Evaluation of Advanced Nanomaterials for Cancer Diagnosis and Treatment
Abstract
1. Introduction
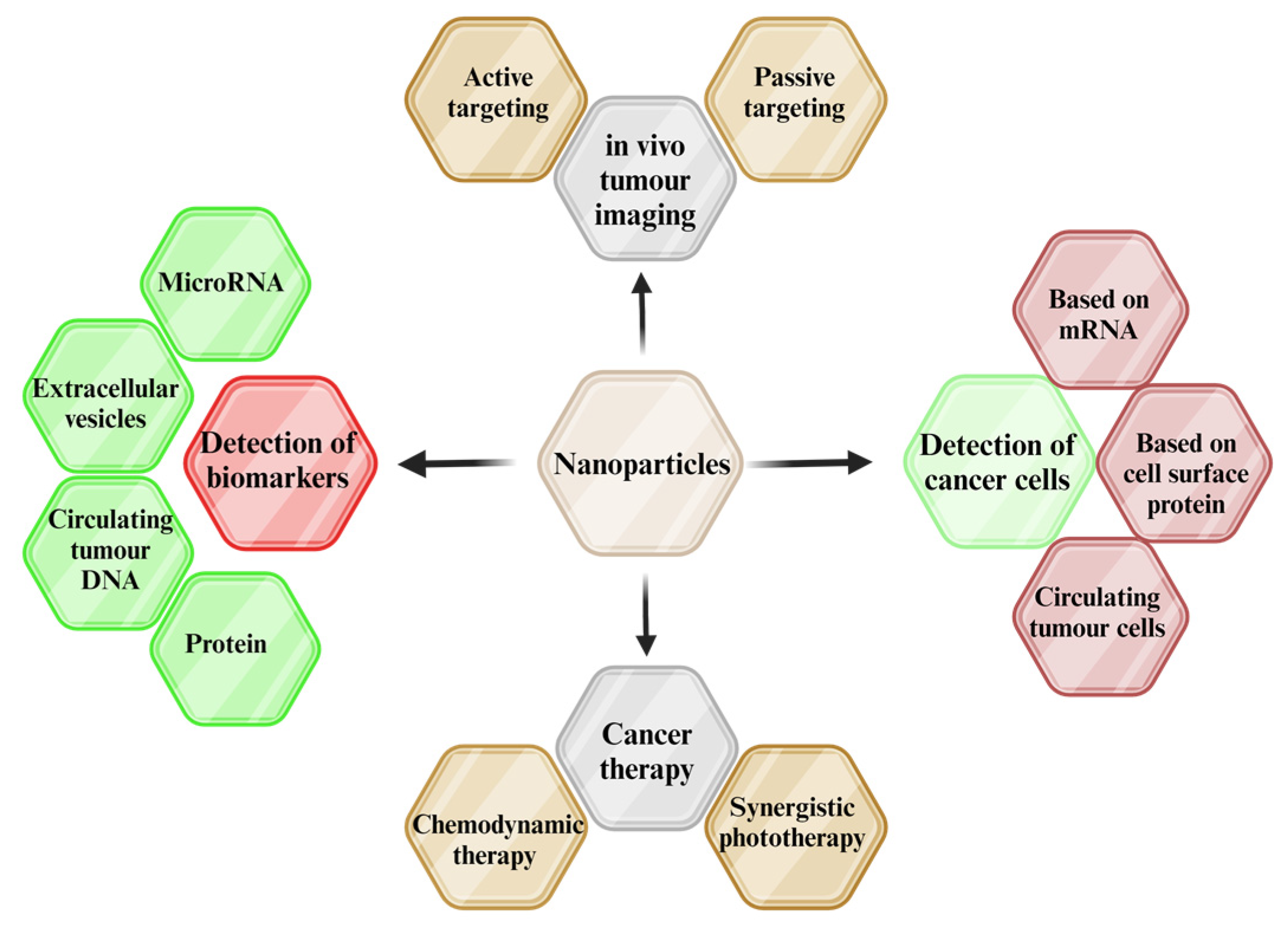
Applications of Nanotechnology for Cancer
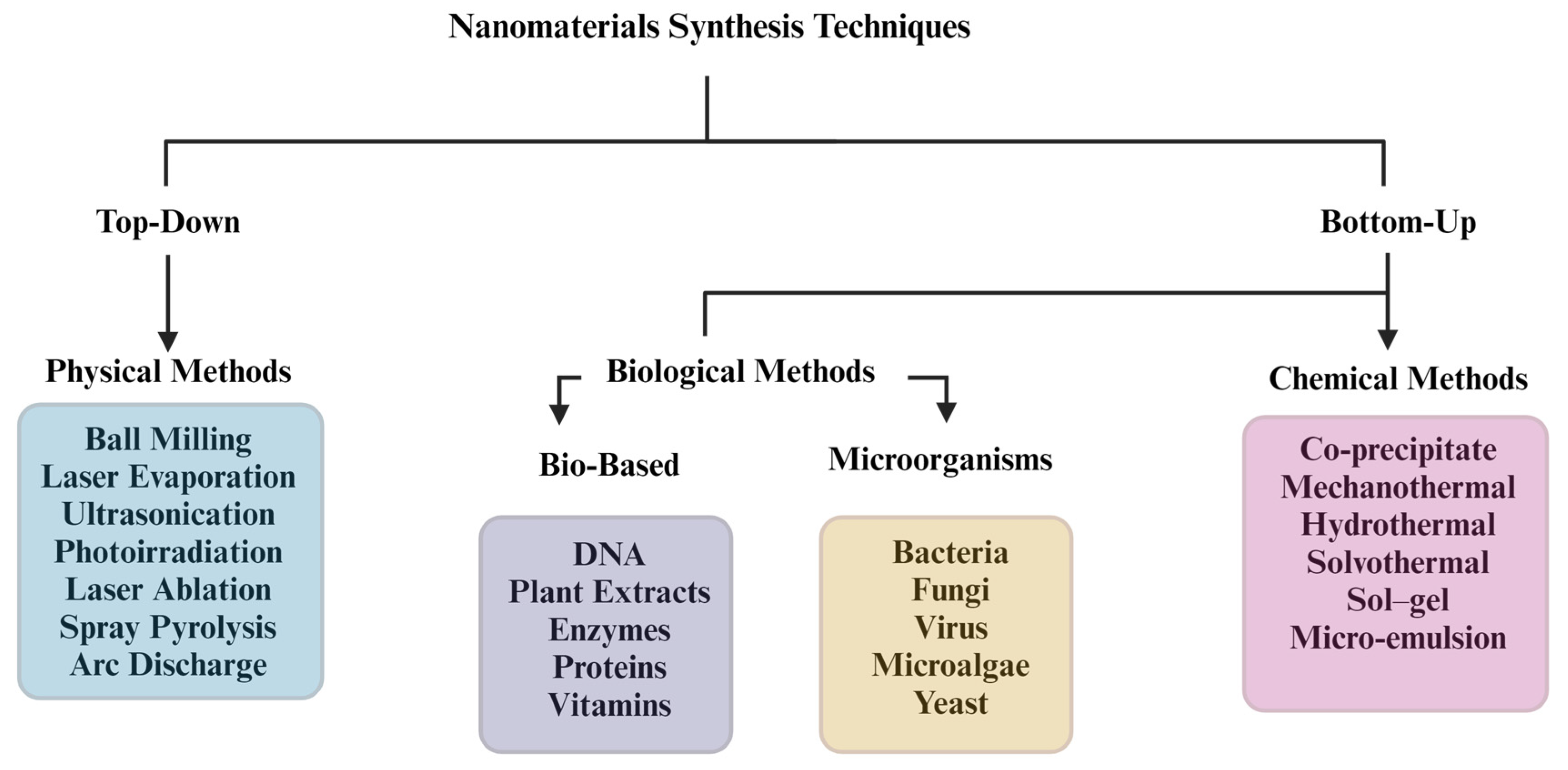
2. Synthesis Methods of NPs
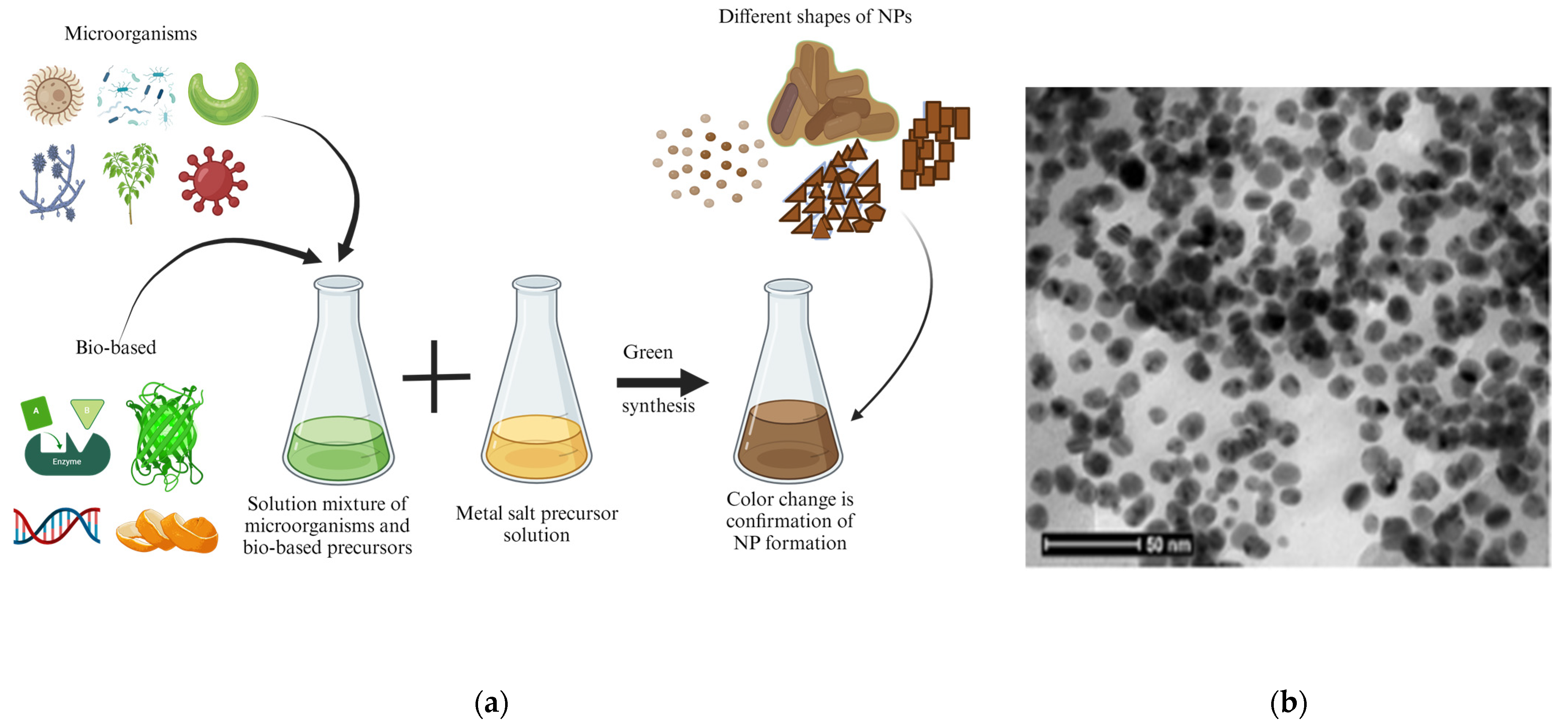
2.1. Biological Method
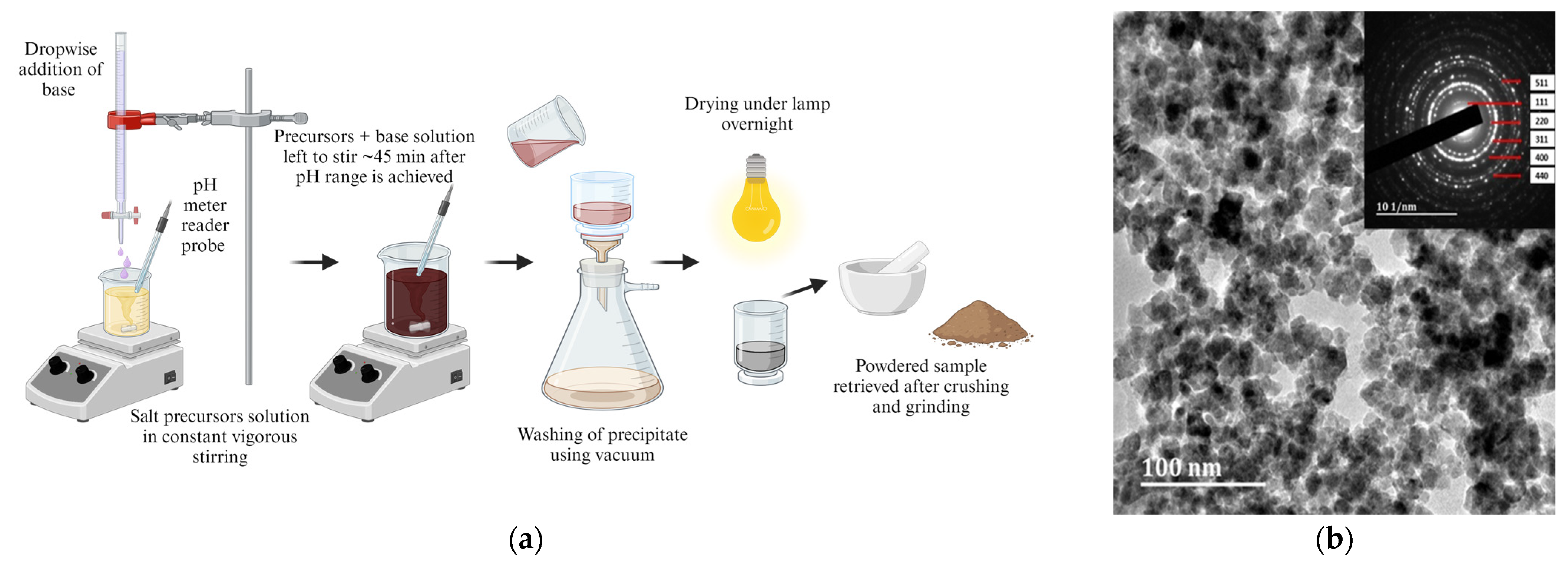
2.2. Chemical Methods
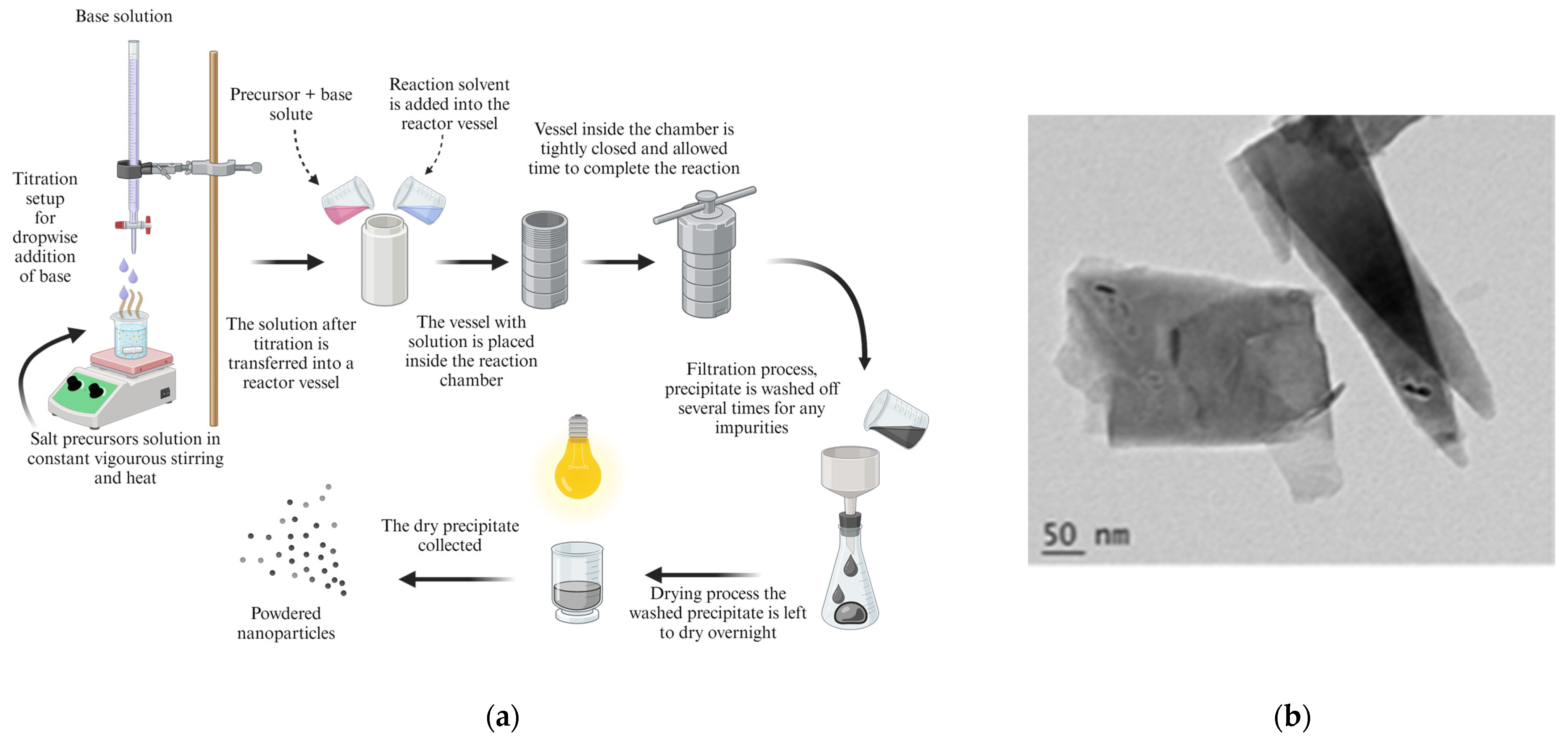
2.2.1. Co-Precipitate Method
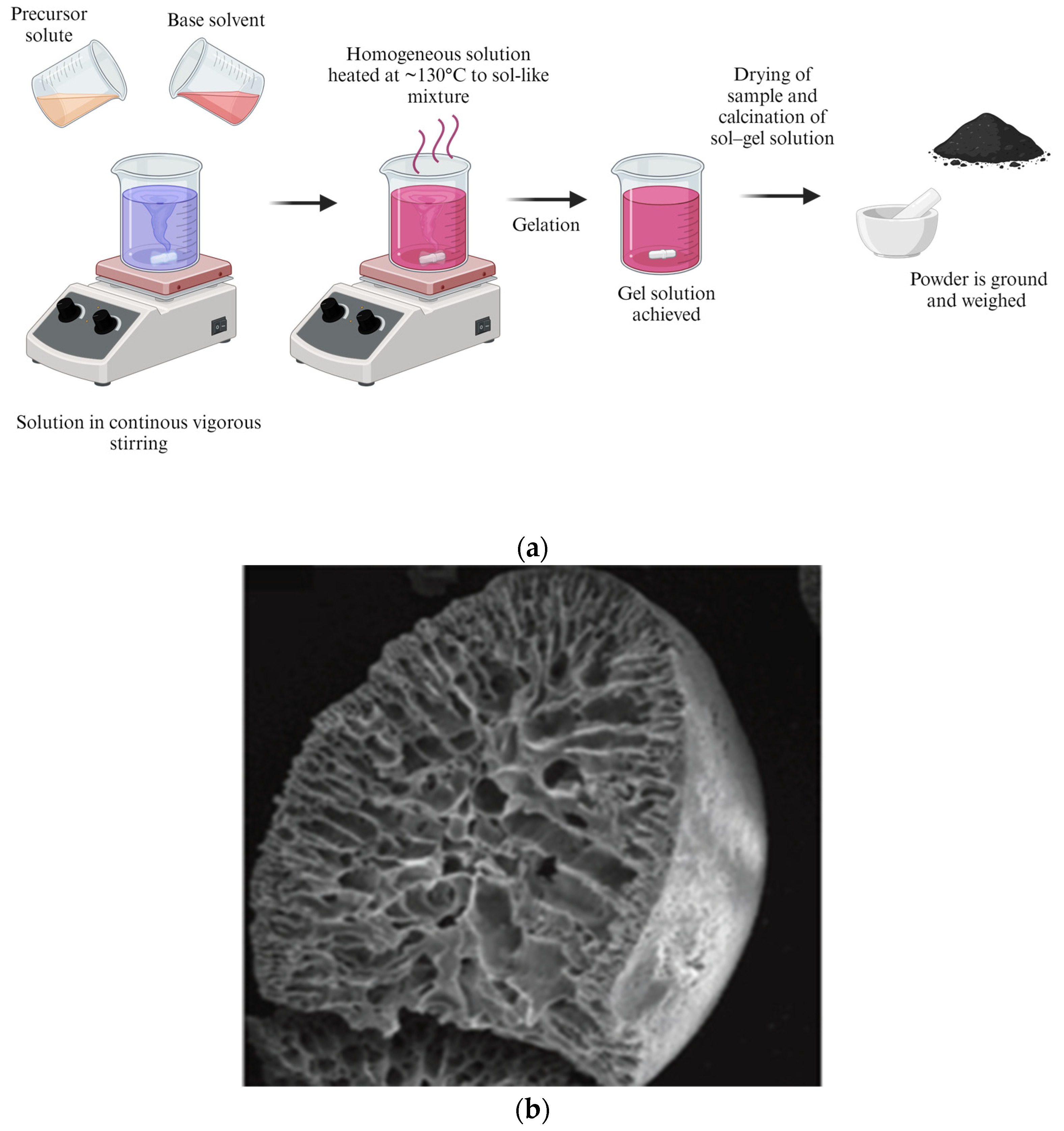
2.2.2. Sol–Gel Method
2.2.3. Thermal Methods
