Synthesis, Characterization, and Docking Study of Novel Thioureidophosphonate-Incorporated Silver Nanocomposites as Potent Antibacterial Agents
Abstract
1. Introduction
2. Materials and Methods
2.1. Characterization Techniques
2.2. Chemicals
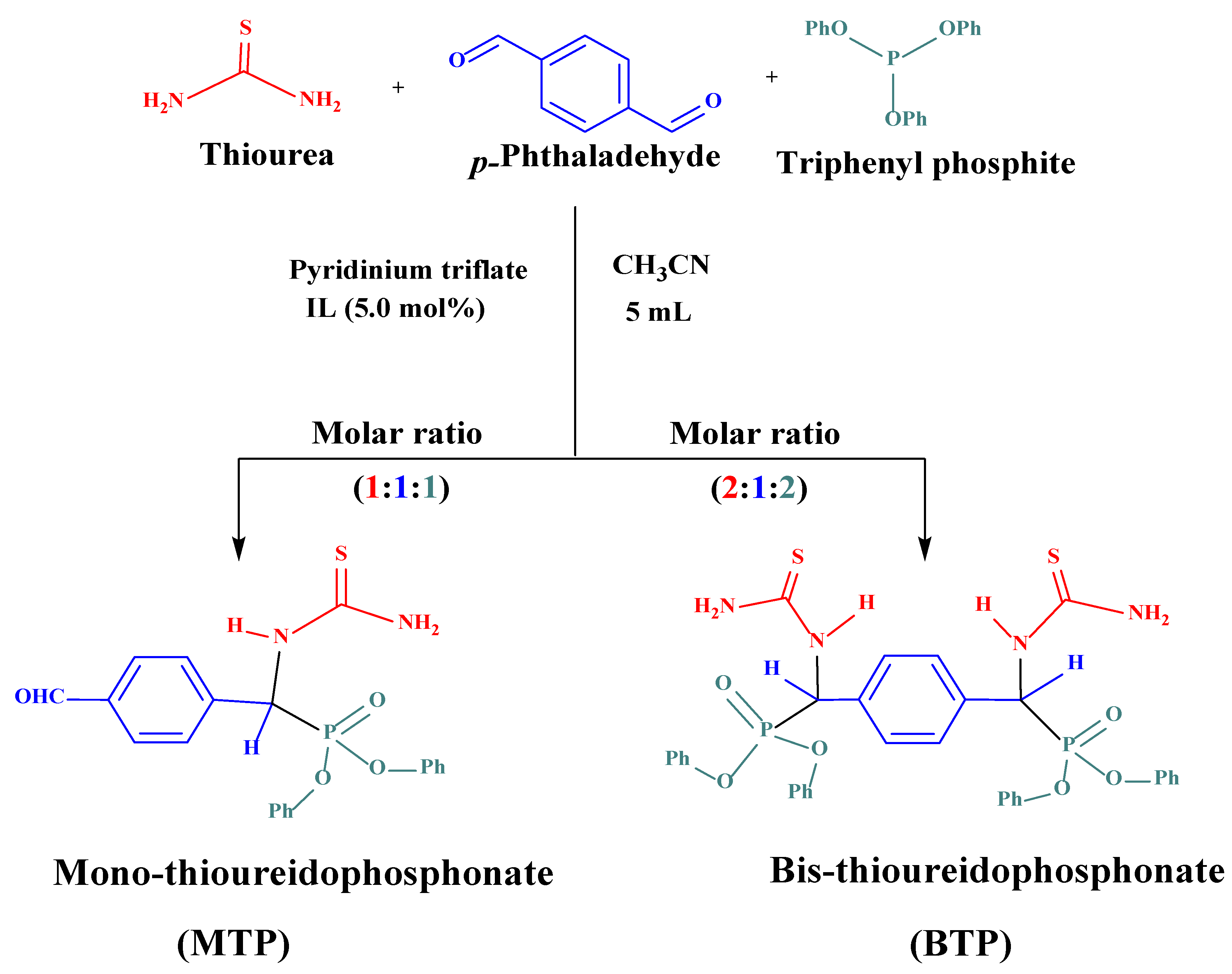
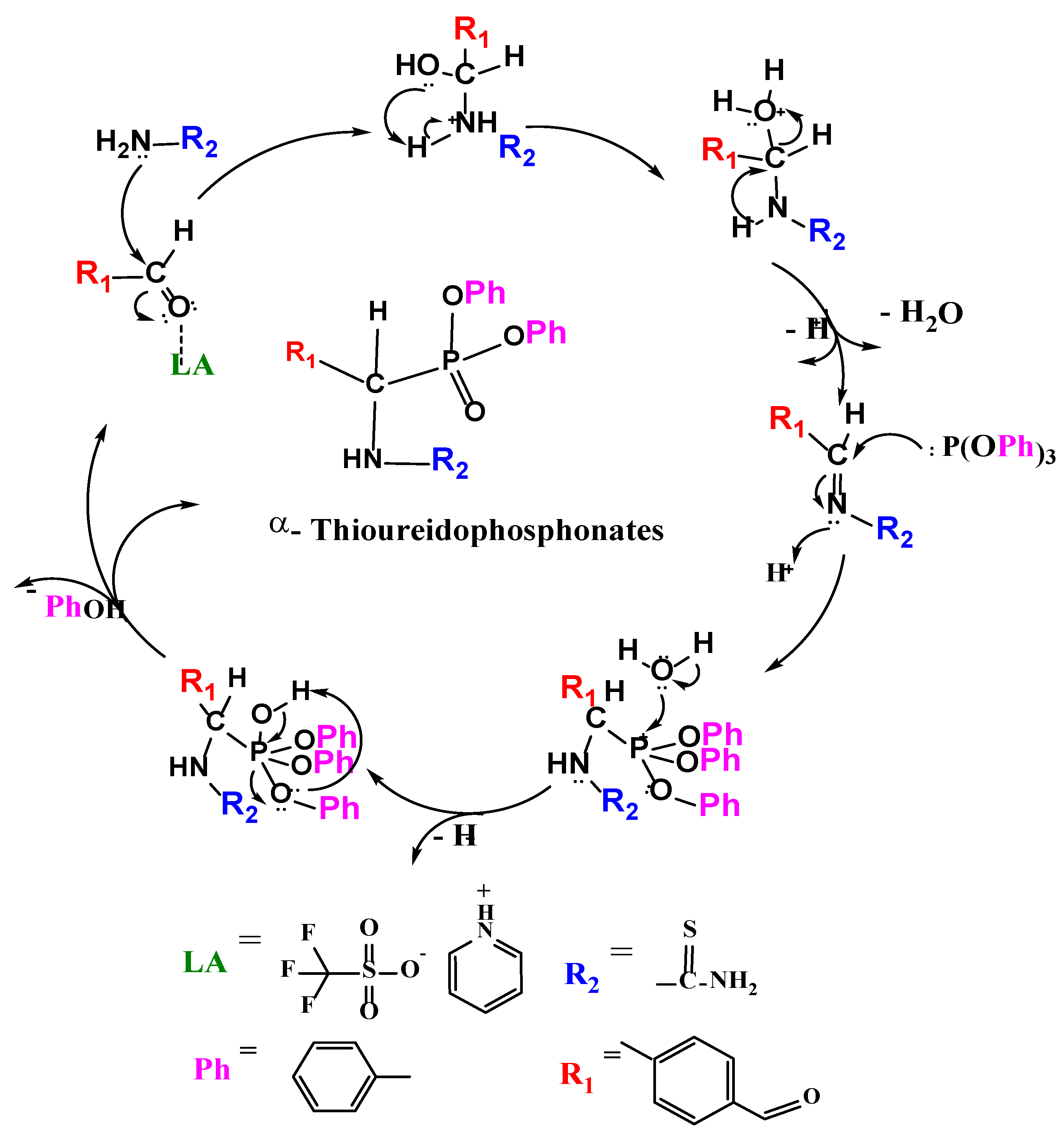
2.3. Preparation of α-Thioureidophosphonate Cores
2.4. Synthesis of α-Thioureidophosphonate-Based Silver Nanoparticles
2.5. Microorganisms and Media
2.6. Molecular Docking Study
2.7. Pharmacokinetics In Silico Screening
3. Results and Discussion
3.1. Chemistry
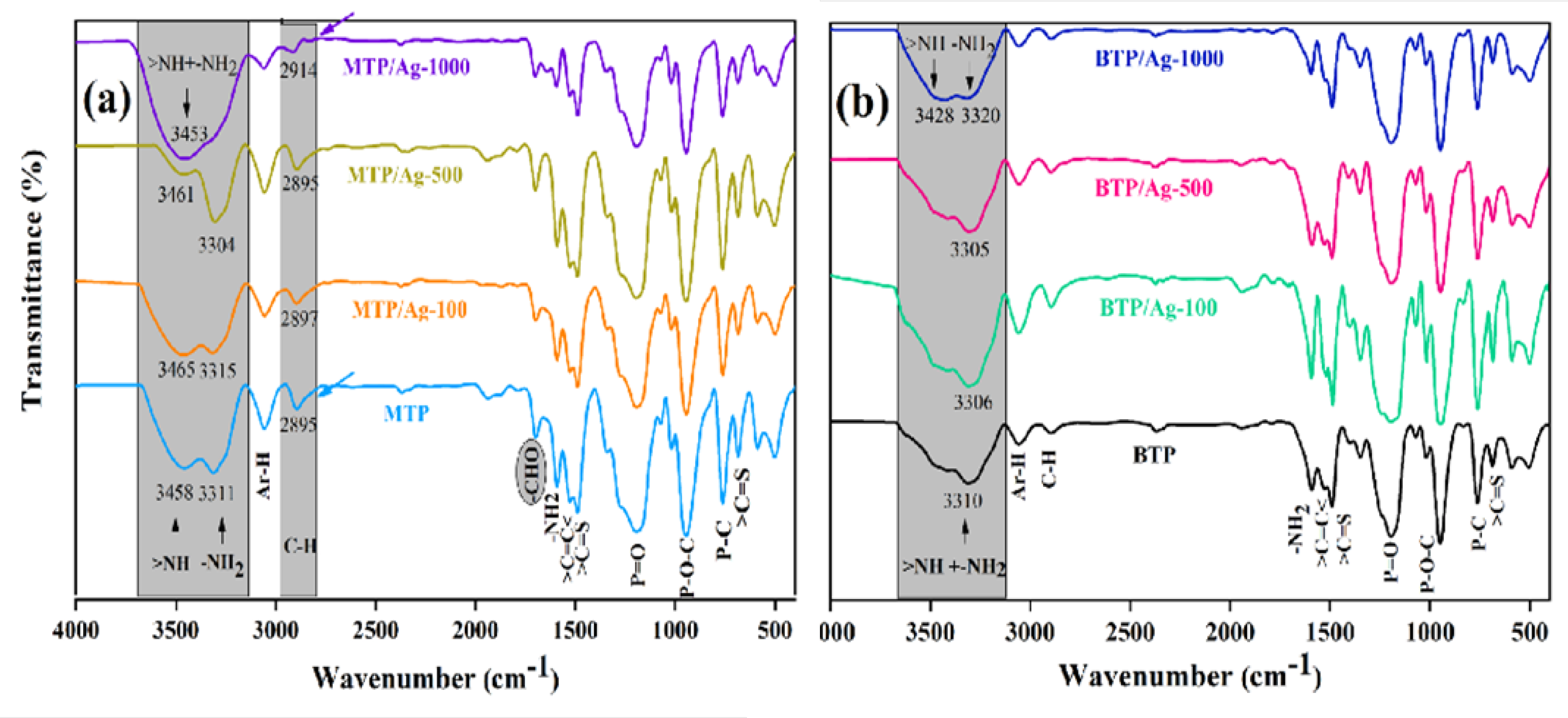
3.1.1. Synthesis and Structural Characterization of Thioureidophosphonate Compounds
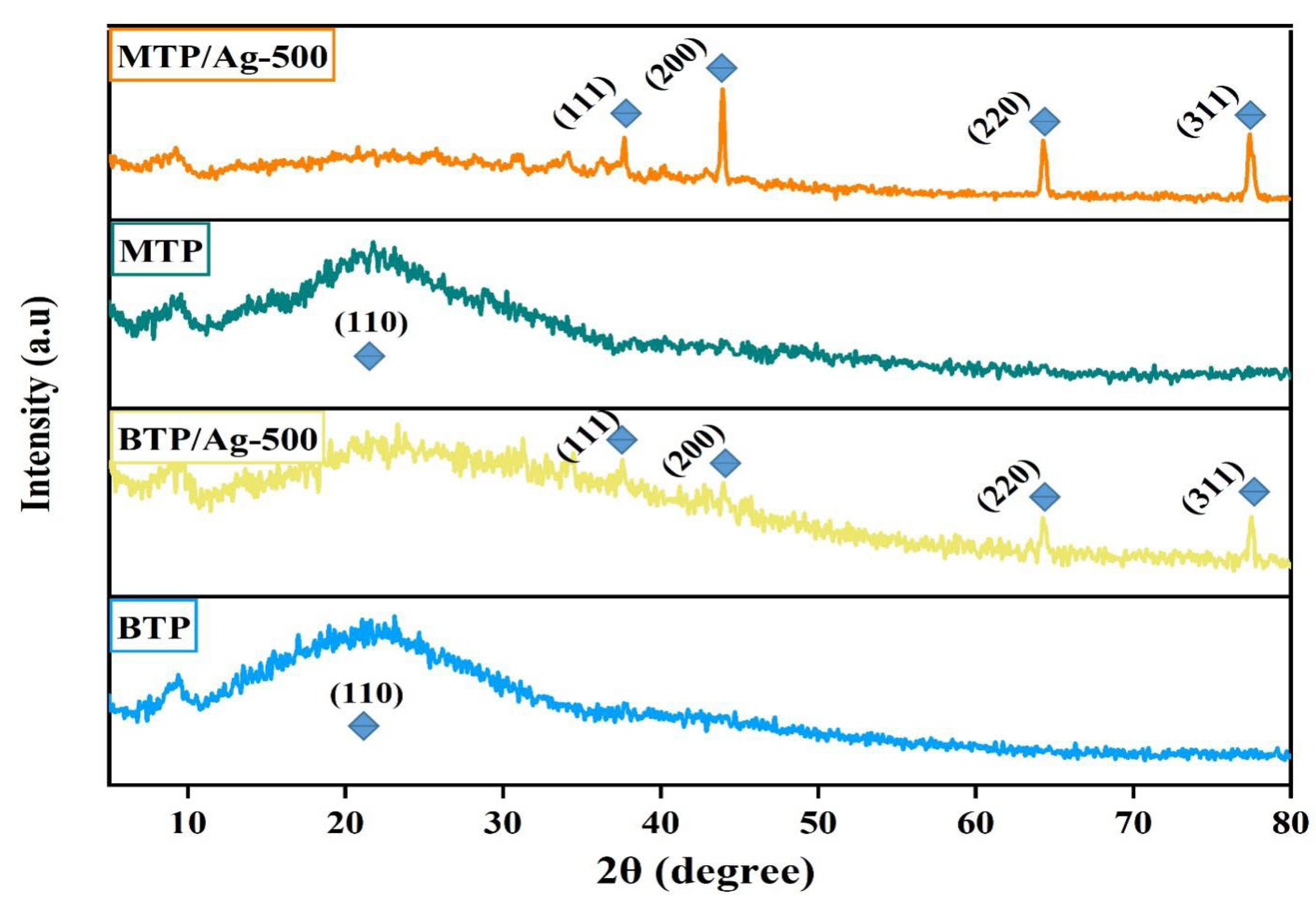
3.1.2. Fabrication and Structural Elucidation of Thioureidophosphonates Capped Silver Nanoparticles
3.2. Antibacterial Activity
3.2.1. Bactericidal Properties
The Killing Action against Gram-Positive Strains
The Killing Action against Gram-Negative Strains
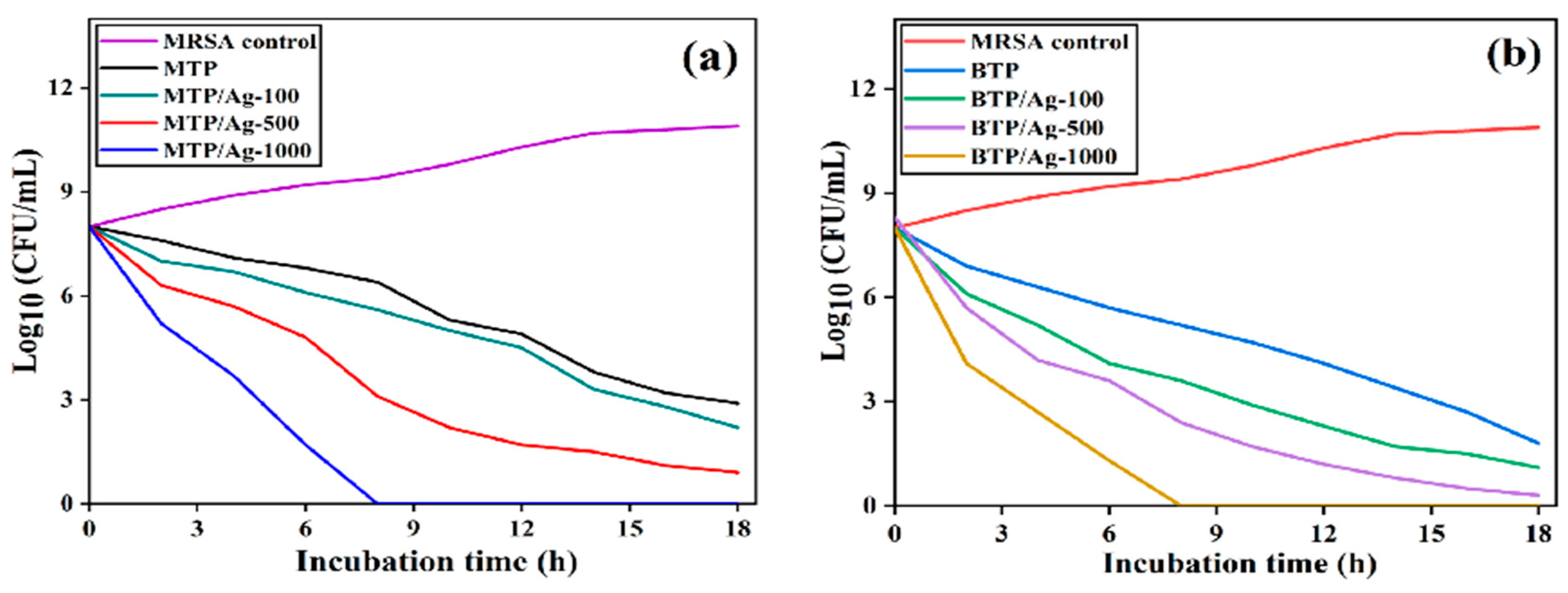
3.2.2. Time–Kill Assay
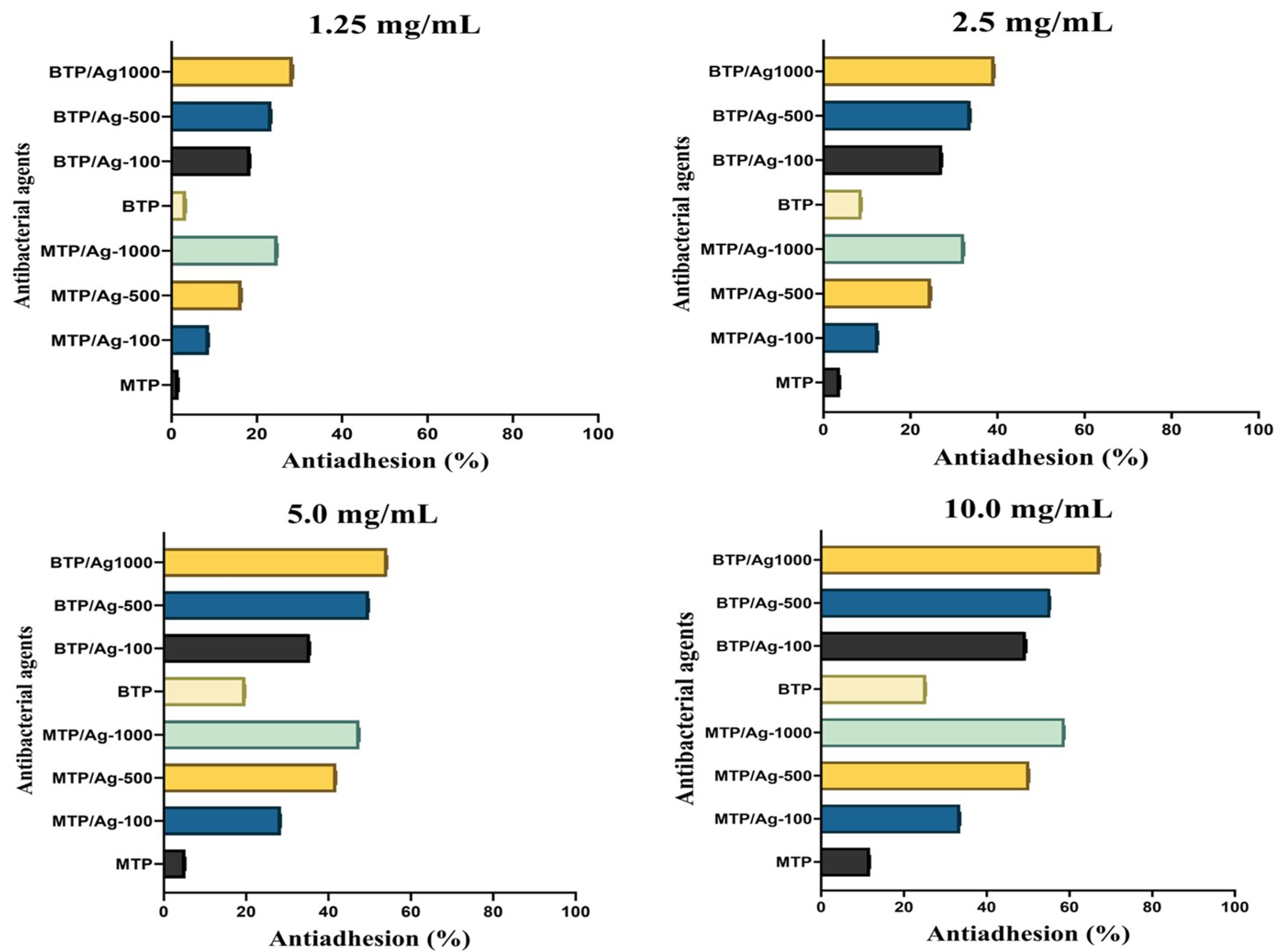
3.2.3. Antiadhesion Activity
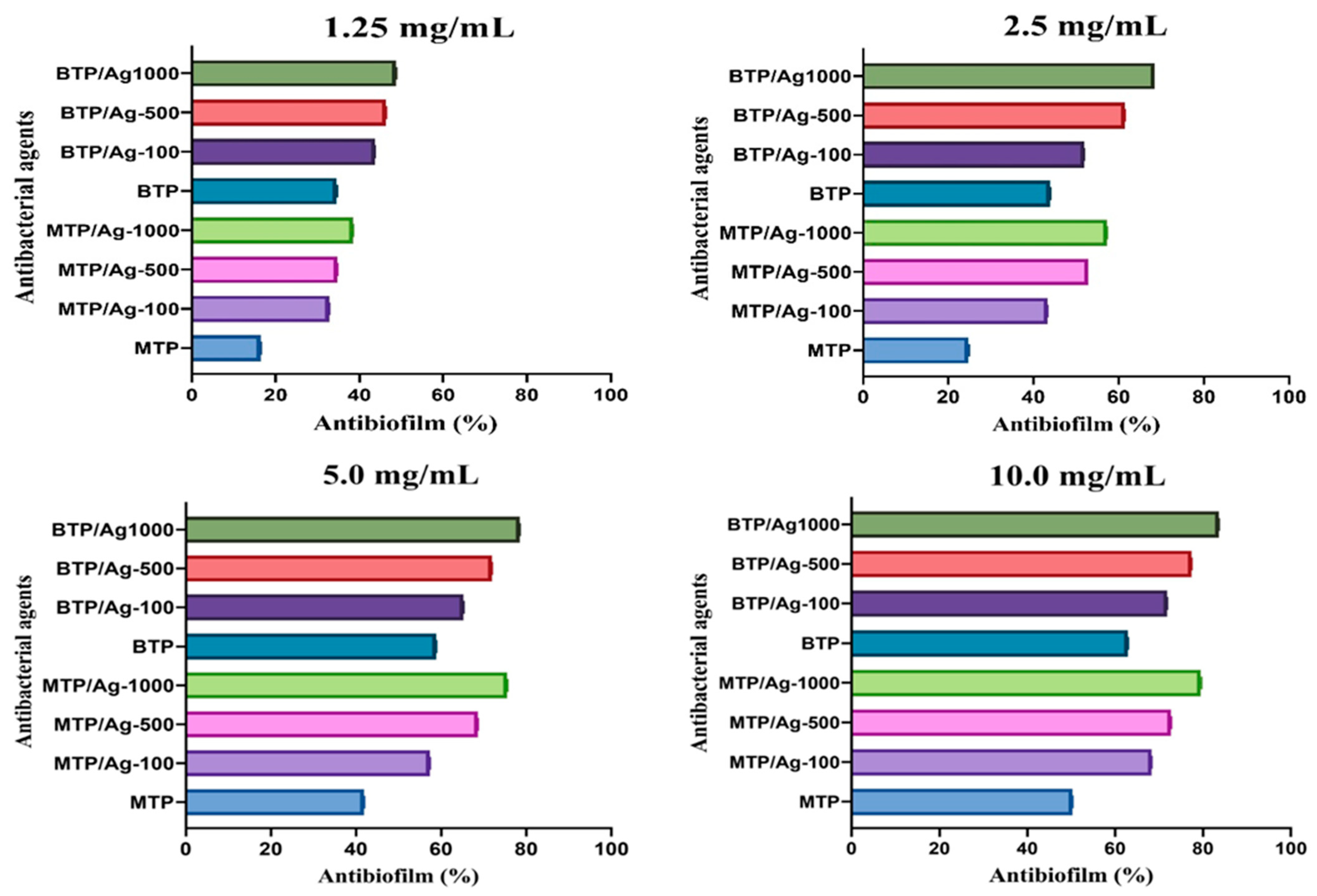
3.2.4. Antibiofilm Assay
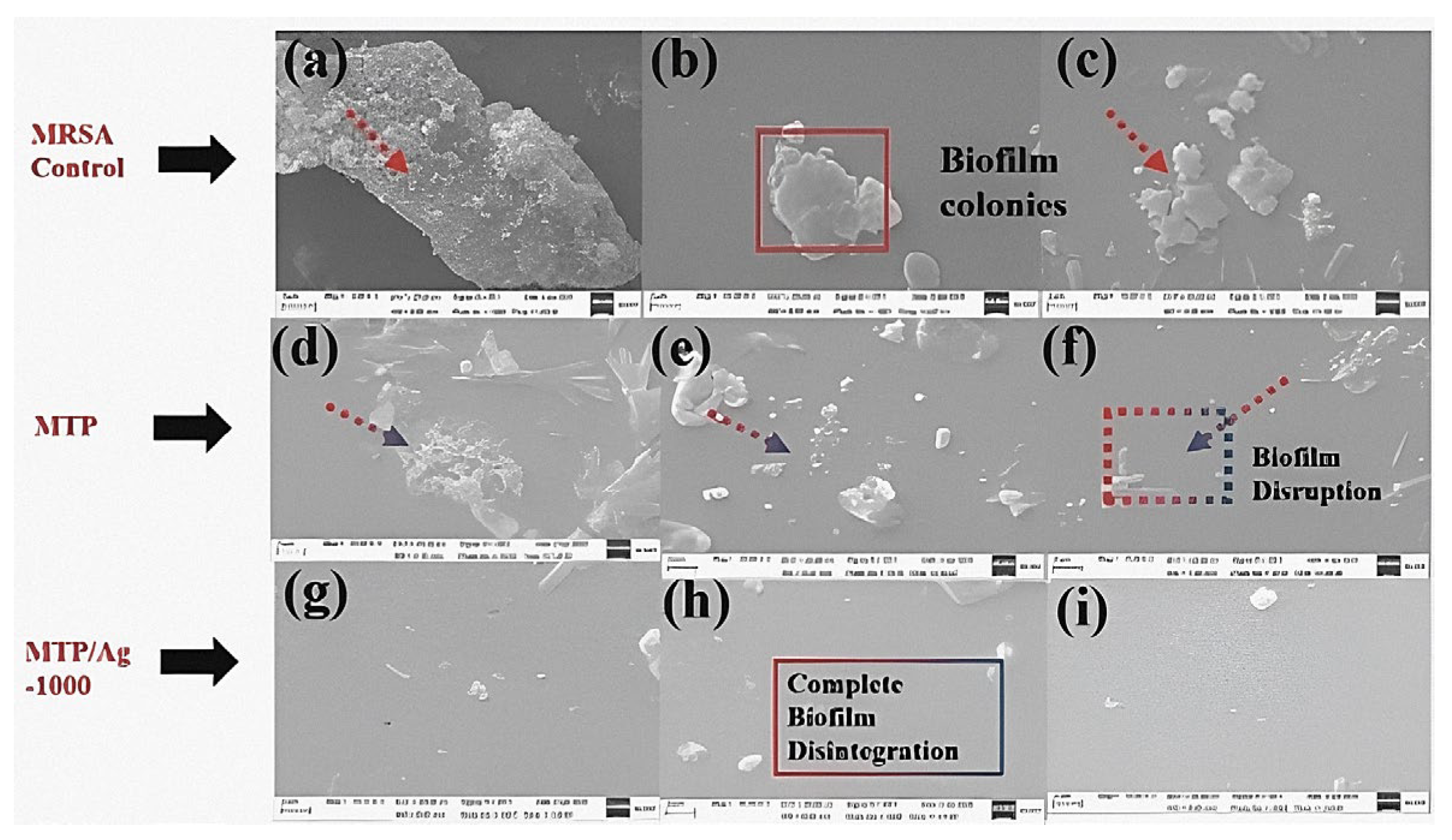
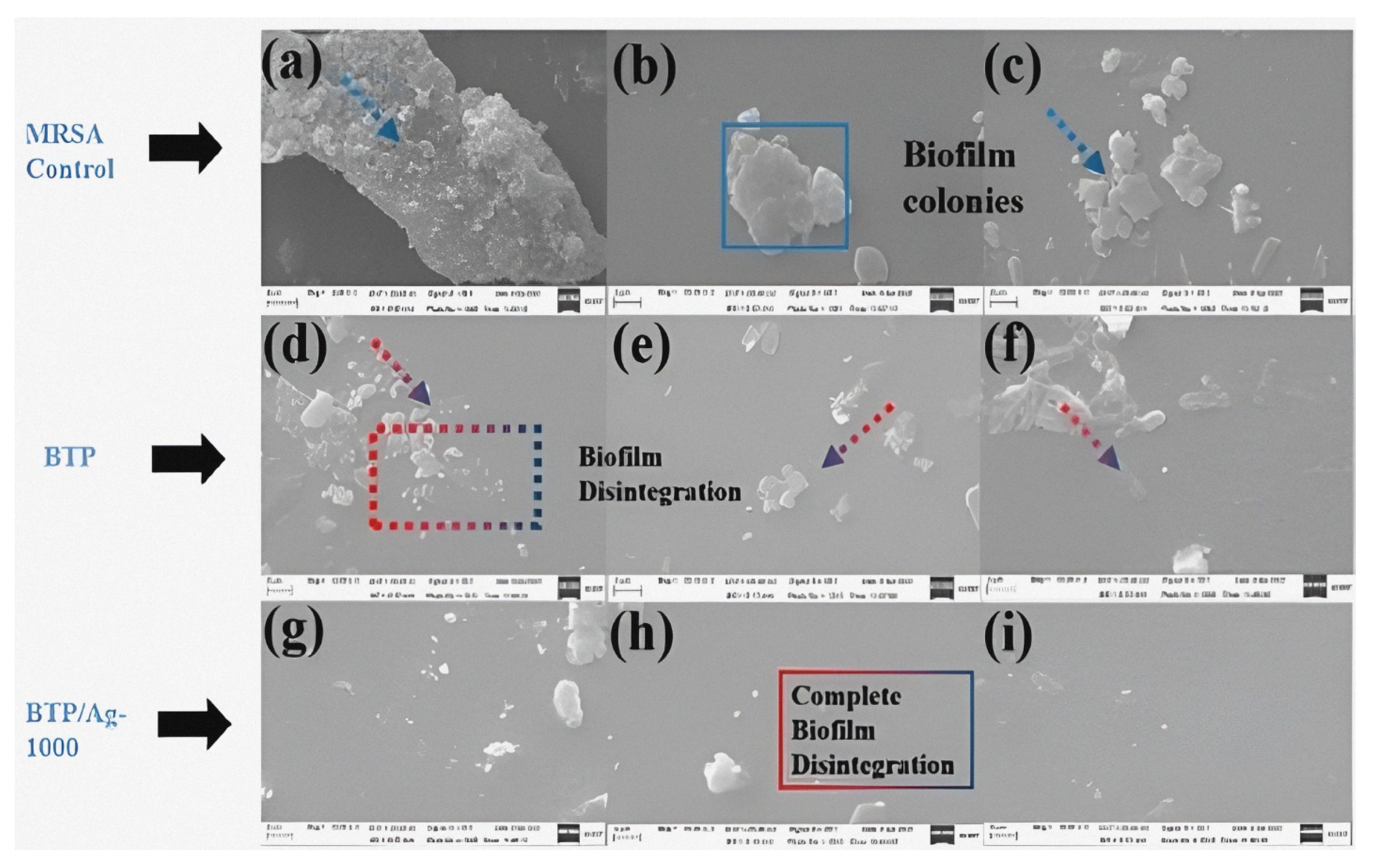
3.2.5. Morphological Imaging of Treated MRSA (ATCC-43300)
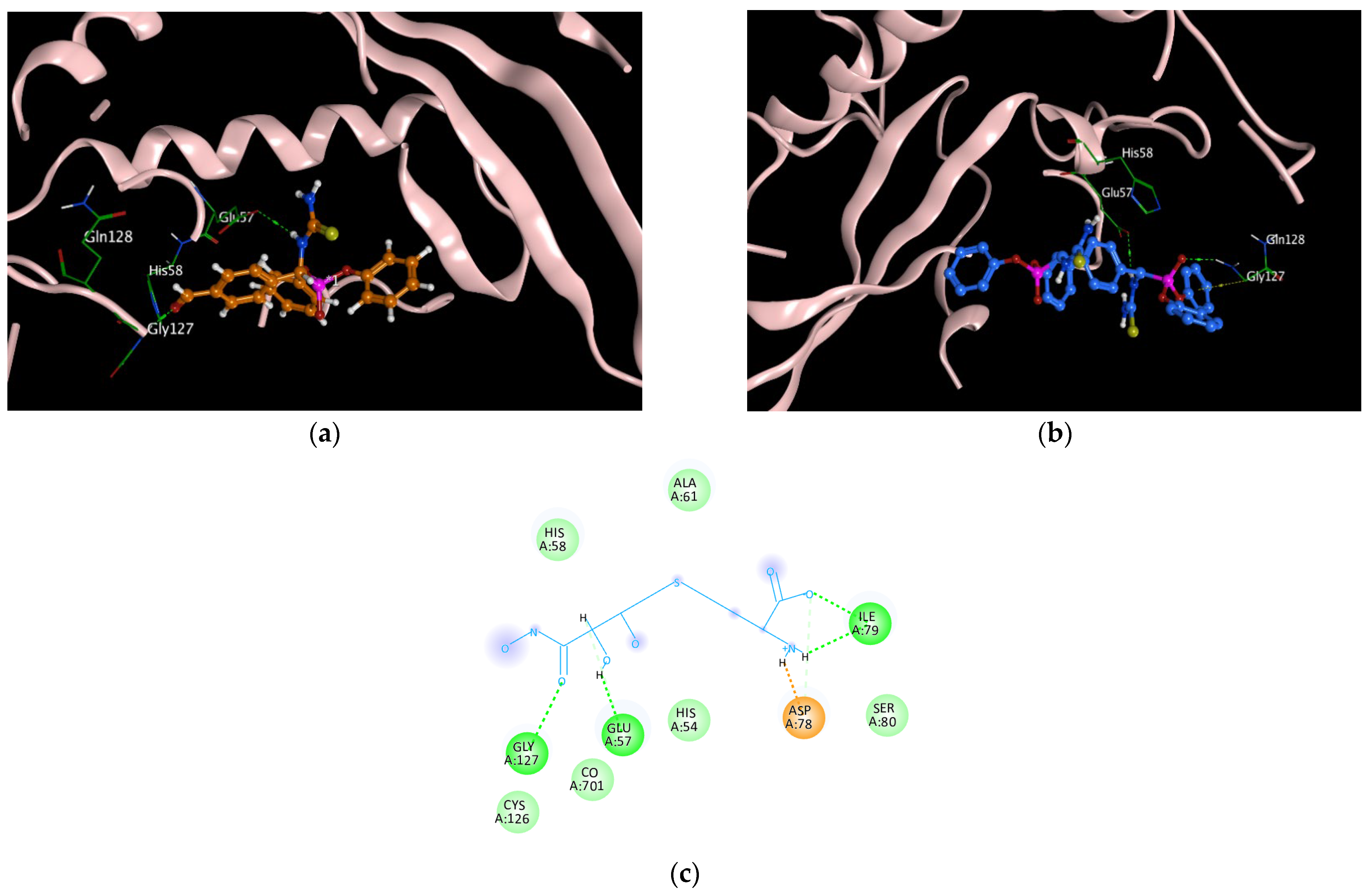
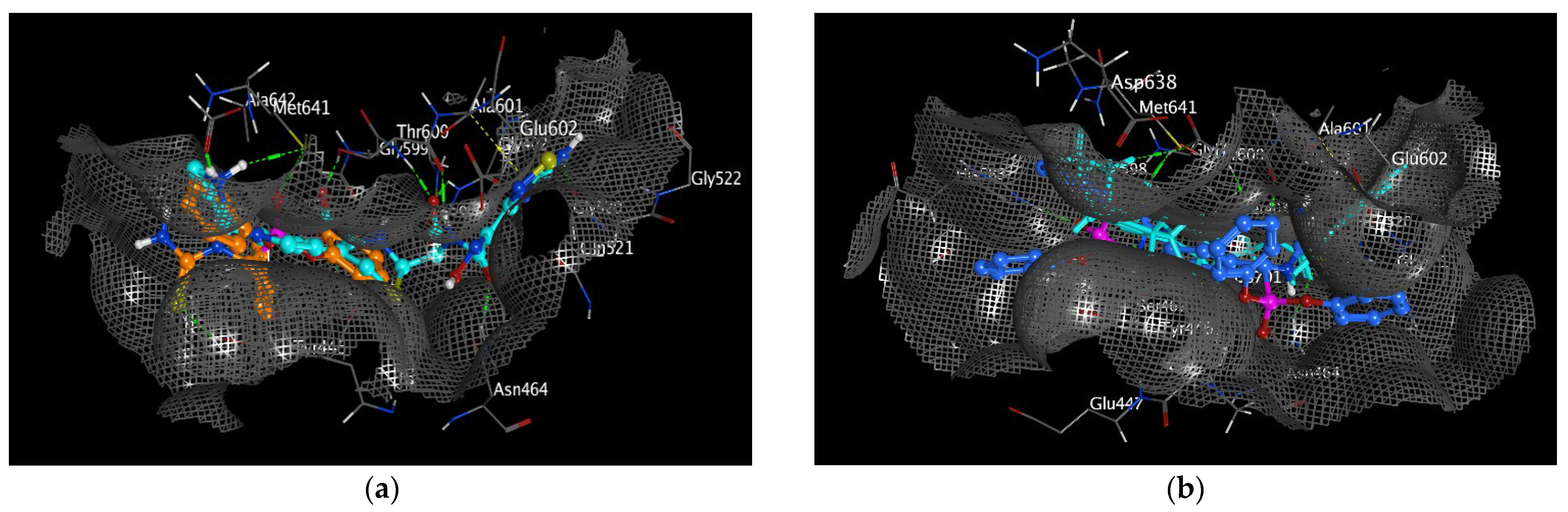
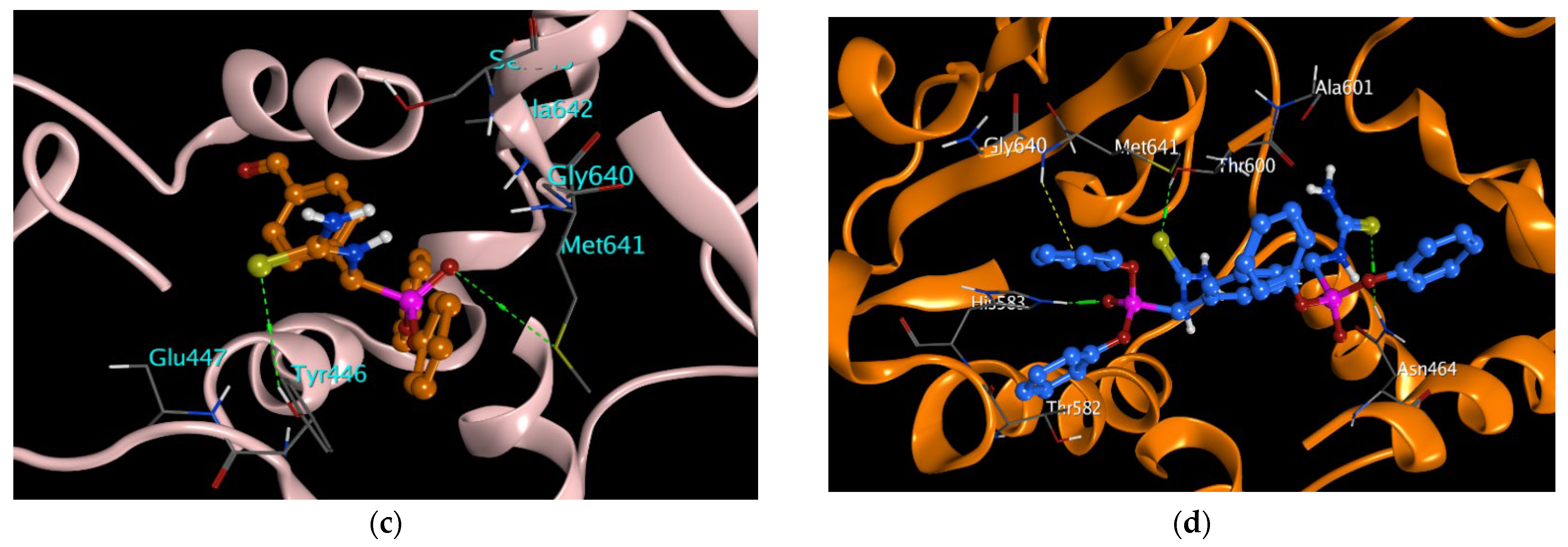
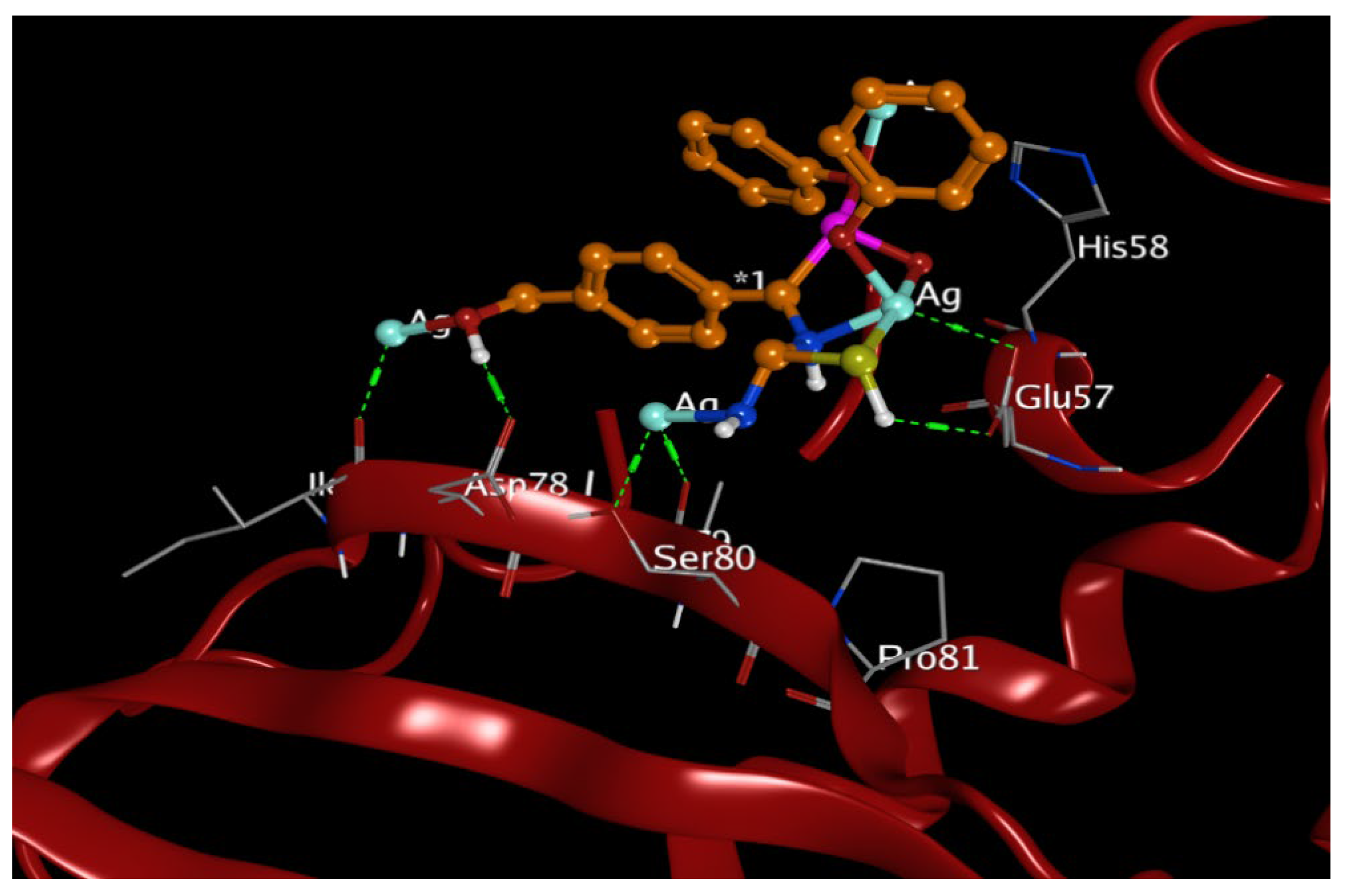
3.3. Molecular Docking Study
3.4. In Silico Pharmacokinetics Investigation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.J.T.L. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Larsson, D.J.; Flach, C. Antibiotic resistance in the environment. Nat. Rev. Microbiol. 2022, 20, 257–269. [Google Scholar] [CrossRef] [PubMed]
- Yadav, H.; Mahalvar, A.; Pradhan, M.; Yadav, K.; Sahu, K.K.; Yadav, R. Exploring the potential of phytochemicals and nanomaterial: A boon to antimicrobial treatment. Med. Drug Discov. 2023, 17, 100151. [Google Scholar] [CrossRef]
- Mirzaei, R.; Ranjbar, R. Hijacking host components for bacterial biofilm formation: An advanced mechanism. Int. Immunopharmacol. 2022, 103, 108471. [Google Scholar] [CrossRef]
- Goel, N.; Hashmi, Z.; Khan, N.; Ahmad, R.; Khan, W.H. Recent Strategies to Combat Multidrug Resistance. In Non-Traditional Approaches to Combat Antimicrobial Drug Resistance; Springer: Berlin/Heidelberg, Germany, 2023; pp. 1–27. [Google Scholar] [CrossRef]
- Singh, R.; Dutt, S.; Sharma, P.; Sundramoorthy, A.K.; Dubey, A.; Singh, A.; Arya, S. Future of Nanotechnology in Food Industry: Challenges in Processing, Packaging, and Food Safety. Glob. Chall. 2023, 7, 2200209. [Google Scholar] [CrossRef] [PubMed]
- Sinha, A.; Simnani, F.Z.; Singh, D.; Nandi, A.; Choudhury, A.; Patel, P.; Jha, E.; Kaushik, N.K.; Mishra, Y.K.; Panda, P. The translational paradigm of nanobiomaterials: Biological chemistry to modern applications. Mater. Today Bio 2022, 17, 100463. [Google Scholar] [CrossRef]
- Sun, Y.; Waterhouse, G.I.; Qiao, X.; Xiao, J.; Xu, Z. Determination of chloramphenicol in food using nanomaterial-based electrochemical and optical sensors—A review. Food Chem. 2023, 410, 135434. [Google Scholar] [CrossRef]
- Xia, K.; Yamaguchi, K.; Suzuki, K. Recent Advances in Hybrid Materials of Metal Nanoparticles and Polyoxometalates. Angew. Chem. Int. Ed. Engl. 2023, 62, e202214506. [Google Scholar] [CrossRef] [PubMed]
- Farooq, U.; Ahmad, T.; Naaz, F.; Islam, S. Review on Metals and Metal Oxides in Sustainable Energy Production: Progress and Perspectives. Energy Fuels 2023, 37, 1577–1632. [Google Scholar] [CrossRef]
- Frei, A.; Verderosa, A.D.; Elliott, A.G.; Zuegg, J.; Blaskovich, M. Metals to combat antimicrobial resistance. Nat. Rev. Chem. 2023, 7, 202–224. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.R.; Wu, Y.; El-Sayed, M. Gold-nanoparticle-assisted plasmonic photothermal therapy advances toward clinical application. Nanomedicine 2019, 123, 15375–15393. [Google Scholar] [CrossRef]
- Chandrakala, V.; Aruna, V.; Angajala, G. Review on metal nanoparticles as nanocarriers: Current challenges and perspectives in drug delivery systems. Emergent Mater. 2022, 5, 1593–1615. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Xiang, J.; Wang, B.; Chen, L.; Tan, S. Recent advances in the development of noble metal NPs for cancer therapy. Bioinorg. Chem. Appl. 2022, 2022, 2444516. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Zhou, S.; Gao, F.; Lin, J.; Liu, J.; Zheng, J. DNA-mediated growth of noble metal nanomaterials for biosensing applications. TrAC Trends Anal. Chem. 2022, 148, 116533. [Google Scholar] [CrossRef]
