H2O2-PLA-(Alg)2Ca Hydrogel Enriched in Matrigel® Promotes Diabetic Wound Healing
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Synthesis of H2O2-PLA Microspheres (OMs)
2.3. Preparation of OMs-Loaded Alginate Hydrogels (HG_OMs and HG_OMs_MG)
2.4. Physicochemical Characterization
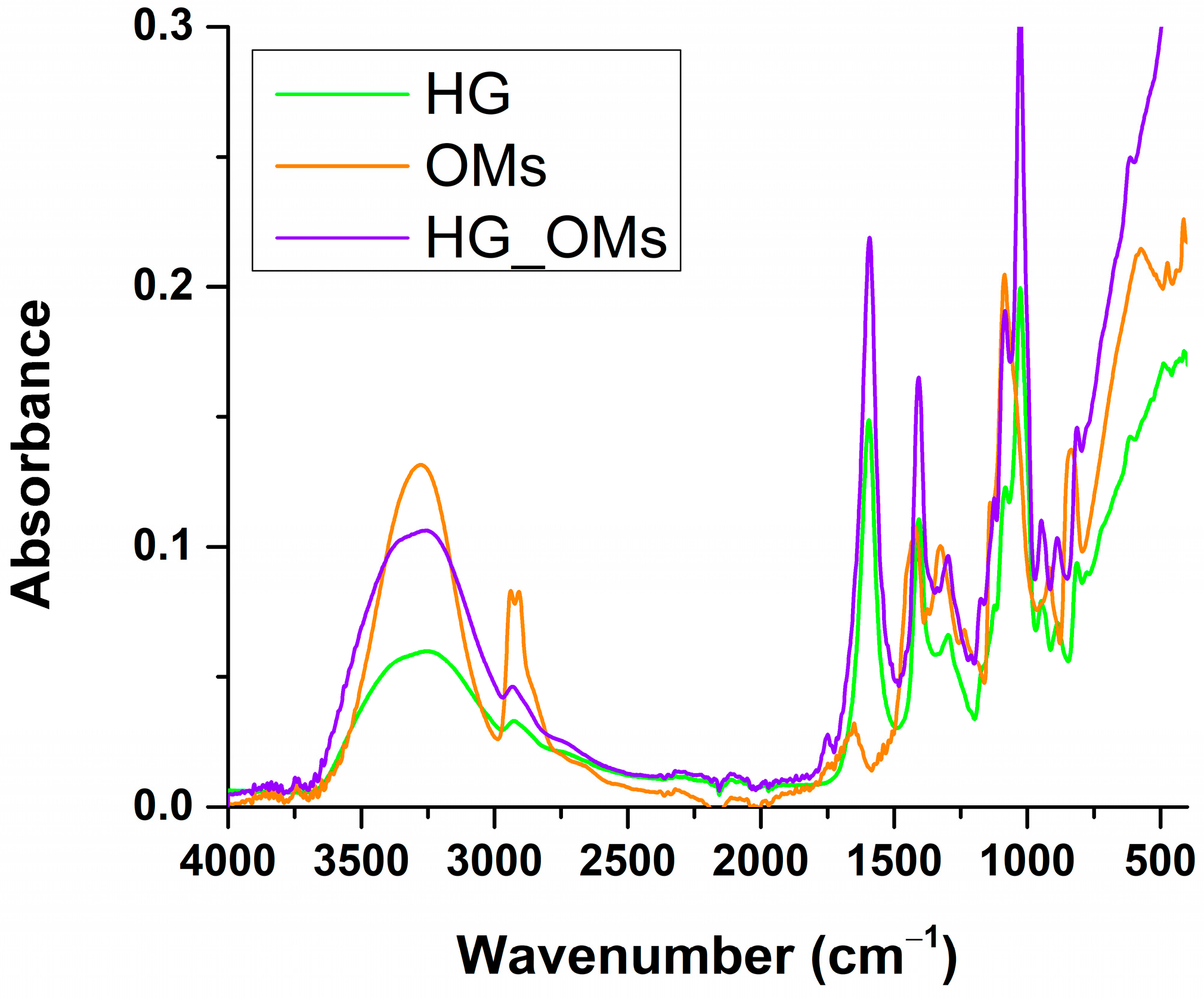
2.4.1. Fourier Transform Infrared Spectroscopy (FTIR)
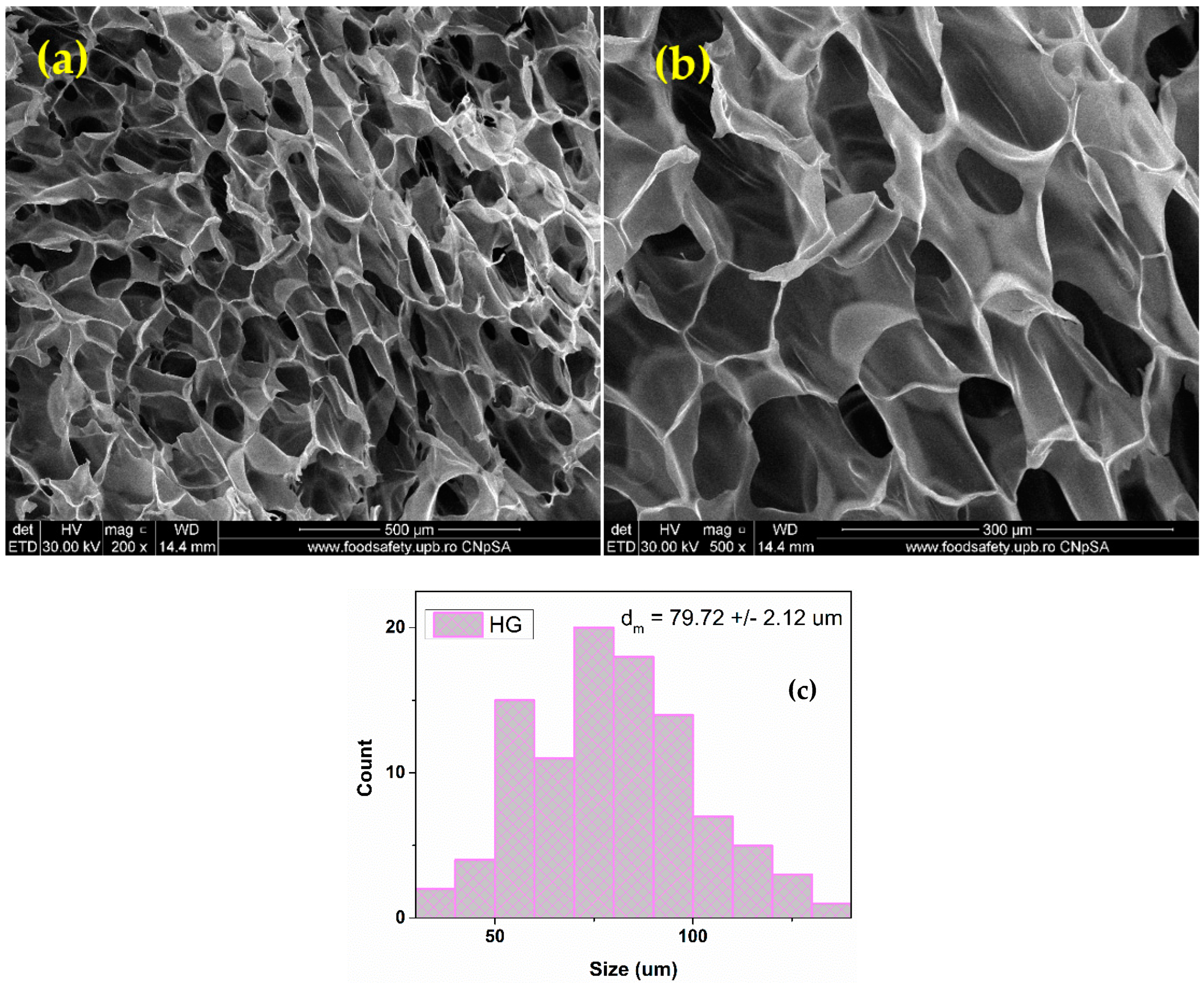
2.4.2. Scanning Electron Microscopy (SEM)
2.4.3. Swelling Rate
2.4.4. Degradation Rate
2.4.5. Hydrogen Peroxide Quantification
2.5. Biological Evaluation
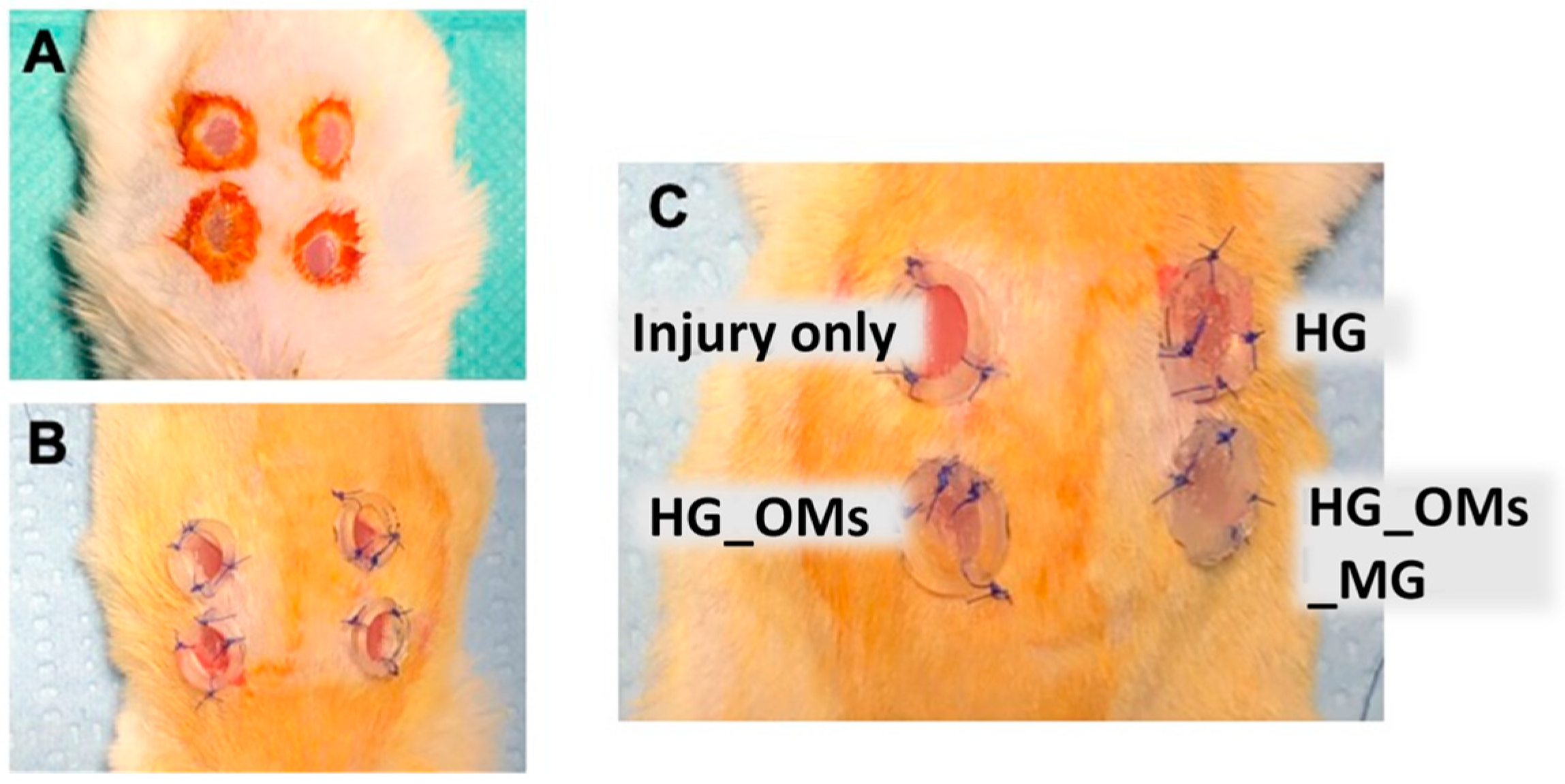
2.5.1. In Vivo Experimental Design
2.5.2. Histopathology
3. Results
3.1. Physicochemical Characterization
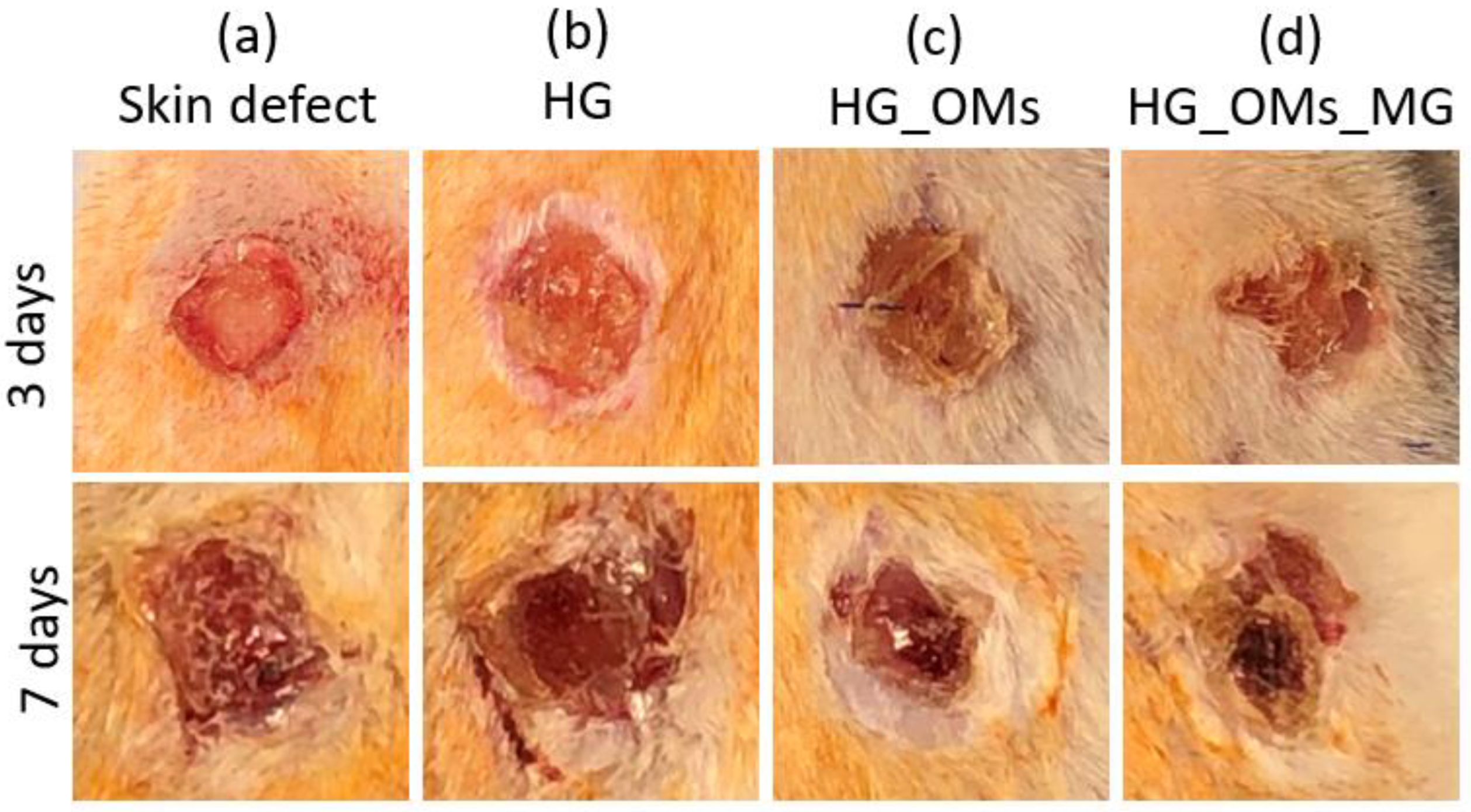
3.2. Gross Morphological Analysis of the Wounds
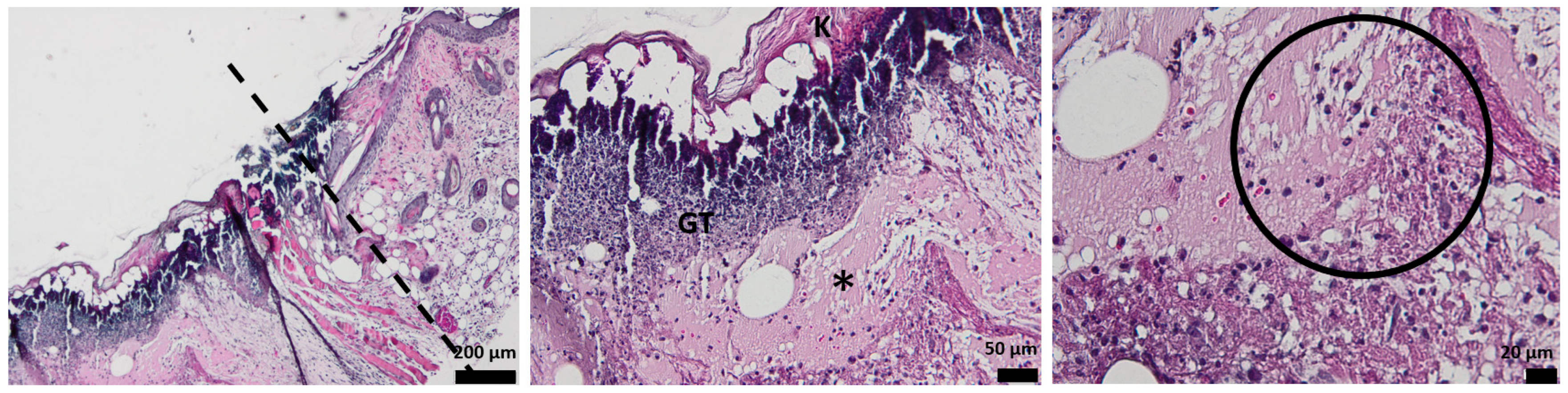
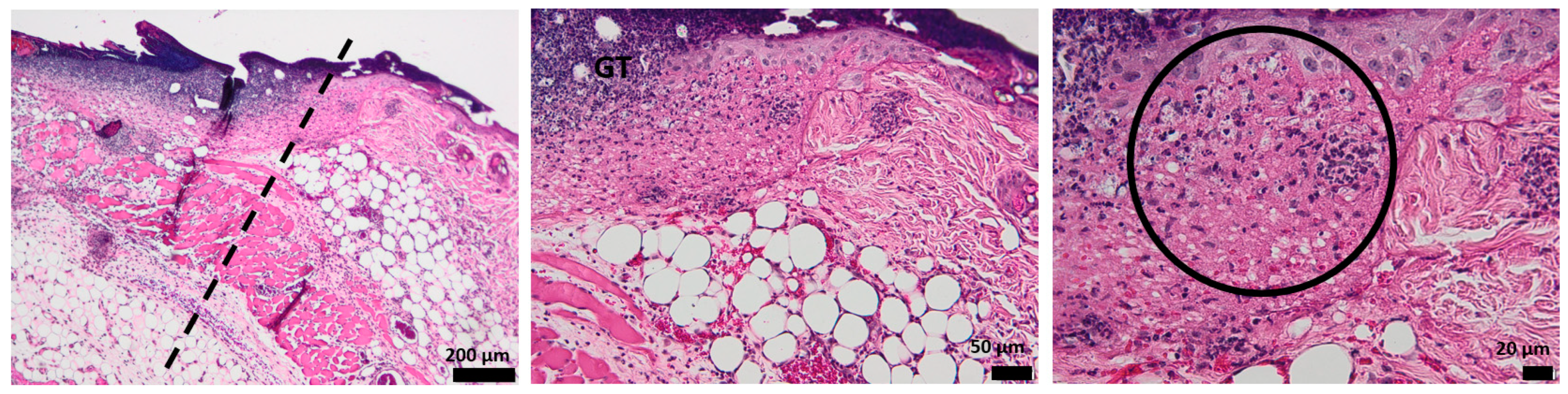
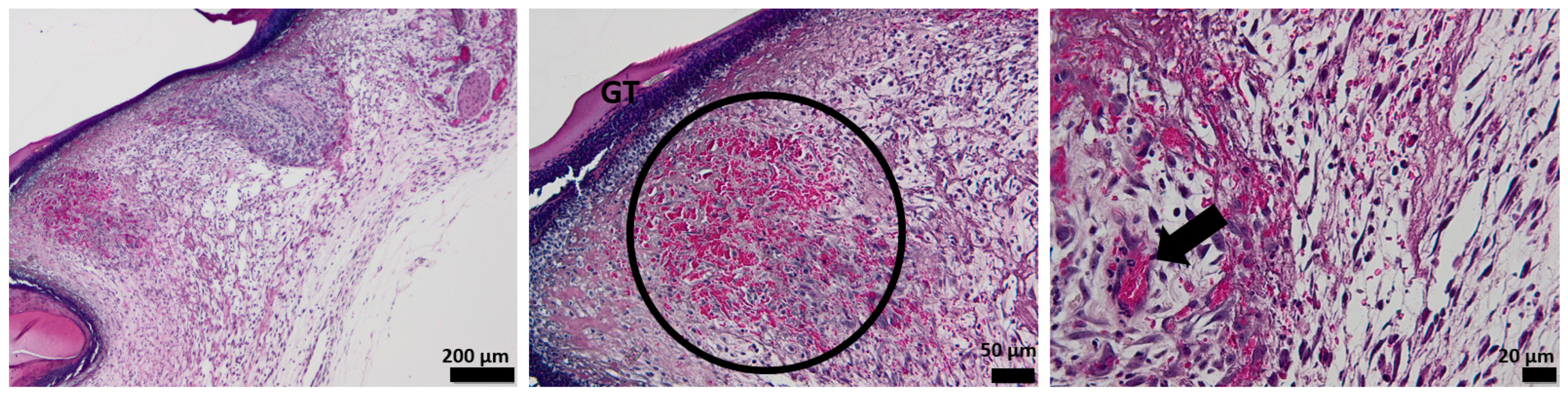
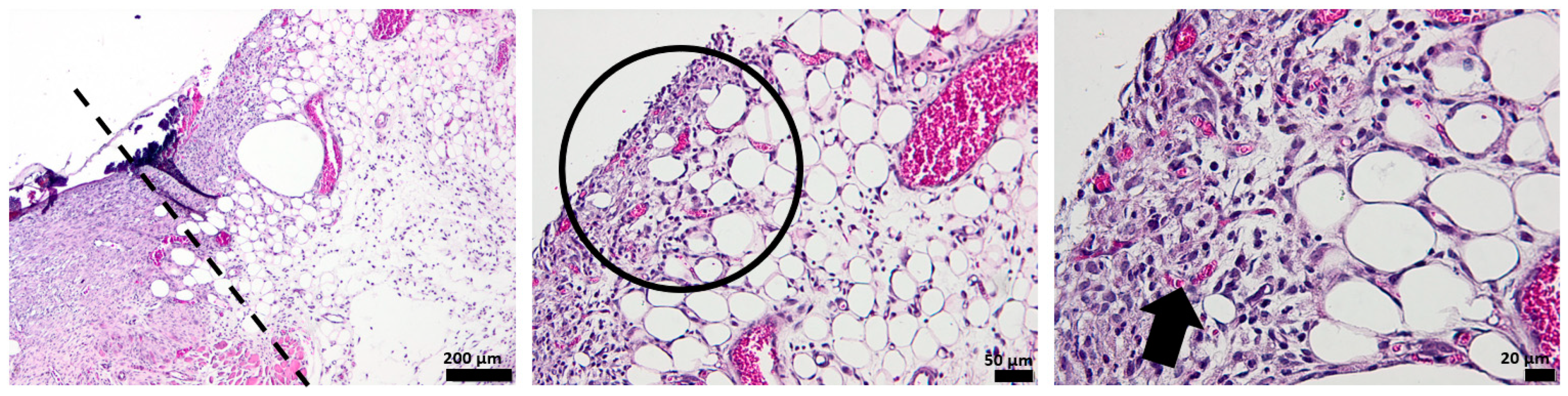
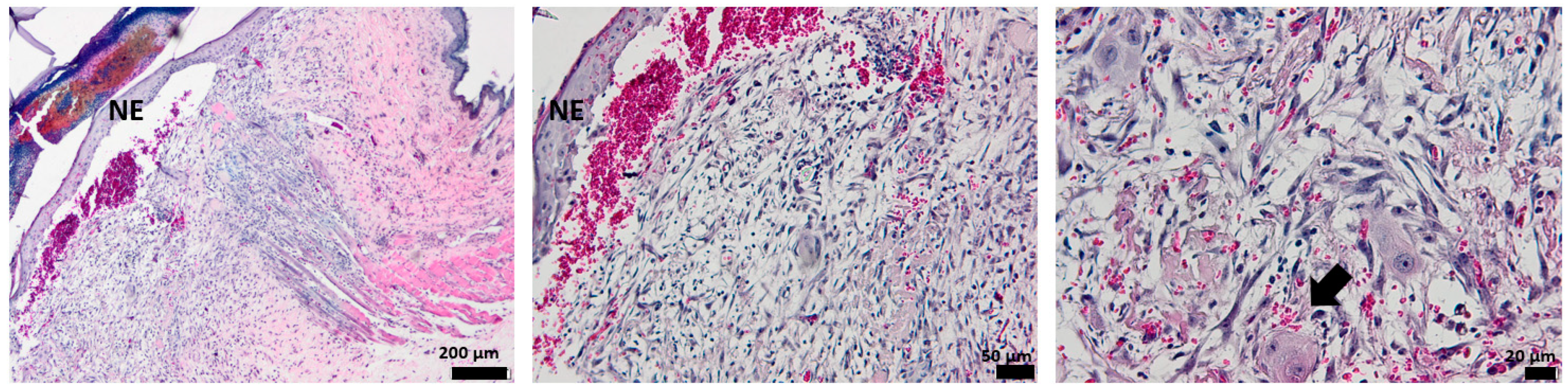
3.3. Histological Aspect of the Wounds 3 Days after Injury (H&E Stain)
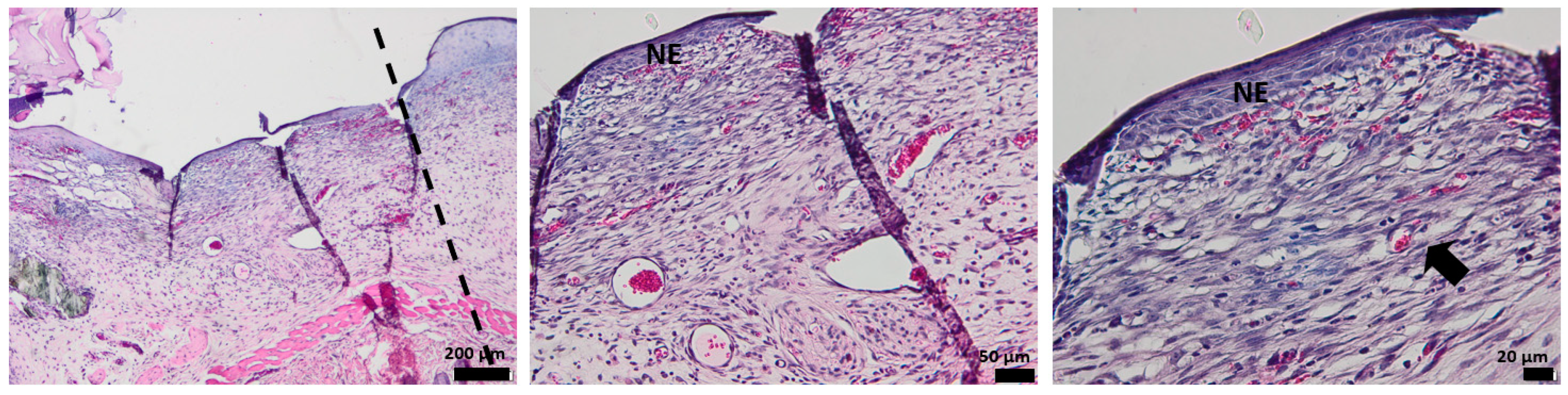
3.4. Histological Aspect of the Wounds 7 Days after Injury (H&E Stain)
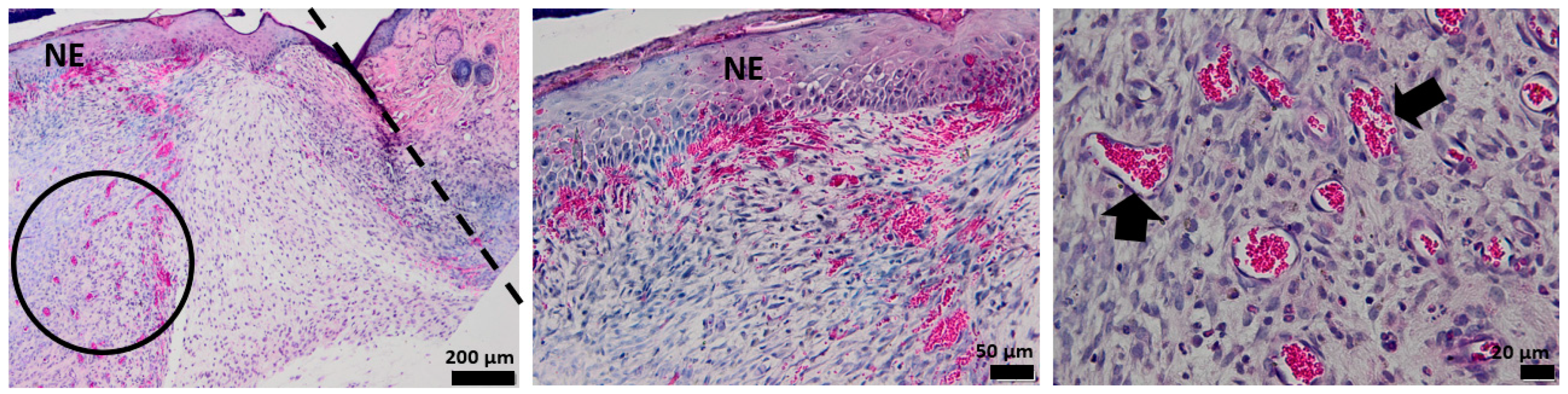
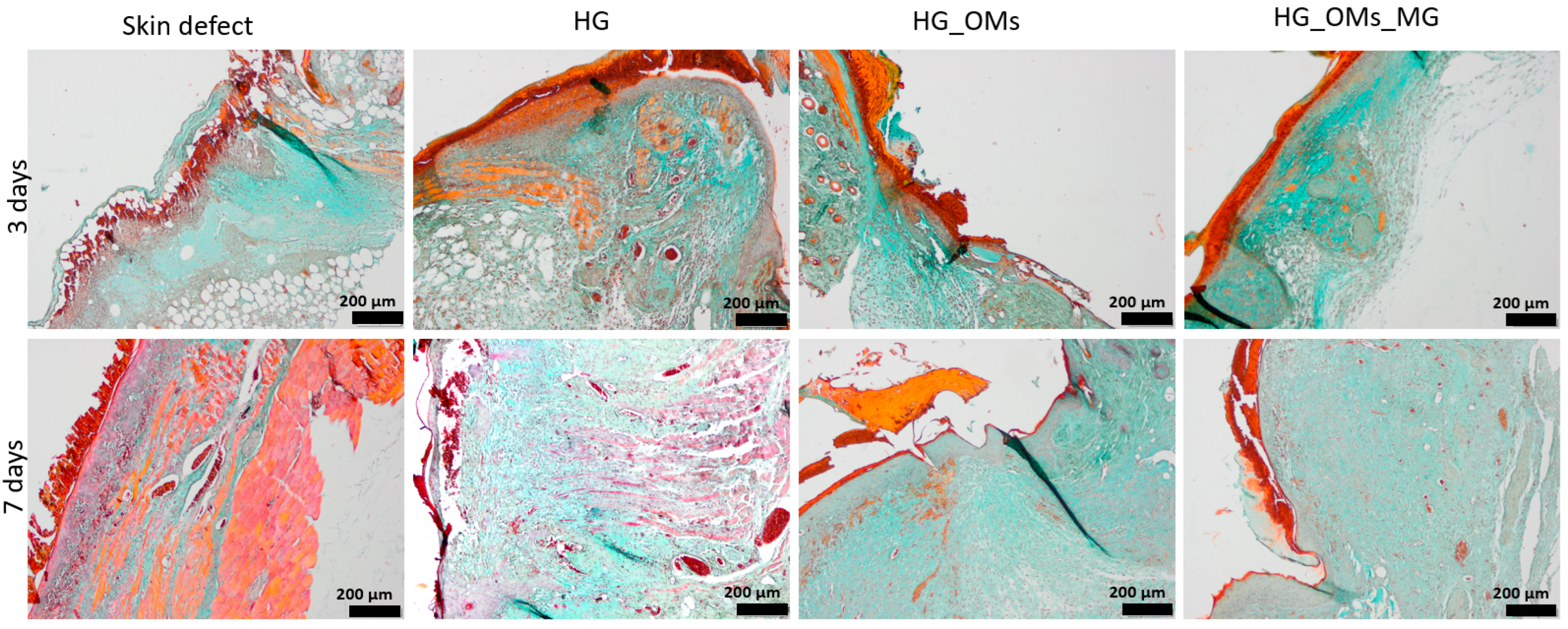
3.5. Histological Aspect of the Keratinization Process (Dane Stain)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, X.; Kang, X.; Jin, L.; Bai, J.; Liu, W.; Wang, Z. Stimulation of wound healing using bioinspired hydrogels with basic fibroblast growth factor (bFGF). Int. J. Nanomed. 2018, 13, 3897. [Google Scholar] [CrossRef]
- Guebitz, G.M.; Nyanhongo, G.S. Enzymes as Green Catalysts and Interactive Biomolecules in Wound Dressing Hydrogels. Trends Biotechnol. 2018, 36, 1040–1053. [Google Scholar] [CrossRef] [PubMed]
- Atma, Y. Synthesis and Application of Fish Gelatin for Hydrogels/Composite Hydrogels: A Review. Biointerface Res. Appl. Chem. 2022, 12, 3966–3976. [Google Scholar] [CrossRef]
- Sun, M.; Zhu, C.; Long, J.; Lu, C.; Pan, X.; Wu, C. PLGA microsphere-based composite hydrogel for dual delivery of ciprofloxacin and ginsenoside Rh2 to treat Staphylococcus aureus-induced skin infections. Drug Deliv. 2020, 27, 632–641. [Google Scholar] [CrossRef] [PubMed]
- Suo, H.; Hussain, M.; Wang, H.; Zhou, N.; Tao, J.; Jiang, H.; Zhu, J. Injectable and pH-Sensitive Hyaluronic Acid-Based Hydrogels with On-Demand Release of Antimicrobial Peptides for Infected Wound Healing. Biomacromolecules 2021, 22, 3049–3059. [Google Scholar] [CrossRef]
- Sanoh, N.C.; Salazar, G.M.; Penaloza, D.P. Magnetic Biopolymeric Hydrogel Composite Material with Self-healing Attribute. Biointerface Res. Appl. Chem. 2021, 11, 14881–14888. [Google Scholar] [CrossRef]
- Dissemond, J.; Augustin, M.; Eming, S.A.; Goerge, T.; Horn, T.; Karrer, S.; Schumann, H.; Stücker, M.; Working Group for Wound Healing (AGW) of the German Society of Dermatology (DDG). Modern wound care–practical aspects of non-interventional topical treatment of patients with chronic wounds. JDDG J. Dtsch. Dermatol. Ges. 2014, 12, 541–554. [Google Scholar] [CrossRef]
- Kamoun, E.A.; Kenawy, E.-R.S.; Chen, X. A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J. Adv. Res. 2017, 8, 217–233. [Google Scholar] [CrossRef]
- Wu, X.; Liu, R.; Lao, T.T. Therapeutic compression materials and wound dressings for chronic venous insufficiency: A comprehensive review. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 892–909. [Google Scholar] [CrossRef]
- Koehler, J.; Brandl, F.P.; Goepferich, A.M. Hydrogel wound dressings for bioactive treatment of acute and chronic wounds. Eur. Polym. J. 2018, 100, 1–11. [Google Scholar] [CrossRef]