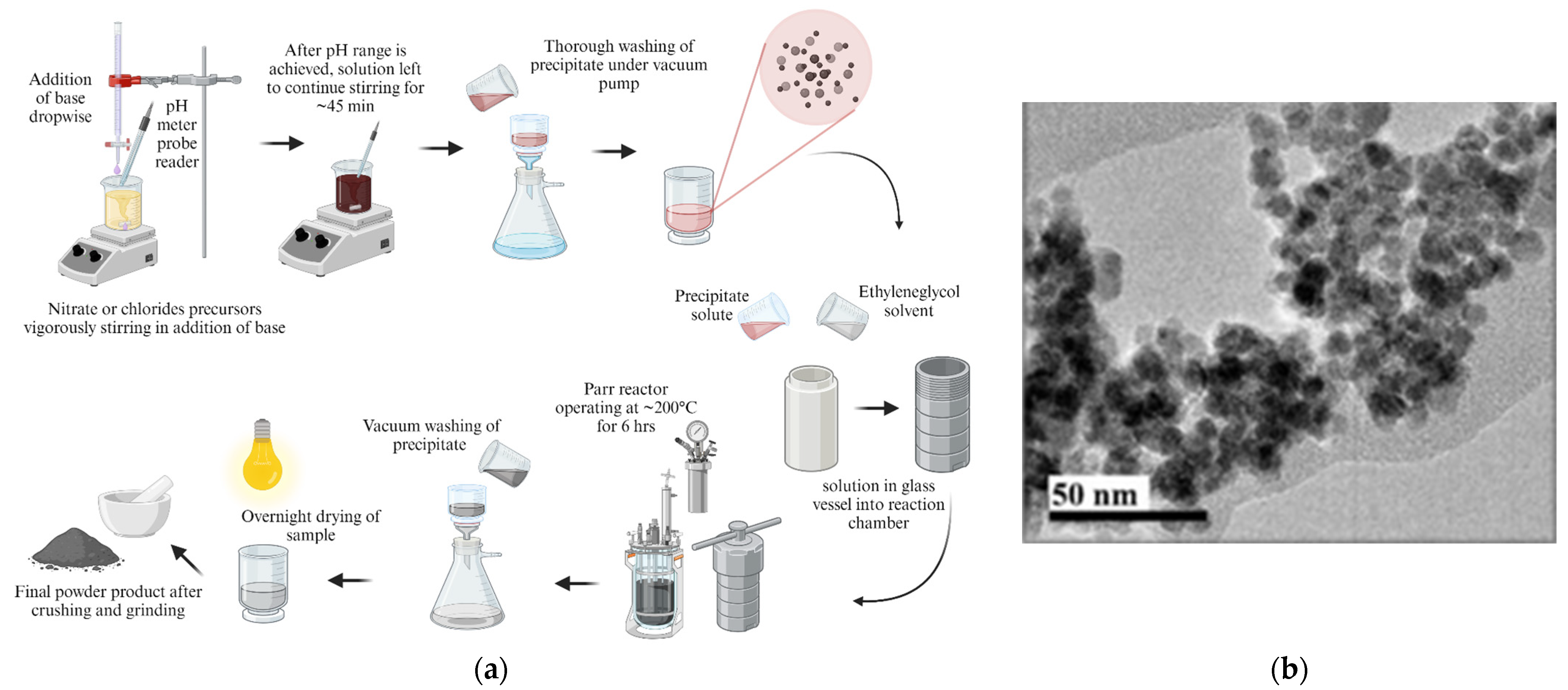
Hydrothermal Method
Solvothermal Method
Glycol-Thermal Reaction
2.3. Physical Methods
Ball Milling

3. Suitable NPs
3.1. Carbon-Based NPs
3.2. Organic Types
3.3. Inorganic Types
3.3.1. Metal Iron Oxides
3.3.2. Ferrite Materials
3.3.3. Rare Earth Metal Iron Oxides
4. Functionalization of NPs
5. Diagnostic Methods
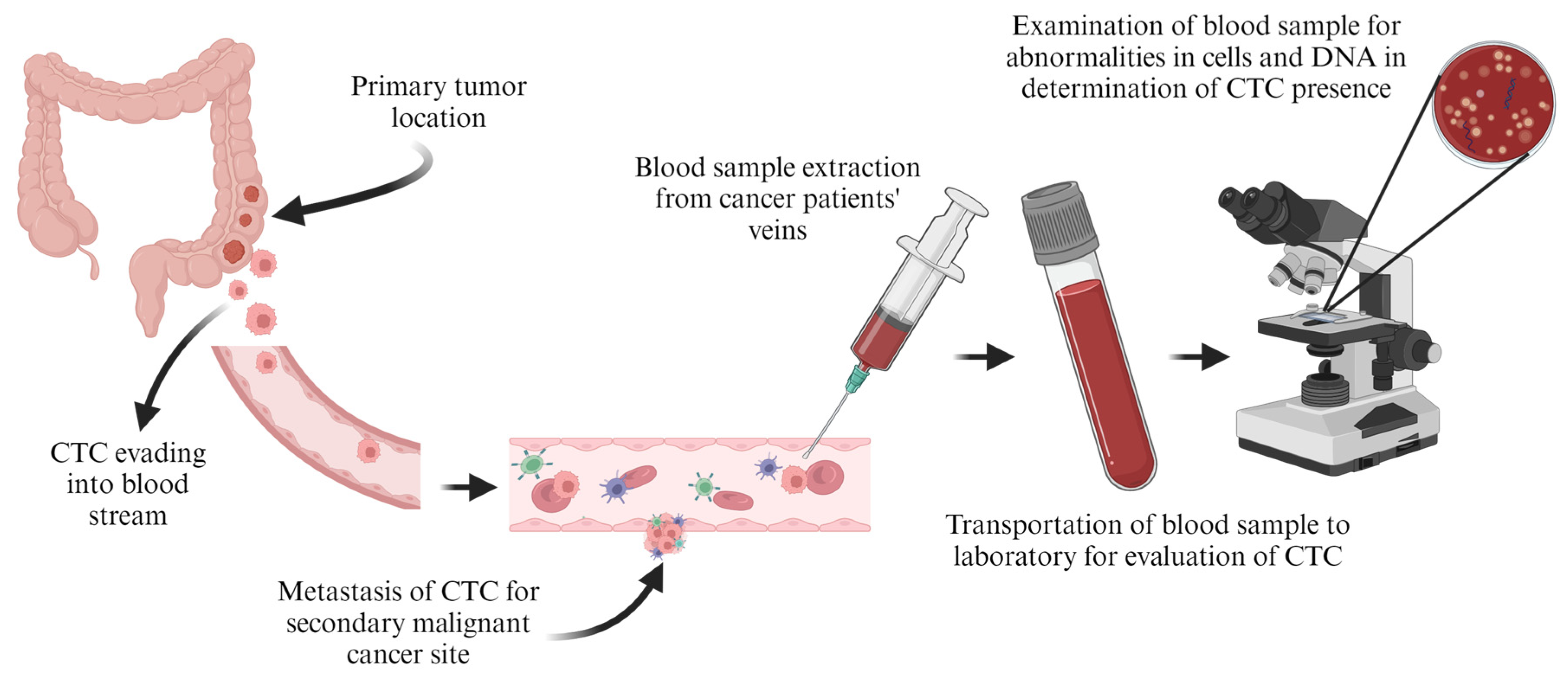
5.1. Tumour Circulation
5.2. Imaging
6. Cancer Treatment Strategies
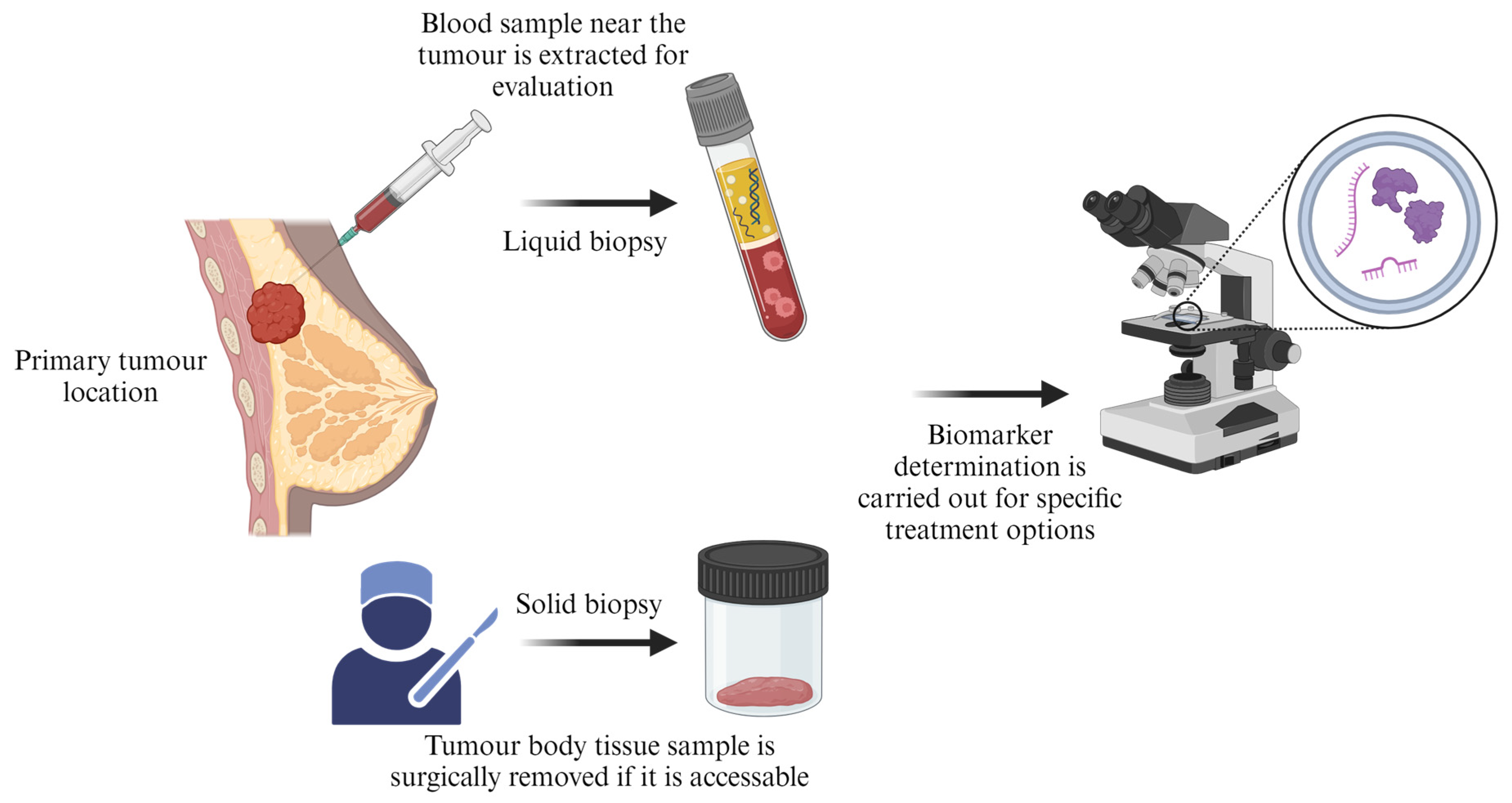
6.1. Biomarkers Testing
6.2. Hormone Therapy