- González-Pedroza, M.G.; Benítez, A.R.T.; Navarro-Marchal, S.A.; Martínez-Martínez, E.; Marchal, J.A.; Boulaiz, H.; Morales-Luckie, R. Biogeneration of silver nanoparticles from Cuphea procumbens for biomedical and environmental applications. Sci. Rep. 2023, 13, 790. [Google Scholar] [CrossRef]
- Napagoda, M.; Wijayaratne, G.B.; Witharana, S. Applications of Nanotechnology in Dermatology. In Nanotechnology in Modern Medicine; Springer: Berlin/Heidelberg, Germany, 2022; pp. 135–168. [Google Scholar] [CrossRef]
- Joshi, A.S.; Singh, P.; Mijakovic, I. Interactions of gold and silver nanoparticles with bacterial biofilms: Molecular interactions behind inhibition and resistance. Int. J. Mol. Sci. 2020, 21, 7658. [Google Scholar] [CrossRef]
- Terzioğlu, E.; Arslan, M.; Balaban, B.G.; Çakar, Z. Microbial silver resistance mechanisms: Recent developments. World J. Microbiol. Biotechnol. 2022, 38, 158. [Google Scholar] [CrossRef]
- Akter, M.; Sikder, M.T.; Rahman, M.M.; Ullah, A.A.; Hossain, K.F.B.; Banik, S.; Hosokawa, T.; Saito, T.; Kurasaki, M. A systematic review on silver nanoparticles-induced cytotoxicity: Physicochemical properties and perspectives. J. Adv. Res. 2018, 9, 1–16. [Google Scholar] [CrossRef]
- Malik, M.; Iqbal, M.A.; Iqbal, Y.; Malik, M.; Bakhsh, S.; Irfan, S.; Ahmad, R.; Pham, P. Biosynthesis of silver nanoparticles for biomedical applications: A mini review. Inorg. Chem. Commun. 2022, 145, 109980. [Google Scholar] [CrossRef]
- Attia, N.F.; Moussa, M.; Sheta, A.M.; Taha, R.; Gamal, H. Synthesis of effective multifunctional textile based on silica nanoparticles. Prog. Org. Coat. 2017, 106, 41–49. [Google Scholar] [CrossRef]
- Attia, N.F.; Eid, A.M.; Soliman, M.A.; Nagy, M. Exfoliation and decoration of graphene sheets with silver nanoparticles and their antibacterial properties. J. Polym. Environ. 2018, 26, 1072–1077. [Google Scholar] [CrossRef]
- Dallas, P.; Sharma, V.K.; Zboril, R. polymeric nanocomposites as advanced antimicrobial agents: Classification, synthetic paths, applications, and perspectives. Adv. Colloid. Interface Sci. 2011, 166, 119–135. [Google Scholar] [CrossRef]
- Li, S.; Mu, B.; Zhang, H.; Kang, Y.; Wang, A. Incorporation of silver nanoparticles/curcumin/clay minerals into chitosan film for enhancing mechanical properties, antioxidant and antibacterial activity. Int. J. Biol. Macromol. 2022, 223, 779–789. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, A.M.; Hassan, K.T.; Hassan, O. Assessment of antimicrobial activity of chitosan/silver nanoparticles hydrogel and cryogel microspheres. Int. J. Biol. Macromol. 2023, 233, 123580. [Google Scholar] [CrossRef]
- Ren, R.; Lim, C.; Li, S.; Wang, Y.; Song, J.; Lin, T.-W.; Muir, B.W.; Hsu, H.-Y.; Shen, H.-H.J.N. Recent Advances in the Development of Lipid-, Metal-, Carbon-, and Polymer-Based Nanomaterials for Antibacterial Applications. Nanomaterials 2022, 12, 3855. [Google Scholar] [CrossRef] [PubMed]
- Yousefi, M.; Ehsani, A.; Jafari, S. Lipid-based nano delivery of antimicrobials to control food-borne bacteria. Adv. Colloid. Interface Sci. 2019, 270, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, V.; Chauhan, P.S.; Tomar, R. Bio-Fabrication of metal nanoparticles: A review. Int. J. Curr. Res. Life Sci. 2018, 7, 1927–1932. [Google Scholar]
- Mao, H.; Zhu, K.; Liu, X.; Yao, C.; Kobayashi, M. Facile synthetic route to Fe3O4/silica nanocomposites pillared clay through cationic surfactant-aliphatic acid mixed system and application for magnetically controlled drug release. Microporous Mesoporous Mater. 2016, 225, 216–223. [Google Scholar] [CrossRef]
- Zhou, R.; Gao, H. Cytotoxicity of graphene: Recent advances and future perspective. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2014, 6, 452–474. [Google Scholar] [CrossRef]
- Wang, Z.; Sun, C.; Yang, K.; Chen, X.; Wang, R. Cucurbituril-Based Supramolecular Polymers for Biomedical Applications. Angew. Chem. Int. Ed. Engl. 2022, 61, e202206763. [Google Scholar] [CrossRef]
- Gurunathan, S.; Kim, J.H. Synthesis, toxicity, biocompatibility, and biomedical applications of graphene and graphene-related materials. Int. J. Nanomed. 2016, 11, 1927–1945. [Google Scholar] [CrossRef] [PubMed]
- Amira, A.; Aouf, Z.; K’tir, H.; Chemam, Y.; Ghodbane, R.; Zerrouki, R.; Aouf, N.-E. Recent Advances in the Synthesis of α-Aminophosphonates: A Review. ChemistrySelect 2021, 6, 6137–6149. [Google Scholar] [CrossRef]
- Keri, R.; Patil, M.; Brahmkhatri, V.P.; Budagumpi, S.; Adimule, V. Copper (II)-β-Cyclodextrin Promoted Kabachnik-Fields Reaction: An Efficient, One-Pot Synthesis of α-Aminophosphonates. Top. Catal. 2022. [Google Scholar] [CrossRef]