- Liu, H.; Wang, C.; Li, C.; Qin, Y.; Wang, Z.; Yang, F.; Li, Z.; Wang, J. A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing. RSC Adv. 2018, 8, 7533–7549. [Google Scholar] [CrossRef] [PubMed]
- Ullah, F.; Javed, F.; Khan, A.; Kudus, M.; Jamila, N.; Minhaz, A.; Akil, H. Synthesis and surface modification of chitosan built nanohydrogel with antiviral and antimicrobial agent for controlled drug delivery. Biointerface Res. Appl. Chem. 2019, 9, 4439–4445. [Google Scholar]
- Kaidi, S.; Belattmania, Z.; Bentiss, F.; Jama, C.; Reani, A.; Sabour, B. Synthesis and Characterization of Silver Nanoparticles Using Alginate from the Brown Seaweed Laminaria ochroleuca: Structural Features and Antibacterial Activity. Biointerface Res. Appl. Chem. 2022, 12, 6046–6057. [Google Scholar] [CrossRef]
- Zhang, M.; Zhao, X. Alginate hydrogel dressings for advanced wound management. Int. J. Biol. Macromol. 2020, 162, 1414–1428. [Google Scholar] [CrossRef] [PubMed]
- Bahadoran, M.; Shamloo, A.; Nokoorani, Y.D. Development of a polyvinyl alcohol/sodium alginate hydrogel-based scaffold incorporating bFGF-encapsulated microspheres for accelerated wound healing. Sci. Rep. 2020, 10, 7342. [Google Scholar] [CrossRef] [PubMed]
- Fahmy, A.; Khafagy, R.; Elhaes, H.; Ibrahim, M. Molecular properties of polyvinyl alcohol/sodium alginate composite. Biointerface Res. Appl. Chem. 2020, 10, 4734–4739. [Google Scholar]
- Weller, C.D.; Team, V.; Sussman, G. First-line interactive wound dressing update: A comprehensive review of the evidence. Front. Pharmacol. 2020, 11, 155. [Google Scholar] [CrossRef]
- Aderibigbe, B.A.; Buyana, B. Alginate in wound dressings. Pharmaceutics 2018, 10, 42. [Google Scholar] [CrossRef]
- Redondo, F.L.; Giaroli, M.C.; Ciolino, A.E.; Ninago, M.D. Preparation of Porous Poly(Lactic Acid)/Tricalcium Phosphate Composite Scaffolds for Tissue Engineering. Biointerface Res. Appl. Chem. 2022, 12, 5610–5624. [Google Scholar] [CrossRef]
- Zarrintaj, P.; Saeb, M.R.; Jafari, S.H.; Mozafari, M. Application of compatibilized polymer blends in biomedical fields. In Compatibilization of Polymer Blends; Elsevier: Amsterdam, The Netherlands, 2020; pp. 511–537. [Google Scholar]
- Hamid, Z.A.; Tham, C.; Ahmad, Z. Preparation and optimization of surface-engineered poly (lactic acid) microspheres as a drug delivery device. J. Mater. Sci. 2018, 53, 4745–4758. [Google Scholar] [CrossRef]
- Da Silva, D.; Kaduri, M.; Poley, M.; Adir, O.; Krinsky, N.; Shainsky-Roitman, J.; Schroeder, A. Biocompatibility, biodegradation and excretion of polylactic acid (PLA) in medical implants and theranostic systems. Chem. Eng. J. 2018, 340, 9–14. [Google Scholar] [CrossRef]
- Singhvi, M.; Zinjarde, S.; Gokhale, D. Polylactic acid: Synthesis and biomedical applications. J. Appl. Microbiol. 2019, 127, 1612–1626. [Google Scholar] [CrossRef]
- Sin, L.T.; Rahmat, A.R.; Rahman, W.A.W.A. 4—Chemical Properties of Poly (lactic Acid). In Polylactic Acid; Sin, L.T., Rahmat, A.R., Rahman, W.A.W.A., Eds.; William Andrew Publishing: Oxford, UK, 2013; pp. 143–176. [Google Scholar]
- Elsawy, M.A.; Kim, K.-H.; Park, J.-W.; Deep, A. Hydrolytic degradation of polylactic acid (PLA) and its composites. Renew. Sustain. Energy Rev. 2017, 79, 1346–1352. [Google Scholar] [CrossRef]
- Darabian, B.; Bagheri, H.; Mohammadi, S. Improvement in mechanical properties and biodegradability of PLA using poly (ethylene glycol) and triacetin for antibacterial wound dressing applications. Prog. Biomater. 2020, 9, 45–64. [Google Scholar] [CrossRef]
- Bi, H.; Feng, T.; Li, B.; Han, Y. In Vitro and In Vivo Comparison study of electrospun PLA and PLA/PVA/SA fiber membranes for wound healing. Polymers 2020, 12, 839. [Google Scholar] [CrossRef]