6.3. Photodynamic and Photothermal Therapies
6.4. Stem Cell Transplant
6.5. Chemodynamic Therapy
6.6. Targeted Therapy
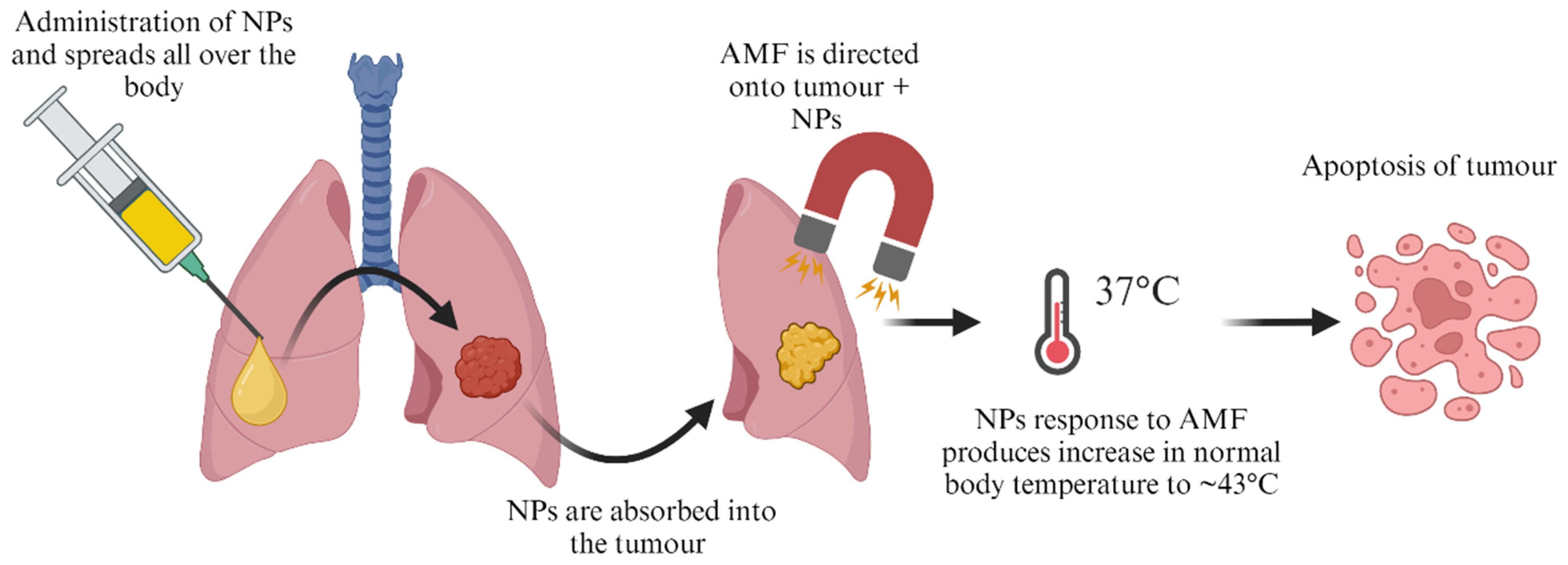
6.7. Magnetic Hyperthermia
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Randall, E. Harris: Epidemiology of Chronic Disease: Global Perspectives. 2019. Available online: https://books.google.co.za/books?id=qKKODwAAQBAJ&lpg=PP1&ots=DseRD1XEuZ&dq=epidemiology%20of%20chronic%20disease&lr&pg=PP1#v=onepage&q=epidemiology%20of%20chronic%20disease&f=false (accessed on 16 November 2023).
