia-Grade Metronidazole Powder and Commercial Metronidazole Tablets. Int. J. Pharm. Compd. 2020, 24, 77–82. [Google Scholar] [PubMed]
- Ausmed Education. Why Children’s Medication Should Be Palatable. A Spoonful of Sugar—The Importance of Palatability in Children’s Medication. Available online: https://www.ausmed.com/learn/articles/palatability-in-childrens-medication (accessed on 1 April 2025).
- US Food and Drug Administration. Guidance for Industry and Other Stakeholders: Redbook 2000 Toxicological Principles for the Safety Assessment of Food Ingredients. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-and-other-stakeholders-redbook-2000 (accessed on 1 April 2025).
- EFSA (European Food Safety Authority). Sweeteners. 2025. Available online: https://www.efsa.europa.eu/it/topics/topic/sweeteners (accessed on 1 April 2025).
- Sylvetsky, A.; Rother, K.I.; Brown, R. Artificial sweetener use among children: Epidemiology, recommendations, metabolic outcomes, and future directions. Pediatr. Clin. N. Am. 2011, 58, 1467–1480. [Google Scholar] [CrossRef] [PubMed]
- Rouaz, K.; Chiclana-Rodríguez, B.; Nardi-Ricart, A.; Suñé-Pou, M.; Mercadé-Frutos, D.; Suñé-Negre, J.M.; Pérez-Lozano, P.; García-Montoya, E. Excipients in the Paediatric Population: A Review. Pharmaceutics 2021, 13, 387. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Food Additives and Flavourings (FAF); Castle, L.; Andreassen, M.; Aquilina, G.; Bastos, M.L.; Boon, P.; Fallico, B.; FitzGerald, R.; Frutos Fernandez, M.J.; Grasl-Kraupp, B.; et al. Re-evaluation of saccharin and its sodium, potassium and calcium salts (E 954) as food additives. EFSA J. 2024, 22, e9044. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- US Food and Drug Administration. GRAS Substances (SCOGS) Database. Available online: https://www.fda.gov/food/generally-recognized-safe-gras/gras-substances-scogs-database (accessed on 1 April 2025).
- Jacqz-Aigrain, E.; Kassai, B.; Cornu, C.; Cazaubiel, J.M.; Housez, B.; Cazaubiel, M.; Prével, J.M.; Bell, M.; Boileau, A.; De Cock, P. Gastrointestinal tolerance of erythritol-containing beverage in young children: A double-blind, randomised controlled trial. Eur. J. Clin. Nutr. 2015, 69, 746–751. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Food Additives and Flavourings (FAF); Younes, M.; Aquilina, G.; Castle, L.; Degen, G.; Engel, K.H.; Fowler, P.J.; Frutos Fernandez, M.J.; Fürst, P.; Gundert-Remy, U.; et al. Re-evaluation of erythritol (E 968) as a food additive. EFSA J. 2023, 21, e8430. [Google Scholar] [CrossRef]
- Arnold, A.R.; Chassaing, B. Maltodextrin, Modern Stressor of the Intestinal Environment. Cell. Mol. Gastroenterol. Hepatol. 2019, 7, 475–476. [Google Scholar] [CrossRef]
- European Medicines Agency. Guideline on Pharmaceutical Development of Medicines for Paediatric Use. 2013. Available online: www.ema.europa.eu/en/documents/scientific-guideline/guideline-pharmaceutical-development-medicines-paediatric-use_en.pdf (accessed on 1 April 2025).
- European Medicines Agency. Reflection Paper on the Use of Methyl- and Propylparaben as Excipients in Human Medicinal Products for Oral Use. 2015. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-use-methyl-propylparaben-excipients-human-medicinal-products-oral-use_en.pdf (accessed on 1 April 2025).