- Fattahi, F.S.; Khoddami, A.; Avinc, O.O. Poly (Lactic Acid) Nano structure mats as potential wound dressings. Pamukkale Üniversitesi Mühendislik Bilim. Derg. 2020, 26, 1193–1203. [Google Scholar] [CrossRef]
- Baqiya, M.A.; Taufiq, A.; Sunaryono, M.; Sari, P.; Dwihapsari, Y. Development of PVA/Fe3O4 as smart magnetic hydrogels for biomedical applications. Hydrogels. Lond. IntechOpen 2018, 159–178. [Google Scholar]
- Kariminejad, M.; Zibaei, R.; Kolahdouz-Nasiri, A.; Mohammadi, R.; Mortazavian, A.M.; Sohrabvandi, S.; Khanniri, E.; Khorshidian, N. Chitosan/Polyvinyl Alcohol/SiO2 Nanocomposite Films: Physicochemical and Structural Characterization. Biointerface Res. Appl. Chem. 2022, 12, 3725–3734. [Google Scholar] [CrossRef]
- Tamer, T.M.; Sabet, M.M.; Omer, A.M.; Abbas, E.; Eid, A.I.; Mohy-Eldin, M.S.; Hassan, M.A. Hemostatic and antibacterial PVA/Kaolin composite sponges loaded with penicillin–streptomycin for wound dressing applications. Sci. Rep. 2021, 11, 3428. [Google Scholar] [CrossRef]
- Gyles, D.A.; Castro, L.D.; Silva, J.O.C., Jr.; Ribeiro-Costa, R.M. A review of the designs and prominent biomedical advances of natural and synthetic hydrogel formulations. Eur. Polym. J. 2017, 88, 373–392. [Google Scholar] [CrossRef]
- Kenawy, E.-R.; Kamoun, E.A.; Eldin, M.S.M.; El-Meligy, M.A. Physically cross-linked poly (vinyl alcohol)-hydroxyethyl starch blend hydrogel membranes: Synthesis and characterization for biomedical applications. Arab. J. Chem. 2014, 7, 372–380. [Google Scholar] [CrossRef]
- Bavya, M.C.; George, L.; Srivastava, R.; VimalRohan, K. Natural and Synthetic Materials in Regenerative Medicine: Progress Over the Past Five Years: Hydrogels: An Insight. In Reference Module in Materials Science and Materials Engineering; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Behnoodfar, D.; Dadbin, S.; Frounchi, M. PLA microspheres-embedded PVA hydrogels prepared by gamma-irradiation and freeze-thaw methods as drug release carriers. Int. J. Polym. Mater. 2013, 62, 28–33. [Google Scholar] [CrossRef]
- Gottrup, F.; Dissemond, J.; Baines, C.; Frykberg, R.; Jensen, P.Ø.; Kot, J.; Kröger, K.; Longobardi, P. Use of oxygen therapies in wound healing: Focus on topical and hyperbaric oxygen treatment. J. Wound Care 2017, 26, S1–S43. [Google Scholar] [CrossRef] [PubMed]
- Thi, P.L.; Lee, Y.; Tran, D.L.; Thi, T.T.H.; Kang, J.I.; Park, K.M.; Park, K.D. In situ forming and reactive oxygen species-scavenging gelatin hydrogels for enhancing wound healing efficacy. Acta Biomater. 2020, 103, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Jee, J.-P.; Pangeni, R.; Jha, S.K.; Byun, Y.; Park, J.W. Preparation and in vivo evaluation of a topical hydrogel system incorporating highly skin-permeable growth factors, quercetin, and oxygen carriers for enhanced diabetic wound-healing therapy. Int. J. Nanomed. 2019, 14, 5449. [Google Scholar] [CrossRef]
- de Smet, G.H.; Kroese, L.F.; Menon, A.G.; Jeekel, J.; van Pelt, A.W.; Kleinrensink, G.J.; Lange, J.F. Oxygen therapies and their effects on wound healing. Wound Repair Regen. 2017, 25, 591–608. [Google Scholar] [CrossRef]
- Hayes, P.; Alzuhir, N.; Curran, G.; Loftus, I. Topical oxygen therapy promotes the healing of chronic diabetic foot ulcers: A pilot study. J. Wound Care 2017, 26, 652–660. [Google Scholar] [CrossRef]
- Laschke, M.; Rücker, M.; Jensen, G.; Carvalho, C.; Mülhaupt, R.; Gellrich, N.C.; Menger, M. Incorporation of growth factor containing Matrigel promotes vascularization of porous PLGA scaffolds. J. Biomed. Mater. Res. Part A Off. J. Soc. Biomater. Jpn. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2008, 85, 397–407. [Google Scholar] [CrossRef]