- Anderson, E.; Durstine, J.L. Physical activity, exercise, and chronic diseases: A brief review. Sports Med. Health Sci. 2019, 1, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Chhikara, B.S.; Parang, K. Chemical Biology Letters Global Cancer Statistics 2022: The Trends Projection Analysis. Available online: https://pubs.thesciencein.org/cbl (accessed on 2 November 2023).
- Neuhouser, M.L. The importance of healthy dietary patterns in chronic disease prevention. Nutr. Res. 2019, 70, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 2 November 2023).
- Chhikara, B.; Parang, K. Global Cancer Statistics 2022: The Trends Projection Analysis. Chemical Biology Letters. Available online: https://digitalcommons.chapman.edu/pharmacy_articles/938 (accessed on 19 November 2023).
- Cancer Prevention and Control in the Context of an Integrated Approach. Available online: https://www.who.int/publications/i/item/cancer-prevention-and-control-in-the-context-of-an-integrated-approach (accessed on 2 November 2023).
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef] [PubMed]
- NCI Cancer Stats: Cancer Statistics—NCI. Available online: https://www.cancer.gov/about-cancer/understanding/statistics (accessed on 2 November 2023).
- Maluleke, R. Cancer in South Africa; Statistics South Africa: Pretoria, South Africa, 2008. [Google Scholar]
- Norouzi, M.; Amerian, M.; Amerian, M.; Atyabi, F. Clinical applications of nanomedicine in cancer therapy. Drug Discov. Today 2020, 25, 107–125. [Google Scholar] [CrossRef] [PubMed]
- Laha, S.S.; Thorat, N.D.; Singh, G.; Sathish, C.I.; Yi, J.; Dixit, A.; Vinu, A. Rare-Earth Doped Iron Oxide Nanostructures for Cancer Theranostics: Magnetic Hyperthermia and Magnetic Resonance Imaging. Small 2022, 18, 2104855. [Google Scholar] [CrossRef] [PubMed]
- Alrushaid, N.; Khan, F.A.; Al-Suhaimi, E.A.; Elaissari, A. Nanotechnology in Cancer Diagnosis and Treatment. Pharmaceutics 2023, 15, 1025. [Google Scholar] [CrossRef]
- Thakur, S.; Thakur, A. A Review on Nanotechnology in Cancer Treatment. AIP Conf. Proc. 2023, 2535, 030005. [Google Scholar] [CrossRef]
- Sangamithra, A. The Causes of Cancer: An Analysis of Avoidable Risk Factors. Shanlax Int. J. Econ. 2021, 9, 37–40. [Google Scholar] [CrossRef]
- Cox, J.D.; Ang, K.K. Radiation Oncology: Rationale, Technique, Results; Elsevier Health Sciences: Amsterdam, The Netherlands, 2010; Volume 1072. [Google Scholar]
- Sohail, M.I.; Waris, A.A.; Ayub, M.A.; Usman, M.; ur Rehman, M.Z.; Sabir, M.; Faiz, T. Environmental application of nanomaterials: A promise to sustainable future. In Comprehensive Analytical Chemistry; Elsevier: Amsterdam, The Netherlands, 2019; pp. 1–54. [Google Scholar]
- Kumar, S.; Nehra, M.; Kedia, D.; Dilbaghi, N.; Tankeshwar, K.; Kim, K.-H. Nanotechnology-based biomaterials for orthopaedic applications: Recent advances and future prospects. Mater. Sci. Eng. 2020, 106, 110154. [Google Scholar] [CrossRef]
- Dessale, M.; Mengistu, G.; Mengist, H.M. Nanotechnology: A Promising Approach for Cancer Diagnosis, Therapeutics and Theragnosis. Int. J. Nanomed. 2022, 17, 3735–3749. [Google Scholar] [CrossRef]
- Yang, K.; Yu, G.; Yang, Z.; Yue, L.; Zhang, X.; Sun, C.; Wei, J.; Rao, L.; Chen, X.; Wang, R. Supramolecular Polymerization-Induced Nanoassemblies for Self-Augmented Cascade Chemotherapy and Chemodynamic Therapy of Tumor. Angew. Chem. Int. Ed. 2021, 60, 17570–17578. [Google Scholar] [CrossRef]
- Yan, S.; Zeng, X.; Tang, Y.; Liu, B.F.; Wang, Y.; Liu, X. Activating Antitumor Immunity and Antimetastatic Effect Through Polydopamine-Encapsulated Core–Shell Upconversion Nanoparticles. Adv. Mater. 2019, 31, 1905825. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, A.; Yadav, K.; Mishra, A.; Singh, M.S.; Chaudhary, S.; Manohar, R.; Parmar, A.S. Early diagnosis of lung cancer using magnetic nanoparticles-integrated systems. Nanotechnol. Rev. 2022, 11, 544–574. [Google Scholar] [CrossRef]
- Parayath, N.N.; Stephan, S.B.; Koehne, A.L.; Nelson, P.S.; Stephan, M.T. In vitro-transcribed antigen receptor mRNA nanocarriers for transient expression in circulating T cells in vivo. Nat. Commun. 2020, 11, 6080. [Google Scholar] [CrossRef]
- Desmond, B.J.; Dennett, E.R.; Danielson, K.M. Circulating Extracellular Vesicle MicroRNA as Diagnostic Biomarkers in Early Colorectal Cancer—A Review. Cancers 2019, 12, 52. [Google Scholar] [CrossRef]
- Key, J.; Leary, J.F. Nanoparticles for multimodal in vivo imaging in nanomedicine. Int. J. Nanomed. 2014, 9, 711–726. [Google Scholar] [CrossRef]
- Qiao, R.; Fu, C.; Forgham, H.; Javed, I.; Huang, X.; Zhu, J.; Whittaker, A.K.; Davis, T.P. Magnetic iron oxide nanoparticles for brain imaging and drug delivery. Adv. Drug Deliv. Rev. 2023, 197, 114822. [Google Scholar] [CrossRef] [PubMed]
- Ajinkya, N.; Yu, X.; Kaithal, P.; Luo, H.; Somani, P.; Ramakrishna, S. Magnetic iron oxide nanoparticle (Ionp) synthesis to applications: Present and future. Materials 2020, 13, 4644. [Google Scholar] [CrossRef]
- Jung, C.W. Surface properties of superparamagnetic iron oxide mr contrast agents: Ferumoxides, ferumoxtran, ferumoxsil. Magn. Reson. Imaging 1995, 13, 675–691. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, M.S.; Eswaraiah, A.; Crombet, T.; Piedra, P.; Saurez, G.; Iyer, H.; Arvind, A.S. Nimotuzumab, a promising therapeutic monoclonal for treatment of tumors of epithelial origin. MAbs 2009, 1, 41–48. [Google Scholar] [CrossRef]
- Xu, S.; Suzarte, M.R.; Bai, X.; Xu, B. Treatment outcome of nimotuzumab plus chemotherapy in advanced cancer patients: A single institute experience. Oncotarget 2016, 7, 33391. [Google Scholar] [CrossRef] [PubMed]
- Yuan, C.; Xu, X.-H.; Xu, L.; Liu, Y.; Sun, M.; Ni, L.-H.; Wang, X.-L.; Chen, Z.; Zhang, K.; Wan, H.-L.; et al. Cetuximab versus nimotuzumab for the treatment of ad-vanced nasopharyngeal carcinoma: A network meta-analysis. J. Buon 2017, 22, 1004–1010. [Google Scholar] [PubMed]
- Arora, H.C.; Jensen, M.P.; Yuan, Y.; Wu, A.; Vogt, S.; Paunesku, T.; Woloschak, G.E. Nanocarriers enhance doxorubicin uptake in drug-resistant ovarian cancer cells. Cancer Res. 2012, 72, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Nolte-Ernsting, C.; Adam, G.; Bücker, A.; Berges, S.; Bjørnerud, A.; Günther, R.W. Abdominal MR angiography performed using blood pool contrast agents: Comparison of a new superparamagnetic iron oxide nanoparticle and a linear gadolinium polymer. Am. J. Roentgenol. 1998, 171, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Van Gansbeke, D.; Metens, T.M.; Matos, C.; Nicaise, N.; Gay, F.; Raeymaekers, H.; Struyven, J. Effects of AMI-25 on Liver Vessels and Tumors on T1-Weighted Turbo-Field-Echo Images: Implications for Tumor Characterization. J. Magn. Reson. Imaging 1997, 7, 482–489. [Google Scholar] [CrossRef]
- Denys, A.; Arrive, L.; Servois, V.; Dubray, B.; Najmark, D.; Sibert, A.; Menu, Y. Hepatic Tumors: Detection and Characterization at 1-T MR Imaging Enhanced with AMI-25. Radiology 1994, 193, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Weissleder, R.; Stark, D.D.; Engelstad, B.L.; Bacon, B.A.; Compton, C.C.; White, D.L.; Jacobs, P.; Lewis, J. Superparamagnetic Iron Oxide: Pharmacokinetics and Toxicity. Am. J. Roentgenol. 1989, 152, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Pauleit, D.; Textor, J.; Bachmann, R.; Conrad, R.; Flacke, S.; Layer, G.; Kreft, B.; Schild, H. Hepatocellular Carcinoma: Detection with Gadolinium- and Ferumoxides-enhanced MR Imaging of the Liver1. Radiology 2002, 222, 73–80. [Google Scholar] [CrossRef]
- Bluemke, D.A.; Weber, T.M.; Rubin, D.; De Lange, E.E.; Semelka, R.; Redvanly, R.D.; Chezmar, J.; Outwater, E.; Carlos, R.; Saini, S.; et al. Hepatic MR Imaging with Ferumoxides: Multicenter Study of Safety and Effectiveness of Direct Injection Protocol1. Radiology 2003, 228, 457–464. [Google Scholar] [CrossRef]
- Montiel Schneider, M.G.; Lassalle, V.L. Magnetic iron oxide nanoparticles as novel and efficient tools for atherosclerosis diagnosis. Biomed. Pharmacother. 2017, 93, 1098–1115. [Google Scholar] [CrossRef]
- Harisinghani, M.G.; Saini, S.; Weissleder, R.; Rubin, D.; DeLange, E.; Harms, S.; Weinreb, J.; Small, W.; Sukerkar, A.; Brown, J.J.; et al. Splenic imaging with ultrasmall superparamagnetic iron oxide ferumoxtran-10 (AMI-7227): Preliminary observations. J. Comput. Assist. Tomogr. 2001, 25, 770–776. [Google Scholar] [CrossRef]
- Bernd, H.; De Kerviler, E.; Gaillard, S.; Bonnemain, B. Safety and tolerability of ultrasmall superparamagnetic iron oxide contrast agent: Comprehensive analysis of a clinical development program. Investig. Radiol. 2009, 44, 336–342. [Google Scholar] [CrossRef]
- Saini, S.; Sharma, R.; Baron, R.L.; Turner, D.A.; Ros, P.R.; Hahn, P.F.; Small, W.C.; Delange, E.E.; Stillman, A.E.; Edelman, R.R.; et al. Multicentre dose-ranging study on the efficacy of USPIO ferumoxtran-10 for liver MR imaging. Clin. Radiol. 2000, 55, 690–695. [Google Scholar] [CrossRef]
- Daldrup-Link, H.E.; Kaiser, A.; Helbich, T.; Werner, M.; Bjørnerud, A.; Link, T.M.; Rummeny, E.J. Macromolecular contrast medium (feruglose) versus small molecular contrast medium (gadopentetate) enhanced magnetic resonance imaging: Differentiation of benign and malignant breast lesions1. Acad. Radiol. 2003, 10, 1237–1246. [Google Scholar] [CrossRef] [PubMed]
- Borse, K.; Shende, P. Advances of nanoworms in diagnosis, treatment, and theranostics. Mater. Adv. 2023, 4, 4041–4053. [Google Scholar] [CrossRef]
- Park, J.H.; Von Maltzahn, G.; Zhang, L.; Schwartz, M.P.; Ruoslahti, E.; Bhatia, S.N.; Sailor, M.J. Magnetic Iron Oxide Nanoworms for Tumor Targeting and Imaging. Adv. Mater. 2008, 20, 1630. [Google Scholar] [CrossRef]
- New Coating Technology Uses “Nanoworms” to Kill COVID-19. Available online: https://phys.org/news/2021-09-coating-technology-nanoworms-covid-.html (accessed on 10 November 2023).
