Development and Characterization of New Miconazole-Based Microemulsions for Buccal Delivery by Implementing a Full Factorial Design Modeling
Abstract
1. Introduction
| Year | Pharmaceutical Formulation | API Content | Excipients | Observation | Ref. |
|---|---|---|---|---|---|
| 1992 | Bioadhesive slow-release buccal tablet | 10 mg | Modified starch, Carbopol 934 Sodium benzoate, SiO2 | The tablet formulation exhibited a pronounced antifungal effect at a lower dose compared to commercial gel. | [54] |
| 2003 | Mucoadhesive buccal patches | 2% | 1 SCMC, Chitosan, 2 PVA, 3 HEC, 4 HPMC ± 5 PVP (0–5%) | Patches had more accurate dosing than the gel form, and the formulation based on PVA 10% and PVP 5% had the best 6 MIC release. | [55] |
| 2017 | Buccal mucoadhesive films based on polyelectrolyte complexes | 2% | Chitosan combined with pectin or HPMC | HPMC increased adhesion and improved the mechanical properties of the chitosan-based films. Improved drug release. | [56] |
| 2017 | Buccal mucoadhesive films based on polyelectrolyte complexes | 2% | Chitosan + Carbopol, Arabic gum, gelatin, or alginate; 7 PEG 400 (30%) used as solubilizer and plasticizer | Chitosan increases antifungal activity of miconazole. Gelatin and Carbopol were appropriate polymers to form chitosan films. | [57] |
| 2017 | Mucoadhesive lipid nanogels | 0.25–1% | Phospholipon 90 H, Polysorbate 80, beeswax, Polycarbophil, sorbitol | Nanogels with SLN improved the antifungal activity of MIC compared to commercial gel. | [37] |
| 2018 | Composite microparticle-based discs | 200 mg | Chitosan, gelatin and HPMC | The combination of chitosan-gelatin protects MIC and determines a controlled release. Therapeutic activity can be better improved. | [35] |
| 2018 | Buccal films | 8% | Chitosan and three types of carrageenan (κ, λ, ι), and PEG 400 as a solubilizer and plasticizer | λ-carrageenan (λ-c) was suitable combined with chitosan. The orientation of sulfate groups in λ-c influenced the interactions with chitosan, but also those with mucin and salivary medium. | [23] |
| 2019 | Hydrogels loaded with self-nanoemulsifying drug delivery systems | 250 mg | 8 HA 2%, crosslinked with Gantrez S-97 0.5% which was treated with a NE containing MIC, and clove oil 10–25%, Labrasol 18–70%, and 9 PG 10–30% | Labrasol and PG, used as surfactants and cosurfactants in nanoemulsion preparation, determined a high residence of MIC at the mucosal area, enhancing drug permeation. Hydrogel-loaded NE enhanced miconazole release and its contact with the oral mucosa. | [39] |
| 2022 | Oral gels | 2% | Carbopol 940 and sodium hydroxide, glycerol as a plasticizer, and adjuvants | The optimal gel contained Carbopol 0.84% and sodium hydroxide 0.32%. Miconazole can be prepared in a gel base, influencing texture, spreadability, viscosity and adequate antifungal activity. | [18] |
| 2023 | Mucoadhesive nanoparticulate lipospheres | 0.25%, 0.5%, 1% | Bos indicus fat, Phospholipon 90 H, Tween 80, sorbitol, Polycarbophil | The gel base sustained the delivery of the nanoparticles to the oral mucosa. The nanoparticles’ high surface area increased the contact with the mucosa, while the hydrogel matrix improved mucoadhesion and controlled release. | [38] |
2. Materials and Methods
2.1. Materials
2.2. Solubility Studies for Miconazole
2.3. Screening Study to Design Pseudo-Ternary Phase Diagrams
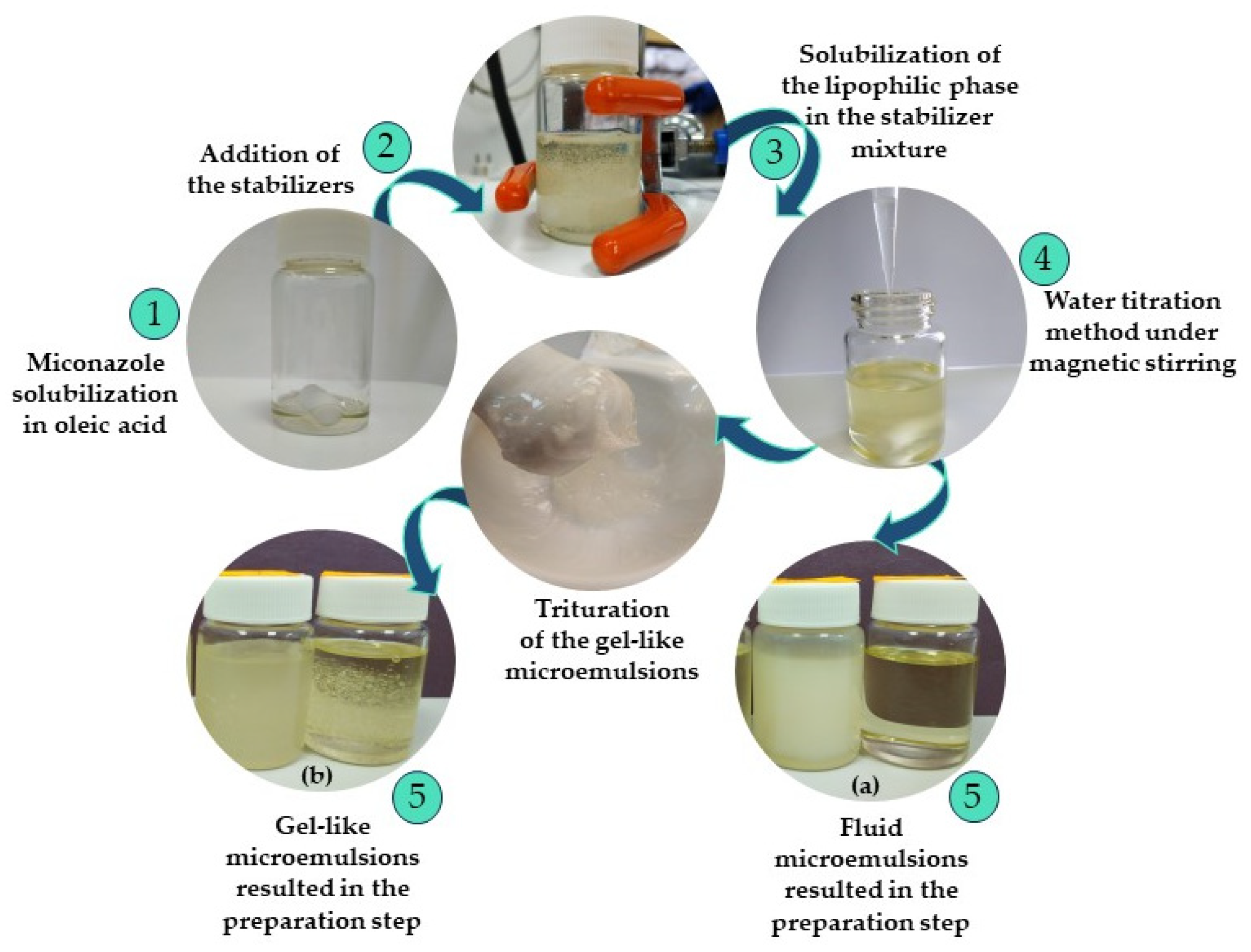
2.4. Preparation of the O/W Miconazole-Based Microemulsions Using a 23 Full Factorial Plan
2.5. Organoleptic Analysis
2.6. pH Determination
2.7. Conductivity Determination
2.8. Refractive Index Determination
2.9. Dynamic Light Scattering Determination
2.10. Zeta Potential Analysis
2.11. Rheological Evaluation
2.12. Superficial Analysis
2.13. In Vitro Release Studies
2.14. Data Analysis and Screening of the Miconazole Microemulsions Using 23 Full Factorial Design
3. Results and Discussion
3.1. Solubility Studies
3.2. Screening Study to Design Pseudo-Ternary Phase Diagrams
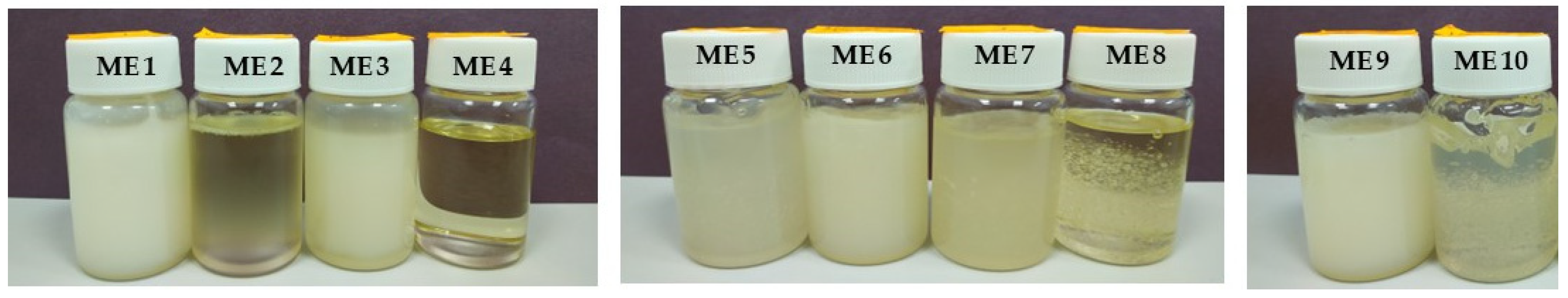
3.3. Formulation Design and Organoleptic Analysis
3.4. pH Determination
3.5. Conductivity Determination
3.6. Refractive Index Determination
3.7. Rheological Evaluation
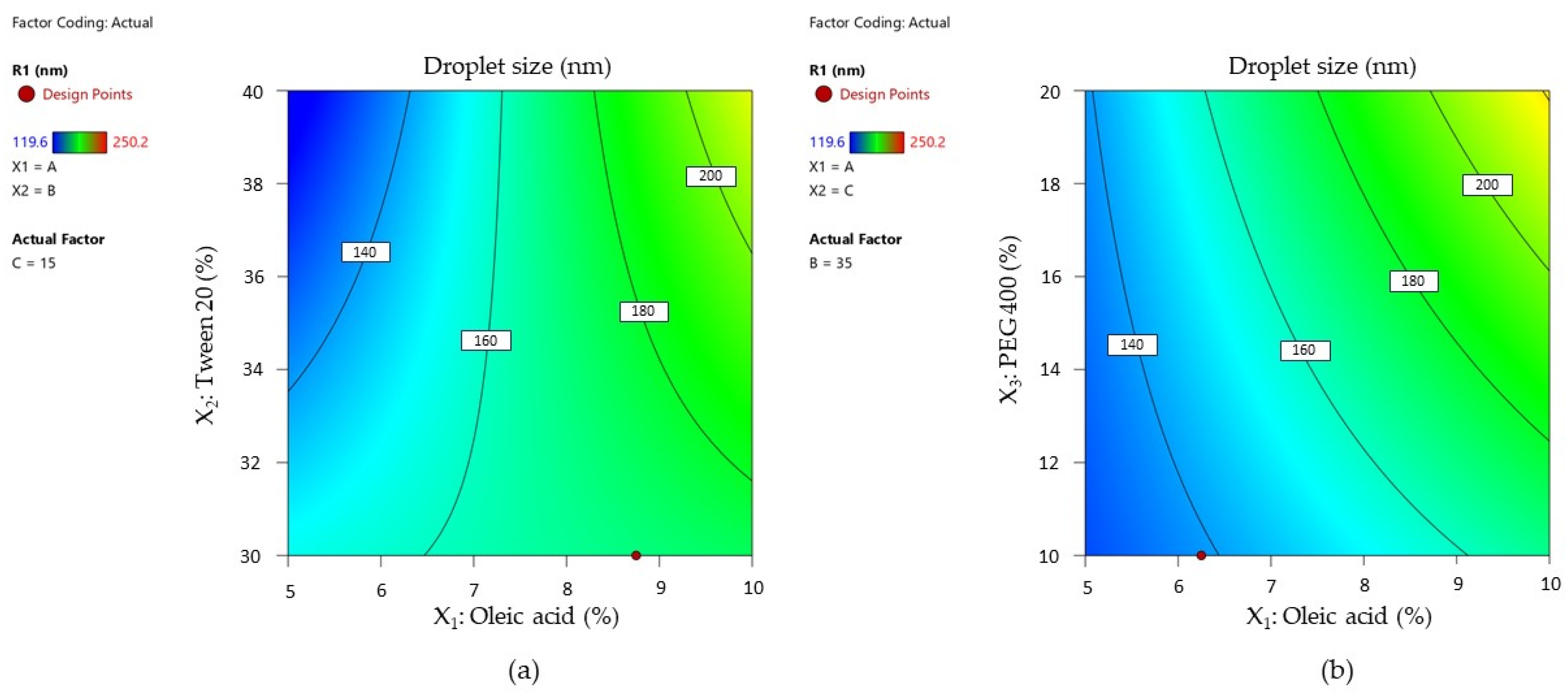
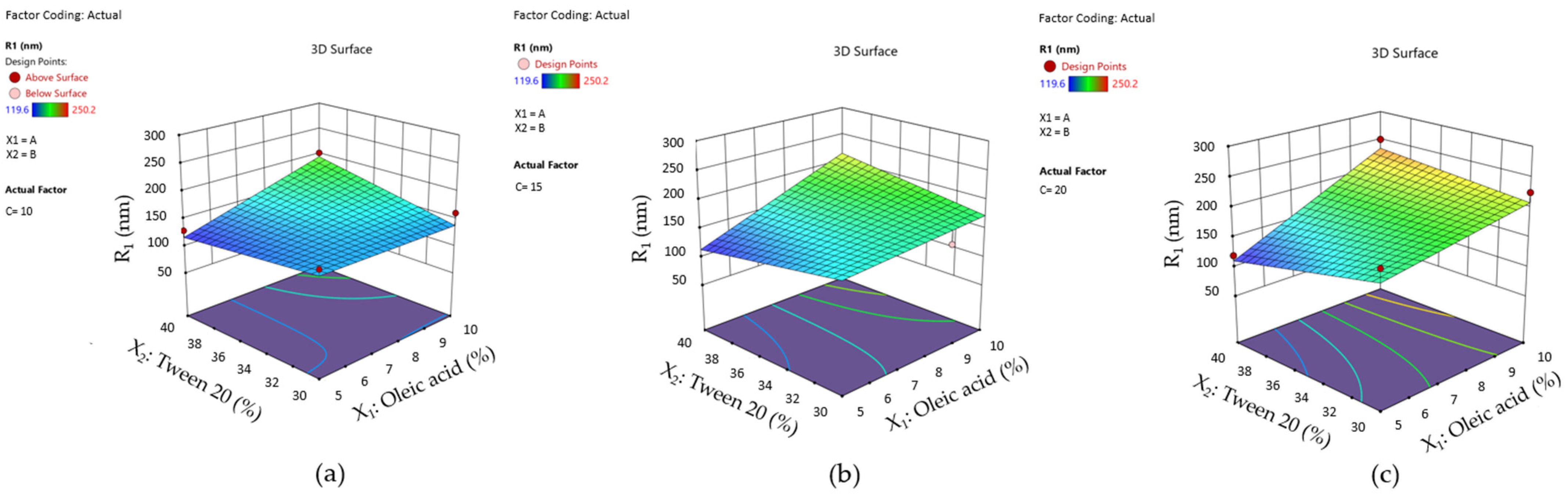
3.8. Dynamic Light Scattering Analysis
- An increase of Tween 20 content from 30% to 40% determined a decrease in Ds from 152.89 nm to 128.90 nm in the case of the ME 1–ME 2 pair and from 188.33 nm to 119.60 nm in the case of the ME 3–ME4 pair; an additive effect of PEG 400 was observed in the ME 2–ME 4 pair where Ds decreased from 128.90 nm to 119.60 nm.