- Kleinman, H.K.; Martin, G.R. Matrigel: Basement membrane matrix with biological activity. In Seminars in Cancer Biology; Academic Press: Cambridge, MA, USA, 2005; pp. 378–386. [Google Scholar]
- Xue, H.; Hu, L.; Xiong, Y.; Zhu, X.; Wei, C.; Cao, F.; Zhou, W.; Sun, Y.; Endo, Y.; Liu, M. Quaternized chitosan-Matrigel-polyacrylamide hydrogels as wound dressing for wound repair and regeneration. Carbohydr. Polym. 2019, 226, 115302. [Google Scholar] [CrossRef]
- Aisenbrey, E.A.; Murphy, W.L. Synthetic alternatives to Matrigel. Nat. Rev. Mater. 2020, 5, 539–551. [Google Scholar] [CrossRef]
- Lakmal, K.; Basnayake, O.; Hettiarachchi, D. Systematic review on the rational use of amniotic membrane allografts in diabetic foot ulcer treatment. BMC Surg. 2021, 21, 87. [Google Scholar] [CrossRef]
- Aldana, P.C.; Khachemoune, A. Diabetic foot ulcers: Appraising standard of care and reviewing new trends in management. Am. J. Clin. Dermatol. 2020, 21, 255–264. [Google Scholar] [CrossRef]
- Lázaro-Martínez, J.L.; García-Madrid, M.; García-Alamino, J.M.; Bohbot, S.; García-Klepzig, J.L.; García-Álvarez, Y. Increasing transcutaneous oxygen pressure in patients with neuroischemic diabetic foot ulcers treated with a sucrose octasulfate dressing: A pilot study. Int. J. Low. Extrem. Wounds 2020, 21, 450–456. [Google Scholar] [CrossRef]
- Lykov, A.; Surovtseva, M.; Bondarenko, N.; Kim, I.; Smagin, M.; Poveshchenko, O. Platelet Lysate and Non-Healing Ulcers. Biointerface Res. Appl. Chem. 2021, 11, 12267–12274. [Google Scholar] [CrossRef]
- Xiang, J.; Wang, S.; He, Y.; Xu, L.; Zhang, S.; Tang, Z. Reasonable glycemic control would help wound healing during the treatment of diabetic foot ulcers. Diabetes Ther. 2019, 10, 95–105. [Google Scholar] [CrossRef]
- Lane, K.L.; Abusamaan, M.S.; Voss, B.F.; Thurber, E.G.; Al-Hajri, N.; Gopakumar, S.; Le, J.T.; Gill, S.; Blanck, J.; Prichett, L. Glycemic control and diabetic foot ulcer outcomes: A systematic review and meta-analysis of observational studies. J. Diabetes Its Complicat. 2020, 34, 107638. [Google Scholar] [CrossRef]
- Rao, S.S.; Venkatesan, J.; Prabhu, A.; Rekha, P. Natural polymeric biomaterials in growth factor delivery for treating diabetic foot ulcers. J. Drug Deliv. Sci. Technol. 2020, 55, 101385. [Google Scholar] [CrossRef]
- Sari, Y.; Purnawan, I.; Taufik, A. Quality of life and associated factors in Indonesian diabetic patients with foot ulcers. Nurse Media J. Nurs. 2018, 8, 13–24. [Google Scholar] [CrossRef]
- Gourishetti, K.; Keni, R.; Nayak, P.G.; Jitta, S.R.; Bhaskaran, N.A.; Kumar, L.; Kumar, N.; Krishnadas, N.; Shenoy, R.R. Sesamol-loaded PLGA nanosuspension for accelerating wound healing in diabetic foot ulcer in rats. Int. J. Nanomed. 2020, 15, 9265. [Google Scholar] [CrossRef]
- Irawan, H.; Semadi, I.N.; Widiana, I. A pilot study of short-duration hyperbaric oxygen therapy to improve HbA1c, leukocyte, and serum creatinine in patients with diabetic foot ulcer Wagner 3-4. Sci. World J. 2018, 2018, 6425857. [Google Scholar] [CrossRef]
- Parizad, N.; Hajimohammadi, K.; Goli, R. Surgical debridement, maggot therapy, negative pressure wound therapy, and silver foam dressing revive hope for patients with diabetic foot ulcer: A case report. Int. J. Surg. Case Rep. 2021, 82, 105931. [Google Scholar] [CrossRef] [PubMed]
- Jeckson, T.A.; Neo, Y.P.; Sisinthy, S.P.; Foo, J.B.; Choudhury, H.; Gorain, B. Formulation and characterisation of deferoxamine nanofiber as potential wound dressing for the treatment of diabetic foot ulcer. J. Drug Deliv. Sci. Technol. 2021, 66, 102751. [Google Scholar] [CrossRef]