- Reirner, P.; Schuierer, G.; Balzer, T.; Peters, P.E. Application of a Superparamagnetic Iron Oxide (Resovistm) for MR Imaging of Human Cerebral Blood Volume. Magn. Reson. Med. 1995, 34, 694–697. [Google Scholar]
- Bleul, R.; Baki, A.; Freese, C.; Paysen, H.; Kosch, O.; Wiekhorst, F. Continuously manufactured single-core iron oxide nanoparticles for cancer theranostics as valuable contribution in translational research. Nanoscale Adv. 2020, 2, 4510–4521. [Google Scholar] [CrossRef] [PubMed]
- Borny, R.; Doz, U.; Funovics, M. Synthesis of a Novel Iron Oxide Contrast Agent as a Platform for Multimodal Molecular Imaging. Ph.D. Thesis, University of Veterinary Medicine, Vienna, Austria, 2014. [Google Scholar]
- Wan, Y.; Zhou, X. Formation mechanism of hafnium oxide nanoparticles by a hydrothermal route. RSC Adv. 2017, 7, 7763–7773. [Google Scholar] [CrossRef]
- Proust, V.; Kirscher, Q.; Nguyen, T.K.N.; Obringer, L.; Ishii, K.; Rault, L.; Demange, V.; Berthebaud, D.; Ohashi, N.; Uchikoshi, T.; et al. Hafnium Oxide Nanostructured Thin Films: Electrophoretic Deposition Process and DUV Photolithography Patterning. Nanomaterials 2022, 12, 2334. [Google Scholar] [CrossRef]
- Chouprik, A.; Negrov, D.; Tsymbal, E.Y.; Zenkevich, A. Defects in ferroelectric HfO2. Nanoscale 2021, 13, 11635–11678. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Kumar, S.; Tiwari, S.; Augustine, S.; Srivastava, S.; Yadav, B.K.; Malhotra, B.D. Highly sensitive protein functionalized nanostructured hafnium oxide based biosensing platform for non-invasive oral cancer detection. Sens. Actuators B Chem. 2016, 235, 1–10. [Google Scholar] [CrossRef]
- Mikolajick, T.; Schroeder, U.; Park, M.H. Special topic on ferroelectricity in hafnium oxide: Materials and devices. Appl. Phys. Lett. 2021, 118, 180402. [Google Scholar] [CrossRef]
- Ali, F.; Zhou, D.; Ali, M.; Ali, H.W.; Daaim, M.; Khan, S.; Hussain, M.M.; Sun, N. Recent Progress on Energy-Related Applications of HfO2-Based Ferroelectric and Antiferroelectric Materials. ACS Appl. Electron. Mater. 2020, 2, 2301–2317. [Google Scholar] [CrossRef]
- Tripathy, A.; Nine, M.J.; Silva, F.S. Biosensing platform on ferrite magnetic nanoparticles: Synthesis, functionalization, mechanism and applications. Adv. Colloid Interface Sci. 2021, 290, 102380. [Google Scholar] [CrossRef] [PubMed]
- Reddy, K.R.; Reddy, P.A.; Reddy, C.V.; Shetti, N.P.; Babu, B.; Ravindranadh, K.; Shankar, M.V.; Reddy, M.C.; Soni, S.; Naveen, S. Functionalized magnetic nanoparticles/biopolymer hybrids: Synthesis methods, properties and biomedical applications. In Methods in Microbiology; Elsevier: Amsterdam, The Netherlands, 2019; pp. 227–254. [Google Scholar]
- Nguyen, M.D.; Tran, H.V.; Xu, S.; Lee, T.R. Fe3O4 nanoparticles: Structures, synthesis, magnetic properties, surface functionalization, and emerging applications. Appl. Sci. 2021, 11, 11301. [Google Scholar] [CrossRef] [PubMed]
- Materón, E.M.; Miyazaki, C.M.; Carr, O.; Joshi, N.; Picciani, P.H.S.; Dalmaschio, C.J.; Davis, F.; Shimizu, F.M. Magnetic nanoparticles in biomedical applications: A review. Appl. Surf. Sci. Adv. 2021, 6, 100163. [Google Scholar] [CrossRef]
- Mollarasouli, F.; Zor, E.; Ozcelikay, G.; Ozkan, S.A. Magnetic nanoparticles in developing electrochemical sensors for pharmaceutical and biomedical applications. Talanta 2021, 226, 122108. [Google Scholar] [CrossRef] [PubMed]
- Spanos, A.; Athanasiou, K.; Ioannou, A.; Fotopoulos, V.; Krasia-Christoforou, T. Functionalized magnetic nanomaterials in agricultural applications. Nanomaterials 2021, 11, 3106. [Google Scholar] [CrossRef]
- Ali, A.; Shah, T.; Ullah, R.; Zhou, P.; Guo, M.; Ovais, M.; Tan, Z.; Rui, Y. Review on recent progress in magnetic nanoparticles: Synthesis, characterization, and diverse applications. Front. Chem. 2021, 9, 629054. [Google Scholar] [CrossRef]
- Andrade, R.G.D.; Veloso, S.R.S.; Castanheira, E.M.S. Shape anisotropic iron oxide-based magnetic nanoparticles: Synthesis and biomedical applications. Int. J. Mol. Sci. 2020, 21, 2455. [Google Scholar] [CrossRef]
- Martínez, S.A.H.; Melchor-Martínez, E.M.; Hernández, J.A.R.; Parra-Saldívar, R.; Iqbal, H.M.N. Magnetic nanomaterials assisted nanobiocatalysis systems and their applications in biofuels production. Fuel 2022, 312, 122927. [Google Scholar] [CrossRef]
- Baki, A.; Wiekhorst, F.; Bleul, R. Advances in magnetic nanoparticles engineering for biomedical applications—A Review. Bioengineering 2021, 8, 134. [Google Scholar] [CrossRef] [PubMed]
- Gavilán, H.; Avugadda, S.K.; Fernández-Cabada, T.; Soni, N.; Cassani, M.; Mai, B.T.; Chantrell, R.; Pellegrino, T. Magnetic nanoparticles and clusters for magnetic hyperthermia: Optimizing their heat performance and developing combinatorial therapies to tackle cancer. Chem. Soc. Rev. 2021, 50, 11614–11667. [Google Scholar] [CrossRef] [PubMed]
- Mokhosi, S.R.; Mdlalose, W.; Nhlapo, A.; Singh, M. Advances in the synthesis and application of magnetic ferrite nanoparticles for cancer therapy. Pharmaceutics 2022, 14, 937. [Google Scholar] [CrossRef] [PubMed]
- Adewunmi, A.A.; Kamal, M.S.; Solling, T.I. Application of magnetic nanoparticles in demulsification: A review on synthesis, performance, recyclability, and challenges. J. Pet. Sci. Eng. 2021, 196, 107680. [Google Scholar] [CrossRef]
- Abid, N.; Khan, A.M.; Shujait, S.; Chaudhary, K.; Ikram, M.; Imran, M.; Haider, J.; Khan, M.; Khan, Q.; Maqbool, M. Synthesis of nanomaterials using various top-down and bottom-up approaches, influencing factors, advantages, and disadvantages: A review. Adv. Colloid Interface Sci. 2022, 300, 102597. [Google Scholar] [CrossRef] [PubMed]
- Joudeh, N.; Linke, D. Nanoparticle classification, physicochemical properties, characterization, and applications: A comprehensive review for biologists. J. Nanobiotechnol. 2022, 20, 262. [Google Scholar] [CrossRef] [PubMed]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; Rodriguez-Torres, M.D.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef]
- Muthu, M.S.; Rajesh, C.V.; Mishra, A.; Singh, S. Stimulus-responsive targeted nanomicelles for effective cancer therapy. Nanomedicine 2009, 4, 657–667. [Google Scholar] [CrossRef]
- Hoshyar, N.; Gray, S.; Han, H.; Bao, G. The effect of nanoparticle size on in vivo pharmacokinetics and cellular interaction. Nanomedicine 2016, 11, 673–692. [Google Scholar] [CrossRef]
- Yusuf, A.; Almotairy, A.R.Z.; Henidi, H.; Alshehri, O.Y.; Aldughaim, M.S. Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers 2023, 15, 1596. [Google Scholar] [CrossRef]
- Dulińska-Litewka, J.; Łazarczyk, A.; Hałubiec, P.; Szafrański, O.; Karnas, K.; Karewicz, A. Superparamagnetic iron oxide nanoparticles-current and prospective medical applications. Materials 2019, 12, 617. [Google Scholar] [CrossRef]
- Li, L.; Jiang, W.; Luo, K.; Song, H.; Lan, F.; Wu, Y.; Gu, Z. Superparamagnetic iron oxide nanoparticles as MRI contrast agents for non-invasive stem cell labeling and tracking. Theranostics 2013, 3, 595. [Google Scholar] [CrossRef]
- Mikušová, V.; Mikuš, P. Advances in chitosan-based nanoparticles for drug delivery. Int. J. Mol. Sci. 2021, 22, 9652. [Google Scholar] [CrossRef]
- Odaudu, O.R.; Akinsiku, A.A. Toxicity and Cytotoxicity Effects of Selected Nanoparticles: A Review. IOP Conf. Ser. Earth Environ. Sci. 2022, 1054, 012007. [Google Scholar] [CrossRef]
- Sun, L.; Liu, H.; Ye, Y.; Lei, Y.; Islam, R.; Tan, S.; Tong, R.; Miao, Y.B.; Cai, L. Smart nanoparticles for cancer therapy. Signal Transduct. Target. Ther. 2023, 8, 418. [Google Scholar] [CrossRef]
- Abbasi, R.; Shineh, G.; Mobaraki, M.; Doughty, S.; Tayebi, L. Structural parameters of nanoparticles affecting their toxicity for biomedical applications: A review. J. Nanopart. Res. 2023, 25, 43. [Google Scholar] [CrossRef] [PubMed]
- Egbuna, C.; Parmar, V.K.; Jeevanandam, J.; Ezzat, S.M.; Patrick-Iwuanyanwu, K.C.; Adetunji, C.O.; Khan, J.; Onyeike, E.N.; Uche, C.Z.; Akram, M.; et al. Toxicity of Nanoparticles in Biomedical Application: Nanotoxicology. J. Toxicol. 2021, 2021, 9954443. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Saeed, K.; Khan, I. Nanoparticles: Properties, applications and toxicities. Arab. J. Chem. 2019, 12, 908–931. [Google Scholar] [CrossRef]
- Patil, S.; Chandrasekaran, R. Biogenic nanoparticles: A comprehensive perspective in synthesis, characterization, application and its challenges. J. Genet. Eng. Biotechnol. 2020, 18, 67. [Google Scholar] [CrossRef] [PubMed]
- Chand, K.; Cao, D.; Eldin Fouad, D.; Hussain Shah, A.; Qadeer Dayo, A.; Zhu, K.; Nazim Lakhan, M.; Mehdi, G.; Dong, S. Green synthesis, characterization and photocatalytic application of silver nanoparticles synthesized by various plant extracts. Arabian J. Chem. 2020, 13, 8248–8261. [Google Scholar] [CrossRef]
- Samrot, A.V.; Sahithya, C.S.; Selvarani, J.; Purayil, S.K.; Ponnaiah, P. A review on synthesis, characterization and potential biological applications of superparamagnetic iron oxide nanoparticles. Curr. Res. Green Sustain. Chem. 2021, 4, 100042. [Google Scholar] [CrossRef]
- Hamdy, N.M.; Boseila, A.A.; Ramadan, A.; Basalious, E.B. Iron Oxide Nanoparticles-Plant Insignia Synthesis with Favorable Biomedical Activities and Less Toxicity, in the “Era of the-Green”: A Systematic Review. Pharmaceutics 2022, 14, 844. [Google Scholar] [CrossRef] [PubMed]
- Sajid, M.; Płotka-Wasylka, J. Nanoparticles: Synthesis, characteristics, and applications in analytical and other sciences. Microchem. J. 2020, 154, 104623. [Google Scholar] [CrossRef]