- Neiber, R.R.; Galhoum, A.A.; El-Tantawy El Sayed, I.; Guibal, E.; Xin, J.; Lu, X. Selective lead (II) sorption using aminophosphonate-based sorbents: Effect of amine linker, characterization and sorption performance. Chem. Eng. J. 2022, 442, 136300. [Google Scholar] [CrossRef]
- Fouda, S.R.; El-Sayed, I.E.; Attia, N.F.; Abdeen, M.M.; Abdel Aleem, A.A.H.; Nassar, I.F.; Mira, H.I.; Gawad, E.A.; Kalam, A.; Al-Ghamdi, A.A.; et al. Mechanistic study of Hg(II) interaction with three different α-aminophosphonate adsorbents: Insights from batch experiments and theoretical calculations. Chemosphere 2022, 304, 135253. [Google Scholar] [CrossRef] [PubMed]
- Galhoum, A.A.; Elshehy, E.A.; Tolan, D.A.; El-Nahas, A.M.; Taketsugu, T.; Nishikiori, K.; Akashi, T.; Morshedy, A.S.; Guibal, E. Synthesis of polyaminophosphonic acid-functionalized poly(glycidyl methacrylate) for the efficient sorption of La(III) and Y(III). Chem. Eng. J. 2019, 375, 121932. [Google Scholar] [CrossRef]
- Imam, E.A.; Hashem, A.I.; Tolba, A.A.; Mahfouz, M.G.; El-Sayed, I.E.-T.; El-Tantawy, A.I.; Galhoum, A.A.; Guibal, E. Effect of mono-vs. bi-functionality of aminophosphonate derivatives on the enhancement of U (VI) sorption: Physicochemical properties and sorption performance. J. Environ. Chem. Eng. 2023, 11, 109951. [Google Scholar] [CrossRef]
- Sipyagina, N.A.; Malkova, A.N.; Straumal, E.A.; Yurkova, L.L.; Baranchikov, A.E.; Ivanov, V.K.; Lermontov, S.A. Novel aminophosphonate ligand for the preparation of catalytically active silica aerogels with finely dispersed palladium. J. Porous Mater. 2023, 30, 449–457. [Google Scholar] [CrossRef]
- Delehedde, C.; Culcasi, M.; Ricquebourg, E.; Cassien, M.; Siri, D.; Blaive, B.; Pietri, S.; Thétiot-Laurent, S. Novel Sterically Crowded and Conformationally Constrained α-Aminophosphonates with a Near-Neutral pKa as Highly Accurate 31P NMR pH Probes. Application to Subtle pH Gradients Determination in Dictyostelium discoideum. Cells 2022, 27, 4506. [Google Scholar]
- Silva, V.B.; Santos, Y.H.; Hellinger, R.; Mansour, S.; Delaune, A.; Legros, J.; Zinoviev, S.; Nogueira, E.S.; Orth, E.S. Organophosphorus chemical security from a peaceful perspective: Sustainable practices in its synthesis, decontamination and detection. Green. Chem. 2022, 24, 585–613. [Google Scholar] [CrossRef]
- Nikitin, E.; Shumatbaev, G.; Terenzhev, D.; Sinyashin, K.O.; Kazimova, K. New α-Aminophosphonates as Corrosion Inhibitors for Oil and Gas Pipelines Protection. Civ. Eng. J. 2019, 5, 963–970. [Google Scholar] [CrossRef]
- Aissa, R.; Guezane-Lakoud, S.; Toffano, M.; Gali, L.; Aribi-Zouioueche, L. Fiaud’s Acid, a novel organocatalyst for diastereoselective bis α-aminophosphonates synthesis with in-vitro biological evaluation of antifungal, antioxidant and enzymes inhibition potential. Bioorganic Med. Chem. Lett. 2021, 41, 128000. [Google Scholar] [CrossRef]
- Elsherbiny, D.A.; Abdelgawad, A.M.; El-Naggar, M.E.; El-Sherbiny, R.A.; El-Rafie, M.H.; El-Sayed, I.E.-T. Synthesis, antimicrobial activity, and sustainable release of novel α-aminophosphonate derivatives loaded carrageenan cryogel. Int. J. Biol. Macromol. 2020, 163, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Boshta, N.M.; Elgamal, E.A.; El-Sayed, I.E.T. Bioactive amide and α-aminophosphonate inhibitors for methicillin-resistant Staphylococcus aureus (MRSA). Monatsh. Chem. 2018, 149, 2349–2358. [Google Scholar] [CrossRef]
- Joossens, J.; Ali, O.M.; El-Sayed, I.; Surpateanu, G.; Van der Veken, P.; Lambeir, A.-M.; Setyono-Han, B.; Foekens, J.A.; Schneider, A.; Schmalix, W.; et al. Small, Potent, and Selective Diaryl Phosphonate Inhibitors for Urokinase-Type Plasminogen Activator with In Vivo Antimetastatic Properties. J. Med. Chem. 2007, 50, 6638–6646. [Google Scholar] [CrossRef]
- Saleh, N.M.; Moemen, Y.S.; Mohamed, S.H.; Fathy, G.; Ahmed, A.A.S.; Al-Ghamdi, A.A.; Ullah, S.; El Sayed, I.E. Experimental and Molecular Docking Studies of Cyclic Diphenyl Phosphonates as DNA Gyrase Inhibitors for Fluoroquinolone-Resistant Pathogens. Antibiotics. 2022, 11, 53. [Google Scholar] [CrossRef]
- Sharaf, A.; Ragab, S.S.; Elbarbary, A.A.; Shaban, E.; El Sayed, I.E.T. Synthesis and biological evaluation of some 3H-quinazolin-4-one derivatives. J. Iran. Chem. Soc. 2022, 19, 291–302. [Google Scholar] [CrossRef]
- Attia, N.F.; Morsy, M.S. Facile synthesis of novel nanocomposite as antibacterial and flame retardant material for textile fabrics. Mater. Chem. Phys. 2016, 180, 364–372. [Google Scholar] [CrossRef]
- Alshehri, L.A.; Attia, N.F. Reinforcement and Antibacterial Properties of Hand Embroidery Threads Based on Green Nanocoatings. Coatings 2023, 13, 747. [Google Scholar] [CrossRef]