- At the minimum concentration of Tween 20 of 30%, the increase of PEG 400 determined an increase in droplet size, as can be observed in the case of the ME 1–ME 3 pair, acting oppositely as it was proposed in the mathematical modeling of the Ds response.
- An increase of Tween 20 from 30% to 40% determined an increase of Ds from 161.34 nm to 202.29 nm in the case of ME 5–ME 6 pair, but also from 225.13 nm to 250.20 nm for ME 7–ME 8 pair.
- When Tween 20 is maintained as constant, PEG 400 variation from 10% to 20% promoted growth in droplet size, and it can be very well emphasized in the case of the ME 5–ME 7 pair and ME 6–ME 8 pair, where the maximum droplet size of 250.20 nm was attributed for ME 8.
3.9. Zeta Potential Analysis
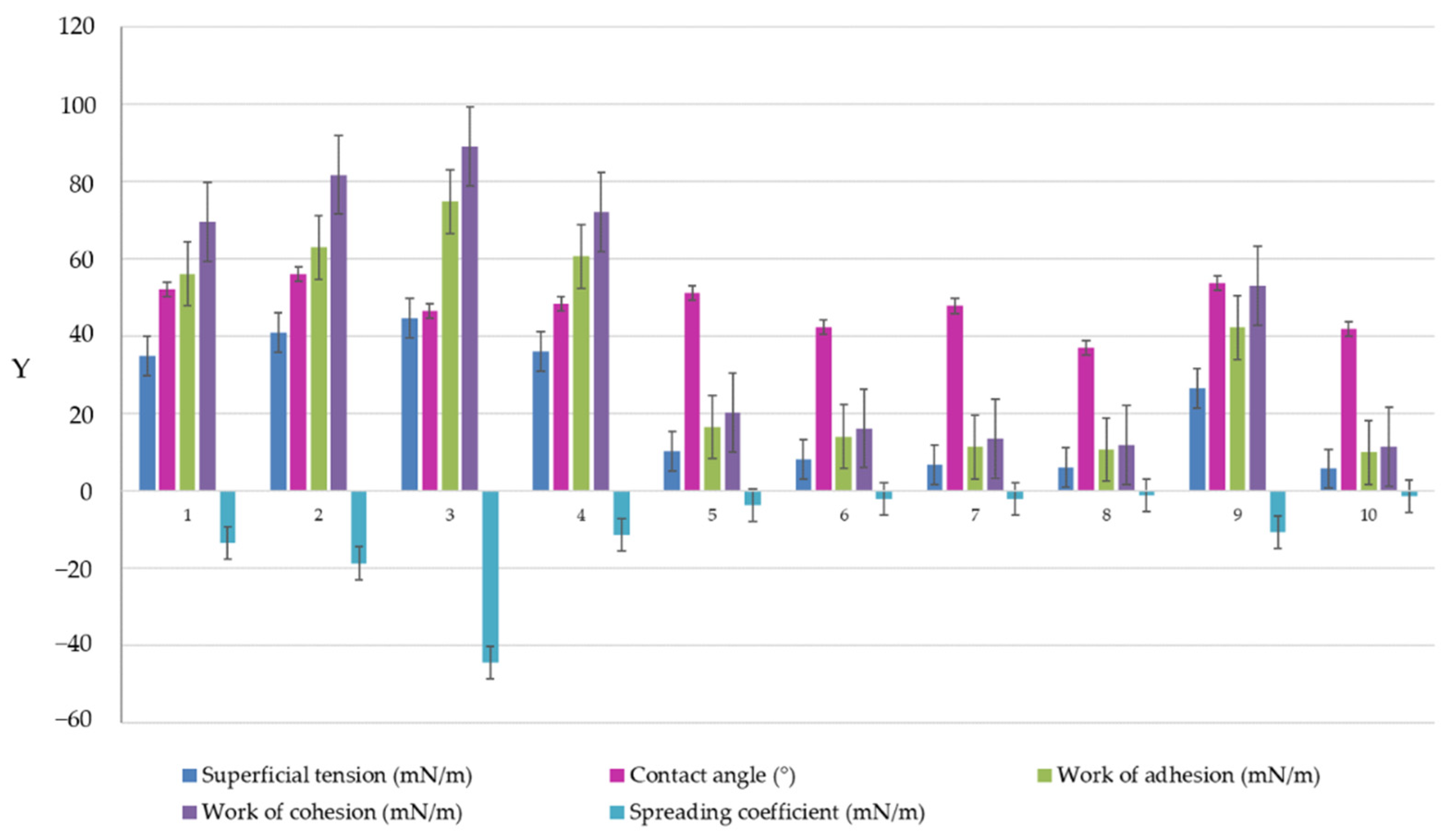
3.10. Superficial Analysis
3.11. In Vitro Drug Release
3.12. Statistical Analysis for the Miconazole Microemulsions Using 23 Full Factorial Design
3.12.1. Statistical Interpretation for Mean Droplet Size
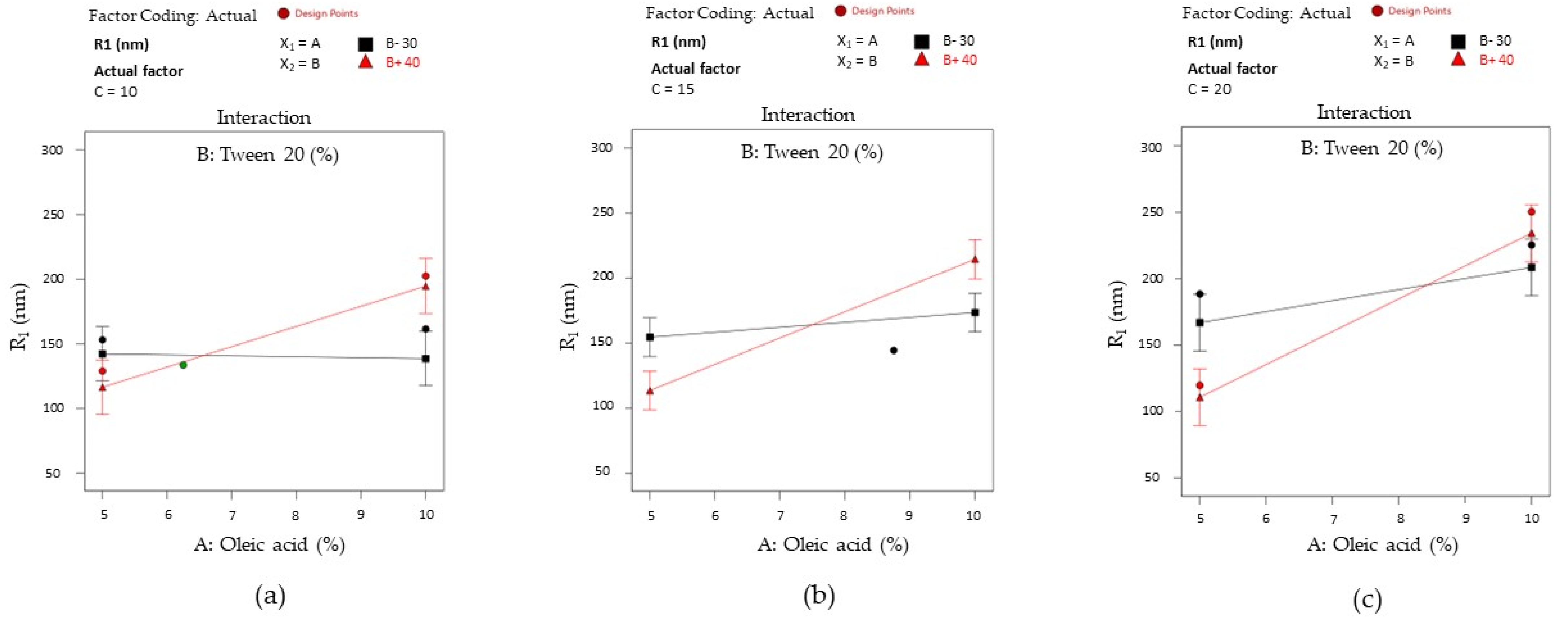
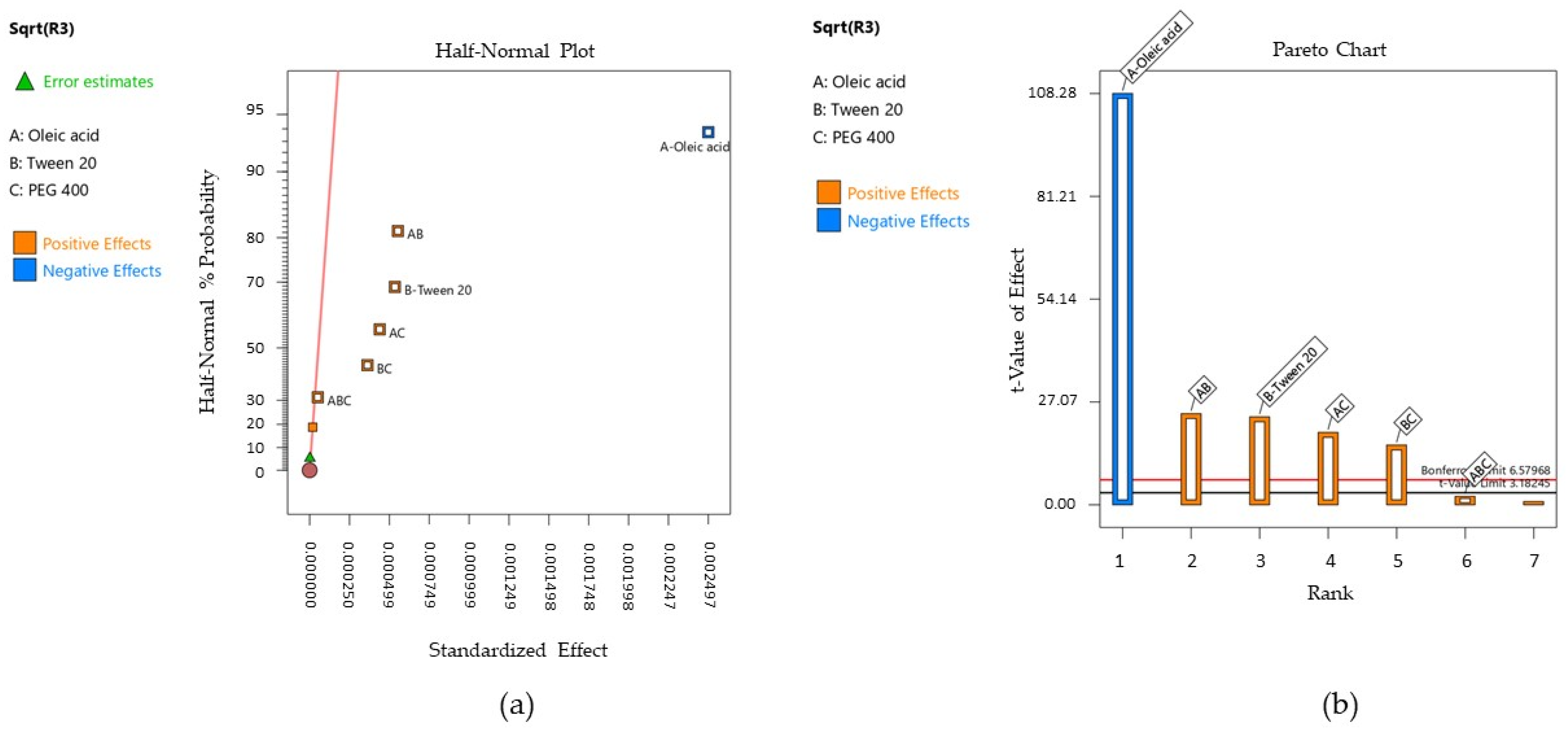
3.12.2. Statistical Interpretation for Work of Adhesion
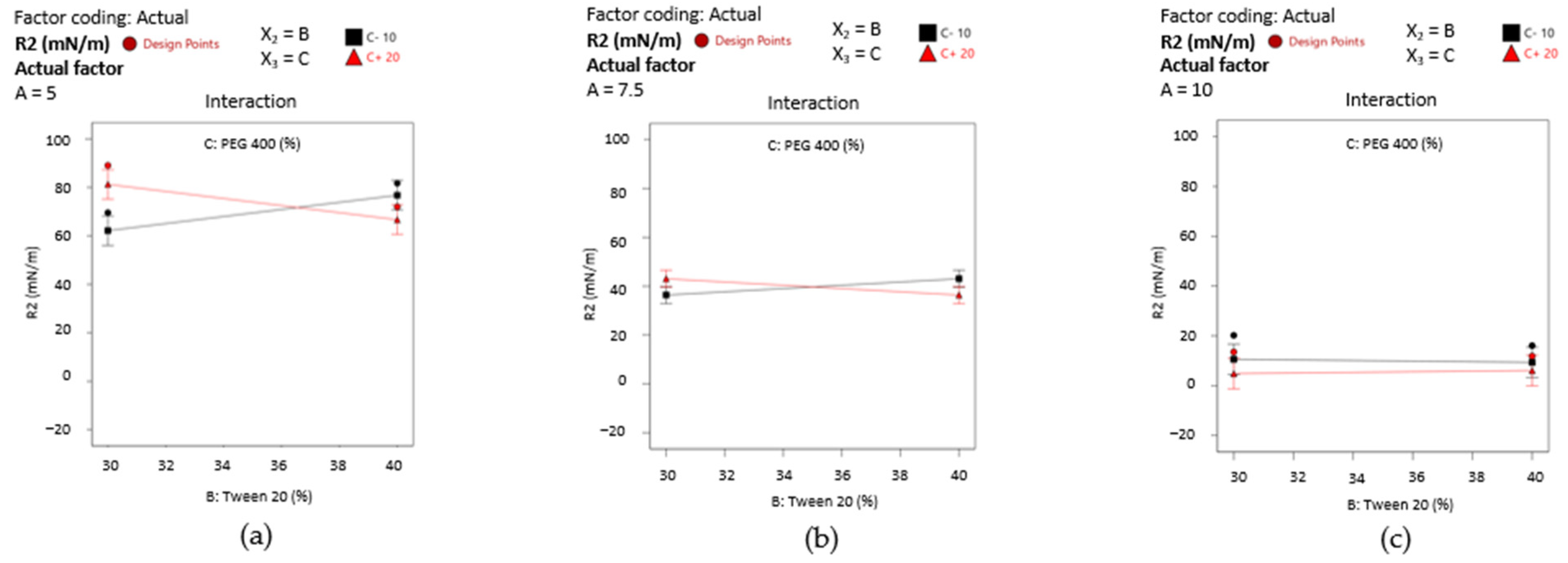
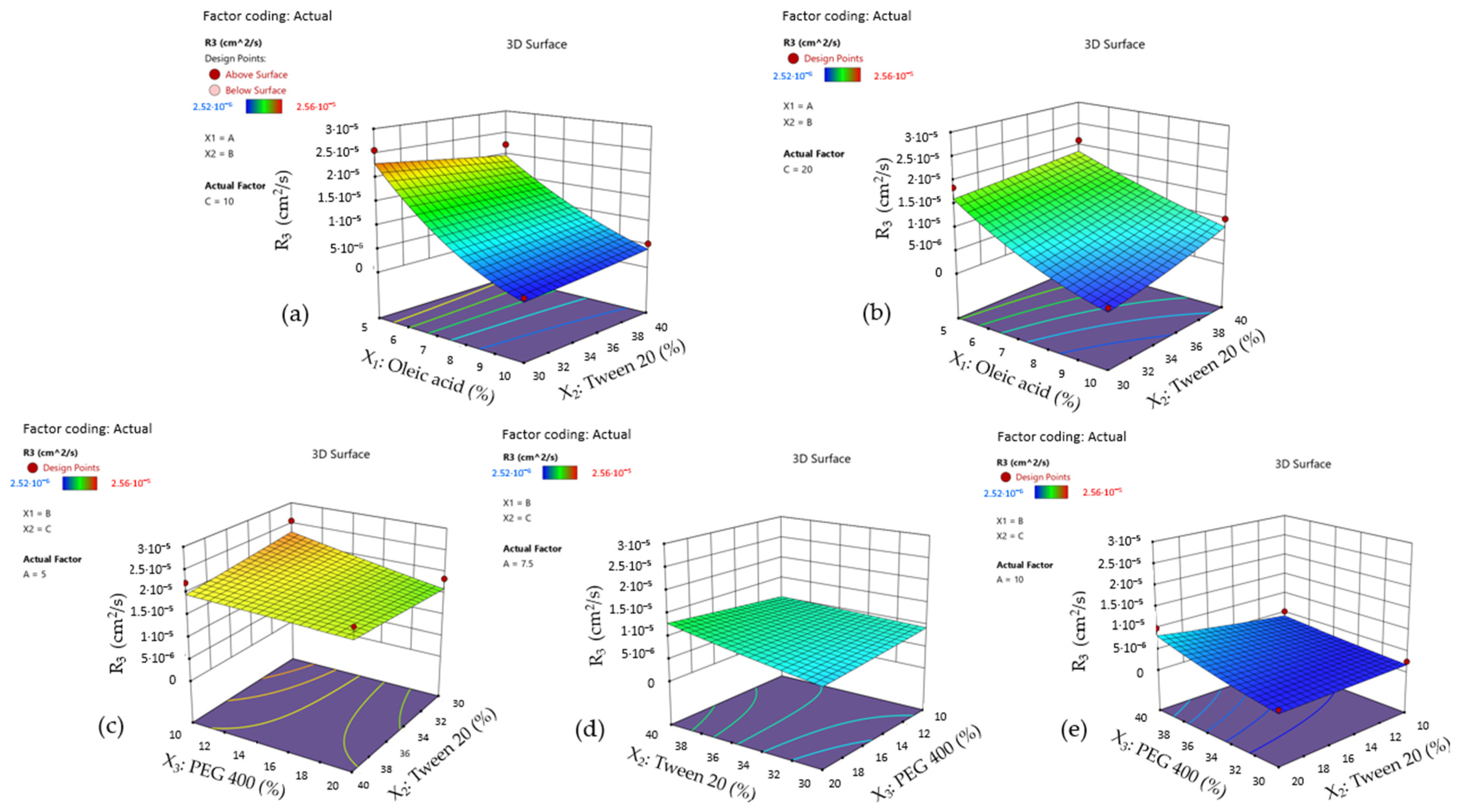
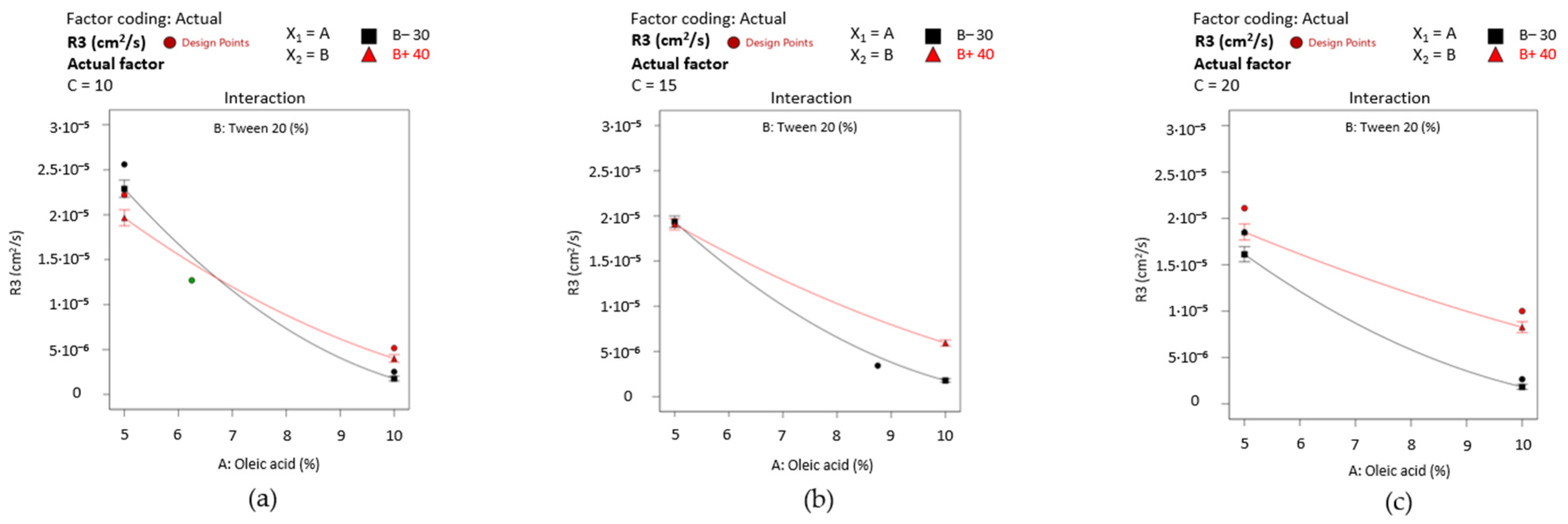
3.12.3. Statistical Interpretation for Diffusion Coefficient of Miconazole
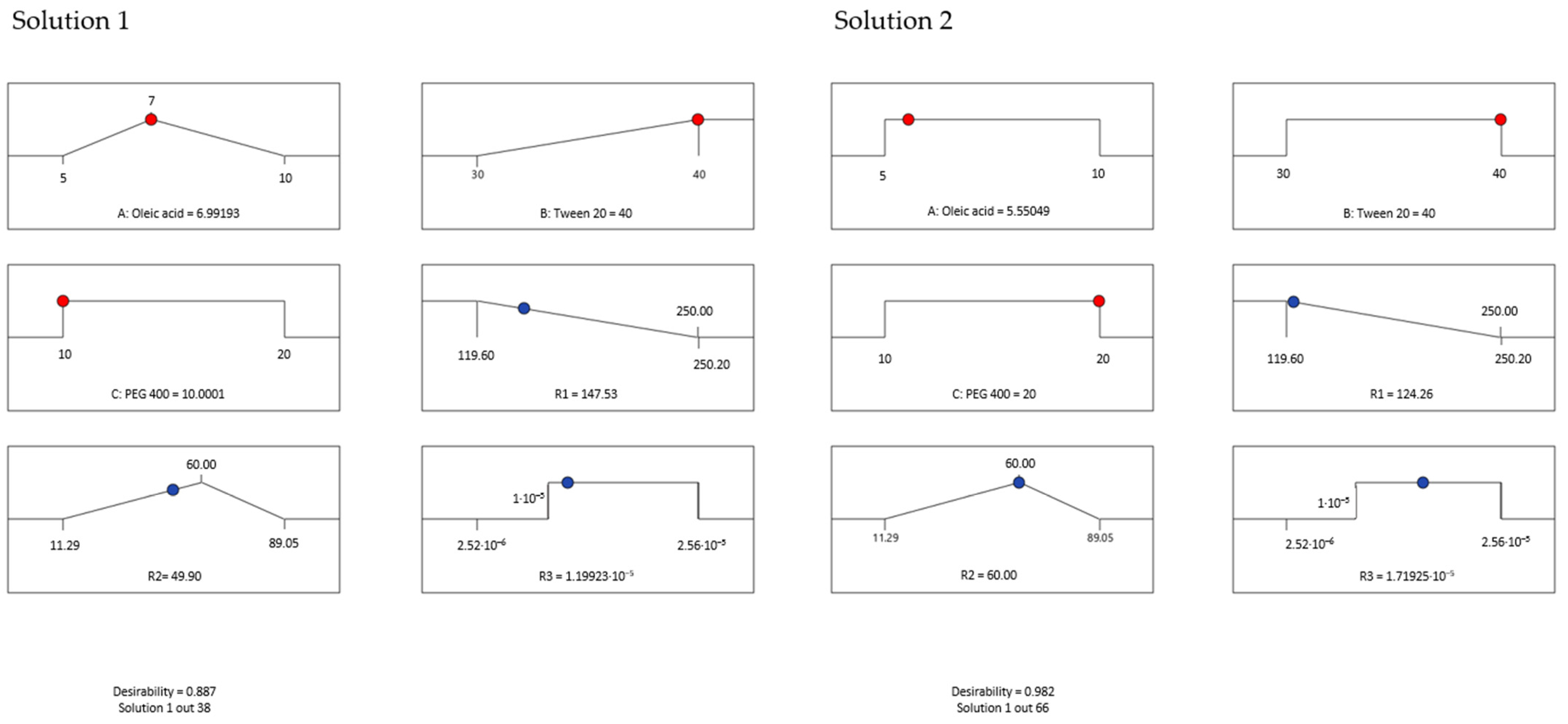
3.12.4. Optimization of Miconazole-Based Microemulsions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vila, T.; Sultan, A.S.; Montelongo-Jauregui, D.; Jabra-Rizk, M.A. Oral Candidiasis: A Disease of Opportunity. J. Fungi 2020, 6, 15. [Google Scholar] [CrossRef]
- Lu, S.-Y. Oral Candidosis: Pathophysiology and Best Practice for Diagnosis, Classification, and Successful Management. J. Fungi 2021, 7, 555. [Google Scholar] [CrossRef] [PubMed]
- Molek, M.; Florenly, F.; Lister, I.N.E.; Wahab, T.A.; Lister, C.; Fioni, F. Xerostomia and Hyposalivation in Association with Oral Candidiasis: A Systematic Review and Meta-Analysis. Evid. Based Dent. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Orrio-Soler, I.; Arias de Luxán, S.; Sheth, C.C. Oral Colonization by Candida Species in Orthodontic Patients before, during and after Treatment with Fixed Appliances: A Prospective Controlled Trial. J. Clin. Exp. Dent. 2020, 12, e1071–e1077. [Google Scholar] [CrossRef] [PubMed]
- Erdoğan, T.; Karakaya, G.; Kalyoncu, A.F. The Frequency and Risk Factors for Oropharyngeal Candidiasis in Adult Asthma Patients Using Inhaled Corticosteroids. Turk. Thorac. J. 2019, 20, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Anuța, V.; Talianu, M.-T.; Dinu-Pîrvu, C.-E.; Ghica, M.V.; Prisada, R.M.; Albu Kaya, M.G.; Popa, L. Molecular Mapping of Antifungal Mechanisms Accessing Biomaterials and New Agents to Target Oral Candidiasis. Int. J. Mol. Sci. 2022, 23, 7520. [Google Scholar] [CrossRef] [PubMed]
- Worthington, H.V.; Clarkson, J.E.; Khalid, T.; Meyer, S.; McCabe, M. Interventions for Treating Oral Candidiasis for Patients with Cancer Receiving Treatment. Cochrane Database Syst. Rev. 2010, 2010, CD001972. [Google Scholar] [CrossRef] [PubMed]
- Mardani, M.; Abolghasemi, S.; Darvishnia, D.; Lotfali, E.; Ghasemi, R.; Rabiei, M.; Fattahi, M. Oral Candidiasis in Hematological Malignancy Patients: Identification and Antifungal Susceptibility Patterns of Isolates. Jundishapur J. Microbiol. 2020, 13, e103290. [Google Scholar] [CrossRef]
- Wanasathop, A.; Patel, P.B.; Choi, H.A.; Li, S.K. Permeability of Buccal Mucosa. Pharmaceutics 2021, 13, 1814. [Google Scholar] [CrossRef]
- Barua, S.; Kim, H.; Jo, K.; Seo, C.W.; Park, T.J.; Lee, K.B.; Yun, G.; Oh, K.; Lee, J. Drug Delivery Techniques for Buccal Route: Formulation Strategies and Recent Advances in Dosage Form Design. J. Pharm. Investig. 2016, 46, 593–613. [Google Scholar] [CrossRef]
- Colombo, P.; Cagnani, S.; Sonvico, F.; Santi, P.; Russo, P.; Colombo, G. 5.12—Biological In Vitro Models for Absorption by Nonoral Routes. In Comprehensive Medicinal Chemistry II; Taylor, J.B., Triggle, D.J., Eds.; Elsevier: Oxford, UK, 2007; Volume 5, pp. 279–299. ISBN 978-0-08-045044-5. [Google Scholar] [CrossRef]
- Chachlioutaki, K.; Iordanopoulou, A.; Bouropoulos, N.; Meikopoulos, T.; Gika, H.; Ritzoulis, C.; Andreadis, D.; Karavasili, C.; Fatouros, D.G. Pediatric and Geriatric-Friendly Buccal Foams: Enhancing Omeprazole Delivery for Patients Encountering Swallowing Difficulties. J. Pharm. Sci. 2023, 112, 2644–2654. [Google Scholar] [CrossRef]
- Guo, Y.; Pratap Singh, A. Emerging Strategies for Enhancing Buccal and Sublingual Administration of Nutraceuticals and Pharamaceuticals. J. Drug Deliv. Sci. Technol. 2019, 52, 440–451. [Google Scholar] [CrossRef]
- Chinna Reddy, P.; Chaitanya, K.S.C.; Madhusudan Rao, Y. A Review on Bioadhesive Buccal Drug Delivery Systems: Current Status of Formulation and Evaluation Methods. Daru 2011, 19, 385–403. [Google Scholar] [PubMed]
- Cirillo, S.; Giacomotti, M.M.; Leggieri, A.; Bordino, F.; Chirio, D.; Gallarate, M. TCH-009 Development of a Stable Nystatin Oral Suspension to Overcome Shortages of the Commercial Medicine. Eur. J. Hosp. Pharm. 2013, 20, A72. [Google Scholar] [CrossRef][Green Version]
- Ardizzoni, A.; Boaretto, G.; Pericolini, E.; Pinetti, D.; Capezzone de Joannon, A.; Durando, L.; Ragni, L.; Blasi, E. Effects of Benzydamine and Mouthwashes Containing Benzydamine on Candida Albicans Adhesion, Biofilm Formation, Regrowth, and Persistence. Clin. Oral Investig. 2022, 26, 3613–3625. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, A.; Rimal, J.; Rao, A.; Sequeira, P.S.; Doshi, D.; Bhat, G.K. In Vitro Antifungal Effect of Mouth Rinses Containing Chlorhexidine and Thymol. J. Dent. Sci. 2011, 6, 1–5. [Google Scholar] [CrossRef]
- Pintea, A.; Vlad, R.-A.; Antonoaea, P.; Rédai, E.M.; Todoran, N.; Barabás, E.-C.; Ciurba, A. Structural Characterization and Optimization of a Miconazole Oral Gel. Polymers 2022, 14, 5011. [Google Scholar] [CrossRef] [PubMed]
- Lertsuphotvanit, N.; Tuntarawongsa, S.; Jitrangsri, K.; Phaechamud, T. Clotrimazole-Loaded Borneol-Based In Situ Forming Gel as Oral Sprays for Oropharyngeal Candidiasis Therapy. Gels 2023, 9, 412. [Google Scholar] [CrossRef]