- Tripathy, S.; Rodrigues, J.; Shimpi, N.G. Top-down and Bottom-up Approaches for Synthesis of Nanoparticles. Nanobiomaterials Perspect. Med. Appl. Diagn. Treat. Dis. 2023, 145, 92–130. [Google Scholar]
- Spoială, A.; Ilie, C.-I.; Crăciun, L.N.; Ficai, D.; Ficai, A.; Andronescu, E. Magnetite-silica core/shell nanostructures: From surface Functionalization towards biomedical applications—A review. Appl. Sci. 2021, 11, 11075. [Google Scholar] [CrossRef]
- Shabani, N.; Javadi, A.; Jafarizadeh-Malmiri, H.; Mirzaie, H.; Sadeghi, J. Potential application of iron oxide nanoparticles synthesized by co-precipitation technology as a coagulant for water treatment in settling tanks. Min. Metall. Explor. 2021, 38, 269–276. [Google Scholar] [CrossRef]
- Andhare, D.D.; Patade, S.R.; Kounsalye, J.S.; Jadhav, K.M. Effect of Zn doping on structural, magnetic and optical properties of cobalt ferrite nanoparticles synthesized via. Co-precipitation method. Phys. B Condens Matter 2020, 583, 412051. [Google Scholar] [CrossRef]
- Ahmaruzzaman, M. Metal oxides (ZnO, CuO and NiO)-based nanostructured materials for photocatalytic remediation of organic contaminants. Nanotechnol. Environ. Eng. 2023, 8, 219–235. [Google Scholar] [CrossRef]
- Bokov, D.; Turki Jalil, A.; Chupradit, S.; Suksatan, W.; Javed Ansari, M.; Shewael, I.H.; Valiev, G.H.; Kianfar, E. Nanomaterial by Sol-Gel Method: Synthesis and Application. Adv. Mater. Sci. Eng. 2021, 2021, 5102014. [Google Scholar] [CrossRef]
- Parashar, M.; Shukla, V.K.; Singh, R. Metal oxides nanoparticles via sol–gel method: A review on synthesis, characterization and applications. J. Mater. Sci. Mater. Electron. 2020, 31, 3729–3749. [Google Scholar] [CrossRef]
- Dharmalingam, P.; Palani, G.; Apsari, R.; Kannan, K.; Lakkaboyana, S.K.; Venkateswarlu, K.; Kumar, V.; Ali, Y. Synthesis of metal oxides/sulfides-based nanocomposites and their environmental applications: A review. Mater. Today Sustain. 2022, 20, 100232. [Google Scholar] [CrossRef]
- Jamkhande, P.G.; Ghule, N.W.; Bamer, A.H.; Kalaskar, M.G. Metal nanoparticles synthesis: An overview on methods of preparation, advantages and disadvantages, and applications. J. Drug Deliv. Sci. Technol. 2019, 53, 101174. [Google Scholar] [CrossRef]
- Walton, R.I. Perovskite oxides prepared by hydrothermal and solvothermal synthesis: A review of crystallisation, chemistry, and compositions. Chem. –A Eur. J. 2020, 26, 9041–9069. [Google Scholar] [CrossRef] [PubMed]
- Mohan, S.; Vellakkat, M.; Aravind, A.; Reka, U. Hydrothermal synthesis and characterization of Zinc Oxide nanoparticles of various shapes under different reaction conditions. Nano Express 2020, 1, 030028. [Google Scholar] [CrossRef]
- Jesus, A.C.B.; de Jesus, J.R.; Lima, R.J.S.; Moura, K.O.; Almeida, J.M.A.; Duque, J.G.S.; Meneses, C.T. Synthesis and magnetic interaction on concentrated Fe3O4 nanoparticles obtained by the co-precipitation and hydrothermal chemical methods. Ceram. Int. 2020, 46, 11149–11153. [Google Scholar] [CrossRef]
- Torres-Gómez, N.; Nava, O.; Argueta-Figueroa, L.; García-Contreras, R.; Baeza-Barrera, A.; Vilchis-Nestor, A.R. Shape tuning of magnetite nanoparticles obtained by hydrothermal synthesis: Effect of temperature. J. Nanomater. 2019, 2019, 7921273. [Google Scholar] [CrossRef]
- de Mello, L.B.; Varanda, L.C.; Sigoli, F.A.; Mazali, I.O. Co-precipitation synthesis of (Zn-Mn)-co-doped magnetite nanoparticles and their application in magnetic hyperthermia. J. Alloys Compd. 2019, 779, 698–705. [Google Scholar] [CrossRef]
- Huo, Y.; Xiu, S.; Meng, L.-Y.; Quan, B. Solvothermal synthesis and applications of micro/nano carbons: A review. Chem. Eng. J. 2023, 451, 138572. [Google Scholar] [CrossRef]
- Ganapathe, L.S.; Mohamed, M.A.; Mohamad Yunus, R.; Berhanuddin, D.D. Magnetite (Fe3O4) nanoparticles in biomedical application: From synthesis to surface functionalisation. Magnetochemistry 2020, 6, 68. [Google Scholar] [CrossRef]
- Nhlapo, T.A.; Moyo, T. The effect of particle size on structural and magnetic properties of Sm3+ ion substituted Zn-Mn nanoferrites synthesized by glycol-thermal method. J. Magn. Magn. Mater. 2020, 513, 167096. [Google Scholar] [CrossRef]
- Anyanwu, V.O.; Friedrich, H.B.; Mahomed, A.S.; Singh, S.; Moyo, T. Phase Transition of High-Surface-Area Glycol–Thermal Synthesized Lanthanum Manganite. Materials 2023, 16, 1274. [Google Scholar] [CrossRef]
- Mdlalose, W.B.; Dlamini, S.; Moyo, T.; Mokhosi, S.R.; Singh, M. Chitosan coating by mechanical milling of MnFe2O4 and Mn0.5Co0.5Fe2O4: Effect of milling. J. Phys. Conf. Ser. 2019, 1310, 012016. [Google Scholar] [CrossRef]
- Balasubramanian, J.; Lemere, J.; Khan, S.S.; Agarwal, N.R. Plasmonic nanosensors and their spectroscopic applications—Current trends and future perspectives. In Molecular and Laser Spectroscopy; Elsevier: Amsterdam, The Netherlands, 2022; pp. 337–372. [Google Scholar]
- Mucsi, G. A review on mechanical activation and mechanical alloying in stirred media mill. Chem. Eng. Res. Des. 2019, 148, 460–474. [Google Scholar] [CrossRef]
- El-Eskandarany, M.S.; Al-Hazza, A.; Al-Hajji, L.A.; Ali, N.; Al-Duweesh, A.A.; Banyan, M.; Al-Ajmi, F. Mechanical milling: A superior nanotechnological tool for fabrication of nanocrystalline and nanocomposite materials. Nanomaterials 2021, 11, 2484. [Google Scholar] [CrossRef]
- Kumar, M.; Xiong, X.; Wan, Z.; Sun, Y.; Tsang, D.C.W.; Gupta, J.; Gao, B.; Cao, X.; Tang, J.; Ok, Y.S. Ball milling as a mechanochemical technology for fabrication of novel biochar nanomaterials. Bioresour. Technol. 2020, 312, 123613. [Google Scholar] [CrossRef]
- Wu, K.; Su, D.; Liu, J.; Saha, R.; Wang, J.-P. Magnetic nanoparticles in nanomedicine: A review of recent advances. Nanotechnology 2019, 30, 502003. [Google Scholar] [CrossRef]
- Wei, X.; Wang, X.; Gao, B.; Zou, W.; Dong, L. Facile Ball-Milling Synthesis of CuO/Biochar Nanocomposites for Efficient Removal of Reactive Red 120. ACS Omega 2020, 5, 5748–5755. [Google Scholar] [CrossRef]
- Grodzinski, P.; Kircher, M.; Goldberg, M.; Gabizon, A. Integrating nanotechnology into cancer care. CS Nano 2019, 13, 7370–7376. [Google Scholar] [CrossRef]
- Gavas, S.; Quazi, S.; Karpiński, T.M. Nanoparticles for Cancer Therapy: Current Progress and Challenges. Nanoscale Res. Lett. 2021, 16, 173. [Google Scholar] [CrossRef]
- Soetaert, F.; Korangath, P.; Serantes, D.; Fiering, S.; Ivkov, R. Cancer therapy with iron oxide nanoparticles: Agents of thermal and immune therapies. Adv. Drug Deliv. Rev. 2020, 163–164, 65–83. [Google Scholar] [CrossRef]
- Madannejad, R.; Shoaie, N.; Jahanpeyma, F.; Darvishi, M.H.; Azimzadeh, M.; Javadi, H. Toxicity of carbon-based nanomaterials: Reviewing recent reports in medical and biological systems. Chem. Biol. Interact. 2019, 307, 206–222. [Google Scholar] [CrossRef]
- Patel, K.D.; Singh, R.K.; Kim, H.-W. Carbon-based nanomaterials as an emerging platform for theranostics. Mater. Horiz. 2019, 6, 434–469. [Google Scholar] [CrossRef]
- Maiti, D.; Tong, X.; Mou, X.; Yang, K. Carbon-based nanomaterials for biomedical applications: A recent study. Front. Pharmacol. 2019, 9, 1401. [Google Scholar] [CrossRef]
- Hosnedlova, B.; Kepinska, M.; Fernandez, C.; Peng, Q.; Ruttkay-Nedecky, B.; Milnerowicz, H.; Kizek, R. Carbon nanomaterials for targeted cancer therapy drugs: A critical review. Chem. Record. 2019, 19, 502–522. [Google Scholar] [CrossRef]
- Zare, E.N.; Padil, V.V.T.; Mokhtari, B.; Venkateshaiah, A.; Wacławek, S.; Černík, M.; Tay, F.R.; Varma, R.S.; Makvandi, P. Advances in biogenically synthesized shaped metal-and carbon-based nanoarchitectures and their medicinal applications. Adv. Colloid Interface Sci. 2020, 283, 102236. [Google Scholar] [CrossRef]
- Mekuye, B.; Abera, B. Nanomaterials: An overview of synthesis, classification, characterization, and applications. Nano Select. 2023, 4, 486–501. [Google Scholar] [CrossRef]
- Virlan, M.J.R.; Miricescu, D.; Radulescu, R.; Sabliov, C.M.; Totan, A.; Calenic, B.; Greabu, M. Organic Nanomaterials and Their Applications in the Treatment of Oral Diseases. Molecules 2016, 21, 207. [Google Scholar] [CrossRef]
- Dong, H.; Hu, W. Organic Nanomaterials. In Springer Handbook of Nanomaterials; Vajtai, R., Ed.; Springer Berlin Heidelberg: Berlin/Heidelberg, Germany, 2013; pp. 905–940. [Google Scholar]
- Gulumian, M.; Thwala, M.; Makhoba, X.; Wepener, V. Current situation and future prognosis of health, safety and environment risk assessment of nanomaterials in South Africa. S. Afr. J. Sci. 2023, 119, 3–7. [Google Scholar] [CrossRef]
- Sun, L.; Wang, P.; Zhang, J.; Sun, Y.; Sun, S.; Xu, M.; Zhang, L.; Wang, S.; Liang, X.; Cui, L. Design and application of inorganic nanoparticles for sonodynamic cancer therapy. Biomater. Sci. 2021, 9, 1945–1960. [Google Scholar] [CrossRef]
- Sun, M.; Wang, T.; Li, L.; Li, X.; Zhai, Y.; Zhang, J.; Li, W. The application of inorganic nanoparticles in molecular targeted cancer therapy: EGFR targeting. Front. Pharmacol. 2021, 12, 702445. [Google Scholar] [CrossRef] [PubMed]
- Aghebati-Maleki, A.; Dolati, S.; Ahmadi, M.; Baghbanzhadeh, A.; Asadi, M.; Fotouhi, A.; Yousefi, M.; Aghebati-Maleki, L. Nanoparticles and cancer therapy: Perspectives for application of nanoparticles in the treatment of cancers. J. Cell. Physiol. 2020, 235, 1962–1972. [Google Scholar] [CrossRef]
- Salih, S.J.; Mahmood, W.M. Review on magnetic spinel ferrite (MFe2O4) nanoparticles: From synthesis to application. Heliyon 2023, 9, e16601. [Google Scholar] [CrossRef] [PubMed]