- Ayad, M.M.; Amer, W.A.; Kotp, M.G.; Minisy, I.M.; Rehab, A.F.; Kopecký, D.; Fitl, P. Synthesis of silver-anchored polyaniline–chitosan magnetic nanocomposite: A smart system for catalysis. RSC Adv. 2017, 7, 18553–18560. [Google Scholar] [CrossRef]
- Vilar, S.; Cozza, G.; Moro, S. Medicinal chemistry and the molecular operating environment (MOE): Application of QSAR and molecular docking to drug discovery. Curr. Top. Med. Chem. 2008, 8, 1555–1572. [Google Scholar] [CrossRef] [PubMed]
- Lovering, A.L.; Gretes, M.C.; Safadi, S.S.; Danel, F.; de Castro, L.; Page, M.G.P.; Strynadka, N.C.J. Structural Insights into the Anti-methicillin-resistant Staphylococcus aureus (MRSA) Activity of Ceftobiprole. J. Biol. Chem. 2012, 287, 32096–32102. [Google Scholar] [CrossRef] [PubMed]
- Shen, G.; Rajan, R.; Zhu, J.; Bell, C.E.; Pei, D. Design and Synthesis of Substrate and Intermediate Analogue Inhibitors of S-Ribosylhomocysteinase. J. Med. Chem. 2006, 49, 3003–3011. [Google Scholar] [CrossRef] [PubMed]
- Zhong, W.; Pasunooti, K.K.; Balamkundu, S.; Wong, Y.H.; Nah, Q.; Gadi, V.; Gnanakalai, S.; Chionh, Y.H.; McBee, M.E.; Gopal, P.; et al. Thienopyrimidinone Derivatives That Inhibit Bacterial tRNA (Guanine37-N(1))-Methyltransferase (TrmD) by Restructuring the Active Site with a Tyrosine-Flipping Mechanism. J. Med. Chem. 2019, 62, 7788–7805. [Google Scholar] [CrossRef]
- Lunelli, M.; Hurwitz, R.; Lambers, J.; Kolbe, M. Crystal structure of PrgI-SipD: Insight into a secretion competent state of the type three secretion system needle tip and its interaction with host ligands. PLoS Pathog. 2011, 7, e1002163. [Google Scholar] [CrossRef]
- Elmongy, E.I.; Altwaijry, N.; Attallah, N.G.M.; AlKahtani, M.M.; Henidi, H.A. In-Silico Screening of Novel Synthesized Thienopyrimidines Targeting Fms Related Receptor Tyrosine Kinase-3 and Their In-Vitro Biological Evaluation. Pharmaceuticals 2022, 15, 170. [Google Scholar] [CrossRef]
- Elmongy, E.I.; Ahmed, A.A.S.; El Sayed, I.E.T.; Fathy, G.; Awad, H.M.; Salman, A.U.; Hamed, M.A. Synthesis, Biocidal and Antibiofilm Activities of New Isatin–Quinoline Conjugates against Multidrug-Resistant Bacterial Pathogens along with Their In Silico Screening. Antibiotics 2022, 11, 1507. [Google Scholar] [CrossRef]
- Attia, N.F.; Lee, S.M.; Kim, H.J.; Geckeler, K.E. Preparation of polypyrrole nanoparticles and their composites: Effect of electronic properties on hydrogen adsorption. Polym. Int. 2015, 64, 696–703. [Google Scholar] [CrossRef]
- Ogundare, S.A.; Muungani, G.; Amaku, J.F.; Ogunmoye, A.O.; Adesetan, T.O.; Olubomehin, O.O.; Ibikunle, A.A.; van Zyl, W.E. Mangifera indica L. stem bark used in the bioinspired formation of silver nanoparticles: Catalytic and antibacterial applications. Chem. Zvesti 2023, 77, 2647–2656. [Google Scholar] [CrossRef]
- Eisa, W.H.; Zayed, M.F.; Anis, B.; Abbas, L.M.; Ali, S.S.M.; Mostafa, A.M. Clean production of powdery silver nanoparticles using Zingiber officinale: The structural and catalytic properties. J. Clean. Prod. 2019, 241, 118398. [Google Scholar] [CrossRef]
- Rather, M.A.; Deori, P.J.; Gupta, K.; Daimary, N.; Deka, D.; Qureshi, A.; Dutta, T.K.; Joardar, S.N.; Mandal, M. Ecofriendly phytofabrication of silver nanoparticles using aqueous extract of Cuphea carthagenensis and their antioxidant potential and antibacterial activity against clinically important human pathogens. Chemosphere 2022, 300, 134497. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ansari, M.F.; Lin, J.-M.; Zhou, C.-H. Design and Synthesis of Sulfanilamide Aminophosphonates as Novel Antibacterial Agents towards Escherichia coli. Chin. J. Chem. 2021, 39, 2251–2263. [Google Scholar] [CrossRef]
- Yang, X.-C.; Zeng, C.-M.; Avula, S.R.; Peng, X.-M.; Geng, R.-X.; Zhou, C. Novel coumarin aminophosphonates as potential multitargeting antibacterial agents against Staphylococcus aureus. Eur. J. Med. Chem. 2023, 245, 114891. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Mishra, P. Bacitracin and isothiocyanate functionalized silver nanoparticles for synergistic and broad spectrum antibacterial and antibiofilm activity with selective toxicity to bacteria over mammalian cells. Adv. Biomater. 2022, 133, 112649. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Salcedo, S.; García, A.; González-Jiménez, A.; Vallet-Regí, M.J.A.B. Antibacterial effect of 3D printed mesoporous bioactive glass scaffolds doped with metallic silver nanoparticles. Acta Biomater. 2023, 155, 654–666. [Google Scholar] [CrossRef]
- Oh, J.K.; Yegin, Y.; Yang, F.; Zhang, M.; Li, J.; Huang, S.; Verkhoturov, S.V.; Schweikert, E.A.; Perez-Lewis, K.; Scholar, E. The influence of surface chemistry on the kinetics and thermodynamics of bacterial adhesion. Sci. Rep. 2018, 8, 17247. [Google Scholar] [CrossRef]