- Czerninski, R.; Pikovsky, A.; Gati, I.; Friedman, M.; Steinberg, D. Comparison of the Efficacy of a Novel Sustained Release Clotrimazole Varnish and Clotrimazole Troches for the Treatment of Oral Candidiasis. Clin. Oral Investig. 2015, 19, 467–473. [Google Scholar] [CrossRef]
- Lalla, R.V.; Bensadoun, R.-J. Miconazole Mucoadhesive Tablet for Oropharyngeal Candidiasis. Expert Rev. Anti Infect. Ther. 2011, 9, 13–17. [Google Scholar] [CrossRef]
- Serra, E.; Saubade, F.; Ligorio, C.; Whitehead, K.; Sloan, A.; Williams, D.W.; Hidalgo-Bastida, A.; Verran, J.; Malic, S. Methylcellulose Hydrogel with Melissa Officinalis Essential Oil as a Potential Treatment for Oral Candidiasis. Microorganisms 2020, 8, 215. [Google Scholar] [CrossRef] [PubMed]
- Tejada, G.; Lamas, M.C.; Svetaz, L.; Salomón, C.J.; Alvarez, V.A.; Leonardi, D. Effect of Drug Incorporation Technique and Polymer Combination on the Performance of Biopolymeric Antifungal Buccal Films. Int. J. Pharm. 2018, 548, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Mady, O.Y.; Donia, A.M.; Al-Madboly, L.A. Miconazole-Urea in a Buccal Film as a New Trend for Treatment of Resistant Mouth Fungal White Patches. Front. Microbiol. 2018, 9, 837. [Google Scholar] [CrossRef] [PubMed]
- Makvandi, P.; Josic, U.; Delfi, M.; Pinelli, F.; Jahed, V.; Kaya, E.; Ashrafizadeh, M.; Zarepour, A.; Rossi, F.; Zarrabi, A.; et al. Drug Delivery (Nano)Platforms for Oral and Dental Applications: Tissue Regeneration, Infection Control, and Cancer Management. Adv. Sci. 2021, 8, 2004014. [Google Scholar] [CrossRef] [PubMed]
- Zambom, C.R.; da Fonseca, F.H.; Crusca, E.J.; da Silva, P.B.; Pavan, F.R.; Chorilli, M.; Garrido, S.S. A Novel Antifungal System With Potential for Prolonged Delivery of Histatin 5 to Limit Growth of Candida albicans. Front. Microbiol. 2019, 10, 1667. [Google Scholar] [CrossRef] [PubMed]
- Sutar, Y.; Nabeela, S.; Singh, S.; Alqarihi, A.; Solis, N.; Ghebremariam, T.; Filler, S.; Ibrahim, A.S.; Date, A.; Uppuluri, P. Niclosamide-Loaded Nanoparticles Disrupt Candida Biofilms and Protect Mice from Mucosal Candidiasis. PLoS Biol. 2022, 20, e3001762. [Google Scholar] [CrossRef] [PubMed]
- Monton, C.; Settharaksa, S.; Suksaeree, J.; Chusut, T. The Preparation, Characterization, and Stability Evaluation of a Microemulsion-Based Oral Spray Containing Clove Oil for the Treatment of Oral Candidiasis. J. Drug Deliv. Sci. Technol. 2020, 57, 101735. [Google Scholar] [CrossRef]
- Sindi, A.M.; Rizg, W.Y.; Khan, M.K.; Alkhalidi, H.M.; Alharbi, W.S.; Sabei, F.Y.; Alfayez, E.; Alkharobi, H.; Korayem, M.; Majrashi, M.; et al. Tailoring and Optimization of a Honey-Based Nanoemulgel Loaded with an Itraconazole-Thyme Oil Nanoemulsion for Oral Candidiasis. Drug Deliv. 2023, 30, 2173337. [Google Scholar] [CrossRef]
- Mali, K.; Dhawale, S.; Dias, R. Microemulsion Based Bioadhesive Gel of Itraconazole Using Tamarind Gum: In-Vitro and Ex-Vivo Evaluation. Marmara Pharm. J. 2017, 21, 688–700. [Google Scholar] [CrossRef]
- Zhang, L.-W.; Fu, J.-Y.; Hua, H.; Yan, Z.-M. Efficacy and Safety of Miconazole for Oral Candidiasis: A Systematic Review and Meta-Analysis. Oral Dis. 2016, 22, 185–195. [Google Scholar] [CrossRef]
- Kim, B.-Y.; Son, Y.; Cho, H.; Lee, D.; Eo, S.-K.; Kim, K. Miconazole Suppresses 27-Hydroxycholesterol-Induced Inflammation by Regulating Activation of Monocytic Cells to a Proinflammatory Phenotype. Front. Pharmacol. 2021, 12, 691019. [Google Scholar] [CrossRef]
- Wu, C.Z.; Gao, M.J.; Shen, L.; Li, B.H.; Bai, X.J.; Gui, J.H.; Li, H.M.; Huo, Q.; Ma, T. Miconazole Triggers Various Forms of Cell Death in Human Breast Cancer MDA-MB-231 Cells. Pharmazie 2019, 74, 290–294. [Google Scholar] [CrossRef]
- Yoon, S.-H.; Kim, B.-K.; Kang, M.-J.; Im, J.-Y.; Won, M. Miconazole Inhibits Signal Transducer and Activator of Transcription 3 Signaling by Preventing Its Interaction with DNA Damage-Induced Apoptosis Suppressor. Cancer Sci. 2020, 111, 2499–2507. [Google Scholar] [CrossRef]
- Tejada, G.; Lamas, M.C.; Sortino, M.; Alvarez, V.A.; Leonardi, D. Composite Microparticles Based on Natural Mucoadhesive Polymers with Promising Structural Properties to Protect and Improve the Antifungal Activity of Miconazole Nitrate. AAPS PharmSciTech 2018, 19, 3712–3722. [Google Scholar] [CrossRef]
- Lefnaoui, S.; Moulai-Mostefa, N. Investigation and Optimization of Formulation Factors of a Hydrogel Network Based on Kappa Carrageenan-Pregelatinized Starch Blend Using an Experimental Design. Colloids Surf. A Physicochem. Eng. Asp. 2014, 458, 117–125. [Google Scholar] [CrossRef]
- Kenechukwu, F.C.; Attama, A.A.; Ibezim, E.C.; Nnamani, P.O.; Umeyor, C.E.; Uronnachi, E.M.; Momoh, M.A.; Akpa, P.A. Tailor-Made Mucoadhesive Lipid Nanogel Improves Oromucosal Antimycotic Activity of Encapsulated Miconazole Nitrate. Eur. J. Nanomed. 2017, 9, 115–126. [Google Scholar] [CrossRef]
- Kenechukwu, F.C.; Kalu, C.F.; Momoh, M.A.; Onah, I.A.; Attama, A.A.; Okore, V.C. Novel Bos Indicus Fat-Based Nanoparticulate Lipospheres of Miconazole Nitrate as Enhanced Mucoadhesive Therapy for Oral Candidiasis. Biointerface Res. Appl. Chem. 2023, 13, 24. [Google Scholar] [CrossRef]
- Hosny, K.M.; Aldawsari, H.M.; Bahmdan, R.H.; Sindi, A.M.; Kurakula, M.; Alrobaian, M.M.; Aldryhim, A.Y.; Alkhalidi, H.M.; Bahmdan, H.H.; Khallaf, R.A.; et al. Preparation, Optimization, and Evaluation of Hyaluronic Acid-Based Hydrogel Loaded with Miconazole Self-Nanoemulsion for the Treatment of Oral Thrush. AAPS PharmSciTech 2019, 20, 297. [Google Scholar] [CrossRef] [PubMed]
- Montes de Oca-Ávalos, J.M.; Candal, R.J.; Herrera, M.L. Nanoemulsions: Stability and Physical Properties. Curr. Opin. Food Sci. 2017, 16, 1–6. [Google Scholar] [CrossRef]
- Gupta, A. Chapter 21—Nanoemulsions. In Nanoparticles for Biomedical Applications; Chung, E.J., Leon, L., Rinaldi, C., Eds.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 371–384. ISBN 978-0-12-816662-8. [Google Scholar] [CrossRef]
- Miastkowska, M.; Kulawik-Pióro, A.; Szczurek, M. Nanoemulsion Gel Formulation Optimization for Burn Wounds: Analysis of Rheological and Sensory Properties. Processes 2020, 8, 1416. [Google Scholar] [CrossRef]