- Van Gosen, B.S.; Verplanck, P.L.; Long, K.R.; Gambogi, J.; Seal, R.R., II; Survey, U.S.G. The Rare-Earth Elements: Vital to Modern Technologies and Lifestyles; US Geological Survey: Reston, VA, USA, 2014. [Google Scholar]
- Vidal Llauradó, J. Rare Earth Elements: The Pillar of Modern Technologies; Universitat Pompeu Fabra: Barcelona, Spain, 2023. [Google Scholar]
- Nikumbh, A.K.; Pawar, R.A.; Nighot, D.V.; Gugale, G.S.; Sangale, M.D.; Khanvilkar, M.B.; Nagawade, A.V. Structural, electrical, magnetic and dielectric properties of rare-earth substituted cobalt ferrites nanoparticles synthesized by the co-precipitation method. J. Magn. Magn. Mater. 2014, 355, 201–209. [Google Scholar] [CrossRef]
- Mukherjee, D.; Sil, M.; Goswami, A.; Lahiri, D.; Nag, M. Antibiofilm Activities of Carbon-Based Nanoparticles and Nanocomposites: A Comparative Review. J. Inorg. Organomet. Polym. Mater. 2023, 33, 3961–3983. [Google Scholar] [CrossRef]
- Jalilinejad, N.; Rabiee, M.; Baheiraei, N.; Ghahremanzadeh, R.; Salarian, R.; Rabiee, N.; Akhavan, O.; Zarrintaj, P.; Hejna, A.; Saeb, M.R.; et al. Electrically conductive carbon-based (bio)-nanomaterials for cardiac tissue engineering. Bioeng. Transl. Med. 2023, 8, e10347. [Google Scholar] [CrossRef]
- Loura, N.; Singh, M.; Dhull, V. Elite nanomaterials in cancer detection and therapy. Emergent Mater. 2023, 6, 1415–1440. [Google Scholar] [CrossRef]
- Narayanan, K.B.; Sakthivel, N.; Han, S.S. From Chemistry to Biology: Applications and Advantages of Green, Biosynthesized/Biofabricated Metal- and Carbon-based Nanoparticles. Fibers Polym. 2021, 22, 877–897. [Google Scholar] [CrossRef]
- Wang, C.; Sun, S.; Wang, P.; Zhao, H.; Li, W. Nanotechnology-based analytical techniques for the detection of contaminants in aquatic products. Talanta 2024, 269, 125462. [Google Scholar] [CrossRef]
- Thomas, D.T.; Baby, A.; Raman, V.; Balakrishnan, S.P. Carbon-Based Nanomaterials for Cancer Treatment and Diagnosis: A Review. ChemistrySelect 2022, 7, e202202455. [Google Scholar] [CrossRef]
- Rao, N.; Singh, R.; Bashambu, L. Carbon-based nanomaterials: Synthesis and prospective applications. In Materials Today: Proceedings; Elsevier Ltd.: Amsterdam, The Netherlands, 2021; pp. 608–614. [Google Scholar]
- Fang, F.; Li, M.; Zhang, J.; Lee, C.S. Different Strategies for Organic Nanoparticle Preparation in Biomedicine. ACS Mater. Lett. 2020, 2, 531–549. [Google Scholar] [CrossRef]
- Vargas-Nadal, G.; Köber, M.; Nsamela, A.; Terenziani, F.; Sissa, C.; Pescina, S.; Sonvico, F.; Gazzali, A.M.; Wahab, H.A.; Grisanti, L.; et al. Fluorescent Multifunctional Organic Nanoparticles for Drug Delivery and Bioimaging: A Tutorial Review. Pharmaceutics 2022, 14, 2498. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Zhang, W.; Liu, S.; Hu, X.; Xie, Z. Mitochondria-Targeting Organic Nanoparticles for Enhanced Photodynamic/Photothermal Therapy. ACS Appl. Mater. Interfaces 2020, 12, 30077–30084. [Google Scholar] [CrossRef] [PubMed]
- Montaseri, H.; Kruger, C.A.; Abrahamse, H. Review: Organic nanoparticle based active targeting for photodynamic therapy treatment of breast cancer cells. Oncotarget 2020, 11, 2120. [Google Scholar] [CrossRef]
- Shang, L.; Zhou, X.; Zhang, J.; Shi, Y.; Zhong, L. Metal nanoparticles for photodynamic therapy: A potential treatment for breast cancer. Molecules 2021, 26, 6532. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Yim, W.; Zhou, J.; Zhou, J.; Jin, Z.; Moore, C.; Borum, R.; Jorns, A.; Jokerst, J.V. The Application of Organic Nanomaterials for Bioimaging, Drug Delivery, and Therapy: Spanning Various Domains. IEEE Nanotechnol. Mag. 2021, 15, 8–28. [Google Scholar] [CrossRef]
- Hu, Q.; He, C.; Lu, Z.; He, Y.; Xie, H.; Li, J.; Fu, Z.; Guo, B. Engineering of small molecular organic nanoparticles for mitochondria-targeted mild photothermal therapy of malignant breast cancers. Biomater. Sci. 2022, 10, 6013–6023. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Feng, W.; Chen, Y.; Shi, J. Inorganic nanoparticles in clinical trials and translations. Nano Today 2020, 35, 100972. [Google Scholar] [CrossRef]
- Ojo, O.A.; Olayide, I.I.; Akalabu, M.C.; Ajiboye, B.O.; Ojo, A.B.; Oyinloye, B.E.; Ramalingam, M. Nanoparticles and their biomedical applications. Biointerface Res. Appl. Chem. 2021, 11, 8431–8445. [Google Scholar] [CrossRef]
- Liu, Q.; Kim, Y.J.; Im, G.B.; Zhu, J.; Wu, Y.; Liu, Y.; Bhang, S.H. Inorganic Nanoparticles Applied as Functional Therapeutics. Adv. Funct. Mater. 2021, 31, 2008171. [Google Scholar] [CrossRef]
- Vijayaram, S.; Tsigkou, K.; Zuorro, A.; Sun, Y.Z.; Rabetafika, H.; Razafindralambo, H. Inorganic nanoparticles for use in aquaculture. Rev. Aquac. 2023, 15, 1600–1617. [Google Scholar] [CrossRef]
- Zhang, Z.; Ahmed, A.I.S.; Malik, M.Z.; Ali, N.; Khan, A.; Ali, F.; Hassan, M.O.; Mohamed, B.A.; Zdarta, J.; Bilal, M. Cellulose/inorganic nanoparticles-based nano-biocomposite for abatement of water and wastewater pollutants. Chemosphere 2023, 313, 137483. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, X.; Shen, P.; Wang, J.; Shen, Y.; Shen, Y.; Webster, T.J.; Deng, J. Applications of inorganic nanomaterials in photothermal therapy based on combinational cancer treatment. Int. J. Nanomed. 2020, 19, 1903–1914. [Google Scholar] [CrossRef] [PubMed]
- Krishna, R.H.; Chandraprabha, M.N.; Monika, P.; Br, T.; Chaudhary, V.; Manjunatha, C. Biomolecule conjugated inorganic nanoparticles for biomedical applications: A review. Biotechnol. Genet. Eng. Rev. 2022, 1–42. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Xia, C.; Cao, J.; AL Garalleh, H.; Garaleh, M.; Khouj, M.; Pugazhendhi, A. A review on current scenario of Nanocatalysts in biofuel production and potential of organic and inorganic nanoparticles in biohydrogen production. Fuel 2023, 338, 127216. [Google Scholar] [CrossRef]
- Rizvi, M.; Gerengi, H.; Gupta, P. Functionalization of Nanomaterials: Synthesis and Characterization. In ACS Symposium Series; American Chemical Society: Washington, DC, USA, 2022; pp. 1–26. [Google Scholar]
- Abd Elrahman, A.A.; Mansour, F.R. Targeted magnetic iron oxide nanoparticles: Preparation, functionalization and biomedical application. J. Drug Deliv. Sci. Technol. 2019, 52, 702–712. [Google Scholar] [CrossRef]
- Aisida, S.O.; Akpa, P.A.; Ahmad, I.; Zhao, T.; Maaza, M.; Ezema, F.I. Bio-inspired encapsulation and functionalization of iron oxide nanoparticles for biomedical applications. Eur. Polym. J. 2020, 122, 109371. [Google Scholar] [CrossRef]
- Gambhir, R.P.; Rohiwal, S.S.; Tiwari, A.P. Multifunctional surface functionalized magnetic iron oxide nanoparticles for biomedical applications: A review. Appl. Surf. Sci. Adv. 2022, 11, 100303. [Google Scholar] [CrossRef]
- Lin, D.; Shen, L.; Luo, M.; Zhang, K.; Li, J.; Yang, Q.; Zhu, F.; Zhou, D.; Zheng, S.; Chen, Y. Circulating tumor cells: Biology and clinical significance. Signal Transduct. Target. Ther. 2021, 6, 404. [Google Scholar] [CrossRef]
- Al Mannai, A.; Al-Ansari, T.; Saoud, K.M. Quantification of Serum Exosome Biomarkers Using 3D Nanoporous Gold and Spectrophotometry. Sensors 2022, 22, 6347. [Google Scholar] [CrossRef] [PubMed]
- Farzin, A.; Etesami, S.A.; Quint, J.; Memic, A.; Tamayol, A. Magnetic nanoparticles in cancer therapy and diagnosis. Adv. Healthc. Mater. 2020, 9, 1901058. [Google Scholar] [CrossRef] [PubMed]
- Debela, D.T.; Muzazu, S.G.Y.; Heraro, K.D.; Ndalama, M.T.; Mesele, B.W.; Haile, D.C.; Kitui, S.K.; Manyazewal, T. New approaches and procedures for cancer treatment: Current perspectives. SAGE Open Med. 2021, 9, 20503121211034370. [Google Scholar] [CrossRef]
- Horvat, N.; Carlos Tavares Rocha, C.; Clemente Oliveira, B.; Petkovska, I.; Gollub, M.J. MRI of rectal cancer: Tumor staging, imaging techniques, and management. Radiographics 2019, 39, 367–387. [Google Scholar] [CrossRef] [PubMed]
- Taghipour, Y.D.; Zarebkohan, A.; Salehi, R.; Rahimi, F.; Torchilin, V.P.; Hamblin, M.R.; Seifalian, A. An update on dual targeting strategy for cancer treatment. J. Control. Release 2022, 349, 67–96. [Google Scholar] [CrossRef] [PubMed]
- Aurelia Chis, A.; Dobrea, C.; Morgovan, C.; Arseniu, A.M.; Rus, L.L.; Butuca, A.; Juncan, A.M.; Totan, M.; Vonica-Tincu, A.L.; Cormos, G.; et al. Applications and Limitations of Dendrimers in Biomedicine. Molecules 2020, 25, 3982. [Google Scholar] [CrossRef]
- Botelho, M.A.I.; Queiroz, D.B.; Barros, G.; Guerreiro, S.; Fechine, P.; Umbelino, S.; Lyra, A.; Borges, B.; Freitas, A.; de Queiroz, D.C.; et al. Nanostructured transdermal hormone replacement therapy for relieving menopausal symptoms: A confocal Raman spectroscopy study. Clinics 2014, 69, 75. [Google Scholar] [CrossRef] [PubMed]
- Rastinehad, A.R.; Anastos, H.; Wajswol, E.; Winoker, J.S.; Sfakianos, J.P.; Doppalapudi, S.K.; Carrick, M.R.; Knauer, C.J.; Taouli, B.; Lewis, S.C.; et al. Gold nanoshell-localized photothermal ablation of prostate tumors in a clinical pilot device study. Proc. Natl. Acad. Sci. USA 2019, 116, 18590–18596. [Google Scholar] [CrossRef]
- Oldenburg, S.J.; Averitt, R.D.; Westcott, S.L.; Halas, N.J. Nanoengineering of optical resonances. Chem. Phys. Lett. 1998, 288, 243–247. [Google Scholar] [CrossRef]
- National Cancer Institute. Administration of Anti-CD19-Chimeric-Antigen-Receptor-Transduced T Cells from the Original Transplant Donor to Patients with Recurrent or Persistent B-Cell Malignancies after Allogeneic Stem Cell Transplantation; National Cancer Institute: Bethesda, MD, USA, 2010.