- Abu Jarad, N.; Rachwalski, K.; Bayat, F.; Khan, S.; Shakeri, A.; MacLachlan, R.; Villegas, M.; Brown, E.D.; Hosseinidoust, Z.; Didar, T.F.; et al. A Bifunctional Spray Coating Reduces Contamination on Surfaces by Repelling and Killing Pathogens. ACS Appl. Mater. Interfaces 2023, 15, 16253–16265. [Google Scholar] [CrossRef]
- Monserud, J.H.; Schwartz, D.K. Effects of molecular size and surface hydrophobicity on oligonucleotide interfacial dynamics. Biomacromolecules 2012, 13, 4002–4011. [Google Scholar] [CrossRef]
- Cui, Q.; Bian, R.; Xu, F.; Li, Q.; Wang, W.; Bian, Q. Chapter 10—New molecular entities and structure–activity relationships of drugs designed by the natural product derivatization method from 2010 to 2018. In Studies in Natural Products Chemistry; Atta ur, R., Ed.; Elsevier: Amsterdam, The Netherlands, 2021; Volume 69, pp. 371–415. [Google Scholar] [CrossRef]
- Sahli, C.; Moya, S.E.; Lomas, J.S.; Gravier-Pelletier, C.; Briandet, R.; Hémadi, M. Recent advances in nanotechnology for eradicating bacterial biofilm. Theranostics 2022, 12, 2383–2405. [Google Scholar] [CrossRef]
- Borse, A.; Shinde, N.; Bhosale, S.K. Dipeptide Conjugates: An Important Class of Therapeutic Agents. Indian J. Pharm. Educ. Res. 2023, 57, 15–21. [Google Scholar] [CrossRef]
- Cella, M.A.; Coulson, T.; MacEachern, S.; Badr, S.; Ahmadi, A.; Tabatabaei, M.S.; Labbe, A.; Griffiths, M.W.J.S.R. Probiotic disruption of quorum sensing reduces virulence and increases cefoxitin sensitivity in methicillin-resistant Staphylococcus aureus. Sci. Rep. 2023, 13, 4373. [Google Scholar] [CrossRef] [PubMed]
- Jan, B.; Jan, R.; Afzal, S.; Ayoub, M.; Masoodi, M.H. Treatment Strategies to Combat Multidrug Resistance (MDR) in Bacteria. In Non-Traditional Approaches to Combat Antimicrobial Drug Resistance; Springer: Berlin/Heidelberg, Germany, 2023; pp. 79–100. [Google Scholar] [CrossRef]
- Li, D.; Bheemanaboina, R.R.Y.; Battini, N.; Tangadanchu, V.K.R.; Fang, X.F.; Zhou, C.H. Novel organophosphorus aminopyrimidines as unique structural DNA-targeting membrane active inhibitors towards drug-resistant methicillin-resistant Staphylococcus aureus. MedChemComm 2018, 9, 1529–1537. [Google Scholar] [CrossRef] [PubMed]
- McNeilly, O.; Mann, R.; Hamidian, M.; Gunawan, C. Emerging Concern for Silver Nanoparticle Resistance in Acinetobacter baumannii and Other Bacteria. Front. Microbiol. 2021, 12, 652863. [Google Scholar] [CrossRef]
- Wu, J.; Li, F.; Hu, X.; Lu, J.; Sun, X.; Gao, J.; Ling, D. Responsive Assembly of Silver Nanoclusters with a Biofilm Locally Amplified Bactericidal Effect to Enhance Treatments against Multi-Drug-Resistant Bacterial Infections. ACS Cent. Sci. 2019, 5, 1366–1376. [Google Scholar] [CrossRef]
- Wang, J.; Li, J.; Guo, G.; Wang, Q.; Tang, J.; Zhao, Y.; Qin, H.; Wahafu, T.; Shen, H.; Liu, X. Silver-nanoparticles-modified biomaterial surface resistant to staphylococcus: New insight into the antimicrobial action of silver. Sci. Rep. 2016, 6, 32699. [Google Scholar] [CrossRef] [PubMed]
- Karthik, C.S.; Chethana, M.H.; Manukumar, H.M.; Ananda, A.P.; Sandeep, S.; Nagashree, S.; Mallesha, L.; Mallu, P.; Jayanth, H.S.; Dayananda, B.P. Synthesis and characterization of chitosan silver nanoparticle decorated with benzodioxane coupled piperazine as an effective anti-biofilm agent against MRSA: A validation of molecular docking and dynamics. Int. J. Biol. Macromol. 2021, 181, 540–551. [Google Scholar] [CrossRef]
- Majumdar, M.; Khan, S.A.; Biswas, S.C.; Roy, D.N.; Panja, A.S.; Misra, T.K. In vitro and in silico investigation of anti-biofilm activity of Citrus macroptera fruit extract mediated silver nanoparticles. J. Mol. Liq. 2020, 302, 112586. [Google Scholar] [CrossRef]
- Duanis-Assaf, D.; Steinberg, D.; Chai, Y.; Shemesh, M. The LuxS Based Quorum Sensing Governs Lactose Induced Biofilm Formation by Bacillus subtilis. Front. Microbiol. 2015, 6, 1517. [Google Scholar] [CrossRef]
- Attia, N.F.; Mohamed, A.; Hussein, A.; El-Demerdash, A.-G.M.; Kandil, S. Bio-inspired one-dimensional based textile fabric coating for integrating high flame retardancy, antibacterial, toxic gases suppression, antiviral and reinforcement properties. Polym. Degrad. Stab. 2022, 205, 110152. [Google Scholar] [CrossRef]
- Sharma, C.; Dhiman, R.; Rokana, N.; Panwar, H. Nanotechnology: An untapped resource for food packaging. Front. Microbiol. 2017, 8, 1735. [Google Scholar] [CrossRef]
- Attia, N. Nanoporous carbon doped with metal oxide microsphere as renewable flame retardant for integrating high flame retardancy and antibacterial properties of thermoplastic polymer composites. J. Therm. Anal. Calorim. 2023, 148, 5335–5346. [Google Scholar] [CrossRef]