- Kaewbanjong, J.; Wan Sia Heng, P.; Boonme, P. Clotrimazole Microemulsion and Microemulsion-Based Gel: Evaluation of Buccal Drug Delivery and Irritancy Using Chick Chorioallantoic Membrane as the Model. J. Pharm. Pharmacol. 2017, 69, 1716–1723. [Google Scholar] [CrossRef]
- Abd-Elbary, A.; Makky, A.M.A.; Tadros, M.I.; Alaa-Eldin, A.A. Laminated Sponges as Challenging Solid Hydrophilic Matrices for the Buccal Delivery of Carvedilol Microemulsion Systems: Development and Proof of Concept via Mucoadhesion and Pharmacokinetic Assessments in Healthy Human Volunteers. Eur. J. Pharm. Sci. 2016, 82, 31–44. [Google Scholar] [CrossRef]
- Pham, M.N.; Van Vo, T.; Tran, V.-T.; Tran, P.H.-L.; Tran, T.T.-D. Microemulsion-Based Mucoadhesive Buccal Wafers: Wafer Formation, In Vitro Release, and Ex Vivo Evaluation. AAPS PharmSciTech 2017, 18, 2727–2736. [Google Scholar] [CrossRef]
- Padula, C.; Telò, I.; Di Ianni, A.; Pescina, S.; Nicoli, S.; Santi, P. Microemulsion Containing Triamcinolone Acetonide for Buccal Administration. Eur. J. Pharm. Sci. 2018, 115, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Rozman, B.; Zvonar, A.; Falson, F.; Gasperlin, M. Temperature-Sensitive Microemulsion Gel: An Effective Topical Delivery System for Simultaneous Delivery of Vitamins C and E. AAPS PharmSciTech 2009, 10, 54–61. [Google Scholar] [CrossRef]
- Tubtimsri, S.; Weerapol, Y. Sustained Release Gel (Polymer-Free) of Itraconazole-Loaded Microemulsion for Oral Candidiasis Treatment: Time-Kill Kinetics and Cellular Uptake. Drug Deliv. 2023, 30, 2234099. [Google Scholar] [CrossRef] [PubMed]
- Tubtimsri, S.; Weerapol, Y.; Soontaranon, S.; Limmatvapirat, C.; Limmatvapirat, S. Monolaurin-Loaded Gel-like Microemulsion for Oropharyngeal Candidiasis Treatment: Structural Characterisation and In Vitro Antifungal Property. AAPS PharmSciTech 2022, 23, 87. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, I.M.; Pinto, C.F.F.; Moreira, C.D.S.; Saviano, A.M.; Lourenço, F.R. Design of Experiments (DoE) Applied to Pharmaceutical and Analytical Quality by Design (QbD). Braz. J. Pharm. Sci. 2018, 54, e01006. [Google Scholar] [CrossRef]
- Elazazy, M.S. Factorial Design and Machine Learning Strategies: Impacts on Pharmaceutical Analysis. In Spectroscopic Analyses—Developments and Applications; Sharmin, E., Zafar, F., Eds.; IntechOpen: Rijeka, Croatia, 2017; pp. 213–230. [Google Scholar] [CrossRef]
- Chuo, W.; Lo, Y.-K.; Huang, Y.T.; Wu, C. Statistical Optimization and Stability Study of Quercetin-Loaded Microemulsion. Int. J. Pharm. Pharm. Sci. 2021, 23–35. [Google Scholar] [CrossRef]
- Castro, S.R.; Ribeiro, L.N.M.; Breitkreitz, M.C.; Guilherme, V.A.; Rodrigues da Silva, G.H.; Mitsutake, H.; Alcântara, A.C.S.; Yokaichiya, F.; Franco, M.K.K.D.; Clemens, D.; et al. A Pre-Formulation Study of Tetracaine Loaded in Optimized Nanostructured Lipid Carriers. Sci. Rep. 2021, 11, 21463. [Google Scholar] [CrossRef]
- Bouckaert, S.; Schautteet, H.; Lefebvre, R.A.; Remon, J.P.; van Clooster, R. Comparison of Salivary Miconazole Concentrations after Administration of a Bioadhesive Slow-Release Buccal Tablet and an Oral Gel. Eur. J. Clin. Pharmacol. 1992, 43, 137–140. [Google Scholar] [CrossRef]
- Nafee, N.A.; Ismail, F.A.; Boraie, N.A.; Mortada, L.M. Mucoadhesive Buccal Patches of Miconazole Nitrate: In Vitro/In Vivo Performance and Effect of Ageing. Int. J. Pharm. 2003, 264, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Tejada, G.; Barrera, M.G.; Piccirilli, G.N.; Sortino, M.; Frattini, A.; Salomón, C.J.; Lamas, M.C.; Leonardi, D. Development and Evaluation of Buccal Films Based on Chitosan for the Potential Treatment of Oral Candidiasis. AAPS PharmSciTech 2017, 18, 936–946. [Google Scholar] [CrossRef] [PubMed]
- Tejada, G.; Piccirilli, G.N.; Sortino, M.; Salomón, C.J.; Lamas, M.C.; Leonardi, D. Formulation and In-Vitro Efficacy of Antifungal Mucoadhesive Polymeric Matrices for the Delivery of Miconazole Nitrate. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 79, 140–150. [Google Scholar] [CrossRef]
- Anuța, V.; Nițulescu, G.M.; Dinu-Pîrvu, C.-E.; Olaru, O.T. Biopharmaceutical Profiling of New Antitumor Pyrazole Derivatives. Molecules 2014, 19, 16381–16401. [Google Scholar] [CrossRef] [PubMed]
- Vlaia, L.; Coneac, G.; Muţ, A.M.; Olariu, I.; Vlaia, V.; Anghel, D.F.; Maxim, M.E.; Dobrescu, A.; Hîrjău, M.; Lupuleasa, D. Topical Biocompatible Fluconazole-Loaded Microemulsions Based on Essential Oils and Sucrose Esters: Formulation Design Based on Pseudo-Ternary Phase Diagrams and Physicochemical Characterization. Processes 2021, 9, 144. [Google Scholar] [CrossRef]
- Bergonzi, M.C.; Hamdouch, R.; Mazzacuva, F.; Isacchi, B.; Bilia, A.R. Optimization, Characterization and In Vitro Evaluation of Curcumin Microemulsions. LWT-Food Sci. Technol. 2014, 59, 148–155. [Google Scholar] [CrossRef]
- Fonseca-Santos, B.; Bonifácio, B.V.; Baub, T.M.; Gremião, M.P.D.; Chorilli, M. In-Situ Gelling Liquid Crystal Mucoadhesive Vehicle for Curcumin Buccal Administration and Its Potential Application in the Treatment of Oral Candidiasis. J. Biomed. Nanotechnol. 2019, 15, 1334–1344. [Google Scholar] [CrossRef]
- Mazonde, P.; Khamanga, S.M.M.; Walker, R.B. Design, Optimization, Manufacture and Characterization of Efavirenz-Loaded Flaxseed Oil Nanoemulsions. Pharmaceutics 2020, 12, 797. [Google Scholar] [CrossRef]
- Anicescu, M.-C.; Dinu-Pîrvu, C.-E.; Talianu, M.-T.; Ghica, M.V.; Anuța, V.; Prisada, R.-M.; Nicoară, A.C.; Popa, L. Insights from a Box–Behnken Optimization Study of Microemulsions with Salicylic Acid for Acne Therapy. Pharmaceutics 2022, 14, 174. [Google Scholar] [CrossRef]
- Maguire, C.M.; Rösslein, M.; Wick, P.; Prina-Mello, A. Characterisation of Particles in Solution—A Perspective on Light Scattering and Comparative Technologies. Sci. Technol. Adv. Mater. 2018, 19, 732–745. [Google Scholar] [CrossRef]
- de Carsalade Du Pont, V. Fractionation and Characterization of Nanoparticles by a Hydrodynamic Method: Modelling and Application to Consumer Products. Ph.D. Thesis, PSL Université Paris, Paris, France, 16 April 2021. [Google Scholar]