- Loera-Valencia, R.; Neira, R.E.; Urbina, B.P.; Camacho, A.; Galindo, R.B. Evaluation of the therapeutic efficacy of dressings with ZnO nanoparticles in the treatment of diabetic foot ulcers. Biomed. Pharmacother. 2022, 155, 113708. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.; Yin, H.; Yu, X.; Wang, L.; Fan, L.; Xin, J.H.; Yu, H. 3D PCL/collagen nanofibrous medical dressing for one-time treatment of diabetic foot ulcers. Colloids Surf. B Biointerfaces 2022, 214, 112480. [Google Scholar] [CrossRef]
- Goi, A.; Veressinina, Y.; Trapido, M. Degradation of salicylic acid by Fenton and modified Fenton treatment. Chem. Eng. J. 2008, 143, 1–9. [Google Scholar] [CrossRef]
- Luță, E.A.; Biță, A.; Moroșan, A.; Mihaiescu, D.E.; Ghica, M.; Mihai, D.P.; Olaru, O.T.; Deculescu-Ioniță, T.; Duțu, L.E.; Popescu, M.L.; et al. The Influence of Phytosociological Cultivation and Fertilization on Polyphenolic Content of Menthae and Melissae folium and Evaluation of Antioxidant Properties through In Vitro and In Silico Methods. Plants 2022, 11, 2398. [Google Scholar] [CrossRef]
- Shivakumara, L.R.; Demappa, T. Synthesis and Swelling Behavior of Sodium Alginate/Poly(vinyl alcohol) Hydrogels. Turk. J. Pharm. Sci. 2019, 16, 252–260. [Google Scholar] [CrossRef]
- Wang, T.; Zhang, F.; Zhao, R.; Wang, C.; Hu, K.; Sun, Y.; Politis, C.; Shavandi, A.; Nie, L. Polyvinyl Alcohol/Sodium Alginate Hydrogels Incorporated with Silver Nanoclusters via Green Tea Extract for Antibacterial Applications. Des. Monomers Polym. 2020, 23, 118–133. [Google Scholar] [CrossRef]
- Kudzin, M.H.; Boguń, M.; Mrozińska, Z.; Kaczmarek, A. Physical Properties, Chemical Analysis, and Evaluation of Antimicrobial Response of New Polylactide/Alginate/Copper Composite Materials. Mar. Drugs 2020, 18, 660. [Google Scholar] [CrossRef]
- Seba, V.; de Lima, G.G.; Pereira, B.L.; Silva, G.; Reinhardt, L.S.; Arantes, P.R.; Chee, B.S.; Dos Santos, M.B.; França, S.C.; Regasini, L.O.; et al. Development, Characterization and Cell Viability Inhibition of PVA Spheres Loaded with Doxorubicin and 4’-Amino-1-Naphthyl-Chalcone (D14) for Osteosarcoma. Polymers 2021, 13, 2611. [Google Scholar] [CrossRef]
- Zhao, W.Y.; Fang, Q.Q.; Wang, X.F.; Wang, X.W.; Zhang, T.; Shi, B.H.; Zheng, B.; Zhang, D.D.; Hu, Y.Y.; Ma, L. Chitosan-calcium alginate dressing promotes wound healing: A preliminary study. Wound Repair Regen. 2020, 28, 326–337. [Google Scholar] [CrossRef]
- Nešović, K.; Janković, A.; Radetić, T.; Vukašinović-Sekulić, M.; Kojić, V.; Živković, L.; Perić-Grujić, A.; Rhee, K.Y.; Mišković-Stanković, V. Chitosan-based hydrogel wound dressings with electrochemically incorporated silver nanoparticles–In vitro study. Eur. Polym. J. 2019, 121, 109257. [Google Scholar] [CrossRef]
- Khorasani, M.T.; Joorabloo, A.; Moghaddam, A.; Shamsi, H.; MansooriMoghadam, Z. Incorporation of ZnO nanoparticles into heparinised polyvinyl alcohol/chitosan hydrogels for wound dressing application. Int. J. Biol. Macromol. 2018, 114, 1203–1215. [Google Scholar] [CrossRef]
- Wang, M.; Yang, Y.; Yuan, K.; Yang, S.; Tang, T. Dual-functional hybrid quaternized chitosan/Mg/alginate dressing with antibacterial and angiogenic potential for diabetic wound healing. J. Orthop. Transl. 2021, 30, 6–15. [Google Scholar] [CrossRef]
- Diniz, F.R.; Maia, R.C.A.; Rannier Andrade, L.; Andrade, L.N.; Vinicius Chaud, M.; da Silva, C.F.; Corrêa, C.B.; de Albuquerque Junior, R.L.C.; da Costa, L.P.; Shin, S.R. Silver nanoparticles-composing alginate/gelatine hydrogel improves wound healing in vivo. Nanomaterials 2020, 10, 390. [Google Scholar] [CrossRef]
- Gupta, A.; Briffa, S.M.; Swingler, S.; Gibson, H.; Kannappan, V.; Adamus, G.; Kowalczuk, M.; Martin, C.; Radecka, I. Synthesis of silver nanoparticles using curcumin-cyclodextrins loaded into bacterial cellulose-based hydrogels for wound dressing applications. Biomacromolecules 2020, 21, 1802–1811. [Google Scholar] [CrossRef]