| Ingredients | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | 33 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Banana flavour (water-soluble) | x | x | |||||||||||||||||||||||||||||||
| Citric acid monohydrate | x | x | |||||||||||||||||||||||||||||||
| Purified water | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Erythritol | x | x | x | x | x | x | x | x | x | x | x | x | |||||||||||||||||||||
| Ethanol | x | ||||||||||||||||||||||||||||||||
| Glucose | x | x | x | x | x | ||||||||||||||||||||||||||||
| Glycerol | x | x | x | x | x | ||||||||||||||||||||||||||||
| Lemon flavour (water-soluble) | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||||||||
| Maltodextrin | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||||||||||||
| Microcrystalline cellulose | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Orange flavour (water-soluble) | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||||||||||
| Propylene glycol | x | x | x | x | x | ||||||||||||||||||||||||||||
| Sodium benzoate | x | x | x | x | x | ||||||||||||||||||||||||||||
| Sodium carboxymethyl cellulose | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Sodium citrate | x | x | |||||||||||||||||||||||||||||||
| Sodium methyl p-hydroxybenzoate | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||
| Sodium saccharin | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||||
| Sorbitol solution 70% | x | x | x | x | x | ||||||||||||||||||||||||||||
| Strawberry flavour (water-soluble) | x | x | x | ||||||||||||||||||||||||||||||
| Sucrose | x | x | |||||||||||||||||||||||||||||||
| Sucrose syrup | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Polysorbate 80 | x | x | x | x | x | x | x | x | x | ||||||||||||||||||||||||
| Xylitol | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Ingredients | Amount (g) |
|---|---|
| Metronidazole | 5.00 |
| Orange flavour (water-soluble) | 4.72 |
| Sodium carboxymethyl cellulose | 1.00 |
| Microcrystalline cellulose | 5.00 |
| Erythritol | 9.40 |
| Maltodextrin | 9.40 |
| Sodium methyl p-hydroxybenzoate | 0.10 |
| Sodium saccharin | 0.19 |
| Purified water | 95.60 |
| T0 | T 180 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Room Temperature | Thermostatic Oven | Fridge | |||||||
| Mean Area Values | Average | Mean Area Values | Δ % Compared to Average Value at T0 | Mean Area Values | Δ % Compared to Average Value at T0 | Mean Area Values | Δ % Compared to Average Value at T0 | ||
| Batches | A | 2429 | 2378 | 2343 | −1.5% | 2286 | −3.8% | 2535 | 6.6% |
| B | 2411 | 2387 | 0.4% | 2264 | −4.8% | 2240 | −5.8% | ||
| C | 2293 | 2189 | −7.9% | 2396 | 0.8% | 2270 | −4.5% | ||
| T0 | T 180 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Room Temperature | Thermostatic Oven | Fridge | |||||||
| Mean Absorbance Values | Average | Mean Absorbance Values | Δ % Compared to Average Value at T0 | Mean Absorbance Values | Δ % Compared to Average Value at T0 | Mean Absorbance Values | Δ % Compared to Average Value at T0 | ||
| Batches | A | 2.2171 | 2.2076 | 2.2744 | 3.02% | 2.1736 | −1.54% | 2.2590 | 2.33% |
| B | 2.2449 | 2.3669 | 7.21% | 2.2552 | 2.15% | 2.0151 | −8.72% | ||
| C | 2.1609 | 2.2994 | 4.16% | 2.3295 | 5.52% | 2.0817 | −5.70% | ||
| T0 | T 180 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Room Temperature | Thermostatic Oven | Fridge | |||||||
| Mean pH Value | Average | Mean pH Value | Δ % Compared to Average Value at T0 | Mean pH Value | Δ % Compared to Average Value at T0 | Mean pH Value | Δ % Compared to Average Value at T0 | ||
| Batches | A | 8.41 | 8.35 | 7.88 | −5.59% | 8.36 | 0.16% | 8.29 | −0.68% |
| B | 8.16 | 7.83 | −6.19% | 8.30 | −0.56% | 8.70 | 4.23% | ||
| C | 8.47 | 7.96 | −4.63% | 8.26 | −1.04% | 7.80 | −6.55% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baratta, F.; Zingarelli, C.; Fanton, F.; Lamy, E.; Di Lascio, G.; Brusa, P. Metronidazole Suspension for Paediatric Use in Developing Countries: Formulation, Quality, and Stability. Pharmaceutics 2025, 17, 787. https://doi.org/10.3390/pharmaceutics17060787
Baratta F, Zingarelli C, Fanton F, Lamy E, Di Lascio G, Brusa P. Metronidazole Suspension for Paediatric Use in Developing Countries: Formulation, Quality, and Stability. Pharmaceutics. 2025; 17(6):787. https://doi.org/10.3390/pharmaceutics17060787
Chicago/Turabian StyleBaratta, Francesca, Chiara Zingarelli, Federica Fanton, Editson Lamy, Gaetano Di Lascio, and Paola Brusa. 2025. "Metronidazole Suspension for Paediatric Use in Developing Countries: Formulation, Quality, and Stability" Pharmaceutics 17, no. 6: 787. https://doi.org/10.3390/pharmaceutics17060787
APA StyleBaratta, F., Zingarelli, C., Fanton, F., Lamy, E., Di Lascio, G., & Brusa, P. (2025). Metronidazole Suspension for Paediatric Use in Developing Countries: Formulation, Quality, and Stability. Pharmaceutics, 17(6), 787. https://doi.org/10.3390/pharmaceutics17060787