- Senarat, S.; Tuntarawongsa, S.; Lertsuphotvanit, N.; Rojviriya, C.; Phaechamud, T.; Chantadee, T. Levofloxacin HCl-Loaded Eudragit L-Based Solvent Exchange-Induced In Situ Forming Gel Using Monopropylene Glycol as a Solvent for Periodontitis Treatment. Gels 2023, 9, 583. [Google Scholar] [CrossRef]
- Bruel, C.; Queffeulou, S.; Darlow, T.; Virgilio, N.; Tavares, J.R.; Patience, G.S. Experimental Methods in Chemical Engineering: Contact Angles. Can. J. Chem. Eng. 2019, 97, 832–842. [Google Scholar] [CrossRef]
- Wang, S.; Zuo, A.; Guo, J. Types and Evaluation of In Vitro Penetration Models for Buccal Mucosal Delivery. J. Drug Deliv. Sci. Technol. 2021, 61, 102122. [Google Scholar] [CrossRef]
- Farooq, U.; Rasul, A.; Zafarullah, M.; Abbas, G.; Rasool, M.; Ali, F.; Ahmed, S.; Javaid, Z.; Abid, Z.; Riaz, H.; et al. Nanoemulsions as Novel Nanocarrieres for Drug Delivery across the Skin: In-Vitro, In-Vivo Evaluation of Miconazole Nanoemulsions for Treatment of Candidiasis albicans. Des. Monomers Polym. 2021, 24, 240–258. [Google Scholar] [CrossRef] [PubMed]
- Klein, S. Influence of Different Test Parameters on In Vitro Drug Release from Topical Diclofenac Formulations in a Vertical Diffusion Cell Setup. Pharmazie 2013, 68, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Shahid, M.; Hussain, A.; Khan, A.A.; Alanazi, A.M.; Alaofi, A.L.; Alam, M.; Ramzan, M. Antifungal Cationic Nanoemulsion Ferrying Miconazole Nitrate with Synergism to Control Fungal Infections: In Vitro, Ex Vivo, and In Vivo Evaluations. ACS Omega 2022, 7, 13343–13353. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Sinha, V.R. Preparation and Optimization of Voriconazole Microemulsion for Ocular Delivery. Colloids Surf. B Biointerfaces 2014, 117, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Dănilă, E.; Moldovan, Z.; Albu Kaya, M.G.; Ghica, M.V. Formulation and Characterization of Some Oil in Water Cosmetic Emulsions Based on Collagen Hydrolysate and Vegetable Oils Mixtures. Pure Appl. Chem. 2019, 91, 1493–1507. [Google Scholar] [CrossRef]
- Padula, C.; Pescina, S.; Nicoli, S.; Santi, P. New Insights on the Mechanism of Fatty Acids as Buccal Permeation Enhancers. Pharmaceutics 2018, 10, 201. [Google Scholar] [CrossRef]
- Yang, T.-L.; Hsieh, C.-M.; Meng, L.-J.; Tsai, T.; Chen, C.-T. Oleic Acid-Based Self Micro-Emulsifying Delivery System for Enhancing Antifungal Activities of Clotrimazole. Pharmaceutics 2022, 14, 478. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Khalid, M.S.; Khan, M.F.; Ullah, Z. Beneficial Effects of Topical 6-Gingerol Loaded Nanoemulsion Gel for Wound and Inflammation Management with Their Comparative Dermatokinetic. J. Drug Deliv. Sci. Technol. 2023, 80, 104094. [Google Scholar] [CrossRef]
- Chen, Y.S.; Chiu, Y.H.; Li, Y.S.; Lin, E.Y.; Hsieh, D.K.; Lee, C.H.; Huang, M.H.; Chuang, H.M.; Lin, S.Z.; Harn, H.J.; et al. Integration of PEG 400 into a Self-Nanoemulsifying Drug Delivery System Improves Drug Loading Capacity and Nasal Mucosa Permeability and Prolongs the Survival of Rats with Malignant Brain Tumors. Int. J. Nanomed. 2019, 14, 3601–3613. [Google Scholar] [CrossRef] [PubMed]
- Taher, S.S.; Al-Kinani, K.K.; Hammoudi, Z.M.; Ghareeb, M. mohammed Co-Surfactant Effect of Polyethylene Glycol 400 on Microemulsion Using BCS Class II Model Drug. J. Adv. Pharm. Educ. Res. 2022, 12, 63–69. [Google Scholar] [CrossRef]
- Anton, N.; Vandamme, T.F. Nano-Emulsions and Micro-Emulsions: Clarifications of the Critical Differences. Pharm. Res. 2011, 28, 978–985. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.J.; McClements, D.J. Nanoemulsions as Delivery Systems for Lipophilic Nutraceuticals: Strategies for Improving Their Formulation, Stability, Functionality and Bioavailability. Food Sci. Biotechnol. 2020, 29, 149–168. [Google Scholar] [CrossRef]
- Mitra, D. Microemulsion and Its Application: An Inside Story. Mater. Today Proc. 2023, 83, 75–82. [Google Scholar] [CrossRef]
- Talianu, M.-T.; Dinu-Pîrvu, C.-E.; Ghica, M.V.; Anuţa, V.; Jinga, V.; Popa, L. Foray into Concepts of Design and Evaluation of Microemulsions as a Modern Approach for Topical Applications in Acne Pathology. Nanomaterials 2020, 10, 2292. [Google Scholar] [CrossRef]
- He, S.; Mu, H. Microenvironmental pH Modification in Buccal/Sublingual Dosage Forms for Systemic Drug Delivery. Pharmaceutics 2023, 15, 637. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Kaplan, I.; Calderon, S.; David, M.; Chan, Y.H.; Weinberger, A. Distribution of Mucosal PH on the Bucca, Tongue, Lips and Palate. A Study in Healthy Volunteers and Patients with Lichen Planus, Behçet’s Disease and Burning Mouth Syndrome. Acta Derm. Venereol. 2001, 81, 178–180. [Google Scholar] [CrossRef]
- Manzoor, A.; Asif, M.; Khalid, S.H.; Ullah Khan, I.; Asghar, S. Nanosizing of Lavender, Basil, and Clove Essential Oils into Microemulsions for Enhanced Antioxidant Potential and Antibacterial and Antibiofilm Activities. ACS Omega 2023, 8, 40600–40612. [Google Scholar] [CrossRef]
- Assaf, S.M.; Maaroof, K.T.; Altaani, B.M.; Ghareeb, M.M.; Abu Alhayyal, A.A. Jojoba Oil-Based Microemulsion for Transdermal Drug Delivery. Res. Pharm. Sci. 2021, 16, 326–340. [Google Scholar] [CrossRef]
- Anicescu, M.C.; Dinu-Pîrvu, C.E.; Ghica, M.V.; Talianu, M.T.; Popa, L. Preliminary Study Regarding the Formulation and Physical Evaluation of Some Biocompatible, Oil in Water Microemulsions with Salicylic Acid for Dermatologic Use. Farmacia 2021, 69, 434. [Google Scholar] [CrossRef]
- Szumała, P.; Kaplińska, J.; Makurat-Kasprolewicz, B.; Mania, S. Microemulsion Delivery Systems with Low Surfactant Concentrations: Optimization of Structure and Properties by Glycol Cosurfactants. Mol. Pharm. 2023, 20, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Djekic, L.; Primorac, M.; Filipic, S.; Agbaba, D. Investigation of Surfactant/Cosurfactant Synergism Impact on Ibuprofen Solubilization Capacity and Drug Release Characteristics of Nonionic Microemulsions. Int. J. Pharm. 2012, 433, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Panoutsopoulou, E.; Zbytovská, J.; Vávrová, K.; Paraskevopoulos, G. Phospholipid-Based Microemulsions for Cutaneous Imiquimod Delivery. Pharmaceuticals 2022, 15, 515. [Google Scholar] [CrossRef] [PubMed]