- Raafat, A.I.; El-Sawy, N.M.; Badawy, N.A.; Mousa, E.A.; Mohamed, A.M. Radiation fabrication of Xanthan-based wound dressing hydrogels embedded ZnO nanoparticles: In vitro evaluation. Int. J. Biol. Macromol. 2018, 118, 1892–1902. [Google Scholar] [CrossRef]
- Patel, S.; Srivastava, S.; Singh, M.R.; Singh, D. Mechanistic insight into diabetic wounds: Pathogenesis, molecular targets and treatment strategies to pace wound healing. Biomed. Pharmacother. Biomed. Pharmacother. 2019, 112, 108615. [Google Scholar] [CrossRef]
- Spampinato, S.F.; Caruso, G.I.; De Pasquale, R.; Sortino, M.A.; Merlo, S. The Treatment of Impaired Wound Healing in Diabetes: Looking among Old Drugs. Pharmaceuticals 2020, 13, 60. [Google Scholar] [CrossRef]
- Oropallo, A.R.; Serena, T.E.; Armstrong, D.G.; Niederauer, M.Q. Molecular Biomarkers of Oxygen Therapy in Patients with Diabetic Foot Ulcers. Biomolecules 2021, 11, 925. [Google Scholar] [CrossRef]
- Carter, M.J.; Frykberg, R.G.; Oropallo, A.; Sen, C.K.; Armstrong, D.G.; Nair, H.K.R.; Serena, T.E. Efficacy of Topical Wound Oxygen Therapy in Healing Chronic Diabetic Foot Ulcers: Systematic Review and Meta-Analysis. Adv. Wound Care 2022, 12, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Grumezescu, V.; Socol, G.; Grumezescu, A.M.; Holban, A.M.; Ficai, A.; Truşcǎ, R.; Bleotu, C.; Balaure, P.C.; Cristescu, R.; Chifiriuc, M.C. Functionalized antibiofilm thin coatings based on PLA–PVA microspheres loaded with usnic acid natural compounds fabricated by MAPLE. Appl. Surf. Sci. 2014, 302, 262–267. [Google Scholar] [CrossRef]
- Gherasim, O.; Grumezescu, A.M.; Grumezescu, V.; Andronescu, E.; Negut, I.; Bîrcă, A.C.; Gălățeanu, B.; Hudiță, A. Bioactive Coatings Loaded with Osteogenic Protein for Metallic Implants. Polymers 2021, 13, 4303. [Google Scholar] [CrossRef] [PubMed]
- Saghebasl, S.; Davaran, S.; Rahbarghazi, R.; Montaseri, A.; Salehi, R.; Ramazani, A. Synthesis and in vitro evaluation of thermosensitive hydrogel scaffolds based on (PNIPAAm-PCL-PEG-PCL-PNIPAAm)/Gelatin and (PCL-PEG-PCL)/Gelatin for use in cartilage tissue engineering. J. Biomater. Science. Polym. Ed. 2018, 29, 1185–1206. [Google Scholar] [CrossRef]
- Kryszak, B.; Gazińska, M.; Gruber, P.; Wieczorek, M.; Krokos, A.; Dzienny, P.; Szymczyk-Ziółkowska, P.; Olejarczyk, M.; Antończak, A.J. Mechanical properties and degradation of laser sintered structures of PLA microspheres obtained by dual beam laser sintering method. Int. J. Adv. Manuf. Technol. 2022, 120, 7855–7872. [Google Scholar] [CrossRef]
- Gherasim, O.; Popescu, R.C.; Grumezescu, V.; Mogoșanu, G.D.; Mogoantă, L.; Iordache, F.; Holban, A.M.; Vasile, B.; Bîrcă, A.C.; Oprea, O.C.; et al. MAPLE Coatings Embedded with Essential Oil-Conjugated Magnetite for Anti-Biofilm Applications. Materials 2021, 14, 1612. [Google Scholar] [CrossRef]
- Motelica, L.; Ficai, D.; Oprea, O.C.; Ficai, A.; Ene, V.L.; Vasile, B.S.; Andronescu, E.; Holban, A.M. Antibacterial Biodegradable Films Based on Alginate with Silver Nanoparticles and Lemongrass Essential Oil-Innovative Packaging for Cheese. Nanomaterials 2021, 11, 2377. [Google Scholar] [CrossRef]
- Motelica, L.; Ficai, D.; Oprea, O.; Ficai, A.; Trusca, R.D.; Andronescu, E.; Holban, A.M. Biodegradable Alginate Films with ZnO Nanoparticles and Citronella Essential Oil-A Novel Antimicrobial Structure. Pharmaceutics 2021, 13, 1020. [Google Scholar] [CrossRef]
- Estrada-Villegas, G.M.; Morselli, G.; Oliveira, M.J.A.; González-Pérez, G.; Lugão, A.B. PVGA/Alginate-AgNPs hydrogel as absorbent biomaterial and its soil biodegradation behavior. Polym. Bull. 2020, 77, 4147–4166. [Google Scholar] [CrossRef]