- Pires, D.E.; Blundell, T.L.; Ascher, D. pkCSM: Predicting small-molecule pharmacokinetic and toxicity properties using graph-based signatures. J. Med. Chem. 2015, 58, 4066–4072. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, D.; Lennernäs, H. Intestinal permeability and drug absorption: Predictive experimental, computational and in vivo approaches. Pharmaceutics 2019, 11, 411. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Zhang, J.; Hu, C.Q.; Zhang, X.; Ma, B.; Zhang, P. In silico ADME and toxicity prediction of ceftazidime and its impurities. Front. Pharmacol. 2019, 10, 434. [Google Scholar] [CrossRef]
- Daoud, A.; Malika, D.; Bakari, S.; Hfaiedh, N.; Mnafgui, K.; Kadri, A.; Gharsallah, N. Assessment of polyphenol composition, antioxidant and antimicrobial properties of various extracts of Date Palm Pollen (DPP) from two Tunisian cultivars. Arab. J. Chem. 2019, 12, 3075–3086. [Google Scholar] [CrossRef]
- Eloff, J.N. A Sensitive and Quick Microplate Method to Determine the Minimal Inhibitory Concentration of Plant Extracts for Bacteria. Planta Medica 1998, 64, 711–713. [Google Scholar] [CrossRef]
- Ozturk, S.; Ercisli, S. Chemical composition and in vitro antibacterial activity of Seseli libanotis. World J. Microbiol. Biotechnol. 2006, 22, 261–265. [Google Scholar] [CrossRef]
- Poonacha, N.; Nair, S.; Desai, S.; Tuppad, D.; Hiremath, D.; Mohan, T.; Vipra, A.; Sharma, U. Efficient Killing of Planktonic and Biofilm-Embedded Coagulase-Negative Staphylococci by Bactericidal Protein P128. Antimicrob. Agents Chemother. 2017, 61, e00457-17. [Google Scholar] [CrossRef]
- Kemung, H.M.; Tan, L.T.-H.; Khaw, K.Y.; Ong, Y.S.; Chan, C.K.; Low, D.Y.S.; Tang, S.Y.; Goh, B.-H. An Optimized Anti-adherence and Anti-biofilm Assay: Case Study of Zinc Oxide Nanoparticles versus MRSA Biofilm. Prog. Microbes Mol. Biol. 2020, 3. [Google Scholar] [CrossRef]
- O’Toole, G.A. Microtiter dish biofilm formation assay. J. Vis. Exp. 2011, e2437. [Google Scholar]
- Badger-Emeka, L.I.; Emeka, P.M.; Ibrahim, H.I.M. A Molecular Insight into the Synergistic Mechanism of Nigella sativa (Black Cumin) with β-Lactam Antibiotics against Clinical Isolates of Methicillin-Resistant Staphylococcus aureus. Appl. Sci. 2021, 11, 3206. [Google Scholar] [CrossRef]
- Sebastian, D. Characterization of Green Synthesized Antibacterial Silver Nanoparticles from Amaranthus spinosus L. Extract. BioNanoScience 2022, 12, 502–511. [Google Scholar]
- Ramzan, M.; Karobari, M.I.; Heboyan, A.; Mohamed, R.N.; Mustafa, M.; Basheer, S.N.; Desai, V.; Batool, S.; Ahmed, N.; Zeshan, B. Synthesis of Silver Nanoparticles from Extracts of Wild Ginger (Zingiber zerumbet) with Antibacterial Activity against Selective Multidrug Resistant Oral Bacteria. Molecules 2022, 27, 2007. [Google Scholar] [CrossRef]
- Bezza, F.A.; Tichapondwa, S.M.; Chirwa, E.M. Synthesis of biosurfactant stabilized silver nanoparticles, characterization and their potential application for bactericidal purposes. J. Hazard. Mater. 2020, 393, 122319. [Google Scholar] [CrossRef] [PubMed]
- Alsakhawy, S.A.; Baghdadi, H.H.; El-Shenawy, M.A.; El-Hosseiny, L.S. Antibacterial Activity of Silver Nanoparticles Phytosynthesized by Citrus Fruit Peel Extracts. BioNanoScience 2022, 12, 1106–1115. [Google Scholar] [CrossRef]
- Hamida, R.S.; Ali, M.A.; A Goda, D.; Al-Zaban, M.I. Lethal Mechanisms of Nostoc-Synthesized Silver Nanoparticles Against Different Pathogenic Bacteria. Int. J. Nanomed. 2020, 15, 10499–10517. [Google Scholar] [CrossRef]
- Kumar, M.; Wangoo, N.; Gondil, V.S.; Pandey, S.K.; Lalhall, A.; Sharma, R.K.; Chhibber, S. Glycolic acid functionalized silver nanoparticles: A novel approach towards generation of effective antibacterial agent against skin infections. J. Drug Deliv. Sci. Technol. 2020, 60, 102074. [Google Scholar] [CrossRef]


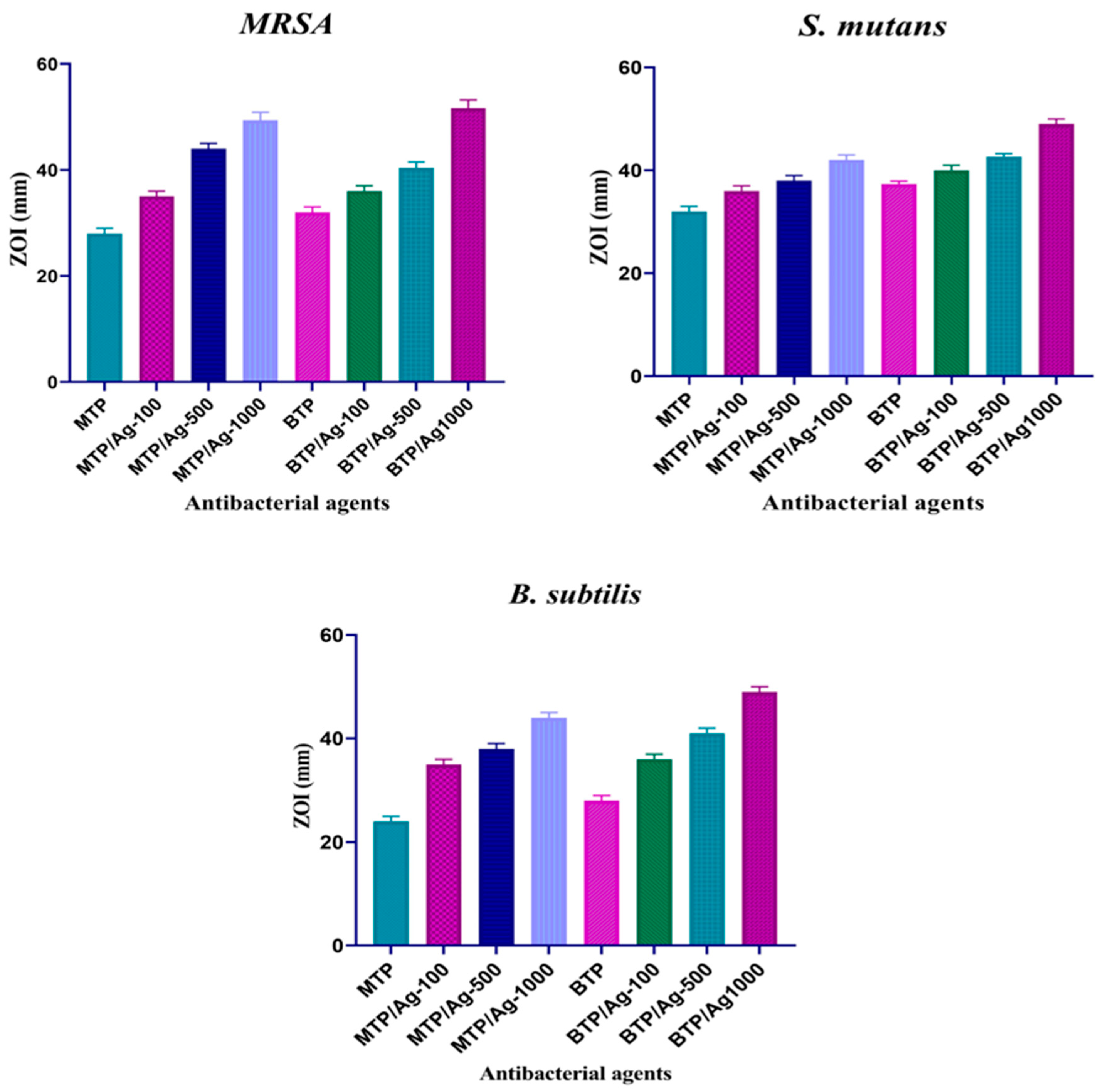


| Compounds | ZOI | MRSA | MRSA (ATCC-43300) | ||||
|---|---|---|---|---|---|---|---|
| MBC | MIC | MBC/MIC | MBC | MIC | MBC/MIC | ||
| MTP | 28 ± 1.00 | 1.25 | 0.625 | 2(+) | 2.5 | 1.25 | 2(+) |
| MTP/Ag-100 | 35 ± 1.00 | 0.3125 | 0.156 | 2(+) | 0.625 | 0.3125 | 2(+) |
| MTP/Ag-500 | 44 ± 1.00 | 0.078 | 0.039 | 2(+) | 0.078 | 0.039 | 2(+) |
| MTP/Ag-1000 | 49 ± 1.50 | 0.0006103 | 0.000305 | 2(+) | 0.0006103 | 0.000305 | 2(+) |
| BTP | 32 ± 1.00 | 0.625 | 0.3125 | 2(+) | 2.5 | 1.25 | 2(+) |
| BTP/Ag-100 | 36 ± 1.00 | 0.3125 | 0.156 | 2(+) | 0.625 | 0.3125 | 2(+) |
| BTP/Ag-500 | 40 ± 1.00 | 0.156 | 0.0781 | 2(+) | 0.156 | 0.0781 | 2(+) |
| BTP/Ag-1000 | 52 ± 1.50 | 0.000305 | 0.0001525 | 2(+) | 0.001220 | 0.0006103 | 2(+) |
| Ampicillin | 14.77 ± 0.60 | 6.25 | 3.13 | 2(+) | 6.25 | 1.56 | 4(+) |
| Ciprofloxacin | 17.32 ± 0.60 | 3.13 | 0.78 | 4(+) | 6.25 | 3.13 | 2(+) |
| Compounds | ZOI | S. mutans | S. mutans (ATCC-35668) | ||||