- Gradzielski, M.; Duvail, M.; de Molina, P.M.; Simon, M.; Talmon, Y.; Zemb, T. Using Microemulsions: Formulation Based on Knowledge of Their Mesostructure. Chem. Rev. 2021, 121, 5671–5740. [Google Scholar] [CrossRef]
- Fonseca-Santos, B.; Araujo, G.; Ferreira, P.; Victorelli, F.; Pironi, A.; Hugo, V.; Carvalho, S.; Chorilli, M. Design and Characterization of Lipid-Surfactant-Based Systems for Enhancing Topical Anti-Inflammatory Activity of Ursolic Acid. Pharmaceutics 2023, 15, 366. [Google Scholar] [CrossRef]
- Tang, H.; Xiang, S.; Li, X.; Zhou, J.; Kuang, C. Preparation and In Vitro Performance Evaluation of Resveratrol for Oral Self-Microemulsion. PLoS ONE 2019, 14, e0214544. [Google Scholar] [CrossRef]
- Badawi, N.M.; Yehia, R.M.; Lamie, C.; Abdelrahman, K.A.; Attia, D.A.; Helal, D.A. Tackling Acne Vulgaris by Fabrication of Tazarotene-Loaded Essential Oil-Based Microemulsion: In Vitro and In Vivo Evaluation. Int. J. Pharm. X 2023, 5, 100185. [Google Scholar] [CrossRef]
- Suhail, N.; Alzahrani, A.K.; Basha, W.J.; Kizilbash, N.; Zaidi, A.; Ambreen, J.; Khachfe, H.M. Microemulsions: Unique Properties, Pharmacological Applications, and Targeted Drug Delivery. Front. Nanotechnol. 2021, 3, 754889. [Google Scholar] [CrossRef]
- Abruzzo, A.; Parolin, C.; Rossi, M.; Vitali, B.; Cappadone, C.; Bigucci, F. Development and Characterization of Azithromycin-Loaded Microemulsions: A Promising Tool for the Treatment of Bacterial Skin Infections. Antibiotics 2022, 11, 1040. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, L.C.; Silva-Abreu, M.; Calpena, A.C.; Rodríguez-Lagunas, M.J.; Fábrega, M.-J.; Garduño-Ramírez, M.L.; Clares, B. Nanoemulsion Strategy of Pioglitazone for the Treatment of Skin Inflammatory Diseases. Nanomedicine 2019, 19, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Coneac, G.; Vlaia, V.; Olariu, I.; Muţ, A.M.; Anghel, D.F.; Ilie, C.; Popoiu, C.; Lupuleasa, D.; Vlaia, L. Development and Evaluation of New Microemulsion-Based Hydrogel Formulations for Topical Delivery of Fluconazole. AAPS PharmSciTech 2015, 16, 889–904. [Google Scholar] [CrossRef] [PubMed]
- Dixit, A.R.; Rajput, S.J.; Patel, S.G. Preparation and Bioavailability Assessment of SMEDDS Containing Valsartan. AAPS PharmSciTech 2010, 11, 314–321. [Google Scholar] [CrossRef]
- Beggs, W.H. Influence of Alkaline PH on the Direct Lethal Action of Miconazole against Candida albicans. Mycopathologia 1992, 120, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.M.; Eldridge, D.S.; Palombo, E.A.; Harding, I.H. Stability Mechanisms for Microwave-Produced Solid Lipid Nanoparticles. Colloids Surf. A Physicochem. Eng. Asp. 2022, 643, 128774. [Google Scholar] [CrossRef]
- Gómez-Guillén, M.C.; Montero, M.P. Enhancement of Oral Bioavailability of Natural Compounds and Probiotics by Mucoadhesive Tailored Biopolymer-Based Nanoparticles: A Review. Food Hydrocoll. 2021, 118, 106772. [Google Scholar] [CrossRef]
- Butt, U.; ElShaer, A.; Snyder, L.A.S.; Al-Kinani, A.A.; Le Gresley, A.; Alany, R.G. Fatty Acid Based Microemulsions to Combat Ophthalmia Neonatorum Caused by Neisseria gonorrhoeae and Staphylococcus aureus. Nanomaterials 2018, 8, 51. [Google Scholar] [CrossRef]
- Wang, W.; Wei, H.; Du, Z.; Tai, X.; Wang, G. Formation and Characterization of Fully Dilutable Microemulsion with Fatty Acid Methyl Esters as Oil Phase. ACS Sustain. Chem. Eng. 2015, 3, 443–450. [Google Scholar] [CrossRef]
- El Maghraby, G.M.; Arafa, M.F.; Essa, E.A. Chapter 33—Phase Transition Microemulsions as Drug Delivery Systems. In Applications of Nanocomposite Materials in Drug Delivery; Inamuddin Asiri, A.M., Mohammad, A., Eds.; Woodhead Publishing: Duxford, UK, 2018; pp. 787–803. ISBN 978-0-12-813741-3. [Google Scholar] [CrossRef]
- Nikolaev, B.; Yakovleva, L.; Fedorov, V.; Li, H.; Gao, H.; Shevtsov, M. Nano- and Microemulsions in Biomedicine: From Theory to Practice. Pharmaceutics 2023, 15, 1989. [Google Scholar] [CrossRef]
- De Stefani, C.; Vasarri, M.; Salvatici, M.C.; Grifoni, L.; Quintela, J.C.; Bilia, A.R.; Degl’Innocenti, D.; Bergonzi, M.C. Microemulsions Enhance the In Vitro Antioxidant Activity of Oleanolic Acid in RAW 264.7 Cells. Pharmaceutics 2022, 14, 2232. [Google Scholar] [CrossRef] [PubMed]
- Tonglairoum, P.; Ngawhirunpat, T.; Rojanarata, T.; Kaomongkolgit, R.; Opanasopit, P. Fabrication of a Novel Scaffold of Clotrimazole-Microemulsion-Containing Nanofibers Using an Electrospinning Process for Oral Candidiasis Applications. Colloids Surf. B Biointerfaces 2015, 126, 18–25. [Google Scholar] [CrossRef]
- El-Badry, M.; Fetih, G.; Shakeel, F. Comparative Topical Delivery of Antifungal Drug Croconazole Using Liposome and Micro-Emulsion-Based Gel Formulations. Drug Deliv. 2014, 21, 34–43. [Google Scholar] [CrossRef]
- Phechkrajang, C.; Phiphitphibunsuk, W.; Sukthongchaikool, R.; Nuchtavorn, N.; Leanpolchareanchai, J. Development of Miconazole-Loaded Microemulsions for Enhanced Topical Delivery and Non-Destructive Analysis by Near-Infrared Spectroscopy. Pharmaceutics 2023, 15, 1637. [Google Scholar] [CrossRef] [PubMed]
- Siddique, M.Y.; Nazar, M.; Mahmood, M.; Saleem, M.; Alwadai, N.; Almuslem, A.; Alshammari, F.; Haider, S.; Akhtar, M.; Hussain, S.Z.; et al. Microemulsified Gel Formulations for Topical Delivery of Clotrimazole: Structural and In Vitro Evaluation. Langmuir 2021, 37, 13767–13777. [Google Scholar] [CrossRef]
- Ghica, M.V.; Albu, M.G.; Popa, L.; Moisescu, S. Response Surface Methodology and Taguchi Approach to Assess the Combined Effect of Formulation Factors on Minocycline Delivery from Collagen Sponges. Pharmazie 2013, 68, 340–348. [Google Scholar] [CrossRef]
- Almehmady, A.M.; El-Say, K.M.; Mubarak, M.A.; Alghamdi, H.A.; Somali, N.A.; Sirwi, A.; Algarni, R.; Ahmed, T.A. Enhancing the Antifungal Activity and Ophthalmic Transport of Fluconazole from PEGylated Polycaprolactone Loaded Nanoparticles. Polymers 2023, 15, 209. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-H.; Tsai, M.-J.; Fang, Y.-P.; Fu, Y.-S.; Huang, Y.-B.; Wu, P.-C. Microemulsion Formulation Design and Evaluation for Hydrophobic Compound: Catechin Topical Application. Colloids Surf. B Biointerfaces 2018, 161, 121–128. [Google Scholar] [CrossRef]