- Badita, C.; Aranghel, D.; Burducea, C.; Mereuta, P.J.R.J.P. Characterization of sodium alginate based films. Rom. J. Phys. 2020, 65, 1–8. [Google Scholar]
- Englert, C.; Brendel, J.C.; Majdanski, T.C.; Yildirim, T.; Schubert, S.; Gottschaldt, M.; Windhab, N.; Schubert, U.S. Pharmapolymers in the 21st century: Synthetic polymers in drug delivery applications. Prog. Polym. Sci. 2018, 87, 107–164. [Google Scholar] [CrossRef]
- Vlachopoulos, A.; Karlioti, G.; Balla, E.; Daniilidis, V.; Kalamas, T.; Stefanidou, M.; Bikiaris, N.D.; Christodoulou, E.; Koumentakou, I.; Karavas, E.; et al. Poly(Lactic Acid)-Based Microparticles for Drug Delivery Applications: An Overview of Recent Advances. Pharmaceutics 2022, 14, 359. [Google Scholar] [CrossRef]
- Tham, C.; Hamid, Z.A.A.; Hanafi, I.; Ahmad, Z. Poly (Vinyl alcohol) in fabrication of PLA micro-and nanoparticles using emulsion and solvent evaporation technique. In Advanced Materials Research; Trans Tech Publications Ltd.: Bäch, Switzerland, 2014; pp. 296–299. [Google Scholar]
- Ekinci, M.; Yeğen, G.; Aksu, B.; İlem-Özdemir, D. Preparation and Evaluation of Poly(lactic acid)/Poly(vinyl alcohol) Nanoparticles Using the Quality by Design Approach. ACS Omega 2022, 7, 33793–33807. [Google Scholar] [CrossRef]
- Nejati, S.; Karimi-Soflou, R.; Karkhaneh, A. Influence of process parameters on the characteristics of oxygen-releasing poly (lactic acid) microparticles: A multioptimization strategy. Polym. Adv. Technol. 2021, 32, 829–841. [Google Scholar] [CrossRef]
- Zhang, M.; Kiratiwongwan, T.; Shen, W. Oxygen-releasing polycaprolactone/calcium peroxide composite microspheres. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 1097–1106. [Google Scholar] [CrossRef]
- Hodge, J.G.; Zamierowski, D.S.; Robinson, J.L.; Mellott, A.J. Evaluating polymeric biomaterials to improve next generation wound dressing design. Biomater. Res. 2022, 26, 50. [Google Scholar] [CrossRef]
- Alven, S.; Peter, S.; Mbese, Z.; Aderibigbe, B.A. Polymer-Based Wound Dressing Materials Loaded with Bioactive Agents: Potential Materials for the Treatment of Diabetic Wounds. Polymers 2022, 14, 724. [Google Scholar] [CrossRef]
- Li, S.; Wang, X.; Chen, J.; Guo, J.; Yuan, M.; Wan, G.; Yan, C.; Li, W.; Machens, H.-G.; Rinkevich, Y. Calcium ion cross-linked sodium alginate hydrogels containing deferoxamine and copper nanoparticles for diabetic wound healing. Int. J. Biol. Macromol. 2022, 202, 657–670. [Google Scholar] [CrossRef]
- Catanzano, O.; D’esposito, V.; Acierno, S.; Ambrosio, M.; De Caro, C.; Avagliano, C.; Russo, P.; Russo, R.; Miro, A.; Ungaro, F. Alginate–hyaluronan composite hydrogels accelerate wound healing process. Carbohydr. Polym. 2015, 131, 407–414. [Google Scholar] [CrossRef]
- Guo, C.; Zhou, Z.; Zhang, S.; Peng, P.; Liu, J.; Yan, Y.; Dong, J. Sulfonated, quaternized, and chlorogenic acid composited sodium alginate hydrogels/Eucommia ulmoides rubber films as in vitro antibacterial wound dressings for accelerating wound healing. Ind. Crops Prod. 2022, 190, 115885. [Google Scholar] [CrossRef]
- PARk, W.H. The effects of exogenous H2O2 on cell death, reactive oxygen species and glutathione levels in calf pulmonary artery and human umbilical vein endothelial cells. Int. J. Mol. Med. 2013, 31, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Hong, G.; Kwon, T.; Lim, J.O. Fabrication of Oxygen Releasing Scaffold by Embedding H2O2-PLGA Microspheres into Alginate-Based Hydrogel Sponge and Its Application for Wound Healing. Appl. Sci. 2018, 8, 1492. [Google Scholar] [CrossRef]
- Lim, D.J.; Jang, I. Oxygen-Releasing Composites: A Promising Approach in the Management of Diabetic Foot Ulcers. Polymers 2021, 13, 4131. [Google Scholar] [CrossRef]