|---|---|---|---|---|---|---|---|
| MBC | MIC | MBC/MIC | MBC | MIC | MBC/MIC | ||
| MTP | 30 ± 1.00 | 0.625 | 0.3125 | 2(+) | 1.25 | 0.625 | 2(+) |
| MTP/Ag-100 | 36 ± 1.00 | 0.156 | 0.0781 | 2(+) | 0.625 | 0.3125 | 2(+) |
| MTP/Ag-500 | 38 ± 1.00 | 0.03906 | 0.01953 | 2(+) | 0.0781 | 0.03906 | 2(+) |
| MTP/Ag-1000 | 42 ± 1.00 | 0.000305 | 0.0001525 | 2(+) | 0.001220 | 0.000305 | 2(+) |
| BTP | 37 ± 0.60 | 0.3125 | 0.156 | 2(+) | 0.625 | 0.3125 | 2(+) |
| BTP/Ag-100 | 40 ± 1.00 | 0.0781 | 0.03906 | 2(+) | 0.156 | 0.0781 | 2(+) |
| BTP/Ag-500 | 43 ± 0.60 | 0.01953 | 0.009765 | 2(+) | 0.0781 | 0.03906 | 2(+) |
| BTP/Ag-1000 | 49 ± 1.00 | 0.000305 | 0.0001525 | 2(+) | 0.0006103 | 0.000305 | 2(+) |
| Ampicillin | 12 ± 1.00 | 3.13 | 1.565 | 2(+) | 6.25 | 3.13 | 2(+) |
| Ciprofloxacin | 18.27 ± 0.60 | 6.25 | 1.56 | 4(+) | 3.13 | 1.565 | 2(+) |
| Compounds | ZOI | B. subtilis | B. subtilis (ATCC-6633) | ||||
|---|---|---|---|---|---|---|---|
| MBC | MIC | MBC/MIC | MBC | MIC | MBC/MIC | ||
| MTP | 24 ± 1.00 | 0.625 | 0.3125 | 2(+) | 1.25 | 0.625 | 2(+) |
| MTP/Ag-100 | 35 ± 1.00 | 0.03906 | 0.01953 | 2(+) | 0.156 | 0.0781 | 2(+) |
| MTP/Ag-500 | 38 ± 1.00 | 0.00488 | 0.00244 | 2(+) | 0.01953 | 0.009765 | 2(+) |
| MTP/Ag-1000 | 44 ± 1.00 | 0.0006103 | 0.000305 | 2(+) | 0.00244 | 0.001220 | 2(+) |
| BTP | 28 ± 1.00 | 0.156 | 0.0781 | 2(+) | 0.625 | 0.3125 | 2(+) |
| BTP/Ag-100 | 36 ± 1.00 | 0.01953 | 0.009765 | 2(+) | 0.03906 | 0.01953 | 2(+) |
| BTP/Ag-500 | 41 ± 1.00 | 0.009765 | 0.00488 | 2(+) | 0.01953 | 0.009765 | 2(+) |
| BTP/Ag-1000 | 49 ± 1.00 | 0.000305 | 0.0001525 | 2(+) | 0.001220 | 0.0006103 | 2(+) |
| Ampicillin | 16.30 ± 0.6 | 8 | 4 | 2(+) | 6.25 | 3.125 | 2(+) |
| Ciprofloxacin | 18.32 ± 0.60 | 6.25 | 1.56 | 4(+) | 3.13 | 0.78 | 4(+) |
| Compounds | ZOI | P. aeruginosa | P. aeruginosa (ATCC-27853) | ||||
|---|---|---|---|---|---|---|---|
| MBC | MIC | MBC/MIC | MBC | MIC | MBC/MIC | ||
| MTP | 28 ± 1.00 | 1.25 | 0.625 | 2(+) | 2.5 | 1.25 | 2(+) |
| MTP/Ag-100 | 34 ± 0.60 | 0.03906 | 0.01953 | 2(+) | 0.156 | 0.0781 | 2(+) |
| MTP/Ag-500 | 39 ± 1.00 | 0.00488 | 0.00244 | 2(+) | 0.01953 | 0.009765 | 2(+) |
| MTP/Ag-1000 | 43 ± 0.60 | 0.000305 | 0.0001525 | 2(+) | 0.001220 | 0.0006103 | 2(+) |
| BTP | 33 ± 0.60 | 0.156 | 0.0781 | 2(+) | 0.625 | 0.3125 | 2(+) |
| BTP/Ag-100 | 39 ± 1.00 | 0.03906 | 0.01953 | 2(+) | 0.156 | 0.0781 | 2(+) |
| BTP/Ag-500 | 43 ± 1.00 | 0.00488 | 0.00244 | 2(+) | 0.01953 | 0.009765 | 2(+) |
| BTP/Ag-1000 | 47 ± 1.00 | 0.000305 | 0.0001525 | 2(+) | 0.001220 | 0.0006103 | 2(+) |
| Ampicillin | 8.7 ± 0.60 | 12.5 | 6.25 | 2(+) | 6.25 | 1.56 | 4(+) |
| Ciprofloxacin | 16.37 ± 0.60 | 6.25 | 1.56 | 4(+) | 3.13 | 0.78 | 4(+) |
| Compounds | ZOI | S. typhi | S. typhi (ATCC-6539) | ||||
|---|---|---|---|---|---|---|---|
| MBC | MIC | MBC/MIC | MBC | MIC | MBC/MIC | ||
| MTP | 28 ± 1.00 | 0.625 | 0.3125 | 2(+) | 1.25 | 0.625 | 2(+) |
| MTP/Ag-100 | 38 ± 1.00 | 0.03906 | 0.01953 | 2(+) | 0.156 | 0.0781 | 2(+) |
| MTP/Ag-500 | 41 ± 1.00 | 0.00488 | 0.00244 | 2(+) | 0.01953 | 0.009765 | 2(+) |
| MTP/Ag-1000 | 48 ± 1.00 | 0.000305 | 0.0001525 | 2(+) | 0.001220 | 0.0006103 | 2(+) |
| BTP | 35 ± 1.00 | 0.156 | 0.0781 | 2(+) | 0.625 | 0.3125 | 2(+) |
| BTP/Ag-100 | 43 ± 1.00 | 0.01953 | 0.009765 | 2(+) | 0.0781 | 0.03906 | 2(+) |
| BTP/Ag-500 | 48 ± 1.00 | 0.00244 | 0.001220 | 2(+) | 0.009765 | 0.00488 | 2(+) |
| BTP/Ag-1000 | 54 ± 1.00 | 0.0001525 | 0.00007629 | 2(+) | 0.0006103 | 0.000305 | 2(+) |
| Ampicillin | 14.32 ± 0.60 | 3.13 | 1.565 | 2(+) | 6.25 | 1.56 | 4(+) |
| Ciprofloxacin | 18.32 ± 0.60 | 12.5 | 6.25 | 2(+) | 3.13 | 0.78 | 4(+) |
| Compounds | ZOI | S. marcescens | S. marcescens (ATCC-13880) | ||||
|---|---|---|---|---|---|---|---|
| MBC | MIC | MBC/MIC | MBC | MIC | MBC/MIC | ||
| MTP | 35 ± 1.00 | 1.25 | 0.625 | 2(+) | 2.5 | 1.25 | 2(+) |
| MTP/Ag-100 | 41 ± 1.00 | 0.0781 | 0.03906 | 2(+) | 0.3125 | 0.156 | 2(+) |
| MTP/Ag-500 | 45 ± 1.00 | 0.009765 | 0.00488 | 2(+) | 0.01953 | 0.009765 | 2(+) |
| MTP/Ag-1000 | 49 ± 1.00 | 0.001220 | 0.0006103 | 2(+) | 0.00244 | 0.00122 | 2(+) |
| BTP | 38 ± 1.00 | 0.3125 | 0.156 | 2(+) | 1.25 | 0.625 | 2(+) |
| BTP/Ag-100 | 44 ± 0.60 | 0.03906 | 0.01953 | 2(+) | 0.156 | 0.0781 | 2(+) |
| BTP/Ag-500 | 47 ± 1.50 | 0.00244 | 0.001220 | 2(+) | 0.01953 | 0.009765 | 2(+) |
| BTP/Ag-1000 | 54 ± 1.00 | 0.000305 | 0.0001525 | 2(+) | 0.002244 | 0.001220 | 2(+) |
| Ampicillin | 14.32 ± 0.60 | 6.25 | 3.125 | 2(+) | 3.13 | 1.565 | 2(+) |
| Ciprofloxacin | 14.50 ± 0.60 | 3.13 | 0.78 | 4(+) | 6.25 | 1.56 | 4(+) |
| Concentration | MTP | MTP/Ag-100 | MTP/Ag-500 | MTP/Ag-1000 | BTP | BTP/Ag-100 | BTP/Ag-500 | BTP/Ag-1000 |
|---|---|---|---|---|---|---|---|---|