- Jia, C.; Guo, Y.; Wu, F.G. Chemodynamic Therapy via Fenton and Fenton-Like Nanomaterials: Strategies and Recent Advances. Small 2022, 18, 2103868. [Google Scholar] [CrossRef]
- Nguyen, C.B.; Oh, E.; Bahar, P.; Vaishampayan, U.N.; Else, T.; Alva, A.S. Novel Approaches with HIF-2α Targeted Therapies in Metastatic Renal Cell Carcinoma. Cancers 2024, 16, 601. [Google Scholar] [CrossRef] [PubMed]
- Grauer, O.; Jaber, M.; Hess, K.; Weckesser, M.; Schwindt, W.; Maring, S.; Wölfer, J.; Stummer, W. Combined intracavitary thermotherapy with iron oxide nanoparticles and radiotherapy as local treatment modality in recurrent glioblastoma patients. J. Neurooncol. 2019, 141, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Sarhadi, V.K.; Armengol, G. Molecular Biomarkers in Cancer. Biomolecules 2022, 12, 1021. [Google Scholar] [CrossRef]
- Yang, S.R.; Schultheis, A.M.; Yu, H.; Mandelker, D.; Ladanyi, M.; Büttner, R. Precision medicine in non-small cell lung cancer: Current applications and future directions. Semin. Cancer Biol. 2022, 84, 184–198. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.L.Y.; Moonshi, S.S.; Ta, H.T. Nanoceria: An innovative strategy for cancer treatment. Cell. Mol. Life Sci. 2023, 80, 46. [Google Scholar] [CrossRef] [PubMed]
- Deli, T.; Orosz, M.; Jakab, A. Hormone replacement therapy in cancer survivors–review of the literature. Pathol. Oncol. Res. 2020, 26, 63–78. [Google Scholar] [CrossRef] [PubMed]
- McMenamin, Ú.; Hicks, B.; Hughes, C.; Murchie, P.; Hippisley-Cox, J.; Ranger, T.; Coupland, C.; Cardwell, C. Hormone replacement therapy in women with cancer and risk of cancer-specific mortality and cardiovascular disease: A protocol for a cohort study from Scotland and Wales. BMC Cancer 2021, 21, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Wang, S.; Huang, P.; Wang, Z.; Chen, S.; Niu, G.; Li, W.; He, J.; Cui, D.; Lu, G.; et al. Photosensitizer-loaded gold vesicles with strong plasmonic coupling effect for imaging-guided photothermal/photodynamic therapy. ACS Nano 2013, 7, 5320–5329. [Google Scholar] [CrossRef] [PubMed]
- Zhi, D.; Yang, T.; O’Hagan, J.; Zhang, S.; Donnelly, R.F. Photothermal therapy. J. Control. Release 2020, 325, 52–71. [Google Scholar] [CrossRef]
- Panaseykin, Y.A.; Kapinus, V.N.; Filonenko, E.V.; Polkin, V.V.; Sevrukov, F.E.; Isaev, P.A.; Ivanov, S.A.; Kaprin, A.D. Photodynamic therapy treatment of oral cavity cancer in patients with comorbidities. Biomed. Photonics 2023, 11, 19–24. [Google Scholar] [CrossRef]
- Zakrzewski, W.; Dobrzyński, M.; Szymonowicz, M.; Rybak, Z. Stem cells: Past, present, and future. Stem Cell Res. Ther. 2019, 10, 68. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Liu, S.; Zhang, X.; Zhu, R.; Chen, S.; Chen, X.; Song, J.; Yang, H. An Ultrasound Activated Vesicle of Janus Au-MnO Nanoparticles for Promoted Tumor Penetration and Sono-Chemodynamic Therapy of Orthotopic Liver Cancer. Angew. Chem. 2020, 132, 1699–1705. [Google Scholar] [CrossRef]
- Yang, K.; Yu, G.; Tian, R.; Zhou, Z.; Deng, H.; Li, L.; Yang, Z.; Zhang, G.; Liu, D.; Wei, J.; et al. Oxygen-Evolving Manganese Ferrite Nanovesicles for Hypoxia-Responsive Drug Delivery and Enhanced Cancer Chemoimmunotherapy. Adv. Funct. Mater. 2021, 31, 2008078. [Google Scholar] [CrossRef]
- Targeted Therapy for Cancer—NCI. Available online: https://www.cancer.gov/about-cancer/treatment/types/targeted-therapies (accessed on 16 November 2023).
- Xie, Y.H.; Chen, Y.X.; Fang, J.Y. Comprehensive review of targeted therapy for colorectal cancer. Signal Transduct. Target. Ther. 2020, 5, 22. [Google Scholar] [CrossRef]
- Oh, D.-Y.; Bang, Y.-J. HER2-targeted therapies—A role beyond breast cancer. Nat. Rev. Clin. Oncol. 2020, 17, 33–48. [Google Scholar] [CrossRef]
- Martínez-Sáez, O.; Prat, A. Current and Future Management of HER2-Positive Metastatic Breast Cancer. JCO Oncol. Pract. 2021, 17, 594–604. [Google Scholar] [CrossRef]
- Rubia-Rodríguez, I.; Santana-Otero, A.; Spassov, S.; Tombácz, E.; Johansson, C.; De La Presa, P.; Teran, F.J.; Morales, M.D.P.; Veintemillas-Verdaguer, S.; Thanh, N.T.K.; et al. Whither Magnetic Hyperthermia? A Tentative Roadmap. Materials 2021, 14, 706. [Google Scholar] [CrossRef]
- Peiravi, M.; Eslami, H.; Ansari, M.; Zare-Zardini, H. Magnetic hyperthermia: Potentials and limitations. J. Indian Chem. Soc. 2022, 99, 100269. [Google Scholar] [CrossRef]
- Obaidat, I.; Narayanaswamy, V.; Alaabed, S.; Sangaraju, S.; Gopi, C. Principles of Magnetic Hyperthermia: A Focus on Using Multifunctional Hybrid Magnetic Nanoparticles. Magnetochemistry 2019, 5, 67. [Google Scholar] [CrossRef]
- Rajan, A.; Sahu, N.K. Review on magnetic nanoparticle-mediated hyperthermia for cancer therapy. J. Nanopart. Res. 2020, 22, 319. [Google Scholar] [CrossRef]
- Fatima, H.; Charinpanitkul, T.; Kim, K.S. Fundamentals to Apply Magnetic Nanoparticles for Hyperthermia Therapy. Nanomaterials 2021, 11, 1203. [Google Scholar] [CrossRef] [PubMed]
- Das, P.; Colombo, M.; Prosperi, D. Recent advances in magnetic fluid hyperthermia for cancer therapy. Colloids Surf. B Biointerfaces 2019, 174, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, Y.; Wang, Y.; Zhu, W.; Li, G.; Ma, X.; Zhang, Y.; Chen, S.; Tiwari, S.; Shi, K. Comprehensive understanding of magnetic hyperthermia for improving antitumor therapeutic efficacy. Theranostics 2020, 10, 3793. [Google Scholar] [CrossRef] [PubMed]


| Type of NPs/Drug/Name | Method of Synthesis | Application/s (Advantages) | Limitation/s (Disadvantages) | References |
|---|---|---|---|---|
| IONP@PMSEA | Thermal decomposition | Potential delivery agents for therapeutics and diagnostics | Reproducibility and scalability | [26,27,28] |
| Nimotuzumab | Biological combination method | Epithelial tumours, carcinoma of head and neck, nasopharyngeal cancer | Asthma, rash, hypertension, microscopic haematuria, and fluctuations in blood pressure | [29,30,31] |
| Doxorubicin (DOX) | Double emulsion, hydrolysis | Breast cancer, ovarian cancer | Cardiac effects due to heart muscle failure | [32,33] |
| Ferumoxide and gadolinium | Hydrothermal reaction | MR imaging reticuloendothelial systems and liver stem cell labelling. | Can cause side effects such as severe backache when administered as intravenous bolus | [28,33,34,35,36,37,38] |
| Ferumoxsil (AMI-121) | Hydrothermal reaction | Bowel MRI, oral GI imaging, atherosclerosis, gastrointestinal as magnetic iron particle solution | Intestinal performance obstruction, metallic taste is a hindrance to routine use | [28,39] |
| Ferumoxtran (AMI-227) | Hydrothermal reaction | Noncancerous lymphatic tissue imaging | Coated with dextran, which can induce allergic reactions | [28,40,41,42] |
| Feruglose | Hydrothermal reaction | Blood pool agent, lymph nodes, and liver spleen imaging | Interferes with iron metabolism after biodegradation | [33,43] |
| Nanoworms (NW) | Co-precipitation | Tumour targeting, COVID-19 | Manufacturing and disposal have negative impacts on the environment, potential side effects to the immune response are not fully explored | [44,45,46] |
| Resosvist (SHU555C) | Biological combination method | MRI signal intensity enhancement | Loss of signal in the healthy tissues | [47,48,49] |
| Hafnium oxide nanoparticle | Hydrothermal | Radiography, optical, sensing, oral cancer detection, biosensing, and electronic fields | Slow kinetics, low adsorption capacity, and leaching problem in low pH environments | [50,51,52,53,54,55] |
| Type of NPs | Applications | Limitations | References |
|---|---|---|---|
| Carbon-based |
|
| [132,133,134,135,136,137,138] |
| Organic |
|
| [139,140,141,142,143,144,145] |
| Inorganic |
|
| [27,146,147,148,149,150,151,152,153] |
| Studied NPs | Type of Treatment | Therapeutic Strategy | Outcome | References |
|---|---|---|---|---|
| Dendrimers | Lung cancer/ imaging diagnostics | Biomarkers testing | Lowers the dose needed to produce images, increasing radioisotope efficiency. | [164] |
| Nanostructured transdermal hormone replacement | Menopausal symptoms | Hormone therapy | Improvements in climacteric symptoms. Every woman’s result from a bilateral mammography evaluation of breasts were normal. | [165] |
| Biocompatible gold–silica nanoshells | Prostate tumours | Photothermal ablation of prostate tumours | Effective GSN-mediated laser ablation, no significant changes in comparison to the “International Prostate Symptom Score or the Sexual Health Inventory for Men”. | [166,167] |
| Anti-CD19-Chimeric-Antigen-Receptor-Transduced T-Cells | B-Cell Malignancies | Stem cell transplant | Study is ongoing and is in follow-up stage currently. NCT01087294 | [168] |
| Dihydroartemisinin-loaded magnetic nanoparticles | Breast cancer cells | Chemodynamic therapy | Proves to be more efficient and cost friendly, although more evaluations need to be conducted. | [169] |
| Belzutifan | Brain cancer | Targeted therapy | Only currently approved inhibitor, with more evaluation research ongoing. | [170] |
| Superparamagnetic iron oxide NPs | Glioblastomas (GBMs) | Magnetic hyperthermia | Long-term stabilization achieved for phase-I trial stage. | [171] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ndlovu, N.L.; Mdlalose, W.B.; Ntsendwana, B.; Moyo, T. Evaluation of Advanced Nanomaterials for Cancer Diagnosis and Treatment. Pharmaceutics 2024, 16, 473. https://doi.org/10.3390/pharmaceutics16040473
Ndlovu NL, Mdlalose WB, Ntsendwana B, Moyo T. Evaluation of Advanced Nanomaterials for Cancer Diagnosis and Treatment. Pharmaceutics. 2024; 16(4):473. https://doi.org/10.3390/pharmaceutics16040473
Chicago/Turabian StyleNdlovu, Nkanyiso L., Wendy B. Mdlalose, Bulelwa Ntsendwana, and Thomas Moyo. 2024. "Evaluation of Advanced Nanomaterials for Cancer Diagnosis and Treatment" Pharmaceutics 16, no. 4: 473. https://doi.org/10.3390/pharmaceutics16040473
APA StyleNdlovu, N. L., Mdlalose, W. B., Ntsendwana, B., & Moyo, T. (2024). Evaluation of Advanced Nanomaterials for Cancer Diagnosis and Treatment. Pharmaceutics, 16(4), 473. https://doi.org/10.3390/pharmaceutics16040473