- Akula, S.; Gurram, A.K.; Devireddy, S.R. Self-Microemulsifying Drug Delivery Systems: An Attractive Strategy for Enhanced Therapeutic Profile. Int. Sch. Res. Notices 2014, 2014, 964051. [Google Scholar] [CrossRef]
- Kovács, A.; Berkó, S.; Csányi, E.; Csóka, I. Development of Nanostructured Lipid Carriers Containing Salicyclic Acid for Dermal Use Based on the Quality by Design Method. Eur. J. Pharm. Sci. 2017, 99, 246–257. [Google Scholar] [CrossRef] [PubMed]
- Sinko, P.J.; Singh, Y. (Eds.) Martin’s Physical Pharmacy and Pharmaceutical Sciences. Physical Chemistry and Biopharmaceutical Principles in the Pharmaceutical Sciences, 6th ed.; Lippincot Williams & Wilkins: Philadelphia, PA, USA, 2006; ISBN 978-1-6091-3402-0. [Google Scholar]
- Vuckovac, M.; Latikka, M.; Liu, K.; Huhtamäki, T.; Ras, R.H.A. Uncertainties in Contact Angle Goniometry. Soft Matter 2019, 15, 7089–7096. [Google Scholar] [CrossRef] [PubMed]
- Issa, C.M.; Fogaca, A.; Palermo, E.; Fontes, M.; Barud, H.S.; Dametto, A.C. A New Cohesive High-Concentrated Hyaluronic Acid Gel Filler: Correlation between Rheologic Properties and Clinical Indications. J. Biomed. Res. Environ. Sci. 2023, 4, 614–618. [Google Scholar] [CrossRef]
- Koliqi, R.; Breznica, P.; Daka, A.; Koshi, B. Application of Design of Expert Software for Evaluating the Influence of Formulation Variables on the Encapsulation Efficacy, Drug Content and Particle Size of PEO-PPO-PEO/Poly(DL-Lactide-Co-Caprolactone) Nanoparticles as Carriers for SN-38. Med. Pharm. Rep. 2021, 94, 483. [Google Scholar] [CrossRef] [PubMed]
- Hattab, M.W. On the Use of Data Transformation in Response Surface Methodology. Qual. Reliab. Eng. Int. 2018, 34, 1185–1194. [Google Scholar] [CrossRef]
- Kraber, S. Improving Your DOE - Analysis with Response Transformations. J. Plast. Film Sheeting 2021, 38, 15–20. [Google Scholar] [CrossRef]
- Prakobvaitayakit, M.; Nimmannit, U. Optimization of Polylactic-Co-Glycolic Acid Nanoparticles Containing Itraconazole Using 23 Factorial Design. AAPS PharmSciTech 2003, 4, 71. [Google Scholar] [CrossRef]
- Maddiboyina, B.; Jhawat, V.; Nakkala, R.K.; Desu, P.K.; Gandhi, S. Design Expert Assisted Formulation, Characterization and Optimization of Microemulsion Based Solid Lipid Nanoparticles of Repaglinide. Prog. Biomater. 2021, 10, 309–320. [Google Scholar] [CrossRef]









| Formulation | Oleic Acid (%) X1 | Tween 20 (%) X2 | 1 PEG 400 (%) X3 | Water (%) | 2 MCZ (%) |
|---|---|---|---|---|---|
| ME 1 | 5 | 30 | 10 | 53 | 2 |
| ME 2 | 5 | 40 | 10 | 43 | 2 |
| ME 3 | 5 | 30 | 20 | 43 | 2 |
| ME 4 | 5 | 40 | 20 | 33 | 2 |
| ME 5 | 10 | 30 | 10 | 48 | 2 |
| ME 6 | 10 | 40 | 10 | 38 | 2 |
| ME 7 | 10 | 30 | 20 | 38 | 2 |
| ME 8 | 10 | 40 | 20 | 28 | 2 |
| ME 9 | 6.25 | 35 | 10 | 51.75 | 2 |
| ME 10 | 8.75 | 30 | 15 | 44.25 | 2 |
| Components | Excipient | Solubility (mg/mL) |
|---|---|---|
| Oils | Isopropyl myristate | 36 ± 3 |
| Oleic acid | 110 ± 5 | |
| Surfactants | Tween 80 | 152 ± 10 |
| Tween 20 | 236 ± 11 | |
| Kolliphor 407 | 27 ± 5 | |
| Cosurfactants | Propylene glycol | 193 ± 7 |
| Polyethylene glycol 200 | 179 ± 12 | |
| Polyethylene glycol 400 | 209 ± 13 |
| Factor | Variable | Level | |
|---|---|---|---|
| Low (−1) | High (+1) | ||
| X1 | Oleic acid (%) | 5 | 10 |
| X2 | Tween 20 (%) | 30 | 40 |
| X3 | PEG 400 (%) | 10 | 20 |
| Std. | Block | Run | X1 | X2 | X3 |
|---|---|---|---|---|---|
| Oleic Acid (%) | Tween 20 (%) | PEG 400 (%) | |||
| 1 | 1 | 1 | −1 | −1 | −1 |
| 3 | 1 | 2 | −1 | +1 | −1 |
| 5 | 1 | 3 | −1 | −1 | +1 |
| 7 | 1 | 4 | −1 | +1 | −1 |
| 2 | 1 | 5 | +1 | −1 | −1 |
| 4 | 1 | 6 | +1 | +1 | −1 |
| 6 | 1 | 7 | +1 | −1 | +1 |
| 8 | 1 | 8 | +1 | +1 | +1 |
| 9 | 2 | 9 | 0.625 | 0 | −1 |
| 10 | 2 | 10 | 0.875 | −1 | 0 |
| Code | pH | Conductivity (μS/cm) | Refractive Index | Zaverage (nm) | PDI | D10% (nm) | D50% (nm) | D90% (nm) | Span | Zeta (mV) |
|---|---|---|---|---|---|---|---|---|---|---|
| ME1 | 5.29 ± 0.01 | 101.90 ± 0.66 | 1.3823 ± 0.0002 | 152.89 ± 2.10 | 0.230 ± 0.001 | 118.11 | 205.71 | 375.23 | 1.24 | +10.76 ± 1.15 |
| ME2 | 5.60 ± 0.01 | 88.70 ± 0.10 | 1.4047 ± 0.0001 | 128.90 ± 2.15 | 0.303 ± 0.002 | 98.17 | 187.54 | 375.23 | 1.47 | +10.68 ± 1.19 |
| ME3 | 5.53 ± 0.07 | 55.70 ± 0.30 | 1.4012 ± 0.0001 | 188.33 ± 5.03 | 0.296 ± 0.011 | 142.11 | 284.33 | 543.17 | 1.41 | +14.00 ± 1.28 |
| ME4 | 5.74 ± 0.02 | 47.60 ± 0.10 | 1.4238 ± 0.0001 | 119.60 ± 1.37 | 0.332 ± 0.002 | 93.73 | 187.54 | 358.28 | 1.41 | +10.68 ± 2.19 |
| ME5 | 5.15 ± 0.02 | 21.67 ± 0.06 | 1.3959 ± 0.0001 | 161.34 ± 4.06 | 0.165 ± 0.003 | 123.7 | 205.71 | 342.09 | 1.06 | +12.34 ± 1.42 |
| ME6 | 5.48 ± 0.01 | 18.07 ± 0.06 | 1.4154 ± 0.0001 | 202.29 ± 5.02 | 0.292 ± 0.002 | 155.87 | 297.78 | 568.88 | 1.38 | +9.62 ± 3.23 |
| ME7 | 5.27 ± 0.01 | 7.96 ± 0.01 | 1.4148 ± 0.0001 | 225.13 ± 5.20 | 0.280 ± 0.005 | 170.9 | 326.63 | 623.99 | 1.38 | +13.30 ± 1.07 |
| ME8 | 5.80 ± 0.01 | 8.80 ± 0.25 | 1.4318 ± 0.0001 | 250.20 ± 6.50 | 0.301 ± 0.007 | 196.41 | 375.23 | 716.84 | 1.38 | +12.62 ± 1.12 |
| ME9 | 5.57 ± 0.01 | 74.43 ± 0.03 | 1.3895 ± 0.0001 | 133.57 ± 3.08 | 0.214 ± 0.012 | 102.81 | 179.07 | 311.87 | 1.16 | +9.10 ± 1.94 |
| ME10 | 5.48 ± 0.00 | 18.89 ± 0.02 | 1.4058 ± 0.0001 | 144.36 ± 1.71 | 0.230 ± 0.005 | 112.77 | 196.41 | 358.28 | 1.24 | +12.85 ± 2.44 |
| Code | Viscosity (Pa·s)/Consistency Index (Pa·sn) | 1 n | 2 R | Rheological Model |
|---|---|---|---|---|
| ME 1 | 1.001 | 0.49 | 0.9974 | Ostwald–de Waele |
| ME 2 | 0.346 | 1.0 | 0.9993 | Newton |
| ME 3 | 0.192 | 1.0 | 0.9998 | Newton |
| ME 4 | 0.304 | 1.0 | 0.9997 | Newton |
| ME 5 | 30.89 | 0.22 | 0.9956 | Herschel–Bulkley |
| ME 6 | 21.81 | 0.22 | 0.9654 | Ostwald–de Waele |
| ME 7 | 8.390 | 0.50 | 0.9973 | Ostwald–de Waele |
| ME 8 | 2.213 | 0.45 | 0.9993 | Ostwald–de Waele |
| ME 9 | 0.285 | 1.0 | 0.9994 | Bingham |
| ME 10 | 20.85 | 0.30 | 0.9986 | Herschel–Bulkley |
| No. | Parameters Tested through Goniometric Technique | |||||||
|---|---|---|---|---|---|---|---|---|
| Pendant Drop (n = 3) | Contact Angle (n = 5) | Wa (mN/m) | Wc (mN/m) | S (mN/m) | ||||
| Vol (μL) | γLG (mN/m) | Vol (μL) | γLG (mN/m) | θ (°) | ||||
| 1 | 4.96 ± 0.09 | 26.44 ± 0.21 | 5.04 ± 0.003 | 34.78 ± 0.525 | 52.14 ± 0.560 | 56.07 ± 0.72 | 69.56 ± 1.05 | −13.49 ± 0.52 |