- Sun, X.K.; Li, R.; Yang, X.L.; Yuan, L. Efficacy and safety of topical oxygen therapy for diabetic foot ulcers: An updated systematic review and meta-analysis. Int. Wound J. 2022, 19, 2200–2209. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, M.; Rahimi, R.; Zhou, J.; Jiang, H.; Yoon, C.K.; Maddipatla, D.; Narakathu, B.B.; Jain, V.; Oscai, M.M.; Morken, T.J.; et al. Integrated sensing and delivery of oxygen for next-generation smart wound dressings. Microsyst. Nanoeng. 2020, 6, 46. [Google Scholar] [CrossRef]
- Zehra, M.; Zubairi, W.; Hasan, A.; Butt, H.; Ramzan, A.; Azam, M.; Mehmood, A.; Falahati, M.; Chaudhry, A.A.; Rehman, I.U.; et al. Oxygen Generating Polymeric Nano Fibers That Stimulate Angiogenesis and Show Efficient Wound Healing in a Diabetic Wound Model. Int. J. Nanomed. 2020, 15, 3511–3522. [Google Scholar] [CrossRef]
- Shiekh, P.A.; Singh, A.; Kumar, A. Exosome laden oxygen releasing antioxidant and antibacterial cryogel wound dressing OxOBand alleviate diabetic and infectious wound healing. Biomaterials 2020, 249, 120020. [Google Scholar] [CrossRef]
- Guan, Y.; Niu, H.; Liu, Z.; Dang, Y.; Shen, J.; Zayed, M.; Ma, L.; Guan, J. Sustained oxygenation accelerates diabetic wound healing by promoting epithelialization and angiogenesis and decreasing inflammation. Sci. Adv. 2021, 7, eabj0153. [Google Scholar] [CrossRef]
- Lu, W.; Bao, D.; Ta, F.; Liu, D.; Zhang, D.; Zhang, Z.; Fan, Z. Multifunctional Alginate Hydrogel Protects and Heals Skin Defects in Complex Clinical Situations. ACS Omega 2020, 5, 17152–17159. [Google Scholar] [CrossRef]
- Zheng, Z.; Qi, J.; Hu, L.; Ouyang, D.; Wang, H.; Sun, Q.; Lin, L.; You, L.; Tang, B. A cannabidiol-containing alginate based hydrogel as novel multifunctional wound dressing for promoting wound healing. Biomater. Adv. 2022, 134, 112560. [Google Scholar] [CrossRef]
- Yip, W.L. Influence of oxygen on wound healing. Int. Wound J. 2015, 12, 620–624. [Google Scholar] [CrossRef]
- Tuca, A.C.; Ertl, J.; Hingerl, K.; Pichlsberger, M.; Fuchs, J.; Wurzer, P.; Pfeiffer, D.; Bubalo, V.; Parvizi, D.; Kamolz, L.P.; et al. Comparison of Matrigel and Matriderm as a carrier for human amnion-derived mesenchymal stem cells in wound healing. Placenta 2016, 48, 99–103. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bîrcă, A.C.; Chircov, C.; Niculescu, A.G.; Hildegard, H.; Baltă, C.; Roșu, M.; Mladin, B.; Gherasim, O.; Mihaiescu, D.E.; Vasile, B.Ș.; et al. H2O2-PLA-(Alg)2Ca Hydrogel Enriched in Matrigel® Promotes Diabetic Wound Healing. Pharmaceutics 2023, 15, 857. https://doi.org/10.3390/pharmaceutics15030857
Bîrcă AC, Chircov C, Niculescu AG, Hildegard H, Baltă C, Roșu M, Mladin B, Gherasim O, Mihaiescu DE, Vasile BȘ, et al. H2O2-PLA-(Alg)2Ca Hydrogel Enriched in Matrigel® Promotes Diabetic Wound Healing. Pharmaceutics. 2023; 15(3):857. https://doi.org/10.3390/pharmaceutics15030857
Chicago/Turabian StyleBîrcă, Alexandra Cătălina, Cristina Chircov, Adelina Gabriela Niculescu, Herman Hildegard, Cornel Baltă, Marcel Roșu, Bianca Mladin, Oana Gherasim, Dan Eduard Mihaiescu, Bogdan Ștefan Vasile, and et al. 2023. "H2O2-PLA-(Alg)2Ca Hydrogel Enriched in Matrigel® Promotes Diabetic Wound Healing" Pharmaceutics 15, no. 3: 857. https://doi.org/10.3390/pharmaceutics15030857
APA StyleBîrcă, A. C., Chircov, C., Niculescu, A. G., Hildegard, H., Baltă, C., Roșu, M., Mladin, B., Gherasim, O., Mihaiescu, D. E., Vasile, B. Ș., Grumezescu, A. M., Andronescu, E., & Hermenean, A. O. (2023). H2O2-PLA-(Alg)2Ca Hydrogel Enriched in Matrigel® Promotes Diabetic Wound Healing. Pharmaceutics, 15(3), 857. https://doi.org/10.3390/pharmaceutics15030857