| 10 mg/mL | 11.8 ± 0.06 | 33.6 ± 0.11 | 50.2 ± 0.11 | 58.8 ± 0.08 | 25.4 ± 0.05 | 49.5 ± 0.22 | 55.4 ± 0.05 | 67.4 ± 0.11 |
| 5 mg/mL | 5.3 ± 0.06 | 28.4 ± 0.08 | 41.9 ± 0.06 | 47.5 ± 0.13 | 19.8 ± 0.08 | 35.5 ± 0.11 | 49.8 ± 0.08 | 54.2 ± 0.11 |
| 2.5 mg/mL | 3.8 ± 0.07 | 12.6 ± 0.09 | 24.7 ± 0.14 | 32.3 ± 0.12 | 8.8 ± 0.07 | 27.3 ± 0.07 | 33.8 ± 0.07 | 39.3 ± 0.09 |
| 1.25 mg/mL | 1.7 ± 0.06 | 8.8 ± 0.06 | 16.4 ± 0.09 | 24.9 ± 0.09 | 3.4 ± 0.05 | 18.5 ± 0.07 | 23.4 ± 0.05 | 28.5 ± 0.09 |
| Concentration | MTP | MTP/Ag-100 | MTP/Ag-500 | MTP/Ag-1000 | BTP | BTP/Ag-100 | BTP/Ag-500 | BTP/Ag-1000 |
|---|---|---|---|---|---|---|---|---|
| 10 mg/mL | 50.2 ± 0.11 | 68.3 ± 0.08 | 72.7 ± 0.06 | 79.5 ± 0.02 | 62.9 ± 0.07 | 71.8 ± 0.06 | 77.4 ± 0.07 | 83.6 ± 0.11 |
| 5 mg/mL | 41.9 ± 0.06 | 57.3 ± 0.08 | 68.6 ± 0.08 | 75.5 ± 0.11 | 58.8 ± 0.07 | 65.3 ± 0.06 | 71.9 ± 0.06 | 78.4 ± 0.08 |
| 2.5 mg/mL | 24.7 ± 0.13 | 43.3 ± 0.05 | 52.8 ± 0.08 | 57.3 ± 0.07 | 43.9 ± 0.07 | 51.8 ± 0.07 | 61.4 ± 0.07 | 68.6 ± 0.09 |
| 1.25 mg/mL | 16.4 ± 0.09 | 32.8 ± 0.06 | 34.7 ± 0.07 | 38.5 ± 0.07 | 34.6 ± 0.08 | 43.7 ± 0.06 | 46.4 ± 0.07 | 48.8 ± 0.06 |
| Compound | Protein | BE (Kcal/mol) | RMSD (Å) | Amino Acid Interactions | |
|---|---|---|---|---|---|
| Bacterial Strains | PDB Code | ||||
| MTP | MRSA | 4DKI | −6.0126 | 1.4454 | MET641 (H-donor), TYR446(H-acceptor). |
| Bacillus | 2FQT | −5.562 | 1.979 | GLU57(H-donor), GLY127(H-acceptor). | |
| Pseudo | 5ZHN | −5.976 | 2.247 | TYR120(H-donor), GLU121(H-donor). | |
| Typhi | 3ZQE | −4.8091 | 1.7241 | ARG58(H-acceptor). | |
| BTP | MRSA | 4DKI | −7.9074 | 1.7812 | THR600(H-acceptor), HIS583(H-acceptor), ASN464(H-acceptor), GLY640 (H-pi). |
| Bacillus | 2FQT | −7.9776 | 1.8475 | GLY127(H-acceptor), GLY127 (pi-H), GLU57 (H-donor) | |
| Pseudo | 5ZHN | −5.7701 | 1.5838 | SER (H-pi). | |
| Typhi | 3ZQE | −6.7920 | 1.8609 | ALA229(H-donor), TYR54 (pi-H). | |
| Model Name | Predicted Value for MTP-AgNPs | Predicted Value for BTP-AgNPs |
|---|---|---|
| Absorption | ||
| Water solubility (log mol/L) | −4.889 | −2.945 |
| Caco-2 permeability (log Papp in 10−6 cm/s | 0.794 | −1.021 |
| Intestinal absorption (human) (% Absorbed) | 92.615 | 69.71 |
| Skin Permeability (log Kp) | −2.738 | −2.735 |
| Distribution | ||
| VDss (human) | −0.573 | −1.411 |
| Fraction unbound (human) | 0 | 0.253 |
| BBB permeability | −1.404 | −2.836 |
| CNS permeability | −2.434 | −3.136 |
| Metabolism | ||
| CYP2D6 substrate | No | Yes |
| CYP3A4 substrate | Yes | Yes |
| CYP1A2 inhibitor | Yes | No |
| CYP2C19 inhibitor | Yes | Yes |
| CYP2C9 inhibitor | Yes | Yes |
| CYP2D6 inhibitor | No | No |
| CYP3A4 inhibition | Yes | Yes |
| Excretion | ||
| Total Clearance (log mL/min/kg) | −0.555 | −1.316 |
| Renal OCT2 substrate (Yes/No) | No | No |
| Toxicity | ||
| AMES toxicity | Yes | No |
| Max. tolerated dose (human) (log mg/kg/day) | 0.145 | 0.412 |
| hERG I inhibitor | No | No |
| hERG II inhibitor | Yes | Yes |
| Oral Rat Acute Toxicity (LD50) (mol/kg) | 2.532 | 2.439 |
| Hepatotoxicity | No | No |
| Skin Sensitization | No | No |
| T. Pyriformis toxicity (log μg/L) | 0.335 | 0.285 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Tantawy, A.I.; Elmongy, E.I.; Elsaeed, S.M.; Abdel Aleem, A.A.H.; Binsuwaidan, R.; Eisa, W.H.; Salman, A.U.; Elharony, N.E.; Attia, N.F. Synthesis, Characterization, and Docking Study of Novel Thioureidophosphonate-Incorporated Silver Nanocomposites as Potent Antibacterial Agents. Pharmaceutics 2023, 15, 1666. https://doi.org/10.3390/pharmaceutics15061666
El-Tantawy AI, Elmongy EI, Elsaeed SM, Abdel Aleem AAH, Binsuwaidan R, Eisa WH, Salman AU, Elharony NE, Attia NF. Synthesis, Characterization, and Docking Study of Novel Thioureidophosphonate-Incorporated Silver Nanocomposites as Potent Antibacterial Agents. Pharmaceutics. 2023; 15(6):1666. https://doi.org/10.3390/pharmaceutics15061666
Chicago/Turabian StyleEl-Tantawy, Ahmed I., Elshaymaa I. Elmongy, Shimaa M. Elsaeed, Abdel Aleem H. Abdel Aleem, Reem Binsuwaidan, Wael H. Eisa, Ayah Usama Salman, Noura Elsayed Elharony, and Nour F. Attia. 2023. "Synthesis, Characterization, and Docking Study of Novel Thioureidophosphonate-Incorporated Silver Nanocomposites as Potent Antibacterial Agents" Pharmaceutics 15, no. 6: 1666. https://doi.org/10.3390/pharmaceutics15061666
APA StyleEl-Tantawy, A. I., Elmongy, E. I., Elsaeed, S. M., Abdel Aleem, A. A. H., Binsuwaidan, R., Eisa, W. H., Salman, A. U., Elharony, N. E., & Attia, N. F. (2023). Synthesis, Characterization, and Docking Study of Novel Thioureidophosphonate-Incorporated Silver Nanocomposites as Potent Antibacterial Agents. Pharmaceutics, 15(6), 1666. https://doi.org/10.3390/pharmaceutics15061666