| 2 | 4.83 ± 0.04 | 25.49 ± 0.08 | 4.72 ± 0.003 | 40.85 ± 0.434 | 57.75 ± 0.596 | 62.91 ± 0.24 | 81.69 ± 0.86 | −18.78 ± 0.77 |
| 3 | 4.73 ± 0.05 | 25.80 ± 0.03 | 4.85 ± 0.008 | 44.53 ± 1.058 | 48.00 ± 0.557 | 74.77 ± 2.23 | 89.05 ± 2.11 | −44.52 ± 0.48 |
| 4 | 4.66 ± 0.03 | 25.38 ± 0.02 | 4.24 ± 0.004 | 35.99 ± 0.634 | 48.49 ± 0.438 | 60.56 ± 1.80 | 71.98 ± 1.26 | −11.41 ± 1.21 |
| 5 | 3.51 ± 0.44 | 21.18 ± 0.60 | 3.62 ± 0.008 | 10.11 ± 0.095 | 51.10 ± 0.413 | 16.44 ± 0.14 | 20.22 ± 0.19 | −3.78 ± 0.09 |
| 6 | 4.29 ± 0.59 | 23.06 ± 0.89 | 3.96 ± 0.003 | 8.05 ± 0.023 | 42.37 ± 0.012 | 13.99 ± 0.04 | 16.09 ± 0.04 | −2.10 ± 0.007 |
| 7 | 3.63 ± 0.10 | 20.90 ± 0.49 | 4.25 ± 0.002 | 6.75 ± 0.050 | 47.75 ± 0.106 | 11.28 ± 0.08 | 13.50 ± 0.09 | −2.21 ± 0.01 |
| 8 | 3.54 ± 0.23 | 19.08 ±0.69 | 4.10 ± 0.003 | 5.92 ± 0.036 | 37.03 ± 0.156 | 10.65 ±0.05 | 11.84 ± 0.07 | −1.19 ± 0.02 |
| 9 | 5.42 ± 0.24 | 25.98 ± 0.49 | 5.27 ± 0.022 | 26.48 ± 1.790 | 53.72 ± 0.309 | 42.23 ± 2.96 | 52.95 ± 3.57 | −10.72 ± 0.63 |
| 10 | 3.50 ± 0.32 | 17.97 ± 0.62 | 2.39 ± 0.001 | 5.65 ± 0.014 | 41.87 ± 0.057 | 9.84 ± 0.02 | 11.29 ± 0.03 | −1.44 ± 0.01 |
| ME | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Gel (R) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| D·10−5 (cm2/s) | 2.569 | 2.22 | 1.85 | 2.11 | 0.252 | 0.516 | 0.265 | 1.00 | 1.27 | 0.343 | 0.0162 |
| R | 0.9904 | 0.9842 | 0.9630 | 0.9812 | 0.9858 | 0.9910 | 0.9959 | 0.9861 | 0.9935 | 0.9961 | 0.9758 |
| Variable | Independent Variables | Dependent Variables | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Oleic Acid (%) | Tween 20 (%) | PEG 400 (%) | 1 Ds (Actual) (nm) | Ds (Predicted) (nm) | 2 W (Actual) (mN/m) | W (Predicted) (mN/m) | 3 D (Actual) (cm2/s) | 4 Sqrt(D) (Actual) (cm2/s) | Sqrt(D) (Predicted) (cm2/s) | |
| Code | X1 | X2 | X3 | Y1 actual | Y1 predicted | Y2 actual | Y2 predicted | Y3 actual | Y3 actual | Y3 predicted |
| ME 1 | 5 | 30 | 10 | 152.89 | 156.78 | 69.56 | 69.19 | 2.56·10−5 | 0.0051 | 0.0051 |
| ME 2 | 5 | 40 | 10 | 128.90 | 131.04 | 81.69 | 83.79 | 2.22·10−5 | 0.0047 | 0.0047 |
| ME 3 | 5 | 30 | 20 | 188.33 | 181.39 | 89.05 | 88.30 | 1.85·10−5 | 0.0043 | 0.0043 |
| ME 4 | 5 | 40 | 20 | 119.60 | 125.34 | 71.98 | 73.70 | 2.11·10−5 | 0.0046 | 0.0046 |
| ME 5 | 10 | 30 | 10 | 161.34 | 153.19 | 20.22 | 17.61 | 2.52·10−6 | 0.0016 | 0.0016 |
| ME 6 | 10 | 40 | 10 | 202.29 | 209.24 | 16.09 | 16.38 | 5.16·10−6 | 0.0023 | 0.0023 |
| ME 7 | 10 | 30 | 20 | 225.13 | 222.99 | 13.50 | 11.86 | 2.65·10−6 | 0.0016 | 0.0017 |
| ME 8 | 10 | 40 | 20 | 250.20 | 248.72 | 11.84 | 13.10 | 1.00·10−5 | 0.0032 | 0.0031 |
| ME 9 | 6.25 | 35 | 10 | 133.57 | 123.92 | 52.95 | 47.56 | 1.27·10−5 | 0.0036 | 0.0036 |
| ME 10 | 8.75 | 30 | 15 | 144.36 | 154.01 | 11.29 | 16.68 | 3.43·10−6 | 0.0019 | 0.0018 |
| Source | Sum of Squares | df | Mean Square | F-Value | p-Value |
|---|---|---|---|---|---|
| Block | 2511.59 | 1 | 2511.59 | ||
| Model | 14,506.93 | 5 | 2901.39 | 21.29 | 0.0150 |
| X1-Oleic acid | 7585.15 | 1 | 7585.15 | 55.67 | 0.0050 |
| X3-PEG 400 | 2171.31 | 1 | 2171.31 | 25.94 | 0.0282 |
| X1X2 | 3390.09 | 1 | 3390.09 | 24.88 | 0.0155 |
| X1X3 | 1035.22 | 1 | 1035.22 | 7.60 | 0.0704 |
| X2X3 | 459.35 | 1 | 459.35 | 3.37 | 0.1637 |
| Residual | 408.77 | 3 | 136.26 | ||
| Cor Total | 17,427.29 | 9 |
| Source | Sum of Squares | Df | Mean Square | F-Value | p-Value |
|---|---|---|---|---|---|
| Block | 342.05 | 1 | 342.05 | ||
| Model | 8925.50 | 4 | 2231.38 | 115.37 | 0.0002 |
| X1-Oleic acid | 8697.67 | 1 | 8697.67 | 449.69 | <0.0001 |
| X1X3 | 41.34 | 1 | 41.34 | 2.14 | 0.2176 |
| X2X3 | 89.31 | 1 | 89.31 | 4.62 | 0.0981 |
| X1X2X3 | 125.37 | 1 | 125.37 | 6.48 | 0.0636 |
| Residual | 77.37 | 4 | 19.34 | ||
| Cor Total | 9344.92 | 9 |
| Source | Sum of Squares | Df | Mean Square | F-Value | p-Value |
|---|---|---|---|---|---|
| Block | 7.987·10−7 | 1 | 7.987·10−7 | ||
| Model | 0.0000 | 6 | 2655·10−6 | 2361.10 | 0.0004 |
| X1-Oleic acid | 0.0000 | 1 | 0.0000 | 11,725.47 | <0.0001 |
| X2-Tween 20 | 6.020·10−7 | 1 | 6.020·10−7 | 535.41 | 0.0019 |
| X1X2 | 6.471·10−7 | 1 | 6.471·10−7 | 575.58 | 0.0017 |
| X1X3 | 4.076·10−7 | 1 | 4.076·10−7 | 362.55 | 0.0027 |
| X2X3 | 2.777·10−7 | 1 | 2.777·10−7 | 247.01 | 0.0040 |
| Residual | 2.249·10−9 | 2 | 1.124·10−9 | ||
| Cor Total | 0.0000 | 9 |
| No. | Variables | Trial 1 | Trial 2 | ||
|---|---|---|---|---|---|
| Goal | Limits | Goal | Limits | ||
| 1 | Oleic acid | 7 % | 5.0–10% | in range | 5–10% |
| 2 | Tween 20 | maximize | 30–40% | in range | 30–40% |
| 3 | PEG 400 | in range | 10–20% | in range | 10–20% |
| 4 | R1 (nm) | minimize | 119.6–250 nm | minimize | 119.6–250 nm |
| 5 | R2 (mN/m) | 60 mN/m | 11.29–89.05 mN/m | 60 mN/m | 11.29–89.05 mN/m |
| 6 | R3 (cm2/s) | in range | 10−5–2.56·10−5 cm2/s | in range | 10−5–2.56·10−5 cm2/s |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talianu, M.-T.; Dinu-Pîrvu, C.-E.; Ghica, M.V.; Anuţa, V.; Prisada, R.M.; Popa, L. Development and Characterization of New Miconazole-Based Microemulsions for Buccal Delivery by Implementing a Full Factorial Design Modeling. Pharmaceutics 2024, 16, 271. https://doi.org/10.3390/pharmaceutics16020271
Talianu M-T, Dinu-Pîrvu C-E, Ghica MV, Anuţa V, Prisada RM, Popa L. Development and Characterization of New Miconazole-Based Microemulsions for Buccal Delivery by Implementing a Full Factorial Design Modeling. Pharmaceutics. 2024; 16(2):271. https://doi.org/10.3390/pharmaceutics16020271
Chicago/Turabian StyleTalianu, Marina-Theodora, Cristina-Elena Dinu-Pîrvu, Mihaela Violeta Ghica, Valentina Anuţa, Răzvan Mihai Prisada, and Lăcrămioara Popa. 2024. "Development and Characterization of New Miconazole-Based Microemulsions for Buccal Delivery by Implementing a Full Factorial Design Modeling" Pharmaceutics 16, no. 2: 271. https://doi.org/10.3390/pharmaceutics16020271
APA StyleTalianu, M.-T., Dinu-Pîrvu, C.-E., Ghica, M. V., Anuţa, V., Prisada, R. M., & Popa, L. (2024). Development and Characterization of New Miconazole-Based Microemulsions for Buccal Delivery by Implementing a Full Factorial Design Modeling. Pharmaceutics, 16(2), 271. https://doi.org/10.3390/pharmaceutics16020271









